Abstract
Background: In December 2019, a viral outbreak occurred in China, and rapidly spread out worldwide. Due to the lack of immediately available vaccines and effective drugs, many policy- and decision-makers have focused on non-pharmacological methods, including social distancing. This study was aimed at assessing the effects of the implementation of this policy in Iran, one of the countries most affected by COVID-19. We conducted a quasi-experimental study, utilizing the interrupted time series analysis (ITSA) approach. Methods: We collected daily data between February 20, 2020 and January 29, 2021, through governmental websites from 954 public hospitals and healthcare settings. The Iranian government launched the social distancing policy on March 27, 2020. Statistical analyses, including ITSA, were carried out with R software Version 3.6.1 (London, UK). Results: During the study period, 1,398,835 confirmed incidence cases and 57,734 deaths occurred. We found a decrease of -179.93 (95% CI: -380.11 to -20.25, P-value=0.078) confirmed incidence cases following the implementation of the social distancing policy, corresponding to a daily decrease in the trend of -31.17 (95% CI: -46.95 to -15.40, P-value=0.08). Moreover, we found a decrease of -28.28 (95% CI: -43.55 to -13.01, P-value=0.05) deaths, corresponding to a daily decrease in the trend of -4.52 (95% CI: -5.25 to -3.78, P-value=0.003). Conclusion: The growth rate of confirmed incidence cases and deaths from COVID-19 in Iran has decreased from March 27, 2020 to January 29, 2021, after the implementation of social distancing. By implementing this policy in all countries, the burden of COVID-19 may be mitigated.
Keywords: pandemics, social distancing policy, COVID-19, Iran, interrupted time series analysis
Introduction
In late December 2019, a viral outbreak occurred in Wuhan, province of Hubei, People’s Republic of China, and rapidly spread out worldwide [1]. The World Health Organization (WHO) identified the infectious agent responsible for the “Coronavirus Disease 2019” (COVID-19) infection and termed it as “Severe Acute Respiratory Syndrome-related Coronavirus type 2” (SARS-CoV-2). As of January 30th, 2021, the virus has infected more than 101,406,059 people and killed approximately 2,400,000 people [2]. The WHO has declared COVID-19 a global pandemic, and the health systems of all countries are making their best efforts to curb the spread of COVID-19, to control and counteract/mitigate its burden and effectively treat patients [3]. In recent decades, many researchers have issued serious warnings about the problems and dangers that emerging infections can pose to human health [4]. The COVID-19 pandemic has caused a serious crisis affecting the public health systems, with many negative effects on the countries’ economies [5,6], including disruption of delivery of healthcare provisions for other diseases, especially the non-communicable ones, unemployment, declining household earnings, and national incomes funding the healthcare system [7,8].
Due to the lack of immediately available effective vaccines or drugs that could be used to prevent and treat COVID-19, respectively, public health policy- and decision-makers in many countries implemented various policies to reduce the effects of the disease, such as quarantine, self-restriction, social distancing, use of face masks, school and university closures, and travel restrictions [9,10]. Only recently, some vaccine products have been authorized. However, since they will not be immediately available for everybody, national allocation plans, based on prioritization-based strategies, are urgently needed. While many developed countries have already secured for themselves sufficient doses, most developing nations, including Iran, are still waiting for vaccine stocks [11].
COVID-19 in Iran
With the global spread of COVID-19, on February 19th 2020, the Ministry of Health and Medical Education (MOHME) announced the first cases in the city of Qom, near the Iranian capital [12]. Following this announcement, by the order of the President of Iran, the anti-Coronavirus headquarters were established under the leadership of the Minister of MOHME, in order to handle all COVID-19 related activities and policies [10].
With the spread of the disease in different cities of Iran, the educational activities of schools and universities were closed [13]. Then, a strict monitoring of the entry of passengers in domestic and foreign travels was implemented. Various awareness campaigns have been launched to reduce hours of social activity, encouraging people to stay home [10], including TV shows, mobile-based apps, phone calls and text messages targeting vulnerable groups, and involving celebrities and religious leaders [14,15]. Also, to curb the disease, the activities of specific manufacturers producing disinfectant liquids and gels, masks and personal protective equipment for the general public and service providers in health centers and hospitals increased eight-fold [10]. COVID-19 in Iran, like other countries, has been having a negative impact on various sectors. In the economic sector, the closure of several companies and factories has put people at risk of unemployment [15]. Although the government has tried to prevent people from becoming unemployed, people’s incomes fell, especially in connection with jobs whose activities were restricted and banned [16]. The most dramatic impact of COVID-19 on Iran’s economy has been in the oil export sector [17]. With all the borders closed, Iran’s oil export has plummeted. Most of Iran’s income comes from oil and petroleum products [14]. From the social dimension, the closure of universities and colleges has reduced the quality of education [18]. Moreover, many people in the community are suffering from stress and anxiety due to the illness or the fear of contracting the virus [19]. Social interactions between individuals and families have dramatically decreased in many cases [20].
