Abstract
Introduction: Lockdowns are designed to slow COVID-19 transmission, but they may have unanticipated relationships with other aspects of public health. Assessing the overall pattern in population health as a country implements and relaxes a lockdown is relevant, as these patterns may not necessarily be symmetric. We aimed to estimate the changing trends in cause-specific mortality in relation to the 2020 COVID-19 related lockdowns in Peru. Methods: Based on data from the Peruvian National Death Information System (SINADEF), we calculated death rates per 10 million population to assess the trends in mortality rates for non-external and external causes of death (suicides, traffic accidents, and homicides). We compared these trends to 2018-2019, before, during, and after the lockdown, stratified by sex, and adjusted by Peruvian macro-region (Lima & Callao (capital region), Coast, Highland, and Jungle). Results: Non-external deaths presented a distinctive pattern among macro-regions, with an early surge in the Jungle and a later increase in the Highland. External deaths dropped during the lockdown, however, suicides and homicides returned to previous levels in the post-lockdown period. Deaths due to traffic accidents dropped during the lockdown and returned to pre-pandemic levels by December 2020. Conclusions: We found a sudden drop in external causes of death, with suicides and homicides returning to previous levels after the lifting of the lockdown. Non-external deaths showed a differential pattern by macro-region. A close monitoring of these trends could help identify early spikes among these causes of death and take action to prevent a further increase in mortality indirectly affected by the pandemic.
Keywords: COVID-19, Lockdown, Suicide, Traffic accidents, Homicides, Mortality
Introduction
Many countries have used lockdowns as a primary non-pharmaceutical intervention during the COVID-19 pandemic, aiming to control and stop the spread of the disease, and to prevent a health system overflow [1,2]. While lockdowns have shown to be effective to sustain reductions of the infection rates [3], and deaths due to COVID-19 [4-6], they may also have unintended consequences in emotional, social, and economic spheres, and could also impact other causes of death and aspects of public health, such as violence, crime, and mental health [7-13].
Initial reports have shown that minor crime offenses decreased in the US during the lockdown, however, serious crimes (eg, homicide and intimate partner violence) have either remained constant or increased [14]. A study in Mexico has described a similar pattern, with a decline in conventional crime but with a steady trend of homicides during the pandemic [15]. Violence against women, including feminicides, has also been of great concern during the pandemic [16-18].
The lockdowns have also impacted mental health, with an increase in awareness for suicide prevention during the pandemic [19]. The COVID-19 pandemic has been associated with moderate-to-severe anxiety, depression, sleep disturbances, and suicidal ideation [20-22]. Although several countries have reported multiple cases of COVID-19-related suicides [23], these events seem to have declined in some regions. In Japan, one study found that the suicide rate declined by 13.5% since the beginning of the pandemic and subsequent containment measures [24]. Similarly, an early Peruvian study conducted by this group, showed that violent deaths, including suicide, declined during the COVID-19 lockdown period [25].
As countries gradually emerge from lockdowns, there is a need to study and understand how population health patterns have changed during the different phases of the pandemic. Our previous study focused on the immediate effect after entering the lockdown on external deaths [25]. The present study aims to expand on this by describing the trends in non-external (disease related), and external causes of death, including homicides, suicides, and traffic accidents. We further expand on the previous study by focusing not only on patterns before and during the national lockdown, but further analyzing what happened after the reopening of economic activities in Peru. Although Peru was praised for having an early response during the pandemic [26,27], by September 2020 it ranked first in COVID-19 mortality among populous countries, with more than 950 deaths per million population [28] while by December 2020, Peru presented the highest excess mortality with 2900 excess deaths per million inhabitants [29].
Materials and Methods
Database
This is a descriptive study based on the Peruvian National Death Information System (SINADEF) [30]. This open database collects death certificates filed by healthcare professionals nationwide and has been running since 2017. SINADEF has improved the quality and coverage of the data in the recent years covering nearly 80% of death certificates in the national territory [31]. In this study, we will focus on nationwide information on deceased adults (18 years old or older) from January 1st to December 31st for 2018, 2019, and 2020. Although there are data available for 2017, we decided to exclude it given that this was the first year that the SINADEF was implemented, and the coverage was not optimal in many regions [32]. Given the lag in the reporting to the system, we evaluated delays in reporting by downloading the official database daily and comparing the number of records for 25 days. During this process, we determined that the total number of records for a given date does not change by more than 1% after 15 days. For this study, we used the database published on February 10th, 2021, to make reliable calculations on complete data through December 31st.
Lockdown
Peru reported its first case of COVID-19 on March 6th, 2020. Ten days later, on March 16th, the Peruvian government declared a state of sanitary emergency, closing its international borders and suspending economic, academic, and social activities across the entire country of 32 million people (20 million adults). Essential activities including food supply, pharmacies, and banking remained active. Moreover, military and police patrolled the streets to reinforce the lockdown, and a curfew was instituted from 8 pm to 5 am and for a full 24 hours on Sundays. Public transport capacity was reduced by half, and movement between regions within the country was banned [33].
