Abstract
Tumors escape immune surveillance by inducing various immunosuppressive pathways, including the activation of inhibitory receptors on tumor-infiltrating T cells. While monoclonal antibodies (mAbs) blocking programmed cell death 1 (PD-1), programmed death-ligand 1 (PD-L1), and cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) have been approved for multiple cancer indications, only a subset of patients benefit from immune checkpoint blockade therapies, highlighting the need for additional approaches. Therefore, the identification of new target molecules acting in distinct or complementary pathways in monotherapy or combination therapy with PD-1/PD-L1 blockade is gaining immense interest. T cell immunoreceptor with Ig and immunoreceptor tyrosine-based inhibitory motif (ITIM) domains (TIGIT) has received considerable attention in cancer immunotherapy. Recently, anti-TIGIT mAb (tiragolumab) has demonstrated promising clinical efficacy in non-small cell lung cancer treatment when combined with an anti-PD-L1 drug (Tecentriq), leading to phase III trial initiation. TIGIT is expressed mainly on T and natural killer cells; it functions as an inhibitory checkpoint receptor, thereby limiting adaptive and innate immunity. CD226 competes for binding with the same ligands with TIGIT but delivers a positive stimulatory signal to the immune cells. This review discusses the recent discoveries regarding the roles of TIGIT and CD226 in immune cell function and their potential application in cancer immunotherapy.
Keywords: cancer immunotherapy, immune checkpoint blockade, CD226, TIGIT, PVR
1. Introduction
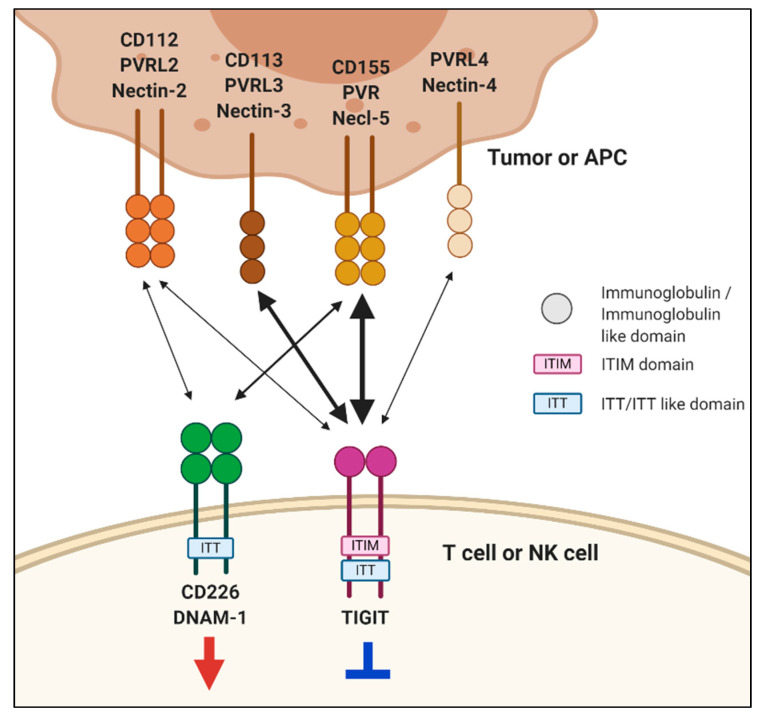
Cancers harbor genetic alterations. The adaptive immune system discriminates between normal and cancer cells according to the protein products of these genetic alterations. T cells express T cell receptors (TCRs) that can recognize antigenic peptides presented by major histocompatibility complex (MHC) molecules [1,2]. Tumor antigens may trigger anti-tumor T cell responses; however, tumor-infiltrating lymphocytes (TILs) fail to efficiently eradicate the cancer cells. This is largely because TILs become dysfunctional or exhausted in the tumor environment, presumably due to persistent tumor antigen stimulation and the presence of immunosuppressive molecules. It is increasingly clear that exhausted T cells (Tex) are the major target population for immune checkpoint blockade (ICB) therapy [3,4]. Tex cells exhibit distinct functional and phenotypic properties, such as impaired proliferation, decreased cytokine production, and high expression of co-inhibitory receptors including cytotoxic T lymphocyte-associated antigen-4 (CTLA-4, CD152), programmed death-1 (PD-1, CD279), T cell immunoglobulin and mucin-domain containing protein-3 (TIM-3, CD366), lymphocyte activation gene-3 (LAG-3, CD223), and T cell immunoreceptor with Ig and immunoreceptor tyrosine-based inhibitory motif (ITIM) domains (TIGIT) [5]. Tumor-derived ligands that interact with the co-inhibitory receptors, such as programmed death-ligand 1 (PD-L1), directly inhibit anti-tumor T cell responses, thereby promoting tumor immune escape [6]. Blockade of the PD-1/PD-L1 pathway using either anti-PD-1 or anti-PD-L1 monoclonal antibodies (mAbs) has only been successful in a subset of patients with particular cancer types [7,8]. Presently, numerous studies have been conducted to improve the therapeutic efficacy of PD-1/PD-L1 blockades [9,10,11,12]. TIGIT family receptors are a cluster of immunoglobulin superfamily receptors, which interact with nectin and nectin-like molecules (Necls) [13]. This group includes TIGIT, CD226 (also known as DNAX accessory molecule [DNAM]-1), CD96 (also known as T cell activation, increased late expression [TACTILE]), and CD112R (also known as poliovirus receptor-related immunoglobulin domain-containing [PVRIG]) [14]. Competitive or cooperative interactions between these receptors and their cognate ligands modulate immune cell activation (Figure 1) [15,16]. Among these, in the present study, we focus on the roles of TIGIT and CD226 in regulating T and natural killer (NK) cell function and the potential therapeutic application of these receptors in cancer immunotherapies.
Figure 1.
Interactions of T cell immunoreceptor with Ig and immunoreceptor tyrosine-based inhibitory motif (ITIM) domains (TIGIT) and CD226 with nectin and nectin-like molecules. TIGIT and CD226 are mainly expressed on T and natural killer (NK) cells. TIGIT has multiple ligands, including poliovirus receptor (PVR), nectin-2, nectin-3, and nectin-4. TIGIT binds to nectin-2 and nectin-3 with lower affinity than PVR. Upon engagement, TIGIT transmits inhibitory signals through ITIM and immunoglobulin tyrosine tail (ITT)-like motifs in its cytoplasmic domain. CD226 interacts with PVR and nectin-2 to deliver a positive signal. TIGIT binds to PVR with higher affinity than CD226. The integrated signals formed by their complex interactions regulate immune-cell functions, which is important for immunity and inflammatory responses. Interactions between receptors and ligands are depicted by two-sided arrows. The arrows are proportional to the reported affinities of the interactions except nectin-4.
2. TIGIT
2.1. TIGIT Structure and Its Ligands
TIGIT is a transmembrane glycoprotein comprising one immunoglobulin variable (IgV) domain, a type I transmembrane domain, and a cytoplasmic tail with an immunoreceptor tyrosine-based inhibitory motif (ITIM) and immunoglobulin tyrosine tail (ITT)-like motif [17,18,19]. The cytoplasmic tail of TIGIT initiates an inhibitory signaling cascade. Previous studies have reported that ITT-like motif (Tyrosine, Y225) mediates a major inhibitory signal in humans, whereas mouse TIGIT inhibitory signal can be triggered by either the ITIM (Y277) or the ITT-like motif residue (Y233) [20]. Upon binding to its ligand, the cytoplasmic tail of TIGIT is phosphorylated and binds to cytosolic adaptor growth factor receptor-bound protein 2 (Grb2), recruiting Src homology 2 (SH2)-containing inositol phosphate-1 (SHIP-1). SHIP-1 inhibits phosphoinositide 3 kinase (PI3K) and mitogen-activated protein kinase (MAPK) signaling cascades [21]. Moreover, phosphorylated TIGIT associates with beta-arrestin 2 and recruits SHIP-1, which further suppresses the auto-ubiquitination of tumor necrosis factor (TNF) receptor-associated factor 6 (TRAF-6) to inhibit nuclear factor kappa B (NF-κB) activation [21,22].
TIGIT has multiple ligands, including PVR (Necl-5 or CD155), nectin-2 (CD112), nectin-3 (CD113), and nectin-4 (PVRL4) [13,23]. Nectin and Necl proteins are cell-surface glycoproteins that belong to the immunoglobulin superfamily. Nectin family comprises four members (nectin-1–4), and the Necl family consists of five members (Necl-1–5). They have three Ig ectodomains, which form homodimeric or heterodimeric complexes in the membrane [24]. The IgV domain of TIGIT exhibits sequence homology with PVR, nectin-1, nectin-2, nectin-3, and nectin-4 [17]. TIGIT binds to PVR with high affinity and nectin-2 and -3 with low affinity. Recently, nectin-4 has been reported to bind to TIGIT with an affinity similar to that of TIGIT and PVR binding [25]. PVR plays immunoregulatory roles by interacting with TIGIT, CD226, and CD96 [26,27,28]. PVR has a greater affinity for TIGIT than either CD226 or CD96, implying a dominant role of TIGIT inhibitory signaling over activation signals. Furthermore, PVR expression is commonly upregulated in several types of cancer and tumor-associated myeloid cells [29,30]. Elevated PVR expression has been associated with an unfavorable prognosis across various solid cancer types [31,32]. Nectin-2 interacts with TIGIT, CD226, and CD112R; however, both TIGIT and CD226 have much weaker binding affinity to nectin-2 than PVR. Similar to PVR, the TIGIT–nectin-2 interaction could transduce an inhibitory signal, but the CD226–nectin-2 interaction triggers immune cell activation. A recent study has demonstrated that the inhibitory effect of nectin-2 is mediated by CD112R and not TIGIT [14].
2.2. Role of TIGIT in Immune Cell Regulation
TIGIT is expressed on most NK and multiple T cell subsets, including memory and activated T cells, regulatory T cells (Treg), and follicular T helper cells (TFH) [17,19,20]. Upon activation with its ligands, TIGIT expression is upregulated in both T and NK cells, where TIGIT inhibits cytotoxic activity. TIGIT-deficient mice do not develop spontaneous autoimmunity; however, they exacerbate experimental autoimmune encephalitis when immunized with myelin oligodendrocyte glycoprotein, indicating a suppressive role of TIGIT [27]. In preclinical mouse tumor models, TIGIT deficiency delays the subcutaneous growth of both B16F10 and MC38 cells and lung metastasis of B16 cells [33,34]. Moreover, TIGIT-deficient mice show increased survival when challenged with VK*MYC myeloma cell lines [35]; however, a recent study revealed that TIGIT-deficient mice did not reject the implanted B16F10 and MC38 more efficiently compared with wild-type (WT) mice [36]. Moreover, in B16F10, RM-1, and E0771 cell lung metastasis models, the beneficial effect of TIGIT deficiency on tumor metastasis was not observed [37,38]. These discrepancies might be results of different experimental setups and/or mouse housing conditions [39]. Further studies with immune cell-type-specific TIGIT-deficient mouse models would be helpful to clarify the suppressive role of TIGIT in vivo [34].
