Abstract
Purpose
The purpose of this study was to evaluate the feasibility of assessing quantitative longitudinal fluid dynamics and total retinal fluid indices (TRFIs) with higher-order optical coherence tomography (OCT) for neovascular age-related macular degeneration (nAMD).
Methods
A post hoc image analysis study was performed using the phase II OSPREY clinical trial comparing brolucizumab and aflibercept in nAMD. Higher-order OCT analysis using a machine learning−enabled fluid feature extraction platform was used to segment intraretinal fluid (IRF) and subretinal fluid (SRF) volumetric components. TRFI, the proportion of fluid volume against total retinal volume, was calculated. Longitudinal fluid metrics were evaluated for the following groups: all subjects (i.e. treatment agnostic), brolucizumab, and aflibercept.
Results
Mean IRF and SRF volumes were significantly reduced from baseline at each timepoint for all groups. Fluid feature extraction allowed high-resolution assessment of quantitative fluid burden. A greater proportion of brolucizumab participants achieved true zero and minimal fluid (total fluid volume between 0.0001 and 0.001mm3) versus aflibercept participants at week 40. True zero fluid during q12 brolucizumab dosing was achieved in 36.6% to 38.5%, similar to the 25.6% to 38.5% during the corresponding q8 aflibercept cycles. TRFI was significantly reduced from baseline in all groups.
Conclusions
Higher-order OCT analysis demonstrates the feasibility of fluid feature extraction and longitudinal volumetric fluid burden and TRFI characterization in nAMD, supporting a unique opportunity for fluid burden assessment and the impact on outcomes.
Translational Relevance
Detection and characterization of disease activity is vital for optimal treatment of nAMD. Longitudinal assessment of fluid dynamics and the TRFI provide important proof of concept for future automated tools in characterizing disease activity.
Keywords: optical coherence tomography (OCT), fluid feature extraction, retinal fluid index, wet age-related macular degeneration (AMD)
Introduction
Neovascular age-related macular degeneration (nAMD) remains a leading cause of significant vision loss.1,2 Improving or maintaining visual acuity is the primary goal of nAMD treatment, and stabilization of the neovascular process through the use of vascular endothelial growth factor (VEGF) inhibitor agents is the gold-standard approach to managing nAMD.2,3 Although visual acuity improvement/maintenance is the functional goal, in clinical trials and in clinical practice, efficacy of a given anti-VEGF agent has been traditionally represented as reduction in the central subfield thickness (CST) of the entire retina or by resolution of retinal fluid (i.e. intraretinal fluid [IRF] and subretinal fluid [SRF]) as an anatomic surrogate of exudative activity.1,2,4 Retinal fluid is generally evaluated in a binary fashion (e.g. presence/absence) using optical coherence tomography (OCT); and in particular with spectral domain OCT (SD-OCT).2,5
Although anti-VEGF agents have vastly improved outcomes and OCT subjective interpretation allows physicians to provide individualized care, long-term studies demonstrate less favorable visual outcomes over time in real-world studies, most likely due to undertreatment over time.5–7 One key reason for undertreatment includes not recognizing underlying fluid activity. Next-generation computational image analysis techniques, including higher-order OCT analysis, enable in-depth assessment of fluid burden features through extraction of fluid compartments and characterization of IRF and SRF volumes throughout the macular OCT scans.8–15 These higher-order segmentation features enable evaluation of additional anatomic biomarkers, such as the total retinal fluid index (i.e. volumetric fluid burden/total retinal fluid volume).8
The phase II OSPREY study compared brolucizumab, a newly developed anti-VEGF molecule for the treatment of nAMD, with aflibercept during a matched q8 dosing regimen up to week 40; it also assessed a q12 dosing regimen with brolucizumab.16 In contrast to the phase III HAWK and HARRIER studies, in which patients’ disease activity assessments were used to determine q12 or q8 dosing intervals,17 in the OSPREY study, all brolucizumab-treated participants were extended to a q12 interval, whereas the aflibercept-treated participants remained on a q8 interval.
The purpose of the current analysis was to evaluate the feasibility of assessing quantitative longitudinal fluid dynamics and retinal fluid indices with higher-order OCT for nAMD. This novel analysis utilized a prospective clinical trial data set (i.e. OSPREY nAMD study) to provide an in-depth longitudinal evaluation of the OCT-based anatomic imaging biomarkers (volumetric measurements of IRF and SRF and the total retinal fluid index).