The de-escalation plan for the COVID-19 lockdown and the reopening of economic activities in Peru encompassed four different phases. Phase 1 began in May 2020, including the resumption of activities such as mining, construction, commerce, and services related to tourism such as restaurants and hotels [34]. Phase 2 started in June and expanded the reopening of activities to agriculture, manufacturing, and professional services [35]. Phase 3 started on July 1st, and gradually incorporated almost 100% of productive activities, including the reopening of retail stores and the lift of the lockdown. By July 15th, air transport activities at the national level and services related to air transportation were resumed, and the lockdown was lifted in 18 of 25 regions. In the remaining seven regions (mostly in the Highland), with rising infection rates, lockdowns persisted until July 31st. The curfew was also reduced to the interval from 10:00 pm to 4:00 am including Sundays [36]. Phase 4 started in October 1st, with an increase in the capacity of restaurants to 50% and retail stores to 60%, while the reopening of international borders and international air travel started in October 5th with the resumption of flights to six countries in the Americas region [37]. An annotated timeline is available in Appendix A: Supplementary Figure 1.
Because Phase 3 marked an important milestone during the pandemic due to the greatest economic reopening of activities and the lifting of the lockdown, we decided to divide the study period into three intervals: (1) pre-lockdown: January through March 15th; (2) lockdown itself: March 16th through June 30th; and (3) post-lockdown, July 1st to December 31st.
Outcomes
The primary outcome of this study are mortality rates per 10 million of non-external causes of death and external causes of death. Non-external causes of death encompass all diseases or underlying medical conditions, including communicable, maternal, neonatal, nutritional, and all non-communicable diseases. External causes of death include suicides, homicides, and traffic accidents, and other types of accidental injury. The classification between non-external and external cause of death and the specification of each type of external cause of death are reported in an independent item in the death certificate. This item was used to identify the type of death, obviating the need to use the International Classification of Diseases (ICD) 10 coding, which is underreported in the death certificates [31].
Because the relatively low count of daily external deaths, we chose to aggregate the data in bins of 15 days each to have a uniform time unit throughout our study period.
To have a measure of mobility and compliance during the lockdown we used data from the mobile-phone mobility data provided by Google Community Mobility Reports. This mobility report uses anonymized data provided by Google services, such as Google Maps or Google Search, to measure visitor numbers to specific categories of location including residential areas and transit stations. The mobility report provides the relative change per day compared to a baseline value for that day of the week before the pandemic outbreak [38].
Statistical Analysis
Due to the differences in mortality between regions, we grouped the 25 regions of Peru into four macro-regions based on the main Peruvian ecosystems and the major capital cities of the country accounting for one-third of the population: (1) Lima & Callao (capital region), (2) Coast (costa), (3) Highland (sierra), and (4) Jungle (selva) [39,40]. See Appendix A: Supplementary Table 1 for the definition of these regions.
To assess the change in the trends of mortality, before, during and after the of COVID-19 lockdown we compared the mortality trends per 10 million population for non-external deaths and for external-deaths during the time bins of 2020 to their counterparts of the years 2018 and 2019. For non-external deaths, the analysis was stratified by sex and macro-region. Since the low number of external deaths does not allow for the examination of stratified trends by region, the analysis was adjusted by macro-region population and stratified by sex. Because the macro-regions present the peaks of the pandemic at different times and not necessarily consistent with the lockdown times, we also decided to evaluate the mortality trends before and after the date of the first 5000/10 million non-external deaths among macro-regions.
Non-external deaths are presented in scatter plots with a LOESS smoother with a 0.3 span, while external deaths are presented with a linear fit per study period. The analysis was conducted using R 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Non-external Causes of Death
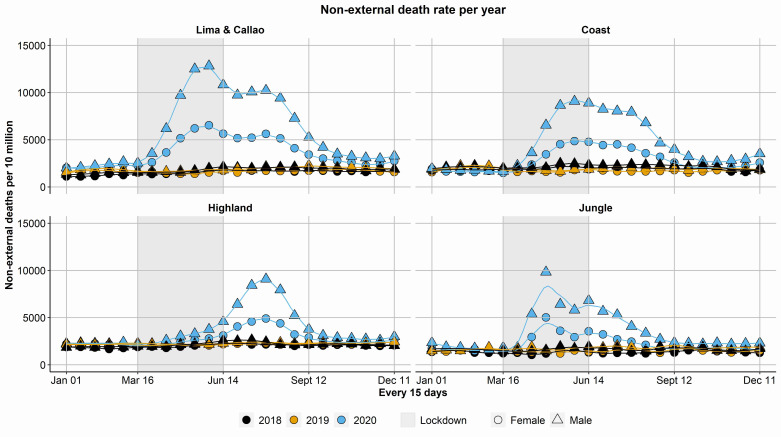
Among the four macro-regions the baseline trends for non-external causes of death were consistent at about 1000 deaths per 10 million per 15 days during the years 2018 and 2019, without any major difference by sex or year. In 2020, there was an increase in mortality that occurred at different times among macro-regions. The first macro-region to reach the pandemic peak was the Jungle at around 6 weeks after the implementation of the lockdown, followed by Lima & Callao at around 12 weeks, the Coast at 13 weeks. The Highland presented its pandemic peak 20 weeks after the implementation of the lockdown, 5 weeks following the lift of the nationwide lockdown (Figure 1).
Figure 1.
Mortality from non-external causes per macro-region by year and sex. The fitted line is from a LOESS smoother with bandwidth = 0.3.
The ratio of deaths per 10 million per week between men and women was around 1:1 during the baseline years, however, during the pandemic peak, this ratio was 2:1 across all macro-regions (Appendix A: Supplementary Figure 2).