Social Distancing Policy
Due to the transmission dynamics of COVID-19 through social interactions, reducing contact rates may play a role in disease prevention [21]. Countries such as People’s Republic of China, South Korea, Indonesia, and Hong Kong have pursued this policy and have been able to achieve positive results in reducing the transmission of the disease [22,23]. Due to the high prevalence and mortality of COVID-19, health policy-makers have decided to implement this policy to control the disease also in Iran [21].
The precise rules underlying the policy of social distancing vary according to the country in which the policy has been implemented. Distance can be one meter (in China, Hong Kong and Singapore, and in some European countries such as Denmark, France, and Lithuania), 1.4 meters (in South Korea), 1.5 meters (in Australia and in several European countries, including Belgium, Germany, Greece, Italy, Portugal, Spain and the Netherlands), 1.8 meters (in the US (six feet) and in Iran), and two meters (in Canada and in the UK) [24].
Social Distancing in Iran
On March 27th, 2020, Iran implemented a 1.8-meters social distancing policy in all Iranian cities to curb and further control the disease. The implementation of this policy was advocated by all political groups, organizations, society elites, celebrities, non-governmental organizations (NGOs), and militaries. Social networks (such as WhatsApp, Instagram, and Telegram, as well as Twitter, YouTube, and Facebook) have endorsed this policy and are supporting it by means of several campaigns [10]. The use of community and volunteer forces, the establishment of cohesive health networks in disadvantaged and underserved rural areas, and the formation of the COVID-19 National Headquarters were among the factors of the success of the implemented measure [7].
The Iranian President, as the country’s chief executive officer, took over the committee and the Health Minister was appointed to oversee the implementation of the various COVID-19 related programs [15]. After an initial surge in cases, public health authorities decided to implement social distancing and self-isolation policies [10]. To preserve the economy and essential businesses, jobs and economic/financial activities were subdivided into categories, based on the nature of services offered: category 1 included recreational activities or businesses providing health, economic/financial support, whereas category 4 included mostly non-recreational activities. Activities belonging to the first category remained open, while those belonging to category 4 underwent complete shut-down. Activities belonging to categories 2 and 3 could remain open and continue operating and providing services under certain strict conditions and protocols. Smart working was encouraged, by developing and enhancing ad hoc electronic infrastructure for service delivery [25]. There was initially no punishment for those who violated social distancing, but as the number of violations increased, the government decided to introduce penalties, with the highest fines being imposed on vehicles traveling during curfew hours [17].
When the government decided to implement the social distancing policy, some companies, especially the private ones (in the field of transportation, traveling, sporting events, and clothing, among others), opposed to the introduction of the measures, due to declining incomes and the risk of bankruptcy [10,15].
The aim of this study was is investigate the effects of the social distancing policy on the confirmed incidence cases and deaths of COVID-19 by applying the interrupted time series analysis (ITSA) method.
Materials and Methods
Ethics Approval and Consent to Participate
The ethics committee of the Lorestan University of Medical Sciences (LUMS) approved this study (approval code no. IR.LUMS. REC.1399.083).
Design of Study
This study was designed as a quasi-experimental study and was interpreted utilizing the ITSA approach.
Study Population
Population studied was the Iranian population (81,672,300 inhabitants), including 1,398,835 confirmed incidence cases and 57,734 deaths.
Study Outcomes
Study outcomes included the number of confirmed COVID-19 incidence cases and number of deaths due to COVID-19 in Iran. Cases were confirmed by polymerase chain reaction (PCR), following the WHO guidelines [26].
Data Sources
We used daily data related to COVID-19 on confirmed incidence cases and deaths, which were collected through the websites of the MOHME and the WHO from 954 public hospitals and health center settings [25,27]. The MOHME announces daily the statistics of all the provinces of Iran. Daily data was collected between February 20th, 2020 and January 29th, 2021. The social distancing policy was launched on March 27th, 2020. During the study period, 1,398,835 confirmed incidence cases and 57,734 deaths occurred.