Methods
Higher-Order OCT Analysis: Fluid Segmentation
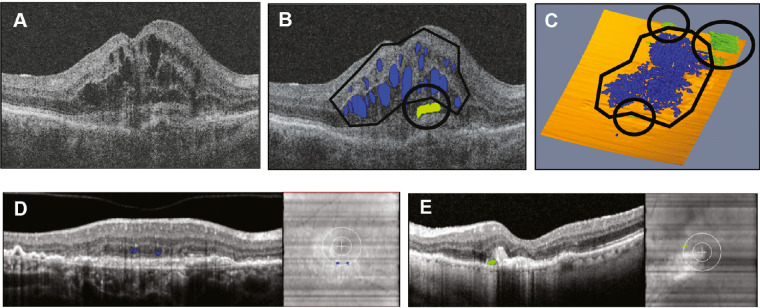
As part of the OSPREY study (see below), macular cube scans with a 512 × 128 macular cube covering a nominal 6 × 6 mm square area of the macula centered on the foveal center point using the Cirrus (Carl Zeiss Meditec; Dublin, CA), or a 49-line, high-speed, preset scan covering a 20 degrees × 20 degrees area of the macula centered on the foveal center point in high-speed mode with an ART setting of 16 using Spectralis (Heidelberg Engineering, Heidelberg, Germany) were obtained at every visit.16 These images were transferred to the Cleveland Clinic for further analysis. Utilizing a previously described OCT machine learning−augmented multilayer segmentation and feature extraction platform (i.e. OCTViewer), each macular cube was imported for higher-order OCT analysis.8–10 Each macular cube was automatically segmented for fluid boundaries as shown in Figures 1A–C.8,9 Two masked expert/trained readers conducted sequential checks of the segmentation created by the software, and segmentation errors were manually corrected, as needed.8,18 The reading environment was standardized based on location, computer configuration, monitor settings, and lighting configuration to minimize variability.8 In addition, to minimize inter-timepoint and inter-user variation, the same trained reader reviewed all timepoints of a single subject.8 Following the initial read, the project lead reviewed each scan to confirm consistency and segmentation accuracy. An en face IRF/SRF map was generated to visualize regional fluid accumulation. Fluid volume parameters were exported. Variables analyzed included macular IRF and SRF volume, proportional reduction of fluid volumes from baseline, and proportion of patients with true zero fluid and with anatomically minimal total fluid (IRF and SRF). Anatomically minimal fluid, volumetrically defined as total fluid volume between 0.0001 mm3 and 0.001 mm3 (Figs. 1D, 1E), represented fluid volumes that did not cause any readily visible anatomic disturbance and might be a marker for “real-world dry” scenarios. The proportional reduction of fluid volumes from baseline was described as stable when fluctuations between visits were not observed.
Figure 1.
Representative fluid feature extraction. (A) B-scan. (B) B-scan with intraretinal fluid (IRF; blue) and subretinal fluid (SRF; green) volume segmentation. (C) Volumetric visualization of macular IRF (blue) and SRF (green) volume of 0.59 mm3 and 0.06 mm3, respectively. (D) Anatomically minimal IRF, defined as total fluid volume between 0.0001 mm3 and 0.001 mm3. (E) Anatomically minimal SRF.
Total retinal fluid index (TRFI) was defined as follows: 100 × (IRF + SRF) / total retina + fluid compartment volume. TRFI represents a percentage of IRF and SRF volume against retinal + fluid volume in a designated area (e.g. central subfield [central 1 mm], panmacular, central macular [central 2 mm]), a number ranging between 0% (no IRF + SRF) and 100% (total IRF + SRF). TRFI takes into consideration the retinal tissue and is the percentage of space from the RPE to the internal limiting membrane made up of SRF or IRF.
OSPREY Study Design
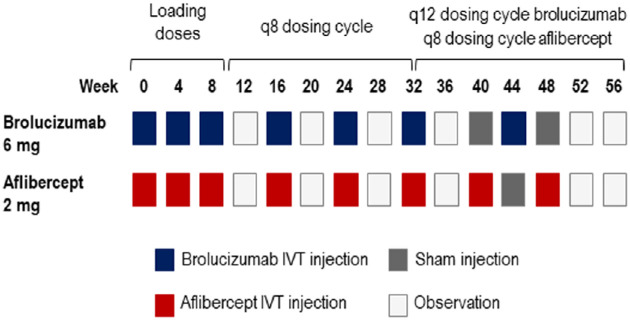
This was a post hoc exploratory analysis of the OSPREY study, in which 81 eyes (41 treated with brolucizumab and 40 treated with aflibercept) of the 89 had received treatment and OCT measures at baseline and at least one other timepoint. OSPREY was a prospective, randomized, double-masked, two-arm phase II clinical trial conducted at 41 investigational centers in the United States (ClinicalTrials.gov identifier NCT01796964). The trial protocol was approved by all institutional review boards and complied with the ethical standards defined by the Declaration of Helsinki and Good Clinical Practice. All participants provided written informed consent before participating in the study. Details of the study design have been published previously.16 Briefly, eligible participants had to be ≥ 50 years of age with untreated active choroidal neovascularization due to AMD in the study eye, with a best corrected visual acuity (BCVA) between 73 and 23 letters, inclusive. The study eye had to have SRF, IRF, or subretinal pigment epithelium (sub-RPE) fluid on SD-OCT.16 During this trial, participants were randomized 1:1 to brolucizumab 6 mg or aflibercept 2 mg. There were 3 treatment periods: the first consisted of administration of the loading doses at baseline, week 4 and week 8; the second period included a q8 dosing regimen with corresponding assessments up to week 40; and the final cycle was conducted to week 56, with all brolucizumab participants extended to allow for assessment of q12 dosing while the aflibercept group was maintained on q8 dosing (Fig. 2).16 BCVA and SD-OCT in the study eye were evaluated at all visits.16 As part of this feasibility assessment, the combined study group (treatment agnostic), the brolucizumab group, and the aflibercept group were all evaluated. This post hoc analysis of the OSPREY study was a proof of concept for automated tools to characterize disease activity. It was not powered to demonstrate how anatomic features impact functional outcomes, particularly in a 56-week study.
Figure 2.
OSPREY Study Design. Schematic representation of dosing regimen. Three treatment periods included (1) loading doses (study drug was administered at baseline and at weeks 4 and 8, with an efficacy assessment at week 12); (2) matching q8 dosing cycles for brolucizumab and aflibercept, with a corresponding assessment period at week 40 (8 weeks after the last q8 dose administration for both treatments); and (3) a nonmatched period, during which all participants in the brolucizumab group received a q12 dose at week 44 and a second q12 cycle was completed at week 56, whereas participants in the aflibercept group continued on a q8 cycle with treatments at weeks 40 and 48. Sham injections were given to both treatment groups to preserve masking during the nonmatched period.
