Abstract
Background
Several actions in the realm of public policies and programs have been implemented worldwide to prevent and control the spread of COVID-19. As Brazil and many parts of the world are marked by regional, cultural, and social inequalities, risk communication and assimilation of protection recommendations by the public may be erratic, hampering the proper measurement of their effectiveness.
Scope and approach
Even though transmission of SARS-CoV-2 by foods is unlikely, this work aimed to evaluate the population's adherence to the recommended food hygiene and personal protection measures to prevent COVID-19. An online survey containing questions on food hygiene and personal protection was publicly disseminated via internet and social networks. Data from 3000 respondents were collected and discussed herein.
Key findings and conclusions: Most respondents adopted the recommended hygienic and personal protection measures to avoid contamination with SARS-CoV-2. However, some important flaws were detected, such as lack of use of face masks when in public places (6%), improper hand washing and sanitizing (10–12%) and use of incorrect products for food or environment cleaning and sanitization (28%), indicating that adequate risk communication and preventive recommendations must continue in order to avoid contamination with the coronavirus. The heighten awareness with food hygiene during the pandemic may have an enduring positive effect on food safety.
Keywords: SARS-CoV-2, Food safety, Personal protection, Sanitizers, Food handing
1. Introduction
In December 2019, an outbreak of a new respiratory disease called COVID-19 (Coronavirus Disease 2019) was reported in China. The disease, caused by a new coronavirus called SARS-CoV-2 (Severe Acute Respiratory Syndrome – Coronavirus-2), quickly became pandemic, reaching Latin America on February 25, 2020, when the first case was reported in the city of Sao Paulo, Brazil (De Souza et al., 2020; Rodriguez-Morales et al., 2020).
To prevent the spread of COVID-19, the World Health Organization (WHO) and the Brazilian Ministry of Health, through the National Health Surveillance Agency (ANVISA) were quick in publishing advices for the public, using various means of communication (Brasil, 2020; FAO & WHO, 2020). The recommendations were related to personal hygiene and changes in social behavior, in addition to the use of personal protective equipment, rigorous cleaning and disinfection of surfaces and foods to be eaten raw, among others. Early containment was established as crucial to stop the dissemination of the pandemic and to prevent the collapse of the local health systems.
However, the adherence to these recommendations is challenging, as they demand significant changes in people's routine behavior (Casero-Ripollés, 2020; Masip et al., 2020; Moreno, Fuentes-Lara, & Navarro, 2020). Additionally, the fear of contracting COVID-19 may cause overreaction, with people going beyond sound recommendations, originating new health risks. Moreover, as pointed out by Franco, Landgraf, and Pinto (2020), the dissemination of low-quality information has placed foods as possible disseminators of the disease, raising concerns in the food production chain, consumers, and governments. Thus, a proper risk communication strategy is essential.
As Brazil is marked by social inequalities, it is crucial to assess the degree of assimilation to the health authorities’ recommendations in order to subsidize effective strategies to control the spread of the pandemic. This study assessed the reach, understanding and adherence of the Brazilian population to the food hygiene and individual protection measures necessary for the prevention and containment of COVID-19, by means of a questionnaire disseminated via the internet and social networks.
2. Survey design and approach
A cross-sectional study was carried out by the application of a questionnaire prepared on the Google®Forms platform, publicly disseminated via the internet and social networks, comprising 31 questions related to the prevention and control of COVID-19. Data collection took place between June 25th and July 14th, 2020, with anonymous voluntary participation. Adults above 18 years old residing in Brazil answered the questionnaire. The research was approved by the Research Ethics Committee of the Faculty of Pharmaceutical Sciences, University of Sao Paulo (CAAE 31781720.9.0000.0067).
The questions were distributed in three categories: 1. Sociodemographic profile (sex, age, marital status, education, and family income); 2. Hygiene practices (personal, environment and food); and 3. Issues related to the social environment of the respondent. Part 2 of the questionnaire comprised questions in nine topics: use of masks, avoidance of crowded places, use of alcohol-based hand sanitizers, frequency of hand washing, social distancing, avoidance of touching the face, avoidance of public places, proper food handling and cleaning of surfaces. Part 3 had questions related to the way the population got informed about the pandemic.
Data were collected from Brazilians, configuring a non-probabilistic sample with convenience bias (Bezerra, Silva, Soares, & Silva, 2020). The data were tabulated in Excel spreadsheets and the absolute and relative frequencies of all study variables were calculated. When appropriate, specific groups, such as marital status, age, or education, where evaluated separately in order to get insights related to specific behaviors.
