Accumulating evidence has clearly suggested that cardiometabolic risk factors such as obesity, hypertension, dyslipidemia and diabetes mellitus (DM) are associated with a more severe disease course and worse clinical outcomes of coronavirus disease 2019 (COVID-19) [1].
COVID-19 severity is predicted by the presence of older age and a variety of obesity-related comorbidities [2]. Patients with obesity are at increased risk for developing severe pneumonia and requiring mechanical ventilation due to impaired respiratory mechanics and the concomitant presence of comorbidities such as DM, cardiovascular and renal disease, which further increase their vulnerability to multi-organ dysfunction [2].
Black, Latinos and Native Americans suffer disproportionate rates of severe acute respiratory syndrome-coronavirus 2 (SARS-CoV2) infections, hospitalizations and deaths [3]. Socioeconomic factors including racial discrimination, food insecurity, limited availability of healthy food, poor access to health care facilities, low level of education and socioeconomic status, and lack of job flexibility may all contribute to this disparity. These social determinants of health, combined with underlying health inequities in obesity-related chronic diseases, may inevitably culminate in severe COVID-19 outcomes in these socioeconomically deprived populations.
DM is characterized by enhanced susceptibility to infections due to inherent neutrophil dysfunction, reduced T-cell responses and disordered humoral immunity [4]. Furthermore, there seems to be a direct underlying endocrine/metabolic link between DM and severe COVID-19 [5]. In patients at metabolic risk, hyperglycemia, metabolic inflammation, enhanced cytokine release and endothelial dysfunction have been all implicated in the COVID-19-associated multi-organ dysfunction. [4,5]. SARS-CoV2 utilizes host angiotensin converting enzyme 2 (ACE2) to facilitate viral fusion and cell entry. ACE2 is highly expressed in the lungs, heart, endothelium, kidneys and pancreatic beta cells. The acute infection of beta cells by SARS-CoV2 has been associated with subsequent dysfunction and hyperglycemia due to diminished insulin secretion. The resultant acute hyperglycemia seems to upregulate ACE2 expression in other tissues, possibly enhancing viral entry into additional host cells. The downstream effects of angiotensin (1–9) and (1–7), resulting from the conversion of angiotensin I and II respectively by ACE2, include anti-inflammatory and anti-proliferative actions which are thought to limit acute inflammatory injury. Chronic hyperglycemia due to DM down-regulates the anti-inflammatory effects of ACE2 [4,5]. This vulnerability, coupled with the inherent underlying inflammatory milieu and immune defects seen in obesity and DM, provides SARS-CoV2 a pathway for causing exaggerated and prolonged lung injury and severe multi-system disease.
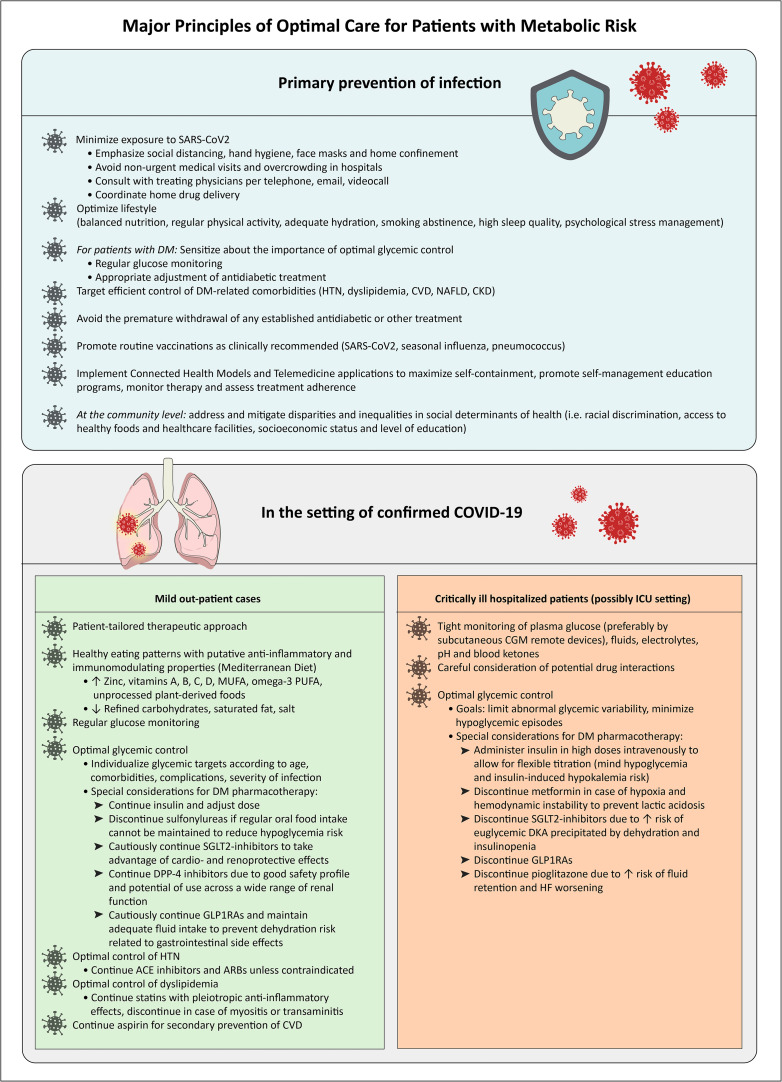
In the absence of randomized clinical trials, the optimal strategy for achieving metabolic control in patients with COVID-19 remains unknown. Relevant recommendations have been published last year [[4], [5], [6]], but have not yet been updated in 2021 in view of novel scientific evidence. In Fig. 1 , we summarize the major principles of optimal care for patients with metabolic risk and COVID-19 based on the currently available evidence.
