Abstract
Background:
Due to the relative early lockdown in India, relative greater availability of reverse transcription polymerase chain reaction (RT-PCR) testing, and mandate to admit all positive corona virus disease 2019 (COVID-19) patients, the protocol in our hospital is to perform a baseline chest X-ray (CXR) at the time of admission and for follow up. There are currently limited publications demonstrating the radiographic findings and the role of CXR of COVID-19 patients at presentation.
Aims:
Evaluatethe radiographic findings on CXR in COVID-19 patients at presentation. Recommend a guideline for its judicious use.
Settings and Design:
Retroprospective study performed on RT-PCR confirmed COVID-19 patients admitted in our hospital between March 31,2020 to May 25, 2020. The study included symptomatic and asymptomatic patients. CXR was performed for218 patients.
Materials and Methods:
Portable bedside CXR was performed. The CXRs were evaluated by three radiologists to record the findings and grade the disease. All variables were expressed as mean, ranges, counts, and percentages.
Results:
157 patients (72%) were symptomatic and 61 (28%) were asymptomatic. 104 CXRs (48%) were abnormal (97 in symptomatic (62%) and fourin asymptomatic (6%)). 74 patients (47%) in the symptomatic group had known comorbidities and of these, 62 (84%) had abnormal CXR. 97 CXRs (93%) had bilateral findings and 87 CXRs (84%) had peripherally predominant abnormalities. The lower zone was the most common area of involvement (73%). Ground glass opacity (GGO) was the most common finding (94%–98 CXRs). Mild disease was seen in 56 (54%).
Conclusion:
CXR can be used to assess symptomatic COVID-19 patients at presentation and to grade the severity of disease. It may be avoided in asymptomatic patients.
Keywords: Chest X-ray (CXR), COVID-19, consolidation, ground glass opacity
Introduction
The world is in the midst of an ongoing pandemic by novel corona virus COVID-19, which started in Wuhan, China in December 2019. The disease is believed to have a zoonotic origin and is highly infectious.[1] The virus was named COVID-19 by WHO in February 11, 2020 and severe acute respiratory syndrome coronavirus 2 (SARS COV -2) by the International Committee of Taxonomy of Viruses.[2] It has rapidly spread from China to a total of 213 countries and territories till date, including major part of the densely populated country like India which accounts for 17.7% of the total world population.[3]
The disease primarily affects the respiratory system before causing other systemic complications and may be fatal. Early detection and diagnosis are of paramount importance to isolate the patient and prevent transmission.[4] The disease has four stages: stage 1 is the first appearance of disease; stage 2 is local transmission; stage 3 is community transmission, and stage 4 is widespread outbreak. Classical clinical presentation is varied ranging from mild fever, sore throat, dry cough, and malaise to pneumonia and severe respiratory disease syndrome. Patients may rapidly deteriorate with dyspnea, severe illness, and acute respiratory distress syndrome (ARDS) and often require intensive care unit (ICU) admission andoxygen therapy, especially those with advanced age and comorbidities.[5,6] The confirmatory diagnosis is made by RT -PCR on throat swab, sputum, other respiratory secretions, andblood samples.
During the early phase of the pandemic in countries such as China and Italy, CT scan played a significant role in establishing the diagnosis, management, and monitoring disease, due to its high sensitivity and specificity in detecting pulmonary changes.[7,8] However, as the disease spread globally, testing with RT-PCR became more widely available and government-mediated lockdowns andsocial distancing came into effect, and the role of CT in diagnosis and follow up has now become limited.[9] CXR is an easily available investigation tool in resource-constrained geographies; can be readily performed in the emergency department and is portable; and detects typical lung changes which facilitate early diagnosis.[10,11] Clinical deterioration happens rapidly in the disease and chest radiograph is able to assess progression.[10,12]
The aim of our study was to evaluate the findings in CXR in symptomatic and asymptomatic patients with COVID-19 disease at presentation and recommend a guideline for judicious use of CXR.