3. Findings and implications
3.1. Sociodemographic analysis
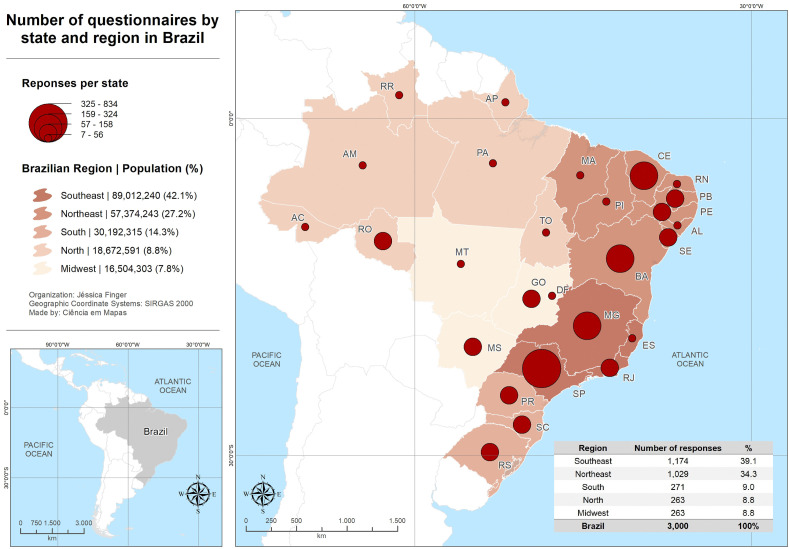
A total of 3000 individuals responded the questionnaire, covering all Brazilian territory (Fig. 1 ). Brazilian states are grouped into five regions (Southeast, Northwest, South, North and Midwest), and the number of respondents per region was proportional to the population in each region (IBGE, 2019).
Fig. 1.
Number of questionnaires answered by Brazilian state and region.
The survey did not intend to target a specific social segment, but responses of people with graduate (47.6%) and undergraduate degrees (26.2%) prevailed (Table 1 ). Reported professions, monthly incomes and education status were compatible with the Brazilian middle-class. In fact, the educational level of the Brazilian population as of 2019 is as follows: 14% hold an undergraduate degree; 30% have completed the high-school and the remaining 66% of the population have lower education levels than a high-school degree, including 6.9% which do not have any formal education (IBGE, 2019). Hence the survey failed to reach the most vulnerable segments of the population, which have limited, if any, access to the internet. Notably, the most vulnerable population is more prone to contamination with COVID-19 and other infectious diseases, including those of food origin, due to difficulties to adhere to public preventive measures because of living in unsanitary conditions with lack of sewage treatment and potable water distribution, overcrowded homes, food insecurity, and possibly low-quality information (Coelho et al., 2020; IBGE, 2019; Natividade et al., 2020; Pereira, do Nascimento, Gratão, & Pimenta, 2020).
Table 1.
Sociodemographic characteristics of the respondents.
| Category | Group | Number of answers | % |
|---|---|---|---|
| Sex | Female | 2166 | 72.2 |
| Male | 831 | 27.7 | |
| Not answered | 3 | 0.1 | |
| Age | 26–40 years | 1263 | 42.1 |
| 41–55 years | 795 | 26.5 | |
| 18–25 years | 456 | 15.2 | |
| 56–70 years | 424 | 14.1 | |
| Over 70 years | 62 | 2.1 | |
| Marital status | Married | 1385 | 46.2 |
| Single | 1092 | 36.4 | |
| Living together | 266 | 8.9 | |
| Divorced | 202 | 6.7 | |
| Widow/widower | 47 | 1.6 | |
| Not answered | 8 | 0.3 | |
| Education | Graduate degree | 1428 | 47.6 |
| Undergraduate degree | 785 | 26.2 | |
| Incomplete undergraduate degree | 410 | 13.7 | |
| Complete high school degree | 294 | 9.8 | |
| Incomplete high school degree | 28 | 0.9 | |
| Complete primary education | 27 | 0.9 | |
| Not answered | 15 | 0.5 | |
| Incomplete primary education | 12 | 0.4 | |
| No schooling | 1 | 0.03 | |
| Profession | Public server | 667 | 22.2 |
| Student or researcher | 461 | 15.4 | |
| Private practice (lawyers, architects, journalists, businessmen, among others) | 345 | 11.5 | |
| Teacher | 332 | 11.1 | |
| Retired/Pensioner | 261 | 8.7 | |
| Health professionals | 245 | 8.2 | |
| Retail | 176 | 5.9 | |
| Unemployed | 115 | 3.8 | |
| Other professions | 309 | 10.3 | |
| Monthly family income | 05 to 15 minimum wages | 1053 | 35.1 |
| 03 to 05 minimum wages | 656 | 21.9 | |
| More than 15 minimum wages | 504 | 16.8 | |
| 01 to 03 minimum wages | 477 | 15.9 | |
| Not answered | 210 | 7.0 | |
| Less than one minimum wage | 100 | 3.3 | |
| Number of residents in the same home | 2 or 3 persons | 1724 | 57.5 |
| 4 or 5 persons | 892 | 29.7 | |
| Living alone | 274 | 9.1 | |
| 6 or 7 persons | 96 | 3.2 | |
| More than 8 persons | 14 | 0.5 |
3.2. Awareness of COVID-19 preventive measures
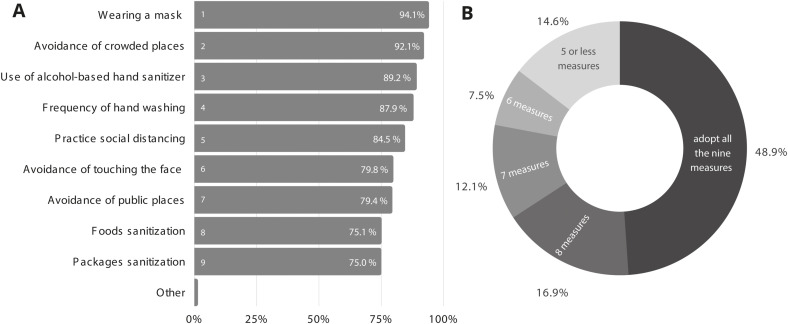
Despite being aware of the recommended COVID-19 prevention and control measures, only 48.5% of the respondents followed all of them correctly (Fig. 2 ). Wearing a mask in public spaces was the most adopted preventive measure (94.1%) followed by avoidance of crowded places (92.1%), use of alcohol-based hand sanitizers (89.2%) and social distancing (84.5%). Frequent hand washing, avoidance of touching the face, avoidance of public places, proper food handling and cleaning of surfaces were also common practices (Fig. 2). Proper food handling, cleaning of surfaces and hand washing are important measures to reduce the burden of foodborne diseases (Finger, Baroni, Maffei, Bastos, & Pinto, 2019). In fact, Djekic et al. (2021) reported that COVID-19 has influenced food safety by improving staff awareness to hygiene practices in the food sector.
