Abstract
Background
No risk stratification tool has been validated in hospitalised patients with coronavirus disease 2019 (COVID‐19), despite a high rate of intensive care requirement and in‐hospital mortality. We aimed to determine whether the National Early Warning Score (NEWS) at admission can accurately predict in‐hospital mortality and ICU transfer.
Methods
This was a retrospective cohort study from January 24 to April 16, 2020, at Lille University Hospital. All consecutive adult patients with laboratory‐confirmed COVID‐19 who were initially admitted to non‐ICU wards were included. The primary outcome was a composite criterion consisting of ICU transfer or in‐hospital mortality. We evaluated the prognostic performance of NEWS by calculating the area under (AUC) the receiver operating characteristic curve, the optimal threshold value of NEWS, and its association with the primary outcome.
Results
Of the 202 COVID‐19 patients, the median age was 65 (interquartile range 52‐78), 38.6% were women and 136 had at least one comorbidity. The median NEWS was 4 (2‐6). A total of 65 patients were transferred to the ICU or died in the hospital. Compared with patients with favourable outcome, these patients were significantly older, had more comorbidities and higher NEWS. The AUC for NEWS was 0.68 (0.60‐0.77) and the best cutoff value was 6. Adjusted odds ratio for NEWS ≥ 6 as an independent predictor was 3.78 (1.94‐7.09).
Conclusions
In hospitalised COVID‐19 patients, NEWS was an independent predictor of ICU transfer and in‐hospital death. In daily practice, NEWS ≥ 6 at admission may help to identify patients who are at risk to deteriorate.
What’s known
No risk stratification tool has been evaluated in hospitalised patients with coronavirus disease 2019 (COVID‐19) to predict clinical deterioration.
What’s new
A National Early Warning Score (NEWS) ≥6 at admission may help to predict ICU transfer and in‐hospital death.
1. INTRODUCTION
Following the outbreak of coronavirus disease 2019 (COVID‐19) in China, 1 the first confirmed case of COVID‐19 occurred in France on January 24, 2020 and the pandemic spread all over the country from several autochthonous clusters at the end of February. As of the end of October 2020, more than one million cases were confirmed in France with more than 34 000 deaths.
In initial reports, around 25% of patients needed to be transferred to intensive care units (ICU). 2 Mortality is mainly related to acute respiratory failure in COVID‐19 hospitalised patients, especially for those with comorbidities. 3 , 4 , 5 , 6
At admission, risk stratification and early identification of patients with high risk of clinical deterioration remain a major challenge. Although different tools are currently used to evaluate septic patient, none has been specifically assessed in COVID‐19. Amongst these, the National Early Warning Score (NEWS) has been shown to have equivalent or superior prognostic value compared with either quick SOFA or Systemic Inflammatory Response Syndrome (SIRS) criteria to predict clinical status worsening and mortality. 7 , 8 A NEWS ≥ 5 is defined as a key threshold to predict severe clinical deterioration. 9
This study aims to determine whether the NEWS at admission can accurately predict in‐hospital mortality and ICU transfer in hospitalised patients with proven COVID‐19.
2. METHODS
2.1. Study design and participants
This was a retrospective cohort study of all consecutive adult patients with laboratory‐confirmed severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2)infection who were initially admitted to non‐ICU wards of Lille University Hospital between January 24 and April 16, 2020. Patients were identified using the French administrative prospective database PMSI (Programme de Médicalisation des Systèmes d’Informations), which contains all discharge reports from hospitals in France. The following data were extracted from each patient's electronic medical record: NEWS at hospital admission, presence of the following comorbidities: hypertension, diabetes, obesity (BMI ≥ 30 kg/m2), cardiovascular disease, chronic respiratory failure, dialysis, cirrhosis, immunosuppression, pregnancy, and active cancer.
The NEWS is determined from seven simple parameters: respiration rate, oxygen saturation, supplemental oxygen, systolic blood pressure, pulse rate, level of consciousness, and temperature. The score ranges from 0 to 20. 9
2.2. Outcomes
The primary outcome was a composite criterion consisting of ICU transfer or in‐hospital mortality.
ICU admission criteria were (a) increased respiratory frequency ≥ 20/min or decreased arterial PO2 < 60 mmHg or standard oxygen support of 3L/min oxygen therapy as these patients were more likely to rapidly require advanced respiratory support in the context of SARS‐CoV2 infection, (b) septic shock and (c) support for another failing organ system.
