Abstract
Introduction
Sixty percent of all carpal fractures affect the scaphoid bone, with an annual incidence of 4.3/10,000. Displacement and instability are the main risk factors for non-union, but missed diagnosis, location of fracture and poor blood supply are also risk factors. Non-union is defined as non-healed fracture on radiographs 6 months after the injury and this can lead to degenerative wrist arthritis. Treatment options vary from internal fixation with bone grafting to salvage procedures including arthrodesis of carpals. We aimed to determine the effectiveness of screw fixation without bone grafting for the treatment of stable well-aligned scaphoid non-union.
Methods
In this systematic review, MEDLINE, Science Direct, Web of Science and CINHAL were searched from inception to May 2019. All clinical studies that examined the functional and radiological outcomes of screw fixation without bone grafting to treat stable scaphoid non-union were included.
Results
838 articles were retained of which 6 case series, describing 95 patients who had undergone scaphoid non-union fixation without bone grafting, were included. Favourable functional outcomes were reported by the 6 included studies using validated functional outcome measures ROM improved to weighted mean of 67.5° (±13°) and 62.12° (±13°) for flexion and extension respectively. The fracture had united in 91 out of 95 participants with a union rate of 95.7% (95%, CI 89.5 to 98.8) and the weighted mean time to union was 3.8 (±1.5) months.
Conclusion
Rigid screw fixation without bone grafting can be suggested for the treatment of selected well aligned scaphoid nonunions to achieve healing and good functional outcomes. However, adequately powered clinical studies with good methodology are essential to draw an accurate conclusion.
Keywords: Non-union, Scaphoid, Surgery, Bone graft, Fixation
1. Introduction
Scaphoid fracture is the most common type of carpal bone fractures representing 60% of all carpal fractures.1 In adults, 70% of scaphoid fractures affect the waist, 20% the proximal pole, and the remaining 10% to the distal pole.1 Its annual incidence is 4.3 per 10,000 people and mainly occurs in young active males.2
Scaphoid non-union is defined as non-healed fracture on radiographs 6 months after the injury. The main risk factors for scaphoid non-union are; instability, displacement and the gap between the fracture fragments, location of fracture and missed diagnosis of acute scaphoid fractures.3, 4, 5
Scaphoid Non-union can be stable or unstable.3 In stable non-union, usually the scaphoid shape is preserved, and the fracture fragments are connected with firm fibrous band. However, with time this may progress to unstable pattern of degenerative changes and eventually leads to scaphoid non-union advanced collapse, which is more difficult to treat.3,6
Treatment goals for non-union include achieving fracture union, symptomatic relief, improving hand function and avoiding long term complications like arthritis and carpal collapse.3,4 The options of treatment vary from fixation with vascularised or non-vascularised bone grafting to salvage procedure including arthrodesis of carpal bones.3,7 The standard method for treatment of scaphoid non-union is an open approach for deformity correction, bone grafting and rigid internal fixation.8 The introduction of non-vascularised graft showed an improvement in union rate when combined with internal fixation. However, there are some small published studies which reported that internal fixation without bone grafting is good enough to achieve union in selected cases of stable well-aligned scaphoid non-union. To our knowledge, no systematic reviews have addressed the role of rigid fixation without bone grafting in the treatment of stable scaphoid non-union.
1.1. Aim
Explore the literature to identify evidence on the effectiveness of mechanical stabilization using screw fixation without bone grafting to treat stable well-aligned scaphoid non-union.
2. Material and methods
All reported retrospective or prospective clinical studies that examined the clinical and radiological outcomes of rigid fixation without bone grafting in the treatment of stable well-aligned scaphoid non-union were included in this systematic review. Surgical intervention included percutaneous or open technique by any means of screw fixation (retrograde or antegrade) and any approach (dorsal or volar).
Preferences were given to validated functional outcome measures such as Modified Mayo Wrist Score (MMWS)9 and Disability of the Arm, Shoulder and Hand (DASH) score,10 but other different clinical measures were also considered. Radiological evaluation of fracture healing was measured by plain radiographs or CT scans.
Studies on participants with acute injuries or delayed union (<6 months) were excluded. Studies which failed to separate delayed union from non-union were also excluded. Studies were excluded if participants had scaphoid malalignment, excessive sclerosis, arthritis, avascular necrosis, or revision surgery.
