Abstract
Background
Asia has been at the forefront of leveraging big data and digital technologies to strengthen measures against SARS-CoV-2 spread. Understanding strengths and challenges of these new approaches is important to inform improvements and implementation. In this review, we aimed to explore how these tools were utilized in four countries in Asia to facilitate COVID-19 preventative control measures.
Methods
We conducted a pragmatic review of English-language literature and web-based information in Pubmed, MedRxiv, national and international public health institution websites and media sources between 1st January-3rd August 2020 to identify examples of big data and digital technologies to facilitate COVID-19 preventative control measures in Taiwan, South Korea, Hong Kong, and Singapore. Results were summarized narratively by common technological themes, and examples of integration highlighted.
Results
Digital tools implemented included real-time epidemiological dashboards, interactive maps of case location, mobile apps for tracing patients’ contacts and geofencing to monitor quarantine compliance. Examples of integration of tools included linkage of national health and immigration databases to identify high-risk individuals in Taiwan, and the use of multiple digital surveillance sources to map patients’ movements in South Korea. Challenges in balancing privacy and public good were identified.
Conclusions
Digital technologies have facilitated and strengthened traditional public health measures for prevention of SARS-CoV-2 spread in Asia. Resolving issues around privacy concerns would improve future preparedness, implementation speed and uptake of digital measures. The significant technological advances and lessons learned can be adopted or adapted by other countries to ensure public health preparedness for future waves of COVID-19 and other pandemics.
Keywords: Digital health, public health, COVID-19, data analytics, epidemiology, individual rights, mitigation, isolation, quarantine
Introduction
Coronavirus disease 2019, or ‘COVID-19’, caused by the severe acute respiratory syndrome (SARS)-CoV-2 coronavirus, has spread rapidly across the globe since it was first identified in December 2019. Without vaccines or widely available treatment options, non-pharmaceutical interventions were the only available tools for reducing human-to-human transmission early in the pandemic, and still remain essential for minimising the ongoing burden until herd immunity can be achieved. Non-pharmaceutical interventions include measures such as isolation of confirmed cases, social distancing, community containment measures, and quarantine.
Our experience in the past from the Spanish flu (1918), Asian influenza (1957), Hong Kong influenza (1968), swine flu (2009), SARS (2003), and Middle East respiratory syndrome (MERS) epidemics and pandemics, has provided us with some key lessons, which includes: the need to act quickly (early detection of cases and early implementation of quarantine/lockdown measures are vital); the fact that aggressive quarantining measures may be necessary, especially if there are large numbers of cases and asymptomatic transmission is possible; the need to obtain the public’s consent to measures that limit their freedom or compromise their privacy; and the need for international cooperation and coordination, including guidance on how to balance the interests of public health and those of trade and economics.1–5 The rapid spread of COVID-19 indicates that, in general, these lessons may not have been timeously implemented. If measures are implemented too late or are breached, their effectiveness may be limited. Adherence to government-imposed restrictions will also influence effectiveness. Populations will be unlikely to adhere to restrictive measures over long periods unless their ‘buy-in’ is achieved through a clear understanding of the need for the rules and the consequences of breaking them.
The non-pharmaceutical response to COVID-19 greatly differs from earlier pandemics due to the tremendous advances in digital technologies over the last decade, together with the availability of data from the growing number of smartphones in use (smartphone ownership grew from an estimated 172 million in 2009 to 1·56 billion forecast for 2020).6 In recent years, developments in data analytics have made it possible to analyse big data and convert them into useful information, virtually in real-time. This is vital from an epidemic perspective, where rapid decisions are required, often on the basis of incomplete raw data. Digital technology can facilitate the implementation and monitoring of measures to prevent epidemic spread. Technology has also been leveraged for improving diagnosis and treatment.7–9 However, prevention of transmission is of utmost importance in the pandemic context, therefore this review focusses on how application of big data and technology can be used to strengthen preventative rather than diagnostic or therapeutic measures.
Several Asian countries have been at the forefront of leveraging big data and digital technologies as part of a package of measures to successfully control the first waves of COVID-19 and to maintain low levels of ongoing transmission.10 This experience could hold useful lessons for other countries and future pandemics.
Challenges to overcome
During the early part of the pandemic when vaccines or treatment options were yet to be identified, non-pharmacological mitigation measures were the cornerstone of the pandemic response. Given the rapid spread of SARS-CoV-2 globally, due to high transmissibility paired with extreme globalisation in recent decades, it was clear that traditional approaches to contain the pandemic might not be adequate. Following experience from past epidemics (e.g. SARS), many countries in Asia quickly understood the magnitude of this contagion and acted with latest digital tools that they could bring together. Designing and implementation of these digital technologies and tools had to face and overcome various roadblocks before proving their benefits.11
Use of digital methods firstly raises policy related questions around sovereignty and privacy, especially when a government is collecting data with regards to travel history, credit card spending, CCTV footages, movements and contacts of a person; and in some cases the measures also restrict the mobility of an individual posing challenges to freedom and the basic rights of living in a country. Other barriers that can derail digital adaption include acceptance to implement the technology, adequate digital infrastructure, and publication without breaching privacy. Digital tools when designed and executed well, have the potential to transform the way we gain insights in public health to make swift informed decisions at times of emergency.12
In this review, we aimed to explore how big data and digital technology were leveraged in four countries in Asia to facilitate the implementation of COVID-19 preventative control measures. First, we explore specific digital technologies and their implementation in different countries, followed by a deep-dive in to two country-level examples of how different technologies have been integrated to provide a robust response to COVID-19 control. Finally, we consider advantages and disadvantages of the technologies, and how such measures could be implemented elsewhere to help control the COVID-19 pandemic and future outbreaks.
