Abstract
Introduction: In controversial fashion, the presence of an enlarged external occipital protuberance has been recently linked to excessive use of handheld electronic devices. We sought to determine the prevalence of this protuberance in a diverse age group of adults from two separate time periods, before and approximately 10 years after the release of the iPhone, to further characterize this theory, as if indeed valid, such a relationship could direct preventative behavior. Materials and Methods: Eighty-two cervical spine radiographs between March 7, 2007 through June 29, 2007 and 147 cervical spine radiographs between October 25, 2017 through January 1, 2018 were reviewed for the presence or absence of an exophytic external occipital protuberance. Influence of sex and age were also assessed. Results: There were 41/82 (50%) patients within the 2007 pre-iPhone group with an exophytic external occipital protuberance, ranging from 2.7-33.8 mm in length. Twenty-seven out of 82 (32.9%) had an external occipital protuberance at or above 10 mm. There were 49/147 (33.3%) patients within the 2017 post-iPhone group with an exophytic external occipital protuberance, ranging from 4.4-53.8 mm in length. Thirty-three out of 147 (22.4%) had an external occipital protuberance at or above 10 mm. When considering accessibility to the iPhone, sex, and age to the presence of an exophytic external occipital protuberance, only sex has a statistically significant association, p=0.000000033. Conclusion: We found no significant association with iPhone accessibility and an exophytic external occipital protuberance. Due to inherent limitations in the retrospective nature of the study, future research is needed to better examine the association of handheld electronic devices with exophytic external occipital protuberances.
Keywords: enthesophyte, external occipital protuberance, handheld electronic device, iPhone
Introduction
An enthesophyte is an osseous spur that occurs at an enthesis, the site of insertion of a tendon, ligament, fascia, or joint capsule onto the bone [1-3]. While the enthesophyte can be seen in the context of a variety of pathologies, they may also occur with no clear underlying cause, and have been reported as an asymptomatic part of aging [1-3].
Radiologists commonly encounter enthesophytes on a routine basis as an incidental finding on imaging when evaluating for alternative sites of pain. Recently, they have gained widespread attention by the popular press and social media as a result of a proposed association of their formation at the occipital protuberance with handheld electronic devices, such as the smartphone. Social media plays a significant role in providing the public with timely disease-related information, altering risk perception, and influencing preventative behaviors [4]. However, before such preventative measures are instituted, the cause of disease must first be established.
Shahar and Sayers have recently published several research studies investigating the prevalence of an enlarged external occipital protuberance (EOP), as defined by the authors, across a young and diverse age population [5-7]. Due to the unexpected finding of a high prevalence of the enlarged EOP in a young population, devoid of a genetic or inflammatory explanation, the authors concluded that poor posture, influenced by modern, extensive use of handheld devices may reflect a cause of this phenomenon. Because the enthesophyte is potentially symptomatic at this site, and in general enthesopathy may require some form of medical or surgical management, the authors drew attention to this possible association. Notably, the authors have since published an erratum to their work, acknowledging that such an association is speculative [8]. Regardless, the results of these studies were widely disseminated by the popular press and through social media drawing attention and concern [9,10].
We sought to determine the prevalence of the exophytic EOP in a diverse age group of adults from two separate time periods to help further characterize the theory that its presence may be a byproduct of the extensive use of handheld electronic devices. Within this category of handheld technology is the smartphone, revolutionized by Steve Jobs and Apple Inc. with the release of the iPhone on June 29, 2007. We reviewed cervical spine radiographs acquired in a cohort on or before June 29, 2007, prior to the major uptick in handheld electronic device use prompted by the release of the iPhone, and compared them to a second group with cervical spine radiographs completed approximately 10 years later, well into the smartphone trend.
Materials and Methods
Following formal request for research approval, the Institutional Review Board at Yale School of Medicine granted exemption status for this project to be conducted.
