Abstract
Intravenous thrombolysis is the only approved systemic reperfusion treatment for patients with acute ischaemic stroke. These European Stroke Organisation (ESO) guidelines provide evidence-based recommendations to assist physicians in their clinical decisions with regard to intravenous thrombolysis for acute ischaemic stroke. These guidelines were developed based on the ESO standard operating procedure and followed the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. The working group identified relevant clinical questions, performed systematic reviews and meta-analyses of the literature, assessed the quality of the available evidence, and wrote recommendations. Expert consensus statements were provided if not enough evidence was available to provide recommendations based on the GRADE approach. We found high quality evidence to recommend intravenous thrombolysis with alteplase to improve functional outcome in patients with acute ischemic stroke within 4.5 h after symptom onset. We also found high quality evidence to recommend intravenous thrombolysis with alteplase in patients with acute ischaemic stroke on awakening from sleep, who were last seen well more than 4.5 h earlier, who have MRI DWI-FLAIR mismatch, and for whom mechanical thrombectomy is not planned. These guidelines provide further recommendations regarding patient subgroups, late time windows, imaging selection strategies, relative and absolute contraindications to alteplase, and tenecteplase. Intravenous thrombolysis remains a cornerstone of acute stroke management. Appropriate patient selection and timely treatment are crucial. Further randomized controlled clinical trials are needed to inform clinical decision-making with regard to tenecteplase and the use of intravenous thrombolysis before mechanical thrombectomy in patients with large vessel occlusion.
Keywords: Ischaemic stroke, thrombolysis, fibrinolysis, recommendations, thrombectomy
In memory of Professor Eivind Berge

This guideline was co-chaired and led by Professor Eivind Berge, Consultant Cardiologist at the Department of Internal Medicine at Oslo University Hospital. The ESO IVT guideline module working group deeply felt the loss of his calm leadership, thoughtfulness, and thoroughness after his death. Any mistakes or omissions are ours alone.
Introduction
Intravenous thrombolysis (IVT) with alteplase is the only approved systemic reperfusion treatment for patients with acute ischaemic stroke.1 The drive to reduce times to IVT has led to more rapid treatment for stroke patients in some areas of Europe. It has blazed the trail for early stroke unit care, mechanical thrombectomy, and reduced disability due to stroke where this treatment is available. The widespread availability of IVT is a mark of success for researchers, stroke physicians and health care planners.
However, the use of IVT varies across Europe, and demonstrates the ‘inverse care law’2: in those areas of Europe where disability due to stroke in the mid-years of life is the highest, IVT use is amongst the lowest. Those people who live in more rural areas, outside University centres with large hospitals and in countries with more modest incomes have less access to IVT, a marker of access to acute stroke care.3 Another reason for the low IVT treatment rates in acute ischaemic stroke patients may be related to the strict inclusion and exclusion criteria of pivotal randomized-controlled clinical trials.
A well-functioning health care system is needed to provide rapid IVT to patients with acute stroke: emergency dispatch centres, primary care, ambulance services, emergency departments, radiologists, and stroke teams coordinated by a vascular neurologist or a stroke physician. A stroke physician needs to ensure optimal patient selection, and rapid decision making because IVT is more effective when given sooner after stroke.
Therefore, we set out to provide guidelines on the use of intravenous thrombolytics for stroke physicians in Europe. We sought to update previous guidelines from the European Stroke Organisation (ESO).1 Since 2008, new randomised controlled clinical trials (RCTs) have added to our knowledge. Here we review and make recommendations from randomized and observational studies that support a wider use of IVT, particularly about patient selection in late time windows and in patients with relative contraindication to alteplase.
In this document, we outline the current state of the evidence on the effect of IVT in different patient subgroups and time windows, with different thrombolytic agents, and with different imaging selection strategies. We hope to facilitate decision-making in patients where there is uncertainty about eligibility for IVT.
Methods
This guideline was initiated by the ESO and prepared according to the ESO standard operating procedure,4 which is based on the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system.5 The ESO Guideline Board and Executive Committee reviewed the intellectual and financial disclosures of all module working group (MWG) members (Supplemental Table 1) and approved the composition of the group, which was chaired by Eivind Berge and William Whiteley up to January 2020. Following the sad death of Eivind Berge, the MWG was chaired by Guillaume Turc and William Whiteley.
The steps undertaken by the MWG are summarized as follows:
A list of topics of clinical interest to Guidelines’ users was produced and agreed by all MWG members, avoiding: intra-arterial thrombolysis, mechanical thrombectomy, early secondary prophylactic treatment after IVT, service provision or delivery of treatment (e.g. thrombolysis in a spoke hospital before transfer to stroke hub [‘drip and ship’], or thrombolysis in a hub hospital with rapid access to a thrombectomy suite [‘mothership’]), drugs other than alteplase and tenecteplase (e.g. desmoteplase, streptokinase, urokinase), stroke in children, and stroke in pregnancy or in the peripartum period.
- A list of relevant outcomes was produced and the MWG used the Delphi method to score their importance (mean score from 10 respondents on a scale from 1 to 10):
- Functional outcome including death (modified Rankin Scale [mRS] scores 0–6): 8.3
- Symptomatic intracranial haemorrhage (sICH): 7.6
- Death: 7.4
- Quality of life: 6.2
- Imaging-measured recanalisation: 5.9
- Major extracranial bleeding: 5.7
- Neurological outcome (e.g. NIHSS score): 5.5
- Imaging-measured final infarct size: 4.7
Based on this vote, functional outcome was the outcome of highest priority and was considered first, followed by sICH and death. Unless specified otherwise, ‘excellent’ and ‘good’ outcome were defined as three-month mRS scores of 0–1 and 0–2, respectively. Unless specified otherwise, ‘better functional outcome’ corresponded to a reduction of at least one point in the mRS score at three months. sICH was defined according to each study’s original criteria. In case of limited data for the outcomes of highest importance, outcomes of lesser importance were also considered.
3. The MWG formulated a list of Population, Intervention, Comparator, Outcome (PICO) questions, which were reviewed and subsequently approved by the ESO Guideline Board and Executive Committee.
4. The main recommendations were based on a systematic review of RCTs of IVT versus control. To this aim, we have updated the results of a previously published systematic review that was conducted up to March 2012.6 We have applied the same search strategy6 for a period from March 2012 to May 2020. We have also included relevant literature published afterwards in the final manuscript.
5. The authors independently screened the titles and abstracts of the publications identified by the electronic search and assessed the full text of potentially relevant RCTs.
6. For each PICO question, a PICO group consisting of two or three MWG members was formed. Whenever no RCT was available on a certain topic, each PICO group conducted a literature search to identify systematic reviews of non-randomized studies or key observational studies.
7. Whenever appropriate, random-effects meta-analyses were conducted using Stata software version 11.0 (Statacorp). Results were summarized as odds ratios (ORs) or common odds ratio (cOR) and their 95% confidence intervals (CIs). Heterogeneity across studies was assessed using the I2 statistic. Heterogeneity was classified as moderate (I2 ≥ 30%), substantial (I2 ≥ 50%), or considerable (I2 ≥ 75%).7
8. The results of data analysis were imported into the GRADEpro Guideline Development Tool (McMaster University, 2015; developed by Evidence Prime, Inc.). For each PICO question and each outcome, the risk of bias was assessed and quality of evidence was rated as high, moderate, low or very low based on the type of available evidence (randomized or observational studies) and considerations on inconsistency of results, indirectness of evidence, imprecision of results, and risk of bias.5 GRADE evidence profiles/summary of findings tables were generated using GRADEPro.
9. Each PICO group addressed their respective PICO question by writing up to three distinct paragraphs. First, a paragraph named ‘Analysis of current evidence’, in which the results of the dedicated RCTs were summarized and briefly discussed. Where no RCT was available, this paragraph described results of systematic reviews of non-randomized studies. At the end of the first paragraph, an evidence-based recommendation was provided, based on the GRADE methodology. The direction, the strength and the formulation of the recommendation were determined according to the GRADE evidence profiles and the ESO standard operating procedure. Second, an ‘Additional information’ paragraph could be added to provide more details on randomized trials mentioned in the first paragraph, to summarize results of observational studies, or to provide information on ongoing or future trials. Third, according to the first addendum to the ESO standard operating procedure, an ‘Expert consensus statement’ paragraph was added whenever the PICO group considered that insufficient evidence was available to provide evidence-based recommendations for situations in which practical guidance is needed for the everyday clinical practice. In that particular case, a pragmatic suggestion was provided, with the results of the votes of all MWG members on this proposal. Importantly, the suggestions provided in this paragraph should not be mistaken as evidence-based recommendations.
10. The Guideline document was subsequently reviewed several times by all MWG members and modified until a consensus was reached. Finally, the Guideline document was reviewed and approved by external reviewers and members of the ESO Guideline Board and Executive Committee.
Results
1. Treatment within 4.5 h of onset
PICO 1.1: In patients with acute ischaemic stroke of <4.5 h duration, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis?
Analysis of current evidence
Two summaries provide evidence for this question: a systematic review and meta-analysis of study-level data from 10 RCTs by Wardlaw et al. (6887 patients)6 and an individual participant data meta-analysis from 9 RCTs by Emberson et al. (6756 patients).8 These reviews included patients with a wide range of ages and stroke severities.
The study level meta-analysis demonstrated that alteplase within six hours of stroke onset reduced the risk of death or disability defined as a mRS score of 3–6 [odds ratio (OR) 0.84, 95% CI: 0.77–0.93, P = 0.0006, I2 = 63%], and that the effect was greatest within three hours (OR 0.68, 95% CI: 0.53–0.87, P = 0.002, I2 = 0.0%).
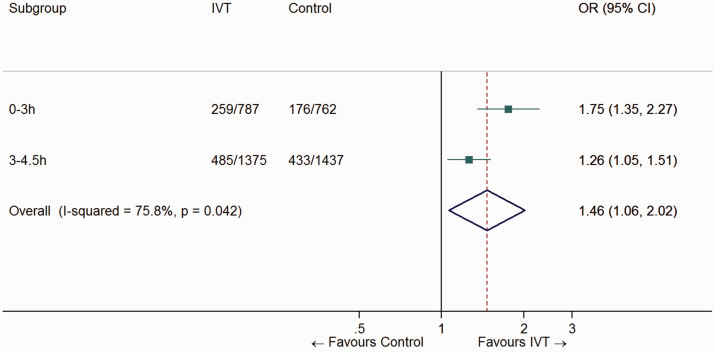
The individual participant data meta-analysis was consistent with these results. It showed that alteplase significantly increased the odds of excellent outcome (no or non-disabling symptoms, mRS score 0–1) at three months (six months in the third International Stroke Study [IST-3]9), with earlier treatment resulting in greater proportional benefit (p for interaction = 0.016). Alteplase significantly increased the odds of an excellent outcome when given within three hours (OR 1.75, 95% CI: 1.35–2.27, p < 0.0001) from 3 to 4.5 h (OR 1.26, 95% CI: 1.05–1.51, P = 0.0132, Figure 1), but not after 4.5 h (OR 1.15, 95% CI: 0.95–1.40, P = 0.15).
Figure 1.
Pooled odds ratio for excellent outcome (mRS 0–1) in patients treated with IVT vs. control in the 0–4.5 h time window.
The numbers and the ORs for the two time subgroups are from the individual patient data meta-analysis of nine RCTs by Emberson et al.
The overall quality of evidence was rated as high, with no serious risk of bias, inconsistency, indirectness, or imprecision (Table 1).
Recommendation
For patients with acute ischaemic stroke of <4.5 h duration, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: High ⊕⊕⊕⊕
Strength of recommendation: Strong ↑↑
Table 1.
GRADE evidence profile for PICO 1.1.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| mRS 0–1 at three months (six months in IST-3) | ||||||||||||
| 9 | randomised trials | not serious | not serious | not serious | not serious | none | 744/2162(34.4%) | 608/2199(27.6%) | OR 1.46(1.06–2.02) | 82 more per 1 000(from 12 more to 159 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
| Death at three months | ||||||||||||
| 9 | randomised trials | not serious | not serious | not serious | not serious | none | 407/2162(18.8%) | 395/2199(18.0%) | HR 1.08(0.94–1.24) | 13 more per 1 000(from 10 fewer to 38 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
Additional information
The study-level systematic review showed that alteplase increased the odds of sICH (OR 3.72, 95% CI: 2.98–4.64, P = 0.00001, I2 = 28%) and of fatal intracranial haemorrhage within 7–10 days (OR 4.18, 95% CI: 2.99–5.84, p < 0.00001, I2 = 0.0%).6 Although alteplase was associated with an excess of early deaths, it had no clear effect on death by the end of follow-up (OR 1.06, 95% CI: 0.94–1.20, P = 0.34, I2 = 38%).
The meta-analysis of individual patient data showed that IVT with alteplase significantly increased the risk of sICH defined as parenchymal haemorrhage of type 2 (OR 5.55, 95% CI: 4.01–7.70, p < 0.0001) or fatal haemorrhage within seven days (OR 7.14, 95% CI: 3.98–12.79, p < 0.0001).8 The absolute excess risk of intracranial haemorrhage increased with increasing stroke severity, but the absolute risk of haemorrhage was less than the benefit from treatment with alteplase at all levels of stroke severity: for the average patient treated within 4.5 h the absolute increase in the proportion of patients with a mRS score of 0 or 1 (6.8%, 95% CI: 4.0–9.5) exceeded the absolute increase in risk of fatal intracranial haemorrhage (2.2%, 95% CI: 1.5–3.0).10
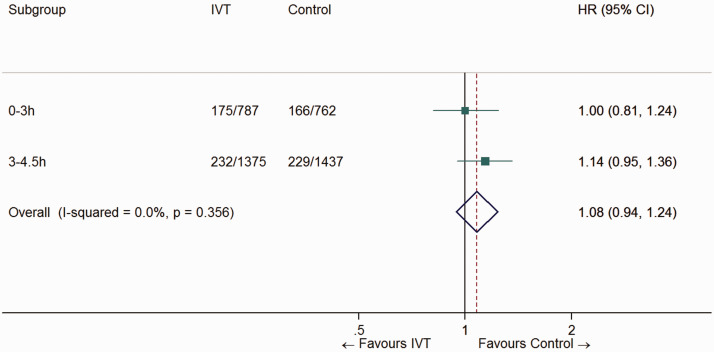
The meta-analysis of individual patient data showed that the early excess case fatality caused by intracranial haemorrhage did not translate into a significant excess case fatality at 90 days in patients treated in the 0–4.5 h time window (HR 1.08, 95% CI: 0.94–1.24, P = 0.27, Figure 2).8 With longer follow-up, there was no evidence of reduced survival in alteplase-treated patients at 18 months,11 and at 3 years there was a non-significant risk difference in favour of alteplase (risk difference 3.6%, 95% CI: –0.8 to 8.1%).12
Figure 2.
Pooled hazard ratio for death at three months in patients treated with IVT vs. control in the 0–4.5 h time window.
The numbers and the HRs for the two time subgroups are from the individual patient data meta-analysis of nine RCTs by Emberson et al.
It has been recently argued that the evidence supporting the use of IVT 3–4.5 h after stroke is frail, and that imbalance in baseline NIHSS score may have been solely responsible for the positive results of the ECASS-3 trial.13 However, the individual participant data meta-analysis by Emberson et al. does provide support for this time window, and did adjust for NIHSS score at baseline.8
Although IVT is currently recommended prior to mechanical thrombectomy,14 there is a debate about whether IVT is necessary for patients directly arriving at stroke centre with thrombectomy capability. The recently published Direct Intraarterial Thrombectomy in Order to Revascularize Acute Ischemic Stroke Patients with Large Vessel Occlusion Efficiently in Chinese Tertiary Hospitals Multicenter Randomized Clinical Trial (DIRECT-MT) suggested that direct mechanical thrombectomy alone was non-inferior to mechanical thrombectomy preceded by IVT with alteplase (0.9 mg/kg) administered within 4.5 h after symptom onset (n = 656, adjusted cOR for better functional outcome at three months 1.07, 95% CI: 0.81–1.40; P = 0.04).15 However, the trial had a liberal non-inferiority margin (20%); a long onset-to-IVT time (median approximately 184 min); and very short delay from start of IVT to groin puncture (median approximately 29 min). In addition, alteplase was not reimbursed in the setting of DIRECT MT, which may have resulted in delaying the allowed time for consenting the patient and in further delaying the door to needle time (median 59 min). Moreover, 31 patients in the bridging therapy (IVT plus mechanical thrombectomy) group did not receive endovascular thrombectomy, while another 30 patients from the same group did not receive any or the full-dose of alteplase.16 The proportion of patients with successful reperfusion after thrombectomy (eTICI ≥2 b) was 79.4% vs. 84.5% (OR 0.70, 95% CI: 0.47–1.06) in the direct mechanical thrombectomy and the bridging therapy groups, respectively. sICH occurred in 4.3% and 6.1% of patients in the direct thrombectomy and bridging therapy groups, respectively (OR 0.70, 95% CI: 0.36–1.37). Other trials comparing direct mechanical thrombectomy and bridging therapy in mothership patients with large vessel occlusion are ongoing (NCT03192332, NCT03494920, ISRCTN80619088).
Whether IVT is effective in patients with lacunar stroke has been debated. In the subgroup of patients with clinically defined lacunar infarct in the National Institute of Neurological Disorders and Stroke (NINDS) tPA trial (13% of enrolled patients), the OR for excellent outcome was 2.53 (95% CI: 1.00–6.37; P = 0.047).17 In patients with clinically defined lacunar infarct in IST-3 (11% of enrolled patients), the adjusted OR for good functional outcome at six months was 0.91 (0.48–1.72). However, there was no evidence of heterogeneity of the effect of IVT across stroke clinical syndromes (P for interaction = 0.46).9 In a post-hoc analysis of participants with MRI-defined lacunar stroke from the Efficacy and Safety of MRI-Based Thrombolysis in Wake-Up Stroke (WAKE-UP) trial (21% of included patients), the OR for excellent outcome was 1.68, 95% CI: 0.78–3.69, without evidence of heterogeneity of the effect of IVT in participants with lacunar stroke or other stroke types (P for interaction = 0.94).18
Vessel occlusion status was not available for the majority of patients included in pivotal trials of IVT vs. no IVT, in which the imaging modality of choice was plain CT. In IST-3, there was a non-significant trend toward a better effect of IVT in patients with obstructed (cOR for better functional outcome 1.86; 95% CI: 0.76–4.53) versus patent (OR, 0.72; 95% CI: 0.42–1.25) arteries (P for interaction = 0.075).19 However, the number of patients without arterial occlusion was modest (n = 140). A study-level meta-analysis suggested a significant interaction, but the thrombolytic used in 3 of the 5 included RCTs was desmoteplase rather than alteplase.19 A post-hoc analysis of the WAKE-UP trial was presented at the ESO Conference in 2019 but has not been published yet.20 Among patients who underwent time-of-flight magnetic resonance angiography (96% of the whole cohort), a total of 308 (63%) patients did not have visible arterial occlusion after assessment by a core lab. There was no evidence of modification of the effect of alteplase by the presence or absence of visible vessel occlusion (OR for mRS 0–1 at three months: 2.04, 95% CI: 1.00–4.18 and 1.58, 95% CI: 0.97–2.56, respectively; P for interaction = 0.56).
In summary, IVT increases the risk of intracranial haemorrhage and early death, but for those treated within 0–4.5 h there are no clear excess of deaths by 90 days. Although there are ongoing discussions about the use of IVT in acute stroke in particular circumstances – before thrombectomy, in patients with lacunar stroke, and in patients with no visible large artery occlusion – there is currently no strong evidence that it should be avoided.
2. Treatment between 4.5 and 9 h after known onset without use of advanced imaging
PICO 2.1 In patients with acute ischaemic stroke of 4.5–9 h duration (known onset time) selected with plain CT, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis?
Analysis of current evidence
The great majority (98.5%) of patients included in an individual participant meta-analysis of 9 RCTs were randomized after brain imaging with plain CT.8 In 6 RCTs, patient could be randomized beyond 4.5 h and up to 6 h after symptom onset (1229 patients treated with alteplase vs. 1166 receiving placebo).9,21–25 This individual participant data meta-analysis showed no evidence of significant benefit of alteplase compared to placebo after 4.5 h of stroke onset or when last seen well (OR for excellent outcome at 3–6 months: 1.15, 95% CI: 0.95–1.40).8 Qualitatively similar results were obtained for good outcome (mRS 0–2), and with an ordinal logistic regression model (cOR for better functional outcome beyond 4.5 h: 1.03, 95% CI: 0.90–1.18).26 The time at which the lower 95% CI for the estimated treatment benefit (mRS 0–1) crossed 1.0 was estimated to be 5.1 h.8
In a study level meta-analysis, the 4.5 h threshold was not examined specifically,6 but there was no significant effect of alteplase in patients randomised more than three hours after stroke (OR 0.97, 95% CI: 0.85–1.09; 5 trials, 1449 participants, I2 = 45%), although this estimate was not statistically different from patients randomised less than three hours after stroke.
The increase in risk of fatal ICH or type 2 parenchymal hemorrhage with alteplase in comparison with placebo was similar irrespective of treatment delay.8 In patients treated more than 4.5 h after stroke, the OR for parenchymal haemorrhage type 2 with alteplase was 6.89 (95% CI: 4.17–11.38), similar to what is observed for patients treated within 4.5 h from symptom onset (OR 5.58, 95% CI: 3.35–9.30).27 Using the SITS-MOST definition of symptomatic intracranial haemorrhage, the absolute excess risk of intracerebral haemorrhage with alteplase was 3.1% within three hours (95% CI: 1.7–5.2), 3.0% between 3 and 4.5 h (95% CI: 1.6–5.0), and 3.6% (95% CI: 2.0–6.0) beyond 4.5 h (p-value for interaction 0.73).10 In patients treated more than 4.5 h after stroke onset, IVT with alteplase led to a non-significant higher three-month mortality (HR: 1.22; 95% CI: 0.99–1.50).8
Other studies have found that patient selection using a prognostic score based on simple clinical variables and plain CT alone cannot identify a patient population for which alteplase given between 4.5 and 6 h of stroke is safe or effective.28
Because the evidence in this chapter is from a subgroup of high-quality RCTs, we have downgraded the quality of evidence from high to moderate.
Recommendation
For patients with acute ischaemic stroke of 4.5–9 h duration (known onset time), and with no brain imaging other than plain CT, we recommend no intravenous thrombolysis.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↓↓
3. Treatment between 4.5 and 9 h after known onset with the use of advanced imaging
PICO 3.1 In patients with ischaemic stroke of 4.5–9 h duration (known onset time), and with CT or MRI core/perfusion mismatch, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis?
Analysis of current evidence
Mismatch between non-contrast CT and CT Perfusion (CTP), or between diffusion-weighted and perfusion-weighted MRI (DWI and PWI) may quantify the penumbral cerebral tissue and could identify patients who benefit of alteplase beyond 4.5 h. However, most RCTs of IVT in later time windows allowed not only the inclusion of patients with known onset >4.5 h but also of patients with wake-up stroke (unknown onset, time last seen well >4.5 h).29,30 We decided to provide distinct recommendations for these two different clinical situations, because the true stroke onset of patients awakening from sleep may frequently be < 4.5 h before randomisation.31,32 This PICO question focuses on patients with known stroke onset 4.5–9 h before presentation.
The Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET) randomised 101 patients with ischaemic stroke with 3–6 h duration to alteplase or placebo. MRI was performed in all patients, but the imaging results were not used for patient selection. Overall, 85 patients (86%) had PWI-DWI mismatch, but the trial did not demonstrate a clinical benefit of alteplase.25 A pooled analysis of the EPITHET trial and an observational study showed that, among patients with PWI-DWI mismatch within 3–6 h of symptom onset (101 patients), those treated with alteplase (60 patients) had significantly smaller infarct growth and higher reperfusion rate, but clinical outcomes were not different between the two groups.33
The fourth European Cooperative Acute Stroke Study (ECASS-4) compared alteplase with placebo in 119 patients presenting between 4.5 and 9 h after stroke onset or after awakening with stroke, and used MRI core/perfusion mismatch to select patients for treatment.30 Inclusion criteria were infarct core volume <100 ml, absolute perfusion lesion volume ≥20 ml (at Tmax >6 s) and mismatch ratio between perfusion and core >1.2. This RCT stopped early when recruitment dropped after publication of the positive thrombectomy trials. Of the 119 included patients, 37 (31%) had known stroke duration of 4.5–9 h (median time to treatment 6.9 h), and 82 (69%) had woken with stroke. There was no significant effect of alteplase on better functional outcome at three months (cOR 1.20, 95% CI: 0.63–2.27, P = 0.57). The treatment effect was similar in the dichotomized mRS analysis for excellent outcome (mRS 0–1) which showed a 6.4% absolute difference in favour of alteplase that did not reach statistical significance (P = 0.45). No analysis of the subgroup of patients with known onset time has been presented.
The Extending the Time for Thrombolysis in Emergency Neurological Deficits (EXTEND) trial compared alteplase with placebo in 225 patients presenting between 4.5 and 9 h after stroke onset or after awakening with stroke, using CT or MRI core/perfusion mismatch to select patients.29 Inclusion criteria were infarct core volume ≤70 ml, absolute perfusion lesion volume of >10 ml and mismatch ratio between perfusion and core >1.2. Of the 225 included patients, 79 (35%) had stroke duration of 4.5–9 h, and 146 (65%) had woken with stroke. The study showed that IVT with alteplase was associated with higher proportion of patients with excellent outcome (mRS 0–1 at three months: 35.4% alteplase vs. 29.5% placebo, adjusted RR 1.44, 95% CI: 1.01–2.06, P = 0.04), and there was no evidence that the effect was different in patients treated during different time intervals (4.5–6 h or 6–9 h), or in patients with wake-up stroke. A secondary pre-specified ordinal analysis did not show a significant difference in functional outcome (cOR for better functional outcome, 1.55, 95% CI: 0.96–2.49). The risk of sICH was higher in the alteplase group (adjusted RR 7.22, 95% CI: 0.97–53.5, P = 0.05).
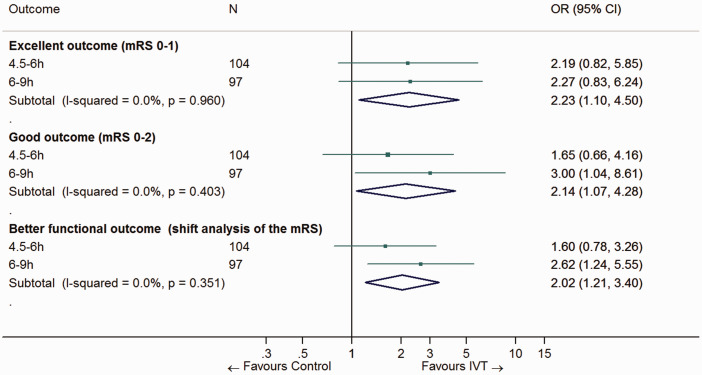
Campbell et al.34 conducted an individual participant data meta-analysis of EPITHET,25 ECASS-430 and EXTEND.29 The main analysis was based on all patients who met the inclusion criteria of the original studies (n = 414; 52% imaged with perfusion-diffusion MRI, 48% with perfusion CT). IVT led to a higher rate of excellent outcome (36% alteplase vs. 29% placebo, OR 1.86, 95% CI: 1.15–2.99, P = 0.01), higher rate of symptomatic intracerebral hemorrhage (5% vs. < 1%; OR 9.7, 95% CI: 1.23–76.55, P = 0.03) with no significant difference in mortality (14% vs. 9%; OR 1.55, 95% CI: 0.81–2.96, P = 0.19).34 However, 51% of included patients had woken with stroke. There was no evidence of a modification of the effect of alteplase in an analysis across the 3 predefined time strata (4.5–6 h, 6–9 h, wake-up stroke; P for interaction = 0.87). In the subgroups of patients with known onset treated between 4.5–6 h and 6–9 h, the ORs for excellent outcome (mRS score 0–1) were 2.19 (95% CI: 0.82–5.85) and 2.27 (95% CI: 0.83–6.24), respectively. Similar results were observed for good outcome and better functional outcome (Figure 3).
Figure 3.
Pooled odds ratio for excellent outcome (mRS 0–1), good outcome (mRS 0–2) and better functional outcome (common OR across the whole range of the mRS) in patients with ischaemic stroke of 4.5–9 h duration (known onset time) treated with IVT vs. control. This analysis comprises all patients enrolled in the EXTEND, ECASS 4 and EPITHET trials, stratified by time window (4.5–6 h and 6–9 h).
The numbers and the ORs for the 4.5–6 h and 6–9 h time windows (adjusted on age and baseline NIHSS score) are taken from the individual patient data meta-analysis of three RCTs (EXTEND, ECASS 4 and EPITHET) by Campbell et al.
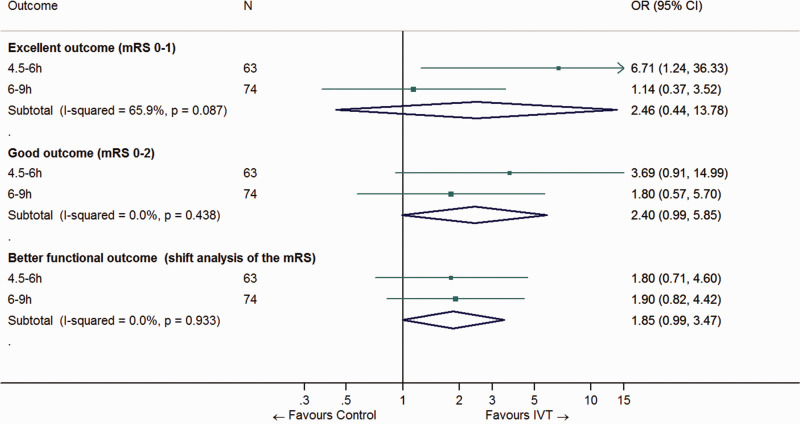
The authors conducted a sensitivity analysis restricted to the subgroup of 303 patients who met the mismatch criteria of the EXTEND trial (see above). To this aim, imaging data for individual patients were reprocessed using an automated software. Alteplase remained associated with excellent outcome (OR 2.06, 95% CI: 1.17–3.62). However, after exclusion of patients with wake-up stroke, the associations between IVT and excellent outcome, good outcome or better functional outcome failed to reach statistical significance (Figure 4).
Figure 4.