Several mechanisms may explain TIGIT-mediated inhibition of T and NK cell activities. First, as aforementioned, TIGIT delivers an inhibitory signal resulting from ITIM and/or ITT motifs within its cytoplasmic domain. Agonistic anti-TIGIT antibodies inhibit human and mouse T cell proliferation and cytokine production without antigen presenting cells (APC) by suppressing T cell receptor/CD28-activating signaling [27,40]; however, TIGIT engagement increases the expression of receptors for T cell maintenance (e.g., interleukin [IL]-2R, IL-7R, and IL-15R) and anti-apoptotic molecules (e.g., Bcl-xL) [27], implying that TIGIT signaling could mediate the survival of Tex cells. Additionally, TIGIT signaling also inhibits cytotoxicity, degranulation, and cytokine secretion of NK cells [19,41]. Moreover, TIGIT disrupts CD226 co-stimulation. TIGIT has higher affinity for the same set of ligands (PVR and CD112) than CD226. Thus, TIGIT outcompetes CD226 for binding to its ligands [17]. Knockdown of TIGIT in human CD4+T cells induces T-bet-mediated interferon (IFN)-γ production, which can be overcome by blocking CD226-CD155 signaling [40]. Additionally, TIGIT hinders CD226 signaling through the physical prevention of CD226 homodimerization [42]. A recent study by Jin et al. has demonstrated that TIGIT directly affects the intracellular regulation of CD226 activation. By using an antibody specifically recognizing the phosphorylated form of CD226 (phospho-Y322), they have shown that CD226 phosphorylation at Y322 is reduced in TIGIT WT-expressing Jurkat cells upon PVR engagement but not in the cells expressing TIGIT mutant (Y225A/Y231A) [43]. In addition, TIGIT has been known to suppress T cell function in a cell-extrinsic manner. Following TIGIT ligation, PVR signaling leads to increased production of IL-10 and diminished production of IL-12p40 in human dendritic cells (DCs), which further downregulates T cell activation [17]. In accordance with this result, TIGIT ligation inhibits macrophage activation and leads to increased M2 macrophage polarization through PVR [44].
The role of TIGIT has been implicated in modulating Treg cell responses. [45,46]. TIGIT expression is observed in a subset of natural Treg cells in both mice and human. TIGIT+Treg cells express higher levels of Treg signature genes, including Foxp3, CD25, and CTLA-4, compared with TIGIT−Treg cells. TIGIT expression is strongly correlated with the suppressive capacity and the lineage stability of human Treg cells [45,46,47]. Furthermore, TIGIT engagement leads to the induction of IL-10 and fibrinogen-like protein 2, which selectively suppress T helper type 1 (Th1) and Th17 responses [45].
2.3. Targeting TIGIT for Cancer Immunotherapy
2.3.1. TIGIT as a Potential Prognostic Marker for Cancer
Accumulating data from the immune monitoring of cancer patients have revealed that TIGIT expression is elevated in T and NK cells, and it often appears to be associated with advanced disease status and poor clinical outcomes [34,35,48,49,50,51,52,53,54,55,56,57,58]. In follicular lymphoma (FL) patients, TIGIT is highly expressed on intratumoral Treg and late-stage memory CD8+T cells, and increased numbers of TIGIT-expressing tumor infiltrating T cells reveal a correlation with poor survival rate [48]. Multidimensional flow cytometric analysis of intratumoral T cells obtained from FL patients before and after anti-PD-1 therapy has revealed that TIGIT+ Tex cells majorly respond to this therapy. It has been observed that TIGIT+ exhausted T cell populations are downregulated and TIGIT+ effector cells are upregulated by anti-PD-1 therapy [48]. Increase in the proportion of highly suppressive tumor-infiltrating Treg cells following TIGIT expression is associated with poor clinical outcomes in patients with hepatocellular carcinoma (HCC) and metastatic melanoma [47,57]. Moreover, upregulation of TIGIT indicates unfavorable disease status. High-risk patients with myelodysplastic syndrome (MDS) express higher levels of TIGIT and PD-1 in peripheral blood T and NK cells than low-risk patients [58]. High TIGIT expression renders CD4+T, CD8+T, and NK cells hypo-responsive to stimulation in high-risk MDS patients. Several studies have reported that TIGIT upregulation after treatment is correlated with recurrence. In patients with high-grade serous carcinoma, NanoString analysis of tumor tissues has indicated that recurrent tumors acquire a more inflamed phenotype with increased expression of TIGIT, CTLA4, Lag-3, and Tim-3 compared to primary tumors [59]. The proportion of TIGIT+CD8+T cells is increased in peripheral blood collected from acute myeloid leukemia (AML) patients, and it becomes more evident in patients with primary refractory disease and leukemia relapse post-allogeneic stem-cell transplantation [49]. Furthermore, TIGIT and/or PD-1 expression in CD8+T cells is increased in patients with gastric cancer relapse after treatment with SOX (S-1 and oxaliplatin) regimen, whereas no notable increase in the proportion of TIGIT+ and/or PD-1+CD8+T cells was found in relapse-free patients [60]. The compensatory increase in TIGIT expression post-treatment has also been observed in high-grade neuroendocrine neoplasms upon anti-PD-1 therapy [61].
2.3.2. TIGIT Blockade in Anti-Tumor Immunity
Based on the mechanism underlying TIGIT-mediated regulation of anti-tumor immune responses, efforts have been made to enhance T or NK cell activity by blocking TIGIT binding to its ligands, PVR and nectin-2, with monoclonal antibodies (mAbs) for therapeutic interventions. Several preclinical mouse models have been used to assess the anti-tumor efficacy of anti-TIGIT blocking mAbs. In CT26 colon carcinoma, EMT6 breast carcinoma, MC38 colon carcinoma, and GL261 glioblastoma models, treatment with anti-TIGIT-blocking mAbs combined with anti-PD-1 or PD-L1-blocking mAbs leads to nearly complete remission of tumor growth, whereas the treatment of anti-TIGIT mAbs as a single agent presents limited efficacy [42,62,63]. CD8+T cell depletion using anti-CD8α-depleting mAbs in CT26-bearing mice has revealed that the synergistic effect of dual blockade of TIGIT and PD-1 is mainly driven by the promotion of CD8+T cell responses. A triple combination of anti-TIGIT mAbs, anti-PD-L1 mAbs, and radiotherapy elicits almost complete remission of tumor growth in CT26-bearing mice [64].
Sufficient tumor regression by treatment with anti-TIGIT mAbs alone has been reported in different mouse tumor models. In multiple myeloma (MM) mouse tumor model, TIGIT blockade leads to reduced tumor growth and increased survival compared with mice receiving control IgG or anti-PD-1 mAbs [35]. Moreover, TIGIT blockade presents anti-tumor efficacy in Tgfbr1/Pten2 conditional knock-out (KO) mouse model that spontaneously develops head and neck squamous cell carcinoma (HNSCC) upon tamoxifen injection [55,65]. Both studies suggest that TIGIT is highly expressed on CD8+T and Treg cells in MM or HNSCC TILs and that anti-TIGIT mAbs reverse TIGIT-mediated suppression of CD8+T cell effector functions; however, the potent anti-tumor effect of anti-TIGIT mAbs as a single agent may not be fully guaranteed simply by the increased expression of TIGIT in TILs, since high TIGIT expression is also observed in CD8+ TILs in CT26-bearing mice that are not responsive to TIGIT blockade [42]. A recent study by Chiu et al. provided additional insights into the mechanism through which TIGIT blockade mitigates tumor immune evasion and resistance to PD-1 blockade [66]. They found that anti-PD-1 mAb treatment induced the upregulation of TIGIT in CD8+ TILs in Trp53 KO/C-MycOE mice, which is a highly aggressive HCC model; however, the compensatory expression of TIGIT upon PD-1 blockade was not observed in Hepa1-6-bearing mice that are known to be an anti-PD-1-sensitive orthotopic HCC model. PVRL1, which does not directly bind to TIGIT, contributed to TIGIT-mediated suppression of CD8+T cells by stabilizing PVR in HCC cells, and PVRL1 deficiency rendered HCC to be more sensitive to anti-PD-1 mAb treatment. In accordance with this finding, a differential level of the ligand expression, such as PVR and PD-L1, or an increase in the binding affinity of TIGIT to PVR under an acidic tumor microenvironment has been recently identified to contribute toward the sensitivity of tumor cells to TIGIT blockade [67,68].
Although TIGIT blockade is known to mainly act on CD8+T and Treg cells, NK cell dependent efficacy of anti-TIGIT mAbs is also suggested. A recent study by Zhang et al. reported that treatment with anti-TIGIT mAbs 3 days after tumor cell implantation prevented tumor-infiltrating NK cell exhaustion in CT26 or methylcholanthrene (MCA)-induced fibrocarcinoma-bearing mice, which resulted in the enhancement of CD8+T cell responses and tumor rejection [34]. However, the mechanism through which TIGIT blockade has an impact primarily on NK cells compared to T cells and the mechanism through which NK cells promote CD8+T cell responses need to be further elucidated, since these results are contradictory to those of previous studies, revealing the CD8+T or the Treg cell-mediated effect of TIGIT blockade using temporary depletion of these populations with specific antibodies [35,42,55]. A more recent study reported that anti-TIGIT mAbs enhanced IL-15-driven NK cell cytotoxicity in both B16F10 and LWT1 metastatic melanoma-bearing mice [69].
The potency of human anti-TIGIT blocking mAbs on CD8+T cells has been demonstrated in cancer patients. Cancer testis antigen NY-ESO-1-specific CD8+T cell responses are increased by the addition of blocking mAbs against TIGIT and/or PD-1 when peripheral blood mononuclear cells (PBMCs) from melanoma patients are stimulated with NY-ESO-1157–165 peptide. Furthermore, TIGIT blockade increases the capacity for proliferation and degranulation of CD8+TILs from advanced melanoma patients upon TCR stimulation using autologous non-CD3 cells and anti-CD3 mAbs [50]. Upon TCR stimulation with anti-CD2/anti-CD3/anti-CD28 microbeads, bone marrow (BM) CD8+T cells in MM patients show increased CD107a expression and cytokine production in response to TIGIT blockade [35]. When anti-TIGIT mAbs are added to ex vivo co-culture of CD3+TILs and Mel-624 cells expressing membrane-bound anti-CD3 scFv (Mel-624 OKT3), IFN-γ and IL-2 production by CD3+TILs from patients with endometrial, ovarian, kidney, head and neck, and lung cancers is promoted [14]. A recent study reported that antigen specific responses to CEF (CMV, EBV, flu) peptide are augmented by TIGIT blockade in peripheral blood CD8+T cells derived from pancreatic ductal adenocarcinoma (PDAC) patients after mFOLFIRINOX therapy [43].
2.3.3. Mode of Action of Anti-TIGIT Therapy
Competitive binding of TIGIT and CD226 to PVR has been known as a key mechanism of TIGIT-driven immune suppression, and anti-TIGIT blocking mAbs are presumed to reverse the suppression by inhibiting TIGIT binding to PVR. This may occur as a mode of action; however, several questions need to be addressed for its clinical success and further translation of other members of TIGIT family receptors into cancer immunotherapy.
Intracellular Regulation by Anti-TIGIT mAbs
Despite the importance of understanding the molecular interplay between TIGIT, CD226, and PVR, the mechanism through which extracellular signals from the receptor-ligand binding/receptor dynamics are integrated into the intracellular regulation, particularly in the context of anti-TIGIT therapy, remains unclear.