Fig. 1.
Flowchart summarizing the major general principles of optimal management of patients at metabolic risk during the COVID-19 pandemic
Abbreviations:
ACE: angiotensin converting enzyme; ARBs: angiotensin II type 1 receptor blockers; CGM: continuous glucose monitoring; CKD: chronic kidney disease; COVID-19: coronavirus disease 2019; CVD: cardiovascular disease; DKA: diabetic ketoacidosis; DM: diabetes mellitus; DPP4: dipeptidyl-peptidase 4; GLP1RAs: glucagon-like peptide 1 receptor agonists; ICU: intensive care unit; MUFA: monounsaturated fatty acids; NAFLD: non-alcoholic fatty liver disease; PUFA: polyunsaturated fatty acids; SARS-CoV2: severe acute respiratory syndrome-coronavirus-2; SGLT2: sodium-glucose cotransporter 2.
The adherence to lifestyle interventions can be challenging amidst the pandemic given the limited access to healthy foods and the impact of social distancing and facility closures on regular exercise. This is particularly salient in areas of the world where governments have implemented generalized lockdowns to halt the spread of SARS-CoV2. The amelioration of such barriers will require systemic social programs to be implemented so that this therapeutic modality can be fully accessed.
Optimizing nutrition may produce a tangible impact upon COVID-19 risk. The Mediterranean diet, mostly composed of whole grains, vegetables, fruits, fish, mono- and polyunsaturated fatty acids (PUFA), has significant anti-inflammatory properties and confers multiple cardiometabolic benefits in patients with DM. Omega-3 PUFA, polyphenols, flavonoids, and vitamin D have been all shown to reduce inflammation and improve immune response in respiratory infections. A Mediterranean-style diet rich in these anti-inflammatory components has been hypothesized to blunt the severity of COVID-19 in people with DM [7]. Investigation into the immunomodulatory role of vitamin D has suggested that serum 25-hydroxyvitamin D levels >30 ng/ml are associated with lower rates of in-hospital mortality and mechanical ventilation in COVID-19 [8]. Given the high prevalence of vitamin D deficiency, especially in socioeconomically deprived populations, further study into the role of vitamin D is warranted. Exercise training improves a variety of physiological processes including cardiovascular function, insulin sensitivity, skeletal muscle mass and immune function, and is a cornerstone in the treatment of DM and metabolic diseases. However, mandatory restrictions on fitness facilities and recommendations for individuals to shelter-in-place to reduce SARS-CoV2 exposure, have had unintended consequences promoting sedentary behaviours and physical deconditioning. Thus, home-based training modules and outdoor activities to maintain aerobic capacity and physical strength are highly recommended. For individuals recovering from COVID-19, early mobilization and exercise rehabilitation programs are vital to restore pulmonary, cardiovascular and physical function.
