Abstract
BACKGROUND
High tibial osteotomy (HTO) is a well-known procedure for the correction of knee varus. The purpose of this study was to compare the radiological results and accuracy of deformity correction performed using two different techniques: acute opening wedge correction using a plate and gradual correction with a monolateral external fixator.
AIM
To compare of the radiological results of two different techniques: acute opening wedge correction (a plate and screw) and gradual correction (external fixator).
METHODS
A total of 43 patients with plates and 36 patients with external fixators were included. All patients had moderate uniplanar varus deformities. We measured radiographic parameters, including the mechanical axis deviation (MAD), medial proximal tibial angle (MPTA), Caton-Deschamps Index (CDI), posterior proximal tibial angle, and joint line obliquity angle (JLOA). The accuracy of MAD correction was calculated based on a correction goal of neutral or overcorrection for medial compartment arthritis.
RESULTS
Demographics including age, body mass index, sex, and preoperative deformities were similar between the groups. The MAD significantly improved from 23.6 mm medial to the midline (SD = 8.2 mm) to 6.9 mm lateral to the midline (SD = 5.4 mm) (P < 0.001). The accuracy of MAD correction did not differ between the groups and was 96.1% (SD = 8.1%) in the plate group and 98.2% (SD = 5.2%) in the external fixator group (P = 0.18). The MPTA significantly improved from 83.9° (SD = 2.9°) to 90.9° (SD = 3.3°) (P < 0.001), and the change was similar between the groups. Differences were noted in patella height, with a CDI change of -19.2% (SD = 13.7%) and 3.1% (SD = 8.0%) for the plate and external fixator groups, respectively (P < 0.001). The change in JLOA was 1.6 degrees (SD = 1.1 degrees) and 0.9 degrees (SD = 0.9 degrees) for the plate and external fixator groups, respectively (P = 0.04).
CONCLUSION
Reliable correction of moderate varus alignment was achieved with both the acute opening wedge technique with a plate and the gradual monolateral external fixator technique. The patellar height decreased with the open wedge plate technique. Joint line obliquity decreased to a greater degree with the open wedge plate technique, perhaps as a result of medial collateral ligament release. The appropriate technique should be selected based on surgeon and patient preferences; however, external fixation may be a better choice when the preservation of patellar height is deemed important.
Keywords: High tibial osteotomy, External fixator, Gradual correction, Plate and screw, Genu varum, Radiological
Core Tip: Open wedge high tibial osteotomy with plate and screw fixation is feasible and an appealing operation for surgeons. Overcorrection or under correction of the deformity leads to the persistence of pain. Patellar height changes affect patients with patellofemoral injuries. With the external fixator technique, the residual deformity can be corrected after surgery, and patellar height changes can be prevented. This is a retrospective study that was conducted to compare the accuracy and radiological outcomes of monolateral external fixation and internal fixation for proximal tibial varus deformity correction.
INTRODUCTION
High tibial osteotomy (HTO) is a well-known procedure for the correction of knee deformities. This operation was introduced by Jackson in 1958 for the treatment of knee osteoarthritis (OA)[1]. In genu varum deformities, the load is transferred to the medial compartment of the knee, thus leading to the progression of medial compartment deterioration. HTO realigns the mechanical axis of the lower extremity, and this realignment decreases the load on the medial compartment and slows the progression of OA[2,3].
An abnormal biomechanical axis of the lower extremity not only causes damage to the cartilage of the knee but also affects the outcome of knee ligament reconstruction surgery. The degree of pain relief experienced after varus deformity correction depends on the accuracy of deformity correction. Inaccurate correction may cause pain to persist[4].
There are different techniques for genu varum knee deformity correction, including gradual correction with monolateral external fixation and acute opening wedge correction with internal fixation. HTO with monolateral external frame fixation is a minimal incision technique where the fibula and lateral cortex of the tibia are left intact during the osteotomy[5]. Gradual distraction of the medial cortex is performed with hinging on the intact lateral cortex, leading to realignment.
HTO with internal fixation and acute deformity correction may be performed with different approaches. Closing wedge HTO (CWHTO) and opening wedge HTO (OWHTO) are the two most well-known techniques for knee deformity correction. With OWHTO, patellar height changes can occur, which may adversely affect the patellofemoral cartilage[2,6]. Changes in the posterior tibial slope (PTS) are another possible problem of OWHTO[7-11]. Although CWHTO does not seem to affect the posterior slope, achieving an accurate correction is more difficult with CWHTO than with OWHTO, and there is an increased risk for peroneal nerve injury[12,13]. There is no consensus on which technique is superior.
In this study, we compared OWHTO with a plate to gradual correction with a monolateral fixator in a group of patients with moderate varus deformities of less than 10 degrees. In our practice, complex deformities (greater than 11 degrees or multiplanar deformities) are usually approached with a hexapod frame. The radiological outcome data included the accuracy of coronal plane realignment and the effect on patella height and posterior slope.
