Highlights
-
•
Physical activity potentially has a buffering effect against COVID-19 related outcomes.
-
•
Analysis of data at the county level in the United States.
-
•
Physical activity associated with decreased COVID-19 cases and deaths.
-
•
Relationship between COVID-19 cases and deaths lower when physical activity is high.
Keywords: Coronavirus disease 2019, Deaths, PA
Abstract
Purpose
The study was to examine county-level associations of physical activity with coronavirus disease 2019 (COVID-19) cases and deaths, per 100,000 county residents.
Methods
Data were collected from publicly available data sources for 3142 counties and equivalents, including the District of Columbia. Subjective health ratings, percentage uninsured, percentage unemployed, median household income, percentage female residents, percentage White residents, percentage of residents 65 years of age or older, and rural designation served as controls.
Results
The two-level random intercept regression showed that physical activity rates at the county level were statistically and negatively associated with COVID-19 cases and deaths. Additional analyses showed that physical activity rates moderated the relationship between cases and deaths, such that the relationship was strongest when physical activity rates were low.
Conclusion
The results presented here offer empirical evidence of the benefits of county-level physical activity during a pandemic. Implications for public health and physical activity provision are discussed.
Graphical Abstract
1. Introduction
Given the physical, social, psychological, and economic tolls of the coronavirus disease 2019 (COVID-19) pandemic,1, 2, 3, 4, 5 scientists around the world have staunchly pursued an understanding of factors contributing to virus-related morbidity, hospitalizations, and mortality. Personal characteristics, including age, gender, and race, as well as comorbidities, including diabetes, obesity, respiratory illnesses, and hypertension, are salient predictors.6,7 These effects noted, health behaviors and outcomes are not just a function of the individual but, instead, are also shaped by environmental determinants.8,9 Consistent with this perspective, social and community factors that contribute to COVID-19 cases and deaths include public health ordinances,10 structural inequalities,11 collective racial biases,12 and socioeconomic disparities,13 among others.
Missing from the examination of social and environmental factors potentially related to COVID-19 cases and deaths is a focus on physical activity (PA) among community members. Systematic reviews show that most of the scholarship in this area has focused on PA during the pandemic among individuals.14 For example, people around the world were more likely to lead sedentary lives, especially during lockdowns; and these findings were prevalent among countries hit hardest by the pandemic.15, 16, 17 PA decreases were linked with corresponding reductions in psychological well-being18 and subjective health.15 Such inactivity has the potential to have lasting negative effects on people's physical health.19 As a result, sport managers and public health officials have identified creative solutions for being active at home or in otherwise physically distanced settings.20
Though examination of individual PA during the pandemic is important, a sole focus on that level of analysis necessarily ignores the impact of community norms and behaviors.21 This is an important distinction because community-level PA is associated with better health and lower obesity rates among members of a community as a whole.22, 23, 24 These findings are consistent with related research showing that PA can help reduce the incidence of many COVID-19 risk factors, including obesity, hypertension, heart disease, and respiratory illnesses.25,26 Recognizing this possibility, Simpson and Katsanis25 noted, “the available scientific evidence from other viral infections would indicate that physically active people will have less severe symptoms, shorter recovery time, and may be less likely to infect others they come into contact with.”25
Applied to the aggregate level, these suppositions25 suggest that communities with higher levels of PA might also see fewer COVID-19 cases and deaths. The purpose of this study was to examine these possibilities through an analysis of county-level data in the US. Specifically, it was hypothesized that county-level PA rates would be negatively related to COVID-19 cases (Hypothesis 1) and COVID-19 deaths (Hypothesis 2).
2. Methods
2.1. Data sources and variables
Data were collected for counties and county-equivalents (boroughs, parishes, and the District of Columbia; n = 3142) in the US. A county, or equivalent, represents a major administrative unit within a given state,27 and there are 3243 such units in U.S. states and territories. The current analysis focused only on counties in U.S. states, and all 50 states were represented. All data were gathered from publicly available sources, as outlined in the following sections. The study met the research guidelines of Texas A&M University.
2.1.1. COVID-19 cases and deaths
Data related to COVID-19 cases and deaths were gathered from the USAFacts Website: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/. The website's data are used by a variety of agencies and organizations, including the Centers for Disease Control and Prevention and Google, and other researchers examining predictors of COVID-19 cases and deaths have also used this database.28,29 The site offers details on the data collection process (https://usafacts.org/articles/detailed-methodology-covid-19-data/), which involves collecting daily data from state and county websites and dashboards. The data are collected through scraping or manual entry. Used in this study were the cumulative COVID-19 cases and deaths, respectively, from January 20, 2020 to November 30, 2020 (a period of 314 days). Each count was then converted to reflect the number of cases (Cases) or deaths (Deaths) per 100,000 county residents.