Statistical Analysis
Statistical analyses for participant demographics and mean BCVA have been described previously.16 Statistical analysis for higher-order OCT assessment was performed using SAS (version 9.4). Treatment comparison for change from baseline was analyzed using an analysis of covariance model, with treatment as a factor and baseline as a covariate. Treatment comparisons for the percent reduction were evaluated using an analysis of variance model with treatment as a factor. To evaluate within-group differences, t-tests were applied. A χ2 test was used to evaluate the proportion of participants with true zero as well as minimal fluid. Associations were assessed using Pearson correlation coefficients. These analyses were for hypothesis generation. No adjustment was made for multiple comparisons.
Results
Participant Demographics
Participant disposition and demographics in the OSPREY study have been published previously.16 Briefly, the overall mean age of participants was 78 years and the baseline BCVA values were similar between groups, with 54.1 and 55.6 letters in the brolucizumab and aflibercept groups, respectively. CST and lesion type were similar in the two groups. At baseline, IRF was present in 86.4% and 84.4% of participants in the brolucizumab and aflibercept groups, respectively, and SRF was present in 90.9% and 88.9%, respectively.16
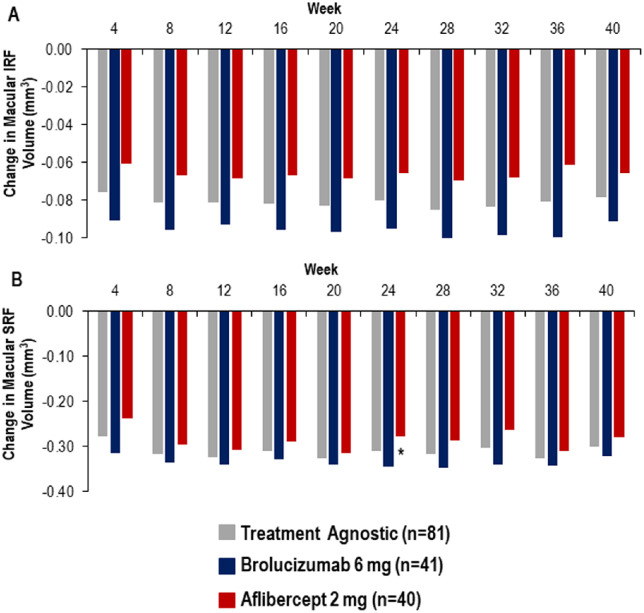
Matched-Phase Fluid Dynamics
Mean macular IRF and SRF volume reductions from baseline during the matched phase (monthly loading doses followed by q8 dosing) are shown in Figure 3. Mean IRF and SRF volume reductions were statistically significant versus baseline at each timepoint for brolucizumab and aflibercept. At each timepoint, the treatment agnostic group demonstrated IRF volume reductions from baseline that ranged from 0.076 to 0.085 mm3, whereas SRF volume reductions from baseline ranged from 0.28 to 0.33 mm3 (see Figs. 3A, 3B). For the treatment-specific groups, the reduction in mean macular IRF volume from baseline ranged from 0.091 to 0.100 mm3 at each timepoint in the brolucizumab group and from 0.061 to 0.070mm3 in the aflibercept group (see Fig. 3A). Similarly, the reduction in mean macular SRF volume from baseline ranged from 0.31 to 0.35 mm3 and from 0.24 to 0.32 mm3 in the brolucizumab and aflibercept groups, respectively (see Fig. 3B).
Figure 3.
Mean fluid reduction from baseline during matched phase. (A) Mean intraretinal fluid (IRF) reduction in treatment agnostic (gray), brolucizumab (blue), and aflibercept (red) groups. (B) Mean subretinal fluid (SRF) reduction in treatment agnostic (gray), brolucizumab (blue), and aflibercept (red) groups. *P < 0.05 brolucizumab versus aflibercept.
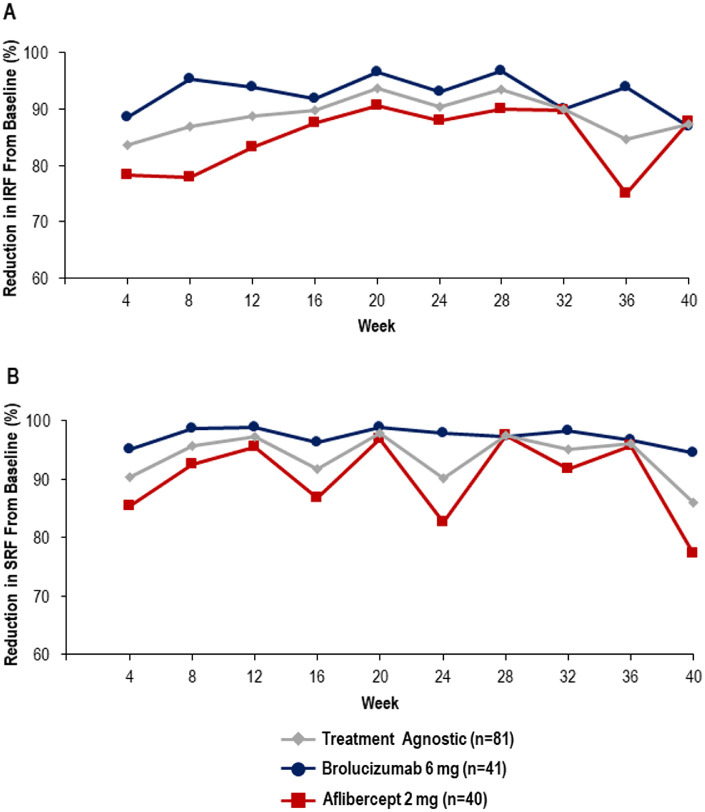
In the treatment agnostic group, baseline IRF was significantly reduced (83.6%) at week 4. Following the first q8 dosing interval (week 16), the percent reduction in IRF was 89.7% and by week 40 it was 87.3% (Fig. 4A). A similar percent reduction from baseline was observed with SRF at week 4 (90.4%), week 16 (91.7%), and week 40 (86.0%) in the treatment agnostic group (see Fig. 4B). Longitudinal analysis of IRF demonstrated generally stable reductions for both brolucizumab and aflibercept (see Fig. 4A). Similarly, the fluid feature extraction system demonstrated a stable SRF percentage reduction from baseline in the brolucizumab-treated eyes from weeks 4 to 40 on a q8 dosing interval (see Fig. 4B). In contrast, the fluid assessment identified fluctuating SRF reduction from baseline for the aflibercept-treated eyes from weeks 4 to 40, oscillating every 8 weeks.