Non‐admission in ICU was the sole responsibility of the intensive care specialist and took into account age, number of comorbidities, and physical frailty.
2.3. Laboratory testing
SARS‐CoV2 was detected in nasopharyngeal or low respiratory tract specimens by reverse transcriptase‐polymerase chain reaction (RT‐PCR) as previously described. 10
2.4. Statistical analysis
Categorical variables are expressed as numbers (percentage). Quantitative variables are expressed as median (interquartile range, IQR). Main patient's characteristics at hospital admission were compared according to the primary outcome (ICU transfer and/or in‐hospital mortality) or according to in‐hospital mortality alone, by the Chi‐square test for categorical variables and Mann‐Whitney U test for quantitative variables. We evaluated the prognostic performance of NEWS to predict primary outcome and in‐hospital mortality alone by calculating the area under (AUC) the receiver operating characteristic (ROC) curve and determined the optimal threshold value by maximising the Youden index. Diagnostic values of the optimal threshold value (and its 95% confidence intervals (CIs)) were evaluated by calculating sensitivity, specificity, positive and negative predictive values, diagnostic odds ratio (OR). We further assessed the prognostic performance of NEWS after adjustment for age and number of comorbidities (both factors associated with study outcomes in univariate analyses) using multivariable logistic regression models; adjusted OR were derived from multivariable models as effect size.
No imputation was made for missing data. All statistical tests were performed at the two‐tailed α level of 0.05 using SAS software, release 9.4 (SAS Institute, Cary, NC).
This study was approved by the institutional ethics board of Lille University Hospital (reference number DEC20‐125).
3. RESULTS
3.1. Demographic, clinical characteristics and outcomes of the patients
We identified 202 non‐ICU hospitalised patients with confirmed SARS‐CoV2 infection. Median hospitalisation duration was 8 days (interquartile range 5‐11). A total of 65 (32%) patients was transferred to the ICU or died in the hospital. In 57 cases, the primary outcomes (ICU transfer or in‐hospital mortality) occurred in the first 10 days following admission. Median time before the primary outcome was 2.5 days (interquartile range 1‐5). Most patients were transferred to ICU because of the worsening of respiratory status. Compared with patients with favourable outcome, patients with primary outcome were significantly older (P = .030), had more comorbidities (P = .037), and a higher NEWS (P < .001) (Table 1). Twenty‐three patients died, of whom six after being transferred to ICU. Median age was 84 years (80‐87). Compared with survivours, deceased patients were significantly older (P <.001), had greater number of comorbidities (P < .001), greater proportions of hypertension (P = .002) and cardiovascular disease (P < .001), and higher NEWS (P < .001) (Table 2).
TABLE 1.
Main patient's characteristics at hospital admission in the overall population and according to ICU transfer and/or in‐hospital mortality
| Overall (n = 202) | ICU transfer and/or in‐hospital mortality | P value | ||
|---|---|---|---|---|
| No (n = 137) | Yes (n = 65) | |||
| Age | 65 (52‐78) | 64 (47‐75) | 68 (55‐82) | .030 |
| Female | 78 (38.6) | 58 (42.3) | 20 (30.8) | .11 |
| Comorbidities | ||||
| Hypertension | 87 (43.1) | 54 (39.4) | 33 (50.8) | .13 |
| Diabetes | 35 (17.3) | 24 (17.5) | 11 (16.9) | .92 |
| BMI > 30 kg/m2 a | 32 (18.8) | 19 (16.8) | 13 (22.8) | .35 |
| Cardiovascular disease | 77 (38.1) | 48 (35.0) | 29 (44.6) | .19 |
| Chronic pulmonary disease | 3 (1.5) | 1 (0.7) | 2 (3.1) | NA |
| Dialysis | 2 (1.0) | 1 (0.7) | 1 (1.5) | NA |
| Cirrhosis | 2 (1.0) | 2 (1.5) | 0 | NA |
| Immunodeficiency | 23 (11.4) | 14 (10.2) | 9 (13.8) | .45 |
| At least one comorbidity | 136 (67.3) | 86 (62.8) | 50 (76.9) | .045 |
| Number of comorbidities | 1 (0‐2) | 1 (0‐2) | 2 (1‐2) | .037 |
| Pregnancy | 4 (2.0) | 4 (2.9) | 0 | NA |
| NEWS | 4 (2‐6) | 3 (1‐5) | 6 (3‐9) | <.001 |
| <5 | 115 (56.9) | 90 (65.7) | 25 (38.5) | |
| ≥5 | 87 (43.1) | 47 (34.3) | 40 (61.5) | |
Values are presented as frequency (percentage) or median (interquartile range). Comparisons between the groups were made using Chi‐square or Mann‐Whitney U tests; Values in bold represent statistical significance P ≤ .05.