Pooled odds ratio for excellent outcome (mRS 0–1), good outcome (mRS 0–2) and better functional outcome (common OR across the whole range of the mRS) in patients with ischaemic stroke of 4.5–9 h duration (known onset time) treated with IVT vs. control. This analysis is restricted to the subgroup of patients enrolled in the EXTEND, ECASS 4 and EPITHET trials who meet the EXTEND mismatch criteria detected by automated software.
The numbers and the ORs for the 4.5–6 h and 6–9 h time windows (adjusted on age and baseline NIHSS score) are taken from the individual patient data meta-analysis by Campbell et al.
Of note, 62% of the patients analysed in the individual participant data meta-analysis had large vessel occlusion but no thrombectomy was performed except for 1 protocol deviation procedure.14,34 Therefore, our evidence-based recommendation only applies to patients who will not undergo mechanical thrombectomy; please see the expert consensus statement below for patients eligible for both IVT and mechanical thrombectomy.
Table 2 provides details regarding the assessment of the quality of evidence, which was judged to be low.
Recommendation
For patients with ischaemic stroke of 4.5–9 h duration (known onset time) and with CT or MRI core/perfusion mismatch*, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↑↑
*In the individual participant data meta-analysis by Campbell et al.,34 core/perfusion mismatch was assessed with an automated processing software and defined as follows:
- Infarct core** volume < 70 ml
- and Critically hypoperfused† volume/Infarct core** volume > 1.2
- and Mismatch volume > 10 ml
** rCBF < 30% (CT perfusion) or ADC < 620 µm2/s (Diffusion MRI)
†Tmax >6 s (perfusion CT or perfusion MRI)
For patients with no CT or MRI core/perfusion mismatch, please see the expert consensus statement below.
Table 2.
GRADE evidence profile for PICO 3.1.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative (95% CI) | Absolute (95% CI) | ||
| mRS 0–1 at three months | ||||||||||||
| 3 | randomised trials | not serious | seriousa | not serious | serious | none | OR 2.23 (1.10–4.50) | ⨁⨁LOW | CRITICAL | |||
| mRS 0–2 at three months | ||||||||||||
| 3 | randomised trials | not serious | serious | not serious | serious | none | OR 2.14 (1.07–4.28) | ⨁⨁LOW | CRITICAL | |||
| Improved mRS score at three months (shift analysis) | ||||||||||||
| 3 | randomised trials | not serious | serious | not serious | serious | none | cOR 2.02 (1.21–3.40) | ⨁⨁LOW | CRITICAL | |||
| Death at three months | ||||||||||||
| 3 | randomised trials | not serious | not serious | not serious | serious | none | OR 1.61 (0.59–4.38) | ⨁⨁⨁MODERATE | CRITICAL | |||
aSerious inconsistency and serious imprecision: when including all patients from EXTEND, ECASS 4 and EPITHET, IVT with alteplase was significantly associated with excellent outcome (mRS 0–1 at three months) compared with control, with a similar OR in the 4.5–6 h and the 6–9 h time windows (pooled OR 2.23, 95% CI: 1.10–4.50, I2 = 0%). However, when only considering those patients who actually had an automated perfusion mismatch, the point estimates for the 4.5–6 h and the 6–9 h time windows varied (OR 6.71 and 1.14, respectively), although there was no statistically significant heterogeneity in these ORs (P for heterogeneity = 0.09, I2 = 66%), which might be due to a modest number of events. The pooled OR did not reach statistical significance and the confidence interval was wide (OR 2.46, 95% CI: 0.44–13.78, I2 = 66%).
Additional information
A recent prospective observational single-centre study reported that, among acute ischemic stroke patients presenting in the 0–9 h window, only 1.3% were eligible for IVT according to EXTEND neuroimaging and clinical eligibility criteria.35
The concept of DWI-FLAIR-mismatch, i.e., presence of an acute ischaemic lesion on DWI in the absence of a hyperintense lesion on FLAIR in the same area, has not been evaluated in RCTs of IVT for the selection of patients with known stroke duration of >4.5 h. One small observational study suggested similar functional outcomes in patients treated within 4.5 h and patients selected with the use of DWI-FLAIR mismatch and treated between 4.5 and 6 h after stroke onset.36
There is no current RCT assessing whether IVT is superior to no IVT in patients who undergo advanced imaging and display no core/perfusion mismatch. In the subgroup of patients who did not meet the EXTEND mismatch criteria after reprocessing imaging data with an automated software in the individual participant data meta-analysis by Campbell et al. (see above),34 no significant difference was observed in the proportions of patients who achieved excellent functional outcome between the alteplase and placebo groups (adjusted OR 1.22, 95% CI: 0.48–3.10, P = 0.68), but there was no significant treatment by mismatch status interaction (P = 0.43). These results should be interpreted with caution because those patients were still considered to have a core/perfusion mismatch according to an alternative definition of penumbral mismatch (i.e., they were deemed to meet the inclusion criteria of the RCT in which they were enrolled). Furthermore, the above-mentioned analysis also encompasses patients with wake-up stroke.
Expert consensus statement
For patients with ischaemic stroke of 4.5–9 h duration (known onset), and with no CT or MRI core/perfusion mismatch, 9 of 9 group members suggest against IVT with alteplase.
There is currently no randomized data to make a recommendation for patients who are scheduled to undergo mechanical thrombectomy and are also eligible for IVT in the 4.5–9 h time window.
Expert consensus statement
For patients presenting directly to a thrombectomy centre with ischaemic stroke of 4.5–9 h duration (known onset) with CT or MRI core/perfusion mismatch and who are eligible for mechanical thrombectomy, the group members could not reach a consensus regarding whether intravenous thrombolysis should be used before mechanical thrombectomy.
For patients presenting to a non-thrombectomy centre with ischaemic stroke of 4.5–9 h duration (known onset) with CT or MRI core/perfusion mismatch and who are eligible for mechanical thrombectomy, 6 of 9 group members suggest intravenous thrombolysis before mechanical thrombectomy.
4. Stroke on awakening from sleep/unknown onset
PICO 4.1 In patients with acute ischaemic stroke on awakening from sleep/unknown onset, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis?
Analysis of current evidence
Up to one in five strokes occur during sleep, but IVT is often withheld in patients with new stroke symptom upon awakening and who were last seen well more than 4.5 h earlier.37,38 Our literature search identified five randomised-controlled trials of IVT with alteplase in patients with wake-up stroke.29,30,39–42
MRI: DWI/FLAIR mismatch
The WAKE-UP trial included 503 patients who woke up with a new stroke and were last known to be well more than 4.5 h earlier, and had an acute ischaemic lesion on DWI but no marked parenchymal hyperintensity on FLAIR (DWI-FLAIR mismatch).39,43 The trial excluded patients for whom thrombectomy was planned. Patients were randomised to alteplase 0.9 mg/kg or placebo, and the primary endpoint was excellent outcome (mRS 0–1 at 90 days). The trial was terminated prematurely owing to cessation of funding after the enrolment of 503 of an anticipated 800 patients. Thirty-four percent of the patients had an intracranial vessel occlusion. The adjusted OR for excellent outcome with alteplase was 1.61 (95% CI: 1.09–2.36, P = 0.02) and the cOR for better functional outcome was 1.62 (95% CI: 1.17–2.23, P = 0.003). Alteplase was also associated with a non-significantly increased risk of sICH (2.0% vs. 0.4%, P = 0.15) and a non-significantly higher mortality at 90 days (4.1% vs. 1.2%, P = 0.07).
The Thrombolysis for Acute Wake-Up and Unclear-Onset Strokes With Alteplase at 0.6 mg/kg (THAWS) trial used the same criteria for patient selection as the WAKE-UP trial, and patients with DWI-FLAIR mismatch on MRI were randomised to low-dose alteplase (0.6 mg/kg) or placebo.44 The trial was terminated early following the positive results of WAKE-UP with recruitment of 131 of the planned 300 patients, leading to a low statistical power. This trial found no difference in excellent outcome (mRS score 0–1) at three months between the alteplase and control groups (RR 0.97, 95% CI: 0.68–1.41, P = 0.89). There was also no difference for death (RR 0.85, 95% CI: 0.06–12.58, P > 0.99). Only 1 patient in the alteplase group had sICH versus 0 in the placebo group.
CT or MRI: core/perfusion mismatch
The EXTEND trial compared alteplase with placebo in 225 patients presenting between 4.5 and 9 h after stroke onset (or between 3 and 9 h, depending on national guidelines) or after awakening with stroke (if within 9 h from the midpoint of sleep),29 using CT or MRI core/perfusion mismatch to select patients. Inclusion criteria were infarct core volume ≤70 ml, absolute perfusion lesion volume of >10 ml and mismatch ratio between perfusion and core >1.2. After 225 of the planned 310 patients had been enrolled, the study was terminated because of a loss of equipoise after the publication of the WAKE-Up trial. The study found that alteplase was associated with excellent outcome (mRS 0–1 at 90 days: adjusted RR 1.44, 95% CI: 1.01–2.06, P = 0.04). Of note, the study would not have demonstrated superiority of alteplase had the investigators used another method of analysis than adjusted Poisson regression and a primary endpoint of mRS 0–1. However, the statistical analysis plan was determined before database lock and the results are therefore valid. Intervention and control groups were generally well balanced, but alteplase-treated patients were slightly older, and with more severe strokes as measured by both core volume and NIHSS score and this may account for the lack of statistical significance for primary and secondary clinical endpoints in the unadjusted analyses.45 The risk of sICH was higher in the alteplase group (adjusted RR 7.22, 95% CI: 0.97–53.5, P = 0.05). The treatment effect was not significantly different across the three time strata (4.5–6 h; 6–9 h; wake-up stroke: P for interaction = 0.41). A total of 146 (65%) patients had woken with stroke. In the subgroup of patients with wake-up stroke, the adjusted RR for excellent outcome was 1.53 (95% CI: 0.97–2.43).
Individual participant data Meta-analysis
A systematic review and individual participant data meta-analysis of RCTs of IVT with alteplase for patients with stroke of unknown time of onset guided by advanced imaging was recently conducted by the Evaluation of unknown Onset Stroke thrombolysis trials (EOS) investigators.46 A total of 843 patients enrolled in studies based on DWI-FLAIR mismatch (WAKE-UP39 and THAWS44) or core/perfusion mismatch (EXTEND29 and ECASS-430) were included. Perfusion data was automatically reprocessed using the RAPID software, and the authors used the definition of penumbral mismatch from the EXTEND trial for their analysis (infarct core volume ≤70 ml, absolute perfusion lesion volume of >10 ml and mismatch ratio between perfusion and core >1.2). The median time between last seen well and treatment initiation was 10.5 h and the imaging modality was MRI in 85% of cases. Compared to placebo or standard care, IVT was significantly associated with excellent outcome (primary endpoint: adjusted OR 1.49, 95% CI: 1.10–2.03, P = 0.01; I2 = 27%) and better functional outcome (adjusted cOR 1.39, 95% CI: 1.05–1.80, P = 0.02), at the expense of a higher risk of sICH (3% vs. 0.5%, P = 0.02) and mortality within three months (adjusted OR 2.06, 95% CI: 1.03–4.09, P = 0.04). The effect of alteplase was consistent across predefined subgroups, including imaging modality (CT vs. MRI) and large vessel occlusion status. Of note, mechanical thrombectomy was not performed in the 25% of included patients with large vessel occlusion.
Albeit based on the EOS meta-analysis, our recommendation for patients with MRI DWI-FLAIR mismatch is mostly driven by the results of the WAKE-UP trial, which used a standard dose of alteplase, unlike the small THAWS trial, in which the dose of 0.6 mg/kg was used. Both studies were terminated early. We rated the quality of the evidence as high (Table 3) because of the relatively large sample size, the fact that the WAKE-UP study was specifically focusing on patients with unknown symptom onset and that the superiority of IVT was consistently observed across secondary endpoints. For patients with CT or MRI perfusion core/perfusion mismatch and unknown time of onset, we rated the quality of evidence as moderate (Table 3) for several reasons. First, no study based on perfusion mismatch was specifically dedicated to patients with unknown time of onset and therefore the evidence comes from subgroups of patients in two relatively small RCTs that were stopped prematurely. Second, the positive association between IVT and excellent outcome was only demonstrated after a reanalysis of individual patient imaging data using the perfusion criteria of the EXTEND trial,29 which slightly differ from those of the ECASS 4 trial.30 Based on the perfusion mismatch criteria of each original study, the association would not have been significant (OR 1.56; 0.81–3.02).34 Of note, in the EOS individual participant data meta-analysis, only 54% (n = 221) of patients with available assessment for perfusion imaging had a penumbral mismatch according to the EXTEND criteria46. However, because this analysis showed a clear benefit of IVT (adjusted OR for excellent outcome 2.14, 95% CI: 1.11–4.12), we provide a strong recommendation in favour of IVT in this situation.
Table 3.
GRADE evidence profile for PICO 4.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| DWI-FLAIR mismatch (WAKE-UP trial 39 & EOS Independent participant data meta-analysis 46 ) | ||||||||||||
| mRS 0–1 at three months | ||||||||||||
| 1 | randomised trials | not serious | not serious | not serious | not serious | none | 131/246(53.3%) | 102/244(41.8%) | OR 1.61(1.09–2.36)* | 118 more per 1 000(from 21 more to 211 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
| Death at three months | ||||||||||||
| 1 | randomised trials | not serious | not serious | not serious | not serious | none | 10/251(4.0%) | 3/244(1.2%) | OR 3.38(0.92–12.52) | 28 more per 1 000(from 1 fewer to 123 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
| sICH (ECASS 2 definition) | ||||||||||||
| 1 | randomised trials | not serious | not serious | not serious | seriousa | strong association | 7/251(2.8%) | 3/244(1.2%) | OR 2.40(0.60–9.53) | 17 more per 1 000(from 5 fewer to 94 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
| Core/Perfusion mismatch (EXTEND, 29 ECASS-4 30 & EOS 46 & Campbell et al. 34 ) | ||||||||||||
| mRS 0–1 at three months | ||||||||||||
| 2 | randomised trials | not serious | seriousb | serious | not serious | none | 45/112(40.2%) | 29/109(26.6%) | Adjusted OR 2.14(1.11–4.12) | 171 more per 1 000(from 21 more to 333 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| Death at three months | ||||||||||||
| 2 | randomised trials | not serious | not serious | not seriousb | seriousc | none | 14/112(12.5) | 9/109(8.3) | OR 1.59(0.66–3.84) | 43 more per 1 000(from 26 fewer to 174 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
*In the EOS meta-analysis of 4 RCTs of IVT vs. placebo/usual care in patients (n = 843) with unknown stroke onset and either DWI-FLAIR mismatch or core/perfusion mismatch,46 the adjusted OR for mRS 0–1 at three months was 1.49, 95% CI: 1.10–2.03 in favor of alteplase (P = 0.01). In the subgroup of patients with DWI-FLAIR mismatch (n = 641), the adjusted OR for mRS 0–1 was 1.45 (0.98–2.13). In the subgroup of patients with core/perfusion mismatch (n = 221), the OR for mRS 0–1 at three months was 2.14 (1.11–4.12).
aVery large confidence interval. Although IVT with alteplase was not significantly associated with any definition of sICH, the point estimates where high (OR >4) for the ECASS 3 and SITS-MOST definitions, with very large confidence intervals as well. Furthermore, IVT was significantly associated with Parenchymal Hemorrhage type 2.
bThese results are based on a reanalysis of individual patient imaging data, using the perfusion criteria of the EXTEND trial, which are slightly different from those of the ECASS 4 trial. Based on the perfusion mismatch criteria of each original study, the association would not have been significant (OR 1.56; 0.81–3.02).34
cLarge confidence interval including 1.0.
There is currently no randomized data to make a recommendation for wake-up stroke patients who are scheduled to undergo mechanical thrombectomy and are also eligible for IVT; please see the expert consensus statement below for this situation.
Recommendation
For patients with acute ischaemic stroke on awakening from sleep, who were last seen well more than 4.5 h earlier, who have MRI DWI-FLAIR mismatch, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: High ⊕⊕⊕⊕
Strength of recommendation: Strong ↑↑
For patients with acute ischaemic stroke on awakening from sleep, who have CT or MRI core/perfusion mismatch* within 9 h from the midpoint of sleep, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
*In the EOS individual participant data meta-analysis,46 core/perfusion mismatch was assessed with an automated processing software and defined as follows:
- Infarct core** volume < 70 ml
- and Critically hypoperfused† volume/Infarct core** volume > 1.2
- and Mismatch volume > 10 ml
** rCBF <30% (CT perfusion) or ADC < 620 µm2/s (Diffusion MRI)
† Tmax >6 s (perfusion CT or perfusion MRI)
Additional information
As of September 2020, two trials on intravenous thrombolytic treatment in patients with a wake-up stroke are ongoing (NCT03181360 [TWIST], and NCT01455935 [WASSABI]).
Expert consensus statement
For patients presenting directly to a thrombectomy centre with acute ischaemic stroke on awakening from sleep, who would be eligible for both IVT and mechanical thrombectomy, 6 of 9 group members suggest IVT before MT.
For patients presenting to a non-thrombectomy centre with acute ischaemic stroke on awakening from sleep, who would be eligible for both IVT and mechanical thrombectomy, 7 of 9 group members suggest IVT before MT.
5. Tenecteplase
PICO 5.1 In patients with acute ischaemic stroke of < 4.5 h duration, does IVT with tenecteplase lead to better functional outcome than IVT with alteplase?
Analysis of current evidence
Tenecteplase has pharmacological advantages over alteplase. It has a higher fibrin affinity, longer half-life, and can be administered with a single intravenous bolus injection. We identified 3 RCTs comparing tenecteplase with alteplase in ‘unselected’ patients with acute ischaemic stroke,47–49 which are reviewed in the present section, and two trials comparing tenecteplase with alteplase in selected patients with acute ischaemic stroke due to large vessel occlusion, which are discussed in the next section (PICO 5.2) in order to limit heterogeneity in meta-analyses.50,51
In the Phase IIB/III Trial of Tenecteplase in Acute Ischemic Stroke (TNK-S2B), 112 patients were randomised within three hours of stroke onset to tenecteplase 0.1 mg/kg, 0.25 mg/kg, 0.4 mg/kg, or alteplase 0.9 mg/kg. The first step of the trial aimed at finding the optimal dose of tenecteplase using a composite outcome measure, and the second step aimed at testing whether this dose was superior to alteplase 0.9 mg/kg in improving functional outcome at three months.47 The trial was terminated prematurely because of slow recruitment. The adaptive dose selection procedure suggested that tenecteplase 0.4 mg/kg was inferior to the two other doses due to an excess of sICH (incidence rate 15.8%, 95% CI: 5.5–37.6%). The proportion of patients with good functional outcome (mRS 0–2) at three months did not differ between the treatment arms, but the study was underpowered for this analysis.
In the Alteplase-Tenecteplase Trial Evaluation for Stroke Thrombolysis (ATTEST) trial, 104 patients were randomised to tenecteplase 0.25 mg/kg or alteplase 0.9 mg/kg within 4.5 h of stroke onset.48 The primary outcome measure was the percentage of penumbra salvaged at 24–48 h, defined as CT perfusion-defined penumbra volume at baseline minus plain CT infarct volume at 24–48 h. Three-quarters of patients had an arterial occlusion on CT angiography. Mechanical thrombectomy was not performed. There were no significant differences for the primary outcome measure or for the secondary outcome measures of mRS scores 0–1 at 90 days (OR 1.1, 95% CI: 0.3–3.5) or sICH.
In the Norwegian Tenecteplase Stroke Trial (NOR-TEST), 1100 patients were randomised to tenecteplase 0.4 mg/kg or alteplase 0.9 mg/kg within 4.5 h of stroke onset or awakening with stroke.49 The trial aimed to show superiority for tenecteplase, and the primary outcome measure was excellent outcome at three months (mRS score 0–1). The included patients had mild strokes (median NIHSS score 4) and 18% of the patients had a stroke mimic. There was no difference in the proportion of patients with excellent outcome (OR 1.08, 95% CI: 0.84–1.38, P = 0.52), and there was no significant difference in the incidence of sICH.
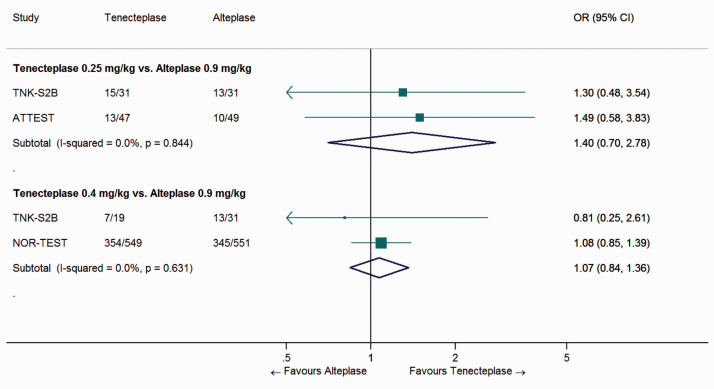
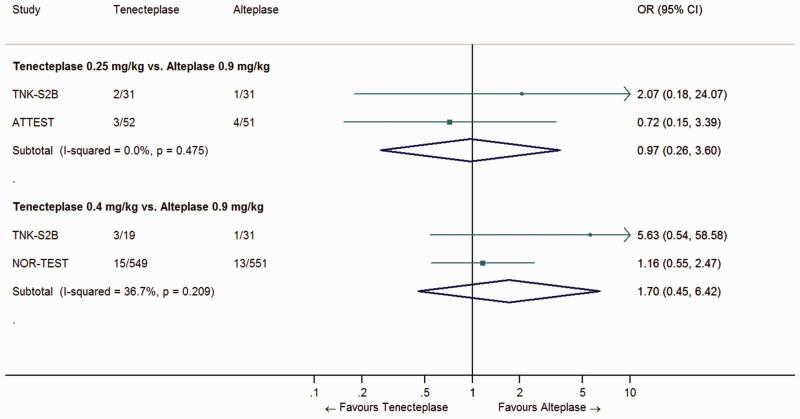
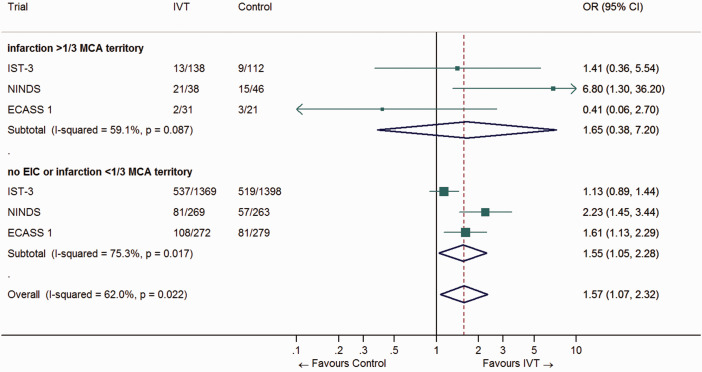
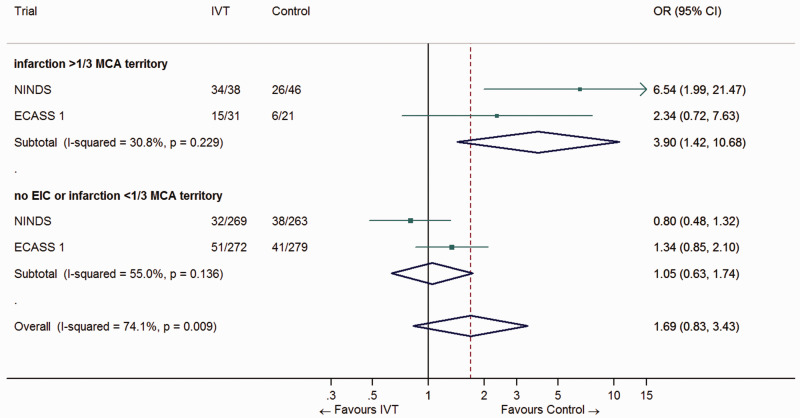
We performed a meta-analysis of study-level data, and found no significant difference between tenecteplase and alteplase in the proportion of patients with excellent (Figure 5) or good outcome at three months (data not shown), irrespective of the tenecteplase dose. There was no significant difference in the incidence of sICH (Figure 6). A published meta-analysis also found similar functional outcomes in the two treatment groups.52
Figure 5.
Pooled odds ratio for excellent outcome (mRS 0–1) in ‘unselected’ patients with ischaemic stroke of < 4.5 h duration, treated with tenecteplase (0.25 or 0.4 mg/kg) vs. alteplase (0.9 mg/kg).
Figure 6.
Pooled odds ratio for sICH in ‘unselected’ patients with ischaemic stroke of < 4.5 h duration, treated with tenecteplase (0.25 or 0.4 mg/kg) vs. alteplase (0.9 mg/kg).
The quality of the evidence was deemed low (see Table 4 for justification). None of the trials were designed to show non-inferiority of tenecteplase compared to alteplase.
Recommendation
For patients with acute ischaemic stroke of <4.5 h duration and not eligible for thrombectomy, we suggest intravenous thrombolysis with alteplase over intravenous thrombolysis with tenecteplase. Please see paragraph 5.2 for patients eligible for mechanical thrombectomy.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↑?
Table 4.
GRADE evidence profile for PICO 5.1.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with tenecteplase 0.25 mg/kg | IVT with alteplase 0.9 mg/kg | Relative(95% CI) | Absolute(95% CI) | ||
| Tenecteplase 0.25 mg/kg vs. Alteplase 0.9 mg/kg (‘unselected’ patients) | ||||||||||||
| mRS 0–1 at three months | ||||||||||||
| 2 | randomised trials | seriousa | not serious | seriousb | not serious | none | 28/78(35.9%) | 23/80(28.7%) | OR 1.40(0.70–2.78) | 73 more per 1 000(from 67 fewer to 241 more) | ⨁⨁◯◯LOW | CRITICAL |
| Death at three months | ||||||||||||
| 2 | randomised trials | seriousa | not serious | seriousb | not serious | none | 15/78(19.2%) | 14/80(17.5%) | OR 0.97(0.45–2.09) | 4 fewer per 1 000(from 88 fewer to 132 more) | ⨁⨁◯◯LOW | CRITICAL |
| sICH | ||||||||||||
| 2 | randomised trials | serious a | not serious | serious c | not serious | none | 5/83(6.0%) | 5/82(6.1%) | OR 1.12(0.49–2.52) | 7 more per 1 000(from 30 fewer to 80 more) | ⨁⨁◯◯LOW | CRITICAL |
| Tenecteplase 0.40 mg/kg vs. Alteplase 0.9 mg/kg (‘unselected’ patients) | ||||||||||||
| mRS 0–1 at three months | ||||||||||||
| 2 | randomised trials | very serious a,d | not serious | not serious | not serious | none | 361/568(63.6%) | 358/582(61.5%) | OR 1.07(0.84–1.36) | 16 more per 1 000(from 42 fewer to 70 more) | ⨁⨁◯◯LOW | CRITICAL |
| Death at three months | ||||||||||||
| 2 | randomised trials | serious d | not serious | not serious | not serious | none | 32/568(5.6%) | 34/582(5.8%) | OR 1.03(0.62–1.72) | 2 more per 1 000(from 21 fewer to 38 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| sICH | ||||||||||||
| 2 | randomised trials | serious d | not serious | not serious | serious e | none | 18/568(3.2%) | 14/582(2.4%) | OR 1.70(0.45–6.42) | 16 more per 1 000(from 13 fewer to 113 more) | ⨁⨁◯◯LOW | CRITICAL |
aThe TNK-S2B trial was terminated prematurely – in the dose finding phase – because of slow recruitment. The following phase would have investigated the superiority of Tenecteplase over Alteplase 0.9 mg/kg.bDifferences in populationscDifferent definitions of sICH were used across studies.dIn NOR-TEST, 18% of included patients had a stroke mimic and were distributed similarly between the Tenecteplase and Alteplase arm.eClinical recommendation (tenecteplase or alteplase) would markedly differ if the upper versus the lower boundary of the 95% CI of the OR represents the truth.
Additional information
A meta-analysis of 5 randomized trials (TNK-S2B, Tenecteplase versus Alteplase for Acute Ischemic Stroke [TAAIS], ATTEST, NOR-TEST, Tenecteplase versus Alteplase before Endovascular Therapy for Ischemic Stroke [EXTEND-IA TNK]) suggested that there is enough evidence to conclude that tenecteplase is non-inferior to alteplase for acute ischemic stroke (risk difference for mRS 0–1: 4%, 95% CI: –1% to 8%).53 However, this result was mostly driven by the inclusion of EXTEND-IA TNK and TAAIS in the meta-analysis, which enrolled only patients with large vessel occlusion as opposed to the other trials. Furthermore, the high proportion of stroke mimics in NOR-TEST could have biased results towards non-inferiority. Of note, the non-inferiority margin was selected using data from a RCT comparing two doses of alteplase (0.9 mg/kg vs. 0.6 mg/kg).54
There are ongoing trials of tenecteplase for acute ischemic stroke (ATTEST-2 [NCT02814409], Tenecteplase versus Alteplase for Stroke Thrombolysis Evaluation (TASTE; ACTRN12613000243718), A Randomized Controlled Trial of TNK-tPA Versus Standard of Care for Minor Ischemic Stroke With Proven Occlusion (TEMPO-2; NCT02398656). We encourage enrolment into ongoing trials.
PICO 5.2 In patients with acute ischaemic stroke of < 4.5 h duration and with large vessel occlusion, who are candidates for mechanical thrombectomy, and for whom intravenous thrombolysis is considered before thrombectomy, does IVT with tenecteplase lead to better functional outcome than IVT with alteplase?
Analysis of current evidence
In the TAAIS trial, 75 patients were randomised to tenecteplase 0.1 mg/kg or 0.25 mg/kg or alteplase 0.9 mg/kg within 6 h of stroke onset.50 Patient selection was based on the finding of occlusion of the anterior, middle, or posterior cerebral artery on CT angiography and a CT perfusion lesion volume that was at least 20 ml and at least 20% greater than the infarct core on CT perfusion. Mechanical thrombectomy was not performed. The two co-primary outcome measures were the percentage of the perfusion lesion that was reperfused at 24 h after treatment (as assessed by perfusion MRI) and the change on the NIHSS score between baseline and 24 h. Tenecteplase was superior to alteplase for both co-primary outcome measures. At three months, good outcome (mRS 0–2) was observed in 72% of patients in the pooled tenecteplase groups vs. 44% in the alteplase group (P = 0.02). The rate of symptomatic intracerebral haemorrhage did not differ significantly between the groups. In the dose-tier analysis, tenecteplase 0.25 mg/kg was associated with clinical improvement during the first 24 h and a non-significant increase in the proportion of patients with good outcome at three months (P = 0.11). The frequency of sICH was similar in the two tenecteplase groups (4%).
