Abstract
Aims
The COVID‐19 pandemic is the most important public health problem in 2020. Millions of people have been infected or died because of the outbreak. We know the common symptoms of the disease such as fever and cough. However, all symptoms and features of COVID‐19 are still were not known. We aimed to evaluate the change in lower urinary tract symptoms (LUTS) after COVID‐19 in men.
Methods
We prospectively assessed 94 patients with COVID‐19 during hospitalisation. The patients were divided into two groups according to age, that being over and under age 50. IPSS scores of all patients were enrolled. Additionally, we compared the scores with pre‐COVID‐19 values.
Results
LUTS scores were found to be increased in elderly patients. Additionally, the severity of the disease did not correlate with LUTS scores.
Conclusion
LUTS may be one of the symptoms of COVID‐19 in some patients. Elderly patients with increased LUTS should be evaluated for COVID‐19 when the reason unclear.
What’s known?
COVID‐19 is a new disease and there are many things still unknown about it. The most known symptoms are clear signs as cough, fever, respiratory infections.
What’s new?
Our results suggest that urinary irritative symptoms may occur regardless of COVID‐19 severity. Therefore, elderly male patients with subclinical or nonspecific symptoms should also be evaluated for COVID‐19 when presenting with increased lower urinary tract symptoms of no apparent cause.
1. INTRODUCTION
The outbreak of Coronavirus Disease‐19 (COVID‐19) is a global public health problem nowadays. COVID‐19 was identified in Wuhan, China in late 2019 and spread to the whole world within a few months. 1 The WHO (World Health Organisation) announced the outbreak of COVID‐19 as a pandemic on 11th March 2020. 2 At the time of writing, COVID‐19 had infected more than 60 million people resulting in almost 1.5 million deaths. 3 Many countries declared national emergencies and closed their borders to prevent the outbreak from spreading. The governments imposed strict rules on social life areas in many countries. Many working places and schools were closed, and people continued their lives at home.
COVID‐19 is a novel virus and there is limited data about it. All of the symptoms of the disease are still unknown. 4 The diagnosis of COVID‐19 occasionally may be difficult because of unclear or subclinical symptoms. 5 Patients with severe COVID‐19 present with predominantly cough, fever, and other respiratory symptoms. However, some studies also have reported serious urinary complications. 6 COVID‐19 patients, mostly presenting with classical urological symptoms, should not be overlooked nowadays. 7 Urinary frequency is one of the most common symptoms in urological disease. However, Mumm et al reported that urinary frequency is a common symptom in COVID‐19 patients. 8 We noticed that hospitalised COVID‐19 patients suffered from low urinary tract symptoms (LUTS). Patients have especially reported increased dysuria symptoms after infection. Therefore, we aimed to evaluate the effect of COVID‐19 on LUTS in men in this study.
2. MATERIALS AND METHODS
We prospectively evaluated male patients hospitalised for more than 3 weeks because of COVID‐19. This study protocol was certified by the Local Ethics Committee and performed in accordance with the Declaration of Helsinki. Written detailed informed consent was obtained from all subjects. Patients whose COVID‐19 infections were confirmed with the real‐time reverse transcriptase‐polymerase chain reaction test were included in the study. Patients who received massive intravenous hydration, drug using affecting urine frequency, benign prostatic hyperplasia or prostate cancer treatment or previously had prostate and urethral surgery were excluded from the study. Additionally, urine analysis was performed for all patients to exclude urinary tract infections.
The International Prostate Symptom Score (IPSS) was used to evaluate patients' symptoms. Patients were questioned to rate their previous situation regarding the COVID‐19 outbreak. The current scores and pre‐COVID‐19 scores of the patients were recorded. The patients were divided into two groups, over 50 and under 50 years of age. The current and previous scores were compared within each group separately.
One of the most common symptoms in patients with severe COVID‐19 is pneumonic infiltration on computed tomography (CT). We categorised the CT images of COVID‐19 patients into three score groups. 9 Score 1 means only one side lung was infected minimally. Score 2 means bilateral lung was infected minimal or moderately. Score 3 means massive infection of the bilateral lung. We analysed the correlation between IPSS scores and CT scores of all patients.
The data were analysed with the Statistical Package for Social Sciences (SPSS) version 22.0™ (IBM Corporation). The distribution of the variables was measured using the Shapiro‐Wilk test. The scores between the two groups were compared with performing the Wilcoxon signed rank test. Spearman's test was used to evaluate correlation. All P values were two‐tailed and a P < .05 was considered statistically significant.
3. RESULTS
We assessed a total of 94 participants. The quantity of patients in the under age 50 group was 32 and in over 50 age group 62. IPSS of all patients is presented in Table 1. The mean age of all patients was 57.5 ± 16.6 years and mean body mass index was 26.2 ± 4.1 kg/m2.
TABLE 1.
