Abstract
The Coronavirus (COVID-19) pandemic sparked rapid widespread adoption of telemedicine throughout specialties, including orthopaedics. A succession of factors, starting with payers, followed by provider adoption, and reciprocated by patient approval, created newly accepted telehealth practices that have moved from trial to norm in a short time span. Orthopaedic surgeons believe telehealth will endure as a permanent change to their practice beyond the COVID-19 era, however, many permanent changes must take place by payers, providers, and patients to sustain telehealth into the future. The goal of this paper is to highlight the indelibility of telemedicine adoption in orthopaedic practices globally, characterize the chain of events that led to its large-scale adoption, and catalyze discussion around actionable next steps to sustain its benefits.
Keywords: Telehealth, Telemedicine, Coronavirus, COVID-19, Orthopaedics, Orthopaedic trauma, U.S. healthcare policy, Global health, Health policy
1. Introduction
The Coronavirus COVID-19 (SARS-CoV-2) pandemic has highlighted the fragility of people, organizations, and economies alike, allowing cross-sectional leadership to reflect upon the many things that are outside of our control and the few that are within it. The very nature of this contagion changed daily operations for communications and transactions previously thought to require face-to-face interaction. In doing so, it has pushed systems and markets to adjust in ways that balanced public health stewardship with simply “getting the job done.”
Due to factors that make healthcare unique from typical economic goods or services—namely, the innate vulnerability of the patient due to health being a largely inelastic demand, and the influence of third-party insurers governing the reimbursement framework—medical providers are held to a different and higher standard when delivering services to their patients. For this reason and others, HIPAA was enacted to protect patient data and privacy rights while provider’s ability to choose what services they bill for were largely taken over by insurance companies. In the midst of COVID-19, however, the U.S. Department of Health and Human Services (HHS) broadened telehealth indications to allow doctors to provide more services, and insurers followed suit by reimbursing those services. The emerging literature highlights that providers and patients have embraced this interim telehealth framework and benefited immensely from its capabilities.1 Orthopaedic practices have also followed this paradigm shift, citing the COVID-19 pandemic as the impetus for implementing telehealth services.1
It remains to be seen, however, whether payers, namely CMS and private insurers, will recognize the value of telehealth demonstrated during the pandemic, in the post-COVID-19 era. It is also yet to be seen whether the other stakeholders in this conversation, specifically the providers and patients, health systems and practice types, have taken to telemedicine out of temporal necessity or longer-term survival. In this paper, we seek to stimulate conversation around the question of whether newly experienced models of care during the COVID-19-induced telehealth era will survive into the post-pandemic period. Our team has summarized some of the existing literature on telemedicine in orthopaedics and linked it to the results of our Global Orthopaedic Trauma Survey describing the effects of COVID-19 on global practices.2 We seek to provide more information to orthopaedic leaders and change agents who, as professionals representing their specialty, may help redefine policies and care models that serve the best interests of payers, providers, and patients.
2. The orthopaedic payer: telehealth background
At its basic level, telehealth is used to improve access to care. It was born out of the recognition that technology could be harnessed to improve healthcare access for patients through vital services such as videoconferences, remote electronic consults and wireless communications. Though little data exists on the scope of telehealth’s global adoption, market outlooks demonstrate continuous growth due in large part to the cumulative rise of emerging economies.3
In the U.S., the percentage of hospitals using some telehealth application grew from 35% to 75% over the last decade. However, telehealth adoption has been stunted by lack of uniform coverage, overwhelming complexity, and ever-changing policies on behalf of the three largest payers – private insurance, Medicare and Medicaid. Much of the hesitancy to cover telehealth is born out of measures meant to protect patient data and privacy.4 Furthermore, its use in orthopaedics and particularly the orthopaedic trauma subspecialty has been sparse. Fair Information Practice Principles (FIPPs) are the internationally accepted policies protecting the collection, use, and disclosure of sensitive patient information. In the U.S., laws under HIPAA are designed to enforce these principles. However, HIPAA’s protective measures and the potential legal consequence of violation, have stifled user adoption of telemedicine for patients and providers alike.