The EXTEND-IA TNK trial compared tenecteplase 0.25 mg/kg with alteplase 0.9 mg/kg within 4.5 h of symptom onset in 202 patients with large vessel occlusion (internal carotid artery, first and second segments of the middle cerebral artery, or the basilar artery) who were candidates for mechanical thrombectomy.51 The trial was designed to demonstrate non-inferiority, but after testing for non-inferiority, superiority testing was performed as pre-specified. The primary outcome measure was reperfusion greater than 50% of the involved ischaemic territory or absence of retrievable thrombus at the time of the initial angiographic assessment, and was found in 22% of the patients treated with tenecteplase versus 10% of those treated with alteplase (p for non-inferiority = 0.002; p for superiority = 0.03). Tenecteplase was borderline associated with better 90-day functional outcome than alteplase (cOR 1.7, 95% CI: 1.0–2.8, P = 0.04 – adjusted on age and baseline NIHSS score). There were no significant differences in the proportions of patients with good (P = 0.06), excellent outcome (P = 0.23) or early neurological improvement (P = 0.70). Symptomatic intracerebral haemorrhage occurred in 1% of the patients in each group.
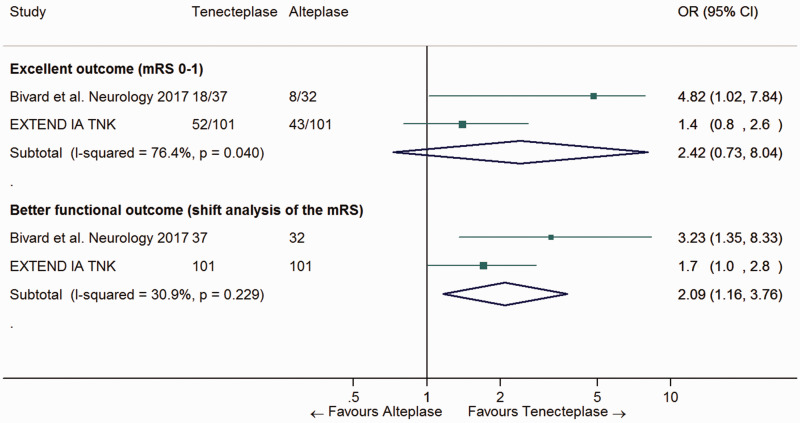
A meta-analysis of patients with large vessel occlusion in EXTEND-IA TNK and TAAIS showed that tenecteplase was associated with a higher likelihood of complete recanalisation (OR 2.01, 95% CI: 1.04–3.87, P = 0.04).52 Furthermore, Bivard et al. conducted a pooled patient subgroup analysis of TAAIS and ATTEST suggesting that tenecteplase compared to alteplase was associated with higher complete recanalization rates at 24 h (71% vs. 43%; p < 0.001) and higher rates of three-month excellent outcome (mRS-scores of 0–1; OR 4.82, 95% CI: 1.02–7.84, P = 0.05) in 69 patients with baseline intracranial occlusion [Thrombolysis in Cerebral Infarction (TICI) grades 0–1].55 This study also suggested that vessel occlusion status (complete vs. partial or no occlusion) was a modifier of the effect of tenecteplase – compared with alteplase – regarding three-month functional outcome (P for interaction =0.01). Some of the included patients had distal vessel occlusion and would therefore not currently be eligible for mechanical thrombectomy.14
We have conducted a study-level meta-analysis of EXTEND-IA TNK and the subgroup of patients with complete vessel occlusion in the pooled analysis by Bivard et al. (Figure 7).55 The pooled OR for excellent outcome and better functional outcome were 2.42 (95% CI: 0.73–8.04) and 2.09 (1.16–3.76), respectively.
Figure 7.
Pooled odds ratio for excellent outcome (mRS 0–1) and better functional outcome (common OR across the whole range of the mRS) in patients with ischaemic stroke of < 4.5 h duration who have documented vessel occlusion and were randomized to IVT with tenecteplase 0.25 mg/kg vs. IVT with Alteplase 0.9 mg/kg.
The study by Bivard et al.55 is a pooled patient subgroup analysis of the TAAIS50 and ATTEST48 randomized trials. The ORs from EXTEND IA TNK51 were adjusted on age and baseline NIHSS score.
EXTEND-IA TNK 2 was a randomised trial comparing two different doses of intravenous tenecteplase (0.25 mg/kg vs. 0.4 mg/kg) within 4.5 h of stroke onset in 300 patients who subsequently underwent mechanical thrombectomy.56 The proportion of patients with greater than 50% reperfusion of the previously occluded vascular territory (eTICI ≥2b50,57 primary endpoint) before thrombectomy was 19% in the two arms. There was not difference between treatment groups regarding functional outcome at three months (adjusted common OR for better functional outcome 0.96, 95% CI: 0.74–1.24, P = 0.73) and mortality. The rate of sICH according to the SITS-MOST definition was non-significantly higher in the 0.4 mg/kg arm: 4.7% vs. 1.3%, RR 3.50 (95% CI: 0.74–16.62, P = 0.12).
Our recommendation is based on one small RCT, with a non-clinical primary outcome measure and a post-hoc pooled subgroup analysis of 2 other small RCTs (Figure 7). The quality of the evidence is graded as low (see Table 5 for justification).
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration and with large vessel occlusion who are candidates for mechanical thrombectomy and for whom intravenous thrombolysis is considered before thrombectomy, we suggest intravenous thrombolysis with tenecteplase 0.25 mg/kg over intravenous thrombolysis with alteplase 0.9 mg/kg.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↑?
Table 5.
GRADE evidence profile for PICO 5.2.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with tenecteplase | IVT with alteplase | Relative(95% CI) | Absolute(95% CI) | ||
| mRS 0–1 at three months | ||||||||||||
| 3 | randomised trials | not serious | seriousa | seriousb | not serious | none | 52/101(51.5%) | 43/101(42.6%) | OR 2.42(0.73–8.04) | 216 more per 1 000(from 75 fewer to 431 more) | ⨁⨁◯◯LOW | CRITICAL |
| Improved mRS score at three months (shift analysis) | ||||||||||||
| 3 | randomised trials | not serious | seriousa | seriousb | not serious | none | cOR 2.09(1.16–3.76) | – per 1 000(from – to –) | ⨁⨁◯◯LOW | CRITICAL | ||
| Death at three months | ||||||||||||
| 1 | randomised trials | not serious | not serious | seriousc | not serious | none | 10/101(9.9%) | 18/101(17.8%) | OR 0.4(0.2–1.1) | 98 fewer per 1 000(from 137 fewer to 14 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| sICH | ||||||||||||
| 1 | randomised trials | not serious | not serious | not serious | very seriousd | none | 1/101(1.0%) | 1/101(1.0%) | OR 1.0(0.1–16.2) | – per 1 000(from – to 0 fewer) | ⨁⨁◯◯LOW | CRITICAL |
The results regarding functional outcome are based on Bivard et al.55 (pooled analysis of the TAAIS50 and ATTEST48 trials) and the EXTEND IA TNK trial51 (Figure 7). The results about death and sICH are solely based on the EXTEND IA TNK trial.aIn EXTEND IA TNK, tenecteplase was only significantly associated with better functional outcome in shift analysis of the mRS. Furthermore, other RCTs in unselected patients did not suggest superiority of tenecteplase over alterplase.bThis result is based on a secondary outcome of the EXTEND IA TNK trial and subgroup analyses of TAAIS and ATTEST. In those last 2 trials, some patients had distal vessel occlusion (M2, M3, ACA, PCA).cThe primary endpoint was radiological, not clinical.dOnly one event in each treatment group.
Additional information
Tenecteplase in Stroke Patients Between 4.5 and 24 h (TIMELESS; NCT03785678) is an ongoing trial of tenecteplase versus placebo for acute ischemic stroke patients with large vessel occlusion presenting in late time windows.
6. Alternative doses
PICO 6.1 In patients with acute ischaemic stroke of < 4.5 h duration, does intravenous thrombolysis with low-dose alteplase lead to non-inferior (not worse) functional outcome compared to standard-dose alteplase?
Analysis of current evidence
The literature search identified one RCT comparing low dose (0.6 mg/kg) with standard dose (0.9 mg/kg) of alteplase in 3310 patients treated with IVT within 4.5 h of stroke onset, the Enhanced Control of Hypertension and Thrombolysis Stroke Study (ENCHANTED).54 The trial aimed to show non-inferiority of the lower dose. About two-thirds of patients were from Asia. Unfavourable functional outcome (mRS scores 2–6) was seen in 53.2% in the low-dose and 51.1% in the standard-dose group, which did not demonstrate non-inferiority (OR 1.09, 95% CI: 0.95–1.25, P for non-inferiority = 0.51).58 The rate of sICH was lower in the low-dose group (1.0% vs. 2.1%, P = 0.01). Mortality at three months did not differ significantly between the groups (8.5% and 10.3%, respectively, P = 0.07). The pre-specified subgroup analyses did not identify patients who benefitted from the low-dose therapy.59–61 but patients using antiplatelet drugs before their strokes had non-significantly better functional outcomes after low-dose alteplase than other patients (OR 0.84, 95% CI: 0.62–1.12 versus OR 1.16, 95% CI: 0.99–1.36, p for interaction = 0.053).62,63 This association was further attenuated in analyses adjusted for potential confounders.62,63
The evidence for this recommendation is limited to one trial. However, the trial was adequately powered to address its scientific question and we could not identify reason that would lead to downgrade the quality of evidence regarding risk of bias, inconsistency, indirectness, or imprecision. The quality of evidence was therefore rated as high. The trial did not show non-inferiority of low-dose alteplase, and the recommendation is therefore strong.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration who are eligible for intravenous thrombolysis, we recommend standard-dose alteplase (0.9 mg/kg) over low-dose alteplase.
Quality of evidence: High ⊕⊕⊕⊕
Strength of recommendation: Strong ↑↑
Additional information
The ENCHANTED trial did not show non-inferiority of low-dose alteplase, despite the fact that almost two-thirds of the patients were from Asia (who have presumed higher risk of sICH). There was also no imbalance in the baseline characteristics that could explain the results. For example, the percentage of large-artery occlusions and successful recanalisation were similar in the two groups.
There are several older Asian registry studies that have inconsistent results regarding the optimal dose of alteplase in Asian populations.64–72
7. Adjunctive therapies (i.e. antithrombotic agents, ultrasound)
PICO 7.1 In patients with acute ischaemic stroke of < 4.5 h duration, does antithrombotic agents in addition to IVT lead to better functional outcome than IVT alone?
Analysis of current evidence
Re-occlusion of a cerebral artery occurs in 14%–34% of patients who have achieved recanalisation after IVT with alteplase, and is associated with clinical deterioration and poor outcome.73,74 It has been suggested that the use of antithrombotic agents (aspirin, glycoprotein IIb/IIIa inhibitors or thrombin inhibitors) during or after alteplase infusion might reduce the risk of re-occlusion and improve functional outcome.75,76
The effect of intravenous aspirin as an adjunct therapy to alteplase was tested in the Antiplatelet therapy in combination with Rt-PA Thrombolysis in Ischemic Stroke (ARTIS) trial.77 A total of 642 patients treated with alteplase were randomly assigned to 300 mg intravenous aspirin within 90 min of alteplase bolus or to no additional treatment. Oral antiplatelet therapy was given 24 h following alteplase treatment in both groups. The trial was terminated prematurely because of an excess of sICH (assessed in a non-blinded fashion) and no evidence of benefit in the aspirin group. The OR for good outcome (mRS 0–2 at three months) with intravenous aspirin was 0.91 (95% CI: 0.66–1.26, P = 0.58), and the relative risk for sICH, defined as in the third European Cooperative Acute Stroke Study (ECASS-3) trial,78 was 2.78 (95% CI: 1.01–7.63, P = 0.04). Of note, follow-up imaging was not systematically performed in patients without neurological deterioration.
Eptifibatide is a glycoprotein IIb/IIIa inhibitor that is being investigated as an adjunct to intravenous thrombolysis. One randomised-controlled trial of 94 patients compared low-dose alteplase (0.3 mg/kg and 0.45 mg/kg) combined with eptifibatide to standard-dose alteplase alone, and did not raise major safety concerns (OR for any ICH with combination therapy compared to alteplase alone: 0.28, 95% CI: 0.06–1.23).79 Another trial randomised 126 patients 4:1 to low-dose alteplase (0.6 mg/kg) plus eptifibatide or standard-dose alteplase alone, and found a non-significantly lower risk of sICH in the combination group (OR 0.15, 95% CI: 0.01–1.40, P = 0.053).80 The safety of eptifibatide as an adjunct to alteplase low-dose or standard-dose has also been reported in observational studies.81,82
We identified no RCTs of the glycoprotein IIb/IIIa inhibitor tirofiban as an adjunctive therapy to alteplase, but there are observational data hinting that tirofiban might be safe (no sICH in 14 patients treated with tirofiban + standard-dose alteplase), although uncertainties remain.83
Argatroban is a direct thrombin inhibitor that has been given as adjunct therapy to alteplase. One small observational study of 65 patients showed that combination therapy compared to alteplase alone had a sICH rate of 4.6% in patients with proximal cerebral artery occlusion.84 A RCT of 90 patients treated with alteplase randomised patients to no argatroban, argatroban bolus followed by low-dose infusion of argatroban, or to argotroban bolus followed by standard-dose infusion of argatroban for 48 h.85 No difference in the rates of sICH was observed across the three groups (10, 13 and 7%, respectively; RR (low-dose argatrobran vs alteplase alone:1.27; 95% CI: 0.32–5.05; RR (high-dose argatrobran vs alteplase alone:0.60; 95% CI: 0.11–3.41), as were the proportions of patients with mRS scores 0–1 at 90 days (21, 30 and 32%, respectively; RR (low-dose argatrobran vs alteplase alone:1.50; 95% CI: 0.64–3.49; RR (high-dose argatrobran vs alteplase alone:1.63; 95% CI: 0.72–3.72). However, the small sample of this trial should be taken into account in the interpretation of these findings.
The recommendation is based on the ARTIS trial and very small randomized trials assessing safety rather than efficacy. The quality of evidence is therefore graded as low.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, we recommend no antithrombotic drugs within 24 h of intravenous thrombolysis over antithrombotic drugs as an adjunct therapy to intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↓↓
Additional information
The effects of eptifibatide and argatroban as adjuncts to alteplase will be further investigated in the ongoing phase Multi-arm Optimization of Stroke Thrombolysis (MOST) trial (NCT03735979). In this trial, 1200 patients treated with standard-dose alteplase within three hours of stroke onset will be randomised to intravenous argatroban, eptifibatide or placebo, and the primary effect variable is functional outcome at 90 days. Patients may also receive mechanical thrombectomy per usual care.
PICO 7.2 In patients with acute ischaemic stroke of < 4.5 h duration, does ultrasound augmentation of IVT lead to better functional outcome than IVT alone?
Analysis of current evidence
Ultrasound delivers mechanical pressure waves to the clot, exposing more thrombus surface to circulating alteplase, which may potentiate fibrinolytic activity.86,87 Moreover, intravenous gaseous microspheres have been introduced with ultrasound as an alternative to fibrinolytic agents to recanalise discrete peripheral thrombotic arterial occlusions or acute arteriovenous graft thromboses.86,87 Small RCTs of high-frequency ultrasound in combination with thrombolytic treatment (sometimes referred to as ‘sonothrombolysis’) have shown promising results in patients who did not receive mechanical thrombectomy.88,89 The Combined Lysis of Thrombus in Brain Ischemia Using Transcranial Ultrasound and Systemic t-PA (CLOTBUST) trial of transcranial ultrasound and meta-analyses of other similar studies have reported that ultrasound could at least double the chance of early recanalisation.90–92 In the CLOTBUST trial of 126 patients, sonothrombolysis was also associated with a higher likelihood of excellent outcome (secondary endpoint, mRS 0–1 at three months) in the subgroup of patients with pre-treatment NIHSS scores ≥10 points.93
These findings were not reproduced in two larger RCTs. The Norwegian Sonothrombolysis in Acute Stroke Study (NOR-SASS) randomised 183 patients with or without evidence of proximal cerebral artery occlusion and without a lower cut-off for baseline NIHSS score to contrast-enhanced high-frequency sonothrombolysis or IVT with alteplase alone (with sham ultrasound monitoring).94,95 The primary endpoints were neurological improvement at 24 h defined as a NIHSS score of 0 or a reduction of ≥4 points compared with baseline NIHSS, and excellent functional outcome. The trial was prematurely terminated because of a lack of funding. The rates of neurological improvement at 24 h, excellent outcome at 90 days and sICH were similar in the two groups. Only 113 out of 183 enrolled patients (61%) were treated according to study protocol in NOR-SASS.
The Combined Lysis of Thrombus using Ultrasound and Systemic Tissue Plasminogen Activator for Emergent Revascularization (CLOTBUST-ER) trial enrolled 676 patients with NIHSS scores of ≥10 points who received IVT with alteplase within 4.5 h (3 h in North America) and were randomised to ultrasound enhancement of IVT or sham.96,97 Vascular imaging was not mandatory and mechanical thrombectomy was not performed. The primary endpoint was improvement in the mRS-score at 90 days. The trial was stopped early because of futility. The adjusted cOR for better functional outcome was 1.05 (95% CI: 0.77–1.45, P = 0.74) for patients treated within three hours and 1.06 (95% CI: 0.80–1.42, P = 0.67) for patients treated within 4.5 h. There was no difference in three-month mortality (OR 1.19, 95% CI: 0.74–1.92, P = 0.48) or sICH (OR 1.39, 95% CI: 0.51–3.95, P = 0.52).
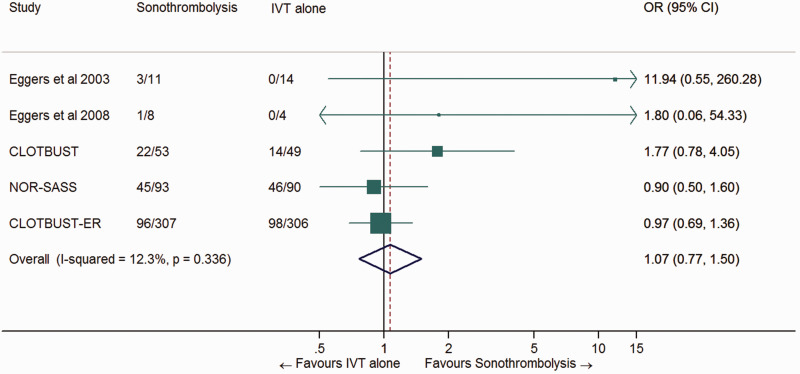
We performed a meta-analysis of the five largest RCTs88–90,95,97 and found no benefit in terms of excellent outcome (mRS score 0–1 at three months) with high-frequency ultrasound in combination with alteplase versus alteplase alone (OR 1.07, 95% CI: 0.77–1.50, P = 0.68, I2 = 12%, Figure 8).
Figure 8.
Pooled odds ratio for excellent outcome (mRS 0–1) in patients randomized to ultrasound augmentation of IVT vs. IVT alone.
All patients received IVT with alteplase.
The recommendation is based on the results of the meta-analysis including two phase 3 and three phase 2 RCTs. The quality of evidence was judged to be low (see Table 6 for justification).
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, we recommend against ultrasound augmentation in patients receiving intravenous thrombolysis.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↓↓
Table 6.
GRADE evidence profile for PICO 7.2.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ultrasound augmentation of IVT with alteplase | IVT with alteplase alone | Relative(95% CI) | Absolute (95% CI) | ||
| mRS 0–1 at three months | ||||||||||||
| 5 | randomised trials | seriousa | seriousb | not seriousc | not serious | none | 167/472(35.4%) | 158/463(34.1%) | OR 1.07(0.77–1.50) | 15 more per 1 000(from 56 fewer to 96 more) | ⨁⨁◯◯LOW | CRITICAL |
aIn the CLOTBUST trial, 19% of the randomized patients were not eligible for the analysis of functional outcome at three months, which was a secondary endpoint. The two trials by Eggers et al. were very small. Furthermore, two phase III trials were stopped early.bTwo small trials by the same group (Eggers et al., 2003, 2008) and one larger study (CLOTBUST) suggested a strong benefit of sonothrombolysis, whereas two large trials did not.cSome trials only included patients with proven arterial occlusion (Eggers et al., CLOTBUST), whereas other studies did not (NOR-SASS, CLOTBUST-ER).
8. Higher age, multimorbidity, frailty or prior disability
PICO 8.1 In patients with acute ischaemic stroke of < 4.5 h duration, who are over 80 years of age, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Most trials of IVT for ischaemic stroke have excluded patients who were over 80 years old or who had multimorbidity/frailty or pre-stroke disability. IST-3 included patients over 80 years of age and added substantial information on this patient group.9 Information about the effect of alteplase in elderly patients can also be found in meta-analyses of RCTs, either with individual patient data8,26,98 or on study-level.6
In the meta-analysis of individual participant data by Emberson et al., the OR for excellent outcome (mRS score 0–1) in patients >80 years treated with alteplase was 1.56 (95% CI: 1.17–2.08), compared to 1.25 (95% CI: 1.10–1.42) in patients ≤ 80 years of age, without evidence of difference in efficacy between the groups (P for interaction = 0.53).26 There was also no evidence in the pooled analysis that patients aged >80 years were at any greater risk of ICH than younger patients. Furthermore, age was not associated with increased risk of sICH in the ENCHANTED trial.59 The Thrombolysis in Elderly Stroke Patients in Italy (TESPI) trial, which investigated IVT with alteplase within three hours of stroke onset in 191 patients over the age of 80 years, was terminated early because the IST-3 trial provided evidence of treatment benefit in in this age group.99 The trial was underpowered and showed a non-significant effect on the proportion of good outcome (mRS score 0–2: 29% versus 23%).
The recommendation for patients who are over 80 years of age is based on an individual patient data meta-analysis of high quality.8,98
Recommendation
For patients with acute ischaemic stroke of <4.5 h duration, who are over 80 years of age, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: High ⊕⊕⊕⊕
Strength of recommendation: Strong ↑↑
Expert consensus statement
Nine of nine group members believe that age alone should not be a limiting factor for IVT, even in other situations covered in the present guidelines (e.g. wake-up stroke; ischaemic stroke of 4.5–9 h duration (known onset time) with CT or MRI core/perfusion mismatch; minor stroke with disabling symptoms).
PICO 8.2 In patients with acute ischaemic stroke of < 4.5 h duration, who have multimorbidity, frailty or prior disability, does intravenous thrombolysis with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
The literature search identified no trials that targeted patients with multimorbidity/frailty or those with pre-stroke disability. An analysis of observational data from 3017 patients in IST-3 used brain imaging findings before treatment with alteplase to identify patients with pre-existing ‘brain frailty’, such as old lesions, brain atrophy or leukoaraiosis. The risk of sICH was higher in patients with old infarct (OR 1.72, 95% CI: 1.18–2.51), and the chance of excellent functional outcome was lower (severe leukoaraiosis: OR 0.62, 95% CI: 0.50–0.78; severe brain atrophy: OR 0.75, 95% CI: 0.57–0.99; old infarct: OR 0.79, 95% CI: 0.64–0.96).100 However, no imaging findings, individually or combined, modified the effect of alteplase on functional outcome or sICH.100 Renal dysfunction, which is another marker of multimorbidity, was not associated with increased risk of sICH in the ENCHANTED trial,60 but was associated with increased risk of other haemorrhagic complications, death and poor functional outcome before and after adjustment for potential confounders in meta-analyses of observational studies.101–104 Finally, one observational study of patients with non-metastatic cancer, found that functional outcome after IVT with alteplase was comparable to that of other patients.105 These findings suggest that cancer should not be an absolute contraindication against thrombolytic treatment, although caution seems appropriate.
Patients with pre-existing disability are often not treated with alteplase.106 Despite high mortality rates, observational studies of patients with pre-existing disability have indicated that IVT may prevent further functional deterioration and that treatment is more beneficial the earlier it is given.107,108 Observational studies have not found evidence that pre-stroke disability is associated with an increased risk of ICH after thrombolytic treatment.107,109,110
The recommendations for patients with multimorbidity, frailty or pre-stroke disability is based on small observational studies, corresponding to a very low quality of evidence.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with multimorbidity, frailty or pre-stroke disability, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↑?
Additional information
The weak recommendations given above imply that the decision to treat must be made on an individual basis and that it must consider the patient’s values and preferences.
A single-centre observational study suggested that the outcome of patients with cognitive impairment no-dementia who are treated with IVT does not significantly differ from that of cognitively normal patients.111
9. Minor stroke and stroke with rapidly improving neurological signs
PICO 9.1 In patients with acute minor, disabling ischaemic stroke of < 4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
About half of all ischaemic strokes are initially minor (defined typically as NIHSS score < 5), but up to one third of patients with minor stroke are disabled or dead three months after the index event.112,113 Emberson et al. conducted an individual participant data meta-analysis of 9 RCTs of IVT with alteplase vs. placebo or open control, which included 666 patients (10%) with a baseline NIHSS score 0–4.8 All trials included in this meta-analysis excluded patients with non-disabling neurological deficits, except IST-3.9 The meta-analysis showed that the proportional benefit of alteplase was not statistically different in patients with mild, moderate and severe strokes (P for interaction = 0.06). In patients with baseline NIHSS score of 0–4, the OR for excellent outcome (mRS score 0–1 at three months) was 1.48 (95% CI: 1.07–2.06). These data support the use of alteplase in patients with minor disabling stroke.
One critical question is how ‘minor disabling stroke’ should be defined in clinical practice. No standardized definition has been used across trials included in the present meta-analysis, which relied on the subjective judgment of each investigator. An operational definition of a disabling deficit has since been proposed in the Potential of Rt-PA for Ischemic Strokes with Mild Symptoms (PRISMS) trial: ‘a deficit that, if unchanged, would prevent the patient from performing basic activities of daily living (i.e., bathing, ambulating, toileting, hygiene, and eating) or returning to work’.114
The quality of evidence for the recommendation is moderate (see Table 7 for justification).
Recommendation
For patients with acute minor, disabling ischaemic stroke of < 4.5 h duration, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
Table 7.
GRADE evidence profile for PICO 9.1.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| mRS 0–1 at three months (six months in IST-3) | ||||||||||||
| 9 | randomised trials | not serious | not serious | seriousa | not serious | none | 237/345(68.7%) | 189/321(58.9%) | OR 1.48(1.07–2.06) | 91 more per 1 000(from 16 more to 158 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| Fatal ICH within seven days | ||||||||||||
| 9 | randomised trials | not serious | not serious | seriousa | very seriousb | strong association | 3/345(0.9%) | 0/321(0.0%) | OR 3.90(1.46–10.44) | 9 more per 1 000(from 4 more to 25 more) | ⨁⨁◯◯LOW | |
Note: All results are based on the individual patient data meta-analysis by Emberson et al.aThis result is based on an analysis of subgroups of patients included in RCTs with various inclusion criteria. There was no clear definition of disabling stroke in patients with NIHSS 0–4.bThe number of events was extremely low.
PICO 9.2 In patients with acute minor, non-disabling ischaemic stroke of < 4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients with minor neurological deficits (NIHSS score 0–5) judged to not be clearly disabling within three hours of stroke onset were assessed in the PRISMS trial of IVT with alteplase vs. aspirin.114 A disabling deficit was defined as ‘a deficit that, if unchanged, would prevent the patient from performing basic activities of daily living (ie, bathing/dressing, ambulating, toileting, hygiene, and eating) or returning to work’. Due to slow recruitment and insufficient funding, the trial was terminated after inclusion of 313 patients, while the calculated sample size was 948. The adjusted risk difference for excellent outcome (mRS 0–1 at three months) with alteplase was –1.1% (95% CI: –9.4 to 7.3%) and the cOR for better functional outcome was 0.81 (95% CI: 0.5–1.2). The risk of sICH (defined as any neurological worsening within 36 h attributed to ICH by local investigators) was significantly higher in the alteplase group (risk difference 3.3%, 95% CI: 0.8–7.4), and there were more patients with serious adverse events (mostly intracranial/intracerebral hemorrhage) in the alteplase group (risk difference 12.9%, 95% CI: 4.1–21.7%). A limitation of this trial was missing three-month mRS score evaluations in 10% of enrolled patients.
Because IST-3 had not explicitly excluded patients with non-disabling neurological deficits, we also used data from that trial.9 Among the subgroup of patients with NIHSS 0–5 in IST-3, the adjusted OR for good functional outcome (Oxford Handicap Scale score 0–2) with alteplase was 0.85 (95% CI: 0.52–1.38).
The recommendation is based on one relatively small RCT that was stopped early and one trial that did not explicitly exclude patients with non-disabling ischaemic stroke. The quality of the evidence is therefore graded as moderate.
Recommendation
For patients with acute minor non-disabling ischaemic stroke of < 4.5 h duration, we suggest no intravenous thrombolysis. For patients with minor stroke and large-vessel occlusion, please refer to the section below (PICO 9.3).
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Weak ↓?
Additional information
A list of examples of non-disabling symptoms was provided to each participating centre in the PRISMS trial and in the published protocol115: isolated mild aphasia (patient still able to communicate meaningfully), isolated facial droop, mild cortical hand (especially non-dominant: NIHSS score = 0), mild hemimotor loss, hemisensory loss, mild hemisensorimotor loss and mild hemiataxia (patient still able to ambulate). Importantly, the two most common neurological deficits of patients enrolled in PRISMS were mild sensory loss (46%) and facial palsy (39%).
PICO 9.3 In patients with acute minor, non-disabling ischaemic stroke of < 4.5 h duration, and with proven large vessel occlusion, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients with large vessel occlusion have a higher risk of stroke progression and poor prognosis than other patients.116 The literature search identified no RCT of IVT with alteplase in patients with NIHSS scores of 0–5 with non-disabling neurologic deficits and with proven intracranial large artery occlusion. TEMPO-1 was a case series of 50 patients with NIHSS sores 0–5 (disabling or non-disabling symptoms) who were given tenecteplase 0.1 or 0.25 mg/kg for acute ischaemic stroke due to any proven and relevant intracranial occlusion.117 The TEMPO-2 trial (NCT02398656) is an ongoing RCT that compares tenecteplase with standard care in a similar population.