MATERIALS AND METHODS
This study was a retrospective, nonrandomized study (level III). The study was reviewed and approved by our institutional review board. We identified 79 consecutive patients who underwent genu varum deformity correction surgery either by internal fixation with opening wedge correction (43 patients) or a monolateral external fixator (36 patients). The inclusion criteria were patients who required less than 11 degrees of correction, patients aged 18 years or older, and patients who did not have an accompanying femoral deformity. Patients with Blount disease and those undergoing revision surgery were excluded from the study. All the surgeries were performed by the senior authors. The different approach for similar patients represents an evolution of practice with a move away from external fixation to OWHTO with a locked plate.
We used the Kellgren-Lawrence classification (KL) system for OA[14]. The severity of arthritis was graded by X-ray as follows (KL): 0, no narrowing of the joint space or reactive changes; 1, doubtful narrowing of the joint space with possible osteophyte formation; 2, possible narrowing of the joint space with definite osteophyte formation; 3, definite narrowing of the joint space, moderate osteophyte formation, some sclerosis, and possible deformity of the bony ends; and 4, large osteophyte formation, severe narrowing of the joint space with marked sclerosis, and definite deformity of bone ends.
Our goal was to correct the mechanical axis in the patients without OA (KL ≤ 2) to normal anatomical alignment and to overcorrect the axis to 10 mm valgus in the patients with OA (KL > 2)[15].
Each patient obtained a bilateral hip-to-ankle X-ray, anteroposterior (AP) view of the knee, and lateral view of the knee both before surgery and six months after surgery. mechanical axis deviation (MAD) and medial proximal tibial angle (MPTA) measurements were performed before and six months after the operation to evaluate the status of deformity correction in the coronal plane. The other radiological parameters used for the evaluation included posterior proximal tibial angle (PPTA), and joint line obliquity angle (JLOA).
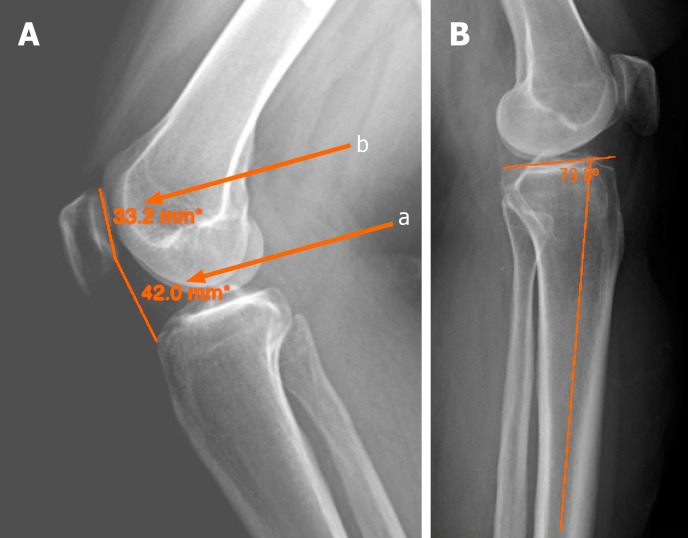
To quantify MAD, we measured the distance of the mechanical axis (center-of-hip to center-of-ankle line) from the center of the tibial plateau either laterally or medially. The lateral knee X-ray was used to measure the patellar height. We used the Caton-Deschamps Index (CDI) to evaluate the patella height before and 6 mo after the surgery (Figure 1). On the lateral view, the CDI was calculated as the distance from the upper part of the tibial plateau to the inferior pole of the patella divided by the length of the patella from the upper pole to the lower pole (Figure 1). All the measurements were performed by limb reconstruction fellowship-trained surgeons.
Figure 1.
Knee X-ray images. A: Caton-Deschamps Index (a/b) for evaluation of the patella height; B: Posterior proximal tibial angle.
We measured PPTA to evaluate the PTS in the lateral view before and 6 mo after the surgery. We drew a line from the center of the diameter of the tibia in the lateral view and a line tangent to the tibial plateau. The angle between these lines was the PTS.
