Abstract
Introduction:
Shorter length of stays (LOS) at a Skilled Nursing Facility (SNF) after hip fracture surgery would be expected to lead to costs savings for the healthcare system. Evidence also suggests that shorter SNF stays also leads to improved 30-day outcomes, thus compounding this value proposition. Our Integrated Fragility Hip Fracture Program created a simple algorithm at discharge to provide each post-operative hip fracture patient with an expected SNF LOS. We studied whether this intervention produced a shorter SNF LOS and other observable short-term outcomes.
Methods:
We retrospectively reviewed all original Medicare hip fracture patients treated with operative fixation who were admitted to our hospital in 2015, 2017 and 2018. We selected patients who were discharged to a single SNF following hospitalization, and excluded patients with incomplete records. The algorithm for the expected LOS recommendation was based on the degree of assistance the patient needed for ambulation: 7 days (“0-person assist”), 14 days (“1-person assist”), or 21 days (“2-person assist”). We compare the SNF LOS of our hip fracture patient population between those discharged to a program participant, those SNF that agreed to this algorithm, and those discharged to a non-program participant SNF.
Results:
We identified 246 patients meeting our selection criteria. 69 were discharged to a program participant SNF. Patients discharged to a participant SNF had similar baseline demographics and ASA distributions to those discharged to a non-participant provider. There was a statistically significant difference in length of stay between the groups, with program participant patients spending an average of 23 days at the SNF while the control group spent an average of 31 days. (p < 0.001). Program participant discharges were also associated with additional cost savings. There was no significant difference in ED visits within 90 days of discharge.
Discussion:
SNF LOS for geriatric hip fractures can be decreased with implementation of a simple physical therapy driven algorithm based on the patient’s ambulatory independence at hospital discharge. Conclusion: This is a simple, yet completely unique program that seems to have increased the value of healthcare provided.
Keywords: geriatric nursing, physical medicine and rehabilitation, trauma surgery, economics of medicine, fragility fractures
Introduction
Hip fractures remain a medical and socioeconomic burden.1 There are over 200,000 hip fractures in the United States every year, most of these in the elderly.2 Besides a high mortality rate, geriatric hip fractures lead to substantial morbidity for patients who survive.3 About 30% of patients require a higher level of care compared to their pre-injury status, and few recover sufficiently to return to their pre-injury level of function.4
Although a discharge to a Skilled Nursing Facility (SNF), also known as a short-term rehabilitation center, immediately after a hip fracture hospitalization is sometimes necessary and unavoidable, the current rate of SNF admissions is very high. The vast majority of patients are discharged to either a SNF or inpatient rehabilitation unit, and less than 20% return directly home after the acute hospitalization.5 Patients also tend to stay at the SNF for a substantial amount of time, with studies reporting average SNF LOS of 24 to 27 days.6,7 This is despite reports that shorter LOS at SNFs following hip fracture are correlated with improved 30-day outcomes.8 This presents a possible target for cost savings and resource optimization. In addition, minimizing SNF stay for patients who don’t necessarily need the additional care parallels patients’ own priorities and wishes.9,10
This study examines a collaboration between a high-volume hip fracture tertiary referral center and SNF facilities. In 2017, our integrated fragility hip fracture program created a guideline of expected in-patient rehabilitation duration for discharge to SNF depending on a patient’s need for assistance after surgical treatment of a fragility hip fracture during the index hospital admission. Each patient was assessed and assigned an expected LOS at the SNF (7, 14 or 21 days). The effect of this program on SNF LOS is assessed. We also assess the programs effect on cost savings.
Method
Expected SNF LOS
On January 2017, in partnership with a few area SNFs, our integrated fragility hip fracture program began recommending expected SNF LOS for hip fracture patients based on the patient’s ambulatory status at the time of hospital discharge. After hip fracture surgery, and once medically cleared for hospital discharge, patients were assessed by a physical therapist who would grade a patient’s level of independence and safety. If the patient was deemed to need SNF discharge and was then accepted into one of the participant SNFs, the physical therapist would recommend an expected SNF LOS of either 7, 14, or 21 days, based on that patient’s need for assistance on transfers.
If a patient was able to ambulate functional distances (>50 ft) with a gait aide, 0-person assist, the expected LOS was 7 days. If the patient required 1-person assist for transfers without the ability to ambulate functional distances (>50 ft) with a gait aide, the recommended length of stay was 14 days. If the patient required 2-person assist for transfers and/or ambulation with a gait aide, the recommended length of stay was for 21 days. We retrospectively reviewed all patients, including patients discharged prior to program implementation and those patients discharged to non-program participants, and assigned them an expected length of stay based on the same parameters. (Table 1).