The following databases were searched from inception to May 2019: MEDLINE, ScienceDirect, Web of Science, CINHAL, using combination of Keywords: “Scaphoid non-union AND surgery” AND “internal fixation” AND “functional outcomes”. In addition, reference lists of relevant studies were checked. The language and publication date were not restricted in the present systematic review. The studies obtained from each database were merged to eliminate replicas. The selection criteria (Table 1) for each included study were defined by population, intervention, outcomes and study design.
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Study Design | Retrospective and prospective | Non-clinical trial |
| Case series | Case report | |
| RCTs and non-randomised studies | ||
| Non-blind and blinded studies | ||
| Any language | ||
| Participants | stable well aligned scaphoid non-union. | Acute injury or <6 months |
| >6 months | AVN | |
| Unstable fracture | ||
| Malalignment | ||
| <6months | ||
| Arthritis | ||
| Interventions | - Any type of screw fixation | - Bone grafting used |
| - Any approach (Open or percutaneous) | - K.wire fixation | |
| - If the data of screw fixation without bone grafting cannot be separated from Grafting data. | ||
| - Previous surgery | ||
| -Malalignment | ||
| Outcomes | - Clearly defined set of relevant assessments on ROM and functional outcome (preferences was given to validated outcome measures) | Not reporting functional outcomes. |
| - Radiological evaluation | ||
| - Adverse events |
Two reviewers (LE) and (AA) evaluated relevant trials against the inclusion and exclusion criteria in Table 1 and any disagreement was resolved by discussion. Both descriptive and outcome data were extracted using a pre-piloted data extraction form by two reviewers (LE) and (AA) separately. Potential biases in the included studies’ practices were assessed by two independent reviewers (LE and AA) and any disagreement was resolved by discussion. A narrative review of all the results of eligible trials was completed and also, where judged appropriate, we pooled and represented data using 95% confidence intervals for all proportions and weighted mean and standard deviation as described by Bland and Kerry, 1998.11
3. Results
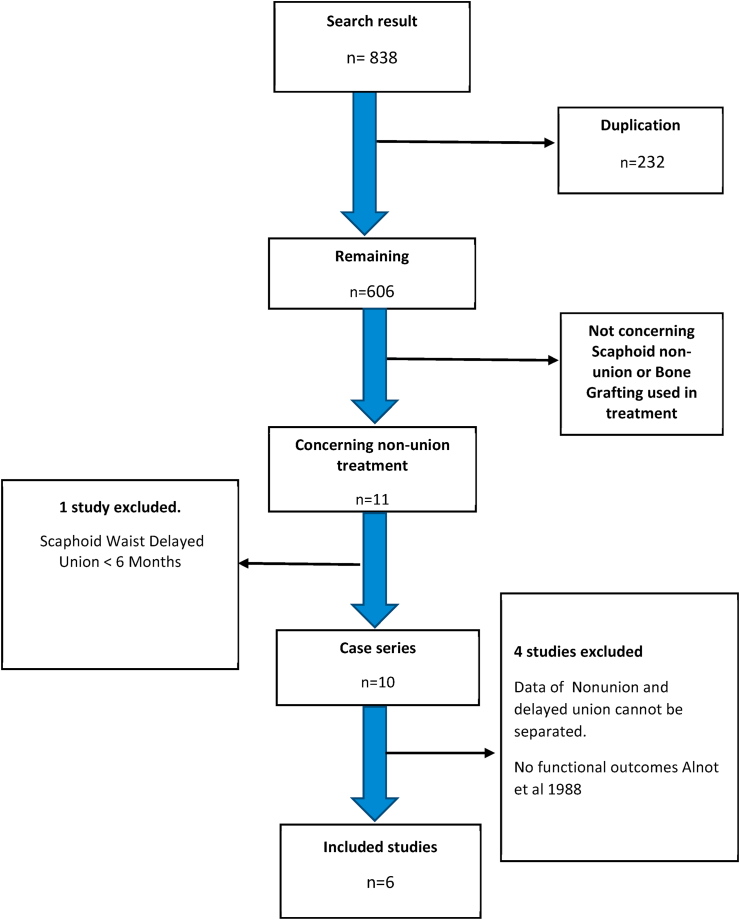
Eight hundred and thirty-eight articles were returned by the search strategy, of which 606 studies remained after filtering the duplicate. Applying the inclusion and exclusion criteria in Table 1 has yielded 6 case series (level of IV evidence) with 95 participants (Fig. 1). These were the subject of our systematic review. Five studies were reported in English and one in Korean. Four were designed retrospectively (Gurger et al. 2018,12 Cha et al. 2017,13 Somerson et al. 201514 & Capo et al. 201215) and 2 prospectively (Mahmoud et al. 201016 & Slade et al. 200317) Table 2.
