Abstract
Objective:
Arthroplasty is the common treatment for intracapsular femoral neck fractures in the elderly. Recent studies have shown that there may be more overall complications related to uncemented hemiarthroplasty compared to cemented, including more subsidence, intraoperative fractures, and postoperative fractures. Uncemented femoral components rely on a press fit, and the risk of these complications would be expected to increase in patients with unrecognized distal extension of femoral neck fractures. The purpose of this study is to determine the frequency of fracture extension of displaced femoral neck fractures in the elderly population.
Methods:
The electronic medical record database at our institution was retrospectively reviewed to search for consecutive reports from 2005 to 2015 of patients 65 years or older that sustained an intracapsular femoral neck fracture who had computed tomography (CT) examinations of the injury. Exclusion criteria were CTs that were not fine cut (<1.5 mm cuts) or occult femoral neck fractures that were seen only on magnetic resonance imaging. This resulted in 60 patients that were included in the study. Within this subset of patients, the CT scans were reassessed to look for extension of the fracture beyond the boundaries of the femoral neck. Of particular interest, were fracture lines that extended distal to the femoral neck, since these have the potential to affect the fit of an uncemented femoral stem. Data on subject age, gender, body mass index (BMI), and bone mineral density (BMD) were also collected, and it was determined if these demographics were predictive in patients having fracture extension. Treatment and follow-up data were collected for the patients as well.
Results:
Seven of 60 patients were identified to have fracture extension of intracapsular femoral neck fractures. The frequency of fracture extension of intracapsular femoral neck fractures distal to the femoral neck was 8.3% (5/60). All cases of fracture extension were nondisplaced or minimally displaced. 60% (3/5) of the distal fracture extensions were not diagnosed preoperatively by the radiologists or the treating orthopaedic surgeons. There was not a statistically significant difference when comparing age, gender, BMI, or BMD of the population group with distal fracture extension to that of the rest of the patient cohort.
Conclusions:
To our knowledge, this is the first study to report the frequency of fracture extension of displaced femoral neck fractures in the elderly population. The 8.3% rate of distal fracture extension in elderly femoral neck fractures may help explain the higher rate of subsidence, postoperative fracture and intraoperative fracture when applying uncemented hemiarthroplasty compared to cemented arthroplasty. It is important to be aware of the potential for this phenomenon.
Keywords: cemented vs uncemented, geriatric hip fracture, hemiarthroplasty, total hip arthroplasty
1. Introduction
Hip fractures in the elderly are becoming an increasingly common source of morbidity and mortality worldwide. Hemiarthroplasty and total hip arthroplasty are the treatments of choice for the majority of displaced intracapsular femoral neck fractures in patients over the age of 65 years.[1–18] However, there is still controversy whether femoral fixation should be performed with an uncemented or cemented technique in this patient population.[1–18] In the United States, uncemented technique is popular due to decreased operative time, decreased blood loss and surgeon familiarity with the uncemented technique.[16–18] Historically, there have been case reports that cemented hip arthroplasty caused rare but severe cardiovascular complications including death, and it is one of the reasons uncemented femoral fixation gained popularity.[3,4,16–18] However, several studies have reported that cemented prostheses have less pain and improved postoperative mobility.[5,6,10–15] Recent prospective studies reported increased surgical complications related to uncemented hemiarthroplasty compared to cemented hemiarthroplasty, including stem subsidence, and a higher rate of intraoperative and postoperative periprosthetic fractures.[1–5,7,8]
The underlying cause(s) of the increased stem subsidence and perioperative periprosthetic fracture rates has not been well studied. We hypothesize that undetected fracture extensions exist in a subset of intracapsular femoral neck fractures which could be a reason for the increased prevalence of stem subsidence, and intraoperative and postoperative fractures in uncemented hip arthroplasty. The calcar/metaphyseal bone is important for the stability and fit of uncemented prostheses, and if there is fracture extension to this area it could lead to failure, especially during femoral canal broaching and/ or postoperative weight bearing. To our knowledge, the prevalence of fracture extension associated with elderly intracapsular femoral neck fractures has not been reported in the orthopaedic literature.
A knowledge of the frequency of fracture extension in this patient group could potentially change the preoperative work-up and surgical technique selected by the operating surgeon. The goal of this paper was to elucidate the prevalence of fracture extension associated with intracapsular femoral neck fractures in patients 65 years or older.