External Causes of Death
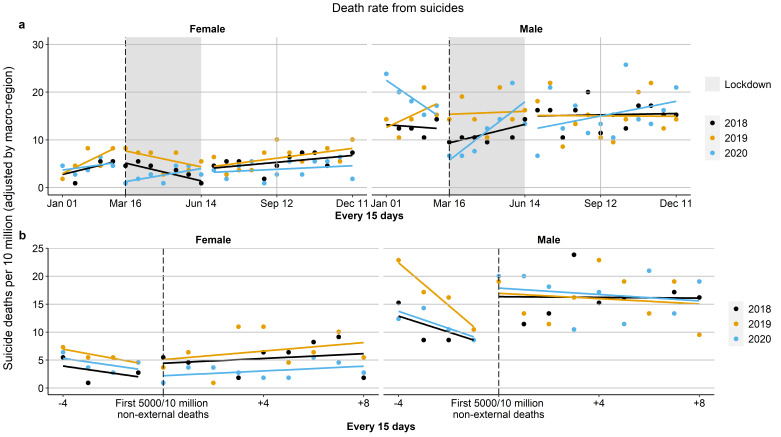
Suicides appeared to have a slight drop compared to previous years during the first weeks of the lockdown for both men and women, especially compared to 2019. In the post-lockdown period, the levels of suicide appear to have returned to the previous year’s baseline levels by the end of the year (Figure 2A, Appendix A: Supplementary Table 2). The change in the trends after the first 5000/10 million non-external deaths also shows a slight decrease in suicides in the immediate time after, mainly in women, which eventually returns to levels close to those of previous years (Figure 2B, Appendix A: Supplementary Table 2).
Figure 2.
Suicide death rate by sex and year adjusted by macro-region. Panel (a) shows the death rate dividing the study period based on the grey-shaded lockdown period. Panel (b) shows the death rate dividing the study period based on the first 5000/10 million non-external deaths. In both panels, solid lines represent best linear fit.
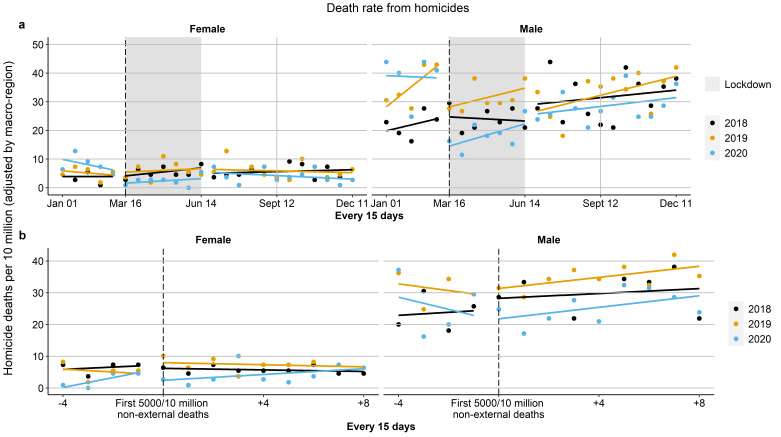
Homicides in 2020 presented the highest levels in the pre-lockdown period. However, during the first week of the lockdown, the number of homicides slightly dropped, with a greater reduction in men (from 39 homicides per 10 million population (95% CI: 30.4, 49.5) to 15 (95% CI: 10.8, 20.8)) compared to women (from 10 homicides per 10 million population (95% CI: 5.9, 15.9) to 1.6 (95% CI: 0.5, 3.9)). During the post-lockdown period the level of homicides in women approached the level of previous years (5 homicides per 10 million population (95% CI: 3.0, 8.2)), while homicides in men remained slightly below the level of previous years (26 homicides per 10 million population (95% CI: 10.8, 20.8)) (Figure 3A, Appendix A: Supplementary Table 3). After the first 5000/10 million non-external deaths the change in homicides in women is less noticeable, however the reduction in men persisted especially when compared to 2019 (Figure 3B).
Figure 3.
Homicide death rate by sex and year adjusted by macro-region. Panel (a) shows the death rate dividing the study period based on the grey-shaded lockdown period. Panel (b) shows the death rate dividing the study period based on the first 5000/10 million non-external deaths. In both panels, solid lines represent best linear fit.
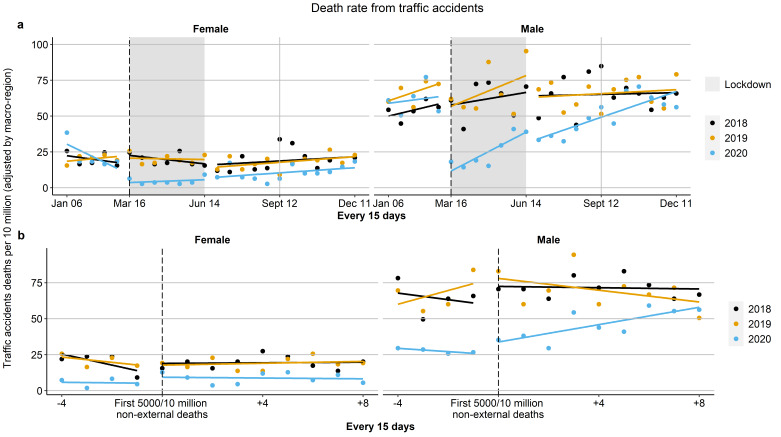
Traffic accident deaths presented the biggest drop among external causes of death. The marked reduction is clearly noticeable during the lockdown period, from 31 deaths per 10 million population (95% CI: 23.1, 41.2) to 3.7 (95% CI: 1.8, 6.8) in women and from 59.5 (95% CI: 48.7, 72.0) to 13.5 (95% CI: 9.7, 18.5) in men. Furthermore, this reduction remained in the post-lockdown period for both men and women, 8 deaths per 10 million population (95% CI: 5.3, 10.8) in women and 35.8 (95% CI: 30.2, 42.0) in men, although the trend in men appears to be steeper and reached pre-pandemic levels by the end of 2020 (Figure 4A, Appendix A: Supplementary Table 4). When the trends were compared after the first 5000/10 million non-external deaths, this reduction was similar (Figure 4B).