Methods
Identification of countries
In our study, inclusion criteria for country selection were 1) countries in East and South East Asia, 2) reported imported cases of SARS-CoV-2 during January 2020, and 3) use of descriptive data analytics and digital technologies to facilitate their non-pharmacological preventative public health measures. Included countries were Taiwan, The Republic of Korea [hereafter referred to as South Korea], Hong Kong, and Singapore. For this analysis, Hong Kong and Taiwan were considered separately from China as they each have an autonomous public health decision-making body. We also selected two examples (Taiwan and South Korea) with particularly interesting integration of several new technologies, for a more detailed discussion.
Selection of digital interventions
In this review we focused on the use of digital technologies and big data as measures to prevent spread. Although many other digital tools were developed for diagnostic and therapeutic applications (e.g. machine learning), these were considered out of scope for this review, which focusses exclusively on preventative measures.
Data analytics refers to a broad category of applications and processes for gathering, accessing, and analysing information.13 Data analytics in healthcare is described in four categories namely: descriptive, diagnostic, predictive and prescriptive. From a public health point of view descriptive analytics is most commonly used. This is also known as dashboarding. It describes the situation with existing datapoints thereby providing various perspectives to explore the data.14 The term ‘big data’ is used to describe a massive volume of structured and unstructured data, which is difficult to capture, store, manage, and analyse using traditional database and software techniques.12,14,15
Search methodology
We screened official public COVID-19 information, from global international institutions (e.g. WHO), national public health institutions, Ministry of Health websites for each country, COVID-19 related press reports and news media websites on a daily basis, and extracted information from relevant reports and tables according to available public updates.
To complement official information, we conducted a non-systematic literature review of English language peer-reviewed articles using Pubmed with the following mesh terms: (“covid 19” OR sars-cov-2 OR “severe acute respiratory syndrome coronavirus 2” OR “sars related coronavirus” OR coronavinirae OR coronavirus) AND cases AND (asia OR “south korea” OR Singapore OR taiwan OR “hong kong”) AND mitigation AND (digital OR technology OR “digital technology” OR tools) AND (data OR “big data”) AND (“data science” OR analytics OR “data analytics”) AND “public health”. Peer-reviewed articles were selected according to the country and relevance of the topic compared to the research objectives. We did not include studies using modelling techniques. As COVID-19 has been evolving rapidly in the first few months of the epidemic we also searched relevant articles presenting epidemiological parameters from observational studies using MedRxiv, the pre-print server for health sciences. In addition, we screened main local newspapers for complementary information in the context of measures implemented and concerns at the national level. The period of search and data collection lasted from 01 January to 03 August 2020. All relevant articles were read, and the results were summarised narratively by country and by common themes/technologies across the countries. The articles cited are those that provided the most pertinent and/or up-to-date information on the examples chosen.
The common technological themes found among the four countries in this review include descriptive data analytics methods to produce interactive data dashboards showing information about the spread of the pandemic in their respective countries, and the more advanced interactive country maps with overlaid COVID-19 case data, showing a clear picture of the geographical location and spread of the cases. All countries covered in the study used mobile phone applications to facilitate manual contact tracing, isolations/quarantines using Bluetooth and geofencing technologies. Additionally, Taiwan and Korea designed unique digital tools integrating several technologies and databases together, like the use of big data, data analytics, GPS from mobile phones, credit card transactions and closed circuit (CC) TV data to track the cases and their contacts quickly (discussed in detail below).
We explored specific digital technologies used for the monitoring of the disease evolution (dashboards and interactive maps) and for the tracking and tracing of cases and contacts (mobile phones and applications) and compared their implementation in different countries. This was followed by a deep-dive into two country-level examples of how different technologies have been integrated to provide a robust response to COVID-19 control.
Results
During the study period, Singapore, Hong Kong, South Korea, and Taiwan managed to limit the spread of SARS-CoV-2. Innovative technologies and big data were used to augment or support traditional mitigation measures to facilitate control, as illustrated in Figures 1 to 4. Digital technologies were used to monitor cases in real-time, facilitate and leverage contact tracing, monitor passage of international travellers, and monitor adherence to quarantine/isolation requirements. Examples of these individually and as integrated measures are summarised below.