Recommendation
For patients with acute minor non-disabling ischaemic stroke of < 4.5 h duration, and with proven large-vessel occlusion, there is insufficient evidence to make an evidence-based recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Additional information
Recommendations for management of patients with large artery occlusions are also provided in the European Guidelines for mechanical thrombectomy.14 Trials are underway to test the effectiveness of thrombectomy in patients with large-artery occlusion and NIHSS scores 0–5 (In Extremis/Minor Stroke Therapy Evaluation [MOSTE; NCT 03796468], Endovascular Therapy for low NIHSS Ischemic Strokes [ENDOLOW; NCT 04167527]). In addition, two recent multicentre observational studies suggest a potential beneficial effect of IVT118 and bridging therapy119 in acute ischaemic stroke patients with minor stroke (NIHSS-scores < 6) and large vessel occlusion.
Expert consensus statement
For patients with acute minor, non-disabling ischaemic stroke of < 4.5 h duration, and with large-vessel occlusion, 6 of 8 group members suggest intravenous thrombolysis with alteplase.
One group member (WW) did not vote or comment on this chapter because he has been involved in the data monitoring committee of a trial related to this topic (TEMPO-2).
PICO 9.4 In patients with acute ischaemic stroke of < 4.5 h duration, and with rapidly improving neurological signs, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
We found no evidence of direct relevance for this question. The literature search did not identify any RCT of IVT in patients with rapidly improving symptoms, although the PRISMS trial included about 5% of such patients.114 One large observational study of 29,200 patients with mild or rapidly improving symptoms, who did not receive IVT, showed that unfavourable outcomes were common (28.3% were not discharged to home, and 28.5% were unable to ambulate without assistance at hospital discharge), and strongly associated with baseline NIHSS score.120
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and rapidly improving neurological signs, which are still disabling, there is insufficient evidence to make a recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Additional information
Rapidly improving stroke symptoms were a contraindication in the NINDS trial.17 The original intent was to avoid inclusion of transient ischaemic attack (TIA) patients, who recover completely without treatment.121 A working group of investigators from the pivotal NINDS trial that reviewed this exclusion criterion concluded that patients with improvement of any degree, but with a persisting neurological deficit that is potentially disabling, should be treated with alteplase.121 The authors performed structured interviews of the original NINDS clinical trialists to form this conclusion.
Expert consensus statement
For patients with acute ischaemic stroke of < 4.5 h duration, and rapidly improving neurological signs, which are still disabling, 8 of 9 group members suggest intravenous thrombolysis with alteplase.
The group agreed that the treatment decision should be based on the clinical status at presentation, and that it is not justifiable to wait for resolution of symptoms.
10. Severe stroke
PICO 10.1 In patients with severe acute ischaemic stroke of < 4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Severe stroke can be defined clinically (e.g. NIHSS score >25), or with CT or other brain imaging prior to IVT, e.g. visible infarction in more than 1/3 of the middle cerebral artery territory or an Alberta Stroke Program Early CT Score (ASPECTS) of < 7.122
Clinically severe stroke
A study-level meta-analysis classified RCTs recruiting patient with ‘more severe stroke’ as trials with a case fatality of ≥20% in the control group.6 There was no evidence of heterogeneity in the effect of IVT with alteplase on death or disability between trials with different levels of average stroke severity, but this study did not use the threshold of NIHSS score 25 to define severe stroke.
In the individual participant data meta-analysis by Emberson et al,8 there was no clear evidence of heterogeneity in the effect of alteplase on excellent outcome (mRS 0–1) between groups of patients with different baseline NIHSS scores, after controlling for age and time to treatment (p for interaction = 0.06). In the 622 participants with the highest level of stroke severity (NIHSS score ≥22) alteplase improved the odds of excellent outcome (OR 3.25, 95% CI: 1.42–7.47; Table 8).8 Regarding for better functional outcome), there was no evidence of an interaction (P for interaction = 0.72) between higher NIHSS score and lesser benefit from alteplase.26
Table 8.
GRADE evidence profile for PICO 10.1 – Clinically severe stroke.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| mRS 0–1 at three months | ||||||||||||
| 9 | randomised trials | seriousa | not serious | seriousb | not serious | strong association | 22/309(7.1%) | 8/313(2.6%) | OR 3.25(1.42–7.47) | 53 more per 1 000(from 10 more to 138 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| Fatal ICH with seven days | ||||||||||||
| 9 | randomised trials | seriousa | not serious | seriousb | seriousc | very strong association | 21/309(6.8%) | 2/313(0.6%) | OR 10.94(2.54–47.15) | 59 more per 1 000(from 10 more to 226 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
Note: All results are based on the individual participant data meta-analysis by Emberson et al.8aAlthough the 9 RCTs included in the individual patient data meta-analysis had patients with NIHSS ≥22, in many trials, patients with clinically very severe stroke (e.g. NIHSS >25 in ECASS-3) or radiologically severe stroke (e.g. attenuation of >1/3 of the MCA in ECASS 2 and ATLANTIS B) were excluded. Therefore, a selection bias is likely: patients with clinically severe stroke were not indiscriminately randomized in those trials.bThis result is based on an independent patient data meta-analysis of subgroups of 9 trials, and was restricted to patients with NIHSS ≥ 22. It is uncertain whether those results would also apply to patients with very severe stroke (e.g., NIHSS >25 or coma).cThe confidence interval is very wide
In IST-3, where the subgroup of patients with NIHSS score ≥25 was reported specifically, there was evidence of an interaction (P = 0.003) between stroke severity and the effect alteplase on good outcome (mRS score 0–2), with greater relative benefit in patients with more severe stroke. In the small subgroup of 146 patients with the most severe strokes (NIHSS scores ≥25) alteplase-treated patients were non-significantly more likely to have a good outcome than patients in the control group (OR 7.43, 95% CI: 0.43–129.0).9
The individual participant data meta-analysis showed that the absolute risk of fatal ICH due to IVT with alteplase was highest in those participants with the highest stroke severity (NIHSS scores ≥22, 6.8% vs 0.6%; Table 8),8 although the odds of fatal ICH with alteplase was similar in patients with high or low stroke severity. Altogether, these studies do not provide evidence that patients with the highest level of stroke severity have a lesser proportional benefit from alteplase.
Extensive ischaemic change on baseline imaging
Studies have also used brain imaging to define severe stroke. A Cochrane review did not demonstrate any important statistical difference between the effect of alteplase in those with more and in those with less extensive ischaemic change on baseline CT scan.6 We found no individual participant data meta-analysis of baseline brain imaging findings in patients in the large trials of alteplase. Although the presence of a greater degree of low attenuation on brain CT is associated with a much poorer outcome after ischaemic stroke,123,124 there is no evidence that patients with larger lesion or with more tissue attenuation benefit less from alteplase in analyses from 3 individual trials, after adjustment for time to randomisation.100,125,126 However, there is no trial specifically addressing this question, and extensive baseline ischemia was an exclusion criteria in the major IVT trials.
We have conducted a study-level meta-analysis of 3 trials in which inclusion of patients in spite of an early ischemic change of more than 1/3 of the middle cerebral artery territory was permitted (IST-3, NINDS and ECASS I).100,125,127 The unadjusted pooled ORs for ‘favourable’ outcome (mRS 0–1 at three months in NINDS and ECASS I, Oxford Handicap Score 0–2 at six months) were 1.65 (0.38–7.20) and 1.55 (1.05–2.28) in patients with and without early ischemic change of more than 1/3 of the middle cerebral artery territory (Figure 9). We found no evidence that the presence of an early ischemic change of more than 1/3 of middle cerebral artery territory significantly modifies the effect of IVT on favourable outcome (P for interaction = 0.67). However, we observed a significant interaction of the presence of early ischemic changes on baseline CT on the association of IVT with three-month mortality (P for interaction = 0.005). Patients treated with alteplase were at higher odds of three-month mortality compared with patients not treated with IVT (OR 3.90, 95% CI: 1.42–10.68; Figure 10).
Figure 9.
Pooled odds ratio for favourable outcome* in patients with ischaemic stroke of < 4.5 h duration randomised to with IVT vs. control, stratified by the extent of early ischaemic change on baseline CT (> 1/3 vs. < 1/3 of middle cerebral artery territory).
Random effects meta-analysis, based on data from von Kummer et al.,127 Patel et al.125 and IST-3 subgroup analyses.100
*Favourable outcome at 3–6 months refers here to Oxford Handicap Scale 0–2 at six months in IST-3 and mRS 0–1 at three months in NINDS and ECASS 1. EIC denotes early ischaemic changes on baseline CT scan. There was no significant interaction between the extent of early ischemic changes (> 1/3 vs. < 1/3 of the MCA territory) and the effect of IVT on favourable outcome (P for interaction = 0.67).
Figure 10.
Pooled odds ratio for death at three months in patients with ischaemic stroke of < 4.5 h duration randomised to IVT vs. control, stratified by the extent of early ischaemic change on baseline CT (> 1/3 vs. < 1/3 of middle cerebral artery territory).
Random effects meta-analysis, based on data from von Kummer et al.127 and Patel et al.125 EIC denotes early ischaemic changes on baseline CT scan. There was a significant interaction between the extent of early ischemic changes (> 1/3 vs. < 1/3 of the MCA territory) and the effect of IVT on death at three months (P for interaction = 0.005).
An ASPECTS of < 7 has also been used to define severe stroke.128
The recommendation for patients with clinically severe acute ischaemic stroke is based on meta-analyses of a number of RCTs. The quality of the evidence is moderate (Table 8). For severe stroke defined by the extent of ischaemic change on CT the recommendation is based on fewer data from fewer trials. The quality of the evidence is rated as very low (see Table 9 for details).
Recommendation
For patients with clinically severe acute ischaemic stroke of < 4.5 h duration, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
For patients with acute ischaemic stroke of < 4.5 h duration, and with severe stroke, defined by the extent of early ischaemic changes on CT, we suggest that intravenous thrombolysis with alteplase be considered in selected cases (see the Expert consensus statement below).
Quality of evidence: Very Low ⊕
Strength of recommendation: Weak ↑?
Table 9.
GRADE evidence profile for PICO 10.1 – Extensive ischaemic change on baseline imaging.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| Favourable outcome: mRS 0–1 at three months in ECASS-1 & NINDS; OHS 0–2 at six months in IST-3 | ||||||||||||
| 3 | randomised trials | seriousa | seriousb | seriousc | seriousd | none | 36/207(17.4%) | 27/179(15.1%) | OR 1.65(0.38–7.20) | 76 more per 1 000(from 88 fewer to 410 more) | ⨁◯◯◯VERY LOW | CRITICAL |
| sICH | ||||||||||||
| 1 | randomised trials | seriousa | not serious | seriousc | seriousd | none | 15/138(10.9%) | 4/112(3.6%) | OR 3.24(0.72–14.60) | 71 more per 1 000(from 10 fewer to 315 more) | ⨁◯◯◯VERY LOW | CRITICAL |
| Death at three months | ||||||||||||
| 2 | randomised trials | seriousa | not serious | seriousc | not seriousd | strong associationother consideratione | 49/69(71.0%) | 32/67(47.8%) | OR 3.90(1.42–10.68) | 303 more per 1 000(from 87 more to 429 more) | ⨁⨁◯◯LOW | CRITICAL |
Note: These results are based on the ECASS-1, NINDS and IST-3 studies.aSelection bias: it is plausible that all patients with very extensive signs of brain infarction on baseline imaging were not systematically randomized. Besides, because advanced imaging was not used, it is likely that the included population is heterogeneous, consisting of patients with and without residual salvageable (penumbral) tissue despite extensive infarction.bA strong benefit of IVT was observed in the NINDS trial (OR for favourable outcome 6.8; 95% CI: 1.30–36.2), whereas a trend towards deleterious effect was observed in ECASS-1 (OR for favourable outcome 0.4; 95% CI: 0.10–2.70).cIn IST-3 and ECASS-1, patients could be treated up to six hours after symptom onset. In IST-3, to our knowledge extent of early ischemic change was not specifically reported as less or more than 1/3 of the MCA territory but according to 4 categories, of which the authors considered ‘large or very large’ to correspond to more than 1/3 of the MCA territory.100 Conversely, in NINDS and ECASS-1, all baseline images were centrally reviewed and classified as less or more than 1/3 of the MCA territory.125dThe confidence interval is wide. However, in our meta-analysis we found evidence that presence of early ischaemic changes >1/3 of the middle cerebral artery territory modifies the effect of IVT on mortality at three months (P for interaction = 0.005).eRegarding IST-3, we could not find published data on the raw numbers or ORs for the association between IVT and death at six months, stratified by the extend of early ischaemic changes.
Additional information
The European Medicine Agency stipulates in the product insert for Actilyse that ‘Patients with severe stroke (as assessed clinically [NIHSS score >25] and/or by appropriate imaging techniques) … at baseline should not be treated with Actilyse’ because ‘patients with very severe stroke are at higher risk for intracerebral haemorrhage and death’.
Expert consensus statement
Seven of nine group members voted for intravenous thrombolysis with alteplase in selected patients with severe stroke associated with extended radiological signs of infarction (e.g., early ischemic change of more than 1/3 of the middle cerebral artery territory or ASPECTS < 7 on plain CT). Patient selection criteria might include eligibility for an alternative reperfusion strategy (mechanical thrombectomy), results of advanced imaging (notably core/perfusion mismatch), time since symptom onset, extent of white matter lesions, other contraindications for IVT, and pre-stroke disability.
11. High blood pressure and high blood glucose level
PICO 11.1 In patients with acute ischaemic stroke of < 4.5 h duration, and with persistently increased blood pressure above 185/110 mmHg, even after blood pressure lowering treatment, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Increased blood pressure is a common finding during the first hours of ischaemic stroke, and may be considered an adaptive physiological response aiming to improve cerebral perfusion. However, increased blood pressure may also increase the risk of sICH after IVT. The majority of the RCTs of IVT with alteplase therefore excluded patients with systolic blood pressure >185 mmHg or diastolic blood pressure >110 mmHg, and aimed to maintain blood pressure below these values during the first 24 h.
In IST-3, an analysis by subgroups of baseline systolic (< 143, 144–164, >164 mmHg) or diastolic blood pressure did not show a modification in the effect of alteplase on sICH, death at seven days, or functional outcome at six months.129 However, results for patients with systolic blood pressure >185 mmHg have not been published.
While analyses of RCTs have not shown an effect modification of IVT by high blood pressure, a number of analyses of observational data have shown that high blood pressure is associated with poorer prognosis. In patients treated with alteplase in the ECASS-2 trial, higher baseline, maximum, mean (per 10 mmHg increase), and variability of systolic blood pressure were all inversely associated with excellent outcome (mRS score 0–1) at three months (OR 0.84, 95% CI: 0.74–0.94; OR = 0.82, 95% CI: 0.73–0.91; OR = 0.81, 95% CI: 0.71–0.93; OR 0.57, 95% CI: 0.35–0.92, respectively) and associated with an increased risk of parenchymal haemorrhage within the first seven days (OR 1.27, 95% CI: 1.07–1.51; OR 1.49, 95% CI: 1.27–1.75; OR 1.52, 95% CI: 1.23–1.87; OR 2.62, 95% CI: 1.40–4.87, respectively) after adjusting for age, sex, time from stroke onset to treatment, stroke severity, history of hypertension, medication with aspirin and the extent of hypodensity on initial CT.130 Likewise, in an analysis of observational data from IST-3, the odds of sICH increased by 10% (95% CI: 2–19) for each 10 mmHg increase in baseline systolic blood pressure, after adjustment for baseline stroke severity.131 In addition, a single-centre observational study reported that pretreatment blood pressure limit violations (systolic blood pressure >185 mmHg and/or diastolic blood pressure >110 mmHg) occurred frequently (12%) in everyday clinical practice and were independently associated with higher likelihood of sICH (OR 2.59, 95% CI: 1.07–6.25).132 Also, in a recent retrospective analysis of the Safe Implementation of Treatments in Stroke (SITS) thrombolysis registry with regard to 11 off-label criteria according to the European licence for alteplase, elevated pretreatment blood pressure levels represented the only off-label criterion that was independently associated with a higher odds of sICH (OR 1.39; 95% CI: 1.08–1.80).133
A systematic review and meta-analysis of observational data from 56,513 patients found that higher pre-treatment systolic blood pressure (OR 1.08, 95% CI: 1.01–1.16 per 10 mm Hg increase, I2 = 82%) and higher post-treatment systolic blood pressure (OR 1.13 95% CI: 1.01–1.25 per 10 mm Hg increase, I2 = 63%) were associated with an increased risk of sICH.134 Higher systolic blood pressure was also associated with lower odds of good outcome (mRS 0–2) at three months: OR 0.91, 95% CI: 0.84–0.98 per 10 mmHg increase in pre-treatment pressure, I2 = 29%, and OR 0.70, 95% CI: 0.57–0.87 per 10 mm Hg increase in post-treatment pressure, I2 = 0%).
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with persistently increased systolic blood pressure >185 mmHg or diastolic blood pressure >110 mm Hg even after blood pressure lowering treatment, we suggest no intravenous thrombolysis.
Quality of evidence: Very low ⊕
Strength of recommendation: Strong ↓↓
Additional information
It should be noted that, based on current acute antihypertensive treatment options, persistent elevated blood pressure of >185/110 excluding patients from treatment is uncommon.
There is evidence suggesting that it is also important to monitor blood pressure after treatment with alteplase. In a cohort of 1868 patients treated with alteplase, patients with sICH had significantly higher systolic blood pressure at several time-points after IVT compared with those without sICH (P < 0.01 at 2 and 4 h; P < 0.05 at 12 and 48 h). The odds ratios for development of sICH per 10 mmHg increase in blood pressure at 2, 4, 12 and 48 h were 1.14 (95% CI: 1.03–1.25), 1.14 (95% CI: 1.03–1.25), 1.12 (95% CI: 1.01–1.23) and 1.12 (95% CI: 1.01–1.23), respectively.135
PICO 11.2 In patients with acute ischaemic stroke of < 4.5 h duration, and with increased blood pressure above 185/110 mm Hg, which has subsequently been lowered to below 185/110 mm Hg, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Blood pressure lowering treatment to values below 185/110 mmHg was allowed in all completed RCTs of IVT with alteplase versus control, and so the results of these trials apply to these patients.
In the ENCHANTED trial, 2196 patients with systolic blood pressure >150 mmHg and < 185/110 mmHg who were eligible for IVT with alteplase were randomised to intensive blood pressure lowering (target systolic blood pressure 130–140 mm Hg within 1 h) or to a target systolic blood pressure < 180 mm Hg, and to keep blood pressure in that range over 72 h.136 Mean systolic blood pressure over 24 h was 144 ± 10 mmHg in the intensive group and 150 ± 12 mmHg in the control group. Functional outcome at 90 days did not differ between groups (unadjusted cOR for better functional outcome 1.01, 95% CI: 0.87–1.17, P = 0.87). Fewer patients in the intensive group (14.8%) than in the control group (18.7%) had any ICH (OR 0.75, 0.60–0.94, P = 0.01). Blood pressure reduction was also related to a non-significant decrease in type 2 parenchymal haemorrhage (OR 0.71, 95% CI: 0.50–1.01).
An analysis of observational data from IST-3 indicated that the use of blood pressure lowering treatment during the first 24 h were associated with a reduced risk of poor outcome (Oxford handicap scale 3–6) at six months (OR 0.78, 95% CI: 0.65–0.93, P = 0.007), irrespective of whether the patient was given alteplase or not (p for interaction > 0.05).131 However, analyses of the effect of blood pressure lowering treatment using observational data from the NINDS trial did not provide conclusive results.137
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with systolic blood pressure >185 mm Hg or diastolic blood pressure >110 mm Hg, which has subsequently been lowered to < 185 and < 110 mm Hg, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↑↑
PICO 11.3 In patients with acute ischaemic stroke of < 4.5 h duration, and with known pre-stroke hypertension, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Only two of the RCTs (ECASS-3 and IST-3) that were included in the individual participant data meta-analysis8 presented the effect of IVT with alteplase for patients with or without known pre-stroke hypertension. There was no evidence that known hypertension modifies the effect of IVT with alteplase on excellent outcome in ECASS-3 (P for interaction = 0.19), or better functional outcome at six months in IST-3 (P for interaction = 0.79).129,138 There was also no evidence that known hypertension modifies the effect of IVT with alteplase on mortality or sICH in these two trials.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with known pre-stroke hypertension, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
PICO 11.4 In patients with acute ischaemic stroke of < 4.5 h duration, and with blood glucose level above >22.2 mmol/L (>400 mg/dL), does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Hyperglycaemia in the acute phase may represent stress, underlying impaired glucose tolerance or unrecognised diabetes mellitus. Higher blood glucose level at admission has been consistently associated with poorer functional outcome and sICH in acute ischemic stroke patients treated with or without IVT.139,140 However, blood glucose level was not a modifier of the effect of alteplase on functional outcome in RCTs.9,129 It is uncertain whether this also holds true for patients with very high blood glucose levels (>22.2 mmol/L, >400 mg/dL) because they were not included in RCTs, owing to concerns of an increased risk of sICH,122 but also because hyperglycaemia can present with focal neurological deficits that mimic acute stroke.141
We identified only one observational study allowing the comparison of IVT and no IVT in acute ischaemic stroke patients with blood glucose levels >22.2 mmol/L. In this analysis of 9613 patients from the Virtual International Stroke Trials Registry (VISTA), only 23 patients had blood glucose levels >22.2 mmol/L. Of these, 6 had been treated with alteplase, and in this very small group no cases of sICH were observed.142 Compared with patients not treated with IVT, those who received IVT had a cOR for better functional outcome of 1.06 (95% CI: 0.19–5.91) and an OR for excellent functional outcome of 1.31 (0.08–20.61).
Large observational registries of patients treated with IVT provide some insight on the risk of sICH in patients with very high blood glucose levels. Out of 56,258 patients treated with IVT in the SITS registry, baseline blood glucose levels >22.2 mmol/L were documented in 91 patients and independently associated with a higher risk of sICH according to ECASS-2 criteria (OR 1.99, 95% CI: 1.01–3.92).133 The incidence rate of sICH was 9.9% (95% CI: 5.3%–17.7%) and 3.3% (95% CI: 1.1–9.4%) according to the ECASS-2 and SITS definitions, respectively.
Of note, persistent hyperglycemia may be a more important predictor of poor functional outcome than baseline hyperglycemia in patients with acute ischaemic stroke.143
Given the lack of evidence of an heterogeneity in the effect of alteplase in patients with higher blood glucose levels, and the available data regarding the risk of sICH in patients with glucose level >22.2 mmol/L, we believe that alteplase should not be withheld in these patients, even though they have a substantial risk of poor functional outcome.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with blood glucose levels above 22.2 mmol/L (400 mg/dL), we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Very Low ⊕
Strength of recommendation: Weak ↑?
Intravenous thrombolysis should not prevent the administration of insulin therapy in acute ischaemic stroke patients with high blood glucose levels.144
Additional information
In an analysis of 16,049 patients treated with alteplase and included in the SITS registry,145 blood glucose as a continuous variable was independently associated with a higher case fatality (p < 0.001), poorer functional outcome (p < 0.001) and increased risk of sICH (P = 0.005). Compared to patients with blood glucose level 80–120 mg/dL, patients with blood glucose from 181 to 200 mg/dL had an increased risk of sICH (OR 2.86, 95% CI: 1.69–4.83, p < 0.001). The associations between blood glucose and outcomes were similar in patients with or without diabetes mellitus, except for case fatality (p for interaction < 0.001) and sICH (p for interaction = 0.02), for which the associations were not statistically significant in patients with diabetes mellitus.
In the SITS-EAST registry, 14 of 5461 patients (0.3%) had blood glucose levels >22.2 mmol/L, and these patients had an increased rate of sICH (unadjusted OR 5.91, 95% CI: 1.18–12.5, P = 0.03) and unfavourable functional outcome (adjusted OR 8.59, 95% CI: 0.88–83.9 P = 0.06).146
Intravenous thrombolysis should not prevent the administration of insulin therapy in acute ischaemic stroke patients with high blood glucose levels. More information about management of hyperglycaemia in patients with acute ischaemic stroke can be found in the ESO guideline on glycaemia management in acute stroke.144
The Stroke Hyperglycemia Insulin Network Effort (SHINE) randomized clinical trial included adult patients with hyperglycemia (glucose concentration of >110 mg/dL in case of diabetes or ≥150 mg/dL in patients without diabetes) and acute ischemic stroke who were enrolled within 12 h from stroke onset.147 Patients were randomized to receive continuous intravenous insulin (target blood glucose concentration of 80–130 mg/dL, intensive treatment group: n = 581) or subcutaneous insulin (target blood glucose concentration of 80–179 mg/d, standard treatment group: n = 570) for up to 72 h. A total of 725 enrolled patients (63%) received IVT. The proportion of patients with favourable outcome at 90 days did not differ in the two arms of the trial (20.5% vs. 21.6%) and in the subgroup of patients receiving IVT (23.0% vs. 24.9%). The number of patients who received blood glucose lowering therapy prior to alteplase bolus was not reported.
PICO 11.5 In patients with acute ischaemic stroke of < 4.5 h duration, and with known diabetes mellitus, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Only two of the RCTs (ECASS-3 and IST-3) that were included in the individual participant data meta-analysis8 presented the effect of IVT with alteplase for patients with or without known diabetes mellitus. There was no evidence that known diabetes mellitus modified the effect of IVT with alteplase on excellent outcome in ECASS-3 (P for interaction = 0.17), or better functional outcome at six months in IST-3 (P for interaction = 0.91).129,138 There was also no evidence that known diabetes mellitus modified the effect of IVT with alteplase on mortality or sICH in these two trials. Amongst 54,206 acute ischemic stroke patients included in the SITS registry and treated with IVT, there was no interaction of the history of diabetes mellitus on the association of admission hyperglycemia (≥144 mg/dL) with sICH according to the SITS definition (P for interaction = 0.27), three-month good functional outcome (P for interaction = 0.92) and three-month mortality (P for interaction = 0.63).148
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with known diabetes mellitus, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
12. Use of antithrombotic drugs before the stroke
PICO 12.1 In patients with acute ischaemic stroke of < 4.5 h duration, who use antiplatelet agents, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Treatment with antiplatelet agents before an ischaemic stroke may increase the risk of sICH in patients given alteplase,149 but antiplatelet treatment was not an exclusion criterion in the completed RCTs. Some of those trials have analysed separately patients who used an antiplatelet agent before stroke onset. A secondary analysis of IST-3 showed that the proportion of sICH in patients treated with antiplatelet therapy within the previous 48 h before stroke onset was 9% for those allocated alteplase versus 1% in control, compared with 5% for alteplase and 1% control for those with no recent antiplatelet therapy (P = 0.019 for interaction).129 A secondary analysis of the ENCHANTED trial indicated an association between standard-dose alteplase and risk of sICH in patients receiving antiplatelets before the stroke,62 but antiplatelet pre-treatment was not associated with worse functional outcome after adjustment for potential confounders.63
Meta-analyses of observational data from RCTs or from a combination of RCTs and observational studies indicated that antiplatelet agents increased the risk of sICH in unadjusted analyses (absolute increase 6.5%, 95% CI: 5.8–7.6%),63 but not after adjustment for confounders.150–152 Another analysis of observational data, from VISTA, indicated that alteplase compared to no alteplase improved functional outcome in patients who had received pre-treatment with a single antiplatelet agent (common OR 1.42, 95% CI: 1.19–1.70).142
The literature search identified no RCT of IVT in patients using dual antiplatelet therapy (DAPT) before the stroke. The VISTA analysis showed a relatively high risk of sICH in patients receiving DAPT (8.5%, 95% CI: 3.9–17.2%), but the analysis was unadjusted and the increase in sICH was statistically non-significant.142 Similarly, an analysis of patients given IVT within the Stroke–Acute Ischemic–NXY Treatment (SAINT) I and II trials indicated that DAPT was associated with a higher risk of sICH but not with a higher risk of poor functional outcome (mRS score 3–6) at three months.153 Other studies have used propensity score matching to attempt to account for imbalances between patients with and without DAPT. These studies indicate that patients who use DAPT before IVT with alteplase have comparable sICH rates and comparable functional outcome and survival at three months compared with patients who don’t use antiplatelet drugs.154,155
Finally, a recent meta-analysis of 9 observational studies comprising 66,675 acute ischaemic stroke patients treated with IVT failed to document any association between DAPT and the likelihood of sICH, three-month good functional outcome (mRS 0–2), three-month excellent functional outcome (mRS 0–1), and three-month mortality in adjusted analyses controlling for potential confounders.156
In summary, analyses of observational data indicate that single or dual antiplatelet pre-treatment is not independently associated with poorer functional outcome and higher risk of sICH. Use of antiplatelet agents should therefore not be used as a reason to withhold IVT with alteplase in patients with acute ischaemic stroke, although more research is needed.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, who used single or dual antiplatelet agents prior to the stroke, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↑↑
PICO 12.2 In patients with acute ischaemic stroke of < 4.5 h duration, who use vitamin K antagonists, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients given vitamin K antagonists (VKA) and with International Normalized Ratio (INR) >1.7 were excluded from the RCTs of IVT, and the European license for alteplase precludes treatment in all patients taking VKA. In a systematic review and meta-analysis of observational studies,157 25 of 240 patients (10.4%) who used VKA (median INR 1.14–1.5) experienced an sICH, compared with 184 of 3391 patients (5.4%) without VKA medication (OR 2.58, 95% CI: 1.13–5.89, P = 0.02; I2 = 56%). However, VKA use was not associated with poor functional outcome (mRS ≥3, OR 1.18, 95% CI: 0.85–1.61, P = 0.32; I2 = 15%) or death (OR 1.22, 95% CI: 0.85–1.75, P = 0.28; I2 = 0%).
Among 45,074 patients from the SITS registry treated with alteplase, 768 (1.7%) used warfarin and had INR ≤1.7.158 After adjustment for potential confounders, warfarin use was not significantly associated with sICH (adjusted OR 1.26, 95% CI: 0.82–1.70), and no increase in poor functional outcome or death at three months was observed. Among 23,437 patients treated with alteplase in the U.S. Get With The Guidelines Registry, 1802 (7.7%) were treated with warfarin with an INR ≤1.7 (median 1.20; IQR 1.07–1.40). After adjustment for potential confounders, warfarin use was not significantly associated with sICH (adjusted OR 1.01, 95% CI: 0.82–1.25), serious systemic haemorrhage, or in-hospital death.159
In patients with INR ≤1.7, other large registries159–161 have also indicated that IVT with alteplase is associated with a low risk of sICH and poor outcomes, both in the 0–3 and in the 3–4.5 h time windows, although this may have been due to confounding.160 Moreover, data from VISTA showed that alteplase was associated with improved functional outcome in patients given VKA and with INR ≤1.7 (cOR for better functional outcome 2.20, 95% CI: 1.12–4.32; Table 10).142
Table 10.