Figure 4.
Traffic accidents death rate by sex and year adjusted by macro-region. Panel (a) shows the death rate dividing the study period based on the grey-shaded lockdown period. Panel (b) shows the death rate dividing the study period based on the first 5000/10 million non-external deaths. In both panels, solid lines represent best linear fit.
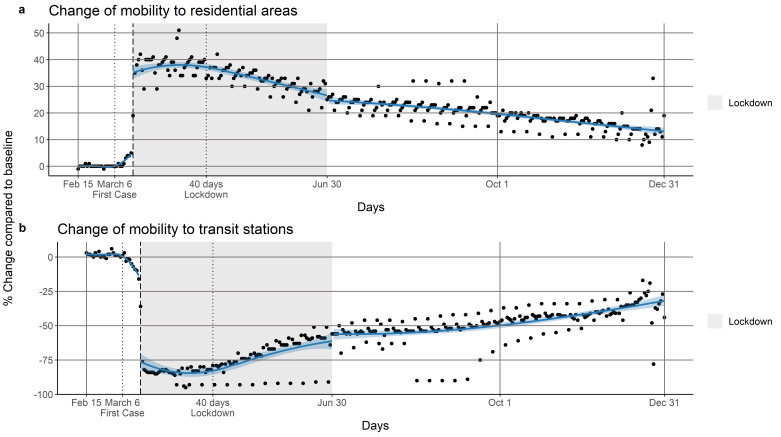
During the first 40 days of the lockdown the mobility to transit stations was reduced by 80% and the mobility to residential areas increased by around 40%. After 40 days, the mobility to transit stations increased to nearly half its average pre-pandemic level, and the mobility to residential areas decreased to 20%. In post-lockdown period, both mobility trends remained constant without further change towards the baseline values. However, there is not a clear change in the trend around the lifting of the lockdown (Figure 5).
Figure 5.
Panel (a) shows the percentage change in community mobility to residential areas before, during and after the lockdown period. Panel (b) shows the percentage change in community mobility to transit stations before, during and after the lockdown period. In both panels, the grey area represents the lockdown. The first vertical black dotted line corresponds to the first confirmed case and the second dotted line the 40th-day of the lockdown. The vertical black dashed line marks the beginning of the lockdown (March 16, 2020). The solid blue line shows a LOESS smoother with bandwidth = 0.6 and the blue shading corresponds to the pointwise 95% confidence limits for the smoothed line.
Discussion
This study has described the different trends in mortality due to external and non-external causes of death before, during, and after the COVID-19-related lockdown of Peru. The increased mortality due to the COVID-19 pandemic is evident in the trends in non-external causes of death, which peaked at different times in different regions of the country.
The first COVID-19 case in the Peruvian Jungle was detected on March 17th, one day after the nationwide lockdown. This first case was apparently a tour guide who was infected by foreign tourists [41]. Due to the inadequate health system in the region and the limitation in accessibility for supplies, as there are no roads connecting the main cities in the Jungle with the rest of Peru and flights were grounded as part of the lockdown, this region was the first to be hit most dramatically by the pandemic in Peru [41]. Furthermore, according to a local serologic study conducted in July, in one of the biggest cities in the Jungle region, the cumulative incidence of COVID-19 infection was 71%, being among the highest reported worldwide [42]. However, recent research in Brazil has shown that these seroprevalence values may be overestimated by cross-reactivity of dengue virus (DENV) antibodies with SARS-COV-2 antibodies [43].
Lima & Callao were the next region to be impacted by the pandemic with a regrowth in the number of deaths two weeks after the lockdown ended (Appendix A: Supplementary Figure 3). This increase in deaths is consistent with an increase in mobility (Figure 5) after around 40 days of lockdown, which may be behind this increase. However, this acceleration in mobility was slowed shortly after lifting the lockdown. This might be due to the reinforcement of protective campaigns that encouraged people to stay at home and limit family gatherings. Likewise, the curfew on Sundays had to be resumed in mid-August as a measure to control the increasing rates of COVID-19 infection.
The Highland was the macro-region that presented the last pandemic peak, potentially linked to the reopening of inter-regional air travel, which restarted 2 weeks after the nationwide lockdown was lifted [44]. As shown in Appendix A: Supplementary Figure 5, many of the regions in the Highlands presented higher levels of mortality weeks after the nationwide lockdown was lifted, with the subsequent need to prolong the confinement in these regions for an extra month.
