Abstract
Objectives:
Aims of the present study were to establish generalizable outcome data on long-term functional outcomes and health-related quality of life (HRQoL) after operative treatment of pilon fractures on a large scale. Second, it was aimed to examine factors associated with these outcomes.
Design:
Retrospective cohort study with follow-up by questionnaire.
Setting:
Two level 1 trauma centers.
Patients:
Two hundred twenty-five of 480 eligible patients completed the survey (response rate 47%).
Intervention:
Open reduction internal fixation for tibial pilon fracture.
Main outcome measurements:
Ankle function measured using the Foot and Ankle Ability Measure, physical function using the Patient-Reported Outcomes Measurement System Physical Function (PROMIS PF, Short Form 10a) questionnaire and HRQoL using the EuroQol 5-Dimensions 3-Level (EQ-5D-3L) questionnaire.
Results:
At a medium follow-up of 82 months (82 (interquartile range (IQR), 45–120), median Foot and Ankle Ability Measure was 74 (IQR, 57–82), median PROMIS PF 49 (IQR, 44–57), median EQ-5D-3L 0.81 (IQR, 0.71–0.84). HRQoL was significantly lower compared to a reference population (P < .001). In multivariable regression analyses, smoking was associated with poorer HRQoL. Higher body mass index, deep infection, and lower HRQoL were associated with worse ankle function.
Conclusions:
Long-term patient-reported outcomes after operative treatment of pilon fractures reveal impaired functionality and lower HRQoL compared to an uninjured reference population. As pilon fractures can have significant effects on a patient's life, patients should be counseled about the expected long-term outcomes to set realistic expectations. This study emphasizes the importance of obtaining both general and region-specific measures when evaluating outcomes after injury, in order to evaluate the injury of interest in the accurate context.
Level of evidence:
Prognostic level III.
Keywords: functional outcome, ORIF, pilon fracture, quality of life, tibial fracture
1. Introduction
Pilon fractures are usually the result of high energy and axial loading.[1–3] These mechanisms often result in associated injuries of the lower extremity and other body regions. Amongst others, high-energy trauma typically results in significant damage of the surrounding soft tissues.[3–6] These soft tissue injuries contribute to the high rate of complications after open reduction internal fixation of pilon fractures.[2,4] High rates of infectious complications, posttraumatic arthritis, impaired union, nonunion, stiffness, and persistent pain after operative treatment of pilon fractures have been reported.[7–9]
It is believed that associated injuries, postoperative complications, and severity of the initial injury may influence long-term functioning of the lower extremity. Previously, the amount of associated (soft-tissue) injury, development of posttraumatic arthritis, severity of the pilon fracture, management of the surrounding soft tissues, type of operative treatment, and anatomic restoration of the articular surface have been described to influence outcomes.[1–3,10] However, long-term functional outcomes after operative treatment for pilon fractures have only been described in relatively small cohorts.[7,9,11–14] Even though it is generally accepted that high-energy mechanisms have negative influence on the eventual outcome of a pilon fracture, no solid evidence on its true influence is available.[8]
Therefore, the aims of the present study were to establish generalizable outcome data on long-term patient-reported functional outcomes and health-related quality of life after operative treatment of pilon fractures on a larger scale. Second, it was aimed to examine factors associated with these outcomes. This information will be useful to surgeons and healthcare providers in expectation management and clinical decision making regarding pilon fractures.