Table 1.
Recommended SNF LOS Based on Mobility Levels on Day of Hospital Discharge.
| Mobility | Expected Length of Stay (LOS) |
|---|---|
| Independent ambulation, zero-person assist | 7 days |
| One-person assist for ambulation | 14 days |
| Two-person assist for ambulation or transfers | 21 days |
Along with the expected LOS recommendations, each program participant SNF also received a rubric of overall expectations for hip fracture convalescence (Appendix 1). In this rubric, each patient was recommended a clinical care pathway designed to progress towards a safe home discharge. The speed of the clinical care pathway was dependent on the expected SNF LOS.
Study Population and Variables
We identified 246 Medicare hip fracture patients over 65 years of age, discharged to SNF in 2015, 2017 and 2018. We began our integrated fragility hip fracture program in 2016. We created the algorithm used in the study in 2017 and collected intervention data for years 2017 and 2018. We did not include patients from 2019 as we did not yet have all cost data in the BPCI bundle for those patients. For our study purpose, we only included patients with Medicare, and excluded HMOs because of the participation of the Bundled Payments for Care Improvement (BPCI). Patients under the age of 65 (n = 4) were excluded from analysis due to differences in mechanism of injury, surgical technique and post-operative recovery between a younger and the target geriatric population.7,11,12
Our primary interest was the impact of program participation on SNF LOS and the resulted cost savings. There were 69 patients who discharged to participating SNFs, while 177 patients went to non-participating SNFs after discharge from hospital. The outcomes are SNF LOS and Medicare payment variance to target. Payment variance to target is a calculation of cost savings per bundle period, the estimated target cost of the episode minus the cost of the episode of care. A higher variance to target reflects an increase in cost savings. All patients admitted during the study period were included in the BPCI Medicare bundle model, which allowed for comparison of variance to target for each hip fracture episode of care.
Patient demographics included age and gender; clinical factors included American Society of Anesthesiologists (ASA) physical status classification, fracture type per AO classification, method of fixation, time-to-surgery reported in 24-hour intervals, hospital length of stay, and post-surgical complications (pneumonia, adverse drug events (ADEs), surgical site infection (SSI), delirium, pulmonary embolism and deep vein thrombosis (PE/DVT), sepsis and hematoma.) We combined fracture type and method of fixation as Intertrochanteric fracture with dynamic hip screw (ITF/DHS), Intertrochanteric fracture with short intramedullary nails (ITF/S-IMN), Intertrochanteric fracture with long intramedullary nails (ITF/L-IMN), and femur neck fracture with cannulated screws (FNF/CS). By reviewing the last inpatient physical therapy note, we estimated the SNF LOS in accordance to the protocol as 7, 14, or 21 days; the percentage effort of the patients when ambulating was defined as no ambulatory capacity (0%), patients with major assistive needs (25% and 50%), and minimal necessary assistance (75% and 100%). We retrospectively reviewed death, re-operation, readmission, and emergency department (ED) visit within 90 days post-surgery.
Statistical Analysis
Categorical variables were compared between SNF participation status using the chi-square test or Fisher exact test when the expected values were small. Continuous variables were compared using the Student t test or Wilcoxon rank sum test based on normality assumption.
We used univariate and multivariate linear regression models to evaluate the impact of the program on the SNF LOS and variance to target. In multivariate models, we included age, gender, ASA classification, Time-to-Surgery, Fracture/Surgery Type, Hospital LOS, Estimated SNF LOS, Gait training dependency, and 90-day mortality, re-surgery, re-admission and ED visit as covariates.
To further evaluate the impact of the program on the same SNF, which subsequently participated into this program during our study period, we built multilevel linear mixed effects model to compare the difference in outcome between pre and post time period. There were 146 patients in this analysis, 77 patient that were pre-program participants and 69 patients that were program participants. Multilevel analysis accounted for the hierarchical structure of the data where patients (level 1) were nested within SNFs (level 2), and enabled quantification of this SNF cluster effect and provides unbiased estimates for each outcome.
Statistical significance was set at p value less than 0.05. All statistical analyses were performed using SAS 9.4 (Cary, NC).
Results
246 patients fit inclusion criteria for all years. 69 of these patients were admitted to program participant SNF. There were no significant differences in the demographics of patients admitted to participant and non-participant SNF. Patients were otherwise similar in sex, ASA classification, time from admission to surgery, fracture pattern, and fixation construct. (Table 2).
Table 2.