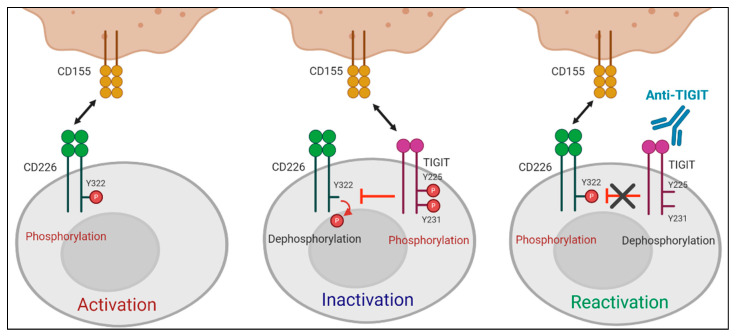
A recent study by Jin et al. reported that the effect of TIGIT blockade depends on tyrosine phosphorylation at Y322 of CD226, which was the first study to define the molecular requirements for anti-TIGIT blocking mAbs [43]. They showed that TIGIT-mediated intracellular inhibition of CD226 phosphorylation at Y322 was restored by TIGIT blockade. Moreover, CD226 mutant at Y322 (CD226Y322A) expressing CD8+T cells did not respond to TIGIT blockade, whereas CD226WT or CD226Y329A expressing CD8+T cells produced increased IFN-γ upon treatment with anti-TIGIT mAbs, suggesting that TIGIT blockade promotes T cell activation via CD226 phosphorylation at Y322 (Figure 2). CD226 dependent effect of anti-TIGIT mAbs was further shown in effector memory CD8+T cells expressing a low level of CD226 (CD226loCD8+Tem) not responsive to both antigen stimulation and anti-TIGIT mAb treatment. CD226 activation using anti-CD226 agonist mAbs renders CD226loCD8+Tem responsive to TIGIT blockade.
Isotype Selection of Anti-TIGIT mAbs
Figure 2.
Role of CD226 in anti-TIGIT immunotherapy. TIGIT has a direct effect on intracellular regulation of CD226 activation in response to PVR binding. (Left) When TIGIT expression is absent or low, engagement of CD226 with PVR induces the phosphorylation of tyrosine 322 (Y322) on CD226, which leads to the activation of intracellular signaling cascades. (Middle) PVR preferentially binds to upregulated TIGIT over CD226. Upon interaction with PVR, the cytoplasmic tail of TIGIT is phosphorylated. This PVR-induced TIGIT phosphorylation inhibits T cell responses by promoting CD226 dephosphorylation. (Right) TIGIT blockade suppresses PVR-induced TIGIT phosphorylation and restores the impaired Y322 phosphorylation of CD226, thereby leading to T cell activation.
Recently, several studies have highlighted the importance of selecting appropriate fragment crystallizable (Fc) region for therapeutic antibodies. To date, the approved human therapeutic IgG antibodies belong to IgG1, IgG2, or IgG4 subclasses [70]. It is increasingly clear that binding of the Fc region of antibody to Fc gamma receptors (FcγRs) can elicit various immunomodulatory functions, including antibody dependent-cellular cytotoxicity (ADCC), complement-dependent cytotoxicity (CDC), and antibody-dependent cellular phagocytosis (ADCP) [71]. In addition, FcγR binding was reported to enhance agonistic activity of mAbs targeting tumor necrosis factor receptor superfamily members, such as CD28, CD137, CD40, and OX40 (CD134) [72].
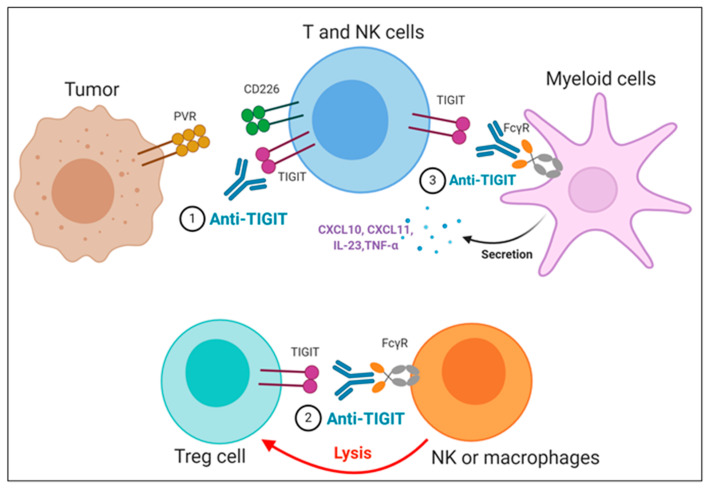
The importance of the Fc domain of anti-TIGIT mAb is emphasized by the findings that anti-TIGIT mAb with Fc devoid of effector functions, which was intended to solely block TIGIT binding to its ligands, fails to exert any of anti-tumor efficacies in preclinical models [36,73,74]. It may be due to the loss of its depleting activity against TIGIT-expressing intratumoral Treg cells, which has been considered as a potential mechanism of anti-TIGIT mAb-mediated anti-tumor effect [74]; however, it is still not clear whether the anti-tumor efficacy of anti-TIGIT mAbs depends on Treg depletion, since there are recent reports that anti-TIGIT mAbs on mIgG2a isotype induce anti-tumor responses without evidence of Treg depletion in mouse tumor models [36,73]. It may possible that FcγR on APC could act as a scaffold to crosslink anti-TIGIT mAb bound to TIGIT on immune cells, which may enhance the effect of TIGIT antagonism independent of Treg cells. In addition, Han et al. recently have shown that the antibody-FcγR engagement induced activation of myeloid cells, leading to pro-inflammatory chemokine and cytokine secretion (Figure 3) [36]. Comparison of clinical activities of anti-human TIGIT mAbs with different Fc scaffolds could provide insight into whether FcγR binding is required for optimal anti-tumor responses of TIGIT blockades.
Figure 3.
Proposed mechanisms of anti-TIGIT monoclonal antibodies (mAbs) in cancer immunotherapy. (1) Blockade of TIGIT could reverse the exhaustion of T and NK cell-mediated anti-tumor immunity. (2) Intratumoral regulatory T cells (Treg_) cells expressing high levels of TIGIT could be preferentially depleted by anti-TIGIT mAbs, presumably through antibody-dependent cellular phagocytosis (ADCP) by macrophages and/or antibody-dependent cellular cytotoxicity (ADCC) by NK cells. (3) The TIGIT mAb- fragment crystallizable (Fc) gamma receptors (FcγR) engagement could activate myeloid cells, leading to enhanced antigen presentation function and proinflammatory chemokine and cytokine secretion.
2.4. Anti-TIGIT Antibodies in Clinical Trials
Approximately 10 human anti-TIGIT mAbs, which have different IgG isotypes or mutant forms, have entered clinical trials. Table 1 summarizes publicly available data regarding antibody isotype, combination with different drugs, current development phase, and cancer types. Numerous clinical trials are evaluating the safety and the efficacy of anti-TIGIT mAb either as a monotherapy or in combination with PD-1/PD-L1 blockade or chemotherapies for the treatment of various cancers. Recently, the phase II CITYSCAPE trial presented significant response rates of tiragolumab plus atezolizumab in PD-L1-positive non-small cell lung cancer (NSCLC). The study revealed a significant objective response rate (ORR) improvement for the combination group (37% vs. 21%) as well as progression-free survival (PFS) improvement (5.6 vs. 3.9 months; hazard ratio [HR] 0.58). Importantly, patients in the combination group with high PD-L1 expression had an ORR of 66% compared with 24% in the atezolizumab group [75].
Table 1.
Clinical trials of TIGIT inhibitors.
| TIGIT Inhibitor | Sponsor | Isotype | Identifiers | Cancer Type | Combination | Phase | Recruitment Status | Start Date |
|---|---|---|---|---|---|---|---|---|
| ASP-8374 | Astellas Pharma Inc. | IgG4 | NCT03260322 | Advanced solid tumor | ASP-8374 alone; Pembrolizumab (anti-PD-1) |
Phase 1b | No longer recruiting | 8 September 2017 |
| NCT03945253 | Advanced solid tumor | ASP-8374 alone | Phase 1 | No longer recruiting | 5 August 2019 | |||
| BGB-A1217 | BeiGene Co Ltd. | IgG1 | NCT04047862 | Advanced solid tumor | Tislelizumab (anti-PD-1) | Phase 1 | Recruiting | 26 August 2019 |
| BMS-986207 | Bristol-Myers Squibb Co. | IgG1 (Fc receptor disabled) |
NCT02913313 | Advanced solid tumor | BMS-986207 alone; Nivolumab (anti-PD-1) |
Phase 1/2 | No longer recruiting | 29 November 2016 |
| NCT04150965 | Multiple myeloma | BMS-986207 alone; Dexamethasone+Pomalidomide |
Phase 1/2 | Recruiting | 16 April 2018 | |||
| NCT04570839 | Advanced solid tumor | COM-701 (PVRIG inhibitor) + Nivolumab (anti-PD-1) | Phase 1/2 | Recruiting | 31 August 2020 | |||
| NCT04065425 | Multiple myeloma | Dexamethasone + Pomalidomide | Phase 1/2 | Not yet recruiting | 1 October 2019 | |||
| COM-902 | Compugen Ltd. | IgG4 | NCT04354246 | Advanced solid tumor | COM-902 alone | Phase 1 | Recruiting | 31 March 2020 |
| AB154 (Domvanalimab) |
Arcus Biosciences Inc. | IgG1 (Fc receptor disabled) |
NCT03628677 | Advanced malignancy | AB154 alone; Zimberelimab (anti-PD-1) |
Phase 1 | Recruiting | 12 September 2018 |
| NCT04656535 | Recurrent Glioblastoma | Zimberelimab (anti-PD-1) | Phase 1 | Not yet recruiting | 31 January 2021 | |||
| NCT04262856 | PD-L1 positive lung cancer | Zimberelimab (anti-PD-1); Zimberelimab + etrumadenant (A2aR and A2bR antagonist) |
Phase 2 | Recruiting | 28 May 2020 | |||
| EOS-884448 | iTeos Therapeutics | IgG1 | NCT04335253 | Advanced tumor | EOS-884448 alone | Phase 1/2 | Recruiting | 18 February 2020 |
| Etigilimab (OMP-313M32) |
OncoMed | IgG1 | NCT03119428 | Advanced solid tumor | Etigilimab alone; Nivolumab (anti-PD-1) |
Phase 1 | Terminated | 2 May 2017 |
| IBI-939 | Innovent Biologics Inc. | Not disclosed | NCT04353830 | Advanced tumor | IBI-939 alone; Sintilimab (anti-PD-1) |
Phase 1a | Recruiting | 22 May 2020 |
| NCT04672356 | Advanced lung cancer | Sintilimab (anti-PD-1) | Phase 1a | Not yet recruiting | 28 January 2021 | |||
| NCT04672369 | Advanced NSCLC | Sintilimab (anti-PD-1) | Phase 1b | Not yet recruiting | 6 June 2021 | |||
| M-6223 | Serono Research Institute Inc, Merck KGaA | Not disclosed | NCT04457778 | Advanced solid tumor | M-6223 alone; Bintrafusp alfa (TGF beta ligand inhibitor) |
Phase 1 | Recruiting | 10 July 2020 |
| Vibostolimab (MK-7684) | Merck Sharp & Dohme Corp. | IgG1 | NCT02964013 | Advanced solid tumor | Vibostolimab alone; Pembrolizumab (anti-PD-1); Pembrolizumab + Pemetrexed + Carboplatin; Pembrolizumab + Carboplatin or Cisplatin + Etoposide |
Phase 1 | Recruiting | 13 December 2016 |
| NCT04305054 | Advanced melanoma | Pembrolizumab (anti-PD-1); | Phase 1/2 | Recruiting | 1 July 2020 | |||
| NCT04303169 | Melanoma | Pembrolizumab (anti-PD-1) | Phase 1/2 | Recruiting | 26 June 2020 | |||
| NCT04305041 | Refractory melanoma | Pembrolizumab + Quavonlimab (anti-CTLA4) | Phase 1/2 | Recruiting | 26 June 2020 | |||