2. Methods
2.1. Study design and participants
This is a retrospective study with follow-up by questionnaire that was approved by our hospital institutional review board (IRB). Adult patients (age >18 years) who underwent open reduction internal fixation (ORIF) for a tibial pilon fracture between January 2000 and December 2015 at 2 level 1 trauma centers were identified using the institution's research patient data registry and a combined hospital operative database. Pilon fractures were defined as Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 43-B and 43-C fractures, excluding fractures deemed mainly tibial shaft with extension into the tibial plafond, and trimalleolar ankle fractures with the posterior malleolar fragment involving less than one-third of the articular surface.[3,8,15] Patients who underwent operative treatment for the pilon fracture at an outside facility, who had amputation of the operated foot or leg, who died during follow-up, were mentally impaired, or were unable to communicate in English, were excluded. All eligible patients were approached through a recruitment letter. No compensation was provided for participation in the study. Questionnaires were administered through telephone interviews or online through a secured web link, without a clinical visit. In case of nonresponse, patients were contacted multiple times in order to maximize the response rate. Responses were collected and managed using REDCap (Research Electronic Data Capture). REDCap is a secure, web-based application designed to support data capture for research studies.[16]
2.2. Outcome measures and explanatory variables
Data on demographics, body mass index (BMI), smoking status, diabetes, American Society of Anesthesiologists (ASA) score, mechanism of injury, fracture and treatment characteristics, and postoperative infections were extracted from electronic patient documentation. BMI was only considered when reported within a range of 6 months prior to or after ORIF. Smoking was considered positive if a patient was a current smoker at the time of surgery or quit smoking less than 2 weeks prior to the fixation. Energy of trauma was subdivided into low- and high-energy and was classified according to the Advanced Trauma Life Support guidelines, with high-energy trauma mechanisms including motor vehicle and motorcycle accidents, falls from height, and crush injuries.[17,18] Fractures were classified by 4 orthopaedic surgeons according to the AO/OTA classification and in case of uncertainty, consensus was reached by group discussion. Deep infection was defined as any type of infection at the surgical site that demanded operative treatment, according to the treating surgeon based on clinical signs with or without positive cultures.[19] All surgical site infections that required nonoperative treatments only (e.g., antibiotics, wound treatments), were considered superficial.
The primary outcome measure, patient-reported functional outcome, was measured using the Foot and Ankle Ability Measure (FAAM) and the PROMIS Physical Function (PROMIS PF) Short Form 10a questionnaires. HRQoL, the secondary outcome measure, was assessed using the EuroQol 5-Dimensions 3-Levels (EQ-5D-3L) questionnaire. The FAAM questionnaire consists of 29 questions assessing physical function in patients with musculoskeletal disorders of the leg, ankle, and foot; 21 questions on activities of daily living with an additional sports subscale containing 8 questions.[20] Scores range from 0 to 100 with higher scores representing higher physical function. The PROMIS PF questionnaire can be used to measure general physical functioning for both research and clinical practice purposes, with a mean score of 50 being representative of the general population of the United States.[21,22] The EQ-5D-3L questionnaire is a standardized instrument to measure generic health based on the level of experienced problems (no problems/some or moderate problems/extreme problems) at the 5 dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.[23] EQ-5D-3L scores for the study population were calculated using a scoring algorithm appropriate for a population of North-American patients, with higher scores representing better HRQoL.[23,24]
2.3. Statistical analyses
Distribution of continuous explanatory and outcome variables was assessed using the Shapiro–Wilk test. Frequencies and percentages were used to present categorical variables, medians, and IQR to display continuous variables. Baseline characteristics between responders and nonresponders were compared using Chi-squared and Mann–Whitney tests. The Student t test was used to compare EQ-5D-3L and PROMIS PF scores of the study population to the norms for a general North-American population of 0.88 and 50, respectively.[21,25] The strength of correlations between the 3 different outcome measures was assessed using Pearson's correlation coefficient. Associations between individual predictors and the patient-reported outcomes of interest were first determined by simple bivariate linear regression (Supplementary Table 1). The final models were selected by forward stepwise regression modeling to avoid overfitting. In this approach, predictors associated with the outcome by bivariate analysis were included in the multivariable regression model. Predictors no longer associated with the outcome were omitted only if doing so did not increase the deviance of the model. Predictors excluded at the bivariate analysis state were reincorporated only if doing so reduced the overall deviance of the model.[26] A 2-tailed P value of < .05 was considered statistically significant. STATA 13.1 (StataCorp LP, TX) was used for the conduct of all statistical analyses.
3. Results
Inclusion criteria were met by 480 patients, of whom 225 completed the survey for a total of 229 tibial pilon fractures (4 patients sustained bilateral injuries), leading to a response rate of 47%. Responders were significantly older, consisted of significantly fewer males and active smokers when compared with nonresponders. The main reason for nonresponse to follow-up by questionnaire was inability to contact the patients. There were no differences with respect to age, gender, race, and ethnicity for those completing the survey online versus by phone.
Median age at injury for the population of responders was 48 (IQR, 37–58) years; the majority of patients were male. Baseline characteristics are depicted in Table 1 and Table 2 shows the fracture and treatment characteristics.
Table 1.