Fig. 1.
Flow diagram of the systematic review.
Table 2.
Population characteristics of the included studies.
| Study | No. | Mean age -yeas | Gender ratio (M: F) | Diagnosis | Onset of injury | treatment | Study design | Level of evidence |
|---|---|---|---|---|---|---|---|---|
| Gurger et al. (2018) | 12 | 27 | 10:2 | Stable nonunion | 7.6 months | Volar P/C 3.3 headless cannulated screw | retrospective case | IV |
| Waist + PP | series | |||||||
| Cha et al. (2017) | 15 | 28.9 ± 6.2 | 15:0 | Nonunion | 10.8 months | Volar P/C 3.0 mm headless compression screw (DepySynthes) | retrospective case | IV |
| Waist | series | |||||||
| Somerson et al. (2015) | 14 | 21.1 ± 10.6 | 13:1 | Fibrous nonunion | >6 months | Volar/dorsal open | retrospective case | IV |
| Waist + PP | A headless screw (Acutrak; Acumed: Hillsboro) | series | ||||||
| Capo et al. (2012) | 12 | 24 | 11:1 | Nonunion waist | 8.7 months | Volar/dorsal | retrospective case | IV |
| P/C headless screw | series | |||||||
| Mahmoud et al. (2010) | 27 | 28.3 | 26:1 | nonunion | 18.2 months | Volar P/C 3.0 mm cannulated screw | Prospective case series | IV |
| with substantial bone loss >2 mm | ||||||||
| Waist | ||||||||
| Slad 2003 et al. (2003) | 15 | 20 | 14:1 | nonunion with minimal sclerosis or Fibrous union | 9 months | Dorsal P/C cannulated headless screw (Acutrak) | Prospective case series | IV |
| Total | 95 | Mean age 24.8 years |
89:6 (93.6% males) | >6 months |
P/C: percutaneous, PP: proximal pole, M: male, F: female.
The pooled participants’ mean age was 24.8 years and 93.6% of them were males. The mean time between the initial injury and the surgical intervention in the studies varies from 6 to 18.2 months (Table 2). In one study by Gurger et al. 201812 the viability of the proximal pole was assessed by obtaining pre-operative MRI for all participants. Cha et al. 201713 and Slade et al. 200317 used MRI to confirm the vascularity for some patients with sclerosis of the proximal pole on plain radiographs. Participants of the other three studies (14, 15 &16) did not show any hyper density of the proximal fragment on routine radiographs, therefore pre-operative MRI scan was not obtained.
The validated DASH score (13, 14 &15) or MMWS (12, 16&17) and Range of Motion (ROM) were used in all included studies to assess the functional outcome of the surgical intervention. One study by Somerson et al., in 201514 used open approach to fix scaphoid fibrous non-union, whereas in the other five studies screw fixation was achieved percutaneously either by dorsal or volar approach (Table 2). All studies used plain radiographs to confirm the radiological signs of union.
Functional and clinical outcomes were evaluated by validated outcome measures in all included studies. There were noticeable differences between the 6 studies, particularly in the duration of follow up, demography of participants and the surgical technique used (Table 2). For example, Studies with longer follow up, more than 20 months, such as Mahmoud et al. 201016 and Capo et al. 201215 have shown better functional outcomes compared to those with follow up less than 6 months (Table 4, Table 5). Bone healing criteria on radiographs were slightly different between the included studies, however presence of bone trabeculae or callus crossing fracture site was defined as union. Therefore, it was difficult to pool an overall functional result from these studies and a narrative review of the functional outcomes was completed.
Table 4.