We utilized the software package Nuance mPower, Innovated by Montage, 2020 Nuance Communications, Inc, Version 3.2.1 to identify approximately 500 cervical spine radiograph series in those 18 years of age or older at our institution acquired on or prior to January 1, 2018. Working retrospectively from this time point, we expanded our timeframe search parameter back to October 25, 2017, which resulted in 539 total radiograph series. While cervical spine radiographs are acquired across multiple sites of our institution’s health network, we elected to isolate only images within this group acquired from one individual site, where the majority of orthopedic radiography is performed at our institution, in order to achieve the most standardized methodology. A total of 191 studies were completed at said site, and subsequently reviewed.
In a consensus fashion all images from this group were reviewed by two radiologists, one with fellowship training in musculoskeletal radiology and a total of 9 years of experience following fellowship (JP), and the other a third-year radiology resident (PS), to determine the presence or absence of an exophytic EOP, in a similar fashion to that described by Shahar et al. [5-7]. We documented the presence or absence of an exophytic EOP and the length of this protuberance when present on the lateral view. Notably, all exophytic EOPs were measured and recorded in our study, in contrast to the prior studies by Shahar et al. [5-7], in which those EOPs less than 5 mm were omitted.
All images were reviewed in the Visage version 7.1 picture archiving and communications system, which is currently used at our institution. When necessary, images were magnified to increase accuracy of measurement. The size of the EOP was measured as the distance in millimeters from the most superior point of the EOP to a point on the EOP that was most distal from the skull (Figure 1). Although there is no discussion in the Shahar et al. articles reviewed [5-7] regarding the distinction between sessile bumps along the posterior occiput from grossly exophytic enthesophytes, all of their figures demonstrate exophytic enthesophytes with a clearly definable distal terminus. To avoid ambiguity in measurement, as well as to most closely mirror those methods used by Shahar et al., we elected to consider sessile bumps along the posterior occiput that lacked an obvious exophytic terminus as being devoid of a true enthesophyte (Figure 2).
Figure 1.

Representative measurement of an external occipital protuberance. The protuberance exhibits a well demarcated pedunculated terminus, with the length measurement denoted by the arrows.
Figure 2.

Representative sessile bump along the posterior occiput. The arrows denote the sessile bump along the posterior occiput, without a well-defined terminus. This study was considered devoid of an external occipital protuberance.
Similar to those methods utilized by Shahar et al. to standardize measurements [5-7], we included only those studies with an identifiable radiology technologist marker, with a known length, present on the image series. Two separate markers were acquired from the radiology technologists prior to image interpretation. One marker measured 60 mm in length and the other 40 mm in length. Those studies without one of the two markers present on the radiograph series were excluded. During image evaluation, the markers were measured on PACS and used as a reference standard. This allowed verification of the general accuracy of the EOP measurement size being obtained. This also verified the absence of EOP size error that may arise from differences in distance of the EOP from the image receptor as a function of differences in patient torso width. We utilized a 3 mm discrepancy of the known radiology technologist marker length from the measurement acquired in PACS during review as our threshold for inclusion and exclusion of an image based on magnification-related artifact. Three mm represents a 5% error for a 60 mm marker and a 7.5% error for a 40 mm marker. Notably, there were no studies with a greater than 3 mm discrepancy between the actual length of the technologist maker and that which was acquired on PACS.
Those studies in which hardware was present at the occiput, or in which imaging technique precluded full visualization of the posterior occiput at the expected location of the EOP, were also excluded. Lastly, when multiple studies were present from the same patient, only the earliest chronologic study was included, and the follow-up studies omitted.