Mental health has been of great concern during the COVID-19 pandemic, with a special focus on suicide prevention [45]. We have shown a decrease in suicide in both men and women right after the start of the lockdown, with the numbers of suicides getting closer to previous years levels as the lockdown was coming to an end. In the post-lockdown period, suicide levels have not exceeded those of previous years. Although many studies have pointed out that risk factors for suicide may be aggravated during the lockdown [46-50], this should be contrasted with the actual acts of suicide as observed in the population. Due to intrinsic characteristics of the lockdown in Peru, such as limited mobility, police patrolling, and strict curfew, access to the usual means to commit suicide might have been hampered. A study conducted in Peru describing the characteristics of suicide intentions, found that more than 50% were planned based on the use of carbamate-based poison while 38% based on benzodiazepines [51], and access to these substances may have been limited during the lockdown. Another potential suicide deterrent may be decreased time living alone during the lockdown, as living alone is a risk factor for committing suicide [52,53].
This pattern of decline in suicides has also been reported in Japan, with a reduction of about 15% after the start of the pandemic [24]. In the same way, Karnataka, India, reported a decline of nearly half the number suicides during the lockdown, compared to the early months of 2020. However, after the lockdown was completed, the number of suicides rose by 20% [54], contrary to what we observed in Peru. Although actual acts of suicide might have resumed to levels comparable to previous years in our study population, we recognize that we are still in an early stage of the pandemic and long-term preventive measures should be kept in place.
Homicides have also been a focus of great concern during the pandemic. In Mexico, homicides related to organized crime remained steady during the pandemic [15], while in the US homicide rates decreased during April and May of 2020 compared with the previous 3-year average, with the highest decreased in April [55]. However, by the end of June, initial reports in the US have shown a surge of homicides, with a 6% increase compared to previous years [56]. These increases should be put in context with recent surges in domestic terrorism from white supremacists in the US [57] and racially motivated police killings and unrest from associated protests [58].
In our study population, we have shown that homicides in 2020 presented the highest levels in the pre-lockdown period compared with previous years. Although Peru is one of the countries with the lowest homicide rates in the region, these rates have been increasing from 5.4 per 100,000 habitants in 2011 to nearly 8 per 100,000 habitants in 2018 [59]. These increases are potentially related to increases in crime, especially in the last 2 years [60]. Annually, about a third of the population is the victim of some criminal act, furthermore, the percentage of crimes committed with a firearm has increased from 7% in 2013 to 11% in 2019 [60]. While we have shown a slight decrease in homicides during the lockdown, homicide rates have returned to baseline levels in the post-lockdown period.
Although most homicides in men might be related to crime, homicides in women have been related to violence against women [61,62]. Early data from the US police departments from various cities have revealed an increase in police reports and calls due to domestic violence during March 2020 compared to previous years [63]. In the same way, the United Nations (UN) has reported an increase of domestic violence in France, Argentina, and Singapore based on calls to help lines and police reports [17]. In Mexico, a study found that crimes against women, reported to national services, presented a drop at the beginning of the stay-at-home order, and later returned to pre-pandemic levels. However, they found that feminicides remained constant and only decreased in those places where there was a restriction on the sale of alcohol [18].
Although we have shown a decrease in homicides among women during the early weeks of the lockdown, the levels of homicides in women in the post-lockdown period have returned to levels similar to those in previous years. This trend is consistent with the reports by the Ministry of the Women, which show a marked decrease in feminicides since the pandemic, compared to previous years [64]. Early data from Peru, collected from calls to the National hotline help service, has also shown an increased demand of support services during the lockdown with a slight decrease 1 month after the lockdown was lifted [64].
The relaxation of some measures such as constant patrolling or the curfew, added to the increase in mobility, could have contributed to the increase in feminicides after the lifting of the lockdown. However, one aspect that remains understudied is the increase in the number of missing women: during the pandemic, 62% of missing persons were women according the National Police Department [65]. Although there is no reliable data due to deficiencies in the reporting system, different government institutions have issued alerts regarding the large number of reports of missing persons that have been made during the lockdown compared to previous years [65]. This unfortunately shows that part of the decrease in the number of registered feminicides could be offset by the increase in missing women.
The most severe change during the pandemic were deaths from traffic accidents. This decline in mortality levels is closely related to the decline and mobility patterns during and after the pandemic. Although the mobility patterns have not fully returned to the baseline levels, the death rates due to traffic accidents reached pre-pandemic levels by the end of 2020.
This descriptive analysis at the national level is one of the first reports that attempts to describe the entire picture of the trends of different causes of mortality during the course of the pandemic, and it is subject to some limitations. The determination of the time when the lockdown was lifted and the measures that have continued to be taken to stop the advance of COVID-19 have not been clear. Although we have presented the results based on the lifting of the lockdown at the national level, a gradient of various measures has been presented at different times that could have affected the trends in mortality in some ways. Another important point to take into account is the quality and coverage of records, which used to be a large cause of concern when using Peruvian vital registration data due to the presence of severe under-registration of deaths [32]. However, with the new SINADEF system, coverage has improved drastically, and a previous study has shown no major change in quality during the pandemic [66]. A second important aspect of data quality is delayed registration of deaths. However, we checked the number of records by date of death in serial downloads of the SINADEF data and found that after 15 days the number of records was essentially complete (>99%). We also did not check for specific causes of death among non-external causes of death, to avoid issues with quality of coding and limited testing capacity to identify COVID-19 deaths. Therefore, we found total mortality as a reliable source for monitoring mortality during COVID-19, as reported in other studies [67]. Future studies should also focus on evaluating the impact of sets of policies to assess concomitant interventions to the lockdown, considering the potential for reverse causality and the different effects of these interventions over time [68].