Despite regulatory and coverage barriers, telehealth has shown to be cost effective.5 It could provide a partial solution for out-of-control healthcare spending that has come to be characterized in the U.S. as a non-sustainable cost albatross.6 Furthermore, the implementation of telemedicine has been shown to improve treatment outcomes and quality of care in several clinical environments including fields such as intensive care. These types of outcomes may be translatable to orthopaedics with more widespread adoption of its use.
3. The orthopaedic provider: telehealth background
In orthopaedics, the most utilized telehealth applications include patient examinations, interpretation of imaging, postoperative care provision, diagnosis, and patient-reported outcomes follow-up.7 Telehealth consults in orthopaedics are cost-effective, requiring less hands-on care from facility resource use, and allowing an avenue to deliver patient care to provide broader coverage for patients who do not have close access to orthopaedic clinics.8 Randomized controlled trials comparing video consultations with standard orthopaedic visits have demonstrated effective care in evaluating new referrals to outpatient clinics, postoperative patients, and patients undergoing follow-up for traumatic and chronic morbidities.9,10 Systematic reviews have demonstrated efficacious uses of telemedicine-based rehabilitation for trauma fracture management and total hip and knee arthroplasty.9,10 Furthermore, Tanaka et al. recently published protocols and methods aimed at standardizing virtual orthopaedic examination categorized by indications for knee, hip, shoulder, and elbow.11 Although not yet widely adopted by orthopaedic surgeons globally, future research may allow for the validation and standardization of modified orthopaedic physical examination techniques and technologies allowing for more widespread use.
Furthermore, there have been examples of orchestrated telehealth alliances amongst orthopaedic providers. Arkansas, a state characterized by low population density and care distribution, has spearheaded a partnership between University of Arkansas for Medical Sciences (UAMS) and the Arkansas Trauma Communications Center (ATCC) aimed at decreasing transfer rates for orthopaedic hand trauma patients.12 This has allowed patients to be treated closer to home while having telehealth access to fellowship-trained hand surgeons.
Not only will the adoption of telehealth benefit orthopaedic patients, but it will also help optimize schedules of orthopaedic surgeons, who as a whole, represent a specialty with high burnout rates, which is partially exacerbated by clinical load. Orthopaedic surgeons must understand their needs in providing valuable clinical functions and utilize their voices as primary revenue drivers to influence governance to make decisions that are in the best interest of clinical care.
4. The orthopaedic patient: telehealth background
Patients who have utilized telehealth services have shown high satisfaction rates.13 In fact, when comparing patient satisfaction scores with the same rating systems for other areas of healthcare and insurance, telehealth satisfaction scores are amongst the highest.13 Surveys in the U.S. found that 84% of patients are more likely to select a provider who offers telemedicine over one who does not.13 However, studies also indicate that due to past barriers associated with telehealth coverage, only 9.6% of Americans have used telehealth services. This paradox indicates that medical professionals must first introduce telehealth to their patients in order for their patients to demand it.