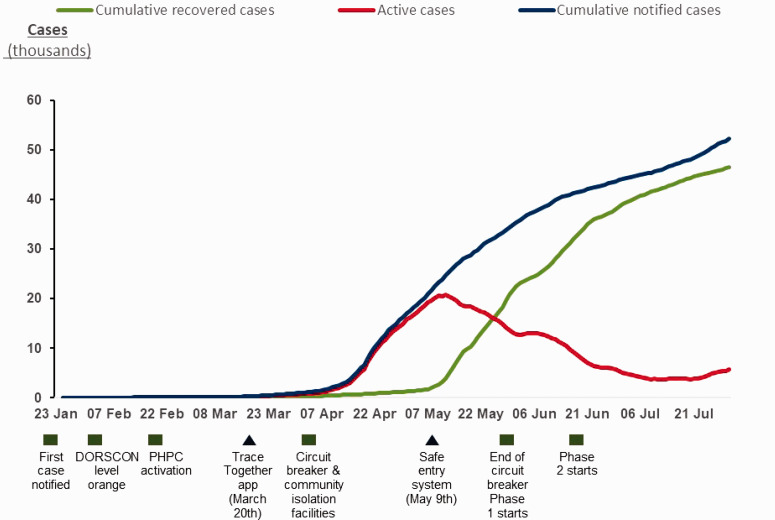
Figure 1.
Singapore.16
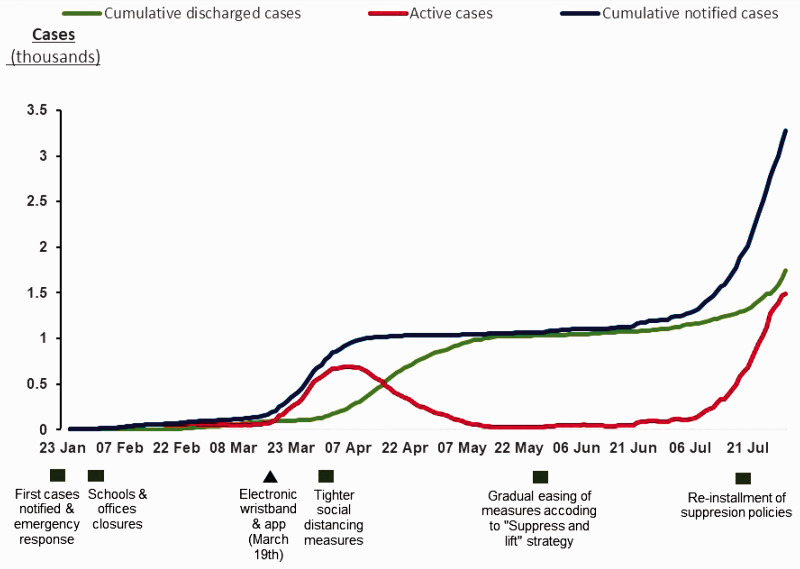
Figure 2.
Hong Kong.17
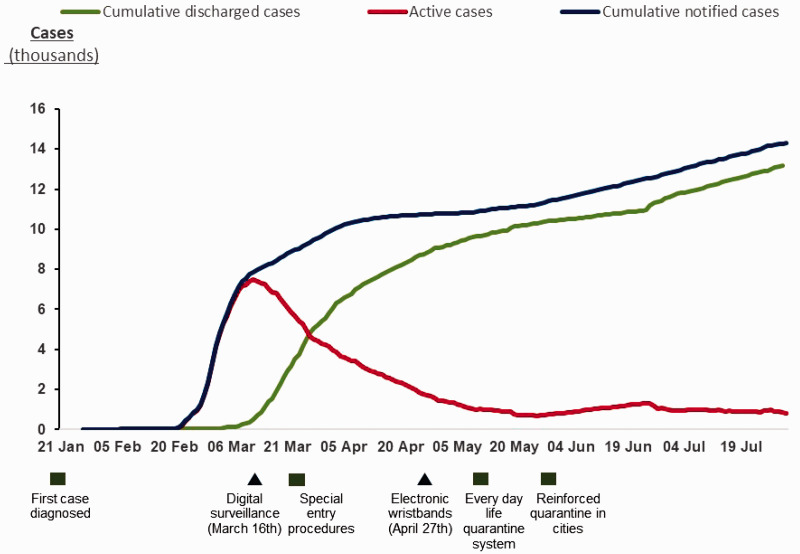
Figure 3.
Taiwan.18
Figure 4.
South Korea.19
Examples of the use of big data and digital technology to control COVID-19 in Asia
Dashboards and interactive maps
Descriptive analytics have been used in Singapore, Hong Kong, South Korea, and Taiwan to provide information on COVID-19, either early or before the first cases were detected, with daily updated dashboards showing graphs, interactive maps and data, including numbers of total active, discharged, and deceased cases (Table 1). The information is broken down by numerous categories such as nationality, age, gender, and country of source. Where patient tracking information is available, the geographic locations of cases where they originated and visited ahead of their diagnosis is shown on publicly available interactive maps and released almost in real-time. Individuals can thus assess their potential risk of exposure, and public health authorities can identify and intervene where a clustering of cases has been identified (Table 1).20 The technology differs from that used earlier in public health in two key aspects: its provision virtually in real-time, and its wide availability to members of the public.
Table 1.
Examples of content included on the dashboards produced by data analytics.
| Countries | Sources | |
|---|---|---|
| Singapore | https://co.vid19.sg/singapore/ | |
| Hong Kong | https://chp-dashboard.geodata.gov.hk/covid-19/en.html | |
| South Korea | http://coronamap.site/ | |
| Taiwan | https://www.cdc.gov.tw/En | |
Note: Links provided for further exploration, taken as of 30 July 2020.
Timeline charts showing the evolution of cases in individual geographies alongside some of the traditional and digital mitigation measures undertaken in chronology.