Patient population and study design
The inclusion criteria were patients admitted in our hospital with a RT-PCR diagnosis of COVID-19, irrespective of the age and gender. One patient was excluded from our study as she was pregnant and CXR was not performed. Period of enrolment in our study was from March 31, 2020 toMay 25, 2020. A total of 218 patients were included in our study.
Materials and Methods
This retroprospective study was approved by our institutional review board. Written informed consent was obtained as a part of the admission formalities. No author has any conflict of interest to declare in relation to this study.
Clinical data
The study included symptomatic and asymptomatic patients diagnosed by nasopharyngeal and oropharyngeal swab test for RT-PCR for COVID-19. The hospital protocol was to admit all COVID-19 positive patients irrespective of symptoms, as per government regulation prevalent at the time of study.[13]
CXR protocol
Dedicated portable digital radiography (DR) mounted X-ray machines (Fuji Microskan Mobile DR) were positioned in the hospital emergency room (ER) and COVID isolation ward. All X-rays were performed on the bedside by the following protocol: 80 kVp and5 mAs. The images were sent to an enterprise radiology information system - picture archiving and communication system (RIS-PACS), centricity viewer, GE Medical Systems (Milwaukee, WI, USA), and reported on dedicated reporting workstations.
Imaging analysis: The CXR pattern of COVID-19 patients wereanalyzed by three experienced radiologists (9 years, 21 years, and 23 years of experience) Following CXR abnormalities were recorded: unilateral or bilateral; symmetrical or asymmetrical; peripheral or central or both; specific findings including ground glass opacity, consolidation, nodularity, reticular opacities, and pleural effusion[8,10] [Figure 1]. These terms were used in accordance to the Fleischner Society glossary of terms.[14] Peripheral location is termed for opacities lateral to mid clavicular line and central location for opacities medial to this line. Zonal predominance (upper, middle, or lower zone) of the findings was also noted. The severity of disease on CXR was also graded as proposed by the British Society of Thoracic Imaging into mild (white area more than black area), moderate (equal white and black areas), or severe (more white area than black area) based on the area of involvement of lung opacities.[15]
Figure 1 (A-D).
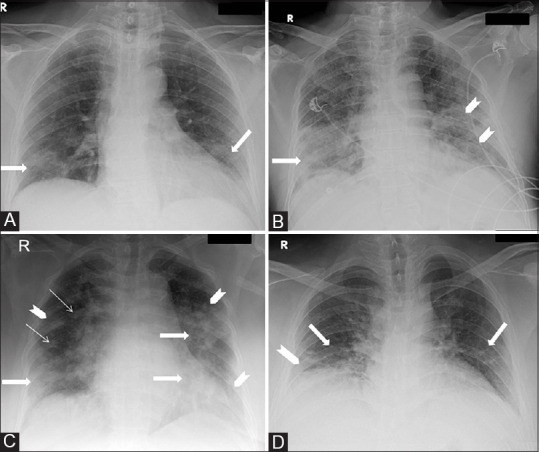
CXR AP views of four different COVID-19 patients at presentation demonstrating various specific findings. (A) Subtle GGOs (arrows) are seen in bilateral lower zones. (B) Consolidation (arrow) is seen in the right lower zone and GGOs are seen in left lower zone (arrow heads). (C) Consolidations are seen in the bilateral lower zones and left mid zone (thick arrows); peripheral GGOs (arrow heads) are seen bilaterally and nodules (thin arrows) are seen in the right mid zone. (D) Reticular opacities are seen in bilateral lower zones (arrows) along with small GGOs in the right lower zone (arrow head)
Statistical analysis
All variables were expressed as mean and ranges and categorical variables as counts and percentages.
Results
Patient population and clinical data
The study population included 218 patients (140 males and 78 females). The age range was from 18 years to 81 years. The age data was reported in Chart 1. The mean age was 49 years among males, 43 years among females, and cumulative mean age was 47 years. 157 patients were symptomatic and 61 were asymptomatic. The mean age of symptomatic patients was 46 years and that of asymptomatic was 40 years. 81 patients had comorbid conditions like diabetes, hypertension, coronary artery disease, chronic renal disease, chronic obstructive pulmonary disease (COPD), and malignancy. One asymptomatic patient had underlying pulmonary tuberculosis with no other radiographic findings. Full results are reported in Table 1.