Figure 4.
Percent reduction in fluid from baseline during matched phase. (A) Reduction in intraretinal fluid (IRF) from baseline in treatment agnostic (gray diamond), brolucizumab (blue circle), and aflibercept (red square) groups. (B) Reduction in subretinal fluid (SRF) from baseline in treatment agnostic (gray diamond), brolucizumab (blue circle), and aflibercept (red square) groups.
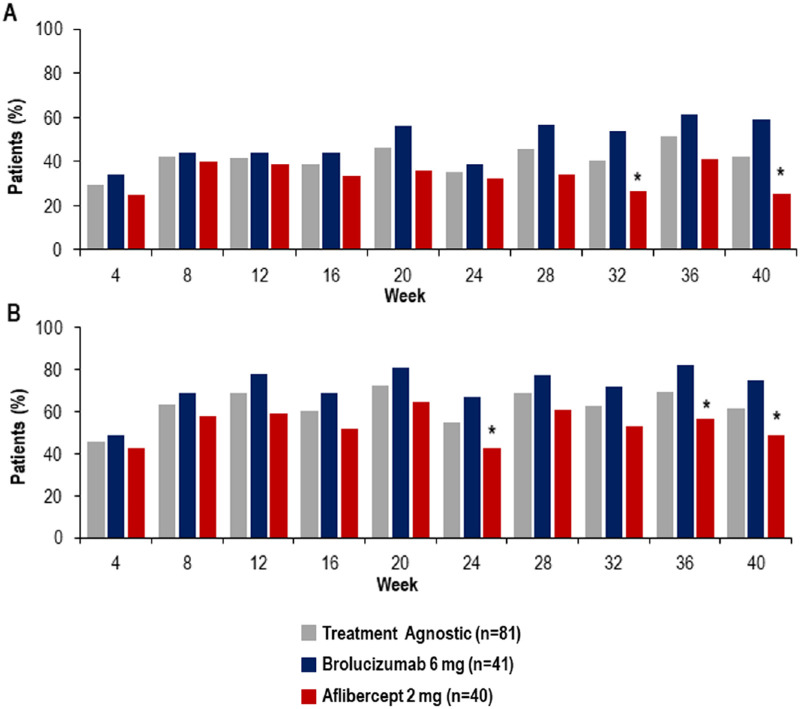
Using higher-order OCT assessment, total fluid burden was assessed by examining the percent of participants with true zero and anatomically minimal fluid. Fluid feature extraction identified true zero fluid in the treatment agnostic group in 29.6% to 51.3% of study eyes between weeks 4 and 40 (Fig. 5A). In the brolucizumab group, the proportion of participants with true zero fluid between weeks 4 and 40 ranged from 34.1% to 61.5%, and in the aflibercept group it ranged from 25.0% to 41.0%. The proportion of participants achieving true zero fluid was greater with brolucizumab than with aflibercept, with statistically significant differences at weeks 32 and 40 (see Fig. 5A). The proportion of participants with anatomically minimal fluid or less in the study eye ranged from 45.7% to 72.5% for the treatment agnostic group, 48.8% to 82.1% in the brolucizumab group, and 42.5% to 64.1% in the aflibercept group (see Fig. 5B). A greater proportion of brolucizumab-treated participants than aflibercept-treated participants had minimal fluid or less in the study eye, and at weeks 24, 36, and 40 the results reached statistical significance.
Figure 5.
Total fluid burden—combined intraretinal and subretinal fluid during matched phase. (A) Proportion of participants with true zero fluid in treatment agnostic (gray), brolucizumab (blue), and aflibercept (red) groups. (B) Proportion of participants with minimal fluid or less in treatment agnostic (gray), brolucizumab (blue), and aflibercept (red) groups. *P < 0.05 brolucizumab versus aflibercept.