Patient Characteristics by Skilled Nursing Facility Program Participant Status.
| Participant provider | ||||
|---|---|---|---|---|
| Yes (N = 69) | No (N = 177) | Total (N = 246) | P value | |
| AGE | ||||
| Mean (SD) | 84.1 (7.5) | 86.1 (8.1) | 85.5 (8.0) | 0.08 |
| Sex | ||||
| Male | 17 (24.6%) | 44 (24.9%) | 61 (24.8%) | 0.97 |
| Female | 52 (75.4%) | 133 (75.1%) | 185 (75.2%) | |
| ASA Classification | ||||
| I/II | 17 (24.6%) | 34 (19.2%) | 51 (20.7%) | 0.58 |
| III/IV | 52 (75.4%) | 143 (80.8%) | 195 (79.3%) | |
| Fracture/Surgery Type | ||||
| ITF/DHS | 19 (27.5%) | 38 (21.5%) | 57 (23.2%) | 0.76 |
| ITF/S-IMN | 32 (46.4%) | 85 (48.0%) | 117 (47.6%) | |
| ITF/L-IMN | 9 (13.0%) | 26 (14.7%) | 35 (14.2%) | |
| FNF/CS | 9 (13.0%) | 28 (15.8%) | 37 (15.0%) | |
| Delay of Surgery (Hrs) | ||||
| Mean (SD) | 25.8 (9.7) | 27.3 (17.6) | 24.0 (18.0 – 31.0) | 0.49 |
| ≤24 | 34 (49.3%) | 94 (53.1%) | 128 (52.0%) | 0.66 |
| >24 | 35 (50.7%) | 83 (46.9%) | 118 (48.0%) | |
| Estimate SNF LOS (Days) | ||||
| 7/14 | 30 (43.5%) | 55 (31.1%) | 85 (34.6%) | 0.07 |
| 21 | 39 (56.5%) | 122 (68.9%) | 161 (65.4%) | |
| Gait Training Patient Dependency | ||||
| Total Dependency (0%) | 11 (15.9%) | 35 (19.8%) | 46 (18.7%) | 0.40 |
| Assistance (25-50%) | 25 (36.2%) | 74 (41.8%) | 99 (40.2%) | |
| Supervision/Independent | 33 (47.8%) | 68 (38.4%) | 101 (41.1%) | |
| Hospital LOS, Median (IQR) (Days) | ||||
| Hospital | 4 (3 – 4) | 4 (3 – 5) | 4 (3 – 5) | 0.043* |
Note:
a sparse table, Fisher Exact test for p value.
* P value less than 0.05.
** P value less than 0.01.
*** P value less than 0.001.
The SNF LOS was significantly different between participating and non-participating providers. (Figure 1) Participant patients spent, on average, 23 days at the SNF, while non-participant providers patients spent 31 days. (p < 0.001) Participant patients also had a significantly higher variance to target dollar amount, signifying increased cost savings compared to non-participant patients. The average participant provider patient had a variance to target amount of $9,785 while the average non-participant provider patient had a variance to target amount of $4,134, a difference of $5,651 in additional cost savings for each episode of care. (Table 3).
Figure 1.
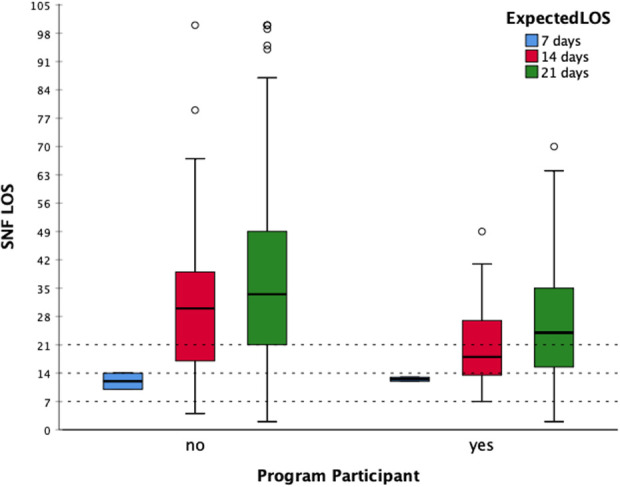
SNF LOS comparison between participant and non-participant SFNs by expected LOS.
Table 3.