Chart 1.
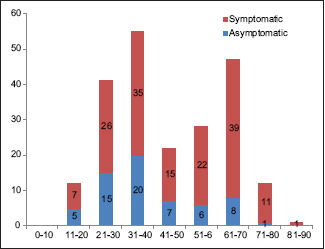
Bar diagram demonstrating the age range of all symptomatic and asymptomatic patients in years (X-axis) and their numerical counts (Y-axis)
Table 1.
Patient population and clinical data
| Total number of patients | 218 |
| Males | 140 (64%) |
| Females | 78 (36%) |
| Age range | 18-81 years |
| Mean age | 45 years |
| Total number of symptomatic patients | 157 (72%) |
| Total number of asymptomatic patients | 61 (28%) |
| Mean duration at presentation from onset of symptoms | 6.2 days |
| Total patients with comorbid conditions | 81 (37%) |
| Hypertension | 58 |
| Diabetes mellitus | 31 |
| Chronic kidney disease | 23 |
| Coronary artery disease | 17 |
| Chronic obstructive pulmonary disease | 8 |
| Malignancy | 5 |
Characteristic pathological findings in CXR
Our study comprised of CXR of 218 patients (157 symptomatic and 61 asymptomatic patients). A total of 104 CXRs (48%) were abnormal (97 in symptomatic patients and fourin asymptomatic patients).
A total of 97 CXRs (93%) had bilateral finding [Figure 2a] (65/97-66% had asymmetrical and 32/97-34% had symmetrical disease [Figure 3]) and sevenCXRs (7%) had unilateral findings [Figure 2b]. A total of 87 CXRs (84%) had peripheralpredominance of abnormalities, sixCXRs (6%) had central abnormalities, and 10 CXRs (10%) had both central and peripheral findings. Isolated lower zone involvement was seen in 35 CXRs (34%) and isolated mid-zone involvement was seen in four (4%). Lower zone dominant with mid-zone involvement was seen in 17 (16%), mid-zone dominant with lower zone involvement in four (4%) and diffuse involvementin 12 CXRs (11.5%).
Figure 2 (A and B).
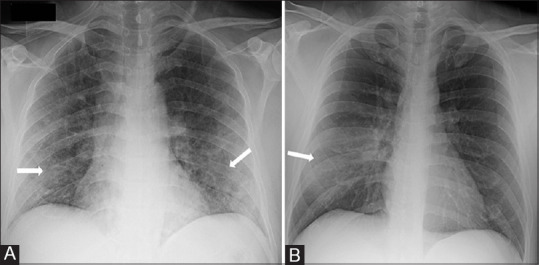
CXR AP views of two different COVID-19 patients demonstrating bilateral and unilateral abnormalities. (A) 42 Y/M presented with six days of fever, cough, and malaise. CXR shows bilateral lower zone peripheral GGOs (arrows). (B) 37 Y/M presented with six days of fever and history of recent contact with a COVID-19 patient. CXR shows unilateral abnormality of consolidation in the right lower zone (arrow)
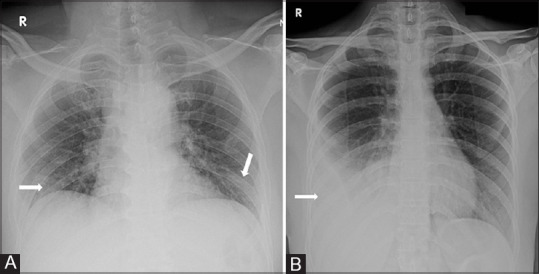
Figure 3 (A and B).