Modified mayo wrist score reported by gurger et Al 2018, mahmoud et al. (2010) and slad 2003 et al. (2003).
| Study or subgroup | Follow up | score |
|---|---|---|
| Gurger et al. (2018) | 4.5 months | 8 Excellent and 3 good |
| Mahmoud et al. (2010) | 24.6 months | 25 excellent (92.6%) and two good (7.4%) results |
| Slad 2003 et al. (2003) | 12 excellent and 3 good results. |
Table 5.
DASH score reported by Cha et al., 2017, Somerson et al., 2015, Capo et al., 2012.
| Study or subgroup | Follow up | Mean score |
|---|---|---|
| Cha et al. (2017) | 12 months | 7 ± 3.9 |
| Somerson et al. (2015) | continued until symptoms resolved | 10.2 |
| Capo et al. (2012) | 35 months | 6 |
MMWS was reported by Gurger et al. 2018,12 Mahmoud et al. 201016 and Slade et al. 200317 in a total of 54 out of 95 participants (Table 3). The MMWS is based on: pain, functional status, movement and grip strength. The score ranges from 0 to 100; where 0 to 64 is poor, 65 to 79 fair, 80 to 89 good and 90 to 100 is excellent. The overall results of the above 3 studies were excellent in 45 (83%) (95%, CI 70.7 to 92.1) and good in 8 (14.8%) out of 54 participants (Table 4).
Table 3.
Outcome measures used by reviewed studies.
| Study | The outcome measures used |
||||
|---|---|---|---|---|---|
| Functional outcome |
Radiological evaluation |
||||
| DASH | Modified Mayo | ROM | X-ray | CT | |
| Gurger et al. (2018) |  |
 |
 |
 |
|
| Cha et al. (2017) |  |
 |
 |
 |
|
| Somerson et al. (2015) |  |
 |
 |
||
| Capo et al. (2012) |  |
 |
 |
||
| Mahmoud et al. (2010) |  |
 |
 |
 |
|
| Slad 2003 et al. (2003) |  |
 |
 |
||
Three studies, Cha et al. 2017,13 Somerson et al. 201514 and Capo et al. 201215 used the validated DASH score in a total of 41 out of 95 participants (Table 3). DASH score is used as an indicator of the impact of an impairment on the level and type of disability and it ranges from 0 (no disability) to 100 (most severe disability). The study with the longest follow up by Capo et al. 201215 demonstrated the lowest DASH score of 6 at 35 months. Similarly, the average DASH scores of Cha et al. 201713 and Somerson et al. 201514 were 7 and 10 respectively at 12-month follow-up (Table 5).
The wrist range of movement (ROM) was also used in the evaluation of clinical outcomes in the 6 included studies (Table 3). In only one study by Mahmoud et al. 2010,16 the post-operative ROM was assessed by an independent hand therapist using a goniometer to reduce the risk of detection bias. Overall, the ROM improved to a weighted mean of 67.5° (±13°) and 62.12° (±13°) for flexion and extension respectively (Table 6).
Table 6.
Radiological outcomes and ROM.
| Study or subgroup | Radiological outcomes |
ROM |
|||
|---|---|---|---|---|---|
| mean time to union | Union | nonunion | flexion | extension | |
| Cha et al. (2017) | 5.5 months | 15 | 0 | 69° | 68° |
| Gurger et al. (2018) | 3.8 months | 11 | 1 | 68° | 66° |
| Somerson et al. (2015) | 4.4 months | 12 | 2 | 73° | 66° |
| Capo et al. (2012) | 4 months | 11 | 1 | 71° | 66° |
| Mahmoud et al. (2010) | 2.9 months | 27 | 0 | 65.7° | 60.7° |
| Slad 2003 et al. (2003) | 3.5 months | 15 | 0 | 61° | 49° |
| Total | Mean 4 months | 91 | 4 | 67.9° | 62.6° |
Overall, there was a general trend in all the included studies that surgical intervention using a screw without bone grafting for the treatment of well aligned stable scaphoid non-union provides favourable functional outcomes and ROM.
The criteria to confirm radiological union were slightly different among the 6 included studies. However, the presence of bone trabeculae crossing fracture site in five scaphoid views or presence of callus in at least three cortices on plain radiographs was defined as union in most of the studies. In addition, two studies (13 & 17) used CT scan to confirm the radiological union. In the 6 included case series the fracture had united in 91 out of 95 participants with a union rate of 95.7% (95%, CI 89.5 to 98.8) and only 4 fractures failed to heal with a non-union rate of 4.3% (Table 6). The weighted mean time to union in the included studies in this review was 3.87 (±1.5) months (range from 2.9 to 5.5 months).
