Abstract
Objective:
To analyze radiological changes in portable chest radiographs in coronavirus disease-19(COVID-19) patients to optimize the management of hospitalized patients.
Methods:
We retrospectively reviewed 638 portable radiographs of 422 hospitalized COVID-19 patients with RT-PCR confirmed COVID-19 infection. All the radiographs were reported in a structured format by two experienced radiologists. A severity score was assigned to every Chest Xray (CXR) and correlation was done with the CT scans whenever available.
Results:
Out of 422 baseline portable radiographs assessed, the ratio of male: female patients was 337:85 that is 79.8% were males and 20.14% were females. The mean age was 50.5 years and the range was 17–84 years. Of these 422 patients, 187 patients (44.3%) had abnormal baseline CXR. 161 out of 187 (86%) had either typical or indeterminate findings for COVID-19 pneumonia, rest 26 (13.9%) patients had CXR findings not consistent with COVID-19, like pleural effusion, hydropneumothorax, or lung cavity. Most commonly observed CXR findings in COVID 19 pneumonia were bilateral, multifocal air space opacities (consolidation and ground-glass opacities) predominantly involving lower zones and peripheral lung fields. X-ray identifiable lung changes of COVID-19 were mostly seen at 9-11 days after symptom onset.
Conclusion:
The presence of multifocal air-space opacities with bilateral, peripheral distribution on chest radiograph is highly suggestive of COVID-19 pneumonia in this pandemic setting. Portable chest radiography is a widely available and quicktool for estimating the evolution and assessing the severity of lung involvement of COVID-19 pneumonia in hospitalized symptomatic patients.
Keywords: CT-computed tomography, CXR-chest radiography, GGO-ground glass opacity, RT-PCR – reverse transcriptase polymerase chain reaction
Introduction
Since the first case of SARS-CoV-2 pneumonia reported in Wuhan in December 2019,[1] the Coronavirus Disease 2019 (COVID-19) has rapidly spread worldwide. Respiratory distress has been the principal source of morbidity and mortality in advanced disease.[2] Thoracic imaging with chest radiography (CXR) and Computed Tomography (CT) are key tools for pulmonary disease management.
Exponentially increased burden over the radiology department for imaging COVID-19 patients in this globally emerging pandemic has been challenging to cope with the background of limited available infrastructure.[3]
In radiology, the diagnostic value of CT for SARS-CoV-2 infection has been widely discussed[4,5] However, there are certain limitations of CT scan like infection control issues, CT room decontamination, imaging critically ill patients, and limited availability. Therefore, mobile chest radiography remains the most commonly utilized modality for management of COVID-19 pneumonia.[6]
CXR is insensitive in mild or early COVID-19 infection.[7] Detailed evaluation of COVID-19 pneumonia including clinical worsening is far better with CT relative to CXR.[8] Ultimately, the choice of imaging modality depends upon the clinical judgment at the point-of-care, accounting for the differing attributes of CXR and CT, availability of CT scanner, and radiologist.
Materials and Methods
A retrospective analysis of 638 chest X rays of 422 patients who were admitted between April 15 to May 15 as COVID-19 suspects and confirmed later by reverse RT-PCR on nasopharyngeal and throat swabs was done at the study institute. All 422 patients had baseline CXR and 216 patients had follow up CXRs. All CXRs were acquired as computed radiographs on three portable radiography machines (Allengers mars 4.2) dedicated to isolation wards and ICU. Few patients also underwent concurrent CT as advised by the clinical team. Written informed consent was waived off for this study by our institutional review board in wake of the exceptional situation of a pandemic.
Scanning protocol and preparations
Ours being the COVID-19 dedicated hospital, we emphasized on portable radiography to largely prevent in-hospital cross-contamination while maintaining consistent workflow and good quality diagnostic imaging in view of the limited availability of digital radiography units. Cross-contamination to radiographer and other patients through cassettes is another problem. Certain infrastructure based measure were taken in our department which are summarized as follows;
To prevent cross-infection within the hospital, three portable radiography CR machines and one CT machine was dedicated exclusively to COVID-19 patients. The non-COVID-19 patients were scanned separately.
All the healthcare professionals in the Radiology department were educated using a short educational video that involved entire steps of donning and doffing, along with disposal of the PPE after use.
The CR cassette for COVID-19 X rays was first wrapped up in a plastic sheet and taped securely. We used garbage disposal bags for the same which were readily available in our hospital supply.