Abbreviations: BMI, body mass index; NA, non‐applicable.
32 missing values.
TABLE 2.
Main patient's characteristics at hospital admission in the overall population and according to in‐hospital mortality
| In‐hospital mortality | P value | ||
|---|---|---|---|
| No (n = 179) | Yes (n = 23) | ||
| Age | 61 (49‐74) | 84 (80‐87) | <.001 |
| Female | 69 (38.5) | 9 (39.1) | .96 |
| Comorbidities | |||
| Hypertension | 70 (39.1) | 17 (73.9) | .002 |
| Diabetes | 29 (16.2) | 6 (26.1) | .25 |
| BMI > 30 kg/m2 a | 30 (19.9) | 2 (10.5) | .53 |
| Cardiovascular disease | 60 (33.5) | 17 (73.9) | <.001 |
| Chronic pulmonary disease | 1 (0.6) | 2 (8.7) | NA |
| Dialysis | 1 (0.6) | 1 (4.3) | NA |
| Cirrhosis | 2 (1.1) | 0 | NA |
| Immunodeficiency | 20 (11.2) | 3 (13.0) | .73 |
| At least one comorbidity | 115 (64.2) | 21 (91.3) | .009 |
| Number of comorbidities | 1 (0‐2) | 2 (2‐3) | <.001 |
| Pregnancy | 4 (2.2) | 0 | NA |
| ICU transfer | 41 (22.9) | 6 (26.1) | .73 |
| NEWS | 4 (2‐6) | 9 (6‐10) | <.001 |
| <5 | 111 (62.0) | 4 (17.4) | |
| ≥5 | 68 (38.0) | 19 (82.6) | |
Values are presented as frequency (percentage) or median (interquartile range). Comparisons between the groups were made using Chi‐square or Mann‐Whitney U tests; Values in bold represent statistical significance P ≤ .05.
Abbreviations: BMI, body mass index; NA, non‐applicable.
32 missing values
Furthermore, 17 out of the 23 non‐survivours died outside the ICU. These patients showed a tendency to be older, have more comorbidities and higher NEWS (Table S2).
3.2. Prognostic performance of NEWS
On the ROC curve, the AUC for NEWS was 0.68 (95%CI 0.60 0.77) for primary outcome and increased to 0.82 (95%CI, 0.69 to 0.93) for in‐hospital mortality alone (Figure 1). According to the Youden Index, the optimal threshold value was 6 to predict both primary outcome and in‐hospital mortality alone. The diagnostic values for this optimal threshold value are reported in Table 3. In multivariate analysis, NEWS ≥ 6 was an independent predictor of ICU transfer and/or in‐hospital mortality with an odds ratio of 3.78 (1.94‐7.09).
FIGURE 1.
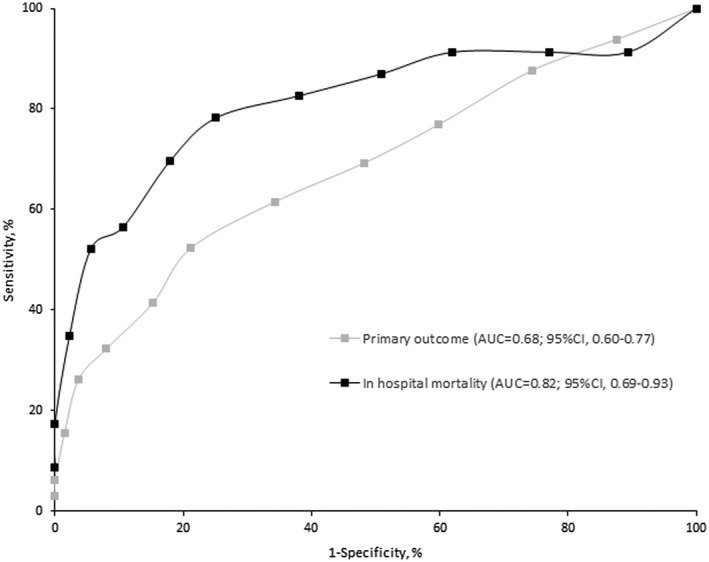
ROC curve of NEWS for predicting the primary outcome (ICU transfer and/or in‐hospital mortality) and in‐hospital mortality alone
TABLE 3.