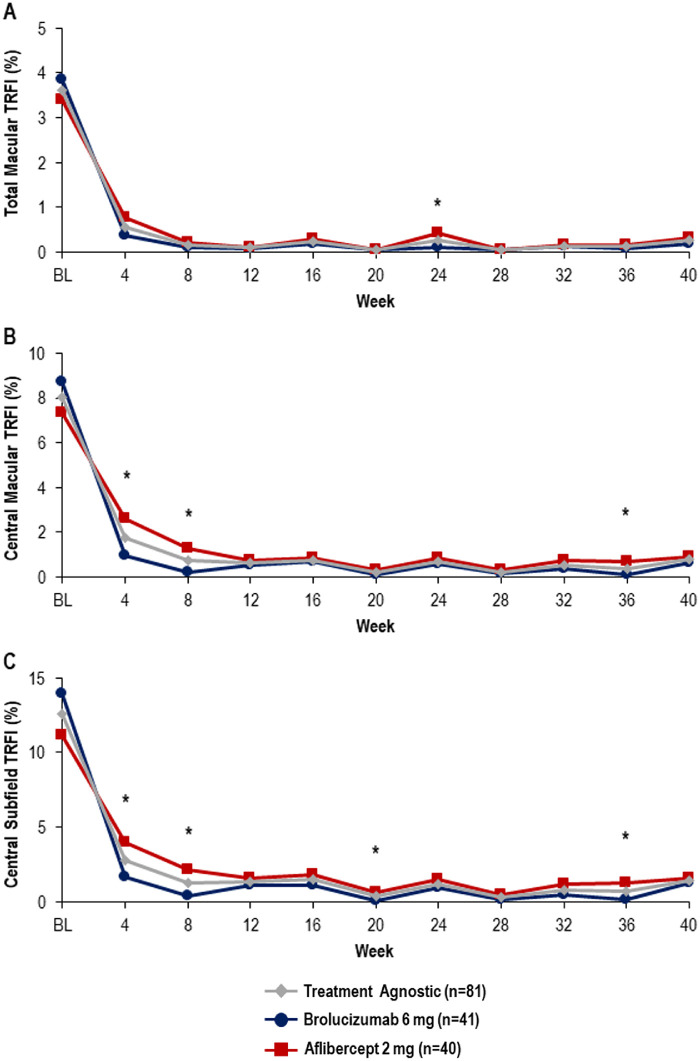
The automated fluid feature segmentation system successfully characterizes the TRFI and the longitudinal dynamics of this OCT biomarker. Significant improvements from baseline in TRFI (total macular, central macular, and central subfield) occurred at all timepoints for the treatment agnostic group and each treatment group (P < 0.001; Fig. 6). The greatest change from baseline for both brolucizumab and aflibercept was seen in central subfield TRFI. In the brolucizumab group, central subfield TRFI was reduced from 13.93% at baseline to 1.62% at week 4 (12.3% change from baseline), whereas in the aflibercept group a reduction from 11.19% to 3.98% (7.2% change from baseline) was observed (Fig. 6C).
Figure 6.
Total retinal fluid index (TRFI) during matched phase. (A) Macular TRFI in treatment agnostic (gray diamond), brolucizumab (blue circle), and aflibercept (red square) groups. (B) Central macular TRFI in treatment agnostic (gray diamond), brolucizumab (blue circle), and aflibercept (red square) groups. (C) Central subfield TRFI in treatment agnostic (gray diamond), brolucizumab (blue circle), and aflibercept (red square) groups. *P < 0.05 brolucizumab versus aflibercept in change from baseline.
Extended Brolucizumab q12 Dosing Versus Aflibercept q8 Dosing Phase Fluid Dynamics
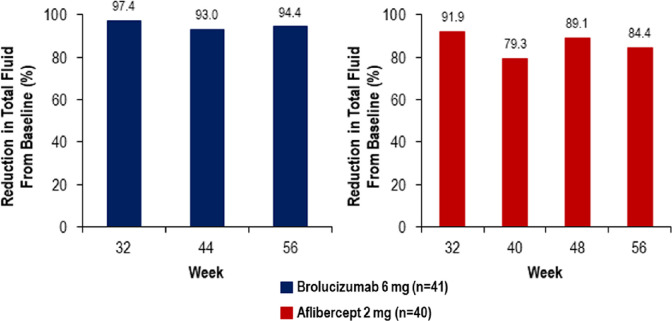
Fluid feature extraction demonstrated feasibility in evaluating therapeutic impact in variable dosing strategies. During the extension phase (weeks 40–56), anti-VEGF treatment continued to demonstrate a mean reduction in both macular IRF volume and SRF volume in the treatment agnostic group. In the brolucizumab group, the percent reduction in total fluid (IRF and SRF combined) from baseline was 93.0% and 94.4% following the first (week 44) and second (week 56) q12 cycles, respectively. The percent reduction in total fluid from baseline in the aflibercept group was 79.3%, 89.1%, and 84.4% at the end of each q8 cycle (weeks 40, 48, and 56, respectively; Fig. 7).
Figure 7.
Brolucizumab q12 and aflibercept q8: total fluid burden—combined intraretinal and subretinal fluid. Reduction in total fluid from baseline with brolucizumab (blue) and aflibercept (red) treatment.
When utilizing the fluid feature extraction platform, the treatment agnostic group demonstrated 38% to 44.4% of participants with true zero fluid between weeks 40 and 56. Following the first (week 44) and the second (week 56) q12 cycle, the proportion of brolucizumab-treated participants achieving true zero fluid was reduced to 36.6% and 38.5%, respectively. During this period, the aflibercept group underwent 3 q8 cycles, and the proportions of participants achieving true zero were 25.6%, 38.5%, and 37.5% at weeks 40, 48, and 56, respectively. For the treatment agnostic group during weeks 40 to 56, minimal fluid or less was achieved in 50.6% to 73.4% of participants when evaluating all timepoints (including 4 weeks after dosing). In the brolucizumab group, 63.4% and 53.8% of participants had minimal fluid or less following the first and second q12 cycles, respectively; between each of the q12 cycles the proportion of participants was at or above 72.5%. The proportion of participants with minimal fluid or less in the aflibercept group was 48.7%, 53.8%, and 47.5% at weeks 40, 48, and 56, respectively.