Surgical technique
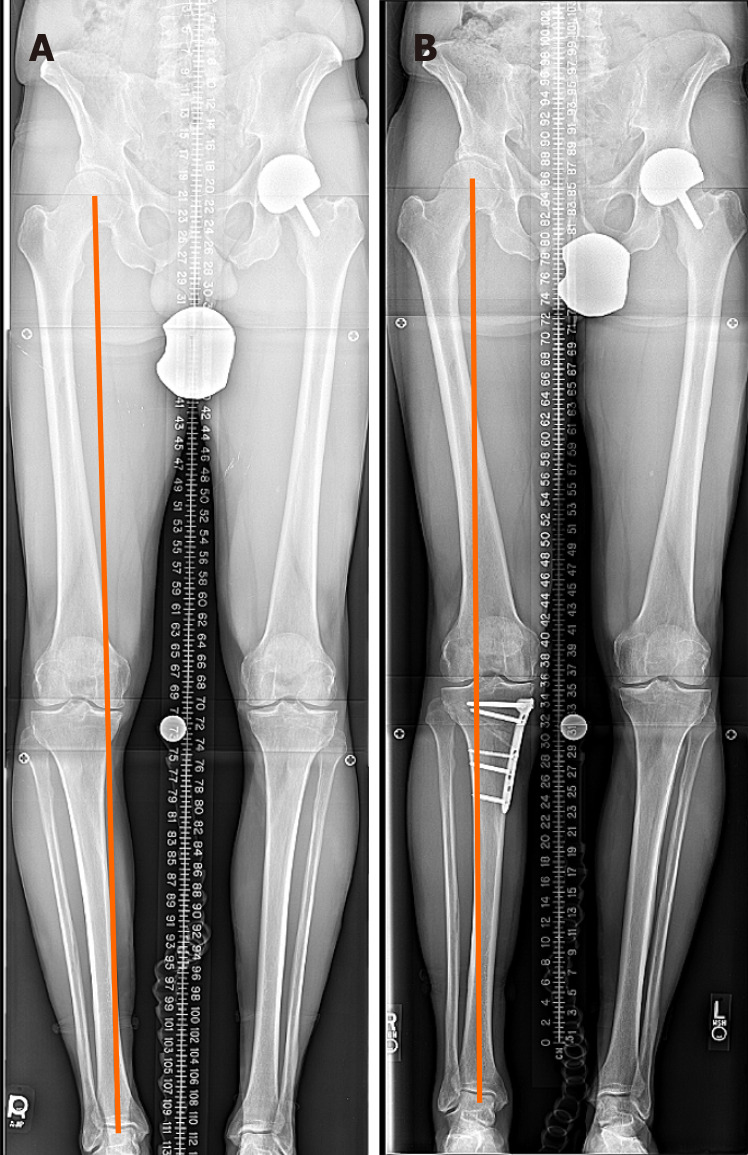
Acute genu varum deformity correction using OWHTO and plate and screw fixation was performed through an incision over the medial surface of the proximal tibia. After incising the pes anserine insertion over the tibia, the superficial fibers of the medial collateral ligament (MCL) were released from the tibia. An oblique wire was inserted from the medial cortex toward the head of the fibula 1.5 cm distal to the lateral tibial plateau. The osteotomy was done along the wire making sure to leave the lateral cortex intact. The posterior half of the osteotomy ended near the tibial tuberosity. This region was connected to the anterior half of the osteotomy, which was performed in an oblique fashion below the tibial tuberosity and continued to the anterior cortex of the proximal tibia. The lateral cortex was left intact, and the cut was stopped 1 cm medial to the lateral cortex. A laminar spreader was used in the posterior part of the osteotomy site to retract the two parts, stretching the soft tissue for several minutes and gradually opening the gap to achieve the preplanned measurement. A metal trial was inserted with a base height matching the preoperative plan. Care was taken to ensure that the opening wedge height was equal between the anterior and posterior parts to avoid unintentional flexion. The alignment of the lower extremity was confirmed during the surgery with a long rod from the hip to the ankle and C-arm fluoroscopy. A tri-cortical allograft was then inserted into the gap after the trial wedge was removed. The graft was not tapped into the osteotomy site to avoid graft fracture. The osteotomy site was then fixed with the plate and screws consisting of four 5-mm locking screws in the proximal segment and three to four locking and nonlocking 4.5- to 5-mm screws in the distal segment. The remaining space in the opening wedge was filled with freeze-dried allograft chips and demineralized bone matrix putty. In the postoperative follow-up period, the OWHTO patients were evaluated in the clinic 2 wk and 6 wk after surgery, and monthly thereafter for 6 mo after surgery (Figure 2). The patients were non weight bearing for 6 wk after surgery and then they were transferred to the partial weight bearing.
Figure 2.
High tibial osteotomy with plate and screws. A: Pre-operation; B: Post-operation.
Gradual genu varum deformity correction with a monolateral external fixator procedure was performed through a small incision over the medial surface of the tibia just below the tibial tubercle. A monolateral frame external fixator with a hinge at the osteotomy level was placed over the medial side of the tibia and connected to the bone with two half-pins proximally and three half-pins distally. The hinge was carefully oriented in the coronal plane. The fixator was positioned parallel to the tibia in the sagittal plane to avoid unintentional flexion during distraction. The 6 mm pins were made of stainless steel and covered with hydroxyapatite. An osteotomy in the tibia was made with multidirectional drilling in a direction perpendicular to the axis of the tibia. A narrow osteotome was used to complete the osteotomy at the medial side. The lateral cortex and fibula remained intact. Distraction at the osteotomy site was started 7 d after the surgery with a rate of 0.25 mm four times a day. Adjustment was evaluated by X-ray 1 wk after starting the distraction, and the distraction gap was reassessed by the senior authors. After the adjustment schedule was completed, a new hip-to-ankle X-ray was taken for the final alignment measurement. For patients with residual malalignment, a new schedule was created to continue correction; this process was continued until the intended final result was achieved.