| NCT04165070 | Advanced NSCLC | Pembrolizumab + Carboplatin + Paclitaxel; Pembrolizumab + Pemetrexed |
Phase 2 | Recruiting | 19 December 2019 | |||
| NCT02861573 | Prostate cancer | Pembrolizumab (anti-PD-1) | Phase 1/2 | Recruiting | 17 November 2016 | |||
| Tiragolumab (MTIG7192A) | Genentech Inc., Chugai Pharmaceutical Co. Ltd., Roche Holding AG | IgG1 | NCT04045028 | Relapse/Refractory Multiple myeloma and B-cell Non-Hodgkin lymphoma | Tiragolumab alone; Daratumumab (anti-CD38); Rituximab (anti-CD20) |
Phase 1 | Recruiting | 22 July 2019 |
| NCT02794571 | Metastatic solid tumor | Tiragolumab alone; Atezolizumab (anti-PD-L1); Chemotherapy (Carboplatin, Cisplatin, Etoposide, Paclitaxel, Pemetrexed) |
Phase 1 | Recruiting | 23 May 2016 | |||
| NCT03281369 | Metastatic esophageal cancer | Atezolizumab (anti-PD-L1); Atezolizumab + Cisplatin+5FU |
Phase 1/2 | Recruiting | 13 October 2017 | |||
| NCT04513925 | NSCLC | Atezolizumab (anti-PD-L1) | Phase 3 | Recruiting | 24 August 2020 | |||
| NCT04294810 | Metastatic NSCLC, PD-L1 selected | Atezolizumab (anti-PD-L1) | Phase 3 | Recruiting | 04 March 2020 | |||
| NCT04665843 | Metastatic head and neck cancer, PD-L1 positive | Atezolizumab (anti-PD-L1) | Phase 2 | Not yet recruiting | 21 January 2021 | |||
| NCT04543617 | Esophagus squamous cell carcinoma | Atezolizumab (anti-PD-L1) | Phase 3 | Recruiting | 28 September 2020 | |||
| NCT04300647 | Metastasis/Recurrent uterine cervix tumor, PD-L1 positive | Atezolizumab (anti-PD-L1) | Phase 2 | Recruiting | 30 June2020 | |||
| NCT03563716 | NSCLC, chemotherapy-naïve | Atezolizumab (anti-PD-L1) | Phase 2 | No longer recruiting | 10 August 2018 | |||
| NCT04665856 | Small-cell lung cancer | Atezolizumab + Carboplatin + Etoposide | Phase 3 | Recruiting | 4 January 2021 | |||
| NCT04619797 | Metastatic NSCLC | Atezolizumab + Pemetrexed + Carboplatin or Cisplatin | Phase 2 | Recruiting | 11 December 2020 | |||
| NCT04584112 | Triple-negative breast cancer | Atezolizumab + Nab-paclitaxel; Atezolizumab + Nab-pac-carbo-AC; Atezolizumab+Nab-pac-AC; |
Phase 1b | Recruiting | 28 September 2020 | |||
| NCT04256421 | Metastatic small-cell lung cancer | Atezolizumab + Carboplatin + Etoposide | Phase 3 | Recruiting | 4 February 2020 | |||
| NCT04540211 | Metastatic esophageal cancer | Atezolizumab + Paclitaxel + Cisplatin | Phase 3 | Recruiting | 4 November 2020 | |||
| NCT04524871 | Metastatic hepatocellular carcinoma | Atezolizumab + Bevacizumab (anti-VEGF) | Phase 1/2 | Recruiting | 2 November 2020 | |||
| NCT03869190 | Advanced urothelial carcinoma | Atezolizumab (anti-PD-L1) | Phase 1/2 | Recruiting | 1 June 2019 | |||
| NCT03193190 | Metastatic pancreatic ductal adenocarcinoma | Atezolizumab + Nab-Paclitaxe l+ Gemcitabine | Phase 1/2 | Recruiting | 5 July 2017 |
PD-L1: programmed death-ligand 1; NSCLC: non-small cell lung cancer; TGF: transforming growth factor; VEGF: vascular endothelial growth factor.
3. CD226
3.1. CD226 Structure and Its Ligands
CD226 is widely expressed in immune cells including T cells, NK cells, and monocytes [76]. CD226 is a transmembrane glycoprotein that comprises two immunoglobulin V-like domains (D1 and D2), a type I transmembrane domain, and an intracellular domain. The intracellular domain harbors two highly conserved phosphorylation sites, Y322 and S329, in humans (Y319 and S326 in murine ortholog). CD226 interacts with PVR and nectin-2. A structural analysis has revealed that the extracellular D1 domain of CD226 binds to PVR via a conserved docking mode [77]. Whether the D2 domain of CD226 is critical for its binding to PVR needs to be further investigated [78]. The measured solution binding affinity between human CD226-Fc and PVR-Fc is similar to that between CD226-Fc and nectin-2-Fc; however, CD226-Fc binds less efficiently to nectin-2 than PVR-expressing cells, suggesting that the homophilic interaction of nectin-2 might hinder CD226 binding to nectin-2 [79]. In addition, it has been reported that mouse CD226 only interacts with mouse PVR but not mouse nectin-2, which needs further clarification. Both PVR and nectin-2 expressions are upregulated on tumor cells, which contributes to tumor recognition and killing. Indeed, loss of PVR and nectin-2 on acute myeloid leukemia cells renders them resistant to NK cell-mediated killing [80]
PVR can be expressed in soluble form, lacking the transmembrane region, by alternative splicing in humans. Moreover, the mechanism by which the expression of membrane-bound PVR and soluble PVR (sPVR) is regulated remains unclear. High levels of sPVR are observed in the serum samples of patients with various types of cancers [81,82]. Okumura et al. have reported that sPVR inhibits CD226-mediated cytotoxicity of NK cells in a mouse tumor model. They suggested that sPVR could compete with membrane bound PVR and function as a neutralizing molecule for CD226 in NK cells. Interestingly, sPVR bound preferentially to CD226 over TIGIT and CD96, implying monomeric and dimeric PVR may function differently [83].
3.2. CD226 Signaling
The CD226 signaling pathway has been widely studied in NK cells. Upon engagement through corresponding ligands, CD226 is localized to lipid rafts and binds to the actin cytoskeleton through its association with human disc large protein or synapse-associated protein 97 (SAP97), the membrane-associated guanylate kinase homolog (MAGUK), and the actin-binding protein 4.1G [84,85]. During the formation of immunological synapse, CD226 transmits an activating signal, and thereafter, it induces the aggregation of lymphocyte function-associated antigen 1 (LFA-1) [86]. Protein kinase C (PKC) phosphorylates the S326 residue of CD226. This causes the association of LFA-1 with CD226. LFA-1 binds to intercellular adhesion molecule 1 (ICAM-1) and promotes its conformational change, leading to the recruitment of Fyn that phosphorylates the Y319 residue of CD226 [86]. CD226 phosphorylation at Y319 triggers activation of extracellular signal-regulated kinase (ERK) and AKT in NK cells upon the engagement of CD226 by the agonist mAbs, which is critical for NK cell cytotoxicity [87]. The physiological importance of CD226 Y319 phosphorylation is assessed in CD226Y319F KI (knock-in) mice that exhibit impaired cytotoxicity and cytokine production by NK cells. A similar observation on the role of CD226 phosphorylation at Y322 is made in human CD8+T cells. Exogenous expression of CD226WT or CD226Y322A in human CD8+T cells revealed that PVR-induced CD226 phosphorylation at Y322 is required for downstream signaling activation including ERK, p38, and AKT and corresponding T cell responses [43]. Next, the CD226 downstream signaling cascade leads to the phosphorylation of lymphocyte cytosolic protein 2 (LCP2) and vav guanine nucleotide exchange factor 1 (Vav1) [88]. Moreover, it activates phosphatidylinositol-4,5-bisphosphate phosphodiesterase gamma-2 (PLCγ2), ERK, and AKT downstream, thereby allowing degranulation and calcium mobilization [89]. The activated AKT phosphorylates forkhead box protein O1 (FOXO1) transcription factor, which induces the translocation of FOXO1 from the nucleus to the cytoplasm, where it is degraded and inactivated, thereby removing the negative regulator of NK cell activation [90].
3.3. CD226 in Tumor Immunity
The importance of the CD226–PVR axis in regulating tumor immunity has been shown in vitro and in vivo in preclinical mouse models. CD8+ T cells or DX5+ (CD49b) NK cells isolated from CD226-deficient mice are less cytotoxic to PVR-expressing tumor cells but not to PVR-negative tumor cells [91]. Moreover, reduced proliferative capacity of CD226 deficient-OT-I CD8+T cells was observed upon stimulation with the ovalbumin (OVA) peptide pulsed EL4 cells expressing PVR. However, the proliferation of CD226-deficient OT-I T cells was not impaired when stimulated with OVA peptide pulsed dendritic cells, suggesting that CD226 may promote effector T cell function in environments where co-stimulatory ligand expressions is limited, such as in tumors [92]. Consistent with the in vitro results, CD226 deficient mice also display a greater tumor burden than WT mice to a variety of tumors [38,90,92,93]. Impaired NK-cell-mediated suppression of tumor growth by CD226 deficiency has been reported in B16/F10 or RM-1 lung-metastases mouse models [38,92]. The effect of inhibiting the CD226–PVR axis on anti-tumor immune responses was investigated using anti-CD226 blocking mAbs. Blockade of CD226 with anti-CD226 antagonist mAb did not influence the tumor growth in mice [42,94,95]. However, administering anti-CD226 mAbs to mice treated with the combination of anti-TIGIT and anti-PD-L1 mAbs or anti-PD-1 and anti-GITR (glucocorticoid-induced TNFR-related protein) mAbs reversed the anti-tumor effect and the survival benefit of the combined treatment, which was accompanied by reduced effector function and frequency of CD8+T cells at the tumor site [42,95].
