Infection with severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) is responsible for the coronavirus disease 2019 (COVID-19) pandemic. Myocardial injury, thrombosis, and a systemic inflammatory response to SARS CoV-2 are common features of COVID-19, and biomarkers of each of these processes (cardiac troponin [cTn], d-dimer, and C-reactive protein [CRP], respectively) are associated with disease severity and mortality.1–3 This study aimed to determine whether a constellation of biomarkers at admission would predict in-hospital clinical outcomes in patients with COVID-19.
Consecutive adults ≥18 years of age with COVID-19 admitted to the New York University Langone Health system between March 1, 2020, and April 16, 2020, were identified and included if cTn, d-dimer, and CRP were measured. Routine multimarker surveillance was standard of care for patients with COVID-19; electronic admission order sets included cTn, d-dimer, and CRP laboratory tests. Myocardial injury was defined as an initial cTn above the site-specific upper limit of normal (ULN) for the assay (Siemens Dimension Vista [>0.045 ng/mL]/Centaur XPT [>0.5 ng/mL], Abbot Architect Troponin I [>0.04 ng/mL]). An elevated d-dimer was defined based on the assay ULN (>230 ng/mL). Given that 98.5% of our hospitalized patients with COVID-19 had an initial CRP concentration above the ULN, we defined increased inflammation as a CRP (Siemens Dimension, Abbot Architect) >50 mg/L. This threshold was prognostically important in prior studies.4,5 Demographics, comorbidities, medications, clinical presentation, and laboratory data were abstracted from the electronic health record. Comorbidities were defined by International Classifications of Diseases, 10th Revision codes. All-cause, in-hospital mortality was recorded. Critical illness was defined by receipt of intensive care, mechanical ventilation, transfer to hospice, or death. Categorical variables are reported as frequencies and proportions and compared by χ2 tests. We used logistic regression models to estimate the odds of study end points on the basis of the number of elevated biomarkers. We used the Harrell C-statistic to evaluate the survival model; areas under the curve were compared using the Delong test. The discriminative ability of the number of elevated biomarkers was characterized by the continuous net reclassification improvement. Adjusted risk models included demographics, clinical comorbidities, and characteristics at hospital presentation as covariates. Statistical analyses were performed using R. Statistical tests were 2-sided, and P values <0.05 were statistically significant. The study was approved by the New York University Langone Health Institutional Review Board with a waiver of informed consent; identifiable data will not be made publicly available.
A total of 3281 consecutive adults with COVID-19 were identified, and 2895 (88.2%) had measurement of all 3 biomarkers (cTn: median 0.015 ng/mL [interquartile range, <0.015–0.03]; D-dimer: median 403 ng/mL [interquartile range, 244–769]; and CRP: median 113 mg/L [interquartile range, 57–178]) at admission. Myocardial injury was present in 486 (16.8%) patients, the D-dimer level was elevated in 2243 (77.5%), and CRP was >50 mg/L in 2261 (78.1%). Only 196 (6.8%) patients had normal cTn, normal D-dimer, and a CRP of <50 mg/L (no elevated biomarkers). Elevations of all 3 biomarkers, reflecting the pathobiological axes of myocardial injury, coagulation, and inflammation, were present in 334 (11.5%; Figure). Patients with no elevated biomarkers were at low risk of critical illness and in-hospital mortality. Continuous CRP (C-statistic, 0.611 [95% CI, 0.587–0.634]), D-dimer (C-statistic, 0.639 [95% CI, 0.615–0.664]), and troponin (C-statistic, 0.680 [95% CI, 0.655–0.705]) concentrations were each separately associated with mortality. Patients with 1, 2, or 3 elevated biomarkers had stepwise increases in the risk of adverse events (Figure). The number of elevated biomarkers alone yielded a C-statistic of 0.672 (95% CI, 0.649–0.696) for mortality, with no difference in model performance compared with continuous data for all 3 biomarkers (0.657 [95% CI, 0.633–0.681], P=0.17). Addition of the number of elevated biomarkers to an adjusted risk model yielded improvements in the C-statistic (from 0.765 [95% CI, 0.745–0.785] to 0.789 [95% CI, 0.770–0.807], P<0.001) and the appropriate reclassification of risk (net reclassification improvement, 0.227 [95% CI, 0.141–0.313]) for mortality.
Figure.