Post-Surgical Complications, Cost and SNF LOS by Skilled Nursing Facility Program Participant Status.
| Participant provider | ||||
|---|---|---|---|---|
| Yes (N = 69) |
No (N = 177) |
Total (N = 246) |
P value | |
| Minor Complications | ||||
| Yes | 004 (005.8%) | 023 (013.0%) | 027 (011.0%) | 0.10 |
| No | 065 (094.2%) | 154 (087.0%) | 219 (089.0%) | |
| Pneumonia | 000 (000.0%) | 002 (001.1%) | 002 (000.8%) | |
| ADEs | 000 (000.0%) | 002 (001.1%) | 002 (000.8%) | |
| SSI | 000 (000.0%) | 000 (000.0%) | 000 (000.0%) | |
| Delirium | 003 (004.3%) | 018 (010.2%) | 021 (008.5%) | |
| PE/DVT | 001 (001.4%) | 000 (000.0%) | 001 (000.4%) | |
| Sepsis | 000 (000.0%) | 001 (000.6%) | 001 (000.4%) | |
| Hematoma | 000 (000.0%) | 000 (000.0%) | 000 (000.0%) | |
| Major Complications | ||||
| Death | 003 (004.3%) | 010 (005.6%) | 013 (005.3%) | 1.00 |
| Re-Operation | 006 (008.7%) | 009 (005.1%) | 015 (006.1%) | 0.37 |
| Re-Admission | 020 (029.0%) | 043 (024.3%) | 063 (025.6%) | 0.45 |
| ER Visit | 024 (034.8%) | 056 (031.6%) | 080 (032.5%) | 0.64 |
| Total Variance to Target | ||||
| Median (IQR) | 9832.9 (713.1 – 13571.2) |
4091.5 (-7517.0 – 12132.8) |
5610.5 (-6121.5 – 12726.7) |
0.018** |
| LOS, Median (IQR) (Days) | ||||
| SNF | 23 (14 – 30) | 31 (19 – 48) | 28 (18 – 42) | <0.001*** |
No significant difference was identified in the rate of death, re-operation, re-admission or ED visits between participating and non-participating provider patients.
A univariate analysis was done to identify all variables associated in a difference in variance to target amount and SNF LOS. (Table 4) We found that variance to target amounts were significantly associated with participating provider status, ASA class III vs class I and II, hospital length of stay, re-operation, re-admission and ED visits. SNF LOS was statistically associated with participating SNF status, ASA class III vs. I and II, expected LOS, death, re-operation, and ED visit.
Table 4.
Univariate Analyses on the SNF Length of Stay and Costs Post-Hip Fracture Surgery.
| Characteristics | Variance to target | LOS, SNF | ||||
|---|---|---|---|---|---|---|
| Parameter estimate | 95% CI | P value | Parameter estimate | 95% CI | P value | |
| Program Participant | ||||||
| Yes vs. No | 5131.7 | (683.2, 9580.2) | 0.024 | -11.9 | (-17.7, -6.0) | <.001 |
| Age | 60.9 | (-192.4, 314.2) | 0.64 | 0.3 | (-0.1, 0.6) | 0.14 |
| Sex | ||||||
| Male vs. Female | 534.0 | (-4142.0, 5210.0) | 0.82 | -1.3 | (-7.5, 5.0) | 0.69 |
| ASA Classification | ||||||
| III/IV vs. I/II | -6760.2 | (-11668.4, -1852.1) | 0.007 | 6.9 | (0.3, 13.5) | 0.04 |
| Fracture/Surgery Type | ||||||
| ITF/DHS vs. FNF/CS | -1937.1 | (-8583.1, 4708.8) | 0.57 | 5.7 | (-3.2, 14.5) | 0.21 |
| ITF/S-IMN vs. FNF/CS | -5931.6 | (-11869.1, 5.9) | 0.05 | 9.2 | (1.3, 17.1) | 0.023 |
| ITF/L-IMN vs. FNF/CS | -2931.9 | (-10354.7, 4490.8) | 0.44 | 8.8 | (-1.1, 18.7) | 0.08 |
| Surgery Delay | ||||||
| >24 Hrs vs ≤24 Hrs | 1231.1 | (-2808.2, 5270.4) | 0.55 | -0.8 | (-6.2, 4.6) | 0.76 |
| Complication | ||||||
| Yes vs. No | -1797.8 | (-8254.4, 4658.7) | 0.58 | 3.7 | (-4.9, 12.3) | 0.4 |
| Length of Stay, Hospital (Days) | -1490.5 | (-2659.1, -322.0) | 0.013 | 1.4 | (-0.2, 2.9) | 0.09 |
| Death in 90 Days | ||||||
| Yes vs. No | 6096.1 | (-2897.7, 15089.8) | 0.18 | -11.7 | (-23.7, 0.2) | 0.05 |
| Re-Operation in 90 Days | ||||||
| Yes vs. No | -23152.8 | (-31071.3, -15234.3) | <.001 | 15.4 | (4.3, 26.5) | 0.007 |
| Re-Admission in 90 Days | ||||||
| Yes vs. No | -19249.9 | (-23188.8, -15311.1) | <.001 | 10.4 | (4.3, 16.4) | <.001 |
| ED Visit in 90 Days | ||||||
| Yes vs. No | -14742.8 | (-18632.3, -10853.3) | <.001 | 9.1 | (3.5, 14.8) | 0.002 |
| Estimate SNF LOS | ||||||
| 7/14 vs. 21 Days | 4112.3 | (-102.6, 8327.2) | 0.06 | -8.9 | (-14.5, -3.4) | 0.002 |
| Gait Training Dependency | ||||||
| Assistance vs. Depdt | 1316.1 | (-4144.1, 6776.3) | 0.64 | -1.7 | (-8.8, 5.3) | 0.63 |
| Supervision/Indepdt vs. Depdt | 9491.1 | (4048.1, 14934.2) | <.001 | -16.5 | (-23.5, -9.4) | <.001 |
Multivariate analysis on the same comparison showed a statistical association for variance to target for participating SNF status, hospital LOS, death re-operation, re-admission, and ED visits. There remained a statistically significant association for SNF LOS for participating status and death in 90 days. (Table 5).
