Abstract
Objective
To assess safety and efficacy of a novel intubation laryngeal mask airway (ILMA) during the recovery period following supratentorial tumour surgery.
Methods
Patients who underwent supratentorial tumour surgery at our centre from January 2012 to December 2016 were eligible for this prospective randomised, parallel group study. We developed a novel ILMA using closely fitting laryngeal masks (No. 4/5) with 7.0/7.5 mm endotracheal tubes (ETT) plus screw fixators and anti-pollution sleeves.
Results
In total, 100 patients were intubated with the novel ILMA and 100 the ETT. There were no differences between groups in haemodynamic variables, oxygen saturation, exhaled CO2, or bispectral index all recorded during the 72-hour recovery period. However, there were significantly fewer incidences of coughing, less fluid drainage and lower haemoglobin levels in surgical fluid in the ILMA group compared with the ETT group.
Conclusion
Our novel ILMA device was associated with reduced coughing, fluid drainage and blood in surgical drain during the recovery period following supratentorial tumour surgery.
Keywords: laryngeal mask, tracheal tube, brain tumour, extubation
Introduction
The standard laryngeal mask airway (sLMA) was clinically approved in the UK in 1988 and opened a new chapter in anaesthesia, mainly for management of difficult airways.1–4 Unlike endotracheal tubes (ETTs) which can stimulate the trachea and cause haemoptysis, unstable circulatory dynamics, and reduced comfort levels, sLMAs are associated with easy non-traumatic intubation and minimal somatic and autonomic responses.5–7 However, sLMAs have some disadvantages, including limited protection against aspiration of gastric contents and lower seal pressures.8,9
A modified version of the sLMA, the intubating laryngeal mask airway (ILMA), that combines a mask with a modified tracheal tube, has been designed for guided tracheal intubations.10 Compared with the sLMA, the ILMA is shorter and wider and allows for large ETTs up to 8 mm in diameter. The ILMA has been shown to be a useful device in the management of patients with difficult airways.11 For this study, we developed an ILMA using second-generation closely fitting laryngeal masks (No. 4/No. 5), ETTs (sizes 7.0/7.5/8.0 mm), screw fixators and anti-pollution sleeves. Following compliance tests to determine the best combination of closely fitting mask and ETT, we compared the ILMA with standard ETTs in the anaesthesia of patients undergoing supratentorial tumour surgery at our hospital and assessed efficacy and safety in the recovery period.
Methods
Patients who underwent supratentorial tumour surgery at Nanfang Hospital, Southern Medical University from January 2012 to December 2016, were eligible for this prospective, randomized, parallel group study. To be included in the study patients were ≥18 years of age and their physical status was American Society of Anaesthesiologists (ASAI)-II grade. Patients excluded from the study had the following: difficult airways (i.e., history of snoring, mouth opening <3 cm, Mallampati class III or IV, limited mandibular advancement and/or thyromental distance <6 cm); lung disease (including chronic obstructive airway disease); liver and/or kidney dysfunction; severe heart disease (including pre-operative ejection fraction <45%, sick sinus syndrome, second or third-degree atrioventricular block with no pacemaker); language/hearing or communication difficulties; abnormal blood coagulation; hypertension; diabetes; history of brain surgery.