4. Discussion
Application of the pre-identified criteria of eligibility lead to the inclusion of 6 case series with 95 patients, which is a relatively small number with low level of evidence. However, the comprehensive electronic search strategy, allowed confidence to conclude that almost all the important studies related to the review question were successfully included. Hence, the conclusion arising from this review was based on the synthesis of evidence from all the key research available in the literature.
Overall, the risk of bias in the 6 included studies was relatively moderate to high because of the inherent limitation of the case series (level IV evidence). None of the included studies reported in detail on their recruitment strategies and this might lead to selection biases, which in turn can affect the outcomes of the intervention.18 Four of the studies (12, 13, 14 & 15) had a retrospective design and relied on the accuracy of medical records which can be subjected to a wide range of bias. The surgical procedures and post-operative protocol were described well in all included studies, making them externally valid. The risk of bias in the assessment of clinical outcome was high in 5 studies (12,13,14,15 and17) due to the nature of the intervention, the study design and the lack of reporting on the outcome assessors. However, in the study by Mahmoud and Koptan in 2011,16 the risk of detection bias was minimised by using an independent hand therapist to complete the clinical and radiological assessment.
Although the participants’ ages were variable among the trials with a range of 14–47 years in one study15 to 17–28 years in another study.17 The mean age in this review was 24.8 years which is representative of the population affected by scaphoid injuries. None of the recruited patients was older than 47 years so it was difficult to assess the applicability of rigid screw fixation without bone grafting for higher age group. Only one study by Somerson et al. 201514 looked at the correlation between age and poor results. It showed that increasing age resulted in lower self-assessed outcomes but not affecting fracture healing time as both unhealed patients sustained proximal pole fracture and a duration of >1 year from injury to surgery. Two more unhealed patients in Capo et al. 201215 and Gurger et al. 2018,12 the first with sickle cell anaemia required revision fixation with grafting after failure and no information provided about the second one. In general, among the four patients who failed to show union the poor results was related to other factors rather than age.
There were some differences between the included studies in their inclusion criteria. For example, and unlike the other studies, Mahmoud and Koptan 201016 included well-aligned scaphoid non-union with specifically bone resorption≥2 mm. This study showed no correlation between gap size and mean time to union. Even non-union with a gap between 2 and 7 mm have the biological ability to heal without bone grafting as long as carpal alignment and mechanical stabilization are maintained.
The main determining factor in time to heal was the delay between injury and surgical intervention. Mahmoud and Koptan, 201016 and Somerson et al., 201514 noted that scaphoid non-unions that were operated upon in less than one year after injury had shorter mean time to union. Slade et al., 200317 reported similar results as fractures operated within 6 months after injury showed a shorter time to union (10.8 weeks) compared to 16 weeks in those treated later (p < 0.02).
With respect to the anatomic location of fractures, 3 studies (13, 15 & 16) included only scaphoid waist fracture and 2 studies (12 & 14) included both proximal one third and waist fractures. There were no clearly reported data in the previous studies on the effect of the anatomical site of non-union on the functional and radiological outcomes. However, in Somerson et al. 201514 and Gurger et al. 201812 both proximal 1/3 and waist non-union had similar healing rate and post-operative functional outcomes.
The current review has several limitations which could affect the overall results. First limitation is the high risk of selection and reporting bias as all the included studies were case series. Secondly, the relatively small number of trials and participants in the included studies could affect the external validity of the review. Finally, the lack of control group in these case series could make it difficult to draw a firm conclusion. Therefore, there is a need of future well designed studies with good methodology and large number of participants to draw a solid conclusion about the effectiveness of rigid fixation without bone grafting in the treatment of stable well-aligned scaphoid non-unions.
5. Conclusion
Overall, this review demonstrates favourable functional outcomes and improve range of movements in selected cases of scaphoid non-union which were treated with rigid fixation without bone grafting. In addition, the reviewed studies reported high union rate with this technique. However, these results should be interpreted with caution because of the inherent limitation of the included studies. Adequately powered clinical studies with robust methodology are essential to draw an accurate conclusion.