Fig. 2.
Adherence to the hygiene measures by type of recommendation (A) and accumulatively (B).
The high adherence to face mask use in public places is noteworthy, as this measure is the most effective in reducing the spread of SARS-CoV-2, especially in places with limited ventilation, which has been confirmed by epidemiological data (Prather, Wang, & Schooley, 2020; Sethuraman, Jeremiah, & Ryo, 2020; Treibel et al., 2020; Zuber & Brüssow, 2020).
The perception of the importance of avoiding crowded places and practicing social distancing to prevent the spread of COVID-19 is variable in Brazil (Henriques & Vasconcelos, 2020; Natividade et al., 2020). Conversely, 84.5% of the respondents of this work reported to practice social distancing, which may be related to the specific population segment that responded the survey. A Brazilian study conducted in April 2020, on factors associated with people's behavior during the pandemic, indicated that most surveyed people are willing to remain in social isolation to stop the spread of COVID-19 (Bezerra et al., 2020). However, favorable living conditions play a major role in the capacity of the population to be able to adhere to social isolation and adopt proper hygiene measures, as shown by Natividade et al. (2020). Social distancing is an effective strategy to delay the spread of the disease and to reduce the number of infected people (Davies, Kucharski, Eggo, Gimma, & Edmunds, 2020; Zuber & Brüssow, 2020).
3.3. Personal hygiene measures
Proper hand washing is a highly recommended measure by health authorities for preventing COVID-19 and other infectious diseases (Huang, Ma, & Stack, 2012; Olaimat, Shahbaz, Fatima, Munir, & Holley, 2020; WHO, 2009). Adherence to personal hygiene recommendations was reported by most respondents, especially when arriving at home. Aside from hand washing, other measures such as removing the shoes, changing clothes, and taking a shower may be less relevant for the spread of SARS-CoV-2 but indicate an increased awareness to practicing hygiene. Conversely, lack of adherence to one of the most relevant personal hygiene recommendations (handwashing when arriving at home) by almost 11% of the respondents is worrisome.
A Brazilian study performed in the beginning of the pandemic, aiming at describing trends in web search queries related to the disease, indicated a greater interest in the use of face masks, social distancing, and hand hygiene with alcohol-based sanitizer than in respiratory etiquette or hand hygiene with soap and water (Garcia Filho, Vieira, & Silva, 2020). It is important to note that hand hygiene should be considered as a complementary measure against COVID-19, as emphasis on hand hygiene can lead individuals to make other measures, such as social distancing and mask use, more flexible, under the illusion that hand hygiene alone can protect them from contracting or transmitting SARS-CoV-2 (Yang, 2020).
3.4. Food and food surface hygiene at home
Common food hygiene and disinfecting procedures are effective at reducing spoilage organisms, eliminating foodborne pathogens and are also effective against SARS-CoV2 (Franco et al., 2020). This survey revealed that nearly 50% of the participants wash their fruits and vegetables as recommended by the Brazilian Health Authority, i.e., rinsing with running water, dipping in water with chlorine solution and then rinsing again with running water to remove chlorine residues (Brasil, 2014). However, 27.4% indicated that they wash fruits with detergent, which may be harmful due to residues left on the product, and 7% use culinary vinegar as sanitizer, which is not as effective as chlorine (Chang et al., 2020; Gil, Selma, López-Gálvez, & Allende, 2009; Pezzuto et al., 2016).