Diagnostic values of optimal threshold values of NEWS score (≥6) to predict primary outcome and in‐hospital mortality alone
| Diagnostic parameters | Primary outcome | In‐hospital mortality |
|---|---|---|
| Values (95% CI) | Values (95% CI) | |
| Sensitivity | 52.3 (40.2‐64.5) | 78.3 (61.4‐95.2) |
| Specificity | 78.8 (72.0‐85.7) | 74.9 (68.5‐81.3) |
| Positive predictive value | 54.0 (41.7‐ 66.3) | 28.6 (17.4‐ 39.7) |
| Negative predictive value | 77.7 (70.8‐84.6) | 96.4 (93.3‐99.5) |
| Unadjusted OR | 4.09 (2.16‐7.72) | 10.72 (3.76‐30.54) |
| Adjusted OR | 3.78 (1.94‐7.09) a | 16.11 (3.80‐68.35) a |
Abbreviations: CI, confidence interval; OR, odd‐ratio.
Adjusted for age and number of comorbidities.
In multivariate analyses including age and number of comorbidities, NEWS score remained independently associated with primary outcome and in‐hospital mortality (Table S1). In these multivariate analyses, age was also significantly associated with hospital mortality, with a significant increase in AUC to 0.94 (95%CI, 0.90 to 0.99).
Amongst the 139 patients with a predicted favourable outcome (NEWS < 6), 27 patients (22%) were transferred to the ICU and 5 patients (4%) died in the hospital. Sex was significantly associated with ICU transfer and/or in‐hospital mortality (P < .001) (Table S3).
4. DISCUSSION
We found that a higher NEWS at admission was predictive of ICU transfer and in‐hospital mortality in COVID‐19, and the optimal threshold was greater or equal to 6.
Baseline characteristics and our ICU transfer and in‐hospital mortality rates were similar to published data from China. 2 Compared with a large US study, our mortality rate is lower (11.4% vs 21%). 11 This might be explained by lower proportions of hypertension (43.1% vs 56.6%), diabetes (17.3% vs 33.8%), and other comorbidities in our population.
Considering that the median time for ICU transfer or in‐hospital mortality was 2.5 days (IQR 1‐5), our findings highlighted the need for validated risk stratification tools directly at admission. Moreover, considering the specific pathophysiology of COVID‐19 such as happy hypoxemia, relative preservation of lung mechanics and rapid deterioration, 12 relevance of risk stratification tools in this setting has to be evaluated. Previous reports found that older age and high Sequential Organ Failure Assessment (SOFA) score were independent prognosis factors. 3 However, the predictive performance of SOFA was not assessed and this score is difficult to calculate in daily practice, in opposition to NEWS which only includes simple clinical parameters. Although our study assessed only predictive performance of NEWS at admission, repeated measurement of NEWS according to initial severity could further help identify patients at risk of deterioration.
Our results also showed that a majority of non‐survivours died outside the ICU. Amongst these patients, we observed a tendency for older age and higher number of comorbidities that might explain why patients were less likely to be admitted to the ICU despite having a higher NEWS. These patients also presented greater physical frailty according to the physician's general assessment, although not recorded according to a frailty score. Although these patients had withhold of life support, all of them were provided with the maximum and most suitable level of care such as the use of the partial rebreather mask to deliver oxygen up to a flow rate of 15 litres per minute and comfort measures that were available in the general ward. Considering the stressed ICU capacities during the COVID‐19 pandemic, if these patients had less comorbidities and frailty, they would have probably been transferred to ICU as they had higher NEWS. However, this does not modify the predictive value of NEWS for our composite outcome of in‐hospital mortality and/or ICU transfer.