Following exclusions, there were 147 studies from 147 patients from October 27, 2017 through January 1, 2018 included in the study for analysis. Using similar methodology as detailed above for the first time cohort, we sought to identify approximately 500 cervical spine radiograph series in those 18 years of age or older at our institution acquired on or before June 29, 2007 for our second cohort. Working retrospectively from this time point, we expanded our timeframe search parameter back to May 7, 2007, which resulted in 527 total radiograph series. After isolating only those performed at our designated site, we reviewed 134 cervical spine radiograph series in those 18 years of age or older completed on March 7, 2007 through June 29, 2007. Following exclusions, which were largely a manifestation of a lack of a verifiable marker size on the image series, 82 radiograph series from 82 patients were included for analysis in this second cohort.
Logistic regression was utilized to simultaneously consider accessibility to the iPhone, sex, and age to the outcome variable of the presence or absence of an EOP. Multiple regression was used with EOP as the outcome variable. A two-tailed t-test was used to compare mean size of an EOP between sexes. All statistical calculations were performed using R version 3.6 [11].
Results
From March 7, 2007 through June 29, 2007, 134 cervical spine radiograph series were performed at a single site in patients 18 years of age or older. Fifty-two studies were excluded (47 related to the lack of a verifiable technologist marker size on the image series, two studies which reflected the follow up cervical spine radiograph series from the same patient already tabulated from an earlier time point, two related to partial visualization of the posterior occiput, and one study with hardware at the occiput). Eighty-two cervical spine radiograph series from 82 patients were included in the review of this cohort. There were 51 females and 31 males. The average age was 46.8 years, with a range of 18-81 years.
There were 41 (22 male and 19 female) patients within this group with an exophytic EOP (41/82 = 50%), with sizes ranging from 2.7 mm to 33.8 mm, and with an average EOP size of 13.4 mm. There were 14 patients with an EOP of less than 10 mm, which reflects the threshold value for an “enlarged” EOP by Shahar et al. [5-7], and therefore 27 (27/82 = 32.9%) patients with an EOP at or above 10 mm in length.
From October 25, 2017 through January 1, 2018, 191 cervical spine radiograph series were performed at a single site in patients 18 years of age or older. Forty-four studies were excluded (40 related to the lack of a verifiable technologist marker size on the image series, two related to partial visualization of the posterior occiput, and two studies with hardware at the occiput). One-hundred-forty-seven cervical spine radiograph series from 147 patients were included in the review of this cohort. There were 110 female and 37 male patients. The average age was 52.5 years, with a range of 20-90 years.
There were 49 (25 male and 24 female) patients within this group with an exophytic EOP (49/147 = 33.3%), with sizes ranging from 4.4 mm to 53.8 mm, and with an average EOP size of 14.3 mm. There were 16 patients with an EOP of less than 10 mm, and therefore 33 (33/147 = 22.4%) patients with an EOP at or above 10 mm in length.
When simultaneously considering accessibility to the iPhone, sex, and age to the presence of an exophytic EOP with logistic regression, only male sex has a statistically significant association, p=0.000000033, with an odds ratio of 5.9.