The radiographer was accompanied by an assistant to the ward and ICU. The radiographer scanned patient in full PPE, the assistant meanwhile waited outside the ward.
After the x-ray exposure, the radiographer discarded, and disposed of the plastic cover in the ward as per guidelines without touching the inner CR cassette.
The CR cassette was handed over to the assistant waiting outside the ward and was disinfected with 95% alcohol-containing solution before transferring to the radiology unit where the CR reader was positioned.
The portable CR radiography unit was also similarly double-coated with a polythene garbage disposal bag and after every round of ward and ICU, the outer sheet was disposed of in the ward and the machine was parked in a secure space of the ward after disinfection.
Image analysis
Baseline as well as follow up CXRs were analyzed by two radiologists with 8 − 10 years of experience. The standard reporting format was used as below [Table 1].
Table 1.
Reporting format for CXR
| CXR FINDINGS | PRESENT/ABSENT | DISTRIBUTION (CENTRAL/PERIPHERAL) | PREDOMINANCE (APICAL/BASAL) | ZONES | |||||
|---|---|---|---|---|---|---|---|---|---|
| RUZ | RMZ | RLZ | LUZ | LMZ | LLZ | ||||
| GROUND GLASS OPACITIES | |||||||||
| CONSOLIDATION | |||||||||
| CAVITY | |||||||||
| NODULES | |||||||||
| UNDERLYING LUNG DISEASE | |||||||||
| LYMPHADNOPATHY | |||||||||
| PLEURAL EFFUSION | |||||||||
| SEVERITY SCORE | |||||||||
| IMPRESSION | |||||||||
A visual assessment severity score (RALE-Radiographic Assessment of Lung Odema derived byWarren, et al.[9]) was also calculated based on total lung involvement [Table 2].
Table 2.
Visual Assessment Severity Score
| VISUAL ASSESSMENT OF OVERALL AREA OFLUNG INVOLVEMENT | SCORE |
|---|---|
| 0 | 0 |
| 1-25% | 1 |
| 25-50% | 2 |
| 50-75% | 3 |
| >75% | 4 |
| FINAL SCORE | 8 |
| SEVERITY ASSESSMENT | Final score |
| MILD | 3 |
| MODERATE | 4-6 |
| SEVERE | >6 |
Table 3: Shows X-ray descriptors used for final impression as per performa described by BSTI (British Society of Thoracic Imaging)[10]
Table 3.
Final descriptors for X ray report
| NORMAL | NO FINDINGS ON CXR: COVID-19 NOT EXCLUDED |
|---|---|
| CLASSIC/PROBABLE | LOWER LOBE PREDOMINANT, |
| PERIPHERAL PREDOMINANT, | |
| MULTIPLE AREAS OF CONSOLIDATION | |
| +/-GGOs | |
| INDETERMINATE | DOES NOT FIT CLASSIC/NON-COVID-19 DESCRIPTORS |
| NON-COVID-19 | LOBAR PNEUMONIA, CAVITY, |
| PLEURAL EFFUSION, PNEUMOTHORAX, | |
| PULMONARY EDEMA |
Aims
To evaluate the role of portable chest radiography in managing COVID-19 patients (BY ASSESSING X-RAY SEVERITY SCORE)
To describe the time course of CXR findings relative to symptom onset
To describe typical COVID -19 features on CXR so that clinicians and radiologists can identify incidental COVID-19 in scans done for other purposes.
Inclusion criteria
All patients who were admitted as COVID-19 suspects and later confirmed to be COVID-19 positive on RT-PCR
All COVID-19 positive patients who underwent portable radiographs and image quality had been diagnostic.
Exclusion criteria
Patients who were diagnosed and being treated for pre-existing lung disease including interstitial lung disease, allergic/asthmatic bronchitis, etc.
Poor quality portable radiographs due to unfavorable position/motion artefacts.
Results
Patient characteristics:
From April 15 2020 to May 15, 2020, 638 mobile chest X-rays were performed in 422 COVID-19 patients (Male: Female, 337:85). The mean age of the study population was 50.5 years (Range, 17–84).
Among total 422 patients, 152 patients were asymptomatic, 225 were having mild symptoms like fever, cough, and rest 45 had moderately severe symptoms like breathlessness. Fever and cough were the most frequent symptoms.
Severity of respiratory disease:
Mild: no or mild (absence of hypoxemia).
Moderate to severe: evidence of significant pulmonary dysfunction or damage.
(e.g., hypoxemia, moderate to- severe dyspnea).