2. Methods
This study is a single center, retrospective chart review using the electronic medical record database at our institution. The study was institutional review board approved and complied with Health Insurance Portability and Accountability Act guidelines with exemption status for individual informed consent. A search was performed in the database for consecutive reports of patients 65 years or older that sustained a hip fracture who had CT examinations of the abdomen/pelvis or dedicated hip at the time of injury. The data search range was between January 1, 2005 and March 18, 2015, which resulted in 70 patients. Eligible CT examinations were required to be fine cut, ≤1.5 mm, with appropriate hip reconstructions. Eight patients were excluded from the study because they did not meet the imaging requirements. Two patients with occult hip fractures that were seen on magnetic resonance imaging but not on CT scans were also excluded. Basicervical and intertrochanteric fractures were excluded. This left us with 60 patients who sustained intracapsular femoral neck fractures seen on CT with appropriate imaging. Data on subject age, gender, BMI, and BMD were also collected (Table 1).
Table 1.
Age, sex, BMI, and BMD distribution of patients with distal fracture extension compared to the remainder of the patient cohort.
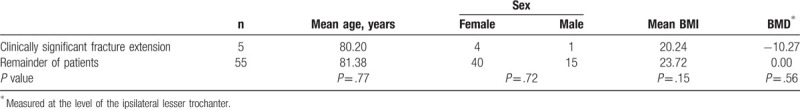
In order to assess the BMD data already gathered on CT scans, opportunistic measurements of calibrated attenuation values in trabecular bone were obtained, as described previously.[19] Briefly, a round 2-cm region of interest was placed within the medullary canal to measure the BMD in Hounsfield units on an axial image at the level of the lesser trochanter on the ipsilateral side of the fracture in question. The femoral neck was not measured because blood next to an acute fracture in the medullary canal spuriously increases Hounsfield unit values. The ipsilateral side was used because occasionally the patient had hardware in place on the contralateral hip that altered measurements. Care was taken to avoid inclusion of the fracture, as well as cortical bone or focal lesions in bone. Measurements were performed using multidetector CT scans acquired at a single energy (120 kVp) using bone windowing and a 512 × 512 matrix. Examinations had been acquired with and without intravenous contrast material, but previous research has shown that the diagnostic performance of opportunistic CT did not significantly differ with versus without contrast use in patients with DEXA-proven osteoporosis.[20] A student's unpaired t-test was used to compare age, BMI, and BMD of the group with distal fracture extension to the remainder of the patient cohort. A chi-square analysis was used to determine if there was a difference in gender demographics of the group with distal fracture extension to the remainder of the patient cohort (Table 1).
All CT scans were assessed for fracture extension by an orthopaedic resident and reviewed by a senior musculoskeletal attending radiologist and 2 senior orthopaedic surgeons. Extension of the fracture was defined as a separate fracture line that went beyond the boundaries of the intracapsular femoral neck. Fracture lines that extended distal to the intracapsular femoral neck were of particular interest because it is necessary to have good supporting bone in the calcar/metaphyseal region for the stability and fit of an uncemented implant. There were 45 patients 65 years or older that sustained a hip fracture who did not obtain a CT scan. We analyzed the patients’ injury mechanisms based on the notes within the electronic medical record to determine whether patients sustained the injury from a low (i.e., ground level fall) or a high-energy mechanism (i.e., pedestrian versus automobile accident). Chi-square analysis was used to determine whether there was a statistically significant difference in injury mechanism in the patient population that did and did not receive CT scans.
3. Results
The overall frequency of fracture extension of intracapsular femoral neck fractures was 11.7% (7/60). There were 2 incidences of proximal extension into the femoral head. Therefore, the frequency of distal fracture extension of intracapsular femoral neck fractures was 8.3% (5/60). All cases of fracture extension were nondisplaced or minimally displaced (<2 mm). Additionally, 3 of the 5 incidences of distal fracture extension were not diagnosed preoperatively by the treating orthopaedic surgeons or the final radiologist review. Figures 1 and 2 are radiographic examples of fracture extension.
Figure 1.