3.3.1. CD226 Downregulation in Dysfunctional T Cells
CD226 downregulation has been reported in T or NK cells of patients with cancer or human immunodeficiency virus (HIV) [26,43,49,50,96,97,98,99,100,101,102,103], which most likely occurs with an upregulation of PD-1 and TIGIT and impaired functionality. NY-ESO-1-specific CD8+TILs express low levels of CD226 and high levels of TIGIT and PD-1 in melanoma patients, but this imbalance is not found in circulating CD8+T cells regardless of specificity for NY-ESO-1 [50]. Moreover, CD226 expression is inversely proportional to TIGIT expression in peripheral blood CD8+T cells from AML patients [49]. A similar phenotype is observed in CD8+TILs from patients with renal cell carcinoma (RCC), colorectal cancer (CRC), and NSCLC that display upregulation of PD-1, TIGIT, Lag-3, and Tim-3 with reduced CD226 expression [43]. Further phenotypic dissection of the CD8+TILs from mouse tumor models reveals that an exhausted phenotype is presented with an increased expression of TIGIT, PD-1, Tim-3, Lag-3, CD101, CD38, and eomesodermin (Eomes) in CD226loCD8+TILs. Consistent with the phenotypic features, both polyfunctionality and proliferative capacity are attenuated in CD226loCD8+TILs compared with CD226hiCD8+TILs [43]. The correlation between CD226 downregulation and functional defect of CD8+T cells is presented in a mouse MM model that had experienced a relapse after autologous stem cell transplantation. BM CD8+T cells from relapsed MM mice display phenotypic and functional characteristics of exhaustion together with reduced CD226 expression, whereas MM-controlled mice retain high CD226 expression in the BM [102]. A recent study reported the transcriptional differences between CD226hi and CD226neg CD8+TILs using single-cell RNA sequencing in conjunction with cellular indexing of transcriptomes and epitopes by sequencing [99]. Furthermore, gene enrichment related to effector function and immunological synapse formation was found in CD226hiCD8+TILs from HCmel12hgp100 melanoma-bearing mice; however, unlike the previous studies on the inverse correlation between CD226 and co-inhibitory receptor expression on the surface of CD8+TILs, the expression of co-inhibitory receptor genes was unaltered in CD8+TILs regardless of CD226 expression. This discrepancy may occur from heterogeneity or different status of Tex cell differentiation depending on the tumor burden or variations in tumor models. Indeed, the gene expression profiles in CD226negCD8+TILs did not appear to be uniformly defined as a particular subset [99].
A similar approach was employed in human CD8+T cells from healthy donors to delineate the molecular differences between CD226+ and CD226− CD8+T cells under resting state and upon TCR stimulation [100]. Resting CD226− CD8+Tem cells displayed gene expression profiles comparable to CD226+CD8+T cells. Although genes involved in T cell activation were found in both CD226− and CD226+CD8+Tem cells upon TCR stimulation, activated CD226− CD8+Tem cells revealed the enrichment of gene signatures of resting T cells, Treg cells, and TGF-β signaling, which would contribute toward understanding the hypo-responsiveness of CD226−CD8+Tem cells upon TCR/CD28 or antigen-specific stimulation [43,100]; however, it remains unclear whether the gene profiles in CD226−CD8+Tem cells are the cause or the result of CD226 downregulation. Since the association of CD226 downregulation with progressive differentiation has been demonstrated in human CD8+T cells under steady-state conditions [43] and upon aging [103], further genetic and epigenetic insights are required to decipher the role of CD226 in T cell regulation. CD226 downregulation is also found in Treg cells, γδ T cells, and NK cells of cancer patients. The proportion of highly suppressive CD25hiFoxp3+Treg cells is increased in melanoma patients who present a high TIGIT/CD226 ratio in tumor-infiltrating Treg cells. This ratio is also associated with dismal clinical outcome after anti-PD-1 and/or anti-CTLA4 therapies [47]. Increased γδ T cell proportions with high TIGIT and low CD226 expression are correlated with decreased overall survival rates in AML patients [101]. In addition, the inverse expression between CD226 and TIGIT and/or PD-1 is indicative of the disease status in MDS patients [58].
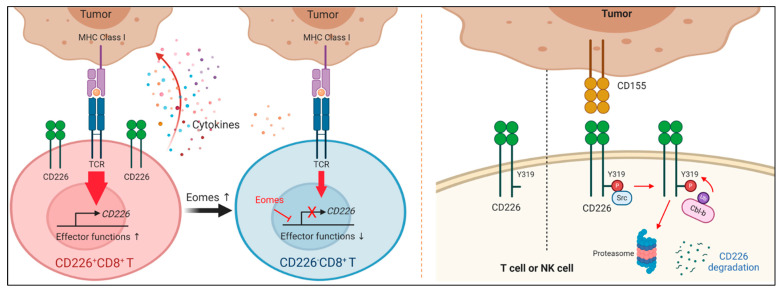
3.3.2. Mechanisms of CD226 Downregulation
Recent studies have suggested that the downregulation of CD226 is mediated via both an eomesodermin (Eomes)-dependent transcriptional mechanism and a CD155-mediated posttranslational mechanism (Figure 4) [99,100]. Weulersse et al. found that Eomes level is higher in CD226−CD8+ T cells and that CD226 downregulation is abrogated in Eomes-deficient CD8+ T cells. In contrast, CD226− CD8+ T cells are increased in the spleens of Eomes-overexpressing mice. Eomes is recruited to a regulatory region of CD226, suggesting it may directly regulate CD226 expression at the transcriptional level; however, since Eomes is a well-known key transcription factor for modulating homeostasis of both CD8+memory T and Tex cells [4], it needs to be further addressed whether Eomes directly regulates CD226, or affected immune responses by Eomes upregulation is responsible for CD226 downregulation. Indeed, all Eomes-expressing T cells do not lose CD226 expression, suggesting that there are other factors regulating CD226 transcription [99]. Braun et al. showed that CD226 expression is higher on TILs in CD155 deficient tumors than in the WT tumors. Mice with a CD226Y319F mutation have increased frequencies of CD226hiCD8+ TILs, correlating with enhanced effector function against tumors. Engagement with PVR induces decreased surface expression of CD226, which is dependent on CD226 Y319 phosphorylation. E3 ubiquitin ligase Casitas B-lineage lymphoma proto-oncogene-b (Cbl-b) could be involved in ubiquitination-dependent degradation of CD226 [100]. However, further clarification on the role of CD226 phosphorylation at Y319 or Y322 in regulating T cell activation is required since these results suggest a conflicting role to those of previous studies [43,87].
Figure 4.
Mechanisms of CD226 downregulation. (Left) Tumor microenvironment promotes the accumulation of a subset of CD8+ T cells that lose CD226. CD226 is transcriptionally downregulated in an eomesodermin (Eomes)-dependent and a PVR-independent manner. CD226 downregulation is abolished in Eomes-deficient CD8+ T cells. Eomes directly interacts with regulatory elements of the CD226 gene. (Right) CD226 expression is posttranslationally regulated through the ubiquitin–proteasome pathway. After engagement with PVR, mouse CD226 is phosphorylated at Y319 by Scr kinase, subsequently recruiting E3 ubiquitin ligase Cbl-b, which induces ubiquitination-dependent proteasomal degradation of phosphorylated CD226.
3.3.3. Predictive Value of CD226 for Immune Checkpoint Blockade Therapy
In accordance with the CD226-dependent regulation of CD8+T cell response, the differential response between CD226hi and CD226loCD8+T cells is reported in immune checkpoint blockade therapies, including anti-TIGIT or anti-PD-1 mAbs. Upon stimulation with CEF peptide, FACS-sorted CD226loCD8+Tem cells from healthy donors fail to respond to TIGIT and/or PD-1 blockade, whereas the CEF-specific responses of CD226hiCD8+Tem cells are enhanced [43]. This observation is further validated in a translational setting. Upregulation of CD226 is found in peripheral blood CD8+T cells from PDAC patients after mFOLFIRINOX chemotherapy, which is associated with an elevated responsiveness of antigen-specific CD8+T cells to treatment with anti-TIGIT or anti-PD-1 mAbs, and has also been reported in the mouse tumor models [43]. Wang et al. demonstrated that combination treatment of anti-PD-1 mAbs with anti-GITR agonist mAbs elicited anti-tumor efficacy in MC38-bearing mice in a CD226-dependent manner [95]. CD226 deficiency or blocking with anti-CD226 mAbs rendered tumor-bearing mice resistant to the combined treatment, which implies that CD226 is required for the efficacy of anti-PD-1 and anti-GITR mAb combination treatment. In a mouse melanoma model, CD8+TILs showed differential responsiveness to anti-PD-1 mAb treatment by CD226 expression [100].
4. Conclusions
TIGIT has emerged as a promising target for next generation cancer immunotherapy. Several clinical trials are currently evaluating the efficacy of anti-TIGIT mAbs in patients with different types of cancer. The most advanced candidate, tiragolumab, has exhibited remarkable efficacy in PD-L1-positive NSCLC patients in phase II clinical trials, in combination with PD-L1 blockade. However, the mode of action of TIGIT blockade remains to be fully elucidated. First, the association of CD226 activation with the efficacy of TIGIT blockade needs to be confirmed in clinical trials. Importantly, CD226hiCD8+T cells representing a predictive biomarker for several ICB therapies in a large cohort of patients with different cancer types need to be examined. Second, whether Fc engagement is necessary and required for the anti-tumor efficacy of TIGIT blockade remains to be defined. Further, it remains unclear whether the therapeutic effect of anti-TIGIT antagonist is mediated by the reactivation of Tex or NK cells, the depletion of Treg cells, the reprogramming of APC functions, or all of them. Several ongoing clinical trials will likely help provide answers to these questions.