IPSS scores of all patients
| <50 age (n:32) | >50 age (n:62) | |
|---|---|---|
| IPSS score before COVID‐19 | 1.3 ± 1.6 | 5.1 ± 4.1 |
| IPSS score during COVID‐19 | 1.5 ± 1,6 | 9 ± 6.4 |
| P = .053 | P < .0001 |
In the under 50 age group, the IPSS score before COVID‐19 was 1.3 ± 1.6 and during COVID‐19 it was 1.5 ± 1.6. There was no statistically significant change in the scores (P = .053). In the over 50 age group, the IPSS score before COVID‐19 was 5.1 ± 4.1 and during COVID‐19 it was 9 ± 6.4. The IPSS score during COVID‐19 was statistically significantly higher than the previous score (P < .0001). Scattering chart of CT scores and IPSS scores was presented in Figure 1. According to correlation analysis, there was no correlation between IPSS scores and CT scores of all patients (P = .485).
FIGURE 1.
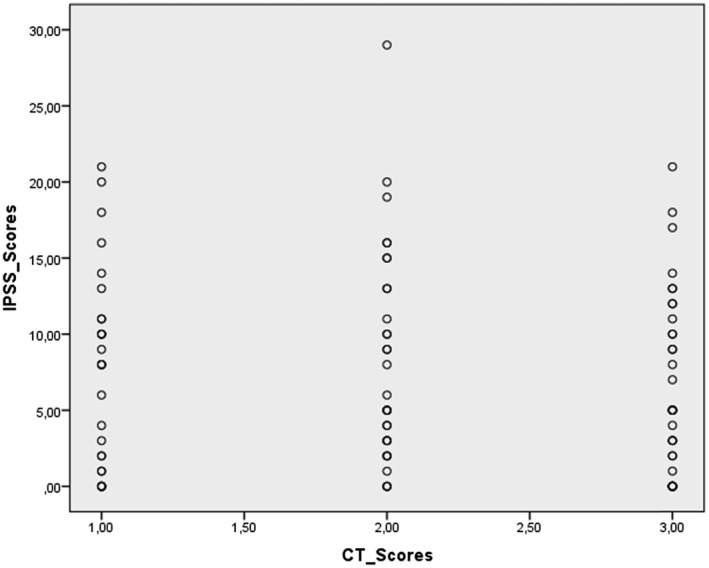
Scattering chart of CT scores and IPSS scores; there is no correlation between CT scores and IPSS scores
4. DISCUSSION
The COVID‐19 outbreak is the most important disease worldwide nowadays. Even the strong healthcare systems of many countries have faced a major crisis. Almost all clinicians have worked together to get through this crisis, regardless of department. Daily urology practice has changed in many countries because of the lack of a sufficient number of clinicians and hospitals, and the danger of disease spread. 10 Many urologists have worked in COVID‐19 clinics during this period. We have noticed that some patients with COVID‐19 suffered from dysuria and irritative urinary symptoms. To our knowledge, there is limited study in the literature investigating the effect of COVID‐19 on LUTS. Therefore, we prospectively designed this study and increased LUTS was found in elderly COVID‐19 patients.
Clinical symptoms of COVID‐19 are mostly related to the respiratory system. The most common of them are fever, cough, and dyspnea. Although all details are unclear, the known infectious pathways in COVID‐19 are nasal, nasopharyngeal, and lower respiratory secretions. 11 There is no certain data supporting that urine is a pathway for the transmission of virus. Recent studies have reported that COVID‐19 is found in human and animal urine. 12 , 13 Moreover, Wang et al could not confirm the indication of the virus in urine samples of patients. 11 Despite these contradictory studies, the urinary frequency was reported as a common symptom of COVID‐19 in a recent study. 8 Furthermore, Kaya et al reported that LUTS might be one of the initial symptoms of COVID‐19. 14
According to our study, LUTS was found statistically significantly increased in elderly patients after COVID‐19 infection. This increase was not apparent in younger patients. We consider that these results are related to the distribution of ACE(Angiotensin‐Converting Enzyme)2 receptors and the different age groups of patients. COVID‐19 has a strong binding affinity to ACE2 receptors. Therefore, organs with high ACE2 receptor expression are at higher risk for COVID‐19. Zou et al demonstrated a cut‐off value for the proportion of ACE2 expression in organs. They interpreted expression rates higher than 1% as high risk for COVID‐19. Bladder urothelium is a high‐risk group for viral invasion with a 2.4% ACE2 expression rate. 15 The viral invasion may lead to endotheliitis in endothelial cells. 16 Irritative symptoms may occur as a result of bladder mucosal damage. Therefore, one of the reasons for increased IPSS after COVID‐19 may be that the urinary bladder is a high‐risk group according to ACE2 expression. We consider the other reasons for increased the symptom scores is the age of patients. Many studies indicated that COVID‐19 infection causes more severe illness in elderly patients. 17 , 18 , 19 The reason for this may be related to comorbidities and weak immunity defence of elderly patients.