The most common co-morbidities were Diabetes (21%), Hypertension (17.8%), and Hypothyroidism (6.0%). 25 patients were TB defaulters.
Outcome:
Among these 422 patients, 360 patients (85.3%) survived and 62 patients (14.6%) had died. Among the survivors (n = 360), 312 were discharged, 45 needed assisted ventilation (including those requiring oxygen by mask and mechanical ventilation),12 patients were still in hospital as on May 15. A total of 131 patients underwent follow up X rays during hospital stay.
The image quality was reasonably diagnostic for all the portable X-rays. Out of these 422 patients, 187 patients (44.3%) had abnormal baseline CXRs.
CXR features:
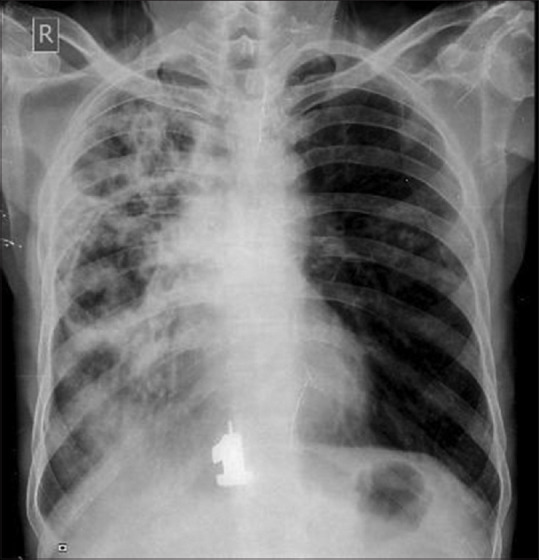
Baseline CXR: The most common reported chest radiograph findings of COVID-19 pneumonia were multifocal air space opacities (consolidation and ground-glass opacities) with bilateral, peripheral, and lower lung predominance–termed as typical for COVID-19 (110 patients, 26.06%) [Figure 1 and Table 4].
Figure 1.
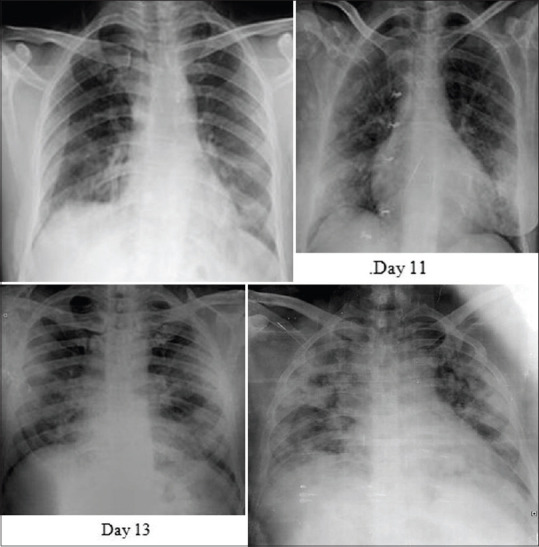
Typical COVID pattern: CXR (PA view) of four different patients shows bilateral peripheral consolidations. Typical pattern with final score 3/8 (mild), 5/8 (moderate),6/8(severe), and 7/8(severe) respectively in 1,2,3, and 4 according to extent of lung involvement
Table 4.
(Original) Final diagnoses on CXR
| MAIN FINDINGS | NO (PERCENTAGE) |
|---|---|
| TYPICAL | 110 (26.06%) |
| INDETERMINATE | 51 (12.08%) |
| NON-COVID | 26 (6.16%) |
| NEGATIVE | 235 (55.7%) |
There were few patients who had either few hazy suspicious opacities or unilateral opacities which didn’t fit into typical COVID-19 pattern or non-COVID-19 diagnosis and termed as indeterminate for COVID-19 (51 patients, 12.08%) [Figure 2].
Figure 2.