Conclusions
Peru has one of the highest mortality rates from COVID-19 and there is still much to understand about the indirect impact of the pandemic and the measures taken to control it on different causes of death. Non-external deaths presented different patterns in relation to time and the level of mortality among the different macro-regions in Peru, with the Jungle being the earliest affected region and the Highlands being the latest one. Suicides and homicides presented an early drop during the first weeks of the lockdown, followed by a return to previous levels in the post-lockdown period. Deaths due to traffic accidents fell during the lockdown and remained low in the post-lockdown period only to reach baseline levels again at the end of 2020. With the ongoing second wave of the COVID-19 pandemic, close monitoring and description of these trends could help identify early changes and take action to prevent higher rates of death.
Glossary
- SINADEF
Peruvian National Death Information System
Appendix A.
Author Contributions
RCA: Conception and design; Data Analysis; Writing; Review and Editing. UB: Conception and design; Review and Editing. JK: Conception and design; Review and Editing.
Funding
RCA was supported by a Tomlinson Doctoral Fellowship by McGill University, and UB was supported by the Office of the Director of the National Institutes of Health under award number DP5OD26429. The funding sources had no role in the analysis, writing or decision to submit the manuscript. No other funding was received.
References
- Killeen GF, Kiware SS. Why lockdown? Why national unity? Why global solidarity? Simplified arithmetic tools for decision-makers, health professionals, journalists and the general public to explore containment options for the 2019 novel coronavirus. Infect Dis Model. 2020. July;5:442–58. 10.1016/j.idm.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak [Internet]. J Travel Med. 2020. March;27(2):taaa020. [cited 2020 Sep 22] Available from: http://academic.oup.com/jtm/article/27/2/taaa020/5735321 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano V, Ercolano S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl Health Econ Health Policy. 2020. August;18(4):509–17. 10.1007/s40258-020-00596-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhry R, Dranitsaris G, Mubashir T, Bartoszko J, Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes [Internet]. EClinicalMedicine. 2020. August;25:100464. [cited 2020 Sep 22] Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30208-X/abstract 10.1016/j.eclinm.2020.100464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiang S, Allen D, Annan-Phan S, Bell K, Bolliger I, Chong T, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020. August;584(7820):262–7. 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- Flaxman S, Mishra S, Gandy A, Unwin HJ, Mellan TA, Coupland H, et al. Imperial College COVID-19 Response Team. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020. August;584(7820):257–61. 10.1038/s41586-020-2405-7 [DOI] [PubMed] [Google Scholar]
- Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2020. April;0:1–2. 10.1080/09638237.2020.1757052 [DOI] [PubMed] [Google Scholar]
- Bullinger LR, Carr JB, Packham A. COVID-19 and Crime: Effects of Stay-at-Home Orders on Domestic Violence [Internet]. National Bureau of Economic Research; 2020. [cited 2020 Sep 22]. Report No.: 27667. Available from: http://www.nber.org/papers/w27667
- Bhuiyan AK, Sakib N, Pakpour AH, Griffiths MD, Mamun MA. COVID-19-Related Suicides in Bangladesh Due to Lockdown and Economic Factors: Case Study Evidence from Media Reports. Int J Ment Health Addict. 2020. May:1–6. 10.1007/s11469-020-00307-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HH, Lin SH. Effects of COVID-19 Prevention Measures on Other Common Infections, Taiwan. Emerg Infect Dis. 2020. October;26(10):2509–11. 10.3201/eid2610.203193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly R, Farina MP. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Soc Sci Med 1982. 2021;269:113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray MJC, Daneshvari NO, Radhakrishnan I, et al. Racial Differences in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug N, Geyrhofer L, Londei A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. 2020. December;4(12):1303–12. 10.1038/s41562-020-01009-0 [DOI] [PubMed] [Google Scholar]
- Boman JH, Gallupe O. Has COVID-19 Changed Crime? Crime Rates in the United States during the Pandemic. Am J Crim Justice AJCJ; 2020. pp. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balmori de la Miyar JR, Hoehn-Velasco L, Silverio-Murillo A. Druglords Don’t Stay at Home: COVID-19 Pandemic and Crime Patterns in Mexico City [Internet]. Rochester, NY: Social Science Research Network; 2020. [cited 2020 Sep 22]. Report No.: ID 3667160. Available from: https://papers.ssrn.com/abstract=3667160 [DOI] [PMC free article] [PubMed]
- Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during covid-19 pandemic restrictions [Internet]. BMJ. 2020. May;369:m1712. [cited 2020 Sep 22] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202944/ 10.1136/bmj.m1712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNWomen . COVID-19 and ending violence against women and girls. New York. https://www.unwomen.org/-/media/headquarters/attachments …; 2020.
- Hoehn-Velasco L, Silverio-Murillo A, Balmori de la Miyar JR. COVID-19 and Crimes Against Women: Evidence from Mexico [Internet]. Rochester, NY: Social Science Research Network; 2020. [cited 2020 Oct 13]. Report No.: ID 3701472. Available from: https://papers.ssrn.com/abstract=3701472
- Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. COVID-19 Suicide Prevention Research Collaboration. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020. June;7(6):468–71. 10.1016/S2215-0366(20)30171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H, Zhang Y, Kong D, Li S, Yang N. Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Med Sci Monit. 2020. March;26:e923921. 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020. March;33(2):e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China [Internet]. Int J Environ Res Public Health. 2020. March;17(5):1729. [cited 2020 Sep 22] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7084952/ 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM Int J Med [Internet]. [cited 2020 Sep 22]; Available from: https://academic.oup.com/qjmed/advance-article/doi/10.1093/qjmed/hcaa202/5857612 [DOI] [PMC free article] [PubMed]
- Tanaka T, Okamoto S. Suicide during the COVID-19 pandemic in Japan. medRxiv. 2020;2020.08.30.20184168.