Statistical Analysis: Interrupted Time Series Analysis (ITSA)
Evaluating the impact of different health policies can be very important and helpful to advise health policy- and decision-makers whether to continue or not the implementation of a given policy or make some changes [28]. Health decision-makers try to implement policies that are highly effective [29]. ITSA is a valuable analysis to evaluate the impact of the implementation of various policies in the health sector [30]. ITSA can be used both for clinical and non-clinical interventions, in cases in which prospective analysis and randomization are not possible [31,32].
Time series analysis examines the relationship between data and a topic over time. In ITSA, the impact of a policy at a given point of time is compared to before and after the implementation [33]. ITSAs can provide a strong assessment of the long-term impact of policy implementation and can often be highly generalizable because they are performed in real-world contexts [34]. ITSA can play a very important role in health-related crises, as it is able to assess the consequences of implementing a policy in a crisis situation [35]. In addition to health consequences, this assessment can also investigate its impact on the economic, social, political, and cultural sectors [33,36,37].
ITSA models were fit using segmented regression models (SRMs) and longitudinal data. For estimating the best analytical approach, we used the Newey‐West method [35]. Also, to assess the robustness of our findings, we conducted several diagnostic and sensitivity assessments. An ordinary least squares (OLS) regression model with a time series specification (an intercept and a trend term, a level and a trend change) was utilized in order to check for serially correlated errors using the Durbin-Watson test and by visualizing the residuals from the OLS regression and plotting the autocorrelation and partial autocorrelation (ACF/PACF) graphs [28]. We employed OLS rather than other regression techniques (like methods based on autoregressive integrated moving-average (ARIMA) or its variants models) as OLS appears to be more robust, flexible, and suitable when analyzing interrupted time-series [38].
All synthesized estimates were reported with their computed 95% confidence interval (CI). p-value < 0.05 was considered significant. All analyses were carried out with R software Version 3.6.1 (London, UK).
Results
Confirmed Incidence Cases
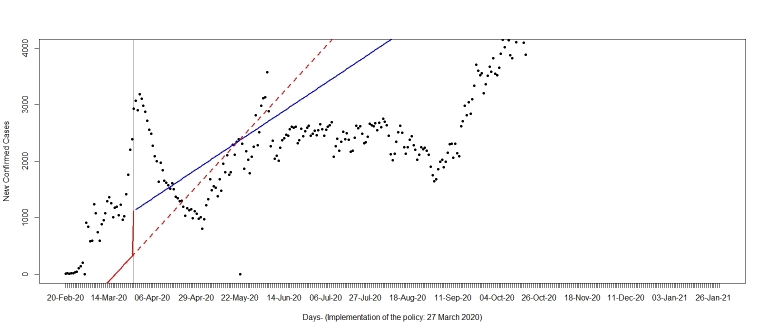
A significant decrease of -179.93 (95% CI: -380.11 to -20.25, P-value=0.078) confirmed incident cases following the implementation of the social distancing policy was found (See Figure 1).
Figure 1.
The rate of confirmed COVID-19 incidence cases between February 20th, 2020 and January 29th, 2021, prior to and following the implementation of the social distancing policy in Iran (launched on March 27th 2020). Dashed line is projected trend without the implementation of the policy; solid line is the trend observed after the implementation of the policy.
This corresponds to a daily decrease in the trend of -31.17 (95% CI: -46.95 to -15.40, P-value=0.08).
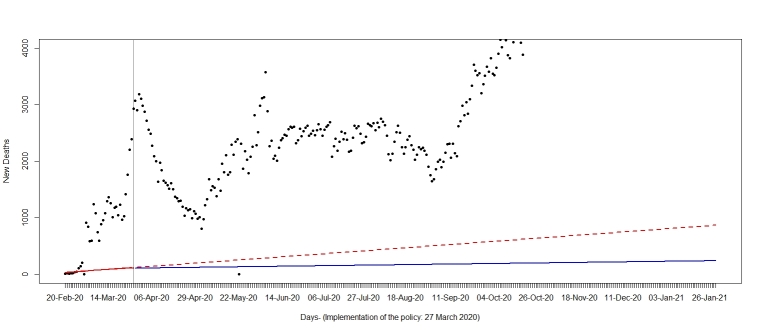
Deaths
A significant decrease of -28.28 (95% CI: -43.55 to -13.01, P-value=0.05) deaths following the implementation of the social distancing policy was observed (See Figure 2). This corresponds to a daily decrease in the trend of -4.52 (95% CI: -5.25 to -3.78, P-value=0.003).
