Abstract
Due to the COVID‐19 crisis, many scheduled medical and surgical activities have been suspended. This interruption to the healthcare system can negatively affect the diagnosis and management of melanoma. Neglecting melanoma throughout the outbreak may be associated with increased rates of mortality, morbidity, and healthcare expenses. We performed a retrospective review of all dermatological and surgical activity performed in our Melanoma Skin Unit between 23 February 2020 and 21 May 2020 and compared these data with those from the same period in 2019. During the lockdown period, we observed a decrease in dermatologic follow‐up (DFU) (−30.2%) and in surgical follow‐up (SFU) (−37%), and no modification of melanoma diagnosis (−3%). Finally, surgical excisions (SE) (+ 31.7%) increased, but sentinel lymph node biopsy (SLNB) (−29%) and lymph node dissections(LND) (−64%) decreased compared to the same period in 2019. Our experience supports the continuation of surgical and diagnostic procedures in patients with melanoma during the COVID‐19 pandemic. Surgical and follow‐up procedures for the diagnosis and treatment of melanoma should not be postponed considering that the pandemic is lasting for an extended period.
Keywords: COVID‐19, melanoma, melanoma management, melanoma surgical management, skin cancer, surgery
1. INTRODUCTION
The COVID‐19 pandemic and all of the consequences related to it affect the reorganization of health resources, including the cancellation of all elective surgery. to redistribute resources by freeing health personnel and beds. 1 During the 12‐week peak, more than 28 million procedures were canceled or postponed. In order to reduce the effects on cancer outcomes and surgical morbidity 2 it is necessary to establish methods for crisis management, according to guidelines about the optimal timing and type of surgery. 3 The interruption of the healthcare system can negatively affect the diagnosis and management of melanoma, increasing rates of mortality, morbidity, and healthcare expenses. 4
2. METHODS
The dermatological and surgical activity performed in our Melanoma Skin Unit between 23 February 2020 (ie, the date of the first Italian act to constrain the COVID‐19 epidemic) and 21 May 2020 (ie, the first day without new COVID‐19 cases in our region), was retrospectively reviewed and compared with that of the same period in 2019. In this analysis, we included the dermato‐oncologic or surgical visits and surgical procedures: surgical excisions (SE), wide excisions (WE), sentinel lymph node biopsies (SLNB), lymph node dissections (LND), electrochemotherapy (ECT), and hyperthermic isolated limb perfusion (HILP).
3. RESULTS
The comparison between the activities in 2020 and 2019 is shown in Table 1 and Figure 1. Melanoma diagnoses were almost the same (64 in 2020 and 66 in 2019; −3%). However, clinical activity decreased during the lockdown except for SEs, which dramatically increased (+31.7%), with 636 SEs during the lockdown in 2020 and 483 in the same period in 2019. Dermatologic follow‐up (DFU) dropped by 2196 in 2019 to 1533 in 2020 (−30.2%), whereas SFUs by 1073 in 2019 to 675 in 2020 (−37%). SLNBs decreased from 31 in 2019 to 22 in the same period of 2020 (−29%), but considering the pT at diagnosis, in pT4a and pT4b group, the decrease was the lowest (1.5%; Table 2). TheLNDs dropped from 14 to 5 (−64%), the number of ECTs remained unchanged (two in 2019 and two in 2020), whereas that of HILP fell from 3 to 0 (−100%).
TABLE 1.
Comparison between 2020 and 2019 activities
| 2020 | 2019 | Difference | % | |
|---|---|---|---|---|
| SE | 636 | 483 | −153 | 31.70% |
| SFU | 675 | 1.073 | −398 | −37.10% |
| DFU | 1.533 | 2.196 | −663 | −30.20% |
| WE | 64 | 66 | 2 | −3% |
| SLNB | 22 | 31 | 9 | −29% |
| LND | 5 | 14 | 9 | −64% |
| ECT | 2 | 2 | 0 | 0% |
| ILP | 0 | 3 | 3 | −100% |
FIGURE 1.
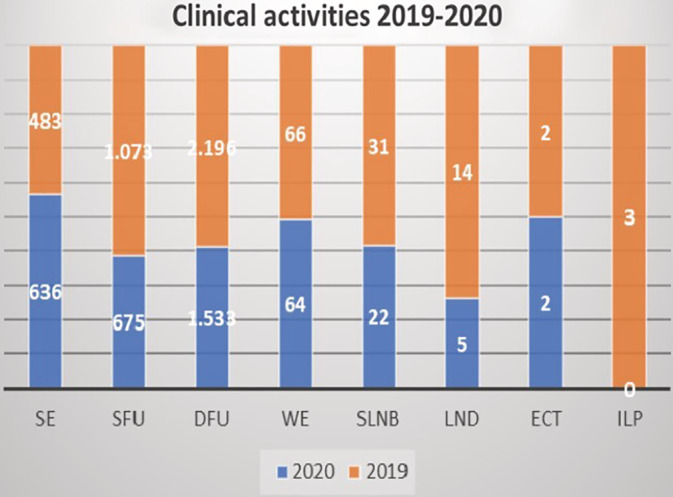
Comparison of clinical activities between 2019 and 2020
TABLE 2.