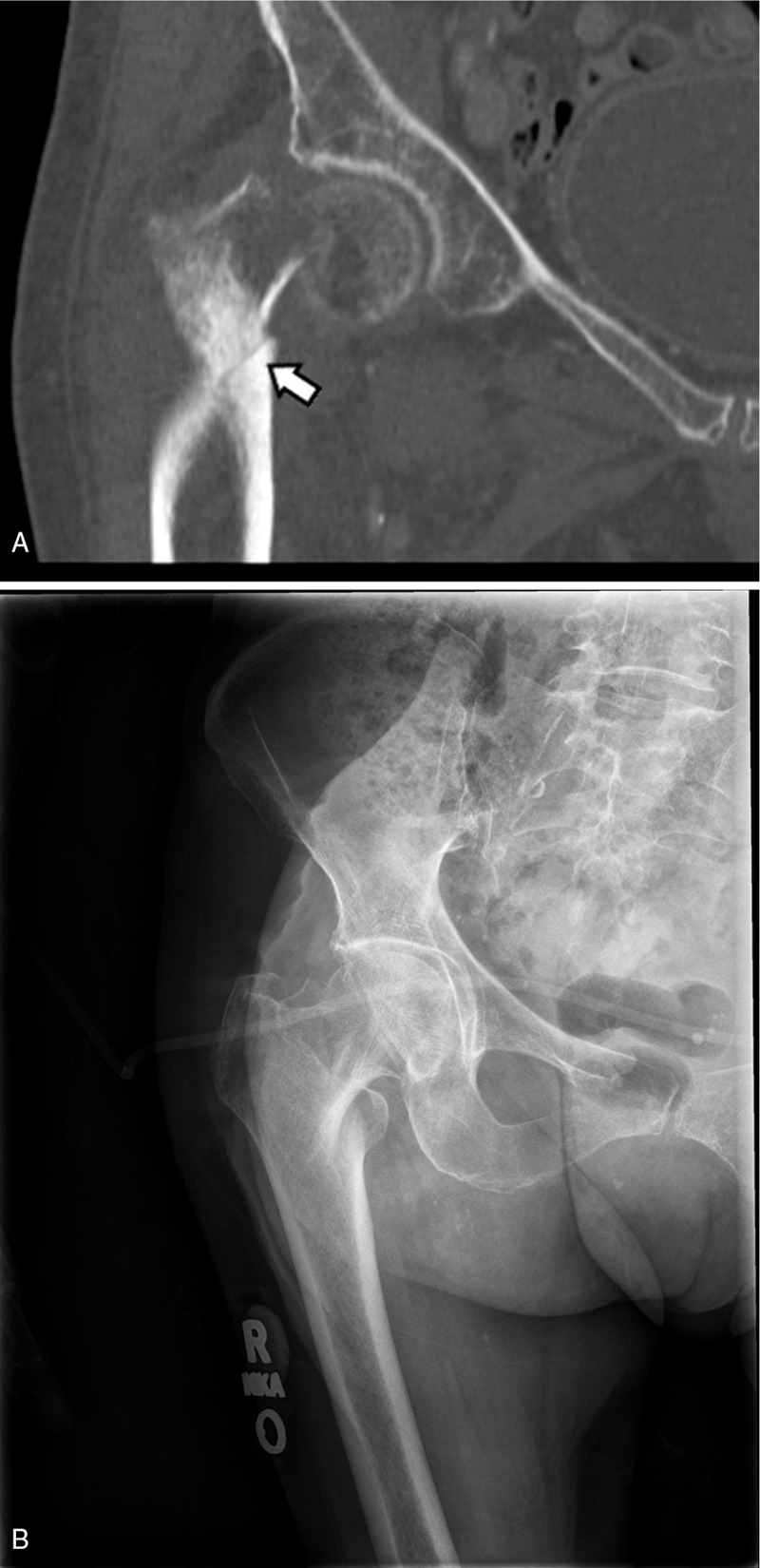
Evidence of distal fracture extension into the intertrochanteric region in an elderly intracapsular femoral neck fracture patient on CT (A) but not well seen on plain x-ray (B).
Figure 2.