Figure 2.
The rate of deaths related to COVID-19 between February 20th, 2020 and January 29th, 2021, prior to and following the implementation of the social distancing policy in Iran (launched on March 27th 2020). Dashed line is projected trend without the implementation of the policy; solid line is the trend observed after the implementation of the policy.
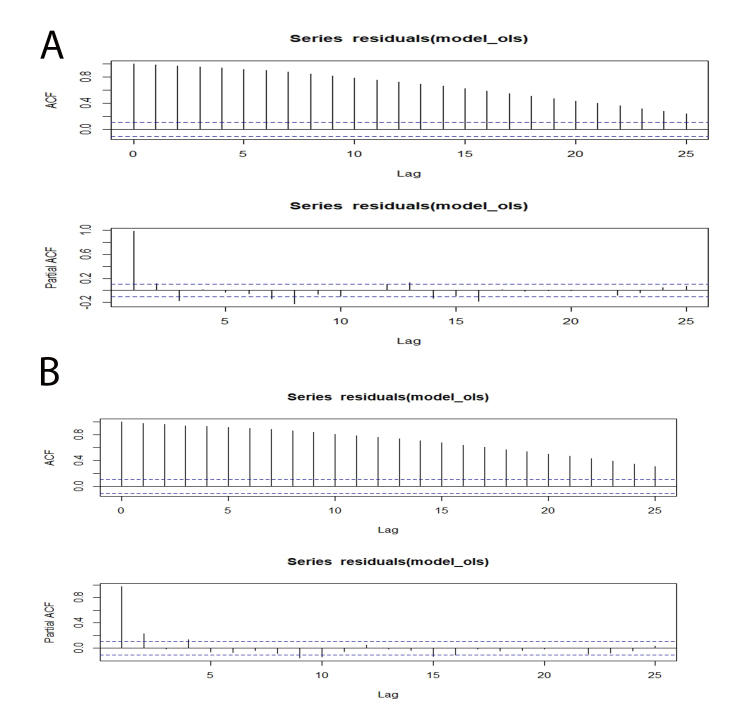
Residuals from the OLS regression for confirmed incidence cases and deaths related to COVID-19 are shown in Figure 3, whereas autocorrelation and partial autocorrelation functions for confirmed incidence cases and deaths related to COVID-19 are shown in Figure 4A and 4B. Both Figures 3 and 4 show presence of autocorrelation, indicating a good relationship of each data point with the previous one. More in detail, for confirmed incidence cases 0, 1, and 15 lags were significant at the autocorrelation function, whereas 0 and 15 lags were significant at the partial autocorrelation function. This indicated a bi-weekly correlation, which, interestingly, is the incubation time of COVID-19. For deaths, 0, 1, 2, 3, 4, 9, 10, 11, 12, 13, 14, and 15 lags were significant at the autocorrelation function while only 0 lag was significant at the partial autocorrelation function. Presence of autocorrelation was taken into account by performing the Newey-West robust estimator.
Figure 3.
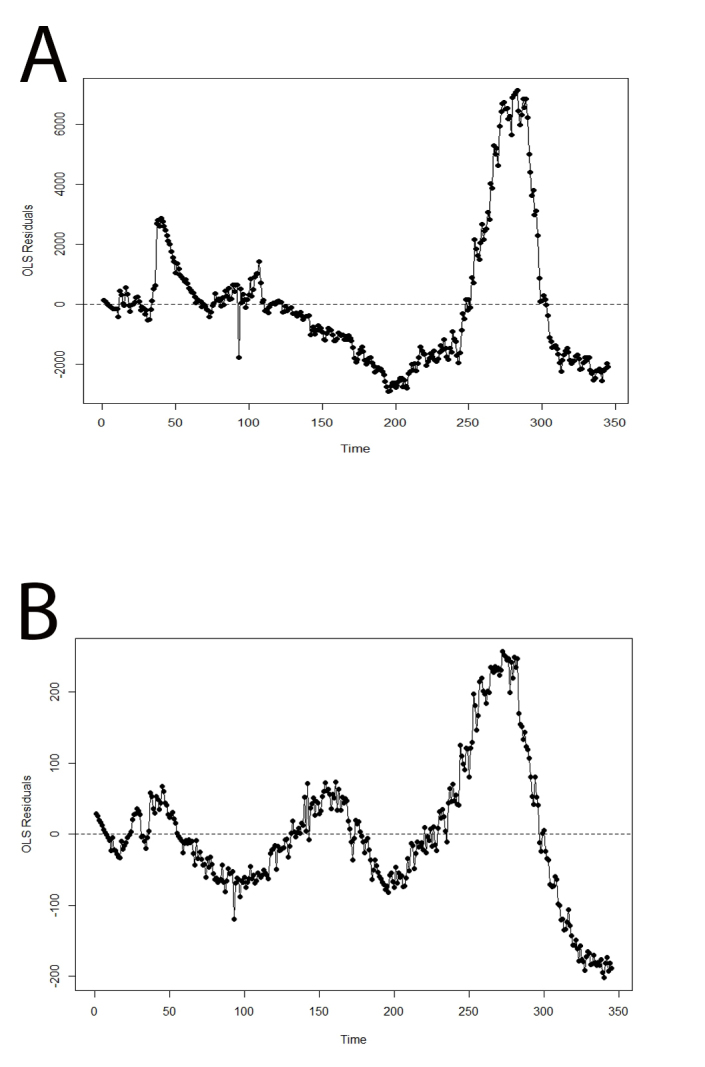
Residuals from the OLS regression (A: COVID-19 confirmed incidence cases, B: deaths between February 20th, 2020 and January 29th, 2021, in Iran). The plot shows presence of correlation.