Table 5.
Multivariate Analyses on the SNF Length of Stay and Costs Post-Hip Fracture Surgery.
| Characteristics | Variance to target | LOS, SNF | ||||||
|---|---|---|---|---|---|---|---|---|
| Parameter estimate | 95% CI | P value | Parameter estimate | 95% CI | P value | |||
| Program Participant | ||||||||
| Yes vs. No | 5374.37 | (1819.32, 8929.42) | 0.003 | -10.9 | (-16.3, -5.4) | <.001 | ||
| Age | 225.33 | (12.53, 438.14) | 0.038 | 0 | (-0.4, 0.3) | 0.81 | ||
| Sex | ||||||||
| Male vs. Female | -1923.28 | (-5593.32, 1746.76) | 0.30 | 1 | (-4.6, 6.6) | 0.72 | ||
| ASA Classification | ||||||||
| III/IV vs. I/II | -1005.72 | (-5121.45, 3110.02) | 0.63 | 1.2 | (-5.1, 7.5) | 0.71 | ||
| Surgery Delay | ||||||||
| >24 Hrs vs ≤24 Hrs | 962.45 | (-2377.77, 4302.67) | 0.57 | -0.9 | (-6.0, 4.3) | 0.74 | ||
| Fracture/Surgery Type | ||||||||
| ITF/DHS vs. FNF/CS | 1096.1 | (-4171.00, 6363.19) | 0.68 | 2.1 | (-6.0, 10.1) | 0.62 | ||
| ITF/S-IMN vs. FNF/CS | -2027.99 | (-6802.43, 2746.45) | 0.40 | 3.9 | (-3.4, 11.2) | 0.30 | ||
| ITF/L-IMN vs. FNF/CS | -896.82 | (-6747.42, 4953.78) | 0.76 | 4.1 | (-4.9, 13.0) | 0.37 | ||
| Length of Stay, Hospital (Days) | -1241.23 | (-2234.13, -248.32) | 0.015 | 1.1 | (-0.5, 2.6) | 0.17 | ||
| Estimate SNF LOS | ||||||||
| 7/14 vs. 21 Days | -953.21 | (-4824.01, 2917.60) | 0.63 | -1.0 | (-6.9, 5.0) | 0.75 | ||
| Gait Training Dependency | ||||||||
| Assistance vs. Depdt | 1887.03 | (-2686.11, 6460.18) | 0.42 | -1.3 | (-8.3, 5.7) | 0.72 | ||
| Supervision/Indepdt vs. Depdt | 9623.52 | (4466.81, 14780.23) | <.001 | -14.3 | (-22.2, -6.4) | <.001 | ||
| Death in 90 Days | ||||||||
| Yes vs. No | 11751.31 | (4344.61, 19158.02) | 0.002 | -17.6 | (-29.0, -6.2) | 0.003 | ||
| Re-Operation in 90 Days | ||||||||
| Yes vs. No | -12290.51 | (-19569.35, -5011.67) | 0.001 | 11.5 | (0.4, 22.7) | 0.042 | ||
| Re-Admission in 90 Days | ||||||||
| Yes vs. No | -12642.35 | (-18110.02, -7174.68) | <.001 | 4.7 | (-3.6, 13.1) | 0.27 | ||
| ED Visit in 90 Days | ||||||||
| Yes vs. No | -5216.47 | (-9893.39, -539.54) | 0.029 | 4.0 | (-3.1, 11.2) | 0.27 | ||
Several additional variables showed independent, statistical associations with both variance to target and SNF LOS. Hospital LOS, re-operation, re-admission and ED visits were all negatively correlated with variance to target, while dependent vs independent gait at discharge and death were positively correlated with variance to target. Dependent vs independent gait at discharge and death were independently associated with shorter SNF LOS. Re-operations were independently associated with longer SNF LOS.