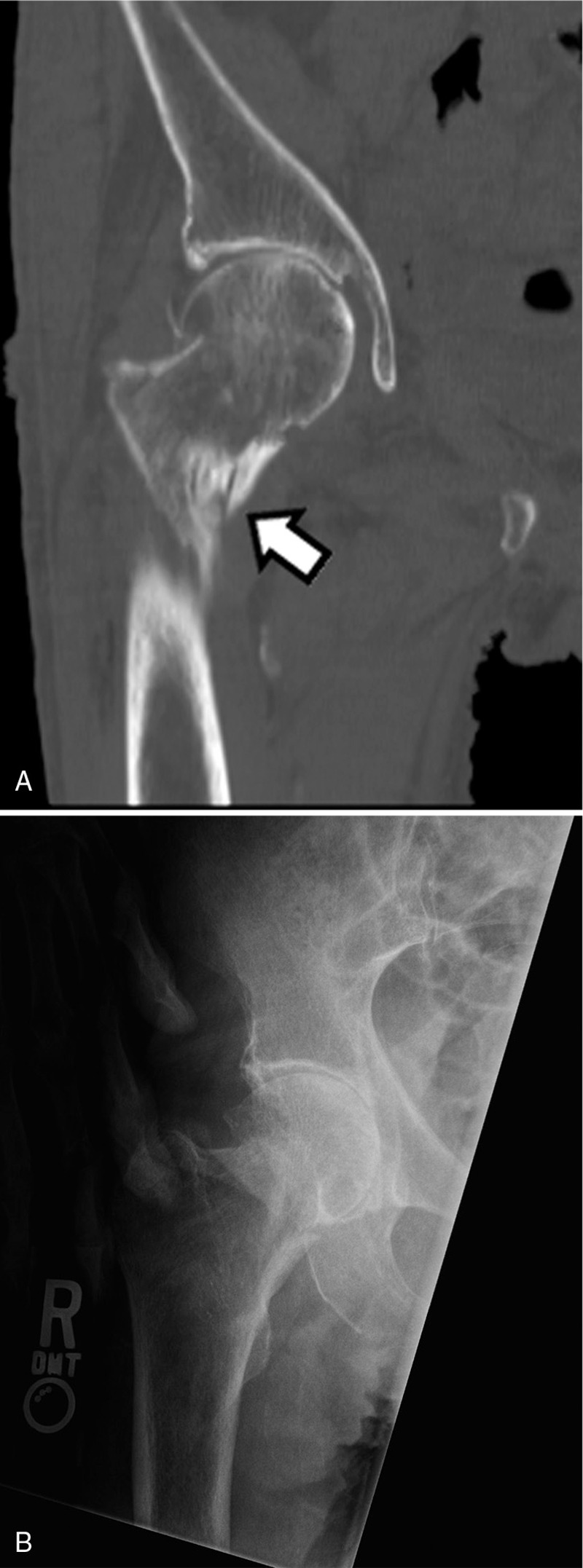
Evidence of distal fracture extension into the lesser trochanter in an elderly intracapsular femoral neck fracture patient on CT (A) but not well seen on plain x-ray (B)
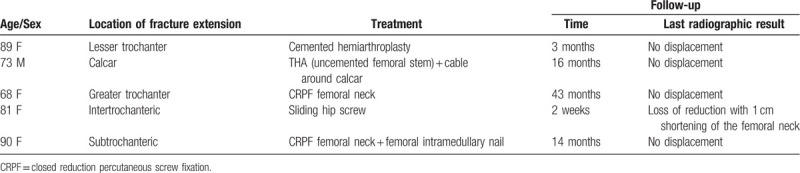
Two of the 5 patients with distal fracture extension were treated with hip arthroplasty (1 cemented and 1 uncemented). The cemented hemiarthroplasty was chosen because the treating surgeon noted “some motion” with the uncemented trial stem on the operative report. One of the 5 patients with fracture extension detected by CT had an intraoperative fracture, which was treated with a cerclage cable and total hip arthroplasty with an uncemented femoral stem. The other patients with distal fracture extension were treated as seen in Table 2. Amongst these patients, there were no other mentions of visualizing fracture extension on any of the intraoperative reports. Follow-up for these patients ranged from 2 weeks to 43 months, often limited because of death or they were lost to follow-up, but there was no evidence of complications for the 2 patients with distal extension of the femoral neck fracture treated with arthroplasty at the time of submission of this study (Table 2).
Table 2.
Diagnostic, treatment, and follow-up details of the patients with distal fracture extension.