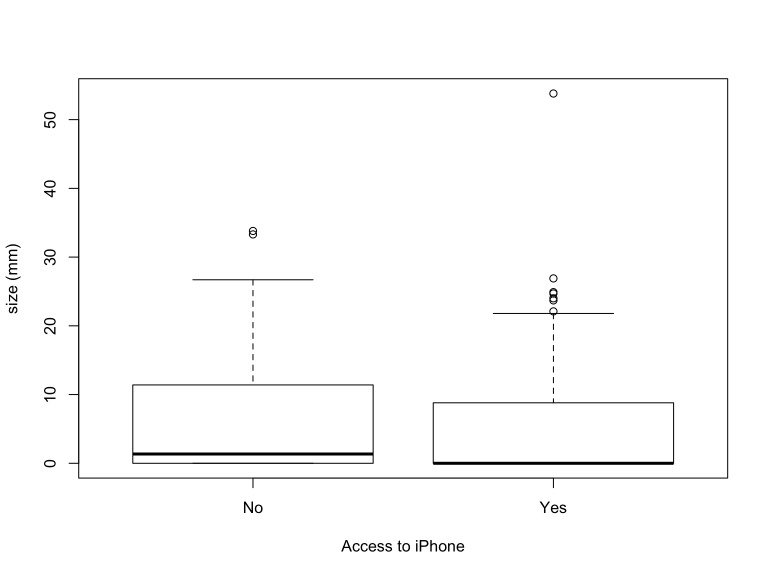
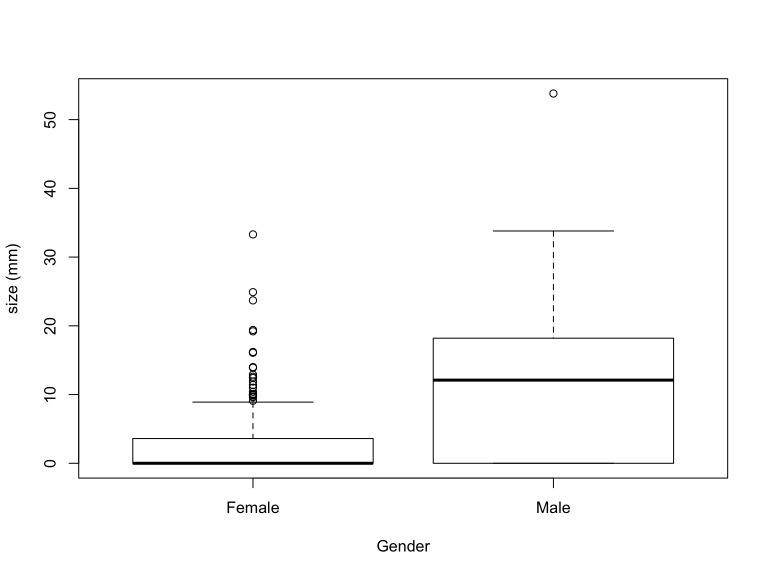
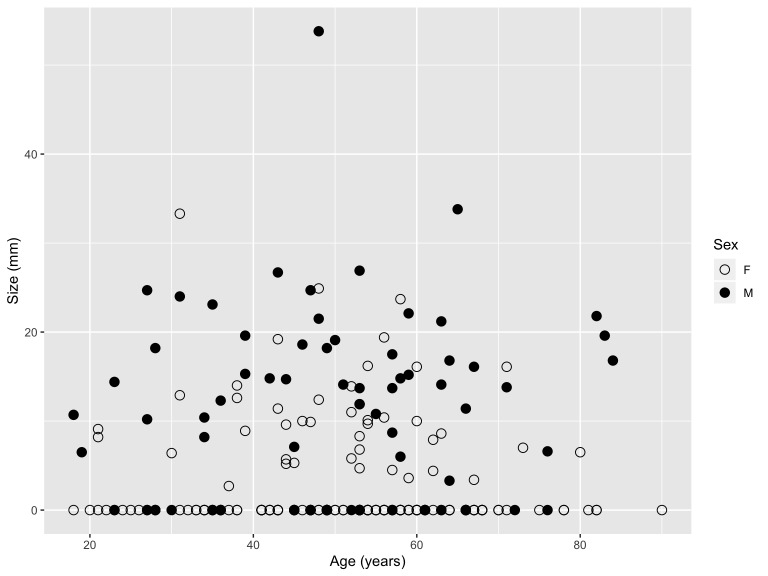
Based on multiple regression with size of an EOP as the outcome variable, not only are males more likely to have an exophytic EOP, but when an exophytic EOP is present, they tend to be larger in males versus females, with mean EOP size in males of 11 mm and in females 2.9 mm. When comparing the size of an EOP between sexes using a two-tailed t-test, EOP size in males is statistically significantly larger when compared to females, p=0.000000006. Size of the EOP is not related to age or accessibility to the iPhone, however (Figures 3,4,5).
Figure 3.