Disclaimer
The authors declare that no part of this study has been taken from existing published or unpublished materials without due acknowledgement and that all secondary materials used herein has been fully referenced.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Mohammed Elmajee, Email: Mohammedelmajee@doctors.net.uk.
Ahmed Aljawadi, Email: ahmed.aljawadi@mft.nhs.uk.
References
- 1.Kozin S.H. Incidence, mechanism, and natural history of scaphoid fractures. Hand Clin. 2001;17(4):515. [PubMed] [Google Scholar]
- 2.Hove L.M. Epidemiology of scaphoid fractures in Bergen, Norway. Scandinavian journal of plastic and reconstructive surgery and hand surgery/Nordisk plastikkirurgisk forening [and] Nordisk klubb for handkirurgi. 1999;33(4):423. doi: 10.1080/02844319950159145. [DOI] [PubMed] [Google Scholar]
- 3.Buijze G.A., Ochtman L., Ring D. Management of scaphoid nonunion. J Hand Surg. 2012;37(5):1095–1100. doi: 10.1016/j.jhsa.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Kawamura K., Chung K.C. Treatment of scaphoid fractures and nonunions. J Hand Surg. 2008;33(6):988. doi: 10.1016/j.jhsa.2008.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capo J.T., Orillaza N.S., Jr., Slade J.F., III Percutaneous management of scaphoid nonunions. Tech Hand Up Extrem Surg. 2009;13(1):23–29. doi: 10.1097/BTH.0b013e3181877644. [DOI] [PubMed] [Google Scholar]
- 6.Al-Jabri T., Mannan A., Giannoudis P. The use of the free vascularised bone graft for nonunion of the scaphoid: a systematic review. J Orthop Surg Res. 2014;9(1):21. doi: 10.1186/1749-799X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capo J.T., Shamian B., Rizzo M. Percutaneous screw fixation without bone grafting of scaphoid non-union. Isr Med Assoc J. 2012;14(12):729–732. [PubMed] [Google Scholar]
- 8.Hegazy G. Percutaneous screw fixation of scaphoid waist fracture non-union without bone grafting. Journal of hand and microsurgery. 2015;7(2):250–255. doi: 10.1007/s12593-015-0194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooney W.P., Bussey R., Dobyns J.H., Linscheid R.L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 10.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Bland J.M., Kerry S.M. Weighted comparison of means. BMJ. 1998;316(7125):129. doi: 10.1136/bmj.316.7125.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurger M., Yilmaz M., Yilmaz E., Altun S. Volar percutaneous screw fixation for scaphoid nonunion. Niger J Clin Pract. 2018;21(3):388. doi: 10.4103/njcp.njcp_24_17. [DOI] [PubMed] [Google Scholar]
- 13.Cha J.K., Park J.K., Choi S.M., Yang J.Y. Bone grafting for scaphoid waist nonunion under local anesthesia. J Korean Soc Surg Hand. 2017;22(2):89–95. [Google Scholar]
- 14.Somerson J.S., Fletcher D.J., Srinivasan R.C., Green D.P. Compression screw fixation without bone grafting for scaphoid fibrous nonunion. Hand. 2015;10(3):450–453. doi: 10.1007/s11552-015-9741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Capo J.T., Shamian B., Rizzo M. Percutaneous screw fixation without bone grafting of scaphoid non-union. Isr Med Assoc J: IMAJ. 2012;14(12):729–732. [PubMed] [Google Scholar]
- 16.Mahmoud M., Koptan W. Percutaneous screw fixation without bone grafting for established scaphoid nonunion with substantial bone loss. J Bone Joint Surg Br. 2011;93(7):932–936. doi: 10.1302/0301-620X.93B7.25418. [DOI] [PubMed] [Google Scholar]
- 17.SLADE J.F., III, Geissler W.B., Gutow A.P., Merrell G.A. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. JBJS. 2003;85:20–32. doi: 10.2106/00004623-200300004-00003. [DOI] [PubMed] [Google Scholar]
- 18.Veenhof C., Dekker J., Bijlsma J.W., Van Den Ende C.H. Influence of various recruitment strategies on the study population and outcome of a randomized controlled trial involving patients with osteoarthritis of the hip or knee. Arthritis Care Res: Official Journal of the American College of Rheumatology. 2005;53(3):375–382. doi: 10.1002/art.21171. [DOI] [PubMed] [Google Scholar]