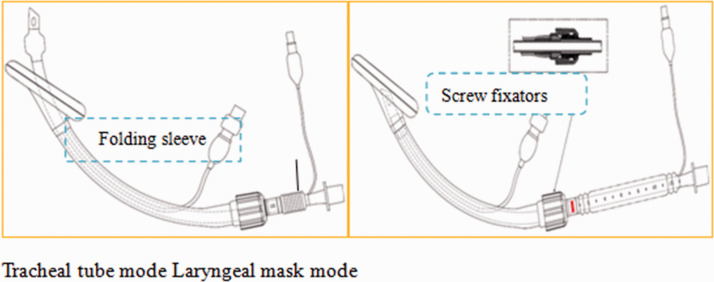
The ILMAs used in this study consisted of second-generation closely fitting laryngeal masks (No. 4/No. 5), ETTs (sizes 7.0/7.5/8.0 mm), screw fixators and anti-pollution sleeves. Five combinations of mask and ETT were investigated: (i) No. 4 mask plus ETT 7.0 mm; (ii) No. 4 mask plus ETT 7.5 mm; (iii) No. 5 mask plus ETT 7.0 mm; (iv) No. 5 mask plus ETT 7.5 mm; (v) No. 5 mask plus ETT 8.0 mm. The end of each mask was fitted with a screw fixation system and an anti-pollution sleeve was placed over the end of the ETT. For each of the five groups of ILMAs, the following were determined: holding force; locking/unlocking time of the screw fixation; conversion time between mask and ETT mode; airway leakage; airway resistance; folding sequence of anti-pollution sleeve. The results of these compliance studies indicated that No. 4 laryngeal mask matched with ETT 7.0 mm and No. 5 mask matched with ETT 7.5 mm were the optimal combinations. The final folded length of the ILMAs ranged from 2–3 cm (Figure 1).
Figure 1.
Design of the intubating laryngeal mask (ILMA).
Diagram showing that the ILMA can easily transition between tracheal tube mode and the laryngeal mask mode.
Following routine induction of anaesthesia using midazolam, propofol, sufentanil, and cistrotracurium, patients were randomly allocated to a ILMA or an ETT device for intubation. The randomization process was performed using an automatic assignment system that concealed allocation. Anaesthesia was maintained with sevoflurane 2.5–3.5% and the tidal volume was set at 600 ml and respiratory rate at 12 breaths/min. Patients were transferred to surgical ICU following the operation. Blood pressure (BP), heart rate (HR), incidence of coughing; drainage of the surgical wound, haemoglobin levels in surgical drain; the amount of carbon dioxide in exhaled air (ETCO2), oxygen saturation (SpO2.) and bispectral index (BIS) were monitored 5 mins before the extubation and thereafter for 72 hours. The BIS monitor ranges from 0 (non-responsive) to 100 (fully awake).
Patients provided written informed consent and the study was approved by the Ethics Committee of Nanfang Hospital, Southern Medical University.
Statistical analyses
Data were analysed using the Statistical Package for Social Sciences (SPSS®) for Windows® release 2019 (IBM Corp., Armonk, NY, USA). All tests were two-sided and a P-value <0.05 was considered to indicate statistical significance. Data were expressed as the mean ± standard deviation (SD). The Kolmogorov-Smirnov/Shapiro-Wilk test was used to determine if variables were normally distributed. Student t-test was used to compare normally distributed continuous variables and Mann–Whitney U test was used for non-normally distributed variables.
Results
In total, 200 patients (108 men/ 92 women) who underwent supratentorial tumour surgery at our hospital between 2012 and 2016 were eligible for the study. Sizes of the supracerebral brain tumours ranged from 2.1 × 1.1 cm to 8.1 × 11.2 cm. One hundred patients were allocated an ILMA and 100 patients an ETT. The ILMA group consisted of 58 men/42 women and the ETT group 50 men/50 women. There were no differences between groups in average age or weight. The ILMA group was 59 ± 19 years of age and weighed 60 ± 18 kg, whereas the ETT group was 64 ± 21 years of age and weighed 56 ± 21 kg.
The incidence of coughing during the extubation period was statistically significantly (P < 0.01) lower in the ILMA group (6.8 ± 1.7%) compared with the ETT group (52.3 ± 12.3%).
The values for cumulative drainage of surgical wounds in the ILMA group at 1, 2, 3, 12, 24, 48 and 72 hours after extubation were statistically significantly (P < 0.01) lower compared with those in the ETT group (data not shown).
Following extubation, haemoglobin levels in the surgical drain at 1, 2, 3, 12, 24, 48 and 72 hours were statistically significantly (P < 0.01) lower compared with those in the ETT group (data not shown).