Author Contributions
Conceptualization, Y.P., H.-s.J.; writing—original draft preparation, J.Y., M.K., D.-H.L., Y.P., H.-s.J.; visualization, M.K., D.-H.L.; writing—review and editing, Y.P., H.-s.J.; supervision, Y.P., H.-s.J.; funding acquisition/resources, Y.P., H.-s.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Research Foundation of Korea (NRF-2020R1I1A1A01073840 and NRF-2020M3A9G7103935) and KIST institutional program.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fritsch E.F., Burkhardt U.E., Hacohen N., Wu C.J. Personal Neoantigen Cancer Vaccines: A Road Not Fully Paved. Cancer Immunol. Res. 2020;8:1465–1469. doi: 10.1158/2326-6066.CIR-20-0526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang T., Shi T., Zhang H., Hu J., Song Y., Wei J., Ren S., Zhou C. Tumor neoantigens: From basic research to clinical applications. J. Hematol. Oncol. 2019;12:93. doi: 10.1186/s13045-019-0787-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zappasodi R., Merghoub T., Wolchok J.D. Emerging Concepts for Immune Checkpoint Blockade-Based Combination Therapies. Cancer Cell. 2018;33:581–598. doi: 10.1016/j.ccell.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLane L.M., Abdel-Hakeem M.S., Wherry E.J. CD8 T Cell Exhaustion During Chronic Viral Infection and Cancer. Annu. Rev. Immunol. 2019;37:457–495. doi: 10.1146/annurev-immunol-041015-055318. [DOI] [PubMed] [Google Scholar]
- 5.Wei S.C., Levine J.H., Cogdill A.P., Zhao Y., Anang N.A.S., Andrews M.C., Sharma P., Wang J., Wargo J.A., Pe’er D., et al. Distinct Cellular Mechanisms Underlie Anti-CTLA-4 and Anti-PD-1 Checkpoint Blockade. Cell. 2017;170:1120–1133.e17. doi: 10.1016/j.cell.2017.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreileder M., Barrett I., Bendtsen C., Brennan D., Kolch W. Signaling Dynamics Regulating Crosstalks between T-Cell Activation and Immune Checkpoints. Trends Cell Biol. 2020;31:224–235. doi: 10.1016/j.tcb.2020.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Lonberg N., Korman A.J. Masterful Antibodies: Checkpoint Blockade. Cancer Immunol. Res. 2017;5:275–281. doi: 10.1158/2326-6066.CIR-17-0057. [DOI] [PubMed] [Google Scholar]
- 8.Miller B.C., Sen D.R., Al Abosy R., Bi K., Virkud Y.V., LaFleur M.W., Yates K.B., Lako A., Felt K., Naik G.S., et al. Subsets of exhausted CD8(+) T cells differentially mediate tumor control and respond to checkpoint blockade. Nat. Immunol. 2019;20:326–336. doi: 10.1038/s41590-019-0312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tray N., Weber J.S., Adams S. Predictive Biomarkers for Checkpoint Immunotherapy: Current Status and Challenges for Clinical Application. Cancer Immunol. Res. 2018;6:1122–1128. doi: 10.1158/2326-6066.CIR-18-0214. [DOI] [PubMed] [Google Scholar]
- 10.Lesokhin A.M., Bal S., Badros A.Z. Lessons Learned from Checkpoint Blockade Targeting PD-1 in Multiple Myeloma. Cancer Immunol. Res. 2019;7:1224–1229. doi: 10.1158/2326-6066.CIR-19-0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arens R., Scheeren F.A. Genetic Screening for Novel Regulators of Immune Checkpoint Molecules. Trends Immunol. 2020;41:692–705. doi: 10.1016/j.it.2020.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Zebley C.C., Gottschalk S., Youngblood B. Rewriting History: Epigenetic Reprogramming of CD8(+) T Cell Differentiation to Enhance Immunotherapy. Trends Immunol. 2020;41:665–675. doi: 10.1016/j.it.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harjunpaa H., Guillerey C. TIGIT as an emerging immune checkpoint. Clin. Exp. Immunol. 2020;200:108–119. doi: 10.1111/cei.13407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whelan S., Ophir E., Kotturi M.F., Levy O., Ganguly S., Leung L., Vaknin I., Kumar S., Dassa L., Hansen K., et al. PVRIG and PVRL2 Are Induced in Cancer and Inhibit CD8(+) T-cell Function. Cancer Immunol. Res. 2019;7:257–268. doi: 10.1158/2326-6066.CIR-18-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marin-Acevedo J.A., Soyano A.E., Dholaria B., Knutson K.L., Lou Y. Cancer immunotherapy beyond immune checkpoint inhibitors. J. Hematol. Oncol. 2018;11:8. doi: 10.1186/s13045-017-0552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorvel L., Olive D. Targeting the “PVR-TIGIT axis” with immune checkpoint therapies. F1000Research. 2020;9 doi: 10.12688/f1000research.22877.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu X., Harden K., Gonzalez L.C., Francesco M., Chiang E., Irving B., Tom I., Ivelja S., Refino C.J., Clark H., et al. The surface protein TIGIT suppresses T cell activation by promoting the generation of mature immunoregulatory dendritic cells. Nat. Immunol. 2009;10:48–57. doi: 10.1038/ni.1674. [DOI] [PubMed] [Google Scholar]
- 18.Boles K.S., Vermi W., Facchetti F., Fuchs A., Wilson T.J., Diacovo T.G., Cella M., Colonna M. A novel molecular interaction for the adhesion of follicular CD4 T cells to follicular DC. Eur. J. Immunol. 2009;39:695–703. doi: 10.1002/eji.200839116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stanietsky N., Simic H., Arapovic J., Toporik A., Levy O., Novik A., Levine Z., Beiman M., Dassa L., Achdout H., et al. The interaction of TIGIT with PVR and PVRL2 inhibits human NK cell cytotoxicity. Proc. Natl. Acad. Sci. USA. 2009;106:17858–17863. doi: 10.1073/pnas.0903474106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levin S.D., Taft D.W., Brandt C.S., Bucher C., Howard E.D., Chadwick E.M., Johnston J., Hammond A., Bontadelli K., Ardourel D., et al. Vstm3 is a member of the CD28 family and an important modulator of T-cell function. Eur. J. Immunol. 2011;41:902–915. doi: 10.1002/eji.201041136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu S., Zhang H., Li M., Hu D., Li C., Ge B., Jin B., Fan Z. Recruitment of Grb2 and SHIP1 by the ITT-like motif of TIGIT suppresses granule polarization and cytotoxicity of NK cells. Cell Death Differ. 2013;20:456–464. doi: 10.1038/cdd.2012.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li M., Xia P., Du Y., Liu S., Huang G., Chen J., Zhang H., Hou N., Cheng X., Zhou L., et al. T-cell immunoglobulin and ITIM domain (TIGIT) receptor/poliovirus receptor (PVR) ligand engagement suppresses interferon-gamma production of natural killer cells via beta-arrestin 2-mediated negative signaling. J. Biol. Chem. 2014;289:17647–17657. doi: 10.1074/jbc.M114.572420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanchez-Correa B., Valhondo I., Hassouneh F., Lopez-Sejas N., Pera A., Bergua J.M., Arcos M.J., Banas H., Casas-Aviles I., Duran E., et al. DNAM-1 and the TIGIT/PVRIG/TACTILE Axis: Novel Immune Checkpoints for Natural Killer Cell-Based Cancer Immunotherapy. Cancers. 2019;11:877. doi: 10.3390/cancers11060877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martinet L., Smyth M.J. Balancing natural killer cell activation through paired receptors. Nat. Rev. Immunol. 2015;15:243–254. doi: 10.1038/nri3799. [DOI] [PubMed] [Google Scholar]
- 25.Reches A., Ophir Y., Stein N., Kol I., Isaacson B., Charpak Amikam Y., Elnekave A., Tsukerman P., Kucan Brlic P., Lenac T., et al. Nectin4 is a novel TIGIT ligand which combines checkpoint inhibition and tumor specificity. J. Immunother. Cancer. 2020;8 doi: 10.1136/jitc-2019-000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carlsten M., Norell H., Bryceson Y.T., Poschke I., Schedvins K., Ljunggren H.G., Kiessling R., Malmberg K.J. Primary human tumor cells expressing CD155 impair tumor targeting by down-regulating DNAM-1 on NK cells. J. Immunol. 2009;183:4921–4930. doi: 10.4049/jimmunol.0901226. [DOI] [PubMed] [Google Scholar]
- 27.Joller N., Hafler J.P., Brynedal B., Kassam N., Spoerl S., Levin S.D., Sharpe A.H., Kuchroo V.K. Cutting edge: TIGIT has T cell-intrinsic inhibitory functions. J. Immunol. 2011;186:1338–1342. doi: 10.4049/jimmunol.1003081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fuchs A., Cella M., Giurisato E., Shaw A.S., Colonna M. Cutting edge: CD96 (tactile) promotes NK cell-target cell adhesion by interacting with the poliovirus receptor (CD155) J. Immunol. 2004;172:3994–3998. doi: 10.4049/jimmunol.172.7.3994. [DOI] [PubMed] [Google Scholar]
- 29.Kucan Brlic P., Lenac Rovis T., Cinamon G., Tsukerman P., Mandelboim O., Jonjic S. Targeting PVR (CD155) and its receptors in anti-tumor therapy. Cell. Mol. Immunol. 2019;16:40–52. doi: 10.1038/s41423-018-0168-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X.Y., Das I., Lepletier A., Addala V., Bald T., Stannard K., Barkauskas D., Liu J., Aguilera A.R., Takeda K., et al. CD155 loss enhances tumor suppression via combined host and tumor-intrinsic mechanisms. J. Clin. Investig. 2018;128:2613–2625. doi: 10.1172/JCI98769. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Nishiwada S., Sho M., Yasuda S., Shimada K., Yamato I., Akahori T., Kinoshita S., Nagai M., Konishi N., Nakajima Y. Clinical significance of CD155 expression in human pancreatic cancer. Anticancer Res. 2015;35:2287–2297. [PubMed] [Google Scholar]
- 32.Triki H., Charfi S., Bouzidi L., Ben Kridis W., Daoud J., Chaabane K., Sellami-Boudawara T., Rebai A., Cherif B. CD155 expression in human breast cancer: Clinical significance and relevance to natural killer cell infiltration. Life Sci. 2019;231:116543. doi: 10.1016/j.lfs.2019.116543. [DOI] [PubMed] [Google Scholar]
- 33.Kurtulus S., Sakuishi K., Ngiow S.F., Joller N., Tan D.J., Teng M.W., Smyth M.J., Kuchroo V.K., Anderson A.C. TIGIT predominantly regulates the immune response via regulatory T cells. J. Clin. Investig. 2015;125:4053–4062. doi: 10.1172/JCI81187. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 34.Zhang Q., Bi J., Zheng X., Chen Y., Wang H., Wu W., Wang Z., Wu Q., Peng H., Wei H., et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat. Immunol. 2018;19:723–732. doi: 10.1038/s41590-018-0132-0. [DOI] [PubMed] [Google Scholar]
- 35.Guillerey C., Harjunpaa H., Carrie N., Kassem S., Teo T., Miles K., Krumeich S., Weulersse M., Cuisinier M., Stannard K., et al. TIGIT immune checkpoint blockade restores CD8(+) T-cell immunity against multiple myeloma. Blood. 2018;132:1689–1694. doi: 10.1182/blood-2018-01-825265. [DOI] [PubMed] [Google Scholar]