SLNB decreasing in 2020
| T | n | % | SLNB performed in 2020 | SLNB to be performed in 2020 | difference | % |
|---|---|---|---|---|---|---|
| pT1a | 38 | 58 | 1 | 0 | 0 | 0.0 |
| pT1b | 2 | 3 | 2 | 2 | 0 | 0.0 |
| pT2a | 11 | 17 | 9 | 11 | −2 | 3.0 |
| pT2b | 1 | 2 | 1 | 1 | 0 | 0.0 |
| pT3a | 3 | 5 | 3 | 3 | 0 | 0.0 |
| pT3b | 2 | 3 | 1 | 2 | 0 | 0.0 |
| pT4a | 3 | 5 | 2 | 3 | −1 | 1.5 |
| pT4b | 4 | 6 | 3 | 4 | −1 | 1.5 |
| pTxN2c | 1 | 2 | 0 | 0 | 0 | 0.0 |
| Total | 65 | 100 | 22 | 26 | ‐4 | 6.2 |
4. DISCUSSION
During the first wave COVID‐19 pandemic, there has been a decrease in patient screening in melanoma and other types of cancer. 5 The lockdown circumstances resulting in inadequate melanoma care conditions could increase the number of advanced stage melanoma cases and healthcare expenses. 6 In patients with stage I to stage III melanoma, a delay of more than 2 months from diagnosis to final surgical management compared to patients treated within 2 months of diagnosis leads to significantly worse survival. 7 Similarly, a delay of more than 30 days from biopsy to surgery is associated with poorer survival for patients with early melanoma 9 , 10 . A study that used the melanoma growth rate (ROG) to estimate the effect of the COVID‐19 lockdown on melanoma thickness and prognosis showed that the diagnostic delay determines an upstaging in the T of melanoma and consequently a worse prognosis. 10 During the Italian lockdown, there were no shared and consolidated treatment guidelines, and postponing most surgical procedures risked diagnosing melanoma incorrectly 12 , 13 . In our series, the number of SEs increased, because major elective surgery was postponed, and all of the surgeons, free also from normal outpatient visits were moved to minor surgery in our oncologic referral center. Furthermore, all of the SEs not performed in the local clinics that were closed because of the lockdown, were carried out in our tertiary level hospital. The decrease of the SLNBs that were to be performed as per protocol was 6.2%. Of the four patients who did not perform the procedure, the T4b patients were both 90 years old. One of the two T2a patients was 80; therefore, it was decided to surgically treat them only with WEs. The decision of surgical management after positive SLNB was not impacted by the pandemic, but it has followed the previous guidelines and protocols in the same unit and reflects the change in management guidelines between 2019 and 2020. Our data regarding DFU are similar to other studies, which show a decrease of 30% in DFU visits but differ regarding new diagnoses and surgical management that were similar and increased, respectively, in the lockdown period. 13 In our case history, there was a decrease of 30% in DFU and 37% in SFU follow‐up visits due to patient cancellation. During the COVID‐19 lockdown, the cancellation of clinical procedures and activities was facilitated when associated with uncertainty about the intent of the treatment. 14 Postponing consultation and follow‐up may cause undetected or late detected skin cancers with higher morbidity and mortality. In our opinion, the patients' feeling of safety must be strengthened to avoid diagnostic delay. Not decreasing primary asportations is essential, perhaps aggregating them in cancer centers outside COVID hospitals to avoid a decrease in visits caused by patient cancellations, which would cause a decrease in removals and therefore new diagnoses. This is imperative in the case of a prolonged COVID‐19 pandemic. Our data are in line with those of a recent UK study 15 showing that the detection rates of melanoma were higher during the lockdown than before the pandemic.
In conclusion during the COVID‐19 lockdown, we had an increase in outpatient clinical activity and no modification in the number of melanomas diagnosed during the lockdown. Our experience supports the need to maintain surgical and diagnostic procedures in patients with melanoma during the lockdown.