Baseline characteristics (n = 225)
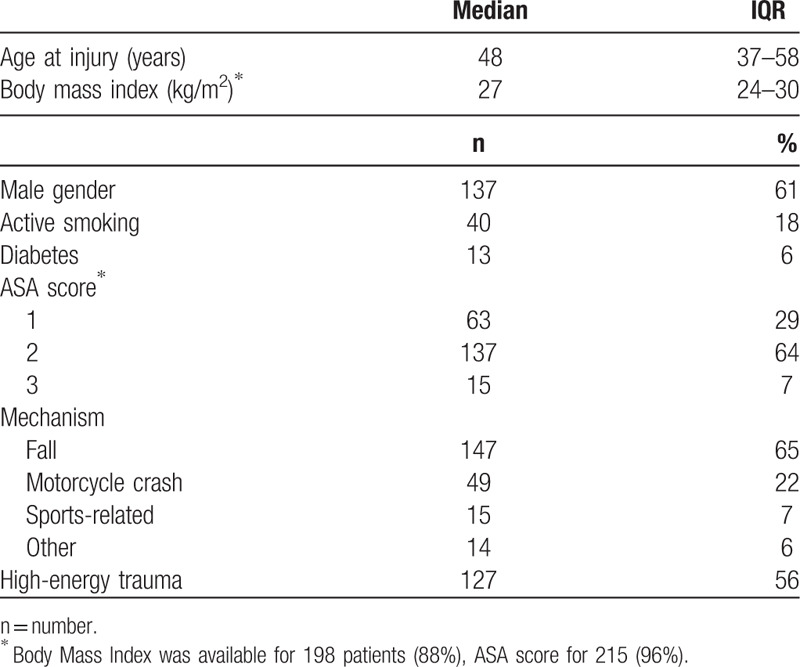
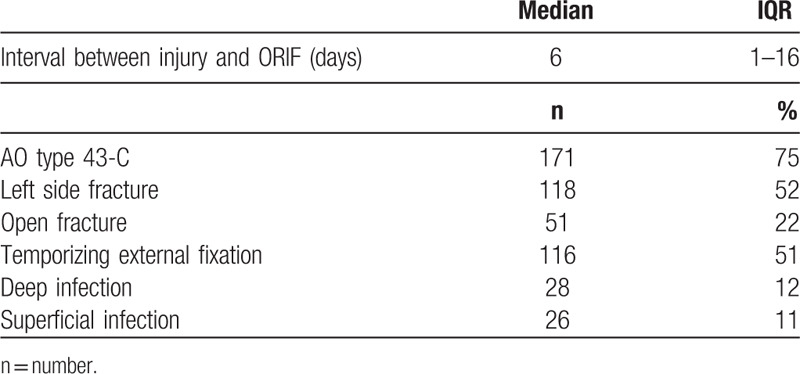
Table 2.
Fracture and treatment characteristics (n = 229).
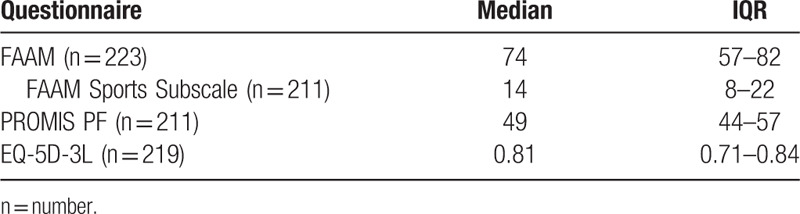
Patient-reported outcome questionnaires were completed after a median duration of 82 (IQR, 45–120) months from injury. Median FAAM score was 74 (IQR, 57–82) and 14 (IQR, 8–22) for the sports subscale (Table 3). PROMIS Physical Function scores had a median of 49 (IQR, 44–57), mean PROMIS PF score was 50 (standard deviation 7.8). HRQoL, measured using the EQ-5D-3L, was reported to be 0.81 (IQR, 0.71–0.84), significantly lower when compared to the 0.88 reference population score (P < .001).[25] For the EQ-5D-3L mobility dimension, nearly half of the patients reported problems in walking about. However, physical function mobility measured using the PROMIS PF was comparable to the general uninjured American population (P .90). All 3 outcome metrics were correlated; FAAM and PROMIS PF (correlation coefficient = 0.79, P < .001), FAAM and EQ-5D-3L (correlation coefficient = 0.69, P < .001), and PROMIS PF and EQ-5D-3L (correlation coefficient=0.50, P < .001). In general, worse HRQoL metrics (EQ-5D-3L scores) were proportional to FAAM and PROMIS PF scores.
Table 3.