At week 56, TRFI remained significantly lower than at baseline for all groups. In the brolucizumab group, the total macular, central macular, and central subfield TRFI at the end of the 2 q12 cycles was 0.20%, 0.69%, and 1.00%, respectively. This reflected a 3.6%, 8.2%, and 13.4% reduction from baseline. At week 56 in the aflibercept group, the total macular, central macular, and central subfield TRFI was 0.35%, 1.98%, and 3.10%, respectively; equivalent to 3.1%, 5.4%, and 8.1% reduction from baseline.
Functional and Anatomic Correlation
At baseline, a negative correlation was observed between IRF volume and BCVA (treatment agnostic group, r = −0.52, P < 0.0001). Following initiation of anti-VEGF therapy, there was no correlation between IRF and SRF volumetric parameters and visual acuity. A weak negative but significant correlation was observed at baseline between total macular TRFI and BCVA (combined groups, r = −0.23, P = 0.04). A weak positive correlation between CST and IRF or SRF volume was observed at baseline and various timepoints throughout the study, suggesting that volumetric fluid metrics may be a better direct measure of disease activity than CST alone.
Discussion
To the best of our knowledge, this is the first published report that provides a quantitative and longitudinal analysis of retinal fluid volumes and the TRFI in an nAMD clinical trial data set using novel higher-order OCT assessment. This higher-order OCT post hoc exploratory analysis successfully demonstrated the reduction in fluid volumes in all treatment groups and across dosing strategies. This platform also enabled enhanced-level characterization of fluid burden, including true zero and anatomically minimal fluid. In addition, using the potentially novel OCT biomarker TRFI, this analysis was able to estimate the proportion of IRF and SRF volume against total retinal volume. The assessment of the OSPREY study demonstrated a significant reduction in fluid volume during the matched q8 dosing phase and a similar effect between brolucizumab q12 and aflibercept q8 dosing. The higher-order OCT analysis of the OSPREY data set is consistent with the previously published OSPREY anatomic data.16 In addition, the analysis demonstrated that with two nonindividualized consecutive q12 dosing cycles in the brolucizumab group, the observed overall reduction in fluid volume from baseline was maintained, supporting the HAWK and HARRIER phase III study results, which demonstrated the anatomic effect of brolucizumab.17
In many clinical trials, evidence of disease activity on OCT has been identified as the presence of IRF, SRF, and/or sub-RPE fluid.17,19–22 Clinically, retinal fluid is considered a key parameter used to measure disease activity and inform treatment decisions in nAMD.2 It has been shown that patients with nAMD who have a dry retina following treatment tend to maintain visual acuity,23 whereas vision loss is more likely to occur with new onset of fluid.24 The current quantitative volumetric analysis using higher-order OCT demonstrated capabilities for variable volumetric thresholds, which may have implications for interval tolerance and outcomes. In this analysis, more participants had true zero fluid in the brolucizumab q8 group compared to the aflibercept q8 group (59.0% versus 25.6%) at week 40, with a corresponding greater reduction in fluid percentage from baseline in the brolucizumab group, consistent with the anatomic data reported by Dugel and colleagues.16 In addition, in the OSPREY phase II study, all brolucizumab-treated participants were extended to q12 dosing.16 Even with a nonindividualized q12 extension, there was a ≥ 93% reduction in total fluid (IRF and SRF combined), and > 36% of brolucizumab-treated participants had true zero fluid at the end of each q12 cycle.
Beyond fluid volumes, the RFI is a novel biomarker that has recently been used in a similar analysis of the VISTA study in diabetic macular edema.8 In the current analysis of nAMD, both IRF and SRF were taken into consideration. TRFI is a potentially important OCT biomarker because it takes into account the retinal tissue and is the percentage of space from the RPE to the internal limiting membrane made up of SRF or IRF. Following one treatment of brolucizumab or aflibercept, the TRFI at week 4 in the central subfield decreased dramatically from 13.93% at baseline to 1.62% and from 11.19% to 3.98%, respectively. Use of TRFI is conceptually attractive as it provides contextual information regarding the relative proportion of fluid to retinal tissue. This may represent an important biomechanical feature assessment that is an early marker of underlying atrophy and retinal tissue reserve. Indeed, this novel OCT biomarker needs further exploration as a biomarker for response and outcomes in a larger data set.
The relationship between functional and anatomical parameters is of interest. Many clinical studies have shown that a zero tolerance to fluid is associated with improved visual outcomes; however, other studies have suggested a difference between IRF and SRF factors on final visual acuity.19,20,23,25–28 The current post hoc analysis of the OSPREY study demonstrated a negative correlation between IRF volume and BCVA at baseline, consistent with the notion that the presence of IRF may be a major factor for visual acuity. Interestingly, following treatment, the correlation of IRF volume and SRF volume with BCVA was no longer significant. Many eyes had dramatic reductions in fluid metrics and this likely contributed to the loss of correlation given the wide variability in vision. Examining thresholds for fluid volumes and impact on visual acuity should be considered for future studies. As expected, there was a correlation between CST and fluid volumes at baseline and various timepoints. However, the relationship was fairly weak, suggesting that there is a disconnect between CST and volumetric fluid parameters. Further research is needed to explore whether volumetric fluid parameters may be a more sensitive marker of disease activity.