Figure 4.
Autocorrelation and partial autocorrelation function (A: confirmed incidence cases, B: deaths between February 20th, 2020 and January 29th, 2021, in Iran). The plots show presence of correlation.
Discussion
The findings of the present study showed that the implementation of the social distancing policy in Iran may have been effective in controlling the spread of the COVID-19 and may have reduced both confirmed incidence cases and deaths. This policy is currently also being used as a public health strategy to control COVID-19 in other countries. A review of studies in 16 countries showed that the virus transmission was lower with social distancing of one meter or more, compared with a distance of less than one meter (n=10,736, pooled adjusted odds ratio [aOR] 0·18, 95% CI 0·09 to 0·38; risk difference [RD] –10·2%, 95% CI –11·5 to –7·5; moderate [39].
Prior to the implementation of the social distancing policy, the trend of COVID-19 infection in Iran was increasing. Policy- and decision-makers have launched various programs to control the disease. Due to the fact that the new year holidays in Iran begin in early spring (Nowruz) [40], policy-makers were very concerned about the transmission of the disease through the numerous trips that take place every year during the holidays. Maximum travel restrictions were imposed on passenger transportation by air, train, and intercity buses, while fully implementing health protocols [10].
A study by Medeiros de Figueiredo and colleagues, conducted by utilizing ITSA, looked at the impact of the social distancing policy in Chinese cities, and found that the implementation of this policy had significantly reduced the incidence and mortality as a result of COVID-19 [41]. In another study employing ITSA, Siedner et al. investigated the effect of social distancing on COVID-19 growth rate in different US states, where, between March 10th and 27th 2020, a policy of self-isolation was implemented and was able to significantly reduce the spread of COVID-19 [42].
The findings of these two studies in China and the US are consistent with the results of our study. These studies show a decrease in the average daily growth rate of cases and deaths, and over time, the social distancing policy may have been able to help the health system of these countries to reduce the burden of disease, providing better services to hospitalized patients and avoiding overwhelming and straining of healthcare facilities.
At the beginning of COVID-19, some cities in Iran were severely affected by the outbreak and many people became quickly infected. Due to its geographical location, the religious city of Qom and the Northern cities of Iran, tourist destinations for Iranian travelers, were affected the most in terms of COVID-19 cases. Therefore, in the first days, these areas started social distancing earlier, since implementing social distancing can be a valuable policy option for the most hit settings [9,10].
The biggest resistance to implementing this policy is due to its economic and social impact. Many people may become unemployed and unable to cover their expenditures. COVID-19 challenged Iranian macroeconomy by decreasing oil demand and reducing the supply and demand cycle, as well as affecting small businesses due to social distancing and quarantine restrictions [15]. Small businesses have experienced reduced production, reduced goods and service delivery and decreased sales, disruption in insurance services, impossibility of re-paying bank-loans, and unemployment [43]. Therefore, a very careful monitoring of the impact of the implementation of this policy should be done. Government should provide financial assistance, such as subsidies and loans, encouraging people to be more compliant with this policy [44].