As with other viruses, SARS-CoV-2 needs to enter specific host cells through specialized biochemical processes to generate new viral particles (Dhama et al., 2020). These specific host cells are not likely to be found in foods which help explain the lack of cases involved in SARS-CoV-2 foodborne transmission. In previous outbreaks caused by SARS-CoV and MERS-CoV, foodborne cases were not reported (Lacombe, Quintela, Liao, & Wu, 2020; Olaimat et al., 2020; Rizou, Galanakis, Aldawoud, & Galanakis, 2020). However, the transfer of coronavirus by handlers to the food surfaces is conceivable, given the extension of the food chain (Duda-Chodak, Lukasiewicz, Zięć, Florkiewicz, & Filipiak-Florkiewicz, 2020; Olaimat et al., 2020).
Despite the lack of enough evidence that foods can transmit SARS-CoV-2, proper food hygiene practices are crucial for preventing foodborne diseases caused by a variety of pathogens (Finger et al., 2019; Franco et al., 2020). International experts on food safety agree that it is highly unlikely that food consumption or touching food packages will result in the spread of SARS-CoV-2 (ICMSF, 2020; FDA, 2021). Besides, it is unknown whether the virus resists passage through the gastrointestinal tract and the fecal-oral transmission still needs to be investigated (Bogler et al., 2020; Franco et al., 2020). Moreover, during an ongoing and devastating pandemic, food and personal hygiene measures should continue to be reinforced to reduce the risk of viral transmission. A Chinese study speculated that imported frozen salmon could be the source of SARS-CoV-2 reintroduction on a Beijing city market, initiating an outbreak that led to hundreds being infected (Pang et al., 2020). However, the study did not provide direct evidence of foodborne viral transmission since it did not show the presence of infective viral particles on the product. It is worth mentioning that measures for cold chain imported foods implemented by Chinese authorities in September of 2020 (WTO document G/SPS/N/CHN/1173) have been a matter of dispute in the World Trade Organization as not being science based (document WTO G/SPS/GEN/1863). Epidemiological studies are crucial for determining whether foods and packages can be considered as vehicles of transmission and potential sources of viral reintroduction in places where it has been contained. Moreover, it is important to consider that people may be infected not by a food source or some contaminated surface, but rather by international workers that come into close contact with local personnel (Xing, Wong, Ni, Hu, & Xing, 2020). Additional studies are necessary and quantitative risk assessments related to foodborne transmission of COVID-19 are of utmost need.
For safety purposes, plant-based foods to be eaten raw should be cleaned with running water and sanitized with sodium hypochlorite, and others must be properly cooked and kept at safe temperature (ASBRAN, 2020; Coelho-Ravagnani et al., 2020; FAO, 2020; Olaimat et al., 2020; Rizou et al., 2020). The increased awareness related to food hygiene during the pandemic should be emphasized for the post-pandemic era, making safety measures a habit not only for essential works in the food sector, but also for the whole population. The pandemic has reinforced the need for rigorous food hygiene measures adopted from farm-to-fork, based on good agricultural and manufacturing practices and HACCP principles, which are able to control foodborne viruses, bacteria, and SARS-CoV-2 (Olaimat et al., 2020; Rizou et al., 2020; Shahidi, 2020).
Most of the survey respondents (55.7%) reported using alcohol-based sanitizers for cleaning non-rigid packages, while 38.4% reported to clean cans, glass containers and plastic recipients too. This is probably due to the quick dissemination of data showing that SARS-CoV-2 can persist on surfaces from hours to days depending on the surface material and porosity, temperature, humidity, and inoculum size (Kampf, Todt, Pfaender, & Steinmann, 2020; Kratzel et al., 2020; Van Doremalen et al., 2020). At the beginning of the pandemic, some organizations have suggested, as an extra precaution, to wash food packages with soap and water or to spray 70% alcohol or a chlorinated solution before usage or storage (ASBRAN, 2020; FDA, 2020). It has become commonly accepted that foods, packages, and food contact surfaces play an insignificant role in transmitting SARS-CoV-2 and proper hand washing with potable running water and soap after handling packages and raw foods are sufficient to eliminate the virus and other common foodborne pathogens from the hands (FAO & WHO, 2020; Franco et al., 2020; Rizou et al., 2020).