Outcome measures
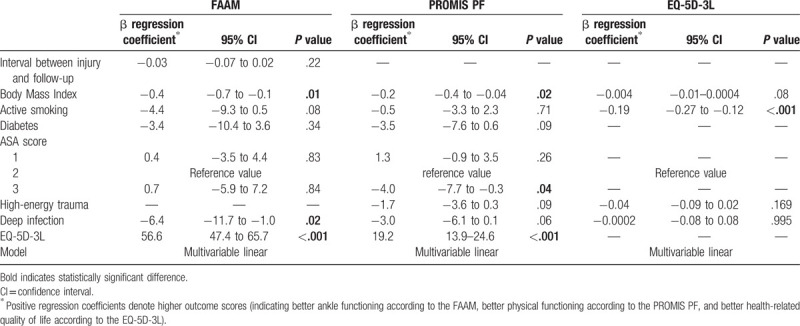
In multivariable regression analyses, higher BMI, deep infection, and lower HRQoL (assessed using the EQ-5D-3L) were found to be independently associated with worse ankle function measured with the FAAM (Table 4). Factors associated with lower PROMIS PF scores were higher BMI, ASA 3 score, and lower HRQoL. Active smoking status was independently associated with lower HRQoL assessed using the EQ-5D-3L. As there was an association between smoking and EQ-5D-3L scores, the effects of smoking were less apparent when including EQ-5D-3L in the regression analyses.
Table 4.
Multivariable regression analyses
4. Discussion
To our knowledge, this is the largest study to report on long-term outcomes (>2 years) after operative repair of pilon fractures[7,9,11–14,27,28]
Similar to our findings, Cutillas-Ybarra reported significantly lower HRQoL, measured using the Short Form [29] Health Survey (SF-36), in their population of patients with tibial plafond fractures when compared to a reference population.[13] Other studies investigating long-term health status and functionality after treatment of pilon fractures showed comparable results, indicating that pilon fractures can have significant effects on a patient's life posttreatment.[7,11,12,14] HRQoL measured in our study population was in fact similar or even worse when compared to values described for patients suffering from a variety of chronic conditions such as malignant breast neoplasms or asthma.[30]
One previous study has shown a correlation between general health function and region-specific patient-reported outcomes.[31] Our results highlight the importance of obtaining both general and region specific measures when evaluating outcomes after injury. This is especially important when evaluating injuries that typically occur in the context of multiple trauma, like pilon fractures, where outcomes are likely to be affected by concomitant injuries and the severity of the initial trauma.[32,33] Adjusting with general health measures allows the region-specific injury of interest to be assessed in the right context.
In our study, the only factor associated with worse long-term results for all outcome measures was active smoking status at the time of definitive fixation of the pilon fracture. Due to the retrospective nature of the study, it was not possible to ascertain if patients were still smoking at the time of follow-up by questionnaire. In addition, the retrospective design also limits the ability to show true causal effects of smoking on outcomes. Furthermore, nonresponders were significantly more often smoking at the time of injury and therefore, the effects measured may even be an underestimation of the impact of tobacco use. Smoking is known to affect HRQoL and function, and hence, the lower outcome scores in our cohort may be only partially attributed to smoking, perhaps even regardless of the pilon fractures. In addition, low income and low level of education (both beyond the scope of our study) have been reported to be associated with HRQoL after pilon fractures negatively and these factors have also been associated with higher rates of daily smoking.[7,34,35]
Perioperative smoking is associated with an increased risk of postoperative complications as well.[36] Therefore, it is assumed that confounding plays an important role in assessing relationships between smoking and outcomes of pilon fractures, perhaps providing an opportunity for future research.
Unfortunately, pilon fractures demand acute treatment, leaving almost no room for smoking cessation. However, even though no definite conclusions on the relationship between smoking and outcomes of operatively treated pilon fractures can be drawn, we believe that the available evidence should be used to counsel active smokers scheduled to undergo operative repair of pilon fractures and to offer these patients smoking cessation interventions.