CXR of 55-year-old male shows left-sided peripheral air space opacities—categorized as Indeterminate pattern
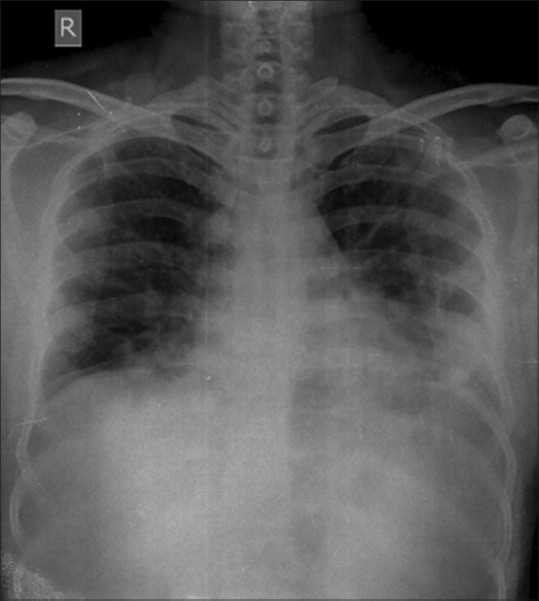
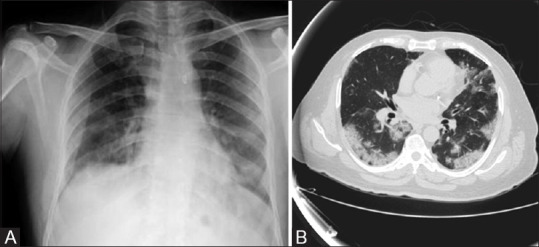
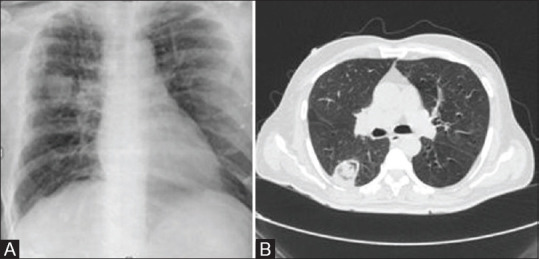
A comparison with CT scan was also done in patients whenever available [Figures 3 and 4].
Figure 3 (A and B).
(A) CXR of 44-year-old patient shows bilateral peripheral air space opacities predominantly bilateral lower zones - Typical COVID-19 (Xray severity score of 2/8). (B) Axial HRCT Chest shows a typical pattern for COVID-19 with CT severity score of 11/25
Figure 4 (A and B).
(A) CXR (PA view) shows bilateral peripheral air space opacities in lower zones—Typical COVID, Score 4/8.(B) Coronal HRCT Chest shows typical for COVID-19 with CT severity score of 20/25
Consolidation was the most common finding (140 patients, 33.18%), the second most common finding was ground-glass opacities (88 patients, 20.85%). The frequency of air space opacities showing bilateral, peripheral, and basal distribution was 110 (26.06%),139 (32.94%), and 146 (34.59%), respectively.
Most of baseline CXRs were performed in the first week at our institute. X-ray identifiable findings were most apparent at 9–11 days from disease onset.
Few patients had CXR findings which were not consistent with diagnosis of COVID-19 like the presence of pleural effusion (14 patients), unilateral lobar/segmental consolidation (10 patients), hydropneumothorax (1 patient), and lung cavity (1 patient) [Figures 5–7].
Figure 5.
CXR shows right-sided patchy opacities along with cavitation suggestive of tuberculosis—categorized as NON-COVID-19 pattern.
Figure 7.

CXR shows right-sided mild pleural effusion- categorized as NON-COVID-19 pattern
Figure 6 (A and B).
(A) CXRshows rounded mass-like consolidation in right mid lung zone—proved as fungal pneumonia later on HRCT chest- NON-COVID-19 pattern.(B) Axial HRCT chest shows thin-wall cavity within apical segment of the right lower lobe with soft tissue density lesion suggestive of fungal etiology
The average X-ray severity score was 2.8(out of 8) in the mild symptom group and 4.2(out of 8) in the moderately severe group of patients.
Thereby, patients with X-ray severity score less than 3 considered as mild and were given symptomatic treatment, and93% of patients with moderately severe symptomatic patients X-ray severity score more than or equal to 4 (i.e., 42 out of 45 patients) required assisted ventilation, i.e., 35 required oxygen by mask and 7 were mechanically ventilated (intubated). Therefore, X-ray severity score 4 was considered a baseline for critical care management.
Rest (n = 235,55.70%) patients were negative for pneumonia on CXR.