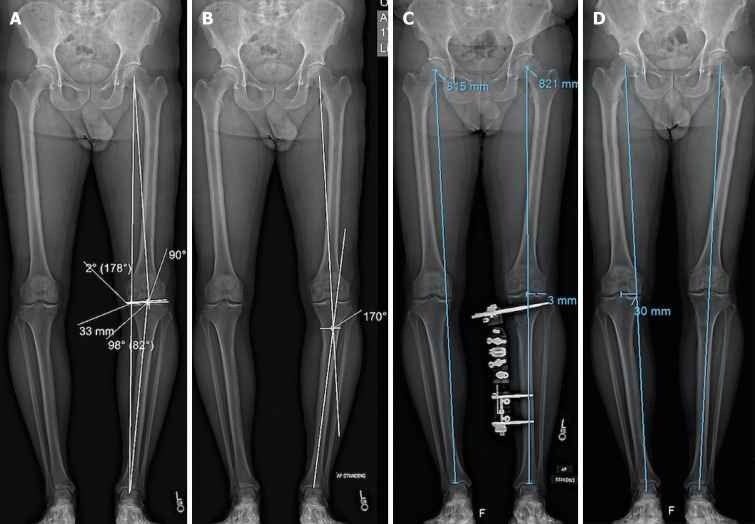
The patients were non weight bearing for 2 wk after surgery, and then transferred to the partial weight bearing. These patients were evaluated in the clinic every month until frame removal. After frame removal, they were seen 6 mo after surgery (Figure 3).
Figure 3.
High tibial osteotomy with external fixator. A and B: Before correction medial proximal tibial angle: 82, joint line obliquity angle: 2, mechanical axis deviation: 33 mm, lateral distal femoral angle: 90; C: After correction with external fixator; D: After removal of external fixator.
RESULTS
There were 43 patients in the plate and screw group and 36 patients in the external fixator group, and these groups were further subdivided based on whether the intraoperative correction goal was neutral alignment or overcorrection.
Age, body mass index, and sex were similar between the plate and external fixator groups (Table 1). We also compared the subgroups of each arm of this study as well as the subgroups within each arm (Table 2). The intra-arm comparison demonstrated several significant results, leading us to conclude that subgrouping and intergroup comparisons were appropriate.
Table 1.
Patients demographic
| Demographics |
Plate and screw (n = 43)
|
External fixator (n = 36)
|
P value | ||
|
n
|
Mean (range)
|
n
|
Mean (range)
|
||
| Age (yr) | 43 | 46.3 (19-68) | 36 | 42.1 (24-67) | 0.14 |
| BMI (kg/m2) | 39 | 26.0 (18.7-35.0) | 11 | 30.0 (20.3-39.1) | 0.08 |
| Sex (female) | 43 | 32.6% | 36 | 47.2% | 0.16 |
BMI: Body mass index.
Table 2.
Patients demographic
| Demographics |
Plate and screw (n = 43)
|
External fixator (n = 36)
|
P
value
|
|||||||||
|
N
1
(n = 25)
|
O (n = 18)
|
N (n = 23)
|
O (n = 13)
|
N vs N | O vs O | N vs O (plate and screw) | N vs O (ex fix) | |||||
|
n
|
Mean (range)
|
n
|
Mean (range)
|
n
|
Mean (range)
|
n
|
Mean (range)
|
|||||
| Age (yr) | 25 | 41.7 (19-68) | 18 | 52.7 (32-67) | 23 | 39.9 (24-55) | 13 | 46.1 (30-67) | 0.61 | 0.12 | < 0.01 | 0.11 |
| BMI (kg/m2) | 23 | 24.1 (18.7-33.5) | 16 | 28.8 (22.4-35.0) | 8 | 27.6 (20.3-39.1) | 3 | 36.4 (33.1-38.4) | 0.15 | 0.03 | < 0.001 | 0.01 |
| Sex (female) | 25 | 36.0% | 18 | 27.8% | 23 | 47.8% | 13 | 46.2% | 0.41 | 0.25 | 0.57 | 0.92 |
In this table and all subsequent ones. T: Total group; N: Neutral goal; O: Overcorrected; BMI: Body mass index.
For the MAD measurements, we included 40 patients in the plate and screw group and 36 patients in the external fixator group. In all the patients who underwent plate and screw fixation, the mechanical axis was transferred from the medial side to the lateral side. The patients who underwent external fixation were divided into two subgroups. In the external fixator group with an overcorrection goal, the mechanical axis of 1 of the 13 cases remained on the medial side. In the external fixator group with a neutral goal, the mechanical axis of all the cases shifted to the lateral side or neutral position (Table 3).
Table 3.
Mechanical axis deviation changes
| MAD |
Plate and screw
|
External fixator
|
P
value
|
|||
|
N
|
O
|
N
|
O
|
N vs N
|
O vs O
|
|
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
|
|
|
| MAD pre-op (mm) | 24.5 med (14 med to 42 med) | 25.9 med (11 med to 37 med) | 21.3 med (9 med to 42 med) | 23.0 med (11 med to 42 med) | 0.15 | 0.38 |
| MAD post-op (mm) | 4.3 lat (1 lat to 13 lat) | 12.7 lat (3 lat to 20 lat) | 3.5 (7 med to 10 lat) | 9.5 (5 med to 20 lat) | 0.40 | 0.08 |
MAD: Mechanical axis deviation; N: Neutral goal; O: Overcorrected; op: Operation.
Among all patients, the MAD significantly improved from 23.6 mm medial to the midline (SD = 8.2 mm) to 6.9 mm lateral to the midline (SD = 5.4 mm) (P < 0.001, results not shown in the table). The mean MAD before surgery in the plate and screw group with a neutral goal was 24.5 mm medially and 4.3 mm laterally after surgery (Table 3). In the plate and screw group with an overcorrected goal, the MAD was 25.9 mm medially preoperatively and 12.7 mm laterally postoperatively. For the external fixator group, the patients with a neutral goal had an average MAD of 21.3 mm medially preoperatively and 3.5 mm postoperatively (no medial vs lateral because average of absolute value). The overcorrected subgroup of patients with external fixators had 23.0 mm of medial MAD before surgery with 9.5 mm after. The results between the two groups were not significantly different.