Finally, Table 6 compares patients that went to a program participant both before (pre) and after (post) the SNF became a program participant. This analysis excludes all SNFs that did not become program participants during the study period. This smaller analysis identifies 146 patients, 69 program participant SNF patients and 77 pre-program participant patients. Both SNF LOS and variance to target remain independently and significantly associated with program participation.
Table 6.
Multilevel Models on the SNF Length of Stay and Costs on SNF Pre and Post Program Participation (N = 146).
| Characteristics (n = 146) |
Variance to target | LOS, SNF | ||||
|---|---|---|---|---|---|---|
| Parameter estimate | 95% CI | P value | Parameter estimate | 95% CI | P value | |
| Individual SNF | ||||||
| Participant vs Non-participant | 5164.4 | (318.4, 10010.4) | 0.039 | -10.3 | (-16.8, -3.8) | 0.006 |
| Age | 237.4 | (-49.6, 524.4) | 0.10 | -0.1 | (-0.4, 0.3) | 0.79 |
| Sex | ||||||
| Male vs. Female | -707.9 | (-6869.5, 5453.8) | 0.79 | 0.9 | (-7.3, 9.0) | 0.81 |
| ASA Classification | ||||||
| III/IV vs. I/II | -1806.0 | (-8047.8, 4435.8) | 0.52 | 2.7 | (-5.5, 11.0) | 0.47 |
| Surgery Delay | ||||||
| >24 Hrs vs ≤24 Hrs | 1154.3 | (-3959.6, 6268.2) | 0.62 | 0.5 | (-6.2, 7.3) | 0.86 |
| Fracture/Surgery Type | ||||||
| ITF/DHS vs. FNF/CS | -1141.2 | (-8143.6, 5861.2) | 0.74 | 2.5 | (-6.7, 11.7) | 0.58 |
| ITF/S-IMN vs. FNF/CS | -5016.7 | (-11560.6, 1527.1) | 0.13 | 5.2 | (-3.4, 13.8) | 0.22 |
| ITF/L-IMN vs. FNF/CS | -2504.6 | (-10505.5, 5496.3) | 0.52 | 2.4 | (-8.2, 12.9) | 0.64 |
| Length of Stay, Hospital (Days) | -765.9 | (-2058.1, 526.3) | 0.24 | 0.9 | (-0.8, 2.6) | 0.32 |
| Estimate SNF LOS | ||||||
| 7/14 vs. 21 Days | -1261.2 | (-7267.5, 4745.2) | 0.64 | -2.1 | (-10.1, 5.9) | 0.56 |
| Gait Training Dependency | ||||||
| Assistance vs. Depdt | 5139.3 | (-1532.8, 11811.4) | 0.12 | -6.0 | (-14.8, 2.8) | 0.17 |
| Supervision/Indepdt vs. Depdt | 12719.1 | (4979.6, 20458.6) | 0.003 | -15.6 | (-25.9, -5.3) | 0.006 |
| Death in 90 Days | ||||||
| Yes vs. No | 8111.7 | (-5778.8, 22002.2) | 0.18 | -15.0 | (-33.3, 3.3) | 0.09 |
| Re-Operation in 90 Days | ||||||
| Yes vs. No | -8243.8 | (-19307.7, 2820.1) | 0.11 | 6.9 | (-7.7, 21.4) | 0.28 |
| Re-Admission in 90 Days | ||||||
| Yes vs. No | -11548.0 | (-19681.4, -3414.6) | 0.011 | 4.1 | (-6.6, 14.8) | 0.41 |
| ED Visit in 90 Days | ||||||
| Yes vs. No | -3698.8 | (-10454.6, 3057.0) | 0.24 | 2.5 | (-6.5, 11.4) | 0.54 |
We also analyzed the targeted LOS based on our algorithm for all patients in this study. We had established a targeted LOS for those patients discharged to a participating SNF. For those patients treated in 2015 prior to the program or discharged to non-participating SNFs, we established a targeted SNF LOS based on the patient’s level of physical function documented in the hospital record at the time of discharge. Figure 1 shows that the targeted LOS based on our algorithm was not consistently met by participating SNFs. However, the LOS was shorter for participating SNFs and the mean LOS for those patients was closer to to the 14- and 21-day targets than for those patients discharged to non-participating SNFs. The number of patients in the 7-day targeted LOS was small in both cohorts.