Similar maps are widely used to update the status of COVID-19 in various countries in the world, such as the Johns Hopkins University COVID-19 dashboard,21 but without detailed information on the movements of individuals.
Mobile phones and applications for contact tracing and tracking isolations/quarantines
Movements of individuals can be tracked without their consent through mobile phone signals, as described below in Hong Kong, Taiwan and South Korea examples. Alternatively, contact tracing can be improved using apps that users choose to download voluntarily. Singapore launched one such app, TraceTogether, on 20th March 2020.22 The app works by exchanging short-distance Bluetooth signals between phones to detect other users of the app who are nearby. These records are not sent to the authorities but are stored in the users’ phones as anonymous numerical IDs, to be shared only if requested by the Ministry of Health as part of contact-tracing investigations. The app does not identify where the exposure to COVID-19 cases may have occurred, but instead it identifies individuals who might have been exposed to the virus, who can then be followed-up by contact tracing teams.22
For security reasons, Apple blocks the apps that run in the background from accessing Bluetooth, which means on iPhones the TraceTogether app must always be open, draining battery power. Apple and Google are jointly working on ways to overcome this problem.23 Furthermore, from a public health perspective, to contain outbreaks tracking apps must cover at least 60% of the population;24 whereas, uptake in Singapore was only about 20%.22 The government therefore introduced a new system of monitoring whereabouts of individuals by requiring them to check in, using their phones or Identity Cards, whenever they enter a shop or public establishment (www.safeentry.gov.sg/);25 refusing which they are denied entry. Users also check out when they leave. If it is subsequently found that a person with COVID-19 was present, everybody present at the same time is alerted.
Mobile apps are generally viewed as more reliable than memory of an individual’s contacts, as they do not have issues of recall bias, nor do they require the contacts to be known to the individual.
From 19 March 2020, Hong Kong placed all arriving passengers under a 2-week quarantine and medical surveillance. Arriving passengers were issued with wristbands connected to a smartphone app to ensure they remained at home. The wristband and the app use geofencing technology, which differs from GPS location tracking. Wearers are instructed to walk around the building where they will be isolated; as they do so, the algorithm on the app samples the signals unique to the building, including its own and nearby Wi-Fi networks, Bluetooth, and cellular networks, to create a composite signature of the building. Any attempt by the wearer to leave their home triggers a warning and alerts the authorities. Violation of the stay-at-home notice is punishable by imprisonment or a large fine.26
Hong Kong was the first metropolitan city to both track people and place a visible marker on their bodies. Some wearers were concerned about the infringement of their civil liberties and the possibility of being wrongly identified by the public and shamed on social media.27
From April 2020, South Korea has also been using electronic wristbands equipped with a location-tracking system for individuals who violate self-isolation rules. Amid rising controversies over privacy, these individuals now have a choice between wearing the bands or being quarantined at state-designated facilities.28
Taiwan is also using a ‘digital fencing’ system, although one without wristbands, to monitor individuals who are under mandatory quarantine (55,000 as of 1 April 2020). The system includes the country’s five major telecom companies who track the quarantined individual by triangulating the location of their phone relative to nearby cell towers. As long as the phone is turned on, the location can be determined. If the phone is turned off or the location indicates quarantine has been violated, an alert is sent to the authorities.29 The system is claimed to be very accurate, with only about 1% of alerts being false alarms. There are some concerns about the privacy implications of the ‘digital fencing’ system due to the vast amount of personal data collected by the government, with fears that it is bound to be intrusive and prone to error.29 To date, public opinion appears to support the Taiwanese government’s handling of the pandemic, and the government has promised to discontinue the tracking system after the pandemic passes.
Examples of integrated technologies implemented in two countries
Individual big data and technology interventions can provide important support to the public health response to COVID-19. The review also identified examples of how different technologies have been integrated to provide a robust response to COVID-19 control. A deep-dive of two country-level examples are as follows:
Taiwan: Integration of national health insurance with immigration and customs database
Taiwan implemented border controls and travel restrictions even before the first cases of COVID-19 were reported in Taiwan. The national health insurance database was integrated with the immigration and customs database within a span of 1 day, in order to classify individuals at high risk based on their flight and travel history.30 Foreign visitors were asked to scan a QR code that led to an online health declaration form requesting contact information and symptoms. Travellers then received a mobile health declaration pass by SMS, allowing faster immigration clearance for those classified as minimal risk based on self-declared data.31 Entry of foreign nationals into Taiwan was later barred (as of 18 March 2020),32 but this system was kept in place for returning nationals.