Several other approaches to automated fluid segmentation have been described, such as custom software, graph-search–based assessment, supervised learning/dimension reduction, and machine learning enhancements.11–15 To date, these tools have remained primarily for research. Having a more efficient and precise way to quantify and characterize fluid may facilitate treatment optimization. In this study, higher-order OCT assessment with an automated machine learning−augmented analysis platform for SD-OCT scans provides quantification of IRF and SRF. This has the potential to provide insights into disease characteristics and imaging biomarkers, which may be helpful in predicting optimal response to treatment and identifying the best dosing regimens.
There are important limitations of the current analysis that should be acknowledged. The post hoc exploratory nature of this analysis and the small sample size used to demonstrate statistical significance for the higher-order OCT assessment in quantifying fluid volume are the main limitations, although the primary focus was the feasibility of fluid feature assessment. Conducting similar analyses on a larger data set in the future should provide further validation of the clinical relevance of these features. These opportunities are currently being explored. However, this data set represents an important proof of concept for preliminary longitudinal analysis of the presence of fluid at numerous timepoints, as it allows for fluid volume quantification in response to treatment in a prospective, randomized nAMD clinical trial. The analysis provides additional information to supplement the fluid segmentation literature as well as insights into the treatment of nAMD with anti-VEGF agents.
The higher-order OCT post hoc exploratory analysis successfully demonstrates the feasibility of longitudinal volumetric fluid quantification and TRFI characterization in nAMD. Utilizing an emerging technology, fluid features were successfully extracted and analyzed for resolution extent and tempo. This study supports the clinical trial evidence demonstrating that brolucizumab dramatically reduces fluid in the retina with the potential to extend to a q12 dosing interval. Future studies will focus on further exploration of fluid compartment thresholds for functional outcomes, volatility of quantitative exudative metrics, and larger data sets to explore outcomes and implications for these assessments.
Acknowledgments
All authors had full control of the study design; data collection, management, and analyses; and manuscript writing. The authors would like to thank all the OSPREY investigators.
Editorial support was provided by IMPRINT Science, New York, NY, USA, and was funded by Novartis Pharmaceuticals.
Supported by a research grant provided by Novartis Pharmaceuticals, East Hanover, NJ, USA, who participated in the design and conduct of the study; data collection, management, and interpretation; and preparation, review, and approval of the manuscript. This work was also supported through the NIH/NEI K23-EY022947-01A1.
Disclosure: J.P. Ehlers, Novartis (F, C), Zeiss (C), Leica/Bioptigen (C), Alcon (F, C), Allergan (F, C), Thrombogenics (F, C), Allegro (C), Regeneron (F, C), Santen (C), and Aerpio (F, C); Genentech (F); Bioptigen/Leica (P), and Zeiss for equipment; J. Clark, Novartis Pharmaceuticals, East Hanover, NJ (E), Novartis Pharmaceuticals, East Hanover, NJ (I) and was a stock/stock option holder at the time of initiation and completion of this study; A. Uchida, unrestricted travel grant from the Alcon Novartis Hida Memorial Award 2015 funded by Alcon Japan Ltd. (R), Betty J. Powers Retina Research Fellowship (R); N. Figueiredo, None; A. Babiuch, Genentech (C) and Regeneron (F); K.E. Talcott, Zeiss (F); L. Lunasco, None; T.K. Le, None; X. Meng, Novartis Pharmaceuticals, East Hanover, NJ (E); M. Hu, None; J. Reese, None; S.K. Srivastava, None
References
- 1. Bakri SJ, Thorne JE, Ho AC, et al.. Safety and efficacy of anti-vascular endothelial growth factor therapies for neovascular age-related macular degeneration: a report by the American Academy of Ophthalmology. Ophthalmology . 2019; 126(1): 55–63. [DOI] [PubMed] [Google Scholar]
- 2. Wykoff CC, Clark WL, Nielsen JS, Brill JV, Greene LS, Heggen CL.. Optimizing anti-VEGF treatment outcomes for patients with neovascular age-related macular degeneration. J Manag Care Spec Pharm . 2018; 24(2-a Suppl): S3–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jaffe DH, Chan W, Bezlyak V, Skelly A.. The economic and humanistic burden of patients in receipt of current available therapies for nAMD. J Comp Eff Res . 2018; 7(11): 1125–1132. [DOI] [PubMed] [Google Scholar]
- 4. Arnold JJ, Markey CM, Kurstjens NP, Guymer RH.. The role of sub-retinal fluid in determining treatment outcomes in patients with neovascular age-related macular degeneration-a Phase IV randomised clinical trial with ranibizumab: the FLUID study. BMC Ophthalmol . 2016; 16: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Venhuizen FG, van Ginneken B, Liefers B, et al.. Deep learning approach for the detection and quantification of intraretinal cystoid fluid in multivendor optical coherence tomography. Biomed Opt Express . 2018; 9(4): 1545–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lad EM, Hammill BG, Qualls LG, Wang F, Cousins SW, Curtis LH.. Anti-VEGF treatment patterns for neovascular age-related macular degeneration among Medicare beneficiaries. Am J Ophthalmol . 2014; 158(3): 537–543.e532. [DOI] [PubMed] [Google Scholar]