The AUC of NEWS for predicting ICU transfer or mortality in hospitalised COVID‐19 patients was low but nevertheless similar to the AUC of NEWS for predicting ICU admission in community‐acquired pneumonia patients, 0.73 (0.67‐0.78) 13 and NEWS for predicting ICU‐admission in suspected sepsis, 0.64 (0.57‐0.71). 7 Taking into consideration our small number of patients, we identified a best cutoff value of 6 in COVID‐19 patients compared with a traditional threshold of 5. 9 Because of its low sensitivity (52.3%), a lower NEWS might not accurately sort patients at admission. This could be partly explained by the fact that NEWS consists of simple physiological parameters; other factors such as age and comorbidities also have to be taken into account. Age and comorbid conditions did not add information to NEWS score to predict the primary outcome, but age added significant information to NEWS score to predict in‐hospital mortality. Because of the fact that no other stratification tool has been validated to this date in COVID‐19 and the ease of computing NEWS, a higher score may be of value to predict in‐hospital poor outcome.
4.1. Limitations
This study had several limitations including the relatively small number of patients related to its monocentric design and the proportion of missing values for obesity (16%), considering that obesity is a risk factor for COVID‐19 severity. 14 In addition, it might be of interest to evaluate NEWS at regular intervals during the hospital stay. This study also had many strengths: the inclusion of all consecutive patients followed in our centre, standardised data collection, and systematic measure of NEWS at admission.
5. CONCLUSION
In hospitalised COVID‐19 patients, a higher NEWS at admission is independently associated with a worsening of outcome (ICU transfer, in‐hospital death). In daily practice, a NEWS ≥ 6 at the time of admission may help to identify high‐risk patients. For a more accurate prediction, it might be relevant to consider biological and chest CT parameters.
DISCLOSURE
The authors declared no conflict of interest.
INSTITUTIONAL ETHICS BOARD APPROVAL
Lille University Hospital (reference number DEC20‐125).
Supporting information
Table S1‐S3
ACKNOWLEDGEMENTS
Lille Covid‐team: Sophie Panaget MD, Aurélie Dozier MD, Fanny Vuotto MD, Jules Bauer MD, Jules Fleuriet MD, Camille Roger MD, Benoit Gachet MD, Victor Fages MD, Perrine Bortolotti MD, PhD, Marielle Boyer‐Besseyre MD, Anne Prevotat MD, Jean‐François Bervar MD, Laurence Bocket MD, Ilka Engelmann MD, Loïc Andre MD, Edgar Bakhache MD, Patrick Goldstein MD. Affiliation: CHU Lille, F‐59000 Lille, France
Pokeerbux MR, Yelnik CM, Faure E, et al. Lille Covid‐team . National early warning score to predict intensive care unit transfer and mortality in COVID‐19 in a French cohort. Int J Clin Pract. 2021;75:e14121. 10.1111/ijcp.14121
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: $ descriptive study. The Lancet. 2020;395:507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: $ retrospective cohort study. Lancet. 2020;395:1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid‐19 in critically Ill patients in the Seattle region case series. N Engl J Med. 2020;382(21):2012‐2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID‐19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846‐848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goulden R, Hoyle M‐C, Monis J, et al. qSOFA, SIRS and NEWS for predicting in hospital mortality and ICU admission in emergency admissions treated as sepsis. Emergency Med J. 2018;35:345‐349. [DOI] [PubMed] [Google Scholar]
- 8. Brink A, Alsma J, Verdonschot RJCG, et al. Predicting mortality in patients with suspected sepsis at the Emergency Department; a retrospective cohort study comparing qSOFA, SIRS and National Early Warning Score. PLoS One. 2019;14:e0211133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Royal College of Physicians . National Early Warning Score (NEWS): Standardising the Assessment of Acute‐Illness Severity in the NHS. Report of a Working Party. London: Royal College of Physicians; 2012. [Google Scholar]
- 10. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019‐nCoV) by real‐time RT‐PCR. Eurosurveillance. 2020;25:2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City Area. JAMA. 2020;323:2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dhont S, Derom E, Van Braeckel E, Depuydt P, Lambrecht BN. The pathophysiology of ‘happy’ hypoxemia in COVID‐19. Respir Res. 2020;21:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sbiti‐Rohr D, Kutz A, Christ‐Crain M, et al. The National Early Warning Score (NEWS) for outcome prediction in emergency department patients with community‐acquired pneumonia: Results from a 6‐year prospective cohort study. BMJ Open. 2016;6:e011021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195‐1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S3