This initial integration enabled the government to track the 14-day travel histories and symptoms of all recent travellers. Furthermore, Taiwan has a very comprehensive national health care system that covers >99% of residents in the country. The integration of the two databases meant that, if any resident uses their health insurance card to contact any healthcare provider, information on their travel history was immediately shared with that provider33 – allowing the authorities to identify and quarantine patients at high risk. Individuals in high-risk groups or with COVID-19 are given government-issued mobile phones and monitored via location tracking. Their phone signals are monitored, and the authorities are alerted if individuals leave their designated locations or turn off their mobile devices. Officials also call twice a day to ensure that people are not leaving their phones at home.34
Quantitative estimates of the contribution of these measures to Taiwan’s success in containing the pandemic are not available. Nevertheless, a modelling study conducted in January 2020 estimated that, due to its close travel connections with mainland China, Taiwan was predicted to have the second highest number of cases in terms of importation risk from China.35 In reality, as of 25th June, the number of confirmed cases were just 447 with seven deaths reported so far.17,18
South-Korea: Recreating patients’ movements to trace contacts using credit card, GPS, and closed circuit (CC) TV data
South Korea attributed much of its success to its digital surveillance capabilities in limiting the first wave of COVID-19, despite an early explosion of confirmed COVID-19 cases following a church gathering.36 These rank among the most extensive in the world: outside of the COVID-19 pandemic specific context and control strategy, South Korea has the world’s highest proportion of cashless transactions and one of the highest phone ownership rates; furthermore, all phone customers have to provide their real names and national registry numbers.37 The authorities are able to access data from credit and debit card transactions, mobile phones, and CCTV cameras.38,39
In the context of the pandemic, by accessing these data, the authorities can compile detailed logs of confirmed patient movements and contacts. Using geographic data from all three sources, the authorities can determine contact between an infected and a non-infected person, facilitating contact tracing. A new patient’s movement can be compared against those of earlier patients, revealing likely epidemiological links with previously identified cases. In March 2020, the Ministries of Health, Infrastructure, and Science and Technology compiled a centralised data collection platform that reduced the tracking time using all three sources to under 10 minutes per patient.38 The tracking and tracing were backed up by an extensive and rapid testing programme, together with hospitalisation or isolation of confirmed cases.36
The surveillance practices are regulated by a legal framework that was established after the 2015 MERS outbreak.36 The health authorities are allowed to collect data of confirmed and potential patients during infectious disease outbreaks, but must promptly disclose information to the public. Although the information was not intended to provide personally identifiable information, in some cases it was detailed enough for members of the public to identify individuals. Once this was noted, new guidelines were issued to protect patient privacy. The sharing of information with the public and the transparency with which the government adapted its practices, both had the effect of encouraging public trust and cooperation.38 Indeed, a survey of 1,000 South Koreans indicated that most ‘preferred the public good to individual rights’.11,30
Discussion
Digital technologies that were not widely available during previous pandemics have been at the heart of the COVID-19 response strategy of Taiwan, South Korea, Hong Kong, and Singapore. These countries seem to have limited the otherwise extensive spread of COVID-19 by using the new technologies to strengthen traditional mitigation measures.16–19 For example, digital technologies were used to facilitate contact tracing, monitor arriving international travellers, and monitor adherence to quarantine/isolation requirements.
The originality of Taiwan’s approach was in combining the national health and immigration databases at an early stage – a strategic move, because stopping importation early in a pandemic can minimise the burden and provide additional time for activating pandemic plans. This worked well due to the comprehensive coverage of the population in the health insurance system. Databases could similarly be combined in countries where most of the population is registered in a national health system, such as the UK’s National Health Service. It may be too late to implement this now, but it could be a lesson for future waves and pandemics. In other settings, merging of information from government and private healthcare providers (such as managed care organisations in the USA) would be needed, with attendant technical and confidentiality issues. Therefore, such merging would need open-mindedness and cooperation between the private and public sectors as well as the general public.
The success of South Korea’s mapping of patient movements was dependent on the largely cashless economy, high prevalence of mobile phone ownership, and wide use of CCTV cameras. This model could be feasible in countries that are moving towards a digital, non-cash-based economy together with high levels of mobile phone ownership.
However, the gathering of an individual’s personal data without consent poses serious privacy concerns. The urgency of controlling the spread of COVID-19 shifted the risk:benefit ratio in favour of relinquishing privacy in Asian countries. In South Korea, for example, the population placed the public good above individual rights and the government sought to establish public consent for its actions.30 A survey of 1,000 adults nationwide showed that 80% of people supported the use of electronic wristbands to monitor adherence with self-isolation rules.40 However, social values differ by country, and the balance between the interests of public health versus those of freedom and liberty will vary according to each society’s values.24 In a recent poll of 4,917 Americans, 52% agreed that it is acceptable for the government to use mobile phone signals to track people positive for COVID-19. Only 37% agreed on using such tracking to ensure that people are complying with social distancing recommendations.41 Nor is there a simplistic divide between East and West regarding concerns over privacy. In Singapore, more than 17,500 people signed a petition against the proposed introduction of wearable devices for every resident in order to facilitate contact tracing.42
It has been suggested that during a pandemic, even confirmed liberals may not reject technologies that might deprive them of liberty if the alternative is ongoing lockdowns, which rob individuals of even more freedom.24 In an effort to ensure that the overriding of individual rights is not exploited for the wrong purposes, the campaign group Privacy International has stated that measures required during the COVID-19 pandemic should be temporary, necessary, and proportionate, and must be ended when the pandemic is over.43
Our suggestion that other countries should invest in the digital technologies used successfully in Asia has been overtaken by events. Since April 2020, a number of countries around the world, including France, Germany, Italy, Denmark, and Australia have launched TraceTogether or similar contact-tracing apps.44 In the USA, a few states have announced that they will use the software provided by Apple and Google to develop contact-tracing apps. Three states launched their own apps without Apple and Google, but none of these were widely adopted.45 Downloading of the apps is generally voluntary, as, for example, in Italy – where privacy and security measures are explained during set-up.46 However, privacy concerns remain even in the case of voluntarily-downloaded apps. A recent article proposed a number of recommendations for safeguards in connection with digital contact tracing.47 These emphasised the need for users to be able to express consent to all collection and use of personal information, to opt in or out of data sharing, and to uninstall the app at any time, as well as the need for strong protections to prevent any central public or private authority from accessing identifiable data. The authors accept that a drawback of an opt-in approach is that coverage is incomplete and therefore less useful.