Orthopaedic patients have reported positive telehealth satisfaction scores as well, particularly in cases where they live far from the provider.9,10 This supports the aforementioned notion that telemedicine may be used as a means to improve discrepancies in healthcare access for patients living in rural settings. Ironically, fewer patients in rural areas have used telehealth, with 72% of patients in rural areas reporting that they are not aware of telehealth provision. It is likely that if introduced to telehealth as an option, patients living in remote areas would be the ideal beneficiaries of telehealth services. Based on numerous reports from organizations conducting follow-up care in low-and middle-income countries (LMICs) where opportunity costs associated with travel and time away from work are burdensome, it is possible that telehealth could be leveraged as a means to overcoming barriers in impoverished geographies.14,15
5. The COVID-19 impact: trickle-down telenomics
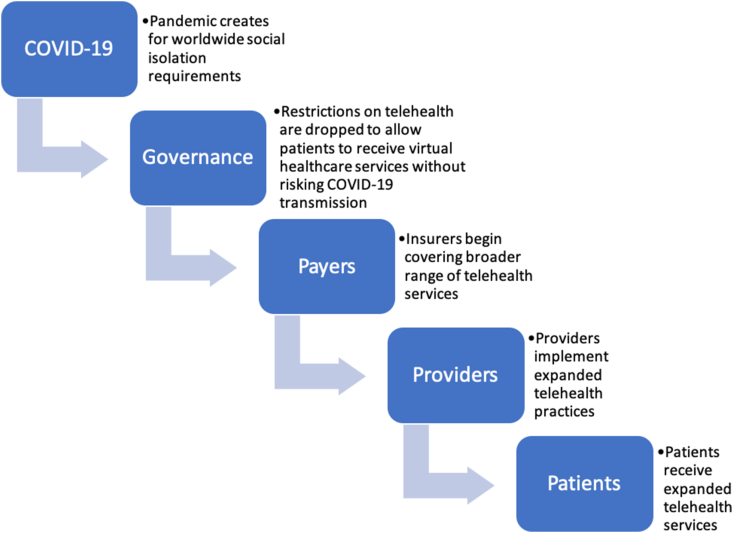
There are certain events throughout history that have fundamentally changed the way people, systems, and industries operate. For example, 9/11 transformed aviation security policies by permanently shifting societal attitudes about the trade-off between privacy and security. The SARS outbreak skyrocketed consumer acceptance of online retail in ways the world had never seen, by instilling a fear in the Chinese about leaving their homes.16 Likewise, the COVID-19 pandemic has forced medical providers to treat their patients virtually to protect each other from viral spread. The immediate explosion of telehealth was only made possible by governance shifting its stance on the cost-benefit between data safety and patient safety and making restrictions more lenient; by healthcare insurers reworking policies to cover telehealth services; by providers pivoting to previously untapped methodologies of virtual medical care; and by patients receiving telehealth consults. In the midst of a pandemic, all parties embraced telemedicine because it was absolutely necessary, but now what? (Fig. 1).
Fig. 1.
This visual depicts the trickle-down effect of COVID-19 on telehealth adoption which impacted behaviors starting with medical governance and ending with patients.
6. The orthopaedic payer: what must Be done?
After HHS declared a public health emergency, the Centers for Medicare & Medicaid Services (CMS) released guidance allowing Medicare to pay for telehealth services, and more recently released a “toolkit” helping States implement telehealth into their Medicaid programs. Meanwhile, HHS removed penalties for HIPAA noncompliance in connection with good-faith telehealth provisions.17 U.S. data supports our findings that telehealth utilization has increased under newly amended telehealth reimbursement frameworks and flexibilities.
Now, health insurers must look ahead at the value in maintaining telehealth offerings into the future. It is plausible that broadened telehealth coverage is an inevitability, and early adopters will win market share in the significant opportunity that lies in expanded patient access and feasibility. However, little has been reported as to whether HHS will re-heighten regulation after the immediate crisis, which could cause a chain of events leading to insurers rescinding telehealth coverage.
Answers likely lie in value-based healthcare demonstration. HHS recently awarded $150 million to support telehealth expansion in rural hospitals, and another $11.5 million to the Telehealth Resource Centers (TRCs) dedicated to providing telehealth expertise and technical assistance, while acting as a clearinghouse for telehealth research.17 If telehealth models reduce overhead while expanding diagnoses and treatments, policymakers must expeditiously design frameworks for a post-COVID-19 healthcare. Clinical and insurance data must be evaluated to tier treatments based upon value optimization, and resources have already been devoted towards promoting best practices and combating fraud.