- 36.Han J.H., Cai M., Grein J., Perera S., Wang H., Bigler M., Ueda R., Rosahl T.W., Pinheiro E., LaFace D., et al. Effective Anti-tumor Response by TIGIT Blockade Associated With FcgammaR Engagement and Myeloid Cell Activation. Front. Immunol. 2020;11:573405. doi: 10.3389/fimmu.2020.573405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blake S.J., Stannard K., Liu J., Allen S., Yong M.C., Mittal D., Aguilera A.R., Miles J.J., Lutzky V.P., de Andrade L.F., et al. Suppression of Metastases Using a New Lymphocyte Checkpoint Target for Cancer Immunotherapy. Cancer Discov. 2016;6:446–459. doi: 10.1158/2159-8290.CD-15-0944. [DOI] [PubMed] [Google Scholar]
- 38.Chan C.J., Martinet L., Gilfillan S., Souza-Fonseca-Guimaraes F., Chow M.T., Town L., Ritchie D.S., Colonna M., Andrews D.M., Smyth M.J. The receptors CD96 and CD226 oppose each other in the regulation of natural killer cell functions. Nat. Immunol. 2014;15:431–438. doi: 10.1038/ni.2850. [DOI] [PubMed] [Google Scholar]
- 39.Vetizou M., Pitt J.M., Daillere R., Lepage P., Waldschmitt N., Flament C., Rusakiewicz S., Routy B., Roberti M.P., Duong C.P., et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015;350:1079–1084. doi: 10.1126/science.aad1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lozano E., Dominguez-Villar M., Kuchroo V., Hafler D.A. The TIGIT/CD226 axis regulates human T cell function. J. Immunol. 2012;188:3869–3875. doi: 10.4049/jimmunol.1103627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stanietsky N., Rovis T.L., Glasner A., Seidel E., Tsukerman P., Yamin R., Enk J., Jonjic S., Mandelboim O. Mouse TIGIT inhibits NK-cell cytotoxicity upon interaction with PVR. Eur. J. Immunol. 2013;43:2138–2150. doi: 10.1002/eji.201243072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnston R.J., Comps-Agrar L., Hackney J., Yu X., Huseni M., Yang Y., Park S., Javinal V., Chiu H., Irving B., et al. The immunoreceptor TIGIT regulates antitumor and antiviral CD8(+) T cell effector function. Cancer Cell. 2014;26:923–937. doi: 10.1016/j.ccell.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 43.Jin H.S., Ko M., Choi D.S., Kim J.H., Lee D.H., Kang S.H., Kim I., Lee H.J., Choi E.K., Kim K.P., et al. CD226(hi)CD8(+) T Cells Are a Prerequisite for Anti-TIGIT Immunotherapy. Cancer Immunol. Res. 2020;8:912–925. doi: 10.1158/2326-6066.CIR-19-0877. [DOI] [PubMed] [Google Scholar]
- 44.Chen X., Lu P.H., Liu L., Fang Z.M., Duan W., Liu Z.L., Wang C.Y., Zhou P., Yu X.F., He W.T. TIGIT negatively regulates inflammation by altering macrophage phenotype. Immunobiology. 2016;221:48–55. doi: 10.1016/j.imbio.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 45.Joller N., Lozano E., Burkett P.R., Patel B., Xiao S., Zhu C., Xia J., Tan T.G., Sefik E., Yajnik V., et al. Treg cells expressing the coinhibitory molecule TIGIT selectively inhibit proinflammatory Th1 and Th17 cell responses. Immunity. 2014;40:569–581. doi: 10.1016/j.immuni.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fuhrman C.A., Yeh W.I., Seay H.R., Saikumar Lakshmi P., Chopra G., Zhang L., Perry D.J., McClymont S.A., Yadav M., Lopez M.C., et al. Divergent Phenotypes of Human Regulatory T Cells Expressing the Receptors TIGIT and CD226. J. Immunol. 2015;195:145–155. doi: 10.4049/jimmunol.1402381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fourcade J., Sun Z., Chauvin J.M., Ka M., Davar D., Pagliano O., Wang H., Saada S., Menna C., Amin R., et al. CD226 opposes TIGIT to disrupt Tregs in melanoma. JCI Insight. 2018;3 doi: 10.1172/jci.insight.121157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang Z.Z., Kim H.J., Wu H., Jalali S., Tang X., Krull J., Ding W., Novak A.J., Ansell S.M. TIGIT expression is associated with T-cell suppression and exhaustion and predicts clinical outcome and anti-PD-1 response in follicular lymphoma. Clin. Cancer Res. 2020 doi: 10.1158/1078-0432.CCR-20-0558. [DOI] [PubMed] [Google Scholar]
- 49.Kong Y., Zhu L., Schell T.D., Zhang J., Claxton D.F., Ehmann W.C., Rybka W.B., George M.R., Zeng H., Zheng H. T-Cell Immunoglobulin and ITIM Domain (TIGIT) Associates with CD8+ T-Cell Exhaustion and Poor Clinical Outcome in AML Patients. Clin. Cancer Res. 2016;22:3057–3066. doi: 10.1158/1078-0432.CCR-15-2626. [DOI] [PubMed] [Google Scholar]
- 50.Chauvin J.M., Pagliano O., Fourcade J., Sun Z., Wang H., Sander C., Kirkwood J.M., Chen T.H., Maurer M., Korman A.J., et al. TIGIT and PD-1 impair tumor antigen-specific CD8(+) T cells in melanoma patients. J. Clin. Investig. 2015;125:2046–2058. doi: 10.1172/JCI80445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.He W., Zhang H., Han F., Chen X., Lin R., Wang W., Qiu H., Zhuang Z., Liao Q., Zhang W., et al. CD155T/TIGIT Signaling Regulates CD8(+) T-cell Metabolism and Promotes Tumor Progression in Human Gastric Cancer. Cancer Res. 2017;77:6375–6388. doi: 10.1158/0008-5472.CAN-17-0381. [DOI] [PubMed] [Google Scholar]
- 52.Lucca L.E., Lerner B.A., Park C., DeBartolo D., Harnett B., Kumar V.P., Ponath G., Raddassi K., Huttner A., Hafler D.A., et al. Differential expression of the T-cell inhibitor TIGIT in glioblastoma and MS. Neurol. Neuroimmunol. Neuroinflamm. 2020;7 doi: 10.1212/NXI.0000000000000712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ostroumov D., Duong S., Wingerath J., Woller N., Manns M.P., Timrott K., Kleine M., Ramackers W., Roessler S., Nahnsen S., et al. Transcriptome profiling identifies TIGIT as a marker of T cell exhaustion in liver cancer. Hepatology. 2020 doi: 10.1002/hep.31466. [DOI] [PubMed] [Google Scholar]
- 54.Stalhammar G., Seregard S., Grossniklaus H.E. Expression of immune checkpoint receptors Indoleamine 2,3-dioxygenase and T cell Ig and ITIM domain in metastatic versus nonmetastatic choroidal melanoma. Cancer Med. 2019;8:2784–2792. doi: 10.1002/cam4.2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu L., Mao L., Liu J.F., Chen L., Yu G.T., Yang L.L., Wu H., Bu L.L., Kulkarni A.B., Zhang W.F., et al. Blockade of TIGIT/CD155 Signaling Reverses T-cell Exhaustion and Enhances Antitumor Capability in Head and Neck Squamous Cell Carcinoma. Cancer Immunol. Res. 2019;7:1700–1713. doi: 10.1158/2326-6066.CIR-18-0725. [DOI] [PubMed] [Google Scholar]
- 56.Xu D., Zhao E., Zhu C., Zhao W., Wang C., Zhang Z., Zhao G. TIGIT and PD-1 may serve as potential prognostic biomarkers for gastric cancer. Immunobiology. 2020;225:151915. doi: 10.1016/j.imbio.2020.151915. [DOI] [PubMed] [Google Scholar]
- 57.Duan X., Liu J., Cui J., Ma B., Zhou Q., Yang X., Lu Z., Du Y., Su C. Expression of TIGIT/CD155 and correlations with clinical pathological features in human hepatocellular carcinoma. Mol. Med. Rep. 2019;20:3773–3781. doi: 10.3892/mmr.2019.10641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meng F., Li L., Lu F., Yue J., Liu Z., Zhang W., Fu R. Overexpression of TIGIT in NK and T Cells Contributes to Tumor Immune Escape in Myelodysplastic Syndromes. Front. Oncol. 2020;10:1595. doi: 10.3389/fonc.2020.01595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Westergaard M.C.W., Milne K., Pedersen M., Hasselager T., Olsen L.R., Anglesio M.S., Borch T.H., Kennedy M., Briggs G., Ledoux S., et al. Changes in the Tumor Immune Microenvironment during Disease Progression in Patients with Ovarian Cancer. Cancers. 2020;12:3828. doi: 10.3390/cancers12123828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tang W., Pan X., Han D., Rong D., Zhang M., Yang L., Ying J., Guan H., Chen Z., Wang X. Clinical significance of CD8(+) T cell immunoreceptor with Ig and ITIM domains(+) in locally advanced gastric cancer treated with SOX regimen after D2 gastrectomy. Oncoimmunology. 2019;8:e1593807. doi: 10.1080/2162402X.2019.1593807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.MacFarlane A.W., Yeung H.M., Alpaugh R.K., Dulaimi E., Engstrom P.F., Dasari A., Campbell K.S., Vijayvergia N. Impacts of pembrolizumab therapy on immune phenotype in patients with high-grade neuroendocrine neoplasms. Cancer Immunol. Immunother. 2021 doi: 10.1007/s00262-020-02811-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dixon K.O., Schorer M., Nevin J., Etminan Y., Amoozgar Z., Kondo T., Kurtulus S., Kassam N., Sobel R.A., Fukumura D., et al. Functional Anti-TIGIT Antibodies Regulate Development of Autoimmunity and Antitumor Immunity. J. Immunol. 2018;200:3000–3007. doi: 10.4049/jimmunol.1700407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hung A.L., Maxwell R., Theodros D., Belcaid Z., Mathios D., Luksik A.S., Kim E., Wu A., Xia Y., Garzon-Muvdi T., et al. TIGIT and PD-1 dual checkpoint blockade enhances antitumor immunity and survival in GBM. Oncoimmunology. 2018;7:e1466769. doi: 10.1080/2162402X.2018.1466769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Grapin M., Richard C., Limagne E., Boidot R., Morgand V., Bertaut A., Derangere V., Laurent P.A., Thibaudin M., Fumet J.D., et al. Optimized fractionated radiotherapy with anti-PD-L1 and anti-TIGIT: A promising new combination. J. Immunother. Cancer. 2019;7:160. doi: 10.1186/s40425-019-0634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bian Y., Hall B., Sun Z.J., Molinolo A., Chen W., Gutkind J.S., Waes C.V., Kulkarni A.B. Loss of TGF-beta signaling and PTEN promotes head and neck squamous cell carcinoma through cellular senescence evasion and cancer-related inflammation. Oncogene. 2012;31:3322–3332. doi: 10.1038/onc.2011.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chiu D.K., Yuen V.W., Wing-Sum Cheu J., Wei L.L., Ting V., Fehlings M., Sumatoh H., Nardin A., Newell E.W., Oi-Lin Ng I., et al. Hepatocellular Carcinoma Cells Up-regulate PVRL1, Stabilizing Poliovirus Receptor and Inhibiting the Cytotoxic T-Cell Response via TIGIT to Mediate Tumor Resistance to PD1 Inhibitors in Mice. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.074. [DOI] [PubMed] [Google Scholar]
- 67.Lee B.R., Chae S., Moon J., Kim M.J., Lee H., Ko H.W., Cho B.C., Shim H.S., Hwang D., Kim H.R., et al. Combination of PD-L1 and PVR determines sensitivity to PD-1 blockade. JCI Insight. 2020;5 doi: 10.1172/jci.insight.128633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jin H.S., Choi D.S., Ko M., Kim D., Lee D.H., Lee S., Lee A.Y., Kang S.G., Kim S.H., Jung Y., et al. Extracellular pH modulating injectable gel for enhancing immune checkpoint inhibitor therapy. J. Control Release. 2019;315:65–75. doi: 10.1016/j.jconrel.2019.10.041. [DOI] [PubMed] [Google Scholar]