When asked about what measures were taken upon receiving food at home, most participants indicated that they wash their hands before and after receiving the products (65.5%), besides keeping a distance from the delivery worker (61.3%) and cleaning the packaging before opening (57.2%). Conversely, 16.9% reported not buying ready-to-eat meals during the pandemic and 2.7% stated not taking any preventive measures. These findings can provide important data for a quantitative risk assessment of SARS-CoV-2 transmission to and from delivery workers and consumers, which can be used to inform the public on the necessary measures to be taken. However, Lacombe et al. (2020) has noted the difficulties in calculating the risk of a person contracting COVID-19 from foods or surfaces because many variables needed to build a model are unknown. Adding to this problem is the fact that the virus infectious dose is currently unknown and likely varies depending on several conditions.
The percentage of respondents failing to adopt all preventive measures during delivery is somewhat concerning, since the questionnaire was applied at the peak of the first wave of the pandemic in Brazil and the population should have behaved with greater caution. Take-away food, drive-thru and food delivery are considered good risk managing strategies as they avoid breaking the stay-at-home recommendations, especially for high-risk populations, such as the elderly (Rizou et al., 2020). Even being the person-to-person contact the most important route of transmission of SARS-CoV-2 due to the inhalation of droplets (with diameter > 5 μm) and aerosols (diameter < 5 μm) expelled in the environment through the mouth and nose of infected individuals (Chu et al., 2020; Prather et al., 2020; Zhang, Li, Zhang, Wang, & Molina, 2020), washing hands before and after receiving foods at home, wearing a face mask, and keeping a safe distance from the delivery worker are additional relevant protection measures during COVID-19 pandemic.
3.5. Hygiene measures at home
To reduce the amount of virus particles on surfaces and the risk of transmission of COVID-19, the US-Center for Disease Control and Prevention recommends cleaning and disinfecting public spaces and homes routinely, using soap and water or disinfectant (CDC, 2020). Some products, such as sodium hypochlorite, ethanol, peracetic acid, quaternary ammonium, hydrogen peroxide, among others, are recognized as effective against SARS-CoV-2 by the United States Environmental Protection Agency and must be used in adequate time and concentration (CDC, 2020; EPA, 2020). Effective inactivation of SARS-CoV-2 can be achieved using common disinfectants, such as 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite, with a minimum contact time of 1 min (Kampf et al., 2020; Kratzel et al., 2020). Additionally, some biocides found in personal hygiene products and general cleaning formulations, such as chlorhexidine, chloroxylenol and benzalkonium chloride were effective at reducing SARS-CoV-2 during 5 minutes at 22 °C (Chin et al., 2020).
When asked about procedures such as cleaning of surfaces, including tables, benches and floors of the home, alcohol-based sanitizers (78.5%) were the preferred products, followed by multipurpose disinfectants (47.6%), detergents (38.4%), chlorine (35.8%) and water (28.4%). For floor cleaning, the main products mentioned were multipurpose disinfectants (70.3%) and chlorine solution, with 66.0%. A significant portion of the participants (86.3%) indicated that bleach was an effective replacement to alcohol-based products. Alcohol-based disinfectants, detergents and chlorine-based products for environmental hygiene are commonly used in Brazil (Behrens et al., 2010). Such procedures are in accordance with the guidelines of the Brazilian National Health Surveillance Agency (Brasil, 2020).
Some studies have shown that exposure to cleaning products and disinfectants increased substantially during the pandemic (Chang et al., 2020), raising new risks for the population. To reduce misuse and avoid unnecessary chemical exposures, health authorities recommend a list of precautions, such as careful reading of labels, strict following instructions and avoiding mixing different products. Eye and skin protection, adequate ventilation, storage out of reach of children and distance from foods are additional recommendations (Brasil, 2020).
4. Risk communication in the COVID-19 pandemic
Care with food hygiene is always important, and the pandemic has brought this issue to the public's attention, even though transmission is mostly airborne. With more people concerned with food safety, it is now possible to better communicate risks associated with food contamination with pathogenic microorganisms. Universities and governments should better use communication tools taking advantage of the interest on SARS-CoV-2 transmission routes and the lessons learnt during the pandemic to better convey messages related to microbial food safety.
The present study provided evidence on which communication channels were used to get information about COVID-19 in Brazil, and television (55.7%), governmental websites (55.0%), news websites (52.1%), social media (32.6%) and messaging apps (24.2%) were the most indicated sources.
According to the Brazilian Institute of Geography and Statistics, 96.4% of the Brazilian households have a television set and 79.1% use internet at home (IBGE, 2019). These numbers evidence the importance of traditional mass media channels, such as television and internet, for instructional messages and communication on risks to a maximum number of people during crises (Frisby, Veil, & Sellnow, 2014; Moreno et al., 2020).
The search for information on social media suggests that health professionals and researchers need to carefully incorporate these platforms in crisis communication, as pointed out by previous researches (Casero-Ripollés, 2020; Masip et al., 2020; Moreno et al., 2020). Search engines also play a considerable role in disseminating information as suggested by the increased use of the terms “use of masks”, “hand washing” and “social distancing” at the beginning of the pandemic in Brazil (Garcia Filho et al., 2020). Thus, COVID-19 prevention and control messages released by the media should continue to emphasize science-based practices.