Another important dimension to consider is the cost-benefit of these digital efforts in mitigating the spread. Traditional cost-benefit analyses might not work in the case of COVID-19, as this seems to be a fat-tailed process with non-linear spreading. While individual-level efforts like isolation, contact tracing and monitoring of the quarantine might be of help, they are not adequate by themselves to mitigate the systemic risk created by the pandemic. Population level efforts to lessen the human interactions and change the behaviours are indispensable if we want to establish a balance between public health priorities alongside trade and economics.48
Newly enacted laws permitting the gathering of data have already led to legal challenges. In Slovakia, for example, a law that permitted state authorities to access telecommunications data for the purposes of contact tracing was declared unconstitutional.49 A useful overview of data privacy issues in relation to contact-tracing apps in 18 countries, updated in real-time, is available on the Norton Rose Fulbright website.50
In addition to any privacy concerns, many of the apps that have been introduced have encountered low uptake,44 as well as technical issues with the Bluetooth technology. For example, the UK abandoned its own contact-tracing app after a field trial, and is working to resolve issues with the Google/Apple framework.51
All the efforts we have seen so far exist at the country-level to contain the spread of the virus. International borders closure cannot be an indefinite solution. There is a pressing need to develop an international level tracking system (a digital passport) that can work in all the countries being able to facilitate contact tracing, monitor incoming international travellers, and monitor adherence to quarantine/isolation requirements and their whereabouts within any country for those willing to compromise on their privacy for the need to travel.
However, the ethical and legal boundaries of deploying digital tools for disease surveillance and control purposes are unclear from a global perspective. Main limitations described include: the accuracy, granularity, and quality of data that vary greatly across the different data sources; the adequacy of computation safeguards; and the interoperability issues and security risks.52
In this situation where there is a need on one hand and a gap in another, governments, private sectors, especially software technology companies and international heath and ethics organizations should be encouraged to work together to define a framework outlining the objectives and mechanisms through which new digital applications can support the fight against COVID-19 and how legal data privacy is secured and preclude any utilisation of personal data for a purpose other than the control of the epidemic itself. This would encourage better adherence to digital tools and ultimately a better control of the epidemic.53
Conclusion
In emerging epidemic or pandemics, early implementation of containment and mitigation strategies is absolutely vital to control the transmission and the spread into the community. During COVID-19, Singapore, Taiwan, South Korea and Hong-Kong have demonstrated the enormous potential that digital technologies and big data have in facilitating and strengthening traditional public health measures in combatting the spread of SARS-CoV-2. Better stakeholder consultation is needed to overcome the concerns about confidentiality and extensive use of individual data, to improve preparedness and speed of implementation and uptake of digital measures. The significant technological advances and lessons learned can be adopted and adapted in other countries to ensure public health preparedness for future waves of COVID-19 and other pandemics.
Acknowledgements
The authors would like to thank Grace Townshend, MSc and Niki Panagiotaki, PhD from HealthCare21 Communications Ltd, Macclesfield, Cheshire, SK10 2XA, UK, a Lucid Group agency, for providing medical writing assistance. The medical writers wrote drafts of the article, guided by discussion with the authors and their input to successive drafts. Support for this assistance was provided by Sanofi Pasteur. The authors would also like to thank Theophile Baissas and Lina Chakir from Corporate Value Associates, Paris for their gracious support in creating the timeline charts. The authors gratefully acknowledge Ombeline Jollivet (Sanofi Pasteur, France) and Laurent Coudeville (Sanofi Pasteur, France) for the discussions regarding the potential impact of digital interventions. The authors would like to thank Roopsha Brahma, PhD (Sanofi Pasteur, Singapore) and Anirban Sanyal, PhD (Sanofi Pasteur, India) for editorial assistance and manuscript coordination on behalf of Sanofi Pasteur.
Footnotes
Contributorship: All authors are employees of Sanofi Pasteur and were involved in formulating the concept of this review article; the collection, analysis, and interpretation of data; the reviewing of drafts; and the decision to submit the paper for publication.
Declaration of conflicting interests: The authors are all employees of Sanofi Pasteur.
Ethical approval: Not applicable.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Sanofi Pasteur provided the funding for medical writing support and article processing fees.
Guarantor: GN.
Peer review: This manuscript was reviewed by reviewers who have chosen to remain anonymous.
