Abstract
Aggressive fibromatosis is a rare type of intra-abdominal desmoid tumour that usually involves the small bowel mesentery. It is a locally-invasive lesion, with a high rate of recurrence, but without metastatic potential. Aggressive fibromatosis is seen more often in young female patients. This case report presents the radiological, intraoperative and histopathological findings from a 37-year-old female patient that presented with epigastric pain and a palpable mass in the right hemiabdomen. Histological and immunohistochemical examinations of the resected tumour, including positive staining for beta-catenin, confirmed a postoperative diagnosis of desmoid type fibromatosis. This specific case showed that desmoid type fibromatosis of the colon can mimic gastrointestinal stromal tumours (GIST) based on its clinical presentation, computed tomography and magnetic resonance imaging findings. Differential diagnosis between desmoid type fibromatosis and GIST is clinically very important due to the different treatments and follow-up protocols that are implemented for these lesions.
Keywords: Aggressive fibromatosis, gastrointestinal stromal tumour, computed tomography, magnetic resonance imaging
Introduction
Aggressive fibromatosis is a rare locally-invasive tumour that usually involves the mesentery.1,2 It is predominantly a benign tumour without metastatic potential, but it has a local aggressive effect on surrounding structures and it is associated with a high recurrence rate.1,3 Desmoid type fibromatosis (DTF) is radiologically difficult to distinguish from mesenchymal tumours, which have malignant potential, so misdiagnosis may lead to inadequate therapy.2
This current case report describes a 37-year-old female patient with epigastric pain and a palpable abdominal mass caused by DTF. However, the preoperative computed tomography (CT) and magnetic resonance imaging (MRI) findings suggested a gastrointestinal stromal tumour (GIST) involving the right colon.
Case report
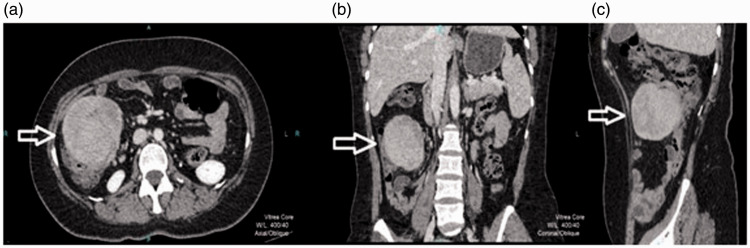
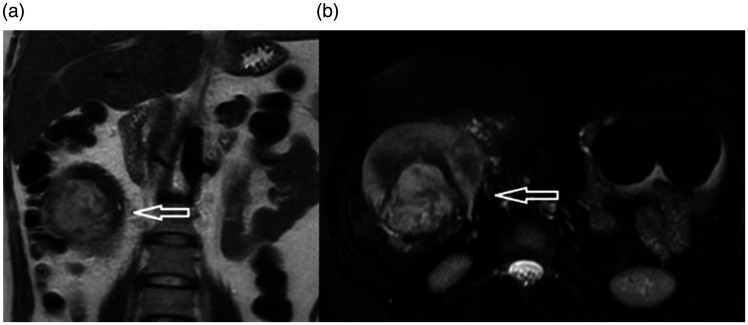
A 37-year-old female presented in September 2019 to the Clinic for Digestive Surgery, University Clinical Centre of Serbia, Belgrade, Serbia with abdominal pain and a palpable mass in the right hemiabdomen. The patient had no comorbidities or a history of previous surgical procedures. The physical examination was otherwise normal. Laboratory findings were unremarkable. Abdominal CT showed an oval, sharply marginated, heterogeneous, mass-like lesion in the wall of the right colon that was 110 × 95 × 90 mm in size (Figure 1). A postcontrast CT examination of the tumour showed heterogeneous enhancement. On MRI, the tumour displayed heterogeneous signal intensity on T2-weighted images with irregular areas of hyperintensity (Figure 2).
Figure 1.
Axial (a), coronal (b) and sagittal (c) contrast-enhanced computed tomography of the abdomen in the portovenous phase of a 37-year-old female that presented with abdominal pain and a palpable mass in the right hemiabdomen showing a sharply marginated solid submucosal mass attached to the caecum wall (arrows).
Figure 2.
Coronal T2-weighted (a) and T2-weighted fat suppressed axial magnetic resonance images (b) of a 37-year-old female that presented with abdominal pain and a palpable mass in the right hemiabdomen showing variable signal intensity of the lesion with irregular internal areas of hyperintensity (arrows).