- 69.Chauvin J.M., Ka M., Pagliano O., Menna C., Ding Q., DeBlasio R., Sanders C., Hou J., Li X.Y., Ferrone S., et al. IL15 Stimulation with TIGIT Blockade Reverses CD155-mediated NK-Cell Dysfunction in Melanoma. Clin. Cancer Res. 2020;26:5520–5533. doi: 10.1158/1078-0432.CCR-20-0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Beers S.A., Glennie M.J., White A.L. Influence of immunoglobulin isotype on therapeutic antibody function. Blood. 2016;127:1097–1101. doi: 10.1182/blood-2015-09-625343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen X., Song X., Li K., Zhang T. FcgammaR-Binding Is an Important Functional Attribute for Immune Checkpoint Antibodies in Cancer Immunotherapy. Front. Immunol. 2019;10:292. doi: 10.3389/fimmu.2019.00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mayes P.A., Hance K.W., Hoos A. The promise and challenges of immune agonist antibody development in cancer. Nat. Rev. Drug Discov. 2018;17:509–527. doi: 10.1038/nrd.2018.75. [DOI] [PubMed] [Google Scholar]
- 73.Waight J.D., Chand D., Dietrich S., Gombos R., Horn T., Gonzalez A.M., Manrique M., Swiech L., Morin B., Brittsan C., et al. Selective FcgammaR Co-engagement on APCs Modulates the Activity of Therapeutic Antibodies Targeting T Cell Antigens. Cancer Cell. 2018;33:1033–1047.e5. doi: 10.1016/j.ccell.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Preillon J., Cuende J., Rabolli V., Garnero L., Mercier M., Wald N., Pappalardo A., Denies S., Jamart D., Michaux A.C., et al. Restoration of T-cell Effector Function, Depletion of Tregs, and Direct Killing of Tumor Cells: The Multiple Mechanisms of Action of a-TIGIT Antagonist Antibodies. Mol. Cancer Ther. 2021;20:121–131. doi: 10.1158/1535-7163.MCT-20-0464. [DOI] [PubMed] [Google Scholar]
- 75.Anonymous. Tiragolumab Impresses in Multiple Trials. Cancer Discov. 2020;10:1086–1087. doi: 10.1158/2159-8290.CD-NB2020-063. [DOI] [PubMed] [Google Scholar]
- 76.Huang Z., Qi G., Miller J.S., Zheng S.G. CD226: An Emerging Role in Immunologic Diseases. Front. Cell Dev. Biol. 2020;8:564. doi: 10.3389/fcell.2020.00564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang H., Qi J., Zhang S., Li Y., Tan S., Gao G.F. Binding mode of the side-by-side two-IgV molecule CD226/DNAM-1 to its ligand CD155/Necl-5. Proc. Natl. Acad. Sci. USA. 2019;116:988–996. doi: 10.1073/pnas.1815716116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Deuss F.A., Watson G.M., Fu Z., Rossjohn J., Berry R. Structural Basis for CD96 Immune Receptor Recognition of Nectin-like Protein-5, CD155. Structure. 2019;27:219–228.e3. doi: 10.1016/j.str.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 79.Tahara-Hanaoka S., Shibuya K., Onoda Y., Zhang H., Yamazaki S., Miyamoto A., Honda S., Lanier L.L., Shibuya A. Functional characterization of DNAM-1 (CD226) interaction with its ligands PVR (CD155) and nectin-2 (PRR-2/CD112) Int. Immunol. 2004;16:533–538. doi: 10.1093/intimm/dxh059. [DOI] [PubMed] [Google Scholar]
- 80.Kearney C.J., Ramsbottom K.M., Voskoboinik I., Darcy P.K., Oliaro J. Loss of DNAM-1 ligand expression by acute myeloid leukemia cells renders them resistant to NK cell killing. Oncoimmunology. 2016;5:e1196308. doi: 10.1080/2162402X.2016.1196308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Iguchi-Manaka A., Okumura G., Kojima H., Cho Y., Hirochika R., Bando H., Sato T., Yoshikawa H., Hara H., Shibuya A., et al. Increased Soluble CD155 in the Serum of Cancer Patients. PLoS ONE. 2016;11:e0152982. doi: 10.1371/journal.pone.0152982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baury B., Masson D., McDermott B.M., Jr., Jarry A., Blottiere H.M., Blanchardie P., Laboisse C.L., Lustenberger P., Racaniello V.R., Denis M.G. Identification of secreted CD155 isoforms. Biochem. Biophys. Res. Commun. 2003;309:175–182. doi: 10.1016/S0006-291X(03)01560-2. [DOI] [PubMed] [Google Scholar]
- 83.Okumura G., Iguchi-Manaka A., Murata R., Yamashita-Kanemaru Y., Shibuya A., Shibuya K. Tumor-derived soluble CD155 inhibits DNAM-1-mediated antitumor activity of natural killer cells. J. Exp. Med. 2020;217 doi: 10.1084/jem.20191290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ralston K.J., Hird S.L., Zhang X., Scott J.L., Jin B., Thorne R.F., Berndt M.C., Boyd A.W., Burns G.F. The LFA-1-associated molecule PTA-1 (CD226) on T cells forms a dynamic molecular complex with protein 4.1G and human discs large. J. Biol. Chem. 2004;279:33816–33828. doi: 10.1074/jbc.M401040200. [DOI] [PubMed] [Google Scholar]
- 85.Hara H., Wada T., Bakal C., Kozieradzki I., Suzuki S., Suzuki N., Nghiem M., Griffiths E.K., Krawczyk C., Bauer B., et al. The MAGUK family protein CARD11 is essential for lymphocyte activation. Immunity. 2003;18:763–775. doi: 10.1016/S1074-7613(03)00148-1. [DOI] [PubMed] [Google Scholar]
- 86.Shibuya K., Lanier L.L., Phillips J.H., Ochs H.D., Shimizu K., Nakayama E., Nakauchi H., Shibuya A. Physical and functional association of LFA-1 with DNAM-1 adhesion molecule. Immunity. 1999;11:615–623. doi: 10.1016/S1074-7613(00)80136-3. [DOI] [PubMed] [Google Scholar]
- 87.Zhang Z., Wu N., Lu Y., Davidson D., Colonna M., Veillette A. DNAM-1 controls NK cell activation via an ITT-like motif. J. Exp. Med. 2015;212:2165–2182. doi: 10.1084/jem.20150792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bryceson Y.T., March M.E., Ljunggren H.G., Long E.O. Synergy among receptors on resting NK cells for the activation of natural cytotoxicity and cytokine secretion. Blood. 2006;107:159–166. doi: 10.1182/blood-2005-04-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kim H.S., Long E.O. Complementary phosphorylation sites in the adaptor protein SLP-76 promote synergistic activation of natural killer cells. Sci. Signal. 2012;5:ra49. doi: 10.1126/scisignal.2002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Du X., de Almeida P., Manieri N., de Almeida Nagata D., Wu T.D., Harden Bowles K., Arumugam V., Schartner J., Cubas R., Mittman S., et al. CD226 regulates natural killer cell antitumor responses via phosphorylation-mediated inactivation of transcription factor FOXO1. Proc. Natl. Acad. Sci. USA. 2018;115:E11731–E11740. doi: 10.1073/pnas.1814052115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Iguchi-Manaka A., Kai H., Yamashita Y., Shibata K., Tahara-Hanaoka S., Honda S., Yasui T., Kikutani H., Shibuya K., Shibuya A. Accelerated tumor growth in mice deficient in DNAM-1 receptor. J. Exp. Med. 2008;205:2959–2964. doi: 10.1084/jem.20081611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gilfillan S., Chan C.J., Cella M., Haynes N.M., Rapaport A.S., Boles K.S., Andrews D.M., Smyth M.J., Colonna M. DNAM-1 promotes activation of cytotoxic lymphocytes by nonprofessional antigen-presenting cells and tumors. J. Exp. Med. 2008;205:2965–2973. doi: 10.1084/jem.20081752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chan C.J., Andrews D.M., McLaughlin N.M., Yagita H., Gilfillan S., Colonna M., Smyth M.J. DNAM-1/CD155 interactions promote cytokine and NK cell-mediated suppression of poorly immunogenic melanoma metastases. J. Immunol. 2010;184:902–911. doi: 10.4049/jimmunol.0903225. [DOI] [PubMed] [Google Scholar]
- 94.Lakshmikanth T., Burke S., Ali T.H., Kimpfler S., Ursini F., Ruggeri L., Capanni M., Umansky V., Paschen A., Sucker A., et al. NCRs and DNAM-1 mediate NK cell recognition and lysis of human and mouse melanoma cell lines in vitro and in vivo. J. Clin. Investig. 2009;119:1251–1263. doi: 10.1172/JCI36022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang B., Zhang W., Jankovic V., Golubov J., Poon P., Oswald E.M., Gurer C., Wei J., Ramos I., Wu Q., et al. Combination cancer immunotherapy targeting PD-1 and GITR can rescue CD8(+) T cell dysfunction and maintain memory phenotype. Sci. Immunol. 2018;3 doi: 10.1126/sciimmunol.aat7061. [DOI] [PubMed] [Google Scholar]
- 96.Sanchez-Correa B., Gayoso I., Bergua J.M., Casado J.G., Morgado S., Solana R., Tarazona R. Decreased expression of DNAM-1 on NK cells from acute myeloid leukemia patients. Immunol. Cell Biol. 2012;90:109–115. doi: 10.1038/icb.2011.15. [DOI] [PubMed] [Google Scholar]
- 97.Cella M., Presti R., Vermi W., Lavender K., Turnbull E., Ochsenbauer-Jambor C., Kappes J.C., Ferrari G., Kessels L., Williams I., et al. Loss of DNAM-1 contributes to CD8+ T-cell exhaustion in chronic HIV-1 infection. Eur. J. Immunol. 2010;40:949–954. doi: 10.1002/eji.200940234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tauriainen J., Scharf L., Frederiksen J., Naji A., Ljunggren H.G., Sonnerborg A., Lund O., Reyes-Teran G., Hecht F.M., Deeks S.G., et al. Perturbed CD8(+) T cell TIGIT/CD226/PVR axis despite early initiation of antiretroviral treatment in HIV infected individuals. Sci. Rep. 2017;7:40354. doi: 10.1038/srep40354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Braun M., Aguilera A.R., Sundarrajan A., Corvino D., Stannard K., Krumeich S., Das I., Lima L.G., Meza Guzman L.G., Li K., et al. CD155 on Tumor Cells Drives Resistance to Immunotherapy by Inducing the Degradation of the Activating Receptor CD226 in CD8(+) T Cells. Immunity. 2020;53:805–823.e15. doi: 10.1016/j.immuni.2020.09.010. [DOI] [PubMed] [Google Scholar]
- 100.Weulersse M., Asrir A., Pichler A.C., Lemaitre L., Braun M., Carrie N., Joubert M.V., Le Moine M., Do Souto L., Gaud G., et al. Eomes-Dependent Loss of the Co-activating Receptor CD226 Restrains CD8(+) T Cell Anti-tumor Functions and Limits the Efficacy of Cancer Immunotherapy. Immunity. 2020;53:824–839.e10. doi: 10.1016/j.immuni.2020.09.006. [DOI] [PubMed] [Google Scholar]
- 101.Jin Z., Lan T., Zhao Y., Du J., Chen J., Lai J., Xu L., Chen S., Zhong X., Wu X., et al. Higher TIGIT(+)CD226(-) gammadelta T cells in Patients with Acute Myeloid Leukemia. Immunol. Invest. 2020:1–11. doi: 10.1080/08820139.2020.1806868. [DOI] [PubMed] [Google Scholar]
- 102.Minnie S.A., Kuns R.D., Gartlan K.H., Zhang P., Wilkinson A.N., Samson L., Guillerey C., Engwerda C., MacDonald K.P.A., Smyth M.J., et al. Myeloma escape after stem cell transplantation is a consequence of T-cell exhaustion and is prevented by TIGIT blockade. Blood. 2018;132:1675–1688. doi: 10.1182/blood-2018-01-825240. [DOI] [PubMed] [Google Scholar]
- 103.Song Y., Wang B., Song R., Hao Y., Wang D., Li Y., Jiang Y., Xu L., Ma Y., Zheng H., et al. T-cell Immunoglobulin and ITIM Domain Contributes to CD8(+) T-cell Immunosenescence. Aging Cell. 2018;17 doi: 10.1111/acel.12716. [DOI] [PMC free article] [PubMed] [Google Scholar]