Patients with severe infection have more dramatic lung involvement. Therefore, patients have received different treatments according to the COVID‐19 severity such as hydroxychloroquine, azithromycin, and favipiravir molecules in our study. According to correlation analyses, there was no correlation between IPSS score and CT degree. These results show us that the IPSS scores of the patients are not related to the received type of drug or the severity of the disease.
There are a couple of limitations to our study. First, a small number of patients was included in the study. Second, we did not evaluate viral RNA in urine samples to demonstrate bladder COVID‐19 invasion. We used urine analysis instead of urine culture. However, cases with any leukocyte or nitrite positive were excluded. Finally, the stress status and mood of the patients may have affected their pre‐COVID‐19 IPSS scores. We did not use a stress scale for this.
5. CONCLUSION
It has been almost 8 months since the pandemic was announced and we may be still at the early phase of the outbreak. All features of COVID‐19 are still uncertain. It is important to determine patients with subclinical or non‐specific symptoms to prevent or slow the spreading of the virus. Urinary irritative symptoms may occur regardless of COVID‐19 severity. Therefore, patients who have presented with LUTS should be evaluated also for COVID‐19 when the reason is unclear. However, prospective large studies are necessary to validate our findings.
DISCLOSURE
The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Concept—AO; Design—AO; Supervision—AO; Resources—OC; Materials—MO; Data Collection and/or Processing—MUK, MO, ME; Analysis and/or Interpretation—MUK, MO; Literature Search—OC; Writing Manuscript—OC; Critical Review—AO.
INFORMED CONSENT
Written consent was obtained.
ETHICS COMMITTEE APPROVAL
Istanbul Prof. Dr. Cemil Tascioglu city Hospital ethics committee approved the study in 16/06/2020. Approval no is 230.
Can O, Erkoç M, Ozer M, Karakanli MU, Otunctemur A. The effect of COVID‐19 on lower urinary tract symptoms in elderly men. Int J Clin Pract. 2021;75:e14110. 10.1111/ijcp.14110
REFERENCES
- 1. Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol. 2020;17:251‐253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Coronavirus disease 2019 (COVID‐19): situation report, 51. World Health Organization. 2020. https://apps.who.int/iris/handle/10665/331475. Accessed March 11, 2020. [Google Scholar]
- 3. World Health Organization . COVID‐19 weekly epidemiological update, 24 November 2020. World Health Organization. 2020. https://apps.who.int/iris/handle/10665/337127. Accessed November 22, 2020. [Google Scholar]
- 4. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 Hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. J Am Med Assoc. 2020;323:1061‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Song JY, Yun JG, Noh JY, Cheong HJ, Kim WJ. Covid‐19 in South Korea ‐ Challenges of subclinical manifestations. N Engl J Med. 2020;382:1858‐1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li Z, Wu M, Guo J, et al. Caution on kidney dysfunctions of 2019‐nCoV patients. medRxiv. 2020. 10.1101/2020.02.08.20021212 [DOI] [Google Scholar]
- 7. Sighinolf MC, Rocco B, Mussini C. COVID‐19: importance of the awareness of the clinical syndrome by urologists. Eur Urol. 2020;78:e40‐e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mumm JN, Osterman A, Ruzicka M, et al. Urinary frequency as a possibly overlooked symptom in covid‐19 patients: does SARS‐CoV‐2 cause viral cystitis? Eur Urol. 2020;S0302–2838:30353‐30355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Prokop M, van Everdingen W, van Rees VT, et al. CO‐RADS: a categorical CT assessment scheme for patients suspected of having COVID‐19‐definition and evaluation. Radiology. 2020;296(2):E97‐E104. 10.1148/radiol.2020201473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chan MC, Yeo SEK, Chong YL, Lee YM. Stepping forward: urologists’ efforts during the COVID‐19 outbreak in Singapore. Eur Urol. 2020;78:e38‐e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang W, Xu Y, Gao R, et al. Detection of SARS‐CoV‐2 in Different types of clinical specimens. J Am Med Assoc. 2020;323:1843‐1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ling Y, Xu SB, Lin YX, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). 2020;133:1039‐1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim YI, Kim SG, Kim SM, Kim EH, Park SJ, Yu KM. Infection and rapid transmission of SARS‐CoV‐2 in ferrets. Cell Host Microbe. 2020;27:704‐709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaya Y, Kaya C, Kartal T, Tahta T, Tokgöz VY. Could LUTS be early symptoms of COVID‐19. Int J Clin Pract. 2021;75(3):e13850. [DOI] [PubMed] [Google Scholar]
- 15. Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single‐cell RNA‐seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019‐nCoV infection. Front Med. 2020;14:185‐192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID‐19. Lancet. 2020;395:1417‐1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li P, Chen L, Liu Z, et al. Clinical features and short‐term outcomes of elderly patients with COVID‐19. Int J Infect Dis. 2020;97:245‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]