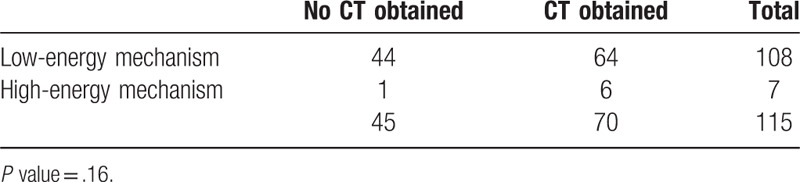
There was not a statistically significant difference when comparing age (P = .77), gender (P = .72), BMI (P = .15) or BMD (P = .56) of the group with distal fracture extension to the remainder of the patient cohort (Table 1). There was also no statistically significant difference in frequency of fracture extension when comparing nondisplaced femoral neck fractures (i.e., Garden I and II classification) versus displaced femoral neck fractures (Garden III and IV classification) (P = .61). Finally, there was no statistically significant difference in the type of injury mechanism (high energy versus low energy) between the hip fracture patient group that received a CT scan versus the group that did not (P = .16) (Table 3).
Table 3.
Comparing the difference in mechanism of injury in patients who obtained a CT pelvis/hip versus those that did not.
4. Discussion
Previous studies have reported an increased risk of subsidence and both intraoperative and postoperative periprosthetic fractures with uncemented hemiarthroplasty versus cemented hemiarthroplasty for the treatment of femoral neck fractures in the elderly.[1–5,7,8] In a large, retrospective study comparing cemented and uncemented hemiarthroplasty used in the treatment of elderly femoral neck fractures, it was shown that uncemented hemiarthroplasties had a 2.1 times increased risk of revision compared to cemented prostheses, which was largely due to periprosthetic fracture and aseptic loosening.[8] Additionally, the current American Academy of Orthopaedic Surgeons guidelines for managing hip fractures in the elderly recommend the use of cemented femoral stems due to the higher fracture risk with press-fit stems.[21] Despite the known increased risk of periprosthetic fracture, subsidence, and aseptic loosening when using an uncemented technique in the elderly femoral neck fracture patient population, there has been little insight into the cause of these increased complications. Our hypothesis is that there is a subset of femoral neck fractures that have unrecognized distal fracture extension, and when an uncemented femoral stem is applied, these fracture lines are propagated and can cause subsidence and loosening of the stem at the time of the operation or postoperatively after weight bearing is initiated. Knowledge of femoral neck fracture extension preoperatively would be important in determining the surgical technique chosen. Two of the 5 patients with distal fracture extension were treated with a hip arthroplasty. In one of those patients, the fracture extension, not recognized preoperatively, was observed intraoperatively and treated with a cable placed around the calcar and then insertion of an uncemented femoral stem. In the other patient, the surgeon noticed a “loose fit” of the uncemented stem and a cemented hemiarthroplasty was placed, although one cannot conclude this was due to the nondisplaced fracture extension. These patients may provide some evidence that unrecognized distal fracture extension is one of the reasons for the reported higher complication rates following uncemented hip arthroplasty. Another noteworthy finding is that 60% (3/5) of the distal fracture extensions were not diagnosed preoperatively by the radiologists or the treating orthopaedic surgeons. This gives insight into how often these associated nondisplaced fractures likely go unrecognized, even with fine cut CT scans.
There are several limitations to our study. There is an inherent selection bias since our data comes from a limited number of patients from a single institution. There is also a selection bias related to the fact that our studied patient population only included those that had received CT scans of their injury. CT scans were most often obtained via the coded trauma protocol of our institution to rule out intra-abdominal pathology or to evaluate for a source of blood loss. CTs were also obtained to better evaluate the fracture pattern or to determine if there was an occult fracture not seen on plain radiographs. We did address the potential confounding variable in our study that there may have been higher energy mechanisms in the patients that received a CT which could have led to increased fracture extension. We found there was no significant difference in the mechanism of injury between the patient group that received CT scans and the group that did not. We did not look at other characteristics between these 2 groups and cannot determine how this would affect our results.
Additionally, we do not have long-term follow-up on most of the patients because the patients were often lost to follow-up or died. We are unable to determine whether the increased subsidence and periprosthetic fracture rate seen with uncemented arthroplasty compared to cemented arthroplasty for femoral neck fractures is in fact due to unrecognized fracture extension. Clearly, further studies are warranted to validate the results of this pilot study. Much larger prospective studies utilizing CT scans should be performed to elucidate the true incidence of fracture extension of geriatric intracapsular femoral neck fractures and determine if fracture extension relates to an increased incidence of perioperative complications such as subsidence and perioperative fracture. Although there was no statistically significant difference in specific risk factors such as BMI and BMD of the fracture extension group, this may be due to our small sample size. Future studies looking into associated factors to help predict which patients are more prone to fracture extension would be useful as well.