2.1.2. PA
PA data were gathered from the 2020 County Health Rankings and Roadmaps (https://www.countyhealthrankings.org), a Robert Wood Johnson Foundation-supported initiative that provides health data for all U.S. counties. Drawing from the Behavioral Risk Factor Surveillance Survey, the site provides the percentage of people age 20 or older who reported no PA in the previous month. The specific item reads: “During the past month, other than your regular job, did you participate in any PAs or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”30 For this study, that measure was reverse scored and labeled Percent Active to represent the percentage who had any level of activity. As discussed in more detail in the limitations section, this measure represents the lowest possible threshold of PA and should not be interpreted as meeting activity guidelines.
2.1.3. Controls
A number of controls were also included, all of which either impact residents’ health in general or are related to COVID-19 prevalence. These data were collected from the aforementioned County Health Rankings and Roadmaps website. A number of comorbidities are associated with COVID-19 risks and mortality,31 so subjective health ratings (Poor or Fair Health) served as the first control. Others have also used this measure when examining residents’ health.32,33 The lack of insurance is also linked with COVID-19 risks,34 so Uninsured served as a control. Relatedly, economic instability is a health risk factor,35 so the percentage of unemployed county residents (Unemployed) and the natural log of the median household Income (log income) served as controls. Finally, a host of personal demographics are related to health outcomes and COVID-19 risk and mortality.12,36,37 Thus, the percentage of residents who were female (Female residents), White (White residents), and age 65 or older (65 or older), as well as the rural designation of the county (Rural) all served as controls.
2.2. Empirical strategy
Means, SDs, and bivariate correlations were computed for all variables. As counties are nested within states, the observations are not independent. That is, even though counties are independent administrative units, state policies and characteristics might influence health behaviors and outcomes at the county level.38 Multilevel modeling is appropriate in such instances.21,39 Other options, such as ordinary least squares regression, result in a misestimation of SEs and inflated Type I error.40 Therefore, two-level random effect regression models using SPSS (Version 27.0; IBM Corp., Armonk, NY, USA) were used to test the hypotheses. Restricted maximum likelihood estimation was used to estimate the models.41,42 The state level (as represented by the Federal Information Processing Standard code) was specified as a random effect, and all other variables were specified as fixed effects. Finally, in presenting the results, the intraclass correlation is included, as well as Akaike's information criterion and Schwarz's Bayesian criterion.
3. Results
3.1. Descriptive statistics
Descriptive statistics are shown in Table 1. Results indicate that counties had, on average, 4577.97 ± 2410.86 Cases per 100,000 residents and 78.54 ± 71.46 Deaths per 100,000 residents through the end of November 2020. Many of the county residents reported being physically active: 72.63% ± 5.70%. Finally, county-level PA held a significant, negative bivariate correlation with both Cases (r = –0.14) and Deaths (r = –0.23).
Table 1.
Means, SDs, and bivariate correlations.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Fair or poor health | — | ||||||||||
| 2. Uninsured | 0.41 | — | |||||||||
| 3. Log income | –0.72 | –0.34 | — | ||||||||
| 4. Unemployed | 0.50 | 0.03 | –0.44 | — | |||||||
| 5. Female residents | 0.03 | –0.10 | 0.02 | –0.01 | — | ||||||
| 6. White residents | –0.53 | –0.47 | 0.17 | –0.29 | 0.03 | — | |||||
| 7. 65 years or older | –0.16 | –0.02 | –0.26 | 0.03 | 0.08 | 0.39 | — | ||||
| 8. Rural | 0.08 | 0.18 | –0.39 | 0.07 | –0.19 | 0.31 | 0.48 | — | |||
| 9. Physical activity | –0.54 | –0.23 | 0.57 | –0.22 | –0.04 | 0.04 | –0.09 | –0.31 | — | ||
| 10. Cases | 0.09 | 0.06 | –0.14 | –0.15 | –0.17 | –0.08 | –0.17 | 0.02 | –0.14 | — | |
| 11. Deaths | 0.29 | 0.21 | –0.27 | 0.10 | 0.04 | –0.30 | –0.03 | 0.03 | –0.23 | 0.45 | — |
| Mean ± SD (%) | 17.94 ± 4.74 | 11.48 ± 5.14 | 10.85 ± 0.24 | 4.13 ± 1.50 | 49.89 ± 2.28 | 75.99 ± 20.19 | 19.27 ± 4.71 | 58.58 ± 31.48 | 72.63 ± 5.70 | 4577.97 ± 2410.86a | 78.54 ± 71.46a |
Notes: Cases represents coronavirus disease 2019 (COVID-19) cases/100,000 country residents. Deaths represents COVID-19 deaths/100,000 county residents.
a Data were cases or deaths, not percentage.