Among all patients, the MPTA significantly improved from 83.9° (SD = 2.9°) to 90.9° (SD = 3.3°) (P < 0.001, results not shown in the table). The changes in MPTA between the plate and screw patients vs the external fixator patients were not significantly different between the subgroups (Table 4). The plate and screw patients’ MPTA increased 6.8 degrees in the neutral group compared to 5.7 degrees in the external fixator’s neutral group. For the respective overcorrected subgroups, these changes were 9.6 degrees and 6.2 degrees.
Table 4.
Medial proximal tibial angle changes
| MPTA |
Plate and screw
|
External fixator
|
P
value
|
|||
|
N
|
O
|
N
|
O
|
N vs N
|
O vs O
|
|
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
|
|
|
| ΔMPTA (degree) | 6.8 (0-13) | 9.6 (3-14) | 5.7 (2-10) | 6.2 (-4 to 15) | 0.25 | 0.05 |
MPTA: Medial proximal tibial angle; N: Neutral goal; O: Overcorrected.
To determine the accuracy of correction, we first defined the error. The error of the correction was calculated as a ratio. The acceptable range from the MAD goal was considered 5 mm. The numerator was the distance from the limits of the acceptable range: 5 mm medial to 5 mm lateral for the neutral goal and 5 mm lateral to 15 mm lateral for the overcorrected goal (15). The denominator was the difference between the MAD preoperatively and the median of the acceptable MAD range postoperatively: 0 mm in the neutral subgroup vs 10 mm lateral in the overcorrection subgroup. The accuracy for each patient was calculated by subtracting the error from 1[5,16,17].
The accuracy was quite high for every subgroup (Table 5). There were no statistically significant differences between the two arms’ respective subgroups.
Table 5.
Accuracy of mechanical axis deviation correction
| Accuracy |
Plate and screw
|
External fixator
|
P
value
|
||||||
|
T
|
N
|
O
|
Total
|
N
|
O
|
T vs T | N vs N | O vs O | |
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
Mean (range)
|
||||
| Accuracy (%) | 96.1 (60 to 100) | 94.8 (60 to 100) | 97.7 (87 to 100) | 98.2 (79 to 100) | 98.2 (82 to 100) | 98.2 (79 to 100) | 0.18 | 0.17 | 0.82 |
T: Total group; N: Neutral goal; O: Overcorrected.
The mean preoperative CDI for the patients in the plate and screw group was 1.1, and that for the patients in the external fixator group was 1.0 (Table 6). This difference was not statistically significant. The postoperative measurements were 0.9 for the plate and screw group and 1.1 for the external fixator group, which was statistically significant. The absolute changes for the two groups were a decrease of 0.2 and an increase of 0.02 respectively for the two groups, and the percent changes were a decrease of 19.2% and an increase of 3.1%. These differences were statistically significant.
Table 6.
Changes in Caton-Deschamps Index
| CDI |
Plate and screw
|
External fixator
|
P
value
|
|
Mean (range)
|
Mean (range)
|
|
|
| CDI pre-op (unitless) | 1.1 (0.7-1.6) | 1.0 (0.8-2.1) | 0.77 |
| CDI post-op (unitless) | 0.9 (0.4-1.1) | 1.1 (0.8-1.9) | 0.01 |
| ΔCDI (unitless) | -0.2 (-0.5 to 0.2) | 0.02 (-0.2 to 0.2) | < 0.001 |
| %ΔCDI (%) | -19.2 (-47.0 to 21.9) | 3.1 (-8.1 to 25.0) | < 0.001 |
CDI: Caton-Deschamps Index.
The average change of the plate and screw patients’ PPTA was a decrease of 3.3 degrees vs a mean decrease of 1.7 degrees of external fixator patients’ change in PPTA (Table 7). The percent changes were -4.1% vs -2.0%. None of these results were statistically significant.
Table 7.
Posterior proximal tibial angle changes
| PPTA |
Plate and screw
|
External fixator
|
P
value
|
|
Mean (range)
|
Mean (range)
|
|
|
| ΔPPTA (degree) | -3.3 (-9 to 1) | -1.7 (-11 to 4) | 0.14 |
| %ΔPPTA (%) | -4.1 (-11.3 to 1.3) | -2.0 (-12.8 to 5.1) | 0.11 |
PPTA: Posterior proximal tibial angle.
The mean absolute value of the change in JLOA preoperatively to postoperatively was an increase of 1.6 degrees for the plate and screw group and a 0.9 degree increase for the external fixator group (Table 8). This difference was statistically significant.
Table 8.
Joint line obliquity angle changes
| JLOA |
Plate and screw
|
External fixator
|
P
value
|
| Mean (range) | Mean (range) | ||
| ΔJLOA (degree) | 1.6 (4 med to 3 lat) | 0.9 (3 med to 2 lat) | 0.04 |
JLOA: Joint line obliquity angle.