Size of external occipital protuberance relative to access to the iPhone. Fifty percent of those without access to an iPhone demonstrated an external occipital protuberance, while 33.3% of those with access to an iPhone demonstrated an external occipital protuberance. Access to the iPhone is not associated with size of an external occipital protuberance.
Figure 4.
Size of external occipital protuberance relative to sex. The odds of having an external occipital protuberance are 5.9 to 1 in males versus females, and protuberance size varies based on sex, with the average size in females being 2.9 mm and in males 11 mm.
Figure 5.
Size of external occipital protuberance relative to age. External occipital protuberance size is independent of age.
Discussion
Entheses represent the site of insertion of a tendon, ligament, fascia, or joint capsule onto bone [1-3]. An enthesophyte is an osseous spur arising at an enthesis, extending in the direction of pull of the ligament or tendon [1,2]. While enthesophytes may have no clear underlying cause, they may be degenerative/mechanical, or associated with seronegative spondyloarthropathy, diabetes mellitus, trauma, and CPPD arthropathy [1-3]. Enthesophytes have also been reported with aging, with an increased prevalence of asymptomatic “radiographic enthesopathy” [3].
The enthesophyte assists with dissipating mechanical stress from the insertion site [2]. Enthesopathy is the term used to describe the involvement of an enthesis in any pathologic process, whether metabolic, inflammatory, traumatic, or degenerative [3]. Alternatively, enthesitis refers specifically to inflammatory enthesopathy, and a hallmark feature of spondyloarthritis [3].
In 2016, Shahar and Sayers [5] sought to quantify the prevalence of an enlarged EOP within healthy, asymptomatic, young subjects, as well as in an age-matched symptomatic cohort. The authors retrospectively reviewed 218 lateral cervical spine radiographs from subjects 18-30 years of age. There were 108 asymptomatic volunteers and 110 “mildly symptomatic” subjects, with imaging collected over an 18-month timeframe. When an EOP was identified on radiographic review, an experienced clinician measured the distance in millimeters from the superior point/origin to the most distal extent. A threshold to measure and record the EOP was set at 5 mm, and protuberances 10 mm or larger were considered to be enlarged. The authors found that 41% of the population had an enlarged EOP equal or greater than 10 mm, with the prevalence of an enlarged EOP significantly higher in males, and with larger EOPs found in males and in the asymptomatic group. Through a review of the literature, the authors noted that enthesophytes were previously believed to have been rarely seen in young adults radiographically and assumed to develop slowly with advancing age. Because of the unexpectedly high prevalence of an enlarged EOP in the young age group studied, the authors questioned whether the finding was the result of excessive forces acting on the EOP at a young age, possibly as a result of extensive use of handheld screen-based activities in children and adolescents which contribute to poor posture and biomechanical stress [5].
Shahar et al. [6] later conducted a separate investigation in four adolescent subjects, in an effort to determine the possible influences of genetic predisposition, inflammation, and mechanical factors in the development of an enlarged EOP. The authors found there to be no active inflammation or genetic predisposition to the enlarged EOPs in the group studied based on laboratory and radiologic testing. All of the subjects presented with concerns over posture, and the authors concluded that mechanics play an important role in the development of large enthesophytes, and potentially an effect of extensive use of screen-based activities, as supported by the interview data collected during the study. The authors noted that enthesophytes represent a marker of structural damage, and that traditional approaches to excessive enthesophyte formation include surgical and pharmacological intervention. Therefore, understanding the role of mechanical load and its modification has clinical value [6].