Given the potential benefits of social distancing seen in some outbreaks, it can also be effective in the COVID-19 outbreak, and policy-makers should try to mitigate the economic and psychological problems that can affect people [45]. Mohammadi et al. have carried out a cross-sectional study, assessing the mental health status of 221 COVID-19 infected patients and 241 controls from the general population. Authors found a high prevalence of mental health issues among patients suffering from COVID-19 [46]. The pandemic particularly affected healthcare workers. Alizadeh and colleagues carried out a qualitative study among 18 healthcare providers, who, being overwhelmed by high workload, reported relevant occupational demands and psychological distress [47].
After the implementation of social distancing, the trend of incidence cases and deaths decreased, which was in line with the expected goals of this policy. This enabled the enhancement and improvement of laboratories and diagnostic testing to identify cases as the policy was implemented, and incidence cases were identified better than in previous days. COVID-19 is spreading rapidly around the world, and implementing social distancing policy is effective [10]. A study by Medeiros de Figueiredo et al. showed that delays in implementing policies that can reduce the spread of the disease can have a major impact on its containment [41].
China’s experience in reducing the burden of COVID-19 compared to other countries has shown that the implementation of social distancing can be effective [9]. However, the variability of the political and social system of different countries should be taken into account, which plays a key role in the implementation of this policy together with several contextual variables. On the other hand, a late implementation of social distancing policy, such as in Italy, can result in a high mortality rate [48,49].
Limitations of the Study
This study has some limitations, including the fact that the data on age and sex were not accessible because at the time of the study, the MOHME had not published them despite their availability.
Besides this main shortcoming, it should be emphasized that different contextual factors and variables such as the quality of healthcare services in Iran, underlying co-morbidities, or selected samples, may contribute to explain the findings of the present study. Improving healthcare facilities and diagnostic testing capacity, changing diagnostic criteria, validating new tests, and introducing some medications can affect the analysis performed in this study. Confirmed data could suffer from under-reporting bias or reporting delays. Moreover, we did not have access to time data at the province level. These data could be valuable in determining the effect of social distancing policy at the province level, because different provinces of Iran can be uniquely affected by the implementation of this policy due to the different conditions they may experience. The implementation of the social distancing policy may have been carried out more vigorously by some provinces, and this could affect the data. Provinces with larger populations can have a greater impact on the data. Moreover, social distancing began during the holidays, with many people staying at home and avoiding or reducing social and working activities. Finally, other measures implemented at similar times of the social distancing measures could also contribute to reducing the spread of the disease. Furthermore, people can also become more aware of the way the disease is spread and, as a consequence, there could be a wide-scale use of individual protective equipment, proper hand hygiene and adoption of other preventative measures. Therefore, all these factors could impact COVID-19 incident cases besides social distancing.
Conclusion
The growth rate of confirmed incidence cases and deaths from COVID-19 in Iran has significantly decreased from March 27, 2020 to January 29, 2021, after the implementation of social distancing policy. Due to the lack of immediately available vaccines and effective drugs for this disease, many policy- and decision-makers have focused on non-pharmacological methods to curb and control this disease. Based on preliminary data, social distancing policy has been proven to be effective in reducing the spread of the outbreak. By monitoring and implementing social distancing policy in all countries, the burden of COVID-19 may be mitigated. However, further research is needed, especially evaluating the long-term effects of the implementation of the social distancing policy. Due to the unpredictable nature of pandemics, assessing the impact of COVID-19 restrictions, such as social distancing, can help policy- and decision-makers enhance health systems’ capacity to promptly respond to crises and design and adopt effective policies.
Glossary
- ITSA
Interrupted time series analysis
- WHO
World Health Organization
- MOHME
Ministry of Health and Medical Education
- NGOs
non-governmental organizations
- SRMs
Segmented regression models
- OLS
Ordinary least squares
- ACF/PACF
Autocorrelation and partial autocorrelation
- CI
Confidence interval
Author Contributions
MaB, MHI, AB, MeB, MS, and NLB were the principal investigators who contributed to the conception and design of the study, collected, entered, analyzed, interpreted the data, prepared the manuscript. MaB acted as a corresponding author. MaB, MeB, NLB, JW, SA, and MKG contributed to data analysis, interpretation, and drafted the manuscript. All authors read and approved the final manuscript.