There was a major complication in the external fixator group with one patient with loss of reduction and collapse in the regenerated bone at the osteotomy site after the removal of the external fixator. Subsequent open reduction and internal fixation with plates and screws were performed for this patient. Some of the patients in the external fixation group had discharge and superficial infections around the half-pin that were successfully treated with oral antibiotics. There were no cases of neurovascular injury, neuropraxia, nonunion, deep infection, or osteomyelitis in either group. There was no significant change in knee range of motion in either group at the last follow-up as compared to the pre-operative baseline measurement.
DISCUSSION
HTO is an appropriate procedure for genu varum deformity correction to correct MAD. The procedure alleviates pain in patients with OA of the medial compartment of the knee. In this study, we compared the results of acute correction with OWHTO to those of gradual correction with an external fixator for knee varus deformities. The reported indication for HTO surgery is varus alignment of the knee combined with any of the situations, such as medial compartment OA, medial compartment overloading (such as post medial meniscectomy), knee instability or osteochondral lesions[18].
The indications for HTO surgery in our study were a varus deformity greater than 5 degrees and knee pain. If there was radiographic medial joint space narrowing, then the goal was overcorrection. If there was no radiographic medial joint space narrowing, then the goal was neutral alignment.
Our results showed that while the re-alignment was substantial, there were not significant differences between the two groups in MAD and MPTA changes, and the accuracy of correction. The PPTA changed less in the external fixator group than the plate and screw group, but this change was not significant.
Patella baja may be a concern after OWHTO[19]. Patella baja causes anterior knee pain and crepitus[4,20]. Because of the transfer of the tibial tuberosity distally and laterally, the biomechanical axis of the patellofemoral joint changes after surgery[8]. One biomechanical study showed that OWHTO tilts the patella medially and increases the pressure over the lateral surface of the patella[21]. It has also been reported that the pressure over the patellar cartilage increases after OWHTO[6].
The literature has shown that there is a significant increase in patellofemoral joint pressure with genu varum knee deformity correction of more than five degrees[6]. Previous work has evaluated the effect of shortening the patellar height over the patellofemoral articular cartilage[7,22]. Researchers have demonstrated that shortening the patellar tendon after OWHTO accelerates the development of patellofemoral OA. Chondral lesions increased in long-term follow-up and likely causes anterior knee pain[23].
In our external fixator group, the patellar tendon height changed less than that in the plate group after surgery. The osteotomy performed in the external fixator group at the distal tibial tuberosity did not affect the patellar height. Additionally, when a varus deformity is gradually corrected, the soft tissue around the knee lengthens gradually, and the patellar tendon length does not change after varus deformity correction. For this reason, this technique may be preferred for genu varum deformity patients with OA of the patellofemoral joint. Also, the JLOA changed less in the external fixator group compared to the plate and screw group. Gradual correction of the deformity may allow the ligaments to stretch more slowly, having less of an effect on the JLOA. Additionally, the medial collateral ligament is released during the acute correction of OWHTO, which may decrease the JLOA. The clinical outcomes were similar between the two groups.
Correction of the knee genu varum deformity is important before anterior cruciate ligament (ACL) reconstruction[13]. The PTS is one of the factors that affects the outcome of ACL reconstruction. Increasing the PTS results in a transfer of the loading to the anterior part of the knee, and this overload may affect the outcome of ACL reconstruction surgery. OWHTO has been shown to increase the PTS[12,24]. Every 10-degree increase in the PTS causes a 6-mm translation of the anterior tibial load axis[4]. Our results show that there was a smaller change in the PTS in the external fixator group than in the OW group. However, the difference in PPTA change between the groups was not significant.
The results of some modifications of open wedge HTO have been reported. One study showed no differences in patellar height or PTS between an ascending vs descending OWHTO, a technique requiring leaving the tuberosity attached to the distal tibia or proximal tibia, respectively[23]. Some surgeons advise releasing the posterior soft tissue to prevent an increase in PTS[4]. Another study recommends against the release of the soft tissue and medial ligament[25]. In this biomechanical study, it was shown that cutting the anterior fiber of the MCL affects the stability of the medial side in HTO[25].
Evaluation of the changes in the MAD and MPTA in both groups showed there was no significant difference in correction of the genu varum deformity between the both groups. The accuracy of the correction was 96.1% (60%-100%) in the plate and screw group and 98.2% (79%-100%) in the external fixator group. Both techniques led to accurate genu varum deformity correction, and there was no significant difference between the two groups.
Undercorrection, or sometimes overcorrection, may compromise the outcome of genu varum deformity correction surgery[4]. Preoperative measurement planning is helpful to achieve optimal alignment correction. However, sometimes, the laxity around the knee that appears on weight-bearing X-rays is not as obvious when the patient is in the supine position intraoperatively[26]. With our external fixator technique, we have the opportunity to continually correct residual deformities after surgery, making it a helpful procedure in patients with soft tissue laxity in the knee. Additionally, because the external fixator allows gradual correction, the formation of bone is well controlled, the rate of lengthening can be adjusted, and nonunion or malunion can be prevented[16,17,27,28].