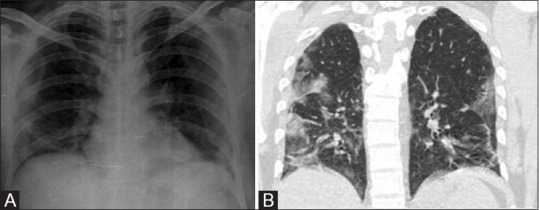
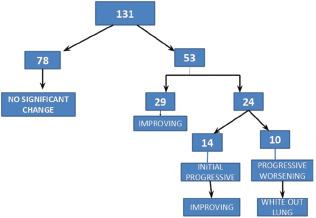
Follow up CXRs: Among 131 patients who underwent follow up X-rays were having either moderate to severe symptoms at presentation or they worsened clinically during the hospital course. Follow-up X rays were taken at 2-3 days interval.(FLOW CHART).
Out of these 131 patients, 78 patients had no significant change in follow-up X-rays. There were 29 patients who showed partial resolution on successive X-rays, 24 patients had a progressive increase in lung opacities. Out of these 24 patients, 14 improved on follow up while 10 had progressive worsening and ultimately resulted in whiteout lung. There were 8 patients who had normal baseline X-rays done in the first week of symptom onset, and visible air space opacities seen on successive X-rays done in the second week (7–10 days). All these serial changes were reported as a change in final severity scores [Figure 8].
Figure 8.
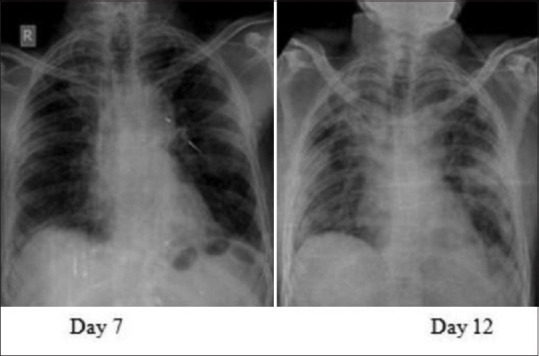
CXR of 48-year-old male shows peripheral air space opacities in bilateral mid zones on Day 7 (Score-2). Significant progression is seen by Day 12 involving upper, mid, and lower zones bilaterally (Score- 6)
Discussion
We retrospectively analyzed a group of 422 hospitalized patientswith laboratory-confirmed COVID-19 infection. Most of COVID-19 patients had mild symptoms, commonly fever and cough 0.161 out of 422 baseline CXR (38.39%), had either typical or indeterminate findings for COVID-19 pneumonia. Our results show poor correlation with the study done by Wong HYF et al. which reported a baseline CXR sensitivity of 69%[7]
This can be attributed to X-rays being performed in the early phase of the disease in our institute.
The most commonly observed CXR findings in COVID-19 pneumonia was bilateral multifocal air space opacities (consolidation) predominantly involving lower zones and peripheral lung consistent with previous case series[6,11,12]
Subtle GGO, a finding in early disease course may not be visible on X rays. X-ray identifiable lung changes of COVID-19 were mostly seen at 9–11 days after symptom onset which correlates well with previous data on CT provided by Pan F et al., stating peak lung parenchymal changes at 6–11 days.[13]
X-ray Severity score was assessed according to the extent of lung involvement on X-ray. All our patients with positive CXR for organizing pneumonia, CT showed similar lung pictures with comparable severity scores which correlates well with a review article by Jacobi A et al. stating that, in cases of high clinical suspicion for COVID-19, a positive CXR may obviate the need for CT.[6]
Most of the patients with clinical deterioration showed increasing consolidations on serial radiographs which is consistent with the study by Hosseiny M et al. stating that older age and progressive consolidation might suggest a poorer prognosis.[14] In moderately severe symptomatic patients, CXR showed white out lung due to diffuse air space opacities as in any infectious or inflammatory cause of ARDS.
Pleural effusion was seen in14 patients, an uncommon observation, which is consistent with a study done by Salehi S et al. Other rare findings described in literature like lung cavity, pneumothorax were seen in two patients in our study (one in each).[15]
Unilateral lobar/segmental consolidation wasseen in 10 patients which were proved later as either co-existent bacterial superinfection or tubercular disease. These results are consistent with a study done by Vilar J et al. stating that community-acquired bacterial pneumonia have unilobar/unisegmental consolidation as opposed to multifocal multilobar opacities in viral pneumonias.[16]
Most of our study patients with no symptoms or mild symptoms at presentation, had normal CXR, while most of the patients with moderate to severe symptoms at presentation or who deteriorated later had abnormal baseline CXR findings. Follow-up X-rays of all patients with clinical deterioration showed progressive worsening resulting in whiteout lungs due to ARDS.