GRADE evidence profile for PICO 12.2.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative (95% CI) | Absolute(95% CI) | ||
| Better functional outcome (shift analysis of the mRS at three months) | ||||||||||||
| 1 | observational studies | not seriousa | not serious | not serious | not serious | none | –/38 | –/119 | cOR 2.20(1.12–4.32) | ⨁⨁◯◯LOW | CRITICAL | |
| sICH | ||||||||||||
| 1 | observational studies | not seriousa | not serious | not serious | seriousb | none | 2/38(5.3%) | 4/119(3.4%) | not estimable | ⨁◯◯◯VERY LOW | CRITICAL | |
| Death at three months | ||||||||||||
| 1 | observational studies | not seriousa | not serious | not serious | not serious | none | OR 0.68(0.25–1.86) | 1 fewer per 1 000(from 2 fewer to 0 fewer) | ⨁⨁◯◯LOW | CRITICAL | ||
Note: Results from VISTA.142aAn important risk of bias, notably of selection bias and confounding, exists in this pooled analysis based on RCTs of neuroprotectants. However, we consider that those limitations are already taken into account in mentioning in GRADEpro that this analysis corresponds to an observantional study and have therefore not further downgraded the quality of evidence.bVery few events.
There is little data on the rates of sICH in patients using VKA and INR >1.7, and the reported rates are highly variable (0% in 14 patients,142 3% in 33 patients159 and 30% in 10 patients162).
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, who use vitamin K antagonists and have INR ≤1.7 we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↑↑
For patients with acute ischaemic stroke of < 4.5 h duration, who use vitamin K antagonists and have INR >1.7 we recommend no intravenous thrombolysis.
Quality of evidence: Very Low ⊕
Strength of recommendation: Strong ↓↓
For patients with acute ischaemic stroke of < 4.5 h duration, who use vitamin K antagonists, and for whom the results of coagulation testing is unknown, we recommend no intravenous thrombolysis.
Quality of evidence: Very low ⊕
Strength of recommendation: Strong ↓↓
Additional information
Case series indicate that prothrombin complex concentrates can be used to reverse the effect of VKAs in patients who are eligible for thrombolytic treatment and have INR >1.7.163,164 However, prothrombin complex concentrates might enhance coagulation, which can lead to a worsening of patients’ neurological deficits.165 Mechanical thrombectomy appears to be safe in patients with large vessel occlusion who have been pre-treated with a VKA and with INR >1.7.166–168
PICO 12.3 In patients with acute ischaemic stroke of < 4.5 h duration, who use NOACs, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
The use of non-VKA oral anticoagulants (NOACs, i.e. direct thrombin inhibitors and factor Xa inhibitors) may increase the risk of sICH after IVT with alteplase, and alteplase is contraindicated if NOAC has been used during the last 48 h before stroke onset, according to the labels for these drugs.
In an observational study of 51 patients taking DOACs and 390 patients treated with VKA, sICH after intravenous alteplase occurred in 4.0% of patients taking NOACs and 3.6% of patients taking VKA (no significant difference).169 Out of 42,887 patients treated with alteplase in the Get With The Guidelines Registry, 251 (0.6%) were treated with NOACs and 1,500 (3.5%) with warfarin.170 Compared with patients without anticoagulants, the adjusted OR for sICH was 0.92 (95% CI: 0.51–1.65) for those on NOACs and 0.85 (95% CI: 0.66–1.10) for those on warfarin. There were also no significant differences across the three groups in the risk for serious systemic haemorrhage or in-hospital deaths.
A recent meta-analysis of cohort studies reported no additional risk of sICH following IVT among selected patients taking NOACs within 48 h compared to patients treated with warfarin (ECASS-2 criteria: OR 0.77, 95% CI: 0.28–2.16) and compared to patients without anticoagulation pretreatment (OR, 0.87, 95% CI: 0.32–2.41).171 Patient selection was based on various coagulation assays.
A number of decision algorithms have been proposed to identify patients treated with NOACs who can be given IVT.165,172–175 According to these algorithms, thrombolytic treatment can be given (i) in patients using dabigatran if thrombin time is normal172 or below 60 seconds,173 (ii) in patients using rivaroxaban if the drug plasma level is < 20 ng/ml174 or < 50 ng/ml,173 or if anti-Xa activity is < 0.5 U/ml,173 (iii) in patients using apixaban if anti-Xa activity is < 0.5 U/ml,173 (iv) in patients using edoxaban if anti-Xa activity < 0.5 U/ml.173 The safety of these treatment decision algorithms has not been tested in clinical practice, with the exception of the cut-off plasma level of rivaroxaban (<20ng/ml).174 The coagulation parameters used to select patients for IVT in these studies were different, and global coagulation tests, such as prothrombin time (PT), activated partial thromboplastin time (aPTT) and INR are not specific for NOACs. Further research is therefore needed to identify the optimal coagulation parameters (e.g. thrombin time for dabigatran, direct factor Xa activity for rivaroxaban, apixaban and edoxaban, or individual NOAC plasma levels). Until such data are available, we believe that IVT with alteplase should not be used indiscriminately in patients who have received a NOAC dose within the last 48 h in patients with normal renal function.
Others have proposed the use of agents to reverse the anticoagulant effects of NOACs.172–174 For example, idarucizumab has been used to reverse dabigatran activity before alteplase treatment, and this treatment algorithm has been tested in small studies in the prehospital and hospital settings.176–178 However, there are theoretical concerns that idarucizumab may potentiate the prothrombotic activity in the acute phase of ischaemic stroke, and increase the risk of ischaemic events.172 Nevertheless, such complications were not documented in two national cohorts from Germany and New Zealand reporting the experience of IVT for acute ischaemic stroke patients pretreated with idarucizumab for dabigatran reversal.177,179
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, who used a NOAC during the last 48 h before stroke onset, and for whom there is no specific coagulation tests available (i.e. calibrated anti-Xa-activity for factor Xa inhibitors, thrombin time for dabigatran, or the NOAC blood concentrations), we suggest no intravenous thrombolysis.
Quality of evidence: Very Low ⊕
Strength of recommendation: Strong ↓↓
For patients with acute ischaemic stroke of < 4.5 h duration, who used a NOAC during the last 48 h before stroke onset, and who have an anti-Xa activity < 0.5 U/ml (for factor Xa inhibitors) or thrombin time < 60 s (for direct thrombin inhibitors), there is insufficient evidence to make an evidence-based recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
For patients with acute ischaemic stroke of < 4.5 h duration, who used dabigatran during the last 48 h before stroke onset, there is insufficient evidence to make a recommendation for or against the use of the combination of idarucizumab and intravenous thrombolysis with alteplase over no intravenous thrombolysis. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Additional information
Measurement of anti-Xa activity has been proposed to select acute ischaemic stroke patients pretreated with factor Xa inhibitors for IVT, particularly where NOAC drug levels are not readily available.173 Of note, mechanical thrombectomy appears to be safe in patients with large vessel occlusion who have used a NOAC within last 48 h of symptom onset.168,172–174,180
Andexanet alfa is a modified recombinant factor Xa. It is catalytically inactive and cannot participate in coagulation, but it retains the ability to bind to and sequester factor Xa inhibitors. It has been conditionally approved by US FDA (Food and Drug Administration) in 2018 and European Medicines Agency in 2019 for the reversal of the anticoagulant effects of the Factor Xa inhibitors (apixaban or rivaroxaban) in patients experiencing uncontrolled or life-threatening bleeding based on the results of the ANNEXA-4 study.181 Andexanet alfa could reverse the anticoagulant effects of Factor Xa inhibitors in acute ischaemic stroke patients otherwise eligible for IVT who have been pretreated with apixaban or rivaroxaban. However, there is only anecdotal published evidence about acute ischaemic stroke patients treated with IVT following rivaroxaban or apixaban reversal with andexanet alfa. Importantly, the infusion of andexanet alfa requires two hours, which may have implications for the eligibility of patients to receive alteplase with regard to the approved time window of 4.5 h.182 Furthermore, a rebound effect of anti-Xa activity may occur. In contrast to idarucizumab in patients treated with dabigatran, andexanet alpha has not been approved for reversing Factor Xa inhibitor activity in patients who require emergency surgery/urgent procedures.183,184 Besides, the cost of andexanet alfa, which has not been approved for edoxaban reversal,184 is considerable.182 Finally, a safety analysis conducted in the overall ANNEXA-4 study population has documented 40 thrombotic events (7 myocardial infarctions, 15 transient ischemic attacks or ischaemic strokes, 18 venous thromboembolic events) occurring in 34 (10%) patients at 30 days.181 Eleven patients had a thromboembolic event within five days of receiving andexanet alfa and 8 patients had an event after restarting anticoagulation.181 Therefore, the U.S. FDA prescribing information for andexanet alfa includes a black box warning regarding the risk of venous and arterial thromboembolic events.185
In summary, we caution against the off-label use of andexanet alfa for reversal of anticoagulant activity of apixaban or rivaroxaban in acute ischaemic stroke patients who are otherwise eligible for IVT.
Expert consensus statement
For patients with acute ischaemic stroke of <4.5 h duration, who used a NOAC during the last 48 h before stroke onset, and who have an anti-Xa activity <0.5 U/ml (for factor Xa inhibitors) or thrombin time <60 s (for direct thrombin inhibitors) 7 of 9 group members suggest IVT with alteplase.
For patients with acute ischaemic stroke of < 4.5 h duration, who used dabigatran during the last 48 h before stroke onset, 8 of 9 group members suggest the combination of idarucizumab and intravenous thrombolysis with alteplase over no intravenous thrombolysis.
For patients with acute ischaemic stroke of < 4.5 h duration, who used factor Xa inhibitors during the last 48 h before stroke onset, 9 of 9 group members suggest against the combination of andexanet and intravenous thrombolysis with alteplase over no intravenous thrombolysis.
13. Potential risk factors for bleeding
An increased risk of bleeding after IVT can be suspected in many clinical situations, but the literature search identified no RCT to guide treatment in such situations. Many observational studies have focused on this topic, often comparing outcomes after IVT in patients with and without a bleeding-prone condition. Although this might identify risk factors for ICH, RCTs would be needed to formally demonstrate or discard a greater harm with IVT in patients with these factors.
PICO 13.1 In patients with acute ischaemic stroke of < 4.5 h duration, who have low platelet count, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients with a platelet count below 100,000/mm3
A platelet count below 100 × 109/L (100,000/mm3) was an exclusion criterion in all RCTs of IVT with alteplase except ECASS I and IST-3. We could not find a subgroup analysis of patients with a platelet count below 100 × 109/L in these two trials. In an observational study from ten European centres including 7,533 patients given alteplase, 595 (7.9%) had thrombocytopenia (<150 × 109/L) and 44 (0.6%) a platelet count below 100 × 109/L.157 Thrombocytopenia was not associated with poor functional outcome (mRS score 3–6) at three months (adjusted OR 0.92, 95% CI: 0.73–1.17, P = 0.50) or death, but was significantly associated with a higher risk of sICH (adjusted OR 1.68, 95% CI: 1.21–2.36, P = 0.002). Compared with other patients, those with a platelet count below 100 × 109/L more often had poor outcome (59.1% vs. 43.1%, P = 0.03), but this association did not reach significance in a multivariable analysis (adjusted OR 1.63, 95% CI: 0.82–3.24, P = 0.16). Similar point estimates were observed for death (adjusted OR 1.42, 95% CI: 0.66–3.07, P = 0.37) and sICH (adjusted OR 1.60, 95% CI: 0.49–5.21, P = 0.43).
Patients with unknown platelet count before initiation of IVT
In our review of the literature, excluding case series, we found that, among 12,701 patients treated with alteplase for acute ischaemic stroke, a total of 66 (0.5%) patients had a platelet count below 100 × 109/L, of which 4 had sICH (incidence rate 6.1%, 95% CI: 2.4–14.6).142,157,186–189 Amongst patients with < 100 × 109 platelets/L in the study by Gensicke et al., median platelet count was 90 × 109/L (IQR 71–96).157 Other observational studies have indicated that the proportion of stroke patients with a platelet count <100 × 109/L is below 0.5%.190,191 It is therefore likely that the benefit of earlier IVT would outweigh the harm of bleeding from inadvertently treating patients with a low platelet count.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with known platelet count < 100 × 109/L, we suggest no intravenous thrombolysis.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↓?
For patients with acute ischaemic stroke of < 4.5 h duration, and with unknown platelet count before initiation of intravenous thrombolysis and no reason to expect abnormal values, we recommend starting intravenous thrombolysis with alteplase while waiting for lab tests results.
Quality of evidence: Very low ⊕
Strength of recommendation: Strong ↑↑
PICO 13.2 In patients with acute ischaemic stroke of < 4.5 h duration, who have a history of recent trauma, surgery, or biopsy, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Significant trauma within the last three months is a contraindication for IVT with alteplase according to the European license.192 The outcome of IVT in patients with this contraindication has been reported in small case series.193,194 A relatively high number of patients had serious intracranial or systemic haemorrhage, although there is a possibility of publication bias.
Major surgery, which can be defined as surgery of the abdomen, chest, skull or well-vascularized tissues or of any large artery,195 has also been an exclusion criteria in all RCTs if performed within 14 days before stroke onset and is therefore also listed as a contraindication on the drug label. Among 4,848 patients treated with alteplase in the Telemedical Project for Integrative Stroke Care (TEMPiS) registry, 49 and 85 patients had undergone surgery within the 10 and 11–90 days preceding stroke onset, respectively.195 In 86 (64%) patients, surgery was classified as major and in 48 (36%) as minor. A total of 9 (7%) patients developed surgical site haemorrhage after IVT, more often after recent than after non-recent surgery. sICH occurred in 9.7% of patients. No information on three-month functional outcome was provided. Other small observational studies of patients treated with alteplase in spite of recent surgery also suggest that surgical site haemorrhage is the main hazard, without evidence of poor neurological outcome.194,196
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration and with major surgery on a non-compressible site where bleeding is likely to lead to significant haemorrhage (e.g., abdomen, chest, skull, well-vascularized tissues, or large artery) during the preceding 14 days, we recommend no intravenous thrombolysis.
Quality of evidence: Very low ⊕
Strength of recommendation: Strong ↓↓
PICO 13.3 In patients with acute ischaemic stroke of < 4.5 h duration, who have a history of intracranial haemorrhage, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients with history of ICH were excluded from RCTs of IVT with alteplase, and our literature search identified very few observational studies on this topic. In one observational study of 1,212 patients treated with alteplase, only 7 (0.6%) had a history of ICH (hematoma volume: 1–21 cm,3 elapsed time between previous ICH and ischemic stroke: 1.5–12 years), none of whom developed sICH or died after IVT.197 There are also case reports.189,196,198 A key question is the time elapsed since the intracranial haemorrhage, but unfortunately this information is not provided in most reports.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and a history of intracranial haemorrhage, there is insufficient evidence to make an evidence-based recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Expert consensus statement
For patients with acute ischaemic stroke of < 4.5 h duration and with a history of intracranial haemorrhage, 8 of 9 members suggest intravenous thrombolysis with alteplase in selected cases. For example, intravenous thrombolysis may be considered if a long time has elapsed since the haemorrhage, or if there was a non-recurrent or treated underlying cause for the haemorrhage (e.g. trauma, subarachnoid haemorrhage with subsequent endovascular or surgical aneurysm removal, or use of specific antithrombotic medication).
PICO 13.4 In patients with acute ischaemic stroke of < 4.5 h duration, who have cerebral microbleeds, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Most patients enrolled in the RCTs of IVT did not undergo MRI before randomisation and therefore their cerebral microbleed (CMB) burden is unknown. In a meta-analysis of 9 observational studies, CMB was observed on pre-treatment MRI in 581 (23.4%) patients, and was associated with an increased risk of sICH (RR 2.36, 95% CI: 1.21–4.61, P = 0.01; I2 = 46%), but the incidence rate of sICH remained relatively low (6.5%, 95% CI: 4.8–8.9 in patients with ≥1 CMB, and 4.4%, 95% CI: 3.5–5.4% in patients without CMB).199 However, in the very small subgroup of 15 patients (0.8%) with more than 10 CMBs, the incidence rate of sICH was 46.9% (95% CI: 22.8–72.5). In an individual participant data meta-analysis of 1973 patients, presence of ≥1 and >10 CMBs were observed in 526 (26.7%) and 35 (1.8%) patients, respectively.200 The association between CMB presence and sICH did not reach statistical significance (adjusted OR 1.42, 95% CI: 0.86–2.35, P = 0,17), but a count of more than 10 CMBs was associated with sICH (adjusted OR 3.65, 95% CI: 1.17–11.42), remote parenchymal haemorrhage (adjusted OR 9.09, 95% CI: 3.25–25.40) and poor functional outcome (adjusted OR 3.99, 95% CI: 1.55–10.22). Increasing CMB burden, defined as a continuous variable, was also independently associated with both sICH and poor functional outcome (mRS score >2) at three months.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, for whom cerebral microbleed burden is unknown or known to be low (e.g. < 10), we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↑?
For patients with acute ischaemic stroke of < 4.5 h duration, for whom cerebral microbleed burden has been previously reported to be high (e.g. >10), we suggest no intravenous thrombolysis.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↓?
Additional information
Susceptibility-weighted imaging (SWI) is more sensitive than T2* for detecting cerebral microbleeds.201 Therefore, it is not certain how generalisable recommendations based on T2* detected microbleeds are to SWI detected microbleeds, notably regarding the threshold that should be used to define high microbleed burden. However, a systematic review and individual participant data meta-analysis did not find that the type of MRI sequence (SWI vs. T2*) was associated with the risk of sICH following IVT (P = 0.74 for the whole sample; P = 0.34 in the subgroup of patients with at least one microbleed).199
A recent study devised a multistep algorithm to model three-month mRS scores in patients with ≤10 versus >10 CMBs who do or do not receive IVT.202 Parameters were extracted from recently published meta-analyses and included pairwise relationships between CMBs. IVT in patients with >10 CMBs significantly increased the odds of mortality, while the beneficial treatment effect of IVT on clinical outcome was attenuated in patients with >10 CMBs as compared with patients with ≤10 CMBs. However, because the general pretest probability of >10 CMBs is low (0.6%–2.7%), the authors hypothesized that pretreatment MRI to quantify CMB burden would be justified only if it delayed IVT by < 10 min.
Expert consensus statement
For patients with acute ischaemic stroke within 4.5 h of stroke onset, 9 of 9 members suggest against systematic screening with MRI to assess cerebral microbleed burden before making a treatment decision regarding intravenous thrombolysis.
PICO 13.5 In patients with acute ischaemic stroke of < 4.5 h duration, who have cerebral white matter lesions, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
In IST-3 there was no evidence for heterogeneity of treatment effect regarding good functional outcome between patients with and without white matter lesions (P for interaction = 0.24).100 However, in an analysis of patients enrolled in 4 RCTs (IST-3, NINDS, ECASS-1, ECASS-2; n = 2234), IVT with alteplase was associated with a higher incidence rate of sICH in patients with white matter lesions (7.9%, 95% CI: 6.4–9.6) than in patients without (1.3%, 95% CI: 0.8–2.2; Table 11). Still, IVT was associated with a lower risk of poor functional outcome in patients with white matter lesions, compared with no IVT (OR 0.75, 95% CI: 0.60–0.95, P = 0.015; I2 = 23%).203
Table 11.
GRADE evidence profile for PICO 13.5.
| Certainty assessment |
No of patients |
Effect |
Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No ofstudies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | IVT with alteplase | no IVT | Relative(95% CI) | Absolute(95% CI) | ||
| Favourable functional outcome at 3–6 months | ||||||||||||
| 4 | randomised trials | not serious | not serious | seriousa | not seriousb | none | 376/1105(34.0%) | 323/1129(28.6%) | OR 1.33(1.05–1.67) | 62 more per 1 000(from 10 more to 115 more) | ⨁⨁⨁◯MODERATE | CRITICAL |
| sICH | ||||||||||||
| 4 | randomised trials | not serious | not serious | seriousa | not seriousc | very strong association | 87/1105(7.9%) | 15/1129(1.3%) | OR 5.50(2.49–12.13) | 56 more per 1 000(from 19 more to 127 more) | ⨁⨁⨁⨁HIGH | CRITICAL |
Note: Results based on data from NINDS, ECASS 1 and 2 and IST-3.aThis result corresponds to presence or absence of leukoaraiosis. It therefore does not directly address the situation of patients with extensive leukoaraiosis.bOf note, there was no evidence that presence of leukoaraiosis modifies the effect of IVT on functional outcome in IST-3 (P for interaction = 0.24).cThere was no evidence in IST-3 that presence of leukoaraiosis significantly modifies the effect of IVT on siCH (P for interaction = 0.14)
In a study-level meta-analysis of observational data from 5910 patients treated with alteplase, presence of white matter lesions on CT was associated with sICH (OR 1.55, 95% CI: 1.17–2.06, P = 0.002; 7 studies; I2 = 21%).203 Severe white matter lesion burden, mostly defined as a score >2 on the Van Swieten scale, was strongly associated with sICH after treatment (OR 2.53, 95% CI: 1.92–3.34, p < 0.001; I2 = 0%). In the 818 patients with severe white matter lesions, the incidence rate of sICH was 9.9% (95% CI: 8.0–12.1). Presence of white matter lesions was associated with poor functional outcome after IVT (OR 2.02, 95% CI: 1.54–2.65, p < 0.001; I2 = 74%), but this association may have been caused by confounding, as larger white matter lesions volumes on MRI are independently associated with worse three-month functional outcome.204
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and small to moderate burden of white matter lesions, we recommend intravenous thrombolysis with alteplase.
Quality of evidence: Moderate ⊕⊕⊕
Strength of recommendation: Strong ↑↑
For patients with acute ischaemic stroke of < 4.5 h duration, and high burden of white matter lesions, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↑?
Additional information
In an observational study of 2,485 patients treated with alteplase, severe white matter lesions on CT, defined as a Blennow rating scale score of 5 or 6, was independently associated with remote parenchymal hemorrhage (adjusted OR 6.79, 95% CI: 2.57–17.94), but not with parenchymal hemorrhage strictly within the ischemic area (adjusted OR 1.45, 95% CI: 0.83–2.53).205 Another study, based on MRI volumetric evaluations of white matter lesions, confirmed that larger whole brain corrected white matter lesion volume was associated with remote ICH, irrespective of the deep or periventricular location of white matter lesions.206
PICO 13.6 In patients with acute ischaemic stroke of < 4.5 h duration, who have an unruptured cerebral aneurysm, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
The discovery of unruptured aneurysms in the acute phase of stroke is becoming more frequent with the increasing use of cerebral artery imaging. Data on IVT in patients with unruptured aneurysms is scarce. In a systematic review and meta-analysis of observational data, the incidence of sICH among 120 patients treated with alteplase for acute ischaemic stroke and having unruptured intracranial aneurysms was 6.7% (95% CI: 3.1–13.7%).207 The mean maximum diameter of the aneurysms was 4.3 ± 2.7 mm. The risk of sICH did not significantly differ between patients with and without unruptured aneurysms (RR 1.60; 95% CI: 0.54–4.77, P = 0.40; I2 = 22%). No case of cerebral artery aneurysm rupture was reported in this study.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, who have an unruptured cerebral artery aneurysm, we suggest IVT with alteplase.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↑?
14. Other co-existing conditions
PICO 14.1 In patients with acute ischaemic stroke of < 4.5 h duration, who have a history of ischaemic stroke during the last three months, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Patients with co-existing conditions thought to increase the risk of sICH or worse outcome were excluded from the RCTs of IVT with alteplase. One such example is ‘history of ischaemic stroke during the last three months’, which was also used as an exclusion criterion in trials of alteplase for acute myocardial infarction.122 In an observational study of alteplase for acute ischaemic stroke, 14(1.5%) of 946 patients had had a prior stroke within three months.146 The risk of poor outcome (mRS 3–6 at three months) was non-significantly increased in these patients (adjusted OR 4.07, 95% CI: 0.97–17.1). In an analysis of the SITS-EAST registry, 249(2%) of 13,007 patients had a stroke in the preceding three months, but it was not independently associated with poor functional outcome defined as an mRS score 3–6 at three months (adjusted OR 0.74, 95% CI: 0.35–1.56) or sICH (adjusted OR 0.74, 95% CI: 0.35–1.56).208 Other observational studies have shown similar results.196,209–211 In addition, a large study using administrative data from 36,599 patients treated with alteplase found that ischaemic stroke during the last three months was not associated with an increased risk of ICH (adjusted OR 0.9, 95% CI: 0.6–1.4, P = 0.62), but was related to an increased risk of death (OR 1.5, 95% CI: 1.2–1.9, P = 0.001) and unfavourable discharge disposition (OR 1.3, 95% CI: 1.0–1.7, P = 0.04).212 Finally, a meta-analysis of observational studies including 52,631 patients treated with alteplase found no evidence of increased risk of sICH, death or poor functional outcome or mortality in the 1.7% of patients who had a history of ischaemic stroke during the last three months.213
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration, and with a history of ischaemic stroke during the last three months, there is insufficient evidence to make an evidence-based recommendation recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Additional information
These observational studies have a number of limitations. Relatively few patients had had an ischaemic stroke within the previous three months, and many studies did not provide data on the baseline characteristics of these patients. Importantly, most studies did not report the time since the previous ischaemic stroke, precluding definitive conclusions about the minimal time interval that should be respected before using IVT in such patients.
Expert consensus statement
For patients with acute ischaemic stroke of < 4.5 h duration, and a history of ischemic stroke within the last three months, nine of nine members voted for intravenous thrombolysis with alteplase in selected cases, for example in case of a small infarct, stroke occurring more than one month earlier, or good clinical recovery.
PICO 14.2 In patients with acute ischaemic stroke of < 4.5 h duration, who had a seizure at time of stroke onset, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
A seizure can be the initial manifestation of a stroke, but patients with seizures at the time of stroke have been excluded from the RCTs of IVT, for several reasons. First, post-ictal state can mimic a stroke. Second, seizures can also be caused by conditions other than stroke, like structural brain lesions or metabolic/infectious states. Third, a seizure can lead to – sometimes unobserved – head trauma that may increase the risk of secondary ICH.
Data from several observational studies suggests that the risk of sICH is low in patients with stroke mimics214,215 and also in patients with suspected acute ischaemic stroke with seizure at stroke onset.216 In an observational study of 5,581 patients treated with alteplase, 100 patients had stroke mimics (1.8%). The rate of sICH in patients with stroke mimics was 1.0% (95% CI: 0.0–5.0) compared with 7.9% (95% CI: 7.2–8.7) in patients with ischaemic strokes.214 Analysis of data from stroke registries have also provided reassurance that inadvertent administration of alteplase to patients with seizures at onset of stroke-like symptoms does not increase the risk of sICH.214 However, the possibility of a head trauma as a consequence of the seizure must always be considered.
Recommendation
For patients with acute ischaemic stroke of <4.5 h duration who have seizures at time of stroke onset, and for whom there is no suspicion of a stroke mimic or significant head trauma, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↑?
Additional information
Advanced imaging methods like MRI with DWI and apparent diffusion coefficient (ADC) sequences and perfusion CT although not used in RCTs may be useful to distinguish between post-ictal deficits and stroke.217,218 Seizures may be associated with transient peri-ictal MRI abnormalities: a) diffusion abnormalities with mixed appearance with simultaneous acute cytotoxic cortical oedema and vasogenic subcortical oedema without a vascular territory lesion distribution; b) gyral enhancement occurring earlier than expected for acute ischemic stroke, c) perfusion studies with normal or increased cerebral blood volume (hyperperfusion) at the epileptogenic area during the ictal phase and hypoperfusion in the postictal phase.
PICO 14.3 In patients with acute ischaemic stroke of <4.5 h duration, who have dissection in the aortic arch, in a carotid artery or in an intracerebral artery, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Most cases of aortic arch dissection receiving IVT with alteplase are patients with acute myocardial infarction. Some of these patients have suffered extension of dissection into the pericardium, leading to cardiac tamponade and death.219 There are only anecdotal case reports in the literature of patients with acute ischaemic stroke who had an aortic arch dissection and were treated with alteplase. Reported complications include cardiac tamponade and intrapleural haemorrhage.220,221 IVT in these patients could also reduce the possibility of survival by leading to the postponement of an emergency operation to treat thoracic aortic dissection.222
Extracranial artery dissection was a not specific exclusion criterion in RCTs of IVT versus placebo, but because dissection is a rare event the number of randomised patients is likely to be very low and no specific subgroup analysis has been published. Few observational studies provide a direct comparison of IVT versus no IVT in patients with artery dissection. The Cervical Artery Dissection and Ischemic Stroke Patients (CADISP) group published an observational study of 616 patients with extracranial artery dissection, of which 68 (11.0%) received alteplase (81% treated with IVT and 19% with intra-arterial alteplase).223 After adjustment for stroke severity and large vessel occlusion status, the likelihood of good outcome (mRS 0–2) did not differ between patients treated with alteplase and controls (adjusted OR 0.95, 95% CI: 0.45–2.00). ICH occurred in 4 (5.9%) of the patients who received alteplase (all of which were asymptomatic) and 3 (0.6%) of patients who did not receive alteplase (two of which were asymptomatic). In a small single-centre study of 46 patients with ischaemic stroke due to artery dissection, of which 19 (41%) were treated with IVT, the proportion of good outcome (mRS 0–2) did not significantly differ between patients treated with or without IVT (95% vs. 82%; adjusted OR 5.49; 95% CI: 0.77–39.11).224 In an unpublished subgroup analysis (n = 49) of patients with dissection and internal carotid occlusion from the Systemic thrombolysis in patients with acute ischemic stroke and Internal Carotid ARtery Occlusion (ICARO) observational study,225 IVT (n = 26) was not significantly associated with excellent (mRS score 0–1) or good (mRS score 0–2) outcome compared with no IVT (unadjusted ORs 2.11, 95% CI: 0.54–8.25 and 1.96, 95% CI: 0.60–6.35, respectively).
Other observational studies provide a comparison of IVT-treated patients with and without dissection. An individual participant data meta-analysis of observational studies including 180 patients with cervical carotid artery dissection indicated that case fatality at three months and risk of sICH was similar in patients with dissection and matched controls (fatality rate 7.3%, 95% CI: 3.7–13.9% vs. 8.8%, 95% CI: 5.1–14.5%, and sICH rate 3.3% 95% CI: 1.2–8.5% vs. rate 5.9% 95% CI: 3.0–10.9%).226 Similar findings were reported in a meta-analysis of 234 patients with co-existent extra- or intracranial dissections who received alteplase.227 The respective rates of sICH and death were 2% (0–5%) and 4% (0–8%), underscoring the safety of alteplase in dissection-related acute ischaemic stroke.