Discussion
Maximizing peri-operative care and streamlining clinical pathways has shown to greatly improve clinical outcomes in hip fracture patients. For example, expedited surgical fixation of hip fractures in medically stable patients has been shown to lead to fewer major complications.13 Similarly, an integrated, multidisciplinary approach to hip fracture care has also been shown to lead to fewer medical complications.14
Our integrated fragility hip fracture program has had success with protocolization of clinical pathways for hip fractures.15 Patients diagnosed with a new hip fracture in one of our emergency departments are rapidly triaged to a specialized nursing floor. A multidisciplinary team of hospitalists, orthopedic surgeons and anesthesia providers are automatically notified of the admission. Among many other evidence-based standardizations, patients who are deemed to be medically appropriate are then booked for surgery the following day, in an operating room blocked exclusively for hip fracture care.
The intent of the skilled nursing facility program described here was to extend the positive value benefits of our institutional protocols upon discharge to SNF. The program appears to have resulted in a significant decrease in SNF LOS and in significant cost savings.
We had noted, as has been reported elsewhere in the literature,6,7 that prior to this program our hip fracture patients had prolonged SNF LOS, maximizing the allotted Medicare reimbursement for yearly sub-acute care stays. This may be partly attributed to financial mis-incentives. SNFs are completely compensated by Medicare for up to 21 days of short-term rehabilitation per year, and there is no financial benefit for the nursing home to expedite discharge prior to those 21 days. The longer a patient stays, the higher the Medicare payment to the SNF. This is despite the absence of evidence that prolonged SNF LOS improves outcomes, patient independence or safe discharge to home.
A recent study by Kumar et al compares the outcomes of patients who were discharged to SNFs following hip fracture. Patients were grouped depending on their insurance status, either Medicare Advantage (MA), a reimbursement plan based on pre-determined rates per patient per year, versus Medicare fee-for-service (FFS), a reimbursement strategy based on utilization events. They analyzed 211,296 FFS and 75,554 MA and found that MA patients, the ones with a bundled system, had a shorter course of rehabilitation, were less likely to experience a 30-day hospital readmission and were more likely to successfully be discharged to the community.8 The research highlights the potential influence of a patient’s insurance on SNF LOS.
Our study shows that SNF LOS can in fact be safely shortened by implementing a targeted length of stay program based on physical function at time of hospital discharge for hip fracture patients treated with operative fixation. Participating SNF patients showed a significantly decreased SNF LOS (p < 0.001) and a resultant decrease in healthcare costs, as shown by the significant increase in variance to target (p < 0.018). This SNF LOS decrease and improvement in costs savings was not associated with worse rates of minor or major complications, including ED visits and mortality.
Particular attention was given to comparing the baseline characteristics of patients going to participating vs. non-participating SNFs in order to minimize confounders. Although we are not aware of any mechanism that would predispose participating SNFs to receive more mobile or healthier patients, we found no difference in patient gender, comorbidities, as measured by ASA classification, delay between hospitalization and surgery, fracture types, and fixation methods. However, although no factors reached statistical significance, we did find a slight increase in age (86.1 vs 84.0 p = 0.08), increased hospital LOS (p = 0.06) and increased expected SNF LOS (proportion of patients expected to stay for 21 day, 68.9% vs 56.5%, p = 0.07) for patients discharged to non-participating SNFs. All of these factors were controlled for in the multivariate analysis, with a persistent, significant difference in SNF LOS and cost savings for participating SNFs. Both the cost savings and decrease in SNF LOS remained independently and statistically significant in a separate analysis that removed all patients discharged to a facility that never became a program provider. This analysis corrected for the potential of program participant SNFs to have been pre-selected for their baseline higher value.
The cost savings, as calculated by a difference in the variance to target amount, was also already strongly adjusted for patient’s baseline comorbidities. The Center for Medicare and Medicaid (CMS) sets target amounts for each bundle payment based on a diagnosis related group (DRG). Each patient’s DRG is based on the extent of their comorbidities. Because CMS sets target dollar amounts for the bundle period based on DRG, the variance to target, or cost savings relative to that target, also takes the patient’s comorbidities into account as an additional control.
This study has several limitations. It is a single institution program and may not be generalizable to other providers. SNF utilization and availability are regional16 and this kind of intervention effect may also be limited by geography. Additionally, several other institutional protocols were put in place at the same time as this program were started, significantly improving clinical care, as judged by 90 day adverse events and mortality.15 It is possible that in-hospital changes to clinical pathways led to a significant decrease in SNF LOS, but this effect is highly unlikely as all patients were treated with the same in-hospital protocols.