The optimal pharmacologic strategy to address the various components of cardiometabolic risk in the setting of COVID-19 is an area of intense debate. Regarding hypertension, current evidence suggests the continuation of ACE inhibitors/angiotensin receptor blockers unless contraindicated [4]. Further continuation of aspirin for secondary prevention of cardiovascular disease is also strongly recommended, given the higher risk of cardiovascular dysfunction during COVID-19 infection [4]. For dyslipidemia, statins with pleiotropic anti-inflammatory effects should generally be continued, as discontinuation might lead to a rebound in levels of interleukin (IL)-6 and IL–1B, which have been implicated in the so-called cytokine storm [4,6]. There may also be a role for approved anti-obesity medications such as phentermine-topiramate, naltrexone-bupropion and liraglutide. These agents may prove to be useful, especially when adherence to a healthy hypocaloric diet is limited, and when elective metabolic surgeries are commonly postponed. Thoughtful consideration should be given to the role of antidiabetic drugs in patients with COVID-19. For patients with mild infection, the usual outpatient antihyperglycemic therapy can be continued with the following precautions: A recent retrospective study has shown a beneficial effect of the prior treatment with metformin on COVID-19 mortality [9]. However, it should be discontinued in those who are severely ill with hypoxia or hemodynamic instability due to the risk of lactic acidosis. Sodium-glucose-co-transporter 2 inhibitors should be withdrawn in severe illness or diminished oral intake due to the increased risk of dehydration and euglycemic diabetic ketoacidosis. Patients taking glucagon-like peptide 1 receptor agonists (GLP1RAs) should be monitored for gastrointestinal symptoms and encouraged to maintain adequate fluid intake to avoid dehydration. Dipeptidyl peptidase-4 inhibitors (DPP4i) are generally well-tolerated and can be continued in non-critically ill patients. Sulfonylureas should be discontinued in those unable to maintain regular food intake and could predispose to hypoglycemia. Patients taking pioglitazone should be monitored for fluid retention and stopped if there is evidence of hemodynamic instability, hepatic or cardiac dysfunction. Insulin therapy requires frequent monitoring and dose adjustment to avoid hypoglycaemia and abnormal glycemic variability [4,6,10]. In the hospital setting, monitoring for new-onset diabetes, awareness of the high prevalence of severe diabetic ketoacidosis and high insulin requirements in severe infections is paramount. The early use of intravenous insulin in hospitalized patients with severe COVID-19 allows for rapid achievement of glycemic control [4,6,10].
Even as vaccine roll out occurs across the globe, COVID-19 will continue its siege for the foreseeable future. Impaired metabolic health identified by the presence of obesity, insulin resistance, DM, hypertension and dyslipidemia, indicates a proinflammatory state and represents an important determinant of COVID-19 severity. A thoughtful approach to the management of DM and other metabolic comorbidities may improve immune response, reduce inflammation and prevent metabolic decompensation during acute illness.
Role of funding source
None.
Declaration of competing interest
C.M.T.: None.
A.K. has received research support or served on advisory boards for Lilly, Sanofi, Novo Nordisk, MSD, Astra Zeneca, ELPEN Pharma, Boehringer-Ingelheim, Bausch Health, Ethicon, Galenica, and Epsilon Health.
G.M. has served as consultant of Novo Nordisk, Johnson and Johnson, Fractyl Inc., ReCor Inc.
C.K.: None.
J.R.Z.: None.
C.S.M. reports grants, personal fees, and other from AltrixBio, Coherus Biosciences, and Novo Nordisk, personal fees and non-financial support from Ansh, Aegerion, California Walnut Commission, and personal fees from Amgen, Lumos, GENFIT, Intercept, Regeneron, CardioMetabolic Health Conference and The Metabolic Institute of America.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Palaiodimos L., Kokkinidis D.G., Li W., et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108:154262. doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belanger M.J., Hill M.A., Angelidi A.M., Dalamaga M., Sowers J.R., Mantzoros C.S. Covid-19 and disparities in nutrition and obesity. N Engl J Med. 2020;383 doi: 10.1056/NEJMp2021264. [DOI] [PubMed] [Google Scholar]
- 4.Katulanda P., Dissanayake H.A., Ranathunga I., et al. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020;63:1440–1452. doi: 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bornstein S.R., Dalan R., Hopkins D., Mingrone G., Boehm B.O. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020;16:297–298. doi: 10.1038/s41574-020-0353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stefan N., Birkenfeld A.L., Schulze M.B., Ludwig D.S. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. 2020;16:341–342. doi: 10.1038/s41574-020-0364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Angelidi A.M., Kokkinos A., Katechaki E., Ros E., Mantzoros C.S. Mediterranean diet as a nutritional approach for COVID-19. Metabolism. 2021;114:154407. doi: 10.1016/j.metabol.2020.154407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angelidi A.M., Belanger M.J., Lorinsky M.K., et al. Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients. Mayo Clin Proc. 2021 doi: 10.1016/j.mayocp.2021.01.001. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crouse A.B., Grimes T., Li P., Might M., Ovalle F., Shalev A. Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol. 2021;11:600439. doi: 10.3389/fendo.2020.600439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koliaki C., Tentolouris A., Eleftheriadou I., Melidonis A., Dimitriadis G., Tentolouris N. Clinical Management of Diabetes Mellitus in the era of COVID-19: practical issues. Peculiarities and Concerns J Clin Med. 2020;9:2288. doi: 10.3390/jcm9072288. [DOI] [PMC free article] [PubMed] [Google Scholar]