The quality of evidence for IVT in patients with isolated cervical artery dissection was rated as low because although extracranial dissection was not a formal exclusion criterion in pivotal RCTs, direct comparison of IVT vs. no IVT in this population relies only on observational studies with important risk of selection bias and confounding by indication. We decided not to perform a meta-analysis of these studies due to notable differences in study design.
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration and with aortic arch dissection we recommend no intravenous thrombolysis.
Quality of evidence: Very low ⊕
Strength of recommendation: Strong ↓↓
For patients with acute ischaemic stroke of < 4.5 h duration and with isolated cervical artery dissections, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Weak ↑?
For patients with acute ischaemic stroke of < 4.5 h duration and with intracerebral artery dissections, there is insufficient evidence to make a recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
Additional information
The presence of intracranial arterial dissection may result in subadventitial extension of the hematoma and increase the risk of subarachnoid haemorrhage (especially when located in the posterior circulation) or intracranial bleeding in acute ischaemic stroke patients receiving antithrombotic and thrombolytic treatments.228
Expert consensus statement
For patients with acute ischaemic stroke of < 4.5 h duration and with an intracerebral artery dissection, 6 of 9 group members suggest against intravenous thrombolysis with alteplase.
PICO 14.4 In patients with acute ischaemic stroke of < 4.5 h duration, who have had myocardial infarction during the last three months, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Myocardial infarction during the last three months was not an exclusion criterion in the completed RCTs, so the results from these trials apply to these patients.
However, there are case reports describing myocardial rupture, cardiac tamponade or embolisation of ventricular thrombus after IVT for acute ischaemic stroke in patients who have had a recent acute myocardial infarction.229–231 Conversely, other case reports describe successful administration of IVT with alteplase in patients with acute ischaemic stroke and recent myocardial infarction. In a systematic review of case series that included 102 patients, four (8.5%) of the 47 IVT-treated patients died from confirmed or presumed cardiac rupture/tamponade, all with subacute (>6 h) ST-elevation Myocardial Infarction (STEMI) in the week preceding stroke.232 This complication occurred in 1 (1.8%) patients in the non-treated group (P = 0.18). No non-STEMI patients receiving IVT with alteplase had cardiac complications.
Non-STEMI patients have a lower risk of complications than transmural STEMI patients, and among ST-elevation infarctions, infarctions in the anterior wall have the highest cardiac complication rates.233 Cardiac complications tend to peak 2–14 days after myocardial infarction.234
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration and with history of subacute (>6 h) ST-elevation myocardial infarction during the last seven days, we suggest no IVT.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↓?
For patients with acute ischaemic stroke of < 4.5 h duration and with history of ST-elevation myocardial infarction of more than a week to three months, there is insufficient evidence to make a recommendation. Please see the Expert consensus statement below.
Quality of evidence: Very low ⊕
Strength of recommendation: -
For patients with acute ischaemic stroke of < 4.5 h duration and with a history of non-ST-elevation myocardial infarction during the last three months, we suggest intravenous thrombolysis with alteplase.
Quality of evidence: Very low ⊕
Strength of recommendation: Weak ↑?
Additional information
IVT with alteplase at a dose of 1.1 mg/kg is indicated in patients with acute (< 6 h) myocardial infarction. Consequently, in the uncommon case scenario of an acute ischaemic stroke complicating an acute myocardial infarction alteplase may be administered if there are no other contraindications to IVT. The dose and the time window should conform to the recommendations of IVT for acute ischaemic stroke to minimize the risk of sICH.
Mechanical thrombectomy may be a therapeutic alternative to bridging therapy in patients with large-vessel occlusion and recent myocardial infarction.
Expert consensus statement
For patients with acute ischaemic stroke of < 4.5 h duration and with history of ST-elevation myocardial infarction of more than a week to three months, nine of nine group members suggest IVT with alteplase in specific situations. Variables to take into account are the size of the myocardial infarction, whether recanalisation therapy was given for the myocardial infarction, and echocardiographic findings.
PICO 14.5 In patients with acute ischaemic stroke of < 4.5 h duration, who have infective endocarditis, does IVT with alteplase lead to better functional outcome than no IVT?
Analysis of current evidence
Stroke is the most common neurological complication of infective endocarditis, affecting up to 35% of all patients.235 Histopathological studies also suggest that cerebral infarcts caused by septic emboli are particularly prone to haemorrhagic transformation as a result of septic arteritis with erosion of the arterial wall in the recipient vessel, with or without the formation of mycotic aneurysms.236 Consequently, there are theoretical reasons to expect that IVT for acute ischaemic stroke due to infective endocarditis will be associated with a higher risk of sICH.222 In a large study based on administrative data, the outcome of patients treated with IVT for acute ischaemic stroke with (n = 222) and without (n = 134,048) infective endocarditis was compared. The rate of post-thrombolytic ICH was significantly higher in patients with infective endocarditis than in those without (20% versus 6.5%, P = 0.006), and the proportion of patients with discharge disposition of home/self-care was significantly lower in the infective endocarditis group (10% versus 37%, P = 0.01).237 Some studies have also shown that alteplase in patients with co-existing infective endocarditis may be complicated with multifocal ICH.238,239
Recommendation
For patients with acute ischaemic stroke of < 4.5 h duration and with a clear or suspected diagnosis of infective endocarditis, we suggest no intravenous thrombolysis.
Quality of evidence: Low ⊕⊕
Strength of recommendation: Strong ↓↓
Discussion
This guideline document was developed following the GRADE methodology and aims to assist physicians in decision-making regarding IVT for acute ischaemic stroke. It includes up-to-date scientific evidence that supersedes the previously published ESO guidelines and Karolinska Stroke Update recommendations.1,240 All recommendations and Expert consensus statements are summarized in Table 12.
Table 12.
Summary of PICO questions, evidence based recommendations, and expert consensus statements.
| Topic/PICO Question | Recommendations | Expert consensus statement |
|---|---|---|
| 0–4.5 h time window1.1: In patients with acute ischaemic stroke of <4.5 h duration, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis? | For patients with acute ischaemic stroke of <4.5 h duration, we recommend intravenous thrombolysis with alteplase.Quality of evidence: High ⊕⊕⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| 4.5–9 h time window (known onset), plain CT | ||
| 2.1: In patients with acute ischaemic stroke of 4.5–9 h duration (known onset time) selected with plain CT, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis? | For patients with acute ischaemic stroke of 4.5–9 h duration (known onset time), and with no brain imaging other than plain CT, we recommend no intravenous thrombolysis.Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↓↓ | |
|
| ||
| 4.5–9 h time window (known onset), perfusion mismatch | ||
| 3.1: In patients with ischaemic stroke of 4.5–9 h duration (known onset time), and with CT or MRI core/perfusion mismatch, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis? | For patients with ischaemic stroke of 4.5–9 h duration (known onset time) and with CT or MRI core/perfusion mismatch*, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↑↑*In the individual participant data meta-analysis by Campbell et al.,34 core/perfusion mismatch was assessed with an automated processing software and defined as follows:- Infarct core** volume < 70 ml- and Critically hypoperfused† volume/ Infarct core** volume > 1.2- and Mismatch volume > 10 ml** rCBF <30% (CT perfusion) or ADC < 620 µm2/s (Diffusion MRI)† Tmax >6 s (perfusion CT or perfusion MRI) | For patients with ischaemic stroke of 4.5–9 h duration (known onset), and with no CT or MRI core/perfusion mismatch, 9 of 9 group members suggest against IVT with alteplase.For patients presenting directly to a thrombectomy centre with ischaemic stroke of 4.5–9 h duration (known onset) with CT or MRI core/ perfusion mismatch and who are eligible for mechanical thrombectomy, the group members could not reach a consensus regarding whether intravenous thrombolysis should be used before mechanical thrombectomy.For patients presenting to a non-thrombectomy centre with ischaemic stroke of 4.5–9 h duration (known onset) with CT or MRI core/perfusion mismatch and who are eligible for mechanical thrombectomy, 6/9 group members suggest intravenous thrombolysis before mechanical thrombectomy. |
|
| ||
| Wake-up stroke/Unknown onset | ||
| 4.1: In patients with acute ischaemic stroke on awakening from sleep / unknown onset, does intravenous thrombolysis with alteplase lead to better functional outcome than no intravenous thrombolysis? | For patients with acute ischaemic stroke on awakening from sleep, who were last seen well more than 4.5 h earlier, who have MRI DWI-FLAIR mismatch, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase. Quality of evidence: High ⊕⊕⊕⊕Strength of recommendation: Strong ↑↑For patients with acute ischaemic stroke on awakening from sleep, who have CT or MRI core/perfusion mismatch* within nine hours from the midpoint of sleep, and for whom mechanical thrombectomy is either not indicated or not planned, we recommend intravenous thrombolysis with alteplase. Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑*In the EOS individual participant data meta-analysis,46 core/perfusion mismatch was assessed with an automated processing software and defined as follows:- Infarct core** volume < 70 ml- and Critically hypoperfused† volume / Infarct core** volume > 1.2- and Mismatch volume > 10 ml** rCBF <30% (CT perfusion) or ADC < 620 µm2/s (Diffusion MRI)† Tmax >6 s (perfusion CT or perfusion MRI) | For patients presenting directly to a thrombectomy centre with acute ischaemic stroke on awakening from sleep, who would be eligible for both IVT and mechanical thrombectomy, 6/9 group members suggest IVT before MT.For patients presenting to a non-thrombectomy centre with acute ischaemic stroke on awakening from sleep, who would be eligible for both IVT and mechanical thrombectomy, 7/9 group members suggest IVT before MT. |
|
| ||
| Tenecteplase – no large vessel occlusion | ||
| 5.1: In patients with acute ischaemic stroke of <4.5 h duration, does IVT with tenecteplase lead to better functional outcome than IVT with alteplase? | For patients with acute ischaemic stroke of <4.5 h duration and not eligible for thrombectomy, we suggest intravenous thrombolysis with alteplase over intravenous thrombolysis with tenecteplase. Please see paragraph 5.2 for patients eligible for mechanical thrombectomy.Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↑? | |
|
| ||
| Tenecteplase – large vessel occlusion | ||
| 5.2: In patients with acute ischaemic stroke of <4.5 h duration and with large vessel occlusion, who are candidates for mechanical thrombectomy, and for whom intravenous thrombolysis is considered before thrombectomy, does IVT with tenecteplase lead to better functional outcome than IVT with alteplase? | For patients with acute ischaemic stroke of < 4.5 h duration and with large vessel occlusion who are candidates for mechanical thrombectomy and for whom intravenous thrombolysis is considered before thrombectomy, we suggest intravenous thrombolysis with tenecteplase 0.25 mg/kg over intravenous thrombolysis with alteplase 0.9 mg/kg. Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↑? | |
|
| ||
| Low-dose alteplase | ||
| 6.1: In patients with acute ischaemic stroke of <4.5 h duration, does intravenous thrombolysis with low-dose alteplase lead to non-inferior (not worse) functional outcome compared to standard-dose alteplase? | For patients with acute ischaemic stroke of <4.5 h duration who are eligible for intravenous thrombolysis, we recommend standard-dose alteplase (0.9 mg/kg) over low-dose alteplase.Quality of evidence: High ⊕⊕⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Adjunct antithrombotic therapy | ||
| 7.1: In patients with acute ischaemic stroke of <4.5 h duration, does antithrombotic agents in addition to IVT lead to better functional outcome than IVT alone? | For patients with acute ischaemic stroke of <4.5 h duration, we recommend no antithrombotic drugs within 24 h of intravenous thrombolysis over antithrombotic drugs as an adjunct therapy to intravenous thrombolysis with alteplase.Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↓↓ | |
|
| ||
| Sonothrombolysis | ||
| 7.2: In patients with acute ischaemic stroke of <4.5 h duration, does ultrasound augmentation of IVT lead to better functional outcome than IVT alone? | For patients with acute ischaemic stroke of <4.5 h duration, we recommend against ultrasound augmentation in patients receiving intravenous thrombolysis.Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↓↓ | |
|
| ||
| Higher age, multimorbidity, prior disability | ||
| 8.1: In patients with acute ischaemic stroke of <4.5 h duration, who are over 80 years of age, does intravenous thrombolysis with alteplase lead to better functional outcome than no IVT?8.2: In patients with acute ischaemic stroke of <4.5 h duration, who have multimorbidity, frailty, or prior disability, does intravenous thrombolysis with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, who are over 80 years of age, we recommend intravenous thrombolysis with alteplase.Quality of evidence: High ⊕⊕⊕⊕Strength of recommendation: Strong ↑↑For patients with acute ischaemic stroke of <4.5 h duration, and with multimorbidity, frailty or pre-stroke disability, we suggest intravenous thrombolysis with alteplase.Quality of evidence: Very low ⊕Strength of recommendation: Weak ↑? | 9/9 group members believe that age alone should not be a limiting factor for IVT, even in other situations covered in the present guidelines (e.g. wake-up stroke; ischaemic stroke of 4.5–9 h duration (known onset time) with CT or MRI core/perfusion mismatch; minor stroke with disabling symptoms). |
|
| ||
| Minor stroke (disabling) | ||
| 9.1: In patients with acute minor, disabling ischaemic stroke of <4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute minor, disabling ischaemic stroke of <4.5 h duration, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Minor stroke (non-disabling) | ||
| 9.2: In patients with acute minor, non-disabling ischaemic stroke of <4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute minor non-disabling ischaemic stroke of <4.5 h duration, we suggest no intravenous thrombolysis. For patients with minor stroke and large-vessel occlusion, please refer to the section below (PICO 9.3).Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Weak ↓? | |
| 9.3: In patients with acute minor, non-disabling ischaemic stroke of <4.5 h duration, and with proven large vessel occlusion, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute minor, non-disabling ischaemic stroke of <4.5 h duration, and with large-vessel occlusion, 6 of 8 group members suggest intravenous thrombolysis with alteplase. | |
|
| ||
| Rapidly improving symptoms | ||
| 9.4: In patients with acute ischaemic stroke of <4.5 h duration, and with rapidly improving neurological signs, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke with < 4.5 h duration, and rapidly improving neurological signs, which are still disabling, 8 of 9 group members suggest intravenous thrombolysis with alteplase. The group agreed that the treatment decision should be based on the clinical status at presentation, and that it is not justifiable to wait for resolution of symptoms. | |
|
| ||
| Severe stroke | ||
| 10.1: In patients with severe acute ischaemic stroke of <4.5 h duration, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with clinically severe acute ischaemic stroke of <4.5 h duration, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑For patients with acute ischaemic stroke of <4.5 h duration, and with severe stroke, defined by the extent of early ischaemic changes on CT, we suggest that intravenous thrombolysis with alteplase be considered in selected cases (see the Expert consensus statement).Quality of evidence: Very Low ⊕Strength of recommendation: Weak ↑? | 7 of 9 group members voted for intravenous thrombolysis with alteplase in selected patients with severe stroke associated with extended radiological signs of infarction (e.g., early ischemic change of more than 1/3 of the middle cerebral artery territory or ASPECTS <7 on plain CT). Patient selection criteria might include eligibility for an alternative reperfusion strategy (mechanical thrombectomy), results of advanced imaging (notably perfusion/core mismatch), time since symptom onset, and pre-stroke disability. |
|
| ||
| High Blood pressure on admission | ||
| 11.1: In patients with acute ischaemic stroke of <4.5 h duration, and with persistently increased blood pressure above 185/110 mmHg, even after blood pressure lowering treatment, does IVT with alteplase lead to better functional outcome than no IVT?11.2: In patients with acute ischaemic stroke of <4.5 h duration, and with increased blood pressure above 185/110 mm Hg, which has subsequently been lowered to below 185/110 mm Hg, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and with persistently increased systolic blood pressure >185 mmHg or diastolic blood pressure >110 mm Hg even after blood pressure lowering treatment, we suggest no intravenous thrombolysis.Quality of evidence: Very low ⊕Strength of recommendation: Strong ↓↓For patients with acute ischaemic stroke of <4.5 h duration, and with systolic blood pressure >185 mm Hg or diastolic blood pressure >110 mm Hg, which has subsequently been lowered to <185 and <110 mm Hg, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Pre-stroke hypertension | ||
| 11.3: In patients with acute ischaemic stroke of <4.5 h duration, and with known pre-stroke hypertension, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and with known pre-stroke hypertension, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| High glucose level on admission | ||
| 11.4: In patients with acute ischaemic stroke of <4.5 h duration, and with blood glucose level above 22.2 mmol/L (>400 mg/dL), does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and with blood glucose levels above >22.2 mmol/L (400 mg/dL), we suggest intravenous thrombolysis with alteplase.Quality of evidence: Very Low ⊕Strength of recommendation: Weak ↑?Intravenous thrombolysis should not prevent the administration of insulin therapy in acute ischaemic stroke patients with high blood glucose levels.144 | |
|
| ||
| Diabetes mellitus | ||
| 11.5: In patients with acute ischaemic stroke of <4.5 h duration, and with known diabetes mellitus, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and with known diabetes mellitus, we recommend intravenous thrombolysis with alteplase.Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Antiplatelet agents prior to stroke | ||
| 12.1: In patients with acute ischaemic stroke of <4.5 h duration, who use antiplatelet agents, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, who used single or dual antiplatelet agents prior to the stroke, we suggest intravenous thrombolysis with alteplase. Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Anticoagulants before stroke (VKA) | ||
| 12.2: In patients with acute ischaemic stroke of <4.5 h duration, who use vitamin K antagonists, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, who use vitamin K antagonists and have INR ≤1.7 we recommend intravenous thrombolysis with alteplase.Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↑↑For patients with acute ischaemic stroke of <4.5 h duration, who use vitamin K antagonists and have INR >1.7 we recommend no intravenous thrombolysis.Quality of evidence: Very Low ⊕Strength of recommendation: Strong ↓↓For patients with acute ischaemic stroke of <4.5 h duration, who use vitamin K antagonists, and for whom the results of coagulation testing is unknown, we recommend no intravenous thrombolysis.Quality of evidence: Very low ⊕Strength of recommendation: Strong ↓↓ | |
|
| ||
| Anticoagulants before stroke (NOACs) | ||
| 12.3: In patients with acute ischaemic stroke of <4.5 h duration, who use NOACs, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, who used a NOAC during the last 48 h before stroke onset, and for whom there is no specific coagulation tests available (i.e. calibrated anti-Xa-activity for factor Xa inhibitors, thrombin time for dabigatran, or the NOAC blood concentrations), we suggest no intravenous thrombolysis. Quality of evidence: Very Low ⊕Strength of recommendation: Strong ↓↓ | For patients with acute ischaemic stroke of <4.5 h duration, who used a NOAC during the last 48 h before stroke onset, and who have an anti-Xa activity <0.5 U/ml (for factor Xa inhibitors) or thrombin time <60 s (for direct thrombin inhibitors) 7 of 9 group members suggest IVT with alteplase.For patients with acute ischaemic stroke of <4.5 h duration, who used dabigatran during the last 48 h before stroke onset, 8/9 group members suggest the combination of idarucizumab and intravenous thrombolysis with alteplase over no intravenous thrombolysis.For patients with acute ischaemic stroke of <4.5 h duration, who used factor Xa inhibitors during the last 48 h before stroke onset, 9/9 group members suggest against the combination of andexanet and intravenous thrombolysis with alteplase over no intravenous thrombolysis. |
|
| ||
| Low platelet count | ||
| 13.1: In patients with acute ischaemic stroke of <4.5 h duration, who have low platelet count, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and with known platelet count <100 × 109/L, we suggest no intravenous thrombolysis.Quality of evidence: Very low ⊕Strength of recommendation: Weak ↓?For patients with acute ischaemic stroke of <4.5 h duration, and with unknown platelet count before initiation of intravenous thrombolysis and no reason to expect abnormal values, we recommend starting intravenous thrombolysis with alteplase while waiting for lab tests results.Quality of evidence: Very low ⊕Strength of recommendation: Strong ↑↑ | |
|
| ||
| Recent trauma or surgery | ||
| 13.2: In patients with acute ischaemic stroke of <4.5 h duration, who have a history of recent trauma, surgery or biopsy, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration and with major surgery on a non-compressible site where bleeding is likely to lead to significant haemorrhage (e.g., abdomen, chest, skull, well-vascularized tissues, or large artery) during the preceding 14 days, we recommend no intravenous thrombolysis. Quality of evidence: Very low ⊕Strength of recommendation: Strong ↓↓ | |
|
| ||
| History of intracranial hemorrhage | ||
| 13.3: In patients with acute ischaemic stroke of < 4.5 h duration, who have a history of intracranial haemorrhage, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration and with a history of intracranial haemorrhage, 8/9 members suggest intravenous thrombolysis with alteplase in selected cases. For example, intravenous thrombolysis may be considered if a long time has elapsed since the haemorrhage, if there was a specific underlying cause for the haemorrhage (e.g. trauma, subarachnoid haemorrhage with subsequent endovascular or surgical aneurysm removal, or use of specific antithrombotic medication). | |
|
| ||
| Microbleeds | ||
| 13.4: In patients with acute ischaemic stroke of <4.5 h duration, who have cerebral microbleeds, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, for whom cerebral microbleed burden is unknown or known to be low (e.g. <10), we suggest intravenous thrombolysis with alteplase. Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↑?For patients with acute ischaemic stroke of <4.5 h duration, for whom cerebral microbleed burden has been previously reported to be high (e.g. >10), we suggest no intravenous thrombolysis.Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↓? | For patients with acute ischaemic stroke within 4.5 h of stroke onset, 9 of 9 members suggest against screening with MRI to assess cerebral microbleed burden before making a treatment decision regarding intravenous thrombolysis. |
|
| ||
| White matter lesions | ||
| 13.5: In patients with acute ischaemic stroke of <4.5 h duration, who have cerebral white matter lesions, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and small to moderate burden of white matter lesions, we recommend intravenous thrombolysis with alteplase. Quality of evidence: Moderate ⊕⊕⊕Strength of recommendation: Strong ↑↑For patients with acute ischaemic stroke of <4.5 h duration, and high burden of white matter lesions, we suggest intravenous thrombolysis with alteplase. Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↑? | |
|
| ||
| Cerebral aneurysm | ||
| 13.6: In patients with acute ischaemic stroke of <4.5 h duration, who have an unruptured cerebral aneurysm, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, who have an unruptured cerebral artery aneurysm, we suggest IVT with alteplase.Quality of evidence: Very low ⊕Strength of recommendation: Weak ↑? | |
|
| ||
| History of ischaemic stroke | ||
| 14.1: In patients with acute ischaemic stroke of <4.5 h duration, who have a history of ischaemic stroke during the last three months, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration, and a history of ischemic stroke within the last three months, nine of nine members voted for intravenous thrombolysis with alteplase in selected cases, for example in case of a small infarct, stroke occurring more than one month earlier, or good clinical recovery. | |
|
| ||
| Seizure | ||
| 14.2: In patients with acute ischaemic stroke of <4.5 h duration, who had a seizure at time of stroke onset, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration who have seizures at time of stroke onset, and for whom there is no suspicion of a stroke mimic or significant head trauma, we suggest intravenous thrombolysis with alteplase. Quality of evidence: Very low ⊕Strength of recommendation: Weak ↑? | |
|
| ||
| Dissection | ||
| 14.3: In patients with acute ischaemic stroke of <4.5 h duration, who have dissection in the aortic arch, in a carotid artery or in an intracerebral artery, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration and with aortic arch dissection we recommend no intravenous thrombolysis.Quality of evidence: Very low ⊕Strength of recommendation: Strong ↓↓For patients with acute ischaemic stroke of <4.5 h duration and with isolated cervical artery dissections, we suggest intravenous thrombolysis with alteplase.Quality of evidence: Low ⊕⊕Strength of recommendation: Weak ↑? | For patients with acute ischaemic stroke of <4.5 h duration and with an intracerebral artery dissection, 6/9 group members suggest against intravenous thrombolysis with alteplase. |
|
| ||
| Myocardial infarction | ||
| 14.4: In patients with acute ischaemic stroke of <4.5 h duration, who have had myocardial infarction during the last three months, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration and with history of subacute (>6 h) ST-elevation myocardial infarction during the last seven days, we suggest no IVT.Quality of evidence: Very low ⊕Strength of recommendation: Weak ↓?For patients with acute ischaemic stroke of <4.5 h duration and with a history of non-ST-elevation myocardial infarction during the last three months, we suggest intravenous thrombolysis with alteplase.Quality of evidence: Very low ⊕Strength of recommendation: Weak ↑? | For patients with acute ischaemic stroke of <4.5 h duration and with history of ST-elevation myocardial infarction of more than a week to three months, 9/9 group members suggest IVT with alteplase in specific situations. Variables to take into account are the size of the myocardial infarction, whether recanalisation therapy was given for the myocardial infarction, and echocardiographic findings. |
|
| ||
| Infective endocarditis | ||
| 14.5: In patients with acute ischaemic stroke of <4.5 h duration, who have infective endocarditis, does IVT with alteplase lead to better functional outcome than no IVT? | For patients with acute ischaemic stroke of <4.5 h duration and with a clear or suspected diagnosis of infective endocarditis, we suggest no intravenous thrombolysis. Quality of evidence: Low ⊕⊕Strength of recommendation: Strong ↓↓ | |
Whenever possible, we based our recommendations on RCTs or individual participant data meta-analyses of RCTs rather than observational studies, which are more prone to selection bias and confounding. We found that there is high quality evidence for recommendations on time to treatment, patients with different ages and stroke severity, based on individual participant data analyses of all trials of IVT with alteplase to date.
We decided to provide separate recommendations for patients with unknown symptom onset and patients with known stroke onset of more than 4.5 hrs, because we believe that they correspond to two distinct clinical scenarios. Indeed, many patients with wake-up stroke may have a ‘true’ stroke onset of < 4.5 hrs.31,32 Therefore, from a pathophysiological standpoint, this situation notably differs from strokes of more than 4.5hrs’ duration. Furthermore, in our experience the information on whether the symptom onset is known or unknown is generally available when the patient arrives in the hospital. Based on the result of an individual participant data meta-analysis of RCTs,46 we recommend IVT in patients with unknown stroke onset selected with advanced imaging (DWI-FLAIR mismatch or core/perfusion mismatch). An extension of the time window beyond 4.5 h of known onset time is also possible if perfusion-diffusion MRI or CT perfusion shows potentially salvageable brain tissue. However, urgent advanced brain imaging is not always available, which may limit the immediate applicability of these recommendations. Moreover, the recent trials on the extended time window –EXTEND and ECASS-4– excluded patients for whom mechanical thrombectomy was planned, which may further reduce the number of patients qualifying of IVT beyond 4.5 h. Although there are several high-quality trials to guide practice, 29 out of 40 recommendations are based on low or very low quality of evidence. These recommendations came from meta-analyses of small trials, single modest-sized randomised trials, or observational studies. Although tenecteplase has a number of potential advantages, it is remains uncertain whether it is non-inferior to alteplase for all patients with acute ischaemic stroke. Still, we found low quality evidence to suggest tenecteplase over alteplase in patients with large vessel occlusion who are candidates for mechanical thrombectomy.
The strengths of this guideline are its systematic approach to searching the literature and guidance by the GRADE recommendations. However, many questions posed to the guideline module working group were about particular subgroups of patients with different clinical characteristics, or who were taking particular drugs at baseline. In many of these patients there are clinical uncertainties about the balance of benefit and harm of IVT. However, in the absence of studies randomly allocating participants in these subgroups to IVT or control, the precise effects of treatments are unknown. It would be a mistake to interpret a modestly higher risk of post-IVT sICH as a reason not to treat such patients, because the benefit of alteplase has not been similarly quantified. Therefore, for almost all patients the best prediction of effect of IVT is that of the average patient treated at that time point in a randomised trial rather than patient with very similar characteristics from an observational study. However, for practical reasons not all remaining questions regarding IVT can be answered by RCTs. Multicentre registries offer observational evidence that could contribute to our knowledge on IVT, particular when they are representative of all treated patients.
To support physicians in their practical decision-making, expert consensus statements are given in a dedicated paragraph. Whenever appropriate, these opinions were systematically collected as polls. About three out of four of these polls (13/17) led to a good agreement of 7–9 of the 9 group members. In the remaining questions, the group members' opinions varied considerably. The recommendations with very low evidence and poor agreement among experts were on the subjects of IVT before thrombectomy in wake-up stroke or ischaemic stroke of 4.5–9 h duration, especially in those patients directly admitted to a thrombectomy-capable centre.
A next priority of research into thrombolysis is how to implement it widely in populations with the greatest need – that is patients in those areas with the highest stroke incidence and lowest use of thrombolysis. This will need methods to make decisions about IVT as rapid and as simple as possible and remove certain barriers related to initial exclusion criteria that are not supported by current randomised or observational evidence. Implementation studies, training, further improvement in safety of IVT, reducing the cost of thrombolytics and resource allocation to stroke in the areas of Europe with the highest stroke incidence are most likely to give the greatest return on investment.
Plain language summary
Patients with stroke due to blood clots in brain arteries (‘ischaemic stroke’) can be treated with clot-dissolving drugs called ‘thrombolytics’. By dissolving blood clots, thrombolytic drugs improve brain blood supply and lead to better recovery. However, thrombolytic drugs may cause bleeding in the brain which can lead to worse disability or death. The most commonly used thrombolytic drug for ischemic stroke is called alteplase. The guideline authors make recommendations about the use of thrombolytic drugs given into a vein for patients with acute ischaemic stroke.
The guideline makes forty recommendations. The most important recommendations are:
To treat ischaemic stroke patients with alteplase if it can be started within 4.5 h of symptoms beginning. The stroke symptoms should be disabling at the time of treatment. The age of the patient does not matter.
Advanced brain imaging (magnetic resonance or CT perfusion) should be used to select patients for treatment with alteplase, if they present between 4.5 and 9 h after the start of symptoms, or if a stroke is noticed at waking from sleep.
To avoid treatment with low dose alteplase, or to add ultrasound or immediate antiplatelet drugs to alteplase because they do not give a better chance of surviving with no disability.