5. Conclusions and remarks
Even knowing that the most important route of transmission of the SARS-CoV-2 is the person-to-person contact, the recommended measures for personal and food hygiene remain important in preventing diseases. Proper risk communication and preventive recommendations are particularly relevant because the viral load necessary to cause an infection remains unknown and the availability of vaccines or effective therapeutics against COVID-19 will still take time to have an enduring impact. While protecting against the spread of COVID-19, these measures also ensure protection against food-borne diseases caused by pathogenic microorganisms.
CRediT authorship contribution statement
Jéssica A.F.F. Finger: Conceptualization, Methodology, Formal analysis, Investigation, Data Curation, Writing – Original Draft, Visualization. Emília M. F. Lima: Conceptualization, Methodology, Formal analysis, Investigation, Data Curation, Writing – Original Draft, Visualization. Kristy S. Coelho: Writing – Review & Editing. Jorge H. Behrens: Validation, Writing – Review & Editing. Mariza Landgraf: Validation, Writing – Review & Editing. Bernadette D. G. M. Franco: Validation, Resources, Writing – Review & Editing, Funding acquisition. Uelinton M. Pinto: Conceptualization, Validation, Resources, Writing – Review & Editing, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgments
We acknowledge the Sao Paulo Research Foundation (FAPESP-Brazil-grant #2013/07914–8) for the financial support to the Food Research Center. U.M.Pinto acknowledges the National Council for Scientific and Technological Development (CNPq-Brazil-grant #422242/2018–7). J.A.F.F.Finger and E.M.F.Lima acknowledge CNPq-Brazil and Coordination for the Improvement of Higher Education Personnel (CAPES-Brazil) for scholarships.
References
- ASBRAN Guide to healthy eating in times of COVID [in Portuguese] 2020. https://www.asbran.org.br/storage/downloads/files/2020/03/guia-alimentar-covid-19.pdf
- Behrens J.H., Barcellos M.N., Frewer L.J., Nunes T.P., Franco B.D., Destro M.T., et al. Consumer purchase habits and views on food safety: A Brazilian study. Food Control. 2010;21(7):963–969. doi: 10.1016/j.foodcont.2009.07.018. [DOI] [Google Scholar]
- Bezerra A.C.V., Silva C.E.M.D., Soares F.R.G., Silva J.A.M.D. Fatores associados ao comportamento da população durante o isolamento social na pandemia de COVID-19. Ciência & Saúde Coletiva. 2020;25:2411–2421. doi: 10.1590/1413-81232020256.1.10792020. [DOI] [PubMed] [Google Scholar]
- Bogler A., Packman A., Furman A., Gross A., Kushmaro A., Ronen A., et al. Rethinking wastewater risks and monitoring in light of the COVID-19 pandemic. Nature Sustainability. 2020:1–10. doi: 10.1038/s41893-020-00605-2. [DOI] [Google Scholar]
- Brasil Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Guia alimentar para a população brasileira – 2. ed., Brasília: Ministério da Saúde. 2014:156. ISBN 978-85-334-2176-9. [Google Scholar]
- Brasil Agência Nacional de Vigilância Sanitária (ANVISA). NOTA TÉCNICA Nº 47. Recomendações sobre produtos saneantes que possam substituir o álcool 70% e desinfecção de objetos e superfícies, durante a pandemia de COVID-19. 2020. http://portal.anvisa.gov.br/documents/219201/5923491/NT+47-2020+-GHCOS/2a2e1688-76f2-4de4-a4c8-c050d780b9d7
- Casero-Ripolles, A Impact of Covid-19 on the media system. Communicative and democratic consequences of news consumption during the outbreak. El Profesional de la Información. 2020;29(2) doi: 10.3145/epi.2020.mar.23. [DOI] [Google Scholar]
- CDC Guidance for cleaning and disinfecting. Available online. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/pdf/Reopening_America_Guidance.pdf Accessed on 31 July 2020.