ORCID iD: Gopinath Nageshwaran https://orcid.org/0000-0002-2682-381X
References
- 1.Mackey TK, Liang BA. Lessons from SARS and H1N1/A: employing a WHO-WTO forum to promote optimal economic-public health pandemic response. J Public Health Policy 2012; 33: 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oh MD, Park WB, Park SW, et al. Middle east respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med 2018; 33: 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peeri NC, Shrestha N, Rahman MS, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol 2020; 49(3): 717–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Short KR, Kedzierska K, van de Sandt CE. Back to the future: lessons learned from the 1918 influenza pandemic. Front Cell Infect Microbiol 2018; 8: 343–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis 2020; 20: e102–e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Dea S. Global smartphone sales to end users 2007–2020, www.statista.com/statistics/263437/global-smartphone-sales-to-end-users-since-2007/ (accessed 23 June 2020).
- 7.Albahri AS, Hamid RA, Alwan JK, et al. Role of biological data mining and machine learning techniques in detecting and diagnosing the novel coronavirus (COVID-19): a systematic review. J Med Syst 2020; 44: 122–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albahri OS, Zaidan AA, Albahri AS, et al. Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: taxonomy analysis, challenges, future solutions and methodological aspects. J Infect Public Health 2020; 13: 1381–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albahri OS, Al-Obaidi JR, Zaidan AA, et al. Helping doctors hasten COVID-19 treatment: towards a rescue framework for the transfusion of best convalescent plasma to the most critical patients based on biological requirements via ml and novel MCDM methods. Comput Methods Programs Biomed 2020; 196: 105617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ting DSW, Carin L, Dzau V, et al. Digital technology and COVID-19. Nat Med 2020; 26: 459–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yasheng Huang MS, Sui Y. How digital contact tracing slowed COVID-19 in East Asia. Harvard Business Review, https://hbr.org/2020/04/how-digital-contact-tracing-slowed-covid-19-in-east-asia (accessed accessed 7 July 2020).
- 12.Raghupathi W, Raghupathi V. Big data analytics in healthcare: promise and potential. Health Inf Sci Syst 2014; 2: 3–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bayrak T. A review of business analytics: a business enabler or another passing fad. Procedia Soc Behav Sci 2015; 195: 230–239. [Google Scholar]
- 14.Dash S, Shakyawar SK, Sharma M, et al. Big data in healthcare: management, analysis and future prospects. J Big Data 2019; 6: 54. [Google Scholar]
- 15.Pastorino R, De Vito C, Migliara G, et al. Benefits and challenges of big data in healthcare: an overview of the European initiatives. Eur J Public Health 2019; 29: 23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singapore MoH. Situation report, www.moh.gov.sg/covid-19/situation-report (accessed 3 August 2020).
- 17.Department of Health HK. Data in coronavirus disease (COVID-19), https://data.gov.hk/en-data/dataset/hk-dh-chpsebcddr-novel-infectious-agent (accessed 3 August 2020).
- 18.Taiwan Centers for Disease Control. Coronavirus disease 2019 (COVID-19), https://www.cdc.gov.tw/En (accessed 25 June 2020).
- 19.Ministry of health and welfare RoK. Coronavirus disease-19, Republic of Korea, http://ncov.mohw.go.kr/en/ (accessed 3 august 2020).
- 20.Law E, Choon CM. How China, South Korea and Taiwan are using tech to curb coronavirus outbreak, www.straitstimes.com/asia/east-asia/how-china-s-korea-and-taiwan-are-using-tech-to-curb-outbreak (accessed 2 June 2020).
- 21.Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), https://coronavirus.jhu.edu/map.html (accessed 25 June 2020).
- 22.Kit TS, Mahmud AH. Singapore launches TraceTogether mobile app to boost COVID-19 contact tracing efforts, www.channelnewsasia.com/news/singapore/covid19-trace-together-mobile-app-contact-tracing-coronavirus-12560616 (accessed 2 June 2020).
- 23.Aravindan A, Phartiyal S. Bluetooth phone apps for tracking COVID-19 show modest early results, www.reuters.com/article/us-health-coronavirus-apps/bluetooth-phone-apps-for-tracking-covid-19-show-modest-early-results-idUSKCN2232A0 (accessed 25 May 2020).
- 24.Kluth A. If we must build a surveillance state, let’s do it properly, www.bloomberg.com/opinion/articles/2020-04-22/taiwan-offers-the-best-model-for-coronavirus-data-tracking (accessed 2 June 2020).
- 25.SafeEntry. A Singapore Government Agency Website, www.safeentry.gov.sg/ (accessed 7 July 2020).
- 26.Hui M. Hong Kong is using tracker wristbands to geofence people under coronavirus quarantine, https://qz.com/1822215/hong-kong-uses-tracking-wristbands-for-coronavirus-quarantine/ (accessed 27 May 2020).
- 27.Murphy H. 14 days with a quarantine tracker wristband: Does it even work? www.nytimes.com/2020/04/08/world/asia/hong-kong-coronavirus-quarantine-wristband.html (accessed 25 May 2020).
- 28.Yonhap S. Korea exports wristband trackers for quarantine violators, www.koreaherald.com/view.php?ud=20200520000654 (accessed 2 June 2020).
- 29.Hui M. How Taiwan is tracking 55,000 people under home quarantine in real time, https://qz.com/1825997/taiwan-phone-tracking-system-monitors-55000-under-coronavirus-quarantine/ (accessed 27 May 2020).
- 30.Huang Y, Sun M, Sui Y. How digital contact tracing slowed COVID-19 in east Asia, https://hbr.org/2020/04/how-digital-contact-tracing-slowed-covid-19-in-east-asia (accessed 7 July 2020).