However, there were no difference between groups in BP, HR, SpO2, ETCO2, or BIS recorded 5 mins before extubation and at 5, 10, 30 mins, 1, 6, 12, 24, 48 and 72 h following extubation (Table 1).
Table 1.
Haemodynamic and respiratory monitoring of the patients during the recovery period (ILMA, n = 100; ETT, n = 100)
| Extubation period |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| −5 min | +1 min | +5 min | +10 min | +30 min | +60 min | +6 hours | +12 hours | +24 hours | +48 hours | +72 hours | ||
| HR, bt/min | ILMA | 75 ± 21 | 96 ± 27 | 82 ± 18 | 82 ± 19 | 79 ± 25 | 76 ± 28 | 78 ± 23 | 73 ± 21 | 73 ± 19 | 75 ± 17 | 78 ± 23 |
| ETT | 78 ± 23 | 80 ± 21 | 75 ± 25 | 76 ± 18 | 71 ± 23 | 69 ± 18 | 71 ± 19 | 75 ± 22 | 73 ± 18 | 69 ± 19 | 68 ± 17 | |
| sBP, mmHg | ILMA | 135 ± 25 | 132 ± 31 | 138 ± 25 | 128 ± 31 | 123 ± 28 | 122 ± 21 | 128 ± 25 | 131 ± 29 | 118 ± 21 | 120 ± 22 | 118 ± 28 |
| ETT | 128 ± 30 | 112 ± 33 | 130 ± 29 | 118 ± 21 | 121 ± 30 | 130 ± 25 | 127 ± 31 | 121 ± 33 | 125 ± 27 | 120 ± 21 | 115 ± 23 | |
| SpO2,% | ILMA | 97 ± 3 | 95 ± 5 | 94 ± 3 | 91 ± 5 | 90 ± 8 | 95 ± 5 | 96 ± 4 | 96 ± 4 | 97 ± 3 | 97 ± 3 | 98 ± 2 |
| ETT | 96 ± 4 | 98 ± 2 | 97 ± 3 | 98 ± 2 | 98 ± 2 | 97 ± 3 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 96 ± 4 | |
| ETCO2,% | ILMA | 40 ± 8 | 42 ± 8 | 48 ± 12 | 45 ± 10. | 42 ± 12 | 42 ± 11 | 38 ± 10 | 42 ± 12 | 38 ± 10 | 40 ± 11 | 40 ± 12 |
| ETT | 36 ± 12 | 35 ± 11 | 41 ± 12 | 41 ± 12 | 40 ± 12 | 40 ± 11 | 42 ± 8 | 36 ± 10 | 39 ± 9 | 42 ± 12 | 36 ± 9 | |
| BIS | ILMA | 55 ± 13 | 58 ± 20 | 77 ± 21 | 78 ± 22 | 79 ± 20 | 80 ± 18 | 82 ± 17 | 88 ± 10 | 89 ± 10 | 89 ± 10 | 89 ± 9 |
| ETT | 56 ± 12 | 56 ± 21 | 80 ± 19 | 78 ± 21 | 79 ± 19 | 80 ± 19 | 82 ± 17 | 87 ± 11 | 90 ± 9 | 90 ± 10 | 89 ± 11 | |
Abbreviations: HR, heart rate; sBP, systolic blood pressure, SpO2, oxygen saturation; ETCO2, carbon dioxide in exhaled air; BIS, bispectral index (0100 [fully awake]); ILMA, intubating laryngeal mask; ETT, endotracheal tube
Discussion
Although tracheal intubation is advantageous in ensuring that the airway is safe during anaesthesia, the procedure is associated with several complications such as tooth and oropharyngeal injuries, laryngeal spasm, laryngeal oedema, dislocation of arytenoid cartilage, and arrhythmias and increased blood pressure.12–14 To overcome these problems, the LMA, was developed and has been in clinical use since 1988.1The LMA is a non-invasive, easy-to-operate ventilation tool that can be rapidly placed in the throat without touching the glottis and trachea; it causes little stimulation to the respiratory tract and has no effect on HR and BP.15 However, the mouth of the classic LMA has a double-sided barrier that blocks the passage of the ETT and the ventilation tube is slender so even the largest LMA can only guide the insertion of a 6.0 mm ETT. In addition, it may be difficult to withdraw the laryngeal mask after a successful tracheal intubation.11 Also, laryngeal masks have limited protection against aspiration of gastric contents and lower seal pressures.8,9,16 The intubating laryngeal mask was developed to correct the aforementioned shortcomings.10,17