We see additional opportunity to improve our program. Our simple algorithm decreased LOS for patients at SNFs. However, the targeted LOS of 7-, 14-, or 21-days was not consistently met by our participating SNFs. We will further study opportunity to improve our algorithm and work with our participating SNF partners but appreciate the easy application of our straightforward approach to creating a targeted LOS.
Patient disposition following a hip fracture can be a challenging process. The restrictions to return home are multifactorial, and undoubtedly involve more than just a patient’s condition and prognosis. Prolonged stays at SNFs are also dictated by a patient’s living situation, including home accessibility and available family support. However, prompt return to home and activities of daily living remain a priority for patients 9,10 and thus should also be the priority for providers and care givers.
Following hip fracture, patients have a very poor understanding of their injury, prognosis and expected course of convalescence.17 A simple algorithm such as the one described in this study, sets clear goals for the patient, permits family and care-givers to anticipate a date of return home, and unifies providers in communicating a targeted LOS at a skilled nursing facility. Additionally, as shown in this study, this recommendation program can also significantly decrease SNF LOS.
Supplemental Material
Supplemental Material, sj-pdf-1-gos-10.1177_2151459321998615 for A Simple Physical Therapy Algorithm Is Successful in Decreasing Skilled Nursing Facility Length of Stay and Increasing Cost Savings After Hip Fracture With No Increase in Adverse Events by Murillo Adrados, Kaicheng Wang, Yanhong Deng, Janis Bozzo, Tara Messina, Amie Stevens, Anne Moore, Jensa Morris and Mary I. O’Connor in Geriatric Orthopaedic Surgery & Rehabilitation
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Murillo Adrados, MD  https://orcid.org/0000-0001-9809-7987
https://orcid.org/0000-0001-9809-7987
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12): 1726–1733. [DOI] [PubMed] [Google Scholar]
- 2. Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;24(10):2725–2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370. [DOI] [PubMed] [Google Scholar]
- 4. Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol. 2003;157(11):1023–1031. [DOI] [PubMed] [Google Scholar]
- 5. Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170(10):1290–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munin MC, Putman K, Hsieh CH, et al. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil. 2010;89(7):530–540. [DOI] [PubMed] [Google Scholar]
- 7. Mallinson T, Deutsch A, Bateman J, et al. Comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after hip fracture repair. Arch Phys Med Rehabil. 2014;95(2):209–217. [DOI] [PubMed] [Google Scholar]
- 8. Kumar A, Rahman M, Trivedi AN, Resnik L, Gozalo P, Mor V. Comparing post-acute rehabilitation use, length of stay, and outcomes experienced by Medicare fee-for-service and Medicare advantage beneficiaries with hip fracture in the United States: a secondary analysis of administrative data. PLoS Med. 2018;15(6):e1002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harrell R, Lynott J, Guzman S, Lampkin C. What is livable? community preferences of older adults. AARP Research Report. 2014. [Google Scholar]
- 10. Wiles JL, Leibing A, Guberman N, Reeve J, Allen RE. The meaning of “aging in place” to older people. Gerontologist. 2012;52(3):357–366. [DOI] [PubMed] [Google Scholar]
- 11. Mayhew PM, Thomas CD, Clement JG, et al. Relation between age, femoral neck cortical stability, and hip fracture risk. Lancet. 2005;366(9480):129–135. [DOI] [PubMed] [Google Scholar]
- 12. Reeve J, Loveridge N. The fragile elderly hip: mechanisms associated with age-related loss of strength and toughness. Bone. 2014;61(100):138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482. [DOI] [PubMed] [Google Scholar]
- 15. Morris JC, Moore A, Kahan J, et al. Integrated fragility hip fracture program: a model for high quality care. J Hosp Med. 2020;15(2):E1–E7. [DOI] [PubMed] [Google Scholar]
- 16. Wang Y, Zhang Q, Spatz ES, et al. Persistent geographic variations in availability and quality of nursing home care in the United States: 1996 to 2016. BMC Geriatr. 2019;19(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eikelboom R, Gagliardi AR, Gandhi R, Kuzyk PRT, Soong C, Cram P. Patient and caregiver understanding of prognosis after hip fracture. Can Geriatr J. 2018;21(3):274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-gos-10.1177_2151459321998615 for A Simple Physical Therapy Algorithm Is Successful in Decreasing Skilled Nursing Facility Length of Stay and Increasing Cost Savings After Hip Fracture With No Increase in Adverse Events by Murillo Adrados, Kaicheng Wang, Yanhong Deng, Janis Bozzo, Tara Messina, Amie Stevens, Anne Moore, Jensa Morris and Mary I. O’Connor in Geriatric Orthopaedic Surgery & Rehabilitation