- 31.Wang C, Ng C, Brook R. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA 2020; 1323: 1341–1342. [DOI] [PubMed] [Google Scholar]
- 32.Flannery R. Taiwan to bar entry of foreign nationals in move to contain coronavirus, www.forbes.com/sites/russellflannery/2020/03/18/taiwan-to-bar-entry-of-foreign-nationals-in-bid-to-contain-coronavirus/#4d2bb1823071 (accessed 25 June 2020).
- 33.Taiwan Today. Special: Minister Chen talks Taiwan’s WHO exclusion, national health insurance, https://taiwantoday.tw/news.php?unit=2,6,10,15,18&post=175684 (accessed 25 June 2020).
- 34.Wired-gov. How Taiwan used tech to fight COVID-19, www.wired-gov.net/wg/news.nsf/articles/How+Taiwan+used+tech+to+fight+COVID19 + 01042020162500?open (accessed 2 June 2020).
- 35.Gardner L. Modeling the spread of 2019-nCoV, https://systems.jhu.edu/research/public-health/ncov-model/ (accessed 30 June 2020).
- 36.Thompson D. What’s behind South Korea’s COVID-19 exceptionalism? www.theatlantic.com/ideas/archive/2020/05/whats-south-koreas-secret/611215/ (accessed 2 June 2020).
- 37.OECD. Testing for COVID-19: a way to lift confinement restrictions, www.oecd.org/coronavirus/policy-responses/testing-for-covid-19-a-way-to-lift-confinement-restrictions-89756248/#section-d1e222 (accessed 23 June 2020).
- 38.Jo EA. South Korea’s experiment in pandemic surveillance, https://thediplomat.com/2020/04/south-koreas-experiment-in-pandemic-surveillance (accessed 27 May 2020).
- 39.Sonn JW. Commentary: South Korea succeeded in controlling COVID-19 panic buying, thanks to tracking and surveillance, www.channelnewsasia.com/news/commentary/covid-19-coronavirus-south-korea-cases-test-data-surveillance-12559252 (accessed 25 May 2020).
- 40.Straits Times. Coronavirus: South Korea to strap tracking wristbands on those who violate quarantine orders, www.straitstimes.com/asia/east-asia/coronavirus-south-korea-to-strap-tracking-wristbands-on-those-who-violate-quarantine (accessed 2 June 2020).
- 41.Auxier B. How Americans see digital privacy issues amid the COVID-19 outbreak, www.pewresearch.org/fact-tank/2020/05/04/how-americans-see-digital-privacy-issues-amid-the-covid-19-outbreak/ (accessed 2 June 2020).
- 42.Security Magazine. Singapore introduces COVID-19 contact tracing app, www.securitymagazine.com/articles/92573-singapore-introduces-covid-19-contact-tracing-app-amid-privacy-concerns (accessed 23 June 2020).
- 43.Privacy International. Fighting the global Covid-19 power-grab, https://privacyinternational.org/campaigns/fighting-global-covid-19-power-grab (accessed 23 June 2020).
- 44.Allen-Kinross P. Does any country have ‘a functioning track and trace app’? https://fullfact.org/health/coronavirus-track-and-trace-app-boris-johnson/ (accessed 25 June 2020).
- 45.Ingram D. Coronavirus contact tracing apps were tech's chance to step up. They haven’t, www.nbcnews.com/tech/tech-news/coronavirus-contact-tracing-apps-were-tech-s-chance-step-they-n1230211 (accessed 7 July 2020).
- 46.Potuck M. Italy launches one of the first Apple Exposure Notification API-based apps with ‘Immuni’, https://9to5mac.com/2020/06/01/italy-apple-exposure-notification-api-app/ (accessed 7 July 2020).
- 47.Bengio Y, Janda R, Yun WY, et al. The need for privacy with public digital contact tracing during the COVID-19 pandemic. Lancet Digit Health 2020; 2: e342–e344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joseph Norman YB-Y, Nicholas Taleb N. Systemic risk of pandemic via novel pathogens – coronavirus: a note. UK: New England Complex Systems Institute, 2020. [Google Scholar]
- 49.Mrva TC. Suspends part of Slovakia’s phone-tracking law to fight virus spread, https://in.reuters.com/article/health-coronavirus-slovakia-tracking-idINKBN22P2E3 (accessed 7 July 2020).
- 50.Fullbright NR. Contact tracing apps: a new world for data privacy, www.nortonrosefulbright.com/en-pl/knowledge/publications/d7a9a296/contact-tracing-apps-a-new-world-for-data-privacy (accessed 23 June 2020).
- 51.Gov.uk. Next phase of NHS coronavirus (COVID-19) app announced, www.gov.uk/government/news/next-phase-of-nhs-coronavirus-covid-19-app-announced (accessed 25 June 2020).
- 52.Gasser U, Ienca M, Scheibner J, et al. Digital tools against COVID-19: taxonomy, ethical challenges, and navigation aid. Lancet Digit Health 2020; 2: e425–e434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vokinger KN, Nittas V, Witt CM, et al. Digital health and the COVID-19 epidemic: an assessment framework for apps from an epidemiological and legal perspective. Swiss Med Wkly 2020; 150: w20282. [DOI] [PubMed] [Google Scholar]