3.2. Hypothesis testing
Results of the two-level random intercept regression models are shown in Table 2. Focusing on Cases, the unconditional means model demonstrated both county-level (Level 1) and state-level (Level 2) differences in the intercepts, suggesting that the cumulative COVID-19 cases per 100,000 residents varied based on the state and the counties within a state. The intraclass correlation (ρ = 0.54) illustrates the appropriateness of including the state in the model as a random second-level variable.
Table 2.
Results of two-level random intercept models with county-level physical activity predicting COVID-19 cases and deaths.
| Variable | COVID-19 cases/100,000 county residents |
COVID-19 deaths/100,000 county residents |
||
|---|---|---|---|---|
| Unconditional model | Full model | Unconditional model | Full model | |
| Fixed effects | ||||
| Intercept | 4129.50⁎⁎⁎ (272.57) | 25,501.40⁎⁎⁎ (3150.40) | 73.09⁎⁎⁎ (5.83) | 694.49⁎⁎⁎ (117.79) |
| Physical activity | –21.95⁎⁎ (7.11) | –0.72⁎⁎ (0.27) | ||
| Covariates | ||||
| Fair or poor health | 66.99⁎⁎⁎ (18.89) | 0.63 (0.70) | ||
| Uninsured | 43.62⁎⁎ (12.99) | –0.48 (0.48) | ||
| Log income | –1031.13⁎⁎⁎ (252.68) | –49.56⁎⁎⁎ (9.53) | ||
| Unemployed | –138.80⁎⁎⁎ (31.07) | –2.82* (1.16) | ||
| Female residents | –162.88⁎⁎⁎ (13.67) | 0.88 (0.52) | ||
| White residents | –15.88⁎⁎⁎ (3.14) | –1.17⁎⁎⁎ (0.12) | ||
| 65 years or older | –67.28⁎⁎⁎ (8.82) | 1.01⁎⁎ (0.33) | ||
| Rural | –8.96⁎⁎⁎ (1.31) | 0.04 (0.05) | ||
| Variance components | ||||
| Level 1 – county-level (σ2) | 3,067,854.24⁎⁎⁎ (78,031.88) | 2,372,859.54⁎⁎⁎ (60,521.04) | 3900.76⁎⁎⁎ (99.22) | 3449.66⁎⁎⁎ (88.01) |
| Level 2 – state-level (τ00) | 3,641,814.78⁎⁎⁎ (754,865.80) | 3,565,919.16⁎⁎⁎ (735,672.31) | 1575.82⁎⁎⁎ (344.84) | 1339.17⁎⁎⁎ (302.39) |
| AIC | 56,037.84 | 55,033.77 | 35,044.45 | 34,559.44 |
| BIC | 56,049.94 | 55,045.86 | 35,056.56 | 34,571.54 |
Notes: The values show mixed effects regression coefficients and their standard errors (SEs). SEs are presented in parentheses.
Abbreviations: AIC = Akaike's information criterion; BIC = Schwarz's Bayesian criterion; COVID-19 = coronavirus disease 2019.
p < 0.05,
p < 0.01,
p < 0.001.
Many of the controls had significant effects. Counties with a high proportion of people in fair or poor health, with many uninsured residents, with lower household incomes, with more men, with more racial minorities, and in urban settings saw more cases per 100,000 residents. In terms of hypothesis testing, results of the full model show that PA held a significant, negative association with Cases (estimate = –21.95, SE = 7.11, p < 0.01); thus, Hypothesis 1 was supported.
Table 2 also provides the results for Deaths. The unconditional means model is examined first, with results showing both county-level and state-level differences in intercepts. That is, COVID-19 deaths per 100,000 county residents varied based on the state and the counties within the states. The intraclass correlation (ρ = 0.28) demonstrates that the state should be included as a random second-level variable in the model.
Many of the covariates were significantly related to Deaths. Counties where residents had lower household incomes, were employed, were racial minority, and age 65 or older were all related to increased COVID-19 deaths. Further, results of the full model support Hypothesis 2: after taking into account the controls and state-level effects, PA held a significant, negative association with Deaths (estimate = –0.72, SE = 0.27, p < 0.01).
3.3. Supplemental analysis
Table 1 shows that the relationship between Cases and Deaths is moderate to high (r = 0.45), suggesting that other factors might influence this relationship. Physical activity levels of county residents are one such factor. In this case, PA would serve as a moderator, or a variable that potentially affects the relationship between an independent and dependent variable.43 To examine this possibility, another two-level random intercept regression was computed. Both Cases and PA were standardized to reduce the effects of multicollinearity,44 and the Cases × PA product term was then computed. As with the other analyses, restricted maximum likelihood estimation was used to estimate the models, and the state level was specified as a random effect. The controls, standardized Cases and PA variables, and the Cases × PA product term were all included as fixed effects.