There are some limitations of our study. First, these operations were performed by experienced surgeons, which may affect the results of the operations and may have reduced the rate of complications after the operations. External fixator adjustments require experience and expertise; thus, these results may be hard to generalize to a large variety of practices. Second, this study is a retrospective study with a limited number of patients. As mentioned above, there were some demographic differences between some subgroups, and we evaluated the radiological outcomes of the two techniques. Future works would be helpful if they evaluate these results in a larger number of patients. Third, this study was a radiological comparison of the two techniques, and a study comparing the early and late clinical outcomes in both groups in a larger number of patients would be helpful to determine the clinical performance of these techniques. Fourth, our patients were confined to those with varus deformities of less than ten degrees. We suggest future studies evaluating patients with larger-degree varus deformity corrections.
CONCLUSION
Reliable degrees of correction of moderate varus alignment were achieved with both the acute opening wedge technique with a plate and the gradual monolateral external fixator technique in patients undergoing HTOs. The appropriate technique should be selected on the basis of the surgeon and patient preferences; however, external fixation may be a better choice when maintenance of patellar height is deemed important.
ARTICLE HIGHLIGHTS
Research background
High tibial osteotomy (HTO) for the correction of painful varus knee deformities is a known surgery. Different HTO techniques have been reported in the literature, including open and closed wedge osteotomies. In this study, the radiological efficacy of the gradual and acute correction of varus deformities with two different fixation methods (external fixator and plate screw) was evaluated.
Research motivation
We aimed to compare the radiological accuracy of the gradual correction of varus deformities with HTO with an external fixator and that of acute correction with a plate and screw.
Research objectives
The changes in radiological parameters (mechanical axis deviation, medial proximal tibial angle, posterior proximal tibial angle, joint line obliquity angle, Caton-Deschamps Index) were evaluated after both acute and gradual correction to determine the accuracy of correction achieved with the two techniques.
Research methods
Retrospective, nonrandomized study (level III).
Research results
Both acute correction (opening wedge and plate and screw) and gradual correction (external fixator) yield reliable degrees of correction of moderate varus alignment. The changes in the radiological parameters achieved with and accuracy of the two techniques are reasonable. There were changes in the patellar height after acute correction with a plate and screw.
Research conclusions
Both techniques (HTO with plate and screw and external fixator) are reliable for the correction of varus deformities, and external fixation may be a better choice when the preservation of patellar height is important.
Research perspectives
Studies with a larger number of patients and evaluations of the early and late clinical outcomes of both techniques are suggested.
Footnotes
Institutional review board statement: The study was reviewed and approved by Hospital for Special Surgery Institutional Review Board.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: None of the authors has any conflict directly relating to the subject of study. Unrelated disclosures: Dr. Fragomen A is a consultant for Smith & Nephew, NuVasive and Synthes. Dr. Rozbruch SR is a consultant for NuVasive, Stryker, Smith & Nephew and Orthospin.
Manuscript source: Unsolicited manuscript
Peer-review started: May 23, 2020
First decision: October 6, 2020
Article in press: February 11, 2021
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Leung PC, Płaszewski M, Prudhon JL S-Editor: Gao CC L-Editor: A P-Editor: Yuan YY
Contributor Information
S Ali Ghasemi, Department of Orthopedic Surgery, Hospital for Special Surgery, Weill Medical College of Cornell University, New York, NY 10021, United States. ghasemisar2@gmail.com.
David T Zhang, Department of Orthopedic Surgery, Hospital for Special Surgery, Weill Medical College of Cornell University, New York, NY 10021, United States.
Austin Fragomen, Department of Orthopedic Surgery, Hospital for Special Surgery, Weill Medical College of Cornell University, New York, NY 10021, United States.
S Robert Rozbruch, Department of Orthopedic Surgery, Hospital for Special Surgery, Weill Medical College of Cornell University, New York, NY 10021, United States.
Data sharing statement
No additional data are available.