CXR AP views of two different COVID-19 patients demonstrating asymmetrical and symmetrical abnormalities. (A) 72 Y/M presented with fever and malaise since 10 days. CXR shows bilateral lung parenchymal abnormalities (right more than left) with areas of bilateral lower zone consolidations (arrows) mixed with right middle zone GGOs (arrow head). (B) 64 Y/F with history of diabetes mellitus presented with fever and dry cough since six days. CXR shows bilateral symmetrical lung parenchymal abnormalities with areas of consolidations (arrows) mixed with GGOs (arrow head)
GGO was seen in 94% (98 CXRs; as a dominant finding in 39, where multiple findings were seen); consolidation were seen in 52% (54 CXRs; dominant in 17); and reticular opacities were seen in 13% (14 CXRs; dominant in four); nodularity was seen in 2% (2CXR, nondominant), and pleural effusion in 21%(22 CXRs; dominant in fourCXRs; it was the only finding in oneCXR). 64% (14 of 22) patients showing consolidation had comorbid condition. Mild disease was seen in 56 (54%), moderate in 33 (32%), and severe in 15 (14%) [Figure 4]. Most of the abnormal CXRs (81 of 104—78%) and the entire severe grade CXRs (15 of 15—100%) were seen in 5–10 days of onset of symptoms. The average time lag for obtaining the baseline X-ray was 6.2 days from the day of onset of symptom. Detailed CXR findings are reported in Table 2. Comorbid conditions were present in 37% patients of our study population. Of the 157 symptomatic patients, 74 patients (47%) had underlying comorbidities. Of these 74 symptomatic patients with known comorbidities, CXR was abnormal in 62 patients (84%). Fifty six patients had GGOs and 17 had consolidation. Of the 15 patients with severe CXR findings, nine (60%) had underlying with comorbid conditions.
Figure 4 (A-C).
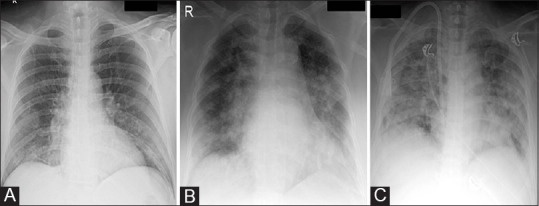
CXR AP views of three different COVID-19 patients demonstrating radiographic grading of severity of disease. (A) Mild grade: small areas of GGOs occupying bilateral lower zones and the abnormal white area is less than the normal black area. (B) Moderate grade: GGOs seen in bilateral peripheral and central lung parenchyma and the areas of white and black are equal. (C) Severe grade: GGOS seen diffusely infiltrating the lung parenchyma and the white area is more than the black area
Table 2.
Characteristics of Chest X-rays in COVID-19 patients (all numerical specify the total number in specific category and their percentage)
| Total CXR | 218 |
| Abnormal CXRs | 104 (48%) |
| Abnormal CXRs in symptomatic patients | 97/157 (62%) |
| Abnormal CXRs in asymptomatic patients | 4/61 (6.5%) |
| Abnormal CXRs in symptomatic patients with comorbid conditions | 62/74 (84%) |
| Abnormal CXRs in symptomatic patients without comorbid conditions | 32/83 (38.5%) |
| Distribution of abnormalities | |
| CXRs with unilateral abnormalities | 7 (7%) |
| CXRs with bilateral abnormalities | 97 (93%) |
| CXRs with symmetrical abnormal findings | 32 (34%) |
| CXRs with asymmetrical abnormal findings | 65 (66%) |
| CXRs findings having peripheral location | 87 (84%) |
| CXRs findings having central location | 6 (6%) |
| CXRs findings having combined peripheral and central location | 10 (10%) |
| Isolated Lower zone abnormality | 35 (34%) |
| Isolated Middle zone abnormality | 4 (4%) |
| Lower zone dominance with middle zone abnormality | 17 (16%) |
| Middle zone dominance with lower zone abnormality | 4 (4%) |
| Diffuse | 12 (11.5%) |
| Prevalence of specific radiographic abnormalities | |
| Ground glass opacities (GGOs) | 98 (94%) |
| Consolidation | 54 (52%) |
| Nodularity | 2 (2%) |
| Reticular opacity | 14 (13%) |
| Pleural effusion | 22 (21%) |
| Grading of disease severity on CXR | |
| Mild | 56 (54%) |
| Moderate | 33 (32%) |
| Severe | 15 (14%) |
CXR – Chest x-ray; GGO- Ground glass opacity
Discussion
There are limited studies till date discussing radiographic findings of COVID-19 infection at presentation on CXR and its role in management.[10] We conducted a retroprospective study on analyzing the CXR radiographic findings at presentation for patients confirmed to be RT-PCR positive for COVID-19.