- Chang A., Schnall A.H., Law R., Bronstein A.C., Marraffa J.M., Spiller H.A., et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19–national poison data system. United States, January 1, 2020–March 31, 2020. Morbidity and Mortality Weekly Report. 2020;69(16):496. doi: 10.15585/mmwr.mm6916e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., et al. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020;1:e146. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Pan Y., Cheng S.M., Hui K.P., Krishnan P., Liu H., et al. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clinical Chemistry. 2020;66(4):549–555. doi: 10.1093/clinchem/hvaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho-Ravagnani C.F., Corgosinho F.C., Sanches F.L.F.Z., Prado C.M.M., Laviano A., Mota J.F. Dietary recommendations during the COVID-19 pandemic. Nutrition Reviews. 2020 doi: 10.1093/nutrit/nuaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho F.C., Lana R.M., Cruz O.G., Villela D.A., Bastos L.S., Pastore y Piontti A., et al. Assessing the spread of COVID-19 in Brazil: Mobility, morbidity and social vulnerability. PloS One. 2020;15(9) doi: 10.1371/journal.pone.02382144. e0238214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N.G., Kucharski A.J., Eggo R.M., Gimma A., Edmunds W.J. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: A modelling study. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Souza W.M., Buss L.F., Candido D.D.S., Carrera J., Li S., Zarebski A.E., et al. Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. Nature Human Behaviour. 2020;4:856–865. doi: 10.1038/s41562-020-0928-4. [DOI] [PubMed] [Google Scholar]
- Dhama K., Khan S., Tiwari R., Sircar S., Bhat S., Malik Y.S., et al. Coronavirus disease 2019-COVID-19. Clinical Microbiology Reviews. 2020;33(4) doi: 10.1128/CMR.00028-20. e00028–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djekic I., Nikolić A., Uzunović M., Marijke A., Liu A., Han J., et al. Covid-19 pandemic effects on food safety-multi-country survey study. Food Control. 2021;122:107800. doi: 10.1016/j.foodcont.2020.107800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duda-Chodak A., Lukasiewicz M., Zięć G., Florkiewicz A., Filipiak-Florkiewicz A. Covid-19 pandemic and food: Present knowledge, risks, consumers fears and safety. Trends in Food Science & Technology. 2020 doi: 10.1016/j.tifs.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA List N: Desinfectants for use against SARS-CoV-2 (COVID-19) 2020. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2-covid-19
- FAO Maintaining a healthy diet during the COVID-19 pandemic. 2020. http://www.fao.org/3/ca8380en/CA8380EN.pdf Accessed on 18 August 2020.
- FAO, WHO . Interim guidance; Rome: 2020. COVID-19 and food safety: Guidance for food businesses. [DOI] [Google Scholar]
- FDA COVID-19-Information for consumers – shopping for food. 2020. https://www.fda.gov/media/137009/download Accessed on 25 August 2020.
- FDA COVID-19 update: USDA, FDA underscore current epidemiologic and scientific information indicating No transmission of COVID-19 through food or food packaging. 2021. https://bit.ly/38c47Db Accessed on March 4th, 2021.
- Finger J.A.F.F., Baroni W.S., Maffei D.F., Bastos D.H., Pinto U.M. Overview of foodborne disease outbreaks in Brazil from 2000 to 2018. Foods. 2019;10:434. doi: 10.3390/foods8100434. v. 8, n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco B.D.G.M., Landgraf M., Pinto U.M. Alimentos, sars-CoV-2 e covid-19: Contato possível, transmissão improvável. Estudos Avançados. 2020;34(100):189–202. doi: 10.1590/s0103-4014.2020.34100.012. [DOI] [Google Scholar]
- Frisby B.N., Veil S.R., Sellnow T.L. Instructional messages during health-related crises: Essential content for self-protection. Health Communication. 2014;29(4):347–354. doi: 10.1080/10410236.2012.755604. [DOI] [PubMed] [Google Scholar]
- Garcia Filho C., Vieira L.J.E.S., Silva R.M.D. Internet searches for measures to address COVID-19 in Brazil: A description of searches in the first 100 days of 2020. Epidemiologia e Serviços de Saúde. 2020;29 doi: 10.5123/S1679-49742020000300011. e2020191. [DOI] [PubMed] [Google Scholar]
- Gil M.I., Selma M.V., López-Gálvez F., Allende A. Fresh-cut product sanitation and wash water disinfection: Problems and solutions. International Journal of Food Microbiology. 2009;134(1/2):37–45. doi: 10.1016/j.ijfoodmicro.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Henriques C.M.P., Vasconcelos W. Crises dentro da crise: Respostas, incertezas e desencontros no combate à pandemia da covid-19 no brasil. Estudos Avançados. 2020;34(99):25–44. doi: 10.1590/s0103-4014.2020.3499.003. 2020.3499.003". [DOI] [Google Scholar]
- Huang C., Ma W., Stack S. The hygienic efficacy of different hand-drying methods: A review of the evidence. Mayo Clinic Proceedings. 2012;87(8):791–798. doi: 10.1016/j.mayocp.2012.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBGE Diretoria de Pesquisas, Coordenação de Trabalho e Rendimento, Pesquisa Nacional por Amostra de Domicílios Contínua - 2018. 2019. https://www.ibge.gov.br/estatisticas/multidominio/condicoes-de-vida-desigualdade-e-pobreza/17270-pnad-continua.html?=&t=o-que-e Accessed on 14 August 2020.
- ICMSF ICMSF opinion on SARS-CoV-2 and its relationship to food safety. 2020. https://www.icmsf.org/wp-content/uploads/2020/09/ICMSF2020-Letterhead-COVID-19-opinion-final-03-Sept-2020.BF_.pdf Accessed on 25 August 2020.