Currently, three types of intubating laryngeal masks are used in clinical practice (Fastrach™, CTrach™, and Cookgas™).17–19 The Fastrach LMA consists of a rigid airway tube, an integrated guiding handle, an elevator bar, an airway tube, and a cuff.17 The tube has a 30° angle with the mask, which is consistent with the natural bending of the oropharynx and is convenient for both placement and guiding. The CTrach system has a built-in optical fibre bundle and its proximal end is connected to a display via a magnetic connector; the distal end is under the epiglottic elevating bar.18 The optical display allows clinicians to look directly at the throat while completing tracheal intubation. The Cookgas LMA has a short transparent ventilation tube with a large lumen, and a large bending angle; a 15 mm connector can be removed prior to intubation which is an effective method for increasing the inner diameter of the ventilation tube and allowing the cuffed ETTs to pass in a smooth manner.19
In this present study, we developed an ILMA and found optimal designs were a No. 4 mask/ ETT 7.0 and No. 5 mask/ ETT 7.5 mm plus screw fixators and anti-pollution sleeves. We used the novel ILMA in the general anaesthesia of patients undergoing supratentorial tumour surgery. Patients with brain tumours may show fluctuating cardiovascular haemodynamic dysfunction which can bring about unwanted complications.20 Therefore, the smooth induction of anaesthesia and its maintenance could lessen any untoward hemodynamic fluctuations for these patients and reduce the occurrence of stress reactions. Indeed, haemodynamic changes such as tachycardia, hypertension, and arrhythmias during laryngoscopy and intubation can cause serious complications in patients with coexisting cardio- or cerebrovascular diseases.5Importantly the coughing reflex which can occur with extubation of traditional ETTs can cause activation of the sympathetic-adrenal system leading to further increases in the incidence of cardiovascular events in these patients.21,22 We found our device was safe and could be smoothly transitioned into both mask and ETT modes. We observed significantly fewer incidences of coughing, less fluid drainage and lower haemoglobin levels in the surgical drain in the group intubated with the ILMAs compared with those intubated with ETTs. Furthermore, there were no differences between groups in BP, HR, SpO2, ETCO2, or BIS during the recovery period.
This study had some limitations. For example, only 200 patients were involved and the study was single-blind. In addition, it was not always possible to identify the tumour borders precisely on imaging and so the defect may have been estimated to be larger than it was.
In conclusion, our novel ILMA was an effective airway device with a similar safety profile to traditional ETT in the recovery period but was associated with less coughing, less fluid drainage and less blood in the surgical drain.
Footnotes
Declaration of conflicting interests: The authors declare that there are no conflicts of interest.
Funding: This work was supported by the 2017 Provincial Science and Technology Plan Project.