- 7. Ciulla TA, Hussain RM, Pollack JS, Williams DF.. Visual acuity outcomes and anti-vascular endothelial growth factor therapy intensity in neovascular age-related macular degeneration patients: a real-world analysis of 49 485 eyes. Ophthalmol Retina . 2020; 4(1): 19–30. [DOI] [PubMed] [Google Scholar]
- 8. Ehlers JP, Uchida A, Hu M, et al.. Higher-order assessment of OCT in diabetic macular edema from the VISTA study: ellipsoid zone dynamics and the retinal fluid index. Ophthalmol Retina . 2019; 3(12): 1056–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Itoh Y, Vasanji A, Ehlers JP.. Volumetric ellipsoid zone mapping for enhanced visualisation of outer retinal integrity with optical coherence tomography. Br J Ophthalmol . 2016; 100(3): 295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xu D, Yuan A, Kaiser PK, et al.. A novel segmentation algorithm for volumetric analysis of macular hole boundaries identified with optical coherence tomography. Invest Ophthalmol Vis Sci . 2013; 54(1): 163–169. [DOI] [PubMed] [Google Scholar]
- 11. Breger A, Ehler M, Bogunovic H, et al.. Supervised learning and dimension reduction techniques for quantification of retinal fluid in optical coherence tomography images. Eye (Lond) . 2017; 31(8): 1212–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chakravarthy U, Goldenberg D, Young G, et al.. Automated identification of lesion activity in neovascular age-related macular degeneration. Ophthalmology . 2016; 123(8): 1731–1736. [DOI] [PubMed] [Google Scholar]
- 13. Kashani AH, Keane PA, Dustin L, Walsh AC, Sadda SR. Quantitative subanalysis of cystoid spaces and outer nuclear layer using optical coherence tomography in age-related macular degeneration. Invest Ophthalmol Vis Sci . 2009; 50(7): 3366–3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Keller B, Cunefare D, Grewal DS, Mahmoud TH, Izatt JA, Farsiu S.. Length-adaptive graph search for automatic segmentation of pathological features in optical coherence tomography images. J Biomed Opt . 2016; 21(7): 76015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee CS, Tyring AJ, Deruyter NP, Wu Y, Rokem A, Lee AY.. Deep-learning based, automated segmentation of macular edema in optical coherence tomography. Biomed Opt Express . 2017; 8(7): 3440–3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dugel PU, Jaffe GJ, Sallstig P, et al.. Brolucizumab versus aflibercept in participants with neovascular age-related macular degeneration: a randomized trial. Ophthalmology . 2017; 124(9): 1296–1304. [DOI] [PubMed] [Google Scholar]
- 17. Dugel PU, Koh A, Ogura Y, et al.. HAWK and HARRIER: phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology . 2020; 127(1): 72–84. [DOI] [PubMed] [Google Scholar]
- 18. Arepalli S, Srivastava SK, Hu M, et al.. Assessment of inner and outer retinal layer metrics on the Cirrus HD-OCT platform in normal eyes. PLoS One . 2018; 13(10): e0203324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wykoff CC, Ou WC, Brown DM, et al.. Randomized trial of treat-and-extend versus monthly dosing for neovascular age-related macular degeneration: 2-year results of the TREX-AMD study. Ophthalmol Retina . 2017; 1(4): 314–321. [DOI] [PubMed] [Google Scholar]
- 20. Silva R, Berta A, Larsen M, et al.. Treat-and-extend versus monthly regimen in neovascular age-related macular degeneration: results with ranibizumab from the TREND study. Ophthalmology . 2018; 125(1): 57–65. [DOI] [PubMed] [Google Scholar]
- 21. Busbee BG, Ho AC, Brown DM, et al.. Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology . 2013; 120(5): 1046–1056. [DOI] [PubMed] [Google Scholar]
- 22. Berg K, Pedersen TR, Sandvik L, Bragadottir R.. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology . 2015; 122(1): 146–152. [DOI] [PubMed] [Google Scholar]
- 23. Brown DM, Tuomi L, Shapiro H, Pier Study Group. Anatomical measures as predictors of visual outcomes in ranibizumab-treated eyes with neovascular age-related macular degeneration. Retina . 2013; 33(1): 23–34. [DOI] [PubMed] [Google Scholar]
- 24. Wickremasinghe SS, Janakan V, Sandhu SS, Amirul-Islam FM, Abedi F, Guymer RH.. Implication of recurrent or retained fluid on optical coherence tomography for visual acuity during active treatment of neovascular age-related macular degeneration with a treat and extend protocol. Retina . 2016; 36(7): 1331–1339. [DOI] [PubMed] [Google Scholar]
- 25. Kertes PJ, Galic IJ, Greve M, et al.. Canadian treat-and-extend analysis trial with ranibizumab in patients with neovascular age-related macular disease: one-year results of the randomized Canadian Treat-and-Extend Analysis Trial With Ranibizumab study. Ophthalmology . 2019; 126(6): 841–848. [DOI] [PubMed] [Google Scholar]
- 26. Jaffe GJ, Martin DF, Toth CA, et al.. Macular morphology and visual acuity in the Comparison of Age-related Macular Degeneration Treatments Trials. Ophthalmology . 2013; 120(9): 1860–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sharma S, Toth CA, Daniel E, et al.. Macular morphology and visual acuity in the second year of the Comparison of Age-related Macular Degeneration Treatments Trials. Ophthalmology . 2016; 123(4): 865–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Simader C, Ritter M, Bolz M, et al.. Morphologic parameters relevant for visual outcome during anti-angiogenic therapy of neovascular age-related macular degeneration. Ophthalmology . 2014; 121(6): 1237–1245. [DOI] [PubMed] [Google Scholar]