The CXR findings in our study were in accordance with other studies published till date on the radiological findings of COVID-19 patients showing the predominance of GGOs with bilateral, peripheral, and lower zone distributions.[12,16,17,18] However, most of these studies used CT scan for evaluation of patients and only few studies used both CXR and CT. Ho Yuen et al. in Hong Kong[10] conducted a similar study and we found some interesting differences: our population had higher prevalence of GGOs (94% v/s 47%) and pleural effusion (21% v/s 3%). The GGOs are characterized as an early pulmonary finding and our study group had an average lower time lag of 6.2 days of baseline CXR from the onset of symptoms as compared to 10–12 days in their study, thus showing a higher prevalence of consolidation which is a later manifestation of disease.[6,10,18] 68% (15/22) of pleural effusion in our study was seen in patients having prior comorbidities (11of these patients had chronic kidney disease (CKD), which may attribute to thehigher prevalence in comparison to the studies by Ho Yuen et al and others.[18,19] However, in one patient without any comorbidity, pleural effusion was the only finding [Figure 5] which could not be explained.
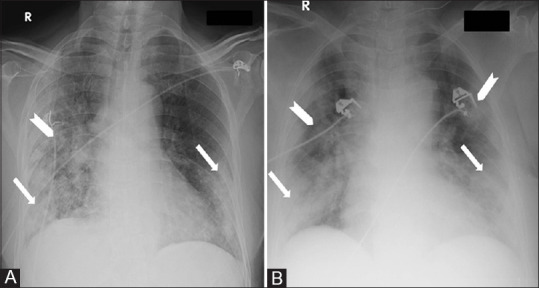
Figure 5 (A and B).
(A) CXR AP view of a 30 Y/M asymptomatic COVID-19 patient showing small GGOs in bilateral lower zones (arrows). (B) CXR AP view of a 32 Y/F presenting with fever and cough since fivedays and history of contact with COVID-19 patient shows pleural effusion on right side without any other specific lung parenchymal abnormality
There are significant differences in the incidence, prevalence, and management of COVID-19 pandemic in different parts of the world, influenced by various factors, including travel restrictions, social distancing, government-driven lockdowns, and population demographics. This has led to differences in the burden of disease in the healthcare systems across the world. In India, the government enforced early travel restrictions and a nationwide lockdown and there has been a lower case per million population incidences of proven cases of COVID-19 and the present government policy of admission of all positive patients possibly demonstrated an earlier manifestation of disease in our group.[20]
We have found that CXR has a vital role in the baseline evaluation of symptomatic patients and a limited role in asymptomatic patients. There is also a higher number of CXRs with positive findings in symptomatic patients with preexisting comorbid conditions, thereby increasing the value of CXR in this subgroup. In our study, this group also had a higher prevalence of severe disease.
The positive CXRs also showed findings specific to COVID-19 disease indicating the ability of CXR to make a specific diagnosis and likely differentiate the disease from other conditions in the right geographical andclinical scenario. In the likelihood of the increasing number of COVID-19 patients in countries such as India, where there is prevalence of other lung diseases such as pulmonary tuberculosis (also in one of the patient in our study), CXR also has the potential for improving the confidence level of differentiating COVID-19 related findings from other prevailing ailments showing CXR abnormalities at presentation.