This study has several limitations. First, the study had a retrospective design. Due to the retrospective nature of this study, it was not possible to account for all variables that carry potential to influence the outcome measures. Amongst others, low income, education level, and insurance status may influence outcomes of (pilon) fractures but was impossible to evaluate for our cohort from the available data and surveys.[29,37] Furthermore, it is possible that operative factors such as the quality of reduction affect outcomes. Unfortunately, this was beyond the scope of our study and long-term postoperative imaging was not available for a sufficient amount of the included patients (as this study was conducted at 2 tertiary referral centers with many patients not receiving routine follow-up at these institutions). Factors associated with our outcome measures, as identified in this study, should therefore not be seen as the only factors influencing HRQoL and functionality after operative treatment of a pilon fracture and may have been confounded by factors. Second, the response rate was relatively low. We believe this to be due to the relatively long interval between surgery and follow-up and the potentially more transient nature of a trauma patient population. Given the complexity of surgery for these injuries, many patients are also transferred in from community hospitals for their surgery and so these patients may have followed up at outside institutions. In addition, there were differences in baseline characteristics between responders and nonresponders. Previous studies also showed important differences between trauma patients responding to surveys and trauma patients not responding to surveys. An important difference is that more severely injured patients are more often responders, possibly causing worse patient-reported outcomes to be reported.[38,39] Third, as the survey was relatively long, questionnaire fatigue may have occurred and influenced the outcomes reported. Fourth, as included patients were treated over a long period of time, changes in treatment techniques and surgeon experience will have taken place. These changes may have affected the outcomes measured. Therefore, the results of the present study are not completely generalizable to all patients who suffer pilon fractures. Nonetheless, to our best knowledge, we still present the largest retrospective series on long-term outcomes after pilon fractures to date and believe our data can be used as generalizable outcome data to counsel a selected group of patients.
Pilon fractures can have significant effects on a patient's life and should therefore be seen as potentially disabling injuries. Long-term ankle functioning was found to be around 75% of full function, with nearly half of all patients experiencing problems in walking about. Impaired long-term outcomes may be expected in patients who report poor HRQoL, are smokers, have a high body mass index, or developed a deep surgical site infection. Regardless of associated factors, patients with a history of a pilon fracture do not enjoy the same health-related quality of life as individuals in the general population. It is important to counsel patients about the severity of their injury and potential long-term outcomes in order to set realistic expectations. This study emphasizes the importance of obtaining both general and region-specific measures when evaluating outcomes after injury, in order to evaluate the injury of interest in the accurate context.
Supplementary Material
References
- 1.Egol KA, Wolinsky P, Koval KJ. Open reduction and internal fixation of tibial pilon fractures. Foot Ankle Clin. 2000;5:873–885. [PubMed] [Google Scholar]
- 2.Scolaro J, Ahn J. In brief: Pilon Fractures. Clin Orthop Relat Res. 2011;469:621–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mauffrey C, Vasario G, Battiston B, et al. Tibial pilon fractures: a review of incidence, diagnosis, treatment,and complications. Acta Orthop Belg. 2011;77:432–440. [PubMed] [Google Scholar]
- 4.Bonar S, Marsh J. Tibial plafond fractures: changing principles of treatment. J Am Acad Orthop Surg. 1994;2:297–305. [DOI] [PubMed] [Google Scholar]
- 5. Marsh JL S. Axial-loading injuries: tibial plafond fractures. In: Charles A. Rockwood, Robert W. Bucholz, Charles M. Court-Brown, James D. Heckman PT, editor. Rockwood and Green's fractures in Adults. 2006: 2203–2234. [Google Scholar]
- 6.Tarkin IS, Clare MP, Marcantonio A, et al. An update on the management of high-energy pilon fractures. Injury. 2008;39:142–154. [DOI] [PubMed] [Google Scholar]
- 7.Pollak AN, McCarthy ML, Bess RS, et al. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Jt Surg Am. 2003;85:1893–1900. [DOI] [PubMed] [Google Scholar]
- 8.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21 (10 suppl):S1–S133. [DOI] [PubMed] [Google Scholar]
- 9.Korkmaz A, Çiftdemir M, Özcan M, et al. The analysis of the variables, affecting outcome in surgically treated tibia pilon fractured patients. Injury. 2013;44:1270–1274. [DOI] [PubMed] [Google Scholar]
- 10.Chen SH, Wu PHLY. Long-term results of pilon fractures. Arch Orthop Trauma Surg. 2007;127:55–60. [DOI] [PubMed] [Google Scholar]