5. Conclusion
To our knowledge, this is the first study to report the frequency of fracture extension of displaced femoral neck fractures in the elderly population. The 8.3% of femoral neck fractures with distal fracture extension is not insignificant and has the potential to affect clinical decision making. Unrecognized fracture extension may help explain the higher rate of subsidence, postoperative fracture, and intraoperative fracture when comparing uncemented arthroplasty to cemented arthroplasty. Additionally, it is important to be aware of the potential for this phenomenon because distal fracture extension may be non-displaced and easily overlooked on imaging.
References
- 1.Figved W, Opland V, Frihagen F, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009;467:2426–2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo CL, Tan SH, Lee HC. Intra-operative fractures in cementless bipolar hemiarthroplasty. J Orthop Surg (Hong Kong). 2015;23:218–222. [DOI] [PubMed] [Google Scholar]
- 3.Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012;94:577–583. [DOI] [PubMed] [Google Scholar]
- 4.Morris K, Davies H, Wronka K. Implant-related complications following hip hemiarthroplasty: a comparison of modern cemented and uncemented prostheses. Eur J Orthop Surg Traumatol. 2015;25:1161–1164. [DOI] [PubMed] [Google Scholar]
- 5.Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010;6:CD001706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures. J Bone Joint Surg (Br). 2010;92-B:116–122. [DOI] [PubMed] [Google Scholar]
- 7.Langslet E, Frihagen F, Opland V, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014;472:1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gjertsen JE, Lie SA, Vinje T, et al. More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11,116 hemiarthroplasties from a national register. J Bone Joint Surg. 2012;94-B:1113–1119. [DOI] [PubMed] [Google Scholar]
- 9.DeAngelis JP, Ademi A, Staff I, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012;26:135–140. [DOI] [PubMed] [Google Scholar]
- 10.Luo X, He S, Li Z, et al. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012;132:455–463. [DOI] [PubMed] [Google Scholar]
- 11.Khan RJ, MacDowell A, Crossman P, et al. Cemented or uncemented hemiarthroplasty for displaced intracapsular femoral neck fractures. Int Orthop. 2002;26:229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh GK, Deshmukh RG. Uncemented Austin-Moore and cemented Thompson unipolar hemiarthroplasty for displaced fracture neck of femur—comparison of complications and patient satisfaction. Injury. 2006;37:169–217. [DOI] [PubMed] [Google Scholar]
- 13.Foster AP, Thompson NW, Wong J, et al. Periprosthetic femoral fractures—a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005;36:424–429. [DOI] [PubMed] [Google Scholar]
- 14.Lausten GS, Vedel P. Cementing v. not cementing the Monk endoprosthesis. Injury. 1982;13:484–488. [DOI] [PubMed] [Google Scholar]
- 15.Lo WH, Chen WM, Huang CK, et al. Bateman bipolar hemiarthroplasty for displaced intracapsular femoral neck fractures. Uncemented versus cemented. Clin Orthop Relat Res. 1994;302:75–82. [PubMed] [Google Scholar]
- 16.Lennox IA, McLauchlan J. Comparing the mortality and morbidity of cemented and uncemented hemiarthroplasties. Injury. 1993;24:185–186. [DOI] [PubMed] [Google Scholar]
- 17.Faraj AA, Branfoot T. Cemented versus uncemented Thompson's prostheses: a functional outcome study. Injury. 1999;30:671–675. [DOI] [PubMed] [Google Scholar]
- 18.Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004;86-A:1983–1988. [DOI] [PubMed] [Google Scholar]
- 19.Gausden EB, Nwachukwu BU, Schreiber JJ, et al. Opportunistic use of CT imaging for osteoporosis screening and bone density assessment: a qualitative systematic review. J Bone Joint Surg Am. 2017;99:1580–1590. [DOI] [PubMed] [Google Scholar]
- 20.Pickhardt PJ, Pooler BD, Lauder T, et al. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158:588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. American Academy of Orthopaedic Surgeons: Management of Hip Fractures in the Elderly. Available at: http://www.aaos.org/research/guidelines/HipFxGuideline.pdf. Accessed October 11, 2018. Published September 5, 2014. [Google Scholar]