Our results are consistent with the consensus statement from Fleischner society about recommendations for imaging in COVID-19 patients which states that “imaging is not routinely indicated for COVID-19 in asymptomatic individuals or those having mild features with low risk of disease progression. Imaging is indicated for patients with moderate to severe features of COVID-19 or with evidence of worsening respiratory status regardless of COVID-19 test results. In a resource-constrained environment where access to CT is limited, CXR may be preferred for patients.”[17]
X-ray severity score assigned to patients with mild and moderately severe symptomatic patients corresponded well to the CT severity score (whenever available) and thereby helping in appropriate management of COVID-19 patients.
We found portable chest X-rays provided reasonably good image quality for helping in assessing the severity of lung involvement and in the follow-up of COVID-19 pneumonia in symptomatic population during the late course of the disease. Therefore, it is a simple, widely available and quickalternativeto CT scan in critically ill COVID-19 patients.
Conclusion
The presence of multifocal air-space opacities with bilateral, peripheral distribution on chest radiographs is highly suggestive of COVID-19 pneumonia in this pandemic setting.
We found portable chest X-rays provided reasonably good image quality for helping in assessing the severity of lung involvement and in follow up of COVID-19 pneumonia in symptomatic population during late course of the disease. Therefore, it is a simple, widely available and quick alternativeto CT scan in critically ill COVID-19 patients.
Therefore, indications for imaging in COVID-19 patient being, patient with mild symptoms with risk factors, patients with moderate to severe features of COVID-19 regardless of RT-PCR result, worsening clinical status of patients, or associated complications.
We can also conclude that imaging should not be used as a screening tool for asymptomatic patients, for diagnosis of COVID-19 pneumonia, or for patients with mild symptoms without risk factors.
However, CXR can be used as a first-line tool in critical resource constraint areas such as primary health centers so that timely isolation of the suspect population can be implemented.
Limitation
Detection sensitivity of CXR for diagnosing COVID-19 pneumonia cannot be calculated due to the lack of non-COVID-19 control group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basha MM, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology department preparedness for Covid-19: Radiology scientific expert panel. Radiology. 2020;295:E8. doi: 10.1148/radiol.2020200988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestation of new Coronavirus disease 2019 (COVID-19): A pictorial review. Eur Radiol. 2020;30:4381–9. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H. Outbreak of novel coronavirus (COVID-19): What is the role of radiologists? Eur Radiol. 2020;30:3266–7. doi: 10.1007/s00330-020-06748-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacobi A, Chung M, Bernheim A, Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review. Clin Imaging. 2020;64:35–42. doi: 10.1016/j.clinimag.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et al. Frequency and distribution of chest radiographic findings in patients positive forCOVID-19. Radiology. 2020;296:E72–8. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orsi MA, Oliva AG, Cellina M. Radiology department preparedness for COVID-19: Facing an unexpected outbreak of the disease. Radiology. 2020;295:E8. doi: 10.1148/radiol.2020201214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warren MA, Zhao Z, Koyama T, Bastarache JA, Shaver CM, Semler MW. Severity score of lung odema on the chest radiograph is asscociated with clinical outcomes in ARDS. Thora×. 2018;73:840–6. doi: 10.1136/thoraxjnl-2017-211280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thoracic Imagingin.COVID-19Infection.Guidance for the Reporting Radiologist. British Society of Thoracic Imaging. Version 2. 16th March. 2020 [Google Scholar]
- 11.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease: Analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng MY, Lee E, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection: Radiologicfindings and literature review. Radiol Cardiothorac Imaging. 2020;2:e200034. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus peumonia. Radiology. 2020;295:715–21. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myer L. Radiology perspective of coronavirus disease 2019(COVID-19): Lessons from severeacute respiratory syndrome and Middle East respiratory syndrome. Cardiopulmonary Imaging. 2020;214:1078–82. doi: 10.2214/AJR.20.22969. [DOI] [PubMed] [Google Scholar]
- 15.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): Asystematic review of imaging findings in 919 patients. AJR Am J Roentgen. 2020;14:87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 16.Vilar J, Domingo ML, Soto C, Cogollos J. Radiology of bacterial pneumonia. J Eur J Radiol. 2004;51:102–13. doi: 10.1016/j.ejrad.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: A multinational consensus statement from the Fleischner Society. Radiology. 2020;296:172–80. doi: 10.1148/radiol.2020201365. [DOI] [PMC free article] [PubMed] [Google Scholar]