ORCID iD: Jinfang Xiao https://orcid.org/0000-0002-7974-1930
References
- 1.Almeida GC. Supraglottic Airway Devices: A Review in a New Era of Airway Management. Journal of Anesthesia & Clinical Research 2016; 7: 7 [Google Scholar]
- 2.Brain AI. The laryngeal mask–a new concept in airway management. Br J Anaesth 1983; 55: 801–805. [DOI] [PubMed] [Google Scholar]
- 3.Brain AI. The laryngeal mask airway–a possible new solution to airway problems in the emergency situation. Arch Emerg Med 1984; 1: 229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brain AI. The development of the Laryngeal Mask–a brief history of the invention, early clinical studies and experimental work from which the Laryngeal Mask evolved. Eur J Anaesthesiol Suppl 1991; 4: 5–17. [PubMed] [Google Scholar]
- 5.Sabuncu U, Kusderci HS, Oterkus M, et al. AuraGain and i-Gel laryngeal masks in general anesthesia for laparoscopic cholecystectomy. Performance characteristics and effects on hemodynamics. Saudi Med J 2018; 39: 1082–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson IG, Fell D, Robinson SL, et al. Cardiovascular responses to insertion of the laryngeal mask. Anaesthesia 1992; 47: 300–302. [DOI] [PubMed] [Google Scholar]
- 7.Braude N, Clements EA, Hodges UM, et al. The pressor response and laryngeal mask insertion. A comparison with tracheal intubation. Anaesthesia 1989; 44: 551–554. [DOI] [PubMed] [Google Scholar]
- 8.Ramaiah R, Das D, Bhananker SM, et al. Extraglottic airway devices: A review. Int J Crit Illn Inj Sci 2014; 4: 77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brimacombe J. The advantages of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anaesth 1995; 42: 1017–1023. [DOI] [PubMed] [Google Scholar]
- 10.Steel A. The intubating laryngeal mask airway. Emerg Med J 2005; 22: 47–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joo HS, Kapoor S, Rose DK, et al. The intubating laryngeal mask airway after induction of general anesthesia versus awake fiberoptic intubation in patients with difficult airways. Anesth Analg 2001; 92: 1342–1346. [DOI] [PubMed] [Google Scholar]
- 12.Simons T, Söderlund T, Handolin L. Radiological evaluation of tube depth and complications of prehospital endotracheal intubation in pediatric trauma: a descriptive study. Eur J Trauma Emerg Surg 2017; 43: 797–804. [DOI] [PubMed] [Google Scholar]
- 13.Hua A, Haight S, Hoffman RS, et al. Endotracheal Intubation after Acute Drug Overdoses: Incidence, Complications, and Risk Factors. J Emerg Med 2017; 52: 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang HE, Peitzman AB, Cassidy LD, et al. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med 2004; 44: 439–450. [DOI] [PubMed] [Google Scholar]
- 15.Cottle D, Shondipon L. (eds). Anaesthetics for Junior Doctors and Allied Professionals: The Essential Guide. London. CRC Press, 2018. [Google Scholar]
- 16.Maltby JR. The laryngeal mask airway in anaesthesia. Can J Anaesth 1994; 41: 888–893. [DOI] [PubMed] [Google Scholar]
- 17.Gerstein NS, Braude DA, Hung O, et al. The Fastrach Intubating Laryngeal Mask Airway: an overview and update. Can J Anaesth 2010; 57: 588–601. [DOI] [PubMed] [Google Scholar]
- 18.Liu EH, Goy RW, Chen FG. The LMA CTrach, a new laryngeal mask airway for endotracheal intubation under vision: evaluation in 100 patients. Br J Anaesth 2006; 96: 396–400. [DOI] [PubMed] [Google Scholar]
- 19.Jagannathan N, Kozlowski RJ, Sohn LE, et al . A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesth Analg 2011; 112: 176–182. [DOI] [PubMed] [Google Scholar]
- 20.Liebner S, Dijkhuizen RM, Reiss Y, et al. Functional morphology of the blood–brain barrier in health and disease. Acta Neuropathol 2018; 135:311–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang C, Chai X, Kang F, et al. I-gel Laryngeal Mask Airway Combined with Tracheal Intubation Attenuate Systemic Stress Response in Patients Undergoing Posterior Fossa Surgery. Mediators Inflamm 2015; 2015: 965925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perelló-Cerdà L, Fàbregas N, López AM, et al. ProSeal Laryngeal Mask Airway Attenuates Systemic and Cerebral Hemodynamic Response During Awakening of Neurosurgical Patients: A Randomized Clinical Trial. J Neurosurg Anesthesiol 2015; 27: 194–202. [DOI] [PubMed] [Google Scholar]