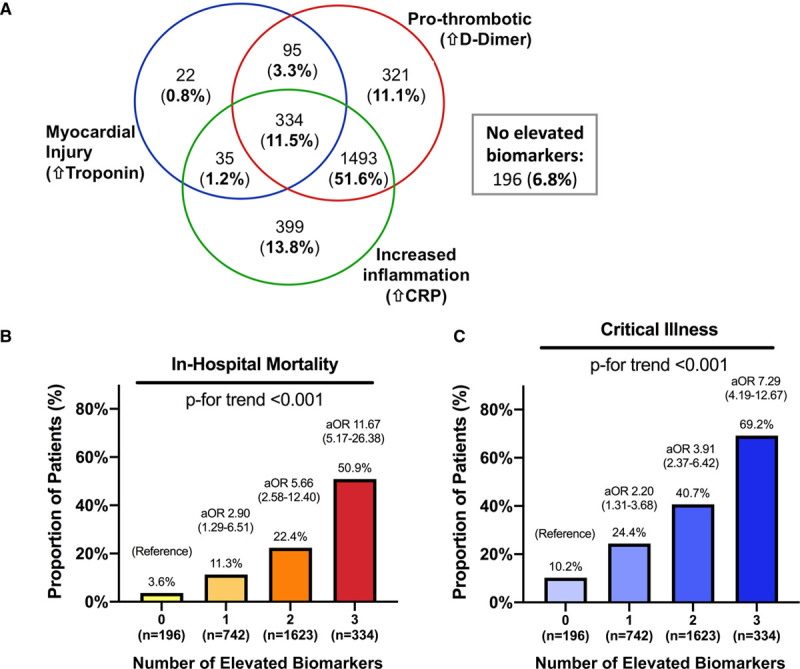
The frequency of elevated biomarkers reflecting myocardial injury, coagulation, and inflammation in COVID-19 and associations with in-hospital outcomes. A, Venn diagram illustrating overlap of elevated biomarkers at the time of initial hospital presentation in patients with COVID-19 and ≥1 elevated biomarker (n=2699). One hundred ninety-six patients had no elevated biomarkers. The proportion of patients with in-hospital mortality (B) and critical illness (C) are shown stratified by the number of elevated biomarkers measured at hospital presentation with COVID-19. Odds ratios (versus 0 biomarkers elevated) shown in B and C are adjusted for age, sex, race, body mass index, tobacco use, hypertension, hyperlipidemia, diabetes, chronic kidney disease, prior myocardial infarction, prior heart failure, atrial fibrillation, temperature at presentation, pulse oximetry at presentation, and outpatient prescriptions for antiplatelets, statin, and β-blockers. aOR indicates adjusted odds ratio; and CRP, C-reactive protein.
In this analysis of patients with COVID-19, 93% had myocardial injury, abnormalities in coagulation, or marked inflammation at hospital presentation. The combination of abnormalities across these pathobiological axes of disease provided incremental prognostic information for risk stratification. Patients with 1, 2, and 3 elevated biomarkers had 3-, 6-, and 11-fold higher adjusted odds of death, respectively, compared with patients who had COVID-19 with no elevated biomarkers at presentation. These findings extend prior observations on the prognostic nature of these biomarkers in COVID-19 and provide a framework for rapid estimation of risk.
This study was retrospective, and selection bias cannot be excluded. Only in-hospital events were recorded. We used dichotomous biomarker data to generate a simple scoring system for clinical use. A threshold higher than the ULN was selected for CRP, myocardial injury was defined by site-specific values for the cTn ULN, and high-sensitivity cTn assays were not used. Last, a separate validation cohort was not available. Still, a simple multimarker strategy, in which patients are categorized based on the number of elevated biomarkers, was effective to identify patients at risk for in-hospital adverse events.
Sources of Funding
Dr Smilowitz is supported, in part, by the National Heart, Lung, and Blood Institute of the National Institutes of Health (grant no. K23HL150315). Dr Newman is funded, in part, by the National Heart, Lung, and Blood Institute of the National Institutes of Health (grant no. K23HL125991). Dr Berger is funded, in part, by the National Heart, Lung, and Blood Institute of the National Institutes of Health (grant no. R01HL139909 and R35HL144993).
Disclosures
Dr Smilowitz reports consulting for Abbott Vascular. The remaining authors report no conflicts.
Footnotes
Contributor Information
Nathaniel R. Smilowitz, Email: Nathaniel.Smilowitz@nyulangone.org.
Vuthy Nguy, Email: Vuthy.Nguy@nyulangone.org.
Yindalon Aphinyanaphongs, Email: yin.a@nyulangone.org.
Jonathan D. Newman, Email: jonathan.newman@nyumc.org.
Yuhe Xia, Email: yuhe.xia@nyulangone.org.
Harmony R. Reynolds, Email: harmony.reynolds@nyumc.org.
Judith S. Hochman, Email: judith.hochman@nyumc.org.
Glenn I. Fishman, Email: glenn.fishman@me.com.
References
- 1.Berger JS, Kunichoff D, Adhikari S, Ahuja T, Amoroso N, Aphinyanaphongs Y, Cao M, Goldenberg R, Hindenburg A, Horowitz J, et al. Prevalence and outcomes of D-dimer elevation in hospitalized patients with COVID-19. Arterioscler Thromb Vasc Biol. 2020;40:2539–2547. doi: 10.1161/ATVBAHA.120.314872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smilowitz NR, Jethani N, Chen J, Aphinyanaphongs Y, Zhang R, Dogra S, Alviar CL, Keller N, Razzouk L, Quinones-Camacho A, et al. Myocardial injury in adults hospitalized with COVID-19. Circulation. 2020;142:2393–2395. doi: 10.1161/CIRCULATIONAHA.120.050434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS, Berger JS. C-reactive protein and clinical outcomes in patients with COVID-19 [published January 15, 2021]. Eur Heart J. doi: 10.1093/eurheartj/ehaa1103. https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehaa1103/6100979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daniels JM, Schoorl M, Snijders D, Knol DL, Lutter R, Jansen HM, Boersma WG. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108–1115. doi: 10.1378/chest.09-2927 [DOI] [PubMed] [Google Scholar]
- 5.Komiya K, Ishii H, Teramoto S, Takahashi O, Eshima N, Yamaguchi O, Ebi N, Murakami J, Yamamoto H, Kadota J. Diagnostic utility of C-reactive protein combined with brain natriuretic peptide in acute pulmonary edema: a cross sectional study. Respir Res. 2011;12:83. doi: 10.1186/1465-9921-12-83 [DOI] [PMC free article] [PubMed] [Google Scholar]