- 11.Biz C, Angelini A, Zamperetti M, et al. Medium-long-term radiographic and clinical outcomes after surgical treatment of intra-articular tibial pilon fractures by three different techniques. Biomed Res Int. 2018;2018: 6054021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cisneros L, Gomez M, Alvarez C, et al. Comparison of outcome of tibial plafond fractures managed by hybrid external fixation versus two-stage management with final plate fixation. Indian J Orthop. 2016;50:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cutillas-Ybarra MB, Lizaur-Utrilla A, Lopez-Prats FA. Prognostic factors of health-related quality of life in patients after tibial plafond fracture. A pilot study. Injury. 2015;46:2253–2257. [DOI] [PubMed] [Google Scholar]
- 14.Jansen H, Fenwick A, Doht S, et al. Clinical outcome and changes in gait pattern after pilon fractures. Int Orthop. 2013;37:51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kellam JF, Meinberg EG, Agel J, et al. Introduction: Facture and Dislocation Classification Compendium-2018: International Comprehensive Classification of Fractures an Dislocations Committee. J Orthop Trauma. 2018;32:S1–S10. [DOI] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The ATLS Subcommittee and the International ATLS working group AC of SC on T Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013;74:1363–1366. [DOI] [PubMed] [Google Scholar]
- 18.Linder F, Mani K, Juhlin C, et al. Routine whole body CT of high energy trauma patients leads to excessive radiation exposure. Scand J Trauma Resusc Emerg Med. 2016;24:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gitajn IL, Heng M, Weaver MJ, et al. Culture-negative infection after operative fixation of fractures. J Orthop Trauma. 2016;30:538–544. [DOI] [PubMed] [Google Scholar]
- 20.Martin RRL, Irrgang JJ, Burdett RG, et al. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26:968–983. [DOI] [PubMed] [Google Scholar]
- 21.Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63:1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabin R, De Charro F. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. [DOI] [PubMed] [Google Scholar]
- 24.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43:203–220. [DOI] [PubMed] [Google Scholar]
- 25.Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related indexes from the national health measurement study. Med Care. 2007;45:1162–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shankaran V, Jolly S, Blough D, et al. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol. 2012;30:1608–1614. [DOI] [PubMed] [Google Scholar]
- 27.Hill CE. Does external fixation result in superior ankle function than open reduction internal fixation in the management of adult distal tibial plafond fractures? Foot Ankle Surg. 2016;22:146–151. [DOI] [PubMed] [Google Scholar]
- 28.Davidovitch RI, Elkataran R, Romo S, et al. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA Type 43C). Foot Ankle Int. 2011;32:955–961. [DOI] [PubMed] [Google Scholar]
- 29.Paksima N, Pahk B, Romo S, et al. The association of education level on outcome after distal radius fracture. Hand. 2014;9:75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Mak. 2006;26:410–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Turchin DC, Schemitsch EH, McKee MD, et al. Do foot injuries significantly affect the functional outcome of multiply injured patients? J Orthop Trauma. 1999;13:1–4. [DOI] [PubMed] [Google Scholar]
- 32.van der Vliet QMJ, Hietbrink F, Casari F, et al. Factors influencing functional outcomes of subtalar fusion for posttraumatic arthritis after calcaneal fracture. Foot Ankle Int. 2018;39: 1062–1069. [DOI] [PubMed] [Google Scholar]
- 33.Gallay S, Hupel T, Beaton D, et al. Functional outcome of acromioclavicular joint injury in polytrauma patients. J Orthop Trauma. 1998;12:159–163. [DOI] [PubMed] [Google Scholar]
- 34.Huisman M, Van Lenthe FJ, Giskes K, et al. Explaining socio-economic inequalities in daily smoking: a social-ecological approach. Eur J Public Health. 2012;22:238–243. [DOI] [PubMed] [Google Scholar]
- 35.Goldenberg M, Danovitch I, IsHak WW. Quality of life and smoking. Am J Addict. 2014;23:540–562. [DOI] [PubMed] [Google Scholar]
- 36.Gronkjaer MM, Eliasen LS, Skov-Ettrup JS, et al. Preoperative smoking status and postoperative complications: a systematic review and meta-analysis. Ann Surg. 2014;259:52–71. [DOI] [PubMed] [Google Scholar]
- 37.Shields E, Sundem L, Childs S, et al. Factors predicting patient-reported functional outcome scores after humeral shaft fractures. Injury. 2015;46:693–698. [DOI] [PubMed] [Google Scholar]
- 38.Rios-Diaz AJ, Herrera-Escobar JP, Lilley EJ, et al. Routine inclusion of long-term functional and patient reported outcomes (PROs) into trauma registries. J Trauma. 2016;61:1393–1399. [DOI] [PubMed] [Google Scholar]
- 39.Gabbe BJ, Cameron PA, Hannaford AP, et al. Routine follow up of major trauma patients from trauma registries: what are the outcomes? J Trauma Inj Infect Crit Care. 2006;61:1393–1399. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