Shahar and Sayers [7] recently attempted to determine the distribution of enlarged EOPs throughout a broad age group, in a larger sample, as an extension of their earlier, aforementioned research which revealed an unexpectedly high number of enlarged EOPs in a young cohort. Using similar methods to their earlier study, the authors reviewed 1200 cervical spine radiographs of those ranging from 18-86 years of age. The prevalence of an enlarged EOP was 33% in the study population. Males were 5.48 times more likely to have an enlarged EOP than females. An increase in forward head protraction resulted in increased likelihood of having an enlarged EOP. Every decade increase in age resulted in a 1.03 times reduction in the likelihood of having an enlarged EOP; the 18-30-year age group was significantly more likely to present with an enlarged EOP. The authors noted that the mean forward head projection in their study was significantly larger than the mean recorded prior to the “handheld technological revolution.” They concluded that the development of an enlarged EOP may be explained by extensive use of screen-based activities by individuals of all ages, including children, and the associated poor posture [7]. Notably, the authors of this study have since issued an erratum, in which they have acknowledged that the language used in this study was speculative, and that direct causation of an enlarged EOP with use of the handheld electronic device cannot be established based on the methodology utilized [8]. Nevertheless, their work has drawn attention to this possible association, and prompted our study to help provide further characterization.
If an enthesophyte represents a marker of structural damage as a result of poor posture and biomechanical stress, investigating possible causes and implementing preventative measures is a worthy task. The vigorous popular press and social media response to the work performed by Shahar and Sayers appeared to be fueled by one’s emotions and personal-level health risk perception, and when people recognize risk, they become motivated to engage in preventative health behaviors [4]. Intervening before disease occurs is a primary disease prevention strategy, while the detection and treatment of disease at an early stage are secondary forms of prevention [12]. However, before these preventative measures can be implemented, a cause of disease must first be established and substantiated. As such, we sought to help further characterize the role of the handheld electronic device on the development of the exophytic EOP, albeit in a limited retrospective fashion focusing on the introduction of the iPhone, as detailed.
When comparing two separate cohorts divided chronologically by a date on and just prior to the release of the iPhone, and a second date approximately 10 years later, we found no association with the accessibility of this ubiquitous handheld device and the presence or absence of an exophytic EOP. In fact, exophytic EOPs were more common in the 2007 cohort (50%) versus the 2017 cohort (33.3%), and there were more with an enlarged EOP (that being 10 mm or greater) within the 2007 cohort (32.9%) versus the 2017 cohort (22.4%). In 2007, there were 1.39 million Apple iPhone sales worldwide, while in 2018 there were 217.72 million [13]. Additionally, there were 8.65 million smartphone sales in the United States in 2007 and 79.1 million in 2018 [14]. However, despite these sale values and that the iPhone represents one of the more common handheld devices utilized, exophytic EOPs were more prevalent in the pre-iPhone introduction cohort compared to the post-iPhone introduction cohort in our study. Similar to the recently conducted study by Shahar and Sayers [7], we found the exophytic EOP to be present more commonly in males. Conversely, there was no influence of age with the presence of an exophytic EOP in our study.
There are certain limitations of our study. A granular definition of what constitutes an EOP was never defined in the studies by Shahar et al., which created an opportunity to either over or underestimate this finding during our analysis. We relied on the representative figures in the authors’ prior studies to define the EOP, and measured only those with exophytic morphology, in keeping with their examples. By utilizing this methodology in both cohorts assessed, our results are consistent, and therefore the differences in the two cohorts are an accurate representation of the influence, or lack thereof, of the introduction of the iPhone on the presence or absence of an exophytic EOP. Additionally, data acquired from radiographs was obtained retrospectively, and as such, we had no control of the standardization of image acquisition. To mitigate potential issues with magnification related measurement error, we utilized images obtained from a single site within our network, and omitted images that were without a reference size marker. Lastly, due to the retrospective nature of our study, we were unable to identify those with and those without symptoms localizing to the posterior occiput. However, it should be noted, the association of symptoms was never attributed to an enlarged EOP by Shahar and Sayers, who reported the mean enlarged EOP size for the asymptomatic population in their 2016 study was significantly greater than that recorded for the mildly symptomatic group. Further, in the follow-up study performed by Shahar and Sayers in 2018, the influence of symptoms and the presence of an enlarged EOP was not explicitly addressed in their results [5,7].