7. The orthopaedic provider: what must Be done?
Those on the front lines during COVID-19, such as the ones polled in this study,2 experienced a mechanism of clinical care that benefited their patients and practices immensely. Since the onset of the pandemic, there have been multiple contributions to the literature on how to best utilize telehealth in orthopaedics.11,18, 19, 20, 21, 22, 23, 24 Now, orthopaedists must recognize telehealth for what it could offer their patients in the future: mitigating access disparities, avoiding crowded waiting rooms, reducing time away from work, increasing healthcare satisfaction, and reducing costs.
More research is needed to understand which telehealth methodologies yield positive patient outcomes and where limitations may exist. Such limitations may include increased likelihood of misdiagnosis, variability amongst patients in technological literacy and virtual access, inability to replicate complete in-person physical exam inclusive of accurate outcomes assessments such as range of motion, potential difficulties in identifying cases of domestic violence and child abuse, and everchanging legislative implications for telehealth use. Orthopaedic providers must study these potential limitations while continuing to drive telehealth solutions and push the systems that govern policies affecting them. In doing so, and in advocating for our patients, those orthopaedists who are earlier adopters of telehealth diffusion will benefit to the likes of those in our sampling.25
8. The orthopaedic patient: what must Be done?
As more people come to value telehealth, it is likely that more insurance purchasers will demand telehealth coverage in their plans. COVID-19 created a concomitance of factors that exposed more patients to telehealth, and it has been well documented that patients will embrace telehealth services.13 If offered correctly, patients stand to gain the most from telehealth – whether patients living rural areas, geriatric patients with chronic conditions, or younger generation patients savvy in shopping around for on-demand services, the time is now for patients to be beneficiaries of the services that telehealth has to offer.
9. Conclusion
Emerging literature supports three high level but important conclusions: Orthopaedic surgeons globally have implemented telemedicine in the wake of COVID-19; Orthopaedic surgeons globally believe telemedicine will be a permanent change to their practice; Orthopaedic surgeons globally who implemented telemedicine practices in the wake of COVID-19 are more likely to embrace it in the future.2 As these findings are disseminated, more rigor must be applied to studies which go vertical into telehealth adoption across orthopaedics. What we know at the basic level is that telemedicine will continue to proliferate, and COVID-19 was an accelerant. The question remains, how will these newly adopted behaviors change for the long term? The answer may lie in what actions are taken for each stakeholder – the payer, the provider, and the patient. Orthopaedic surgeons must take responsibility to lead in the wake of the COVID-19, as it has shed light on the possibilities of telemedicine for those in the U.S. and throughout the world.
References
- 1.Parisien R.L., Shin M., Constant M. Telehealth utilization in response to the novel Coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28(11):e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lezak B.A., Cole P.A., Schroder L.K., Cole P.A. Global experience of orthopaedic trauma surgeons facing COVID-19: a survey highlighting the global orthopaedic response. Int Orthop. 2020;13 doi: 10.1007/s00264-020-04644-4. Published online June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fact sheet: telehealth | AHA. https://www.aha.org/factsheet/telehealth Accessed July 2, 2020.
- 4.Hall J.L., McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff. 2014;33(2):216–221. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 5.Buvik A., Bergmo T.S., Bugge E., Smaabrekke A., Wilsgaard T., Olsen J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2) doi: 10.2196/11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NHE fact sheet | CMS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet Accessed July 2, 2020.