Due to the faster turnaround of reporting and a higher percentage of abnormal CXRs and high specificity of radiographic findings in these patients in our study, we see a potential role of performing CXR in symptomatic patients in regions with high disease burden and/or limited RT-PCR testing to triage patients requiring admission from those needing home quarantine.
Our study has the limitations of a small dataset and beingfocused on the radiographic findings at presentation in both asymptomatic and symptomatic patients. The correlation between the radiographic findings at presentation with duration of disease, severity, and outcomes needs evaluation.
The evolution of radiographic findings in symptomatic patients’, correlation with the clinical course of disease, and utility of serial CXRs in clinical management needs further research.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ge H, Wang X, Yuan X, Xiao G, Wang C, Deng T, et al. The epidemiology and clinical information about COVID-19. Eur J Clin Microbiol Infect Diseases. 2020;39:1011–9. doi: 10.1007/s10096-020-03874-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang W, Sirajuddin A, Zhang X, Liu G, Teng Z, Zhao S, et al. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19) Eur Radiol. 2020 doi: 10.1007/s00330-020-06827-4. doi: 10.1007/s00330-020-06827-4. 2020 Apr 15 : 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National registration of Indian citizens. Office of the Registrar General & Census Commissioner, India. Ministry of Home Affairs, Government of India. [Last updated on 2020 Jul 16]. Available from: https://censusindia.gov.in .
- 4.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu N, Zhang DY, Wang WL, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases? [Last accessed on 2020 May 29];Radiology. 2020 doi: 10.1148/radiol.2020200642. doi: 10.1148/radiol.2020200642. [Published on 2020 Feb 26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT features of COVID-19 in Rome, Italy. [Last accessed on 2020 Apr 25];Radiology. 2020 doi: 10.1148/radiol.2020201237. doi: 10.1148/radiol.2020201237. [Published 2020 Apr 03] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hope MD, Raptis CA, Henry TS. Chest computed tomography for detection of coronavirus disease 2019 (COVID-19): Don’t rush the science. [Last accessed on 2020 Apr 26];Ann Intern Med. 2020 doi: 10.7326/M20-1382. doi: 10.7326/M20-1382. Online ahead of print April 8, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. [Last accessed on 2020 Apr 25];Radiology. 2020 doi: 10.1148/radiol.2020201160. doi: 10.1148/radiol.2020201160. [Published on 2020 Mar 27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. [Last accessed on 2020 Apr 30];AJR Am J Roentgenol. 2020 :1–7. doi: 10.2214/AJR.20.23034. doi: 10.2214/AJR.20.23034. Ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.Jacobi A, Chung M, Bernheim A, Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review. Clin Imaging. 2020;64:35–42. doi: 10.1016/j.clinimag.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Revised Guidelines on Clinical Management of COVID-19. Government of India Ministry of Health & Family Welfare Directorate General of Health Services. [Last accessed on 2020 Apr 25]. Published on 2020 Mar 31. Available from: https://www.mohfw.gov.in/pdf/RevisedNationalClinicalManagementGuideline for COVID19 .
- 14.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: Glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 15.Guidance for the Reporting Radiologist British Society of Thoracic Imaging. [Last accessed on 2020 Mar 30]. Published on 2020 Mar 16. Available from: https://www.bsti.org.uk/media/resources/files/BSTI_COVID-19 Radiology Guidanceversion 2_16.03.20.pdf .
- 16.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect Dis. 2020;20:425–34. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song FX, Shi NN, Shan F, Zhang ZY, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–7. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–39. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 19.Lee EY, Ng MY, Khong PL. COVID-19 pneumonia: What has CT taught us? Lancet Infect Dis. 2020;20:384–5. doi: 10.1016/S1473-3099(20)30134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Novel Corona disease (COVID 19) Situation update report-13. India: World Health Organization; [Last accessed on 2020 Apr 30]. Published on 2020 Apr 26. Available from: https://www.who.int/docs/default-source/wrindia/situation-report/india-situation-report-13.pdf . [Google Scholar]