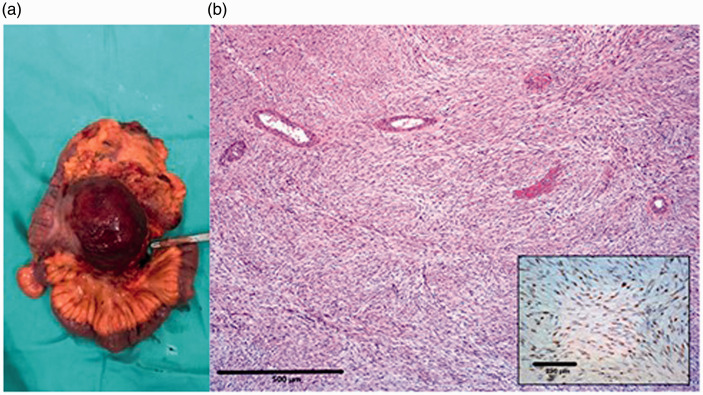
This well-circumscribed, solid submucosal tumour was highly suspicious for GIST. The patient underwent surgery after written informed consent was obtained. A well-marginated mass that invaded the wall of the caecum and small bowel mesentery near the terminal ileum was found intraoperatively (Figure 3a). Thus, a right hemicolectomy with partial resection of the terminal ileum was performed, with latero-lateral ileocolonic anastomosis. Histological examination revealed mesenchymal proliferation with uniform bland spindle-shaped cells in long ‘sweeping’ fascicles or loose, vague storiform arrays. Moreover, medium-sized stromal blood vessels with some perivascular hyalinization and smaller vessels often elongated and compressed between lesional fascicles were found. Further immunohistochemical examination showed nuclear immunohistochemical identification of beta-catenin (inset in Figure 3b) and the diagnosis of DTF was made. At 1 year after surgery, the patient remains disease free and has no signs of disease recurrence.
Figure 3.
Macroscopic image of the resected specimen from a 37-year-old female that presented with abdominal pain and a palpable mass in the right hemiabdomen, which shows a well-circumscribed mass that invaded the caecum wall and small bowel mesentery near the terminal ileum without mucosal infiltration (a). Representative photomicrographs of the tumour showing the immunohistochemical staining for beta-catenin. Scale bar 500 µm (inset image, scale bar 250 µm) (b). The colour version of this figure is available at: http://imr.sagepub.com.
All patient data in the present case were de-identified to ensure that the patient remained anonymous. Ethical approval was not required as the patient underwent standard medical and surgical treatment. Verbal consent was obtained from the patient for publication of this case report and the images included herein.
Discussion
Intra-abdominal desmoid tumours represents a type of fibroblastic proliferation with a tendency for local invasion, a high recurrence rate and no metastatic potential.1 Based on the location, desmoid tumours are divided into extra-abdominal, intra-abdominal and abdominal wall desmoids.1 Among all groups, intra-abdominal desmoids have the highest local recurrence rates.4 Solitary intestinal desmoid tumours are extremely rare, especially those located in the colon.3 These tumours have been classified into four groups: (i) tumours with spontaneous resolution; (ii) tumours with cycles of progression and resolution; (iii) tumours that remain stable; and (iv) neoplasms with aggressive progression.5
Intra-abdominal desmoid tumours are locally aggressive lesions, which can cause ureteric and intestinal obstruction, or vascular and neural compression.5 Complications occur if mesenteric vessels or abdominal organs are involved with consequent ischaemia, perforation, fistula formation and gastrointestinal or intratumoral bleeding.4
Desmoid type fibromatosis usually presents as well-defined homogenous lesions, iso- or hyperdense on CT with very rare necrotic changes.2 In contrast, large GISTs are mostly inhomogeneous tumours with frequent central zones of necrosis and haemorrhage.5 MRI is the preferred imaging modality for the diagnosis of DTF as these lesions are mainly hypointense on T1-weighted images with variable signal intensity on T2-weighted images.2,6 In the majority of cases, DTF are hypointense on T2-weighted images due to a rich fibrous content as compared with GISTs, which are commonly slightly hyperintense.5 Therefore, large and homogenous tumours without internal necrosis and haemorrhage are highly suggestive of aggressive fibromatosis. However, in clinical practice, it is not easy to make a differential diagnosis among these lesions. In the present case, the heterogeneous appearance of the lesion on T2-weighted MRI scans, its clear demarcation and the submucosal propagation led to a preoperative diagnosis of GIST. A definite diagnosis of mesenteric fibromatosis is based on microscopic and immunohistochemical examination.5 In doubtful cases, expression of beta-catenin helps in the differential diagnosis.2 Desmoids do not express CD34 and S100 protein, in contrast to GISTs.2 To the best of our knowledge, this is the second case of a colonic desmoid type of fibromatosis reported in the published literature. In this regard, intra-abdominal desmoid tumours present a diagnostic challenge and should be considered in cases where mesenchymal tumours are attached to the bowel wall with mesenteric involvement.5 In addition, the typical MRI and CT appearance of this rare entity could help in the preoperative distinction between DTF and more common gastrointestinal stromal tumours.