Surgical and follow up procedures for the diagnosis and treatment of melanoma should not be postponed considering that the pandemic is lasting for an extended period.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
Angela Filoni, Paolo del Fiore, Mauro Alaibac, Rocco Cappellesso, Alessandra Buja, and Simone Mocellin conceptualized the study. Angela Filoni and Paolo del Fiore conducted the literature search. Romina Spina, Nick Salimian, Alessandra Collodetto, and Mattia D'Amico collected data. Saveria Tropea, Marco Rastrelli, Francesco Russano, Luigi Dall'Olmo, Antonella Vecchiato, and Carlo Riccardo Rossi reviewed the manuscript. Angela Filoni, Paolo del Fiore, and Luigi Dall'Olmo drafted the article with input from all authors. All authors read and approved the final manuscript.
ACKNOWLEDGMENT
The authors thank “Piccoli Punti ONLUS”, Mr. Giuseppe Valentini and “Fondazione Lucia Valentini Terrani” for the long‐lasting support.
Filoni A, Del Fiore P, Cappellesso R, et al. Management of melanoma patients during COVID‐19 pandemic in an Italian skin unit. Dermatologic Therapy. 2021;34:e14908. 10.1111/dth.14908
Angela Filoni, Paolo del Fiore, Rocco Cappellesso, and Alessandra Buja have contributed equally to this study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Ives J, Huxtable R. Surgical ethics during a pandemic: moving into the unknown? Br J Surg. 2020;107:1089‐1090. 10.1002/bjs.11638. [DOI] [PubMed] [Google Scholar]
- 2. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440‐1449. 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Spinelli A, Pellino G. COVID‐19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107:785‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zanus G, Romano M, Santoro GA, Rossi S, Grossi U. Impact of COVID‐19 on urgent surgical activity. BJS. 2020;107:e414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buja A, Rivera M, de Polo A, et al. Real‐world data for direct stage‐specific costs of melanoma healthcare. Br J Dermatol. 2020;183(1):171‐172. [DOI] [PubMed] [Google Scholar]
- 6. London JW, Fazio‐Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID‐19 pandemic on cancer‐related patient encounters. JCO Clin Cancer Inform. 2020;4:657‐665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guhan S, Boland G, Tanabe K, et al. Surgical delay and mortality for primary cutaneous melanoma. J Am Acad Dermatol. 2020;S0190‐9622(20)32279‐9. 10.1016/j.jaad.2020.07.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Basnet A, Wang D, Sinha S, Sivapiragasam A. Effect of a delay in definitive surgery in melanoma on overall survival: a NCDB analysis. J Clin Oncol. 2018;36:e21586. [Google Scholar]
- 9. Elmas ÖF, Demirbaş A, Düzayak S, Atasoy M, Türsen Ü, Lotti T. Melanoma and COVID‐19: a narrative review focused on treatment. Dermatol Ther. 2020;33:e14101. 10.1111/dth.14101. [DOI] [PubMed] [Google Scholar]
- 10. Conic RZ, Cabrera CI, Khorana AA, Gastman BR. Determination of the impact of melanoma surgical timing on survival using the National Cancer Database. J Am Acad Dermatol. 2018;78:40‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tejera‐Vaquerizo A, Nagore E. Estimated effect of COVID‐19 lockdown on melanoma thickness and prognosis: a rate of growth model. J Eur Acad Dermatol Venereol. 2020;34(8):e351‐e353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Caliendo V, Picciotto F, Quaglino P, Ribero S. COVID infection and sentinel lymph node procedure for melanoma: management in a dermato‐oncology center in a high‐risk pandemic area. Dermatol Ther. 2020;e13536.33(4):e13536 10.1111/dth.13536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rossi CR, Mocellin S, Campana LG, et al. Prediction of non‐sentinel node status in patients with melanoma and positive sentinel node biopsy: an Italian melanoma intergroup (IMI) study. Ann Surg Oncol. 2018;25(1):271‐279. 10.1245/s10434-017-6143-5. [DOI] [PubMed] [Google Scholar]
- 14. Barruscotti S, Giorgini C, Brazzelli V, et al. A significant reduction in the diagnosis of melanoma during the COVID‐19 lockdown in a third‐level center in the northern Italy. Dermatol Ther. 2020;33:e14074. 10.1111/dth.14074 [DOI] [PubMed] [Google Scholar]
- 15. Younger E, Smrke A, Lidington E, et al. Health‐related quality of life and experiences of sarcoma patients during the COVID‐19 pandemic. Cancers (Basel). 2020;12(8):e2288. 10.3390/cancers12082288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schauer AA, Kulakov EL, Martyn‐Simmons CL, Bunker CB, Edmonds EVJ. Melanoma defies 'lockdown': ongoing detection during COVID‐19 in Central London. Clin Exp Dermatol. 2020. 45(7):900 10.1111/ced.14324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