- If an ischaemic stroke patient could be treated with alteplase, do not avoid treatment if the patient:
- has a diagnosis of high blood pressure, diabetes, previous stroke, or a heart attack
- takes antiplatelet drugs like aspirin
- At the time of stroke has a high blood glucose level, or an epileptic seizure (if the diagnosis of stroke is certain) or dissection of the carotid artery
- Has had a brain scan that shows a brain aneurysm that has not burst, or < 10 tiny brain bleeds (microbleeds), or damage to the brain ‘white matter’
- has had a brain bleed because of a cause unlikely to re-occur
- Generally, to avoid treatment with alteplase if the ischaemic patient is taking blood thinning drugs such as a ‘direct oral anticoagulants’ or warfarin, unless:
- The patient is taking warfarin and the INR (a measure of blood clotting) is known to be < 1.7.
- The patient had been prescribed a ‘direct oral anticoagulant’ (such as apixaban, dabigatran, rivaroxaban, edoxaban) but has not taken the drug in the 48 h before stroke.
Generally to avoid treatment with alteplase if the patient has recently had major surgery, major trauma, infection of the heart valves (endocarditis), or dissection of the aorta. If the patient is known to have more than ten tiny bleeds of the brain (microbleeds) or very low levels of blood platelets, treatment should be avoided, but looking for these with blood tests or extra brain scans should not delay treatment.
An alternative thrombolytic drug, tenecteplase, may be favored over alteplase before clot pulling treatment (thrombectomy), but its place to treat all patients is uncertain.
Once blood pressure is lower than 185 mmHg systolic or 110 mmHg diastolic, alteplase can be given safely.
The major recommendations were supported by high to moderate quality evidence. Other than for age and stroke severity, there was weaker evidence to support when to use alteplase in very particular situations.
Supplemental Material
Supplemental material, sj-pdf-1-eso-10.1177_2396987321989865 for European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke by Eivind Berge, William Whiteley, Heinrich Audebert, Gian Marco De Marchis, Ana Catarina Fonseca, Chiara Padiglioni, Natalia Pérez de la Ossa, Daniel Strbian, Georgios Tsivgoulis and Guillaume Turc in European Stroke Journal
Acknowledgments
We thank Joshua Cheyne for his help with the systematic review of the literature.
Footnotes
Declaration of conflicting interests: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All disclosures are listed in Supplemental Table 1
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: No ethical approval was needed for this manuscript, which is an ESO Guideline.
Informed consent: Not relevant for this type of manuscript.
Guarantor: G Turc
Contributorship: EB, WW and G Turc conceived the study. All authors searched the literature. G Turc, GMDM and G Tsivgoulis conducted the statistical analysis. All authors contributed to writing the first draft of the manuscript, under the supervision of EB, WW and G Turc. All authors reviewed and edited the manuscript several times and approved the final version of the manuscript.
ORCID iDs: Ana Catarina Fonseca https://orcid.org/0000-0001-6913-5526
Guillaume Turc https://orcid.org/0000-0001-5059-4095
Supplemental material: Supplemental material for this article is available online.
References
- 1.European Stroke Organisation. Guidelines for management of ischaemic stroke and transient ischaemic attack. Cerebrovasc Dis 2008; 25: 457–507. [DOI] [PubMed] [Google Scholar]
- 2.Hart JT. The inverse care law. Lancet 1971; 1: 405–412. [DOI] [PubMed] [Google Scholar]
- 3.Aguiar de Sousa D, von Martial R, Abilleira S, et al. Access to and delivery of acute ischaemic stroke treatments: a survey of national scientific societies and stroke experts in 44 European countries. Eur Stroke J 2019; 4: 13–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ntaios G, Bornstein NM, Caso V, et al.; European Stroke Organisation. The European stroke organisation guidelines: a standard operating procedure. Int J Stroke 2015; 10 Suppl A100: 128–135. [DOI] [PubMed] [Google Scholar]
- 5.Guyatt GH, Oxman AD, Schunemann HJ, et al. GRADE guidelines: a new series of articles in the journal of clinical epidemiology. J Clin Epidemiol 2011; 64: 380–382. [DOI] [PubMed] [Google Scholar]
- 6.Wardlaw JM, Murray V, Berge E, et al. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 2014: CD000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019), www.training.cochrane.org/handbook (accessed 21 August 2020).
- 8.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384: 1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.IST-3 collaborative group. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 2012; 379: 2352–2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whiteley WN, Emberson J, Lees KR, et al. ; Stroke Thrombolysis Trialists’ Collaboration. Risk of intracerebral haemorrhage with alteplase after acute ischaemic stroke: a secondary analysis of an individual patient data meta-analysis. Lancet Neurol 2016; 15: 925–933. [DOI] [PubMed] [Google Scholar]
- 11.IST-3 Collaborative Group. Effect of thrombolysis with alteplase within 6 h of acute ischaemic stroke on long-term outcomes (the third international stroke trial [IST-3]): 18-month follow-up of a randomised controlled trial. Lancet Neurol 2013; 12: 768–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berge E, Cohen G, Roaldsen MB, et al.; IST-3 Collaborative Group. Effects of alteplase on survival after ischaemic stroke (IST-3): 3 year follow-up of a randomised, controlled, open-label trial. Lancet Neurol 2016; 15: 1028–1034. [DOI] [PubMed] [Google Scholar]
- 13.Alper BS, Foster G, Thabane L, et al. Thrombolysis with alteplase 3–4.5 hours after acute ischaemic stroke: trial reanalysis adjusted for baseline imbalances. BMJ Evid Based Med 2020; 25: 168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO) – European society for minimally invasive neurological therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischaemic stroke. Eur Stroke J 2019; 4: 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang P, Zhang Y, Zhang L, et al.; DIRECT-MT Investigators. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med 2020; 382: 1981–1993. [DOI] [PubMed] [Google Scholar]
- 16.Nogueira RG, Tsivgoulis G. Large vessel occlusion strokes after the DIRECT-MT and SKIP trials: is the alteplase syringe half empty or half full? Stroke 2020; 51: 3182–3186. [DOI] [PubMed] [Google Scholar]
- 17.NINDS rtPA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995; 333: 1581–1587. [DOI] [PubMed] [Google Scholar]
- 18.Barow E, Boutitie F, Cheng B, et al.; WAKE-UP Investigators. Functional outcome of intravenous thrombolysis in patients with lacunar infarcts in the WAKE-UP trial. JAMA Neurol 2019; 76: 641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mair G, von Kummer R, Adami A, et al. Arterial obstruction on computed tomographic or magnetic resonance angiography and response to intravenous thrombolytics in ischemic stroke. Stroke 2017; 48: 353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiebach JB, Galinovic I, Boutitie F, et al. Large vessel occlusion does not modify treatment effects of intravenous alteplase in the WAKE-UP trial. In: European Stroke Organisation conference, Milan, Italy, 22–24 May 2019.
- 21.Clark WM, Albers GW, Madden KP, et al. The rtPA (alteplase) 0- to 6-hour acute stroke trial, part A (A0276g): results of a double-blind, placebo-controlled, multicenter study. Thromblytic therapy in acute ischemic stroke study investigators. Stroke 2000; 31: 811–816. [DOI] [PubMed] [Google Scholar]
- 22.Clark WM, Wissman S, Albers GW, et al. Recombinant tissue-type plasminogen activator (alteplase) for ischemic stroke 3 to 5 hours after symptom onset. The ATLANTIS study: a randomized controlled trial. Alteplase thrombolysis for acute noninterventional therapy in ischemic stroke. JAMA 1999; 282: 2019–2026. [DOI] [PubMed] [Google Scholar]
- 23.Hacke W, Kaste M, Fieschi C, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European cooperative acute stroke study (ECASS). JAMA 1995; 274: 1017–1025. [PubMed] [Google Scholar]
- 24.Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). second European-Australasian acute stroke study investigators. Lancet 1998; 352: 1245–1251. [DOI] [PubMed] [Google Scholar]
- 25.Davis SM, Donnan GA, Parsons MW, et al. Effects of alteplase beyond 3 h after stroke in the echoplanar imaging thrombolytic evaluation trial (EPITHET): a placebo-controlled randomised trial. Lancet Neurol 2008; 7: 299–309. [DOI] [PubMed] [Google Scholar]
- 26.Lees KR, Emberson J, Blackwell L, et al.; Stroke Thrombolysis Trialists’ Collaborators Group. Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke 2016; 47: 2373–2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hacke W, Lyden P, Emberson J, et al.; Stroke Thrombolysis Trialists’ Collaborators Group. Effects of alteplase for acute stroke according to criteria defining the European union and United States marketing authorizations: individual-patient-data meta-analysis of randomized trials. Int J Stroke 2018; 13: 175–189. [DOI] [PubMed] [Google Scholar]
- 28.Fulton RL, Lees KR, Bluhmki E, et al.; VISTA Collaboration and ECASS, ATLANTIS, NINDS, and EPITHET Investigators. Selection for delayed intravenous alteplase treatment based on a prognostic score. Int J Stroke 2015; 10: 90–94. [DOI] [PubMed] [Google Scholar]
- 29.Ma H, Campbell BCV, Parsons MW, et al.; EXTEND Investigators. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med 2019; 380: 1795–1803. [DOI] [PubMed] [Google Scholar]
- 30.Ringleb P, Bendszus M, Bluhmki E, et al.; ECASS-4 Study Group. Extending the time window for intravenous thrombolysis in acute ischemic stroke using magnetic resonance imaging-based patient selection. Int J Stroke 2019; 14: 483–490. [DOI] [PubMed] [Google Scholar]
- 31.Fink JN, Kumar S, Horkan C, et al. The stroke patient who woke up: clinical and radiological features, including diffusion and perfusion MRI. Stroke 2002; 33: 988–993. [DOI] [PubMed] [Google Scholar]
- 32.Rimmele DL, Thomalla G. Wake-up stroke: clinical characteristics, imaging findings, and treatment option – an update. Front Neurol 2014; 5: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ogata T, Christensen S, Nagakane Y, et al.; EPITHET and DEFUSE Investigators. The effects of alteplase 3 to 6 hours after stroke in the EPITHET-DEFUSE combined dataset: post hoc case-control study. Stroke 2013; 44: 87–93. [DOI] [PubMed] [Google Scholar]
- 34.Campbell BCV, Ma H, Ringleb PA, et al. Extending thrombolysis to 4.5-9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet 2019; 394: 139–147. [DOI] [PubMed] [Google Scholar]
- 35.Psychogios K, Magoufis G, Safouris A, et al. Eligibility for intravenous thrombolysis in acute ischemic stroke patients presenting in the 4.5-9 h window. Neuroradiology 2020; 62: 733–739. [DOI] [PubMed] [Google Scholar]
- 36.Wei XE, Zhou J, Li WB, et al. MRI based thrombolysis for FLAIR-negative stroke patients within 4.5-6h after symptom onset. J Neurol Sci 2017; 372: 421–427. [DOI] [PubMed] [Google Scholar]
- 37.Bassetti C, Aldrich M. Night time versus daytime transient ischaemic attack and ischaemic stroke: a prospective study of 110 patients. J Neurol Neurosurg Psychiatry 1999; 67: 463–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mackey J, Kleindorfer D, Sucharew H, et al. Population-based study of wake-up strokes. Neurology 2011; 76: 1662–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomalla G, Simonsen CZ, Boutitie F, et al.; WAKE-UP Investigators. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med 2018; 379: 611–622. [DOI] [PubMed] [Google Scholar]
- 40.Koga M, Toyoda K, Kimura K, et al.; THAWS Investigators. Thrombolysis for acute wake-up and unclear-onset strokes with alteplase at 0.6 mg/kg (THAWS) trial. Int J Stroke 2014; 9: 1117–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michel P, Ntaios G, Reichhart M, et al. Perfusion-CT guided intravenous thrombolysis in patients with unknown-onset stroke: a randomized, double-blind, placebo-controlled, pilot feasibility trial. Neuroradiology 2012; 54: 579–588. [DOI] [PubMed] [Google Scholar]
- 42.Pfaff JAR, Bendszus M, Donnan G, et al. Abstract WSC18-1299 – the impact of the DWI-FLAIR-mismatch in the ECASS-4 trial – a posthoc analysis. Int J Stroke 2018; 13: 227. [Google Scholar]
- 43.Thomalla G, Cheng B, Ebinger M, et al. DWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4.5 h of symptom onset (PRE-FLAIR): a multicentre observational study. Lancet Neurol 2011; 10: 978–986. [DOI] [PubMed] [Google Scholar]
- 44.Koga M, Yamamoto H, Inoue M, et al.; THAWS Trial Investigators. Thrombolysis with alteplase at 0.6 mg/kg for stroke with unknown time of onset: a randomized controlled trial. Stroke 2020; 51: 1530–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leira EC, Muir KW. EXTEND trial. Stroke 2019; 50: 2637–2639. [DOI] [PubMed] [Google Scholar]
- 46.Thomalla G, Boutitie F, Ma H, et al. Intravenous alteplase for stroke with unknown time of onset guided by advanced imaging: systematic review and meta-analysis of individual patient data. Lancet 2020; 396: 1574–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haley EC, Jr, Thompson JL, Grotta JC, et al.; Tenecteplase in Stroke Investigators. Phase IIB/III trial of tenecteplase in acute ischemic stroke: results of a prematurely terminated randomized clinical trial. Stroke 2010; 41: 707–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang X, Cheripelli BK, Lloyd SM, et al. Alteplase versus tenecteplase for thrombolysis after ischaemic stroke (ATTEST): a phase 2, randomised, open-label, blinded endpoint study. Lancet Neurol 2015; 14: 368–376. [DOI] [PubMed] [Google Scholar]
- 49.Logallo N, Novotny V, Assmus J, et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (nor-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol 2017; 16: 781–788. [DOI] [PubMed] [Google Scholar]
- 50.Parsons M, Spratt N, Bivard A, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Engl J Med 2012; 366: 1099–1107. [DOI] [PubMed] [Google Scholar]
- 51.Campbell BCV, Mitchell PJ, Churilov L, et al.; EXTEND-IA TNK Investigators. Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med 2018; 378: 1573–1582. [DOI] [PubMed] [Google Scholar]
- 52.Kheiri B, Osman M, Abdalla A, et al. Tenecteplase versus alteplase for management of acute ischemic stroke: a pairwise and network Meta-analysis of randomized clinical trials. J Thromb Thrombolysis 2018; 46: 440–450. [DOI] [PubMed] [Google Scholar]
- 53.Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischemic stroke: meta-analysis of 5 randomized trials. Stroke 2019; 50: 2156–2162. [DOI] [PubMed] [Google Scholar]
- 54.Anderson CS, Robinson T, Lindley RI, et al.; ENCHANTED Investigators and Coordinators. Low-dose versus standard-dose intravenous alteplase in acute ischemic stroke. N Engl J Med 2016; 374: 2313–2323. [DOI] [PubMed] [Google Scholar]
- 55.Bivard A, Huang X, Levi CR, et al. Tenecteplase in ischemic stroke offers improved recanalization: analysis of 2 trials. Neurology 2017; 89: 62–67. [DOI] [PubMed] [Google Scholar]
- 56.Campbell BCV, Mitchell PJ, Churilov L, et al.; EXTEND-IA TNK Part 2 Investigators. Effect of intravenous tenecteplase dose on cerebral reperfusion before thrombectomy in patients with large vessel occlusion ischemic stroke: the EXTEND-IA TNK part 2 randomized clinical trial. JAMA 2020; 323: 1257–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liebeskind DS, Bracard S, Guillemin F, et al.; HERMES Collaborators. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg 2019; 11: 433–438. [DOI] [PubMed] [Google Scholar]
- 58.Strbian D, Saposnik G. Review of the ENCHANTED trial (enhanced control of hypertension and thrombolysis stroke study): how low can we go with intravenous tissue-type plasminogen activator dose and blood pressure level? Stroke 2016; 47: 3063–3064. [DOI] [PubMed] [Google Scholar]
- 59.Wang X, Robinson TG, Lee TH, et al.; Enhanced Control of Hypertension and Thrombolysis Stroke Study (ENCHANTED) Investigators. Low-dose vs standard-dose alteplase for patients with acute ischemic stroke: secondary analysis of the ENCHANTED randomized clinical trial. JAMA Neurol 2017; 74: 1328–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carr SJ, Wang X, Olavarria VV, et al. Influence of renal impairment on outcome for thrombolysis-treated acute ischemic stroke: ENCHANTED (enhanced control of hypertension and thrombolysis stroke study) post hoc analysis. Stroke 2017; 48: 2605–2609. [DOI] [PubMed] [Google Scholar]
- 61.Chen G, Wang X, Robinson TG, et al.; ENCHANTED Investigators. Comparative effects of low-dose versus standard-dose alteplase in ischemic patients with prior stroke and/or diabetes mellitus: the ENCHANTED trial. J Neurol Sci 2018; 387: 1–5. [DOI] [PubMed] [Google Scholar]
- 62.Robinson TG, Wang X, Arima H, et al.; ENCHANTED Investigators. Low-versus standard-dose alteplase in patients on prior antiplatelet therapy: the ENCHANTED trial (enhanced control of hypertension and thrombolysis stroke study). Stroke 2017; 48: 1877–1883. [DOI] [PubMed] [Google Scholar]
- 63.Schellinger PD, Tsivgoulis G. Another enchantment from ENCHANTED (enhanced control of hypertension and thrombolysis stroke study): are savings and safety more salutary than efficacy? Stroke 2017; 48: 1720–1722. [DOI] [PubMed] [Google Scholar]
- 64.Yamaguchi T, Mori E, Minematsu K, et al.; Japan Alteplase Clinical Trial (J-ACT) Group. Alteplase at 0.6 mg/kg for acute ischemic stroke within 3 hours of onset: Japan alteplase clinical trial (J-ACT). Stroke 2006; 37: 1810–1815. [DOI] [PubMed] [Google Scholar]
- 65.Mori E, Minematsu K, Nakagawara J, et al.; Japan Alteplase Clinical Trial II Group. Effects of 0.6 mg/kg intravenous alteplase on vascular and clinical outcomes in middle cerebral artery occlusion: Japan alteplase clinical trial II (J-ACT II). Stroke 2010; 41: 461–465. [DOI] [PubMed] [Google Scholar]
- 66.Toyoda K, Koga M, Naganuma M, et al. Routine use of intravenous low-dose recombinant tissue plasminogen activator in Japanese patients: general outcomes and prognostic factors from the SAMURAI register. Stroke 2009; 40: 3591–3595. [DOI] [PubMed] [Google Scholar]
- 67.Nakagawara J, Minematsu K, Okada Y, et al.; for J-MARS Investigators. Thrombolysis with 0.6 mg/kg intravenous alteplase for acute ischemic stroke in routine clinical practice: the Japan post-marketing alteplase registration study (J-MARS). Stroke 2010; 41: 1984–1989. [DOI] [PubMed] [Google Scholar]
- 68.Chao AC, Hsu HY, Chung CP, et al.; Taiwan Thrombolytic Therapy for Acute Ischemic Stroke (TTT-AIS) Study Group. Outcomes of thrombolytic therapy for acute ischemic stroke in Chinese patients: the Taiwan thrombolytic therapy for acute ischemic stroke (TTT-AIS) study. Stroke 2010; 41: 885–890. [DOI] [PubMed] [Google Scholar]
- 69.Kim BJ, Han MK, Park TH, et al. Low-versus standard-dose alteplase for ischemic strokes within 4.5 hours: a comparative effectiveness and safety study. Stroke 2015; 46: 2541–2548. [DOI] [PubMed] [Google Scholar]
- 70.Liao X, Wang Y, Pan Y, et al. Standard-dose intravenous tissue-type plasminogen activator for stroke is better than low doses. Stroke 2014; 45: 2354–2358. [DOI] [PubMed] [Google Scholar]
- 71.Wang Y, Liao X, Zhao X, et al.; China National Stroke Registry Investigators. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese national stroke registry (CNSR). Stroke 2011; 42: 1658–1664. [DOI] [PubMed] [Google Scholar]
- 72.Sharma VK, Ng KW, Venketasubramanian N, et al. Current status of intravenous thrombolysis for acute ischemic stroke in Asia. Int J Stroke 2011; 6: 523–530. [DOI] [PubMed] [Google Scholar]
- 73.Alexandrov AV, Grotta JC. Arterial reocclusion in stroke patients treated with intravenous tissue plasminogen activator. Neurology 2002; 59: 862–867. [DOI] [PubMed] [Google Scholar]
- 74.Rubiera M, Alvarez-Sabin J, Ribo M, et al. Predictors of early arterial reocclusion after tissue plasminogen activator-induced recanalization in acute ischemic stroke. Stroke 2005; 36: 1452–1456. [DOI] [PubMed] [Google Scholar]
- 75.Barreto AD, Alexandrov AV. Adjunctive and alternative approaches to current reperfusion therapy. Stroke 2012; 43: 591–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Harsany M, Tsivgoulis G, Alexandrov AV. Intravenous thrombolysis in acute ischemic stroke: standard and potential future applications. Expert Rev Neurother 2014; 14: 879–892. [DOI] [PubMed] [Google Scholar]
- 77.Zinkstok SM, Roos YB. and ARTIS Investigators. Early administration of aspirin in patients treated with alteplase for acute ischaemic stroke: a randomised controlled trial. Lancet 2012; 380: 731–737. [DOI] [PubMed] [Google Scholar]
- 78.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359: 1317–1329. [DOI] [PubMed] [Google Scholar]
- 79.Pancioli AM, Broderick J, Brott T, et al.; CLEAR Trial Investigators. The combined approach to lysis utilizing eptifibatide and rt-PA in acute ischemic stroke: the CLEAR stroke trial. Stroke 2008; 39: 3268–3276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pancioli AM, Adeoye O, Schmit PA, et al.; CLEAR-ER Investigators. Combined approach to lysis utilizing eptifibatide and recombinant tissue plasminogen activator in acute ischemic stroke-enhanced regimen stroke trial. Stroke 2013; 44: 2381–2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Adeoye O, Sucharew H, Khoury J, et al.; CLEAR-ER, IMS III, and ALIAS Part 2 Investigators. Recombinant tissue-type plasminogen activator plus eptifibatide versus recombinant tissue-type plasminogen activator alone in acute ischemic stroke: propensity score-matched post hoc analysis. Stroke 2015; 46: 461–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Adeoye O, Sucharew H, Khoury J, et al. Combined approach to lysis utilizing eptifibatide and recombinant tissue-type plasminogen activator in acute ischemic stroke – full dose regimen stroke trial. Stroke 2015; 46: 2529–2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li W, Lin L, Zhang M, et al. Safety and preliminary efficacy of early tirofiban treatment after alteplase in acute ischemic stroke patients. Stroke 2016; 47: 2649–2651. [DOI] [PubMed] [Google Scholar]
- 84.Barreto AD, Alexandrov AV, Lyden P, et al. The argatroban and tissue-type plasminogen activator stroke study: final results of a pilot safety study. Stroke 2012; 43: 770–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barreto AD, Ford GA, Shen L, et al.; ARTSS-2 Investigators. Randomized, multicenter trial of ARTSS-2 (argatroban with recombinant tissue plasminogen activator for acute stroke). Stroke 2017; 48: 1608–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tsivgoulis G, Culp WC, Alexandrov AV. Ultrasound enhanced thrombolysis in acute arterial ischemia. Ultrasonics 2008; 48: 303–311. [DOI] [PubMed] [Google Scholar]
- 87.Tsivgoulis G, Alexandrov AV. Ultrasound-enhanced thrombolysis in acute ischemic stroke: potential, failures, and safety. Neurotherapeutics 2007; 4: 420–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Eggers J, Koch B, Meyer K, et al. Effect of ultrasound on thrombolysis of middle cerebral artery occlusion. Ann Neurol 2003; 53: 797–800. [DOI] [PubMed] [Google Scholar]
- 89.Eggers J, KöNig IR, Koch B, et al. Sonothrombolysis with transcranial color-coded sonography and recombinant tissue-type plasminogen activator in acute Middle cerebral artery main stem occlusion: results from a randomized study. Stroke 2008; 39: 1470–1475. [DOI] [PubMed] [Google Scholar]
- 90.Alexandrov AV, Molina CA, Grotta JC, et al.; CLOTBUST Investigators. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 2004; 351: 2170–2178. [DOI] [PubMed] [Google Scholar]
- 91.Tsivgoulis G, Eggers J, Ribo M, et al. Safety and efficacy of ultrasound-enhanced thrombolysis: a comprehensive review and meta-analysis of randomized and nonrandomized studies. Stroke 2010; 41: 280–287. [DOI] [PubMed] [Google Scholar]
- 92.Ricci S, Dinia L, Del Sette M, et al. Sonothrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 2012: CD008348. [DOI] [PubMed] [Google Scholar]
- 93.Barlinn K, Tsivgoulis G, Barreto AD, et al. Outcomes following sonothrombolysis in severe acute ischemic stroke: subgroup analysis of the CLOTBUST trial. Int J Stroke 2014; 9: 1006–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nacu A, Kvistad CE, Logallo N, et al. A pragmatic approach to sonothrombolysis in acute ischaemic stroke: the Norwegian randomised controlled sonothrombolysis in acute stroke study (nor-SASS). BMC Neurol 2015; 15: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nacu A, Kvistad CE, Naess H, et al. Nor-SASS (Norwegian sonothrombolysis in acute stroke study): randomized controlled contrast-enhanced sonothrombolysis in an unselected acute ischemic stroke population. Stroke 2017; 48: 335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schellinger PD, Alexandrov AV, Barreto AD, et al.; CLOTBUSTER Investigators. Combined lysis of thrombus with ultrasound and systemic tissue plasminogen activator for emergent revascularization in acute ischemic stroke (CLOTBUST-ER): design and methodology of a multinational phase 3 trial. Int J Stroke 2015; 10: 1141–1148. [DOI] [PubMed] [Google Scholar]
- 97.Alexandrov AV, Kohrmann M, Soinne L, et al.; CLOTBUST-ER Trial Investigators. Safety and efficacy of sonothrombolysis for acute ischaemic stroke: a multicentre, double-blind, phase 3, randomised controlled trial. Lancet Neurol 2019; 18: 338–347. [DOI] [PubMed] [Google Scholar]
- 98.Bluhmki E, Danays T, Biegert G, et al. Alteplase for acute ischemic stroke in patients aged >80 years: pooled analyses of individual patient data. Stroke 2020; 51: 2322–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lorenzano S, Vestri A, Bovi P, et al. Thrombolysis in elderly stroke patients in Italy (TESPI) trial and updated meta-analysis of randomized controlled trials. Int J Stroke 2021; 16: 43–54. [DOI] [PubMed] [Google Scholar]
- 100.IST-3 Collaborative Group. Association between brain imaging signs, early and late outcomes, and response to intravenous alteplase after acute ischaemic stroke in the third international stroke trial (IST-3): secondary analysis of a randomised controlled trial. Lancet Neurol 2015; 14: 485–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jung JM, Kim HJ, Ahn H, et al. Chronic kidney disease and intravenous thrombolysis in acute stroke: a systematic review and meta-analysis. J Neurol Sci 2015; 358: 345–350. [DOI] [PubMed] [Google Scholar]
- 102.Hao Z, Yang C, Liu M, et al. Renal dysfunction and thrombolytic therapy in patients with acute ischemic stroke: a systematic review and meta-analysis. Medicine (Baltimore) 2014; 93: e286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gensicke H, Zinkstok SM, Roos YB, et al. IV thrombolysis and renal function. Neurology 2013; 81: 1780–1788. [DOI] [PubMed] [Google Scholar]
- 104.Malhotra K, Katsanos AH, Goyal N, et al. Intravenous thrombolysis in patients with chronic kidney disease: a systematic review and meta-analysis. Neurology 2020; 95: e121–e130. [DOI] [PubMed] [Google Scholar]
- 105.Cappellari M, Carletti M, Micheletti N, et al. Intravenous alteplase for acute ischemic stroke in patients with current malignant neoplasm. J Neurol Sci 2013; 325: 100–102. [DOI] [PubMed] [Google Scholar]
- 106.Gumbinger C, Reuter B, Hacke W, et al. Restriction of therapy mainly explains lower thrombolysis rates in reduced stroke service levels. Neurology 2016; 86: 1975–1983. [DOI] [PubMed] [Google Scholar]
- 107.Gensicke H, Strbian D, Zinkstok SM, et al.; Thrombolysis in Stroke Patients (TriSP) Collaborators. Intravenous thrombolysis in patients dependent on the daily help of others before stroke. Stroke 2016; 47: 450–456. [DOI] [PubMed] [Google Scholar]
- 108.Nolte CH, Ebinger M, Scheitz JF, et al. Effects of prehospital thrombolysis in stroke patients with prestroke dependency. Stroke 2018; 49: 646–651. [DOI] [PubMed] [Google Scholar]
- 109.Karlinski M, Kobayashi A, Czlonkowska A, et al.; Safe Implementation of Treatments in Stroke–Eastern Europe (SITS-EAST) Investigators. Role of preexisting disability in patients treated with intravenous thrombolysis for ischemic stroke. Stroke 2014; 45: 770–775. [DOI] [PubMed] [Google Scholar]
- 110.Paley L, Bray B, James M, et al. Abstract 152: complications and outcomes from thrombolysis in stroke patients with significant pre-stroke disability: data from the UK national stroke registry. Stroke 2016; 47: A150. [Google Scholar]