The management of DTF tends to be individualized. Surgery is the most common therapeutic choice, which due to the high rate of recurrence is usually followed with additional therapeutic options.2,6 Radiotherapy can be used for the treatment of recurrent tumours, unresectable lesions or in cases of R1/R2 resection.6,7 Chemotherapy, antihormonal therapies, non-steroidal anti-inflammatory drugs with or without hormonal manipulation and tyrosine kinase inhibitors can be considered as systemic treatment options.6 A randomized, multicentre, two phase study (DESMOPAZ) showed that pazopanib is a sustainable option for the treatment of DTF.8 In cases, like this current patient, with a resectable intra-abdominal tumour, wide resection with tumour-free margins remains the most effective treatment.6 Taking into account the unpredictable clinical behaviour of this disease and the toxic effect of therapeutic options, the initial approach of simple observation has become a standard after curative surgery, as was the case in this current patient. Despite all therapeutic options, the recurrence rate remains very high at 24–77%.1,9 Therefore, these patents should be rigorously monitored with regular CT or MRI examinations every 3–6 months for 2–3 years and then annually therafter.10
Acknowledgements
Conceptualization: M.M.J. & J.D.K.; methodology: D.V. & E.K.; resources: A.J., S.M. & J.D.K.; writing and editing: M.M.J. & J.D.K.; supervision: A.D.S., M.M. & J.D.K.
Footnotes
Declaration of conflicting interest: The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Milica Mitrovic Jovanovic https://orcid.org/0000-0002-7525-7615
References
- 1.Vallabha T, Sindgikar V, Baloorkar R, et al. Desmoid infilterating ileum, a rare complication. Indian J Surg 2013; 75: 192–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wronski M, Ziarkiewicz-Wroblewska B, Slodkowski M, et al . Mesenteric fibromatosis with intestinal involvement mimicking a gastrointestinal stromal tumour. Radiol Oncol 2011; 45: 59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Bree E, Keus R, Melissas J, et al. Desmoid tumors: need for an individualized approach. Expert Rev Anticancer Ther 2009; 9: 525–535. [DOI] [PubMed] [Google Scholar]
- 4.Makis W, Ciarallo A, Abikhzer G, et al . Desmoid tumour (aggressive fibromatosis) of the colon mimics malignancy on dual time-point 18F-FDG PET/CT imaging. Br J Radiol 2012; 85: 37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asenov Y, Genadiev S, Timev A, et al. Ruptured desmoid tumor imitating acute appendicitis – a rare reason for an emergency surgery. BMC Surg 2019; 19: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasper B, Baumgarten C, Garcia J, et al. An update on the management of sporadic desmoid-type fibromatosis: a European Consensus Initiative between Sarcoma PAtients EuroNet (SPAEN) and European Organization for Research and Treatment of Cancer (EORTC)/Soft Tissue and Bone Sarcoma Group (STBSG). Ann Oncol 2017; 28: 2399–2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nuyttens JJ, Rust PF, Thomas CR, Jr, et al. Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: a comparative review of 22 articles. Cancer 2000; 88: 1517–1523. [PubMed] [Google Scholar]
- 8.Toulmonde M, Pulido M, Ray-Coquard I, et al. Pazopanib or methotrexate-vinblastine combination chemotherapy in adult patients with progressive desmoid tumours (DESMOPAZ): a non-comparative, randomised, open-label, multicentre, phase 2 study. Lancet Oncol 2019; 20: 1263–1272. [DOI] [PubMed] [Google Scholar]
- 9.Escobar C, Munker R, Thomas JO, et al. Update on desmoid tumors. Ann Oncol 2011; 23: 562–569. [DOI] [PubMed] [Google Scholar]
- 10.Ghert M, Yao X, Corbett T, et al. Treatment and follow-up strategies in desmoid tumours: a practice guideline. Curr Oncol 2014; 21: 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]