References
- Fauci AS, Lane HC, Redfield RR. Covid-19: navigating the uncharted. N Engl J Med. 2020. March;382(13):1268–9. 10.1056/NEJMe2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worldometer. COVID-19 Coronavirus pandemic 2020. [updated 12 April 2020]. Available from: https://www.worldometers.info/coronavirus/
- Wibbens PD, Koo WW, McGahan AM. Which COVID policies are most effective? A Bayesian analysis of COVID-19 by jurisdiction. PLoS One. 2020. December;15(12):e0244177. 10.1371/journal.pone.0244177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley DM, Perencevich EN. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020. May;323(19):1908–9. 10.1001/jama.2020.5910 [DOI] [PubMed] [Google Scholar]
- Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020. May;46(5):837–40. 10.1007/s00134-020-05979-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A, Badrfam R. Fighting COVID-19 in Iran; economic challenges ahead. Arch Iran Med. 2020. April;23(4):284. 10.34172/aim.2020.14 [DOI] [PubMed] [Google Scholar]
- Behzadifar M, Ghanbari MK, Bakhtiari A, Behzadifar M, Bragazzi NL. Ensuring adequate health financing to prevent and control the COVID-19 in Iran. Int J Equity Health. 2020. May;19(1):61. 10.1186/s12939-020-01181-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoosefi Lebni J, Abbas J, Moradi F, Salahshoor MR, Chaboksavar F, Irandoost SF, et al. How the COVID-19 pandemic effected economic, social, political, and cultural factors: A lesson from Iran. Int J Soc Psychiatry. 2020. July:20764020939984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020. pii: S2468-2667(20):30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raoofi A, Takian A, Akbari Sari A, Olyaeemanesh A, Haghighi H, Aarabi M. COVID-19 pandemic and comparative health policy learning in Iran. Arch Iran Med. 2020. April;23(4):220–34. 10.34172/aim.2020.02 [DOI] [PubMed] [Google Scholar]
- Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. C4591001 Clinical Trial Group. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020. December;383(27):2603–15. 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raeisi A, Tabrizi JS, Gouya MM. IR of Iran National Mobilization against COVID-19 Epidemic. Arch Iran Med. 2020. April;23(4):216–9. 10.34172/aim.2020.01 [DOI] [PubMed] [Google Scholar]
- Zareie B, Roshani A, Mansournia MA, Rasouli MA, Moradi G. A model for COVID-19 prediction in Iran based on China parameters. Arch Iran Med. 2020. April;23(4):244–8. 10.34172/aim.2020.05 [DOI] [PubMed] [Google Scholar]
- Takian A, Bakhtiari A, Ostovar A. Universal health coverage for strengthening prevention and control of noncommunicable diseases in COVID-19 era. Med J Islam Repub Iran. 2020. November;34:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbari MK, Behzadifar M, Bakhtiari A, Behzadifar M, Azari S, Abolghasem Gorji H, et al. Assessing Iran’s health system according to the COVID-19 strategic preparedness and response plan of the World Health Organization: health policy and historical implications. J Prev Med Hyg. 2021. January;61(4):E508–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaei G, Harirchi I, Sajadi HS, Yahyaei F, Majdzadeh R. The harsh effects of sanctions on Iranian health. Lancet. 2019. August;394(10197):468–9. 10.1016/S0140-6736(19)31763-5 [DOI] [PubMed] [Google Scholar]
- Abdi M. Coronavirus disease 2019 (COVID-19) outbreak in Iran: actions and problems. Infect Control Hosp Epidemiol. 2020. June;41(6):754–5. 10.1017/ice.2020.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy A, Abdi Z, Harirchi I, McKee M, Ahmadnezhad E. Economic sanctions and Iran’s capacity to respond to COVID-19. Lancet Public Health. 2020. May;5(5):e254. 10.1016/S2468-2667(20)30083-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. 2020. June;51:101990. 10.1016/j.ajp.2020.101990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monfared A, Balou HA, Hamidi Madani A, Rahbar Taramsari M, Hemmati H, Mohammadzadeh A, et al. Management of COVID-19 Crisis in Guilan Province in Northern Iran. Arch Iran Med. 2020. July;23(7):511–3. 10.34172/aim.2020.52 [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: UK starts social distancing after new model points to 260 000 potential deaths. BMJ. 2020. March;368:m1089. 10.1136/bmj.m1089 [DOI] [PubMed] [Google Scholar]
- Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020;pii: S1473-3099(20):30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K, Stanbrook MB, Laupacis A. Social distancing to combat COVID-19: We are all on the front line. CMAJ. 2020:pii: cmaj.200606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Coronavirus disease (COVID-19) advice for the public 2020. [updated 12 August 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- Ministry of Health and Medical Education. COVID-19 2021. [updated 19 Feb 2021]. Available from: https://behdasht.gov.ir/