- Calderon-Anyosa RJ, Kaufman JS. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med. 2021. February;143:106331. 10.1016/j.ypmed.2020.106331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CNN MC . Why didn’t Peru’s strict measures stop the coronavirus? [Internet]. CNN. [cited 2020 Oct 8]. Available from: https://www.cnn.com/2020/05/25/americas/peru-covid-hotspot-why-intl/index.html
- Peru: Coronavirus spreads despite strict and early measures - CNN [Internet]. [cited 2020 Oct 8]. Available from: https://edition.cnn.com/2020/05/25/americas/peru-covid-hotspot-why-intl/index.html
- Peru: WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [cited 2020 Sep 24]. Available from: https://covid19.who.int
- Karlinsky A, Kobak D. The World Mortality Dataset: Tracking excess mortality across countries during the COVID-19 pandemic. medRxiv [Internet]. 2021. [cited 2021 Feb 17]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7852240/ [DOI] [PMC free article] [PubMed]
- Información de Fallecidos del Sistema Informático Nacional de Defunciones - SINADEF - [Ministerio de Salud] | Plataforma Nacional de Datos Abiertos [Internet]. [cited 2020 Jul 2]. Available from: https://www.datosabiertos.gob.pe/dataset/informaci%C3%B3n-de-fallecidos-del-sistema-inform%C3%A1tico-nacional-de-defunciones-sinadef-ministerio
- Vargas-Herrera J, Ruiz KP, Nuñez GG, Ohno JM, Pérez-Lu JE, Huarcaya WV, et al. Resultados preliminares del fortalecimiento del sistema informático nacional de defunciones. Rev Peru Med Exp Salud Publica. 2018. Jul-Sep;35(3):505–14. 10.17843/rpmesp.2018.353.3913 [DOI] [PubMed] [Google Scholar]
- Vargas-Herrera J, Ruiz KP, Nuñez GG, Ohno JM, Pérez-Lu JE, Huarcaya WV, et al. Resultados preliminares del fortalecimiento del sistema informático nacional de defunciones. Rev Peru Med Exp Salud Publica. 2018. Jul-Sep;35(3):505–14. 10.17843/rpmesp.2018.353.3913 [DOI] [PubMed] [Google Scholar]
- Decreto Supremo N° 044-2020-PCM [Internet]. 2020. [cited 2020 Jul 2]. Available from: https://www.gob.pe/institucion/pcm/normas-legales/460472-044-2020-pcm
- Decreto Supremo N° 080-2020-PCM [Internet]. [cited 2020 Sep 24]. Available from: https://www.gob.pe/institucion/pcm/normas-legales/544911-080-2020-pcm
- Decreto Supremo N° 101-2020-PCM [Internet]. [cited 2020 Sep 24]. Available from: https://www.gob.pe/institucion/pcm/normas-legales/663350-101-2020-pcm
- Decreto Supremo N° 117-2020-PCM [Internet]. [cited 2020 Sep 24]. Available from: https://www.gob.pe/institucion/mtc/informes-publicaciones/850253-fase-3-de-la-reanudacion-de-las-actividades-economicas
- Decreto Supremo No 157-2020-PCM [Internet]. [cited 2020 Oct 9]. Available from: http://busquedas.elperuano.pe/normaslegales/decreto-supremo-que-aprueba-la-fase-4-de-la-reanudacion-de-a-decreto-supremo-n-157-2020-pcm-1888160-3/
- Google LL. Google COVID-19 Community Mobility Reports. [Internet]. [cited 2020 Jul 2]. Available from: https://www.google.com/covid19/mobility/data_documentation.html
- Peñaherrera del Aguila C, Mejia Baca J Geografía física del Perú. Gran geografía del Perú. [Google Scholar]
- Torres-Roman JS, Urrunaga-Pastor D, Avilez JL, Helguero-Santin LM, Malaga G. Geographic differences in overweight and obesity prevalence in Peruvian children, 2010-2015. BMC Public Health. 2018. March;18(1):353. 10.1186/s12889-018-5259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser B. COVID-19 strains remote regions of Peru. Lancet. 2020. May;395(10238):1684. 10.1016/S0140-6736(20)31236-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores J. César Cárcamo: Iquitos sería la primera ciudad del mundo en llegar a la inmunidad de rebaño [Internet]. RPP. 2020. [cited 2020 Sep 30]. Available from: https://rpp.pe/peru/actualidad/cesar-carcamo-iquitos-seria-la-primera-ciudad-del-mundo-en-llegar-a-la-inmunidad-de-rebano-noticia-1290694
- Nicolelis MA, Raimundo RL, Peixoto PS, et al. How super-spreader cities, highways, hospital bed availability, and dengue fever influenced the COVID-19 epidemic in Brazil. medRxiv. 2020. 10.1101/2020.09.19.20197749 [DOI]
- MTC . viajes interprovinciales iniciarán a partir del 15 de julio [Internet]. [cited 2020 Sep 30]. Available from: https://www.gob.pe/institucion/mtc/noticias/208665-mtc-viajes-interprovinciales-iniciaran-a-partir-del-15-de-julio