- 7.Wongworawat M.D., Capistrant G., Stephenson J.M. The opportunity awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Joint Surg. 2017;99(17):e93. doi: 10.2106/JBJS.16.01095. [DOI] [PubMed] [Google Scholar]
- 8.Prada C., Izquierdo N., Traipe R., Figueroa C. Results of a new telemedicine strategy in traumatology and orthopedics. Telemed J e Health. 2020;26(5):665–670. doi: 10.1089/tmj.2019.0090. [DOI] [PubMed] [Google Scholar]
- 9.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25(8):451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 10.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomized controlled trial. BMC Health Serv Res. 2016 Sep 8;16(1):483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanaka M.J., Oh L.S., Martin S.D., Berkson E.M. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102(12):e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hand trauma communication center available 24/7 - UAMS news. https://news.uams.edu/https://news.uams.edu/2018/06/06/hand-trauma-communication-center-available-24-7/ Published June 6, 2018. Accessed July 2, 2020.
- 13.U.S. Telehealth Satisfaction Study J.D. Power. https://www.jdpower.com/business/healthcare/us-telehealth-satisfaction-study Accessed July 2, 2020.
- 14.Torchia M.T., Schroder L.K., Hill B.W., Cole P.A. A patient follow-up program for short-term surgical mission trips to a developing country. J Bone Joint Surg. 2016;98(3):226–232. doi: 10.2106/JBJS.O.00087. [DOI] [PubMed] [Google Scholar]
- 15.O’Hara N.N., Mugarura R., Potter J. The socioeconomic implications of isolated tibial and femoral fractures from road traffic injuries in Uganda. J Bone Joint Surg Am. 2018;100(7):e43. doi: 10.2106/JBJS.17.00439. [DOI] [PubMed] [Google Scholar]
- 16.Reeves M., Carlsson-Szlezak P., Whitaker K., Abraham M. Sensing and shaping the post-COVID era. 2020. https://bcghendersoninstitute.com/sensing-and-shaping-the-post-covid-era-c282cd227a4f Published 292 2020. Accessed July 2.
- 17.Deregulation Sparks Dramatic Telehealth Increase During the COVID-19 Response . The United States Government; 2020. The White House. Accessed April 28. [Google Scholar]
- 18.Loeb A.E., Rao S.S., Ficke J.R., Morris C.D., Riley L.H., Levin A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rao S.S., Loeb A.E., Amin R.M., Golladay G.J., Levin A.S., Thakkar S.C. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020 doi: 10.1016/j.artd.2020.04.014. Published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mo A.Z., Mont M.A., Grossman E.L. The effect of the COVID-19 pandemic on orthopedic practices in New York. Orthopedics. 2020 Jul 1;43(4):245. doi: 10.3928/01477447-20200624-01. PMID: 32674175. [DOI] [PubMed] [Google Scholar]
- 21.Earp B.E., Zhang D., Benavent K.A., Byrne L., Blazar P.E. The early effect of COVID-19 restrictions on an academic orthopedic surgery department. Orthopedics. 2020 Jul 1;43(4):228–232. doi: 10.3928/01477447-20200624-03. PMID: 32674173. [DOI] [PubMed] [Google Scholar]
- 22.Lockey S.D., Postma W.F. Patient Advocacy during COVID-19. Orthopedics. 2020 Jul 1;43(4):203. doi: 10.3928/01477447-20200604-02. PMID: 32674172. [DOI] [PubMed] [Google Scholar]
- 23.Parnes N., Tousant C., Perrine J., DeFranco M.J. Outpatient orthopedic rehabilitation in New York state during the COVID-19 pandemic: therapist perspectives. Orthopedics. 2020 Sep 1;43(5):292–294. doi: 10.3928/01477447-20200721-16. Epub 2020 Aug 6. PMID: 32745217. [DOI] [PubMed] [Google Scholar]
- 24.Halim A., Grauer J.N. Orthopedics in the era of COVID-19. Orthopedics. 2020 May 1;43(3):138–139. doi: 10.3928/01477447-20200426-01. PMID: 32421197. [DOI] [PubMed] [Google Scholar]
- 25.Moisan P., Barimani B., Antoniou J. Orthopedic surgery and telemedicine in times of COVID-19 and beyond: a review. Curr Rev Musculoskelet Med. 2021 doi: 10.1007/s12178-021-09693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]