Conclusions
We found no significant association with iPhone accessibility and an exophytic external occipital protuberance. Due to inherent limitations in the retrospective nature of the study, future research is needed to better examine the association of handheld electronic devices with exophytic EOPs.
Glossary
- EOP
external occipital protuberance
Author Contributions
All authors contributed in some fashion to study design, drafting the manuscript, data analysis, statistics, and editing. There was no funding source for this study.
References
- Hardcastle SA, Dieppe P, Gregson CL, Arden NK, Spector TD, Hart DJ, et al. Osteophytes, enthesophytes, and high bone mass: a bone-forming triad with potential relevance in osteoarthritis. Arthritis Rheumatol. 2014. September;66(9):2429–39. 10.1002/art.38729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson N, Guermazi A, Clancy M, Niu J, Grayson P, Aliabadi P, et al. Relation of hand enthesophytes with knee enthesopathy: is osteoarthritis related to a systemic enthesopathy? J Rheumatol. 2012. February;39(2):359–64. 10.3899/jrheum.110718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’ Agostino MA, Palazzi C, Olivieri I. Entheseal involvement. Clin Exp Rheumatol. 2009. Jul-Aug;27(4 Suppl 55):S50–5. [PubMed] [Google Scholar]
- Oh SH, Lee SY, Han C. The Effects of Social Media Use on Preventive Behaviors during Infectious Disease Outbreaks: The Mediating Role of Self-relevant Emotions and Public Risk Perception. Health Commun. 2020. February:1–10. 10.1080/10410236.2020.1724639 [DOI] [PubMed] [Google Scholar]
- Shahar D, Sayers MG. A morphological adaptation? The prevalence of enlarged external occipital protuberance in young adults. J Anat. 2016. August;229(2):286–91. 10.1111/joa.12466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahar D, Evans J, Sayers MG. Large enthesophytes in teenage skulls: Mechanical, inflammatory and genetic considerations. Clin Biomech (Bristol, Avon). 2018. March;53:60–4. 10.1016/j.clinbiomech.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Shahar D, Sayers MGL. Prominent exostosis projecting from the occipital squama more substantial and prevalent in young adult than older age groups. Sci Rep. 2018;8(1):3354. 10.1038/s41598-018-21625-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahar D, Sayers MG. Author Correction: prominent exostosis projecting from the occipital squama more substantial and prevalent in young adult than older age groups. Sci Rep. 2019. September;9(1):13707. 10.1038/s41598-019-49153-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady D. About the Idea That You’re Growing Horns From Looking Down at Your Phone... [Internet]. NY Times. 2019. [cited 2021 Feb 13]. Available from: https://www.nytimes.com/2019/06/20/health/horns-cellphones-bones.html
- Stanley-Becker I. Horns are growing on young people’s skulls. Phone use is to blame, research suggests. [Internet]. Washington Post. [cited 2021 Feb 13]. Available from: https://www.washingtonpost.com/nation/2019/06/20/horns-are-growing-young-peoples-skulls-phone-use-is-blame-research-suggests/
- R Core Team. Vienna, Austria: R Foundation for Statistical Computing; 2019. [Google Scholar]
- Levine S, Malone E, Lekiachvili A, Briss P Health Care Industry Insights: Why the Use of Preventive Services Is Still Low. Prev Chronic Dis. 2019. 14;16:E30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statista. Unit Sales of the Apple iPhone Worldwide from 2007 to 2018. [Internet]. 2018. [cited 2020 Jul 27]. Available from: https://www.statista.com/statistics/276306/global-apple-iphone-sales-since-fiscal-year-2007/
- Statista. Smartphone Sales in the United States from 2005 to 2019 (in billion US dollars) [Internet]. 2019. [cited 2020 Jul 27]. Available from: https://www.statista.com/statistics/191985/sales-of-smartphones-in-the-us-since-2005/