- Devitt P. Can we expect an increased suicide rate due to Covid-19? Ir J Psychol Med. :1–5. 10.1017/ipm.2020.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick KM, Harris C, Drawve G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide Life Threat Behav. 2020. December;50(6):1241–9. 10.1111/sltb.12655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero-Domínguez CC, Jiménez-Villamizar MP, Campo-Arias A. Suicide risk during the lockdown due to coronavirus disease (COVID-19) in Colombia. Death Stud. 2020. June:1–6. 10.1080/07481187.2020.1784312 [DOI] [PubMed] [Google Scholar]
- Dsouza DD, Quadros S, Hyderabadwala ZJ, Mamun MA. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020. August;290:113145. 10.1016/j.psychres.2020.113145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020. August;290:113104. 10.1016/j.psychres.2020.113104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witteveen D, Velthorst E. Economic hardship and mental health complaints during COVID-19. Proc Natl Acad Sci [Internet]. 2020. [cited 2020 Oct 13]; Available from: https://www.pnas.org/content/early/2020/10/09/2009609117 [DOI] [PMC free article] [PubMed]
- Coronado-Molina O. Características clínico-epidemiológicas y abordaje terapéutico de pacientes que acuden por intento suicida al Hospital General San José del Callao, Perú. Rev Neuropsiquiatr. 2014;77(4):242–9. 10.20453/rnp.v77i4.2198 [DOI] [Google Scholar]
- Lejoyeux M, Léon E, Rouillon F. [Prevalence and risk factors of suicide and attempted suicide]. Encephale. 1994. Sep-Oct;20(5):495–503. [PubMed] [Google Scholar]
- Kposowa AJ, Breault KD, Singh GK. White Male Suicide in the United States: A Multivariate Individual-Level Analysis. Soc Forces. 1995;74(1):315–25. 10.2307/2580634 [DOI] [Google Scholar]
- Karnataka sees grave rise in suicides post lockdown [Internet]. New Indian Express. [cited 2020 Sep 30]. Available from: https://www.newindianexpress.com/states/karnataka/2020/jul/10/ktaka-sees-grave-rise-in-suicides-post-lockdown-2167809.html
- Abt T, Rosenfeld R, Lopez E. COVID-19 and Homicide: Final Report to Arnold Ventures. 2020.
- Eligon J, Dewan S, Bogel-Burroughs N. In the Wake of Covid-19 Lockdowns, a Troubling Surge in Homicides. NY Times [Internet]. 2020. August 24 [cited 2020 Sep 30]; Available from: https://www.nytimes.com/2020/08/11/us/homicides-crime-kansas-city-coronavirus.html
- White Supremacist Terrorism PC. On The Rise And Spreading [Internet]. Forbes. [cited 2020 Oct 12]. Available from: https://www.forbes.com/sites/carlieporterfield/2020/06/25/white-supremacist-terrorism-on-the-rise-and-spreading/
- Weine S, Kohrt BA, Collins PY, Cooper J, Lewis-Fernandez R, Okpaku S, et al. Justice for George Floyd and a reckoning for global mental health [Internet]. Glob Ment Health (Camb). 2020;7:e25. [cited 2020 Oct 9] Available from: https://www.cambridge.org/core/journals/global-mental-health/article/justice-for-george-floyd-and-a-reckoning-for-global-mental-health/BD197ECD27C47F490002668C16B3088B 10.1017/gmh.2020.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estadística e Informática . Homicidios en el Perú, contándolos uno a uno 2011. Inf Estad. 2018;(7):2020. [Google Scholar]
- Instituto Nacional de Estadística e Informática . Estadísticas de Seguridad Ciudadana [Internet]. [cited 2021 Feb 18]. Available from: http://m.inei.gob.pe/media/MenuRecursivo/boletines/boletin_seguridad_ciudadana_departamental.pdf
- Drugs UNO on . Crime. Global Study on Homicide: Gender-related Killing of Women and Girls. UNODC, United Nations Office on Drugs and Crime; 2018. [Google Scholar]
- Motta A. La biología del odio. Retóricas fundamentalistas y otras violencias de género. Lima Siniestra; 2019. [Google Scholar]
- Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med [Internet]. 2020. [cited 2020 Sep 30];0. Available from: https://www.ajemjournal.com/article/S0735-6757(20)30307-7/abstract [DOI] [PMC free article] [PubMed]
- Orihuela Y. Portal Estadístico [Internet]. Portal Estad. [cited 2020 Oct 1]. Available from: https://portalestadistico.pe/
- La “epidemia silente” de la desaparición de mujeres en Perú (y cómo ha impactado el coronavirus). BBC News Mundo [Internet]. [cited 2020 Oct 1]; Available from: https://www.bbc.com/mundo/noticias-america-latina-53761324
- Calderon-Anyosa RJ, Kaufman JS. Impact of COVID-19 Lockdown Policy on Homicide, Suicide, and Motor Vehicle Deaths in Peru. medRxiv. 2020;2020.07.11.20150193. 10.1101/2020.07.11.20150193 [DOI] [PMC free article] [PubMed]
- Modig K, Ahlbom A, Matthews A. [Covid-19 - deaths and analysis]. Lakartidningen. 2020:117. [PubMed] [Google Scholar]
- Goodman-Bacon A, Marcus J. Difference-in-differences to identify causal effects of COVID-19 policies. Discussion Papers of DIW Berlin 1870, DIW Berlin, German Institute for Economic Research. 2020. 10.2139/ssrn.3603970 [DOI]