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratzel A., Todt D., V’kovski P., Steiner S., Gultom M., Thao T.T.N., et al. Inactivation of severe acute respiratory syndrome coronavirus 2 by WHO-recommended hand rub formulations and alcohols. Emerging infectious diseases, 26(7) 2020;1592 doi: 10.3201/eid2607.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacombe A., Quintela I., Liao Y.T., Wu V.C. Food safety lessons learned from the COVID-19 pandemic. Journal of Food Safety. 2020 doi: 10.1111/jfs.12878. e12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masip P., Aran-Ramspott S., Ruiz-Caballero C., Suau J., Almenar E., Puertas-Graell D. Consumo informativo y cobertura mediática durante el confinamiento por el Covid-19: Sobreinformación, sesgo ideológico y sensacionalismo. El Profesional de la Información. 2020;29(3) doi: 10.3145/epi.2020.may.12. [DOI] [Google Scholar]
- Moreno Á., Fuentes-Lara C., Navarro C. Covid-19 communication management in Spain: Exploring the effect of information-seeking behavior and message reception in public's evaluation. El Profesional de la Información. 2020;29(4) doi: 10.3145/epi.2020.jul.02. [DOI] [Google Scholar]
- Natividade M.D.S., Bernardes K., Pereira M., Miranda S.S., Bertoldo J., Teixeira M.D.G., et al. Social distancing and living conditions in the pandemic COVID-19 in Salvador-Bahia, Brazil. Ciência & Saúde Coletiva. 2020;25:3385–3392. doi: 10.1590/1413-81232020259.22142020. [DOI] [PubMed] [Google Scholar]
- Olaimat A.N., Shahbaz H.M., Fatima N., Munir S., Holley R.A. Food safety during and after the era of covid-19 pandemic. Frontiers in Microbiology. 2020;11(1854) doi: 10.3389/fmicb.2020.01854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang X., Ren L., Wu S., Ma W., Yang J., Di L., et al. Cold-chain food contamination as the possible origin of Covid-19 resurgence in Beijing. National Science Review. 2020;7(12):1861–1864. doi: 10.1093/nsr/nwaa264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira R.J., do Nascimento G.N.L., Gratão L.H.A., Pimenta R.S. The risk of COVID19 transmission in favelas and slums in Brazil. Public Health. 2020;183:42–43. doi: 10.1016/j.puhe.2020.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezzuto A., Belluco S., Losasso C., Patuzzi I., Bordin P., Piovesana A., et al. Effectiveness of washing procedures in reducing Salmonella enterica and Listeria monocytogenes on a raw leafy green vegetable (Eruca vesicaria) Frontiers in Microbiology. 2016;7(1663) doi: 10.3389/fmicb.2016.01663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather K.A., Wang C.C., Schooley R.T. Reducing transmission of SARS-CoV-2. Science. 2020 doi: 10.1126/science.abc6197. [DOI] [PubMed] [Google Scholar]
- Rizou M., Galanakis I.M., Aldawoud T.M., Galanakis C.M. Safety of foods, food supply chain and environment within the COVID-19 pandemic. Trends in Food Science & Technology. 2020 doi: 10.1016/j.tifs.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P., Méndez C.A., Zambrano L.I., Franco-Paredes C., et al. COVID-19 in Latin America: The implications of the first confirmed case in Brazil. Travel Medicine and Infectious Disease. 2020;(35):101613. doi: 10.1016/j.tmaid.2020.101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethuraman N., Jeremiah S.S., Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA Health Forum. 2020;323(22):2249–2251. doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- Shahidi F. Does COVID-19 affect food safety and security? Journal of Food Bioactives. 2020;9:1–3. doi: 10.31665/JFB.2020.9212. [DOI] [Google Scholar]
- Treibel T.A., Manisty C., Burton M., McKnight Á., Lambourne J., Augusto J.B., et al. COVID-19: PCR screening of asymptomatic health-care workers at london hospital. The Lancet. 2020;395(10237):1608–1610. doi: 10.1016/S0140-6736(20)31100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2009. WHO guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care.https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf [PubMed] [Google Scholar]
- Xing Y., Wong G.W., Ni W., Hu X., Xing Q. Rapid response to an outbreak in Qingdao, China. New England Journal of Medicine. 2020;383(23):e129. doi: 10.1056/nejmc2032361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C. Does hand hygiene reduce SARS-CoV-2 transmission? Graefes Archive for Clinical and Experimental Ophthalmology. 2020;258:1133–1134. doi: 10.1007/s00417-020-04652-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences. 2020 doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuber S., Brüssow H. Covid 19: Challenges for virologists in the food industry. Microbial Biotechnology. 2020:1–13. doi: 10.1111/1751-7915.13638. [DOI] [PMC free article] [PubMed] [Google Scholar]