- 111.Murao K, Bodenant M, Cordonnier C, et al. Does pre-existing cognitive impairment no-dementia influence the outcome of patients treated by intravenous thrombolysis for cerebral ischaemia? J Neurol Neurosurg Psychiatry 2013; 84: 1412–1414. [DOI] [PubMed] [Google Scholar]
- 112.Fischer U, Baumgartner A, Arnold M, et al. What is a minor stroke? Stroke 2010; 41: 661–666. [DOI] [PubMed] [Google Scholar]
- 113.Khatri P, Conaway MR, Johnston KC; Acute Stroke Accurate Prediction Study (ASAP) Investigators. Ninety-day outcome rates of a prospective cohort of consecutive patients with mild ischemic stroke. Stroke 2012; 43: 560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Khatri P, Kleindorfer DO, Devlin T, et al.; PRISMS Investigators. Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: the PRISMS randomized clinical trial. JAMA 2018; 320: 156–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yeatts SD, Broderick JP, Chatterjee A, et al. Alteplase for the treatment of acute ischemic stroke in patients with low national institutes of health stroke scale and not clearly disabling deficits (potential of rtPA for ischemic strokes with mild symptoms PRISMS): rationale and design. Int J Stroke 2018; 13: 654–661. [DOI] [PubMed] [Google Scholar]
- 116.Seners P, Turc G, Oppenheim C, et al. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry 2015; 86: 87–94. [DOI] [PubMed] [Google Scholar]
- 117.Coutts SB, Dubuc V, Mandzia J, et al.; TEMPO-1 Investigators. Tenecteplase-tissue-type plasminogen activator evaluation for minor ischemic stroke with proven occlusion. Stroke 2015; 46: 769–774. [DOI] [PubMed] [Google Scholar]
- 118.Tsivgoulis G, Goyal N, Katsanos AH, et al. Intravenous thrombolysis for large vessel or distal occlusions presenting with mild stroke severity. Eur J Neurol 2020; 27: 1039–1047. [DOI] [PubMed] [Google Scholar]
- 119.Seners P, Perrin C, Lapergue B, et al.; MINOR-STROKE Collaborators. Bridging therapy or IV thrombolysis in minor stroke with large vessel occlusion. Ann Neurol 2020; 88: 160–169. [DOI] [PubMed] [Google Scholar]
- 120.Smith EE, Fonarow GC, Reeves MJ, et al. Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator: findings from get with the guidelines-stroke. Stroke 2011; 42: 3110–3115. [DOI] [PubMed] [Google Scholar]
- 121.Levine SR, Khatri P, Broderick JP, et al.; Re-examining Acute Eligibility for Thrombolysis (TREAT) Task Force. Review, historical context, and clarifications of the NINDS rt-PA stroke trials exclusion criteria: part 1: rapidly improving stroke symptoms. Stroke 2013; 44: 2500–2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Demaerschalk BM, Kleindorfer DO, Adeoye OM, et al.; American Heart Association Stroke Council and Council on Epidemiology and Prevention. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016; 47: 581–641. [DOI] [PubMed] [Google Scholar]
- 123.Hill MD, Buchan AM; Canadian Alteplase for Stroke Effectiveness Study (CASES) Investigators. Thrombolysis for acute ischemic stroke: results of the Canadian alteplase for stroke effectiveness study. CMAJ 2005; 172: 1307–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Albers GW, Bates VE, Clark WM, et al. Intravenous tissue-type plasminogen activator for treatment of acute stroke: the standard treatment with alteplase to reverse stroke (STARS) study. JAMA 2000; 283: 1145–1150. [DOI] [PubMed] [Google Scholar]
- 125.Patel SC, Levine SR, Tilley BC, et al. Lack of clinical significance of early ischemic changes on computed tomography in acute stroke. JAMA 2001; 286: 2830–2838. [DOI] [PubMed] [Google Scholar]
- 126.Dzialowski I, Hill MD, Coutts SB, et al. Extent of early ischemic changes on computed tomography (CT) before thrombolysis: prognostic value of the Alberta stroke program early CT score in ECASS II. Stroke 2006; 37: 973–978. [DOI] [PubMed] [Google Scholar]
- 127.Von Kummer R, Allen KL, Holle R, et al. Acute stroke: usefulness of early CT findings before thrombolytic therapy. Radiology 1997; 205: 327–333. [DOI] [PubMed] [Google Scholar]
- 128.Hill MD, Demchuk AM, Tomsick TA, et al. Using the baseline CT scan to select acute stroke patients for IV-IA therapy. AJNR Am J Neuroradiol 2006; 27: 1612–1616. [PMC free article] [PubMed] [Google Scholar]
- 129.Lindley RI, Wardlaw JM, Whiteley WN, et al.; IST-3 Collaborative Group. Alteplase for acute ischemic stroke: outcomes by clinically important subgroups in the third international stroke trial. Stroke 2015; 46: 746–756. [DOI] [PubMed] [Google Scholar]
- 130.Yong M, Kaste M. Association of characteristics of blood pressure profiles and stroke outcomes in the ECASS-II trial. Stroke 2008; 39: 366–372. [DOI] [PubMed] [Google Scholar]
- 131.Berge E, Cohen G, Lindley RI, et al. Effects of blood pressure and blood pressure-lowering treatment during the first 24 hours among patients in the third international stroke trial of thrombolytic treatment for acute ischemic stroke. Stroke 2015; 46: 3362–3369. [DOI] [PubMed] [Google Scholar]
- 132.Tsivgoulis G, Frey JL, Flaster M, et al. Pre-tissue plasminogen activator blood pressure levels and risk of symptomatic intracerebral hemorrhage. Stroke 2009; 40: 3631–3634. [DOI] [PubMed] [Google Scholar]
- 133.Mundiyanapurath S, Hees K, Ahmed N, et al. Predictors of symptomatic intracranial haemorrhage in off-label thrombolysis: an analysis of the safe implementation of treatments in stroke registry. Eur J Neurol 2018; 25: e340–e311. [DOI] [PubMed] [Google Scholar]
- 134.Malhotra K, Ahmed N, Filippatou A, et al. Association of elevated blood pressure levels with outcomes in acute ischemic stroke patients treated with intravenous thrombolysis: a systematic review and meta-analysis. J Stroke 2019; 21: 78–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Waltimo T, Haapaniemi E, Surakka IL, et al. Post-thrombolytic blood pressure and symptomatic intracerebral hemorrhage. Eur J Neurol 2016; 23: 1757–1762. [DOI] [PubMed] [Google Scholar]
- 136.Anderson CS, Huang Y, Lindley RI, et al. Intensive blood pressure reduction with intravenous thrombolysis therapy for acute ischaemic stroke (ENCHANTED): an international, randomised, open-label, blinded-endpoint, phase 3 trial. Lancet 2019; 393: 877–888. [DOI] [PubMed] [Google Scholar]
- 137.Brott T, Lu M, Kothari R, et al. Hypertension and its treatment in the NINDS rt-PA stroke trial. Stroke 1998; 29: 1504–1509. [DOI] [PubMed] [Google Scholar]
- 138.Bluhmki E, Chamorro A, Davalos A, et al. Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 2009; 8: 1095–1102. [DOI] [PubMed] [Google Scholar]
- 139.Kent DM, Ruthazer R, Decker C, et al. Development and validation of a simplified stroke-thrombolytic predictive instrument. Neurology 2015; 85: 942–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bruno A, Levine SR, Frankel MR, et al.; NINDS rt-PA Stroke Study Group. Admission glucose level and clinical outcomes in the NINDS rt-PA stroke trial. Neurology 2002; 59: 669–674. [DOI] [PubMed] [Google Scholar]
- 141.Shah NH, Velez V, Casanova T, et al. Hyperglycemia presenting as left middle cerebral artery stroke: a case report. J Vasc Interv Neurol 2014; 7: 9–12. [PMC free article] [PubMed] [Google Scholar]
- 142.Frank B, Grotta JC, Alexandrov AV, et al.; VISTA Collaborators. Thrombolysis in stroke despite contraindications or warnings? Stroke 2013; 44: 727–733. [DOI] [PubMed] [Google Scholar]
- 143.Yong M, Kaste M. Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke 2008; 39: 2749–2755. [DOI] [PubMed] [Google Scholar]
- 144.Fuentes B, Ntaios G, Putaala J, et al.; European Stroke Organisation. European Stroke Organisation (ESO) guidelines on glycaemia management in acute stroke. Eur Stroke J 2018; 3: 5–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ahmed N, Davalos A, Eriksson N, et al. Association of admission blood glucose and outcome in patients treated with intravenous thrombolysis: results from the safe implementation of treatments in stroke international stroke thrombolysis register (SITS-ISTR). Arch Neurol 2010; 67: 1123–1130. [DOI] [PubMed] [Google Scholar]
- 146.Karlinski M, Kobayashi A, Mikulik R, et al. Intravenous alteplase in ischemic stroke patients not fully adhering to the current drug license in Central and Eastern Europe. Int J Stroke 2012; 7: 615–622. [DOI] [PubMed] [Google Scholar]
- 147.Johnston KC, Bruno A, Pauls Q, et al.; Neurological Emergencies Treatment Trials Network and the SHINE Trial Investigators. Intensive vs standard treatment of hyperglycemia and functional outcome in patients with acute ischemic stroke: the SHINE randomized clinical trial. JAMA 2019; 322: 326–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tsivgoulis G, Katsanos AH, Mavridis D, et al. Association of baseline hyperglycemia with outcomes of patients with and without diabetes with acute ischemic stroke treated with intravenous thrombolysis: a propensity score-matched analysis from the SITS-ISTR registry. Diabetes 2019; 68: 1861–1869. [DOI] [PubMed] [Google Scholar]
- 149.Hacke W, Lichy C. Thrombolysis for acute stroke under antiplatelet therapy: safe enough to be beneficial? Nat Clin Pract Neurol 2008; 4: 474–475. [DOI] [PubMed] [Google Scholar]
- 150.Pan X, Zhu Y, Zheng D, et al. Prior antiplatelet agent use and outcomes after intravenous thrombolysis with recombinant tissue plasminogen activator in acute ischemic stroke: a meta-analysis of cohort studies and randomized controlled trials. Int J Stroke 2015; 10: 317–323. [DOI] [PubMed] [Google Scholar]
- 151.Luo S, Zhuang M, Zeng W, et al. Intravenous thrombolysis for acute ischemic stroke in patients receiving antiplatelet therapy: a systematic review and meta-analysis of 19 studies. J Am Heart Assoc 2016; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tsivgoulis G, Katsanos AH, Zand R, et al. Antiplatelet pretreatment and outcomes in intravenous thrombolysis for stroke: a systematic review and meta-analysis. J Neurol 2017; 264: 1227–1235. [DOI] [PubMed] [Google Scholar]
- 153.Cucchiara B, Kasner SE, Tanne D, et al. Factors associated with intracerebral hemorrhage after thrombolytic therapy for ischemic stroke: pooled analysis of placebo data from the Stroke-Acute ischemic NXY treatment (SAINT) I and SAINT II trials. Stroke 2009; 40: 3067–3072. [DOI] [PubMed] [Google Scholar]
- 154.Tsivgoulis G, Katsanos AH, Mavridis D, et al. Intravenous thrombolysis for ischemic stroke patients on dual antiplatelets. Ann Neurol 2018; 84: 89–97. [DOI] [PubMed] [Google Scholar]
- 155.Tsivgoulis G, Goyal N, Kerro A, et al. Dual antiplatelet therapy pretreatment in IV thrombolysis for acute ischemic stroke. Neurology 2018; 91: e1067–e1076. [DOI] [PubMed] [Google Scholar]
- 156.Malhotra K, Katsanos AH, Goyal N, et al. Safety and efficacy of dual antiplatelet pretreatment in patients with ischemic stroke treated with IV thrombolysis: a systematic review and meta-analysis. Neurology 2020; 94: e657–e666. [DOI] [PubMed] [Google Scholar]
- 157.Gensicke H, Al Sultan AS, Strbian D, et al.; Thrombolysis in Stroke Patients (TRISP) Collaborators. Intravenous thrombolysis and platelet count. Neurology 2018; 90: e690–e697. [DOI] [PubMed] [Google Scholar]
- 158.Mazya MV, Lees KR, Markus R, et al.; Safe Implementation of Thrombolysis in Stroke Investigators. Safety of intravenous thrombolysis for ischemic stroke in patients treated with warfarin. Ann Neurol 2013; 74: 266–274. [DOI] [PubMed] [Google Scholar]
- 159.Xian Y, Liang L, Smith EE, et al. Risks of intracranial hemorrhage among patients with acute ischemic stroke receiving warfarin and treated with intravenous tissue plasminogen activator. JAMA 2012; 307: 2600–2608. [DOI] [PubMed] [Google Scholar]
- 160.Rubiera M, Ribo M, Santamarina E, et al. Is it time to reassess the SITS-MOST criteria for thrombolysis?: a comparison of patients with and without SITS-MOST exclusion criteria. Stroke 2009; 40: 2568–2571. [DOI] [PubMed] [Google Scholar]
- 161.Mazya M, Egido JA, Ford GA, et al.; SITS Investigators. Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: safe implementation of treatments in stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke 2012; 43: 1524–1531. [DOI] [PubMed] [Google Scholar]
- 162.Frey JL, Tsivgoulis G, Janhke HK, et al. Intravenous thrombolysis in anticoagulated patients with high INR. Neurology 2007; Suppl 1: A32. [Google Scholar]
- 163.Jalini S, Jin AY, Taylor SW. Reversal of warfarin anticoagulation with prothrombin complex concentrate before thrombolysis for acute stroke. Cerebrovasc Dis 2012; 33: 597. [DOI] [PubMed] [Google Scholar]
- 164.Chausson N, Soumah D, Aghasaryan M, et al. Reversal of vitamin K antagonist therapy before thrombolysis for acute ischemic stroke. Stroke 2018; 49: 2526–2528. [DOI] [PubMed] [Google Scholar]
- 165.Toyoda K, Yamagami H, Koga M. Consensus guides on stroke thrombolysis for anticoagulated patients from Japan: application to other populations. J Stroke 2018; 20: 321–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Pandhi A, Tsivgoulis G, Ishfaq MF, et al. Mechanical thrombectomy outcomes in large vessel stroke with high international normalized ratio. J Neurol Sci 2019; 396: 193–198. [DOI] [PubMed] [Google Scholar]
- 167.Mundiyanapurath S, Tillmann A, Mohlenbruch MA, et al. Endovascular stroke therapy may be safe in patients with elevated international normalized ratio. J Neurointerv Surg 2017; 9: 1187–1190. [DOI] [PubMed] [Google Scholar]
- 168.Goldhoorn RB, Van de Graaf RA, Van Rees JM, et al.; MR CLEAN Registry Investigators—Group Authors. Endovascular treatment for acute ischemic stroke in patients on oral anticoagulants: results from the MR CLEAN registry. Stroke 2020; 51: 1781–1789. [DOI] [PubMed] [Google Scholar]
- 169.Seiffge DJ, Hooff RJ, Nolte CH, et al. Recanalization therapies in acute ischemic stroke patients: impact of prior treatment with novel oral anticoagulants on bleeding complications and outcome. Circulation 2015; 132: 1261–1269. [DOI] [PubMed] [Google Scholar]
- 170.Xian Y, Federspiel JJ, Hernandez AF, et al. Use of intravenous recombinant tissue plasminogen activator in patients with acute ischemic stroke who take non-vitamin K antagonist oral anticoagulants before stroke. Circulation 2017; 135: 1024–1035. [DOI] [PubMed] [Google Scholar]
- 171.Shahjouei S, Tsivgoulis G, Goyal N, et al. Safety of intravenous thrombolysis among patients taking direct oral anticoagulants: a systematic review and meta-analysis. Stroke 2020; 51: 533–541. [DOI] [PubMed] [Google Scholar]
- 172.Diener HC, Bernstein R, Butcher K, et al. Thrombolysis and thrombectomy in patients treated with dabigatran with acute ischemic stroke: expert opinion. Int J Stroke 2017; 12: 9–12. [DOI] [PubMed] [Google Scholar]
- 173.Touze E, Gruel Y, Gouin-Thibault I, et al. Intravenous thrombolysis for acute ischaemic stroke in patients on direct oral anticoagulants. Eur J Neurol 2018; 25: e747–e752. [DOI] [PubMed] [Google Scholar]
- 174.Seiffge DJ, Traenka C, Polymeris AA, et al. Intravenous thrombolysis in patients with stroke taking rivaroxaban using drug specific plasma levels: experience with a standard operation procedure in clinical practice. J Stroke 2017; 19: 347–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tsivgoulis G, Safouris A. Intravenous thrombolysis in acute ischemic stroke patients pretreated with non-vitamin K antagonist oral anticoagulants: an editorial review. Stroke 2017; 48: 2031–2033. [DOI] [PubMed] [Google Scholar]
- 176.Zhao H, Coote S, Pesavento L, et al. Prehospital idarucizumab prior to intravenous thrombolysis in a mobile stroke unit. Int J Stroke 2019; 14: 265–269. [DOI] [PubMed] [Google Scholar]
- 177.Kermer P, Eschenfelder CC, Diener HC, et al. Antagonizing dabigatran by idarucizumab in cases of ischemic stroke or intracranial hemorrhage in Germany – updated series of 120 cases. Int J Stroke 2020; 15: 609–618. [DOI] [PubMed] [Google Scholar]
- 178.Giannandrea D, Caponi C, Mengoni A, et al. Intravenous thrombolysis in stroke after dabigatran reversal with idarucizumab: case series and systematic review. J Neurol Neurosurg Psychiatry 2019; 90: 619–623. [DOI] [PubMed] [Google Scholar]
- 179.Barber PA, Wu TY, Ranta A. Stroke reperfusion therapy following dabigatran reversal with idarucizumab in a national cohort. Neurology 2020; 94: e1968–e1972. [DOI] [PubMed] [Google Scholar]
- 180.Purrucker JC, Wolf M, Haas K, et al. Safety of endovascular thrombectomy in patients receiving non-vitamin K antagonist oral anticoagulants. Stroke 2016; 47: 1127–1130. [DOI] [PubMed] [Google Scholar]
- 181.Connolly SJ, Crowther M, Eikelboom JW, et al.; ANNEXA-4 Investigators. Full study report of Andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med 2019; 380: 1326–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Cuker A, Burnett A, Triller D, et al. Reversal of direct oral anticoagulants: guidance from the anticoagulation forum. Am J Hematol 2019; 94: 697–709. [DOI] [PubMed] [Google Scholar]
- 183.Idarucizumab prescribing information, https://docs.boehringeringelheim.com/Prescribing%20Information/PIs/Praxbind/Praxbind.pdf (accessed 21 August 2020).
- 184.Andexanet alfa prescribing information, www.ema.europa.eu/en/documents/product-information/ondexxya-epar-product-information_en.pdf (accessed 21 August 2020).
- 185.Andexxa package insert, www.fda.gov/media/113279/download (accessed 21 August 2020).
- 186.Breuer L, Huttner HB, Kiphuth IC, et al. Waiting for platelet counts causes unsubstantiated delay of thrombolysis therapy. Eur Neurol 2013; 69: 317–320. [DOI] [PubMed] [Google Scholar]
- 187.Brunner F, Tomandl B, Schroter A, et al. Hemorrhagic complications after systemic thrombolysis in acute stroke patients with abnormal baseline coagulation. Eur J Neurol 2011; 18: 1407–1411. [DOI] [PubMed] [Google Scholar]
- 188.Mowla A, Kamal H, Lail NS, et al. Intravenous thrombolysis for acute ischemic stroke in patients with thrombocytopenia. J Stroke Cerebrovasc Dis 2017; 26: 1414–1418. [DOI] [PubMed] [Google Scholar]
- 189.Kvistad CE, Logallo N, Thomassen L, et al. Safety of off-label stroke treatment with tissue plasminogen activator. Acta Neurol Scand 2013; 128: 48–53. [DOI] [PubMed] [Google Scholar]
- 190.Cucchiara BL, Jackson B, Weiner M, et al. Usefulness of checking platelet count before thrombolysis in acute ischemic stroke. Stroke 2007; 38: 1639–1640. [DOI] [PubMed] [Google Scholar]
- 191.Rost NS, Masrur S, Pervez MA, et al. Unsuspected coagulopathy rarely prevents IV thrombolysis in acute ischemic stroke. Neurology 2009; 73: 1957–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.European licence for Alteplase, www.ema.europa.eu/en/medicines/human/referrals/actilyse (accessed 21 August 2020).
- 193.Aleu A, Mellado P, Lichy C, et al. Hemorrhagic complications after off-label thrombolysis for ischemic stroke. Stroke 2007; 38: 417–422. [DOI] [PubMed] [Google Scholar]
- 194.Guillan M, Alonso-Canovas A, Garcia-Caldentey J, et al. Off-label intravenous thrombolysis in acute stroke. Eur J Neurol 2012; 19: 390–394. [DOI] [PubMed] [Google Scholar]
- 195.Voelkel N, Hubert ND, Backhaus R, et al. Thrombolysis in postoperative stroke. Stroke 2017; 48: 3034–3039. [DOI] [PubMed] [Google Scholar]
- 196.Meretoja A, Putaala J, Tatlisumak T, et al. Off-label thrombolysis is not associated with poor outcome in patients with stroke. Stroke 2010; 41: 1450–1458. [DOI] [PubMed] [Google Scholar]
- 197.Zand R, Tsivgoulis G, Sadighi A, et al. Safety of intravenous thrombolysis in chronic intracranial hemorrhage: a five-year multicenter study. J Stroke Cerebrovasc Dis 2018; 27: 620–624. [DOI] [PubMed] [Google Scholar]
- 198.Buchan AM, Barber PA, Newcommon N, et al. Effectiveness of t-PA in acute ischemic stroke: outcome relates to appropriateness. Neurology 2000; 54: 679–684. [DOI] [PubMed] [Google Scholar]
- 199.Tsivgoulis G, Zand R, Katsanos AH, et al. Risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis in patients with acute ischemic stroke and high cerebral microbleed burden: a meta-analysis. JAMA Neurol 2016; 73: 675–683. [DOI] [PubMed] [Google Scholar]
- 200.Charidimou A, Turc G, Oppenheim C, et al. Microbleeds, cerebral hemorrhage, and functional outcome after stroke thrombolysis. Stroke 2017; 48: 2084–2090. [DOI] [PubMed] [Google Scholar]
- 201.Greenberg SM, Vernooij MW, Cordonnier C, et al.; Microbleed Study Group. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 2009; 8: 165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Schlemm L, Endres M, Werring DJ, et al. Benefit of intravenous thrombolysis in acute ischemic stroke patients with high cerebral microbleed burden. Stroke 2020; 51: 232–239. [DOI] [PubMed] [Google Scholar]
- 203.Charidimou A, Pasi M, Fiorelli M, et al. Leukoaraiosis, cerebral hemorrhage, and outcome after intravenous thrombolysis for acute ischemic stroke: a meta-analysis (v1). Stroke 2016; 47: 2364–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ryu WS, Woo SH, Schellingerhout D, et al. Stroke outcomes are worse with larger leukoaraiosis volumes. Brain 2017; 140: 158–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Curtze S, Putaala J, Sibolt G, et al. Cerebral white matter lesions and post-thrombolytic remote parenchymal hemorrhage. Ann Neurol 2016; 80: 593–599. [DOI] [PubMed] [Google Scholar]
- 206.Chen Y, Yan S, Xu M, et al. More extensive white matter hyperintensity is linked with higher risk of remote intracerebral hemorrhage after intravenous thrombolysis. Eur J Neurol 2018; 25: 380–e315. [DOI] [PubMed] [Google Scholar]
- 207.Goyal N, Tsivgoulis G, Zand R, et al. Systemic thrombolysis in acute ischemic stroke patients with unruptured intracranial aneurysms. Neurology 2015; 85: 1452–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Karlinski M, Kobayashi A, Czlonkowska A, et al.; Safe Implementation of Treatments in Stroke–East Registry (SITS-EAST) Investigators. Intravenous thrombolysis for stroke recurring within 3 months from the previous event. Stroke 2015; 46: 3184–3189. [DOI] [PubMed] [Google Scholar]
- 209.Cappellari M, Moretto G, Micheletti N, et al. Off-label thrombolysis versus full adherence to the current European alteplase license: impact on early clinical outcomes after acute ischemic stroke. J Thromb Thrombolysis 2014; 37: 549–556. [DOI] [PubMed] [Google Scholar]
- 210.Heldner MR, Mattle HP, Jung S, et al. Thrombolysis in patients with prior stroke within the last 3 months. Eur J Neurol 2014; 21: 1493–1499. [DOI] [PubMed] [Google Scholar]
- 211.Chi MS, Chan LY. Thrombolytic therapy in acute ischemic stroke in patients not fulfilling conventional criteria. Neurologist 2017; 22: 219–226. [DOI] [PubMed] [Google Scholar]
- 212.Merkler AE, Salehi Omran S, Gialdini G, et al. Safety outcomes after thrombolysis for acute ischemic stroke in patients with recent stroke. Stroke 2017; 48: 2282–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Tsivgoulis G, Katsanos AH, Schellinger PD, et al. Intravenous thrombolysis in patients with acute ischaemic stroke with history of prior ischaemic stroke within 3 months. J Neurol Neurosurg Psychiatry 2019; 90: 1383–1385. [DOI] [PubMed] [Google Scholar]
- 214.Zinkstok SM, Engelter ST, Gensicke H, et al. Safety of thrombolysis in stroke mimics: results from a multicenter cohort study. Stroke 2013; 44: 1080–1084. [DOI] [PubMed] [Google Scholar]
- 215.Tsivgoulis G, Zand R, Katsanos AH, et al. Safety of intravenous thrombolysis in stroke mimics: prospective 5-year study and comprehensive meta-analysis. Stroke 2015; 46: 1281–1287. [DOI] [PubMed] [Google Scholar]
- 216.Polymeris AA, Curtze S, Erdur H, et al.; TRISP Collaborators. Intravenous thrombolysis for suspected ischemic stroke with seizure at onset. Ann Neurol 2019; 86: 770–779. [DOI] [PubMed] [Google Scholar]
- 217.Vilela P. Acute stroke differential diagnosis: stroke mimics. Eur J Radiol 2017; 96: 133–144. [DOI] [PubMed] [Google Scholar]
- 218.Siegler JE, Rosenberg J, Cristancho D, et al. Computed tomography perfusion in stroke mimics. Int J Stroke 2020; 15: 299–307. [DOI] [PubMed] [Google Scholar]
- 219.Kamp TJ, Goldschmidt-Clermont PJ, Brinker JA, et al. Myocardial infarction, aortic dissection, and thrombolytic therapy. Am Heart J 1994; 128: 1234–1237. [DOI] [PubMed] [Google Scholar]
- 220.Gaul C, Dietrich W, Friedrich I, et al. Neurological symptoms in type a aortic dissections. Stroke 2007; 38: 292–297. [DOI] [PubMed] [Google Scholar]
- 221.Fessler AJ, Alberts MJ. Stroke treatment with tissue plasminogen activator in the setting of aortic dissection. Neurology 2000; 54: 1010. [DOI] [PubMed] [Google Scholar]
- 222.Tsivgoulis G, Safouris A, Alexandrov AV. Safety of intravenous thrombolysis for acute ischemic stroke in specific conditions. Expert Opin Drug Saf 2015; 14: 845–864. [DOI] [PubMed] [Google Scholar]
- 223.Engelter ST, Dallongeville J, Kloss M, et al.; Cervical Artery Dissection and Ischaemic Stroke Patients (CADISP)-Study Group. Thrombolysis in cervical artery dissection – data from the cervical artery dissection and ischaemic stroke patients (CADISP) database. Eur J Neurol 2012; 19: 1199–1206. [DOI] [PubMed] [Google Scholar]
- 224.Budimkic MS, Berisavac I, Beslac-Bumbasirevic L, et al. Intravenous thrombolysis in the treatment of ischemic stroke due to spontaneous artery dissection. Neurologist 2012; 18: 273–276. [DOI] [PubMed] [Google Scholar]
- 225.Paciaroni M, Balucani C, Agnelli G, et al. Systemic thrombolysis in patients with acute ischemic stroke and internal carotid Artery occlusion: the ICARO study. Stroke 2012; 43: 125–130. [DOI] [PubMed] [Google Scholar]
- 226.Zinkstok SM, Vergouwen MD, Engelter ST, et al. Safety and functional outcome of thrombolysis in dissection-related ischemic stroke: a meta-analysis of individual patient data. Stroke 2011; 42: 2515–2520. [DOI] [PubMed] [Google Scholar]
- 227.Tsivgoulis G, Zand R, Katsanos AH, et al. Safety and outcomes of intravenous thrombolysis in dissection-related ischemic stroke: an international multicenter study and comprehensive meta-analysis of reported case series. J Neurol 2015; 262: 2135–2143. [DOI] [PubMed] [Google Scholar]
- 228.Caplan LR. Dissections of brain-supplying arteries. Nat Clin Pract Neurol 2008; 4: 34–42. [DOI] [PubMed] [Google Scholar]
- 229.Maciel R, Palma R, Sousa P, et al. Acute stroke with concomitant acute myocardial infarction: will you thrombolyse? J Stroke 2015; 17: 84–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Dhand A, Nakagawa K, Nagpal S, et al. Cardiac rupture after intravenous t-PA administration in acute ischemic stroke. Neurocrit Care 2010; 13: 261–262. [DOI] [PubMed] [Google Scholar]
- 231.Kasner SE, Villar-Cordova CE, Tong D, et al. Hemopericardium and cardiac tamponade after thrombolysis for acute ischemic stroke. Neurology 1998; 50: 1857–1859. [DOI] [PubMed] [Google Scholar]
- 232.Marto JP, Kauppila LA, Jorge C, et al. Intravenous thrombolysis for acute ischemic stroke after recent myocardial infarction: case series and systematic review. Stroke 2019; 50: 2813–2818. [DOI] [PubMed] [Google Scholar]
- 233.Inohara T, Liang L, Kosinski AS, et al. Recent myocardial infarction is associated with increased risk in older adults with acute ischemic stroke receiving thrombolytic therapy. J Am Heart Assoc 2019; 8: e012450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Ibanez B, James S, Agewall S, et al.; ESC Scientific Document Group. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the european society of cardiology (ESC). Eur Heart J 2018; 39: 119–177. [DOI] [PubMed] [Google Scholar]
- 235.Ferro JM, Fonseca AC. Infective endocarditis. Handb Clin Neurol 2014; 119: 75–91. [DOI] [PubMed] [Google Scholar]
- 236.Pruitt AA. Neurologic complications of infective endocarditis. Curr Treat Options Neurol 2013; 15: 465–476. [DOI] [PubMed] [Google Scholar]
- 237.Asaithambi G, Adil MM, Qureshi AI. Thrombolysis for ischemic stroke associated with infective endocarditis: results from the nationwide inpatient sample. Stroke 2013; 44: 2917–2919. [DOI] [PubMed] [Google Scholar]
- 238.Ong E, Mechtouff L, Bernard E, et al. Thrombolysis for stroke caused by infective endocarditis: an illustrative case and review of the literature. J Neurol 2013; 260: 1339–1342. [DOI] [PubMed] [Google Scholar]
- 239.Bhuva P, Kuo SH, Claude Hemphill J, et al. Intracranial hemorrhage following thrombolytic use for stroke caused by infective endocarditis. Neurocrit Care 2010; 12: 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Ahmed N, Audebert H, Turc G, et al. Consensus statements and recommendations from the ESO-Karolinska stroke update conference, Stockholm 11–13 November 2018. Eur Stroke J 2019; 4: 307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-eso-10.1177_2396987321989865 for European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke by Eivind Berge, William Whiteley, Heinrich Audebert, Gian Marco De Marchis, Ana Catarina Fonseca, Chiara Padiglioni, Natalia Pérez de la Ossa, Daniel Strbian, Georgios Tsivgoulis and Guillaume Turc in European Stroke Journal