- World Health Organization. Country & Technical Guidance - Coronavirus disease (COVID-19) 2020. [updated 27 October 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard 2021. [updated 19 Feb 2021]. Available from: https://covid19.who.int/?gclid=Cj0KCQiAvP6ABhCjARIsAH37rbQCBSLyOPBdExXX5wqVuq-Ybnzab8dx4IX4RTKD080v4-bXHsmgpQYaAp4dEALw_wcB
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017. February;46(1):348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013. Nov-Dec;13(6 Suppl):S38–44. 10.1016/j.acap.2013.08.002 [DOI] [PubMed] [Google Scholar]
- Lau WC, Murray M, El-Turki A, Saxena S, Ladhani S, Long P, et al. Impact of pneumococcal conjugate vaccines on childhood otitis media in the United Kingdom. Vaccine. 2015. September;33(39):5072–9. 10.1016/j.vaccine.2015.08.022 [DOI] [PubMed] [Google Scholar]
- Jandoc R, Burden AM, Mamdani M, Lévesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol. 2015. August;68(8):950–6. 10.1016/j.jclinepi.2014.12.018 [DOI] [PubMed] [Google Scholar]
- Komen J, Forslund T, Hjemdahl P, Andersen M, Wettermark B. Effects of policy interventions on the introduction of novel oral anticoagulants in Stockholm: an interrupted time series analysis. Br J Clin Pharmacol. 2017. March;83(3):642–52. 10.1111/bcp.13150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ. 2013. February;346 feb07 1:f403. 10.1136/bmj.f403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy C, Steinbach R, Edwards P, Green J, Armstrong B, Wilkinson P. Effect of 20 mph traffic speed zones on road injuries in London, 1986-2006: controlled interrupted time series analysis. BMJ. 2009. December;339 dec10 3:b4469. 10.1136/bmj.b4469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011. December;17(6):1231–8. 10.1111/j.1365-2753.2010.01504.x [DOI] [PubMed] [Google Scholar]
- Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015. June;350 jun09 5:h2750. 10.1136/bmj.h2750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis J, Ramsay T, Turgeon AF, Zarychanski R. Helmet legislation and admissions to hospital for cycling related head injuries in Canadian provinces and territories: interrupted time series analysis. BMJ. 2013. May;346(may14 1):f2674. 10.1136/bmj.f2674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden A. Conducting Interrupted Time-series Analysis for Single- and Multiple-group Comparisons. The Stata Journal: Promoting communications on statistics and Stata. 2015;15(2). [Google Scholar]
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020. June;395(10242):1973–87. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahromi MG, Goudarzi R, Yazdi-Feyzabadi V, Amini S, Nazari J, Amiresmaili M. Effect of new year holidays on hospital mortality: a time series study. Int J Emerg Med. 2019. August;12(1):20. 10.1186/s12245-019-0243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros de Figueiredo A, Daponte Codina A, Moreira Marculino Figueiredo DC, Saez M, Cabrera León A. Impact of lockdown on COVID-19 incidence and mortality in China: an interrupted time series study [Submitted]. Bull World Health Organ. 2020. Epub 6 April 2020. [Google Scholar]
- Siedner MR, Harling G, Reynolds Z, Gilbert R, Venkataramani AS, Tsai AC. Social distancing to slow the U.S. COVID-19 epidemic: interrupted time-series analysis. medRxiv. 2020. Epub 8 Mar 2020.
- The Parliament of Iran. The Impact of Corona on the Iranian Economy 2021. Available from: https://www.parliran.ir/
- Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci USA. 2007. May;104(18):7582–7. 10.1073/pnas.0610941104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson NM, Cummings DA, Cauchemez S, Fraser C, Riley S, Meeyai A, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005. September;437(7056):209–14. 10.1038/nature04017 [DOI] [PubMed] [Google Scholar]
- Mohammadi SM, Ashtari S, Khosh Fetrat M. The psychological impact of COVID-19 pandemic on mental health of Iranian population. Int J Travel Med Glob Health. 2019;9(1):19–24. 10.34172/ijtmgh.2021.04 [DOI] [Google Scholar]
- Alizadeh A, Khankeh HR, Barati M, Ahmadi Y, Hadian A, Azizi M. Psychological distress among Iranian health-care providers exposed to coronavirus disease 2019 (COVID-19): a qualitative study. BMC Psychiatry. 2020. October;20(1):494. 10.1186/s12888-020-02889-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA. 2020. April;323(14):1335. 10.1001/jama.2020.4344 [DOI] [PubMed] [Google Scholar]
- Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020. April;395(10231):1225–8. 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]