References
- 1.Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43-B:746–751. doi: 10.1302/0301-620X.43B4.746. [DOI] [PubMed] [Google Scholar]
- 2.Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852–861. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 3.Coventry MB. Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1985;67:1136–1140. [PubMed] [Google Scholar]
- 4.Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20:366–372. doi: 10.1016/j.arthro.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Ashfaq K, Fragomen AT, Nguyen JT, Rozbruch SR. Correction of proximal tibia varus with external fixation. J Knee Surg. 2012;25:375–384. doi: 10.1055/s-0031-1299659. [DOI] [PubMed] [Google Scholar]
- 6.Kloos F, Becher C, Fleischer B, Feucht MJ, Hohloch L, Südkamp N, Niemeyer P, Bode G. High tibial osteotomy increases patellofemoral pressure if adverted proximal, while open-wedge HTO with distal biplanar osteotomy discharges the patellofemoral joint: different open-wedge high tibial osteotomies compared to an extra-articular unloading device. Knee Surg Sports Traumatol Arthrosc. 2019;27:2334–2344. doi: 10.1007/s00167-018-5194-x. [DOI] [PubMed] [Google Scholar]
- 7.Kim KI, Kim DK, Song SJ, Lee SH, Bae DK. Medial Open-Wedge High Tibial Osteotomy May Adversely Affect the Patellofemoral Joint. Arthroscopy. 2017;33:811–816. doi: 10.1016/j.arthro.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 8.Bito H, Takeuchi R, Kumagai K, Aratake M, Saito I, Hayashi R, Sasaki Y, Saito T. Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg Sports Traumatol Arthrosc. 2010;18:955–960. doi: 10.1007/s00167-010-1077-5. [DOI] [PubMed] [Google Scholar]
- 9.Tigani D, Ferrari D, Trentani P, Barbanti-Brodano G, Trentani F. Patellar height after high tibial osteotomy. Int Orthop. 2001;24:331–334. doi: 10.1007/s002640000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaper BP, Bourne RB, Rorabeck CH, Macdonald SJ. Patellar infera after high tibial osteotomy. J Arthroplasty. 2001;16:168–173. doi: 10.1054/arth.2001.20538. [DOI] [PubMed] [Google Scholar]
- 11.Otsuki S, Murakami T, Okamoto Y, Nakagawa K, Okuno N, Wakama H, Neo M. Risk of patella baja after opening-wedge high tibial osteotomy. J Orthop Surg (Hong Kong) 2018;26:2309499018802484. doi: 10.1177/2309499018802484. [DOI] [PubMed] [Google Scholar]
- 12.Bombaci H, Canbora K, Onur G, Görgeç M. [The effect of open wedge osteotomy on the posterior tibial slope] Acta Orthop Traumatol Turc. 2005;39:404–410. [PubMed] [Google Scholar]
- 13.Cantin O, Magnussen RA, Corbi F, Servien E, Neyret P, Lustig S. The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3026–3037. doi: 10.1007/s00167-015-3752-z. [DOI] [PubMed] [Google Scholar]
- 14.Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paley D. Normal Lower Limb Alignment and Joint Orientation. In: Principles of Deformity Correction. Berlin: Springer, 2002: 1-18. [Google Scholar]
- 16.Khakharia S, Bigman D, Fragomen AT, Pavlov H, Rozbruch SR. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2011;469:244–250. doi: 10.1007/s11999-010-1460-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elattar O, Swarup I, Lam A, Nguyen J, Fragomen A, Rozbruch SR. Open Wedge Distal Femoral Osteotomy: Accuracy of Correction and Patient Outcomes. HSS J. 2017;13:128–135. doi: 10.1007/s11420-016-9516-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonasia DE, Dettoni F, Sito G, Blonna D, Marmotti A, Bruzzone M, Castoldi F, Rossi R. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med. 2014;42:690–698. doi: 10.1177/0363546513516577. [DOI] [PubMed] [Google Scholar]
- 19.LaPrade RF, Oro FB, Ziegler CG, Wijdicks CA, Walsh MP. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med. 2010;38:160–170. doi: 10.1177/0363546509342701. [DOI] [PubMed] [Google Scholar]
- 20.Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87:1227–1232. doi: 10.1302/0301-620X.87B9.15972. [DOI] [PubMed] [Google Scholar]
- 21.Gaasbeek R, Welsing R, Barink M, Verdonschot N, van Kampen A. The influence of open and closed high tibial osteotomy on dynamic patellar tracking: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2007;15:978–984. doi: 10.1007/s00167-007-0305-0. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka T, Matsushita T, Miyaji N, Ibaraki K, Nishida K, Oka S, Araki D, Kanzaki N, Hoshino Y, Matsumoto T, Kuroda R. Deterioration of patellofemoral cartilage status after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019;27:1347–1354. doi: 10.1007/s00167-018-5128-7. [DOI] [PubMed] [Google Scholar]
- 23.Krause M, Drenck TC, Korthaus A, Preiss A, Frosch KH, Akoto R. Patella height is not altered by descending medial open-wedge high tibial osteotomy (HTO) compared to ascending HTO. Knee Surg Sports Traumatol Arthrosc. 2018;26:1859–1866. doi: 10.1007/s00167-017-4548-0. [DOI] [PubMed] [Google Scholar]
- 24.Black MS, d'Entremont AG, McCormack RG, Hansen G, Carr D, Wilson DR. The effect of wedge and tibial slope angles on knee contact pressure and kinematics following medial opening-wedge high tibial osteotomy. Clin Biomech (Bristol, Avon) 2018;51:17–25. doi: 10.1016/j.clinbiomech.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 25.Pape D, Duchow J, Rupp S, Seil R, Kohn D. Partial release of the superficial medial collateral ligament for open-wedge high tibial osteotomy. A human cadaver study evaluating medial joint opening by stress radiography. Knee Surg Sports Traumatol Arthrosc. 2006;14:141–148. doi: 10.1007/s00167-005-0649-2. [DOI] [PubMed] [Google Scholar]
- 26.Buckland-Wright C. Which radiographic techniques should we use for research and clinical practice? Best Pract Res Clin Rheumatol. 2006;20:39–55. doi: 10.1016/j.berh.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26:794–798. doi: 10.1097/01.bpo.0000242375.64854.3d. [DOI] [PubMed] [Google Scholar]
- 28.Ogata K, Yoshii I, Kawamura H, Miura H, Arizono T, Sugioka Y. Standing radiographs cannot determine the correction in high tibial osteotomy. J Bone Joint Surg Br. 1991;73:927–931. doi: 10.1302/0301-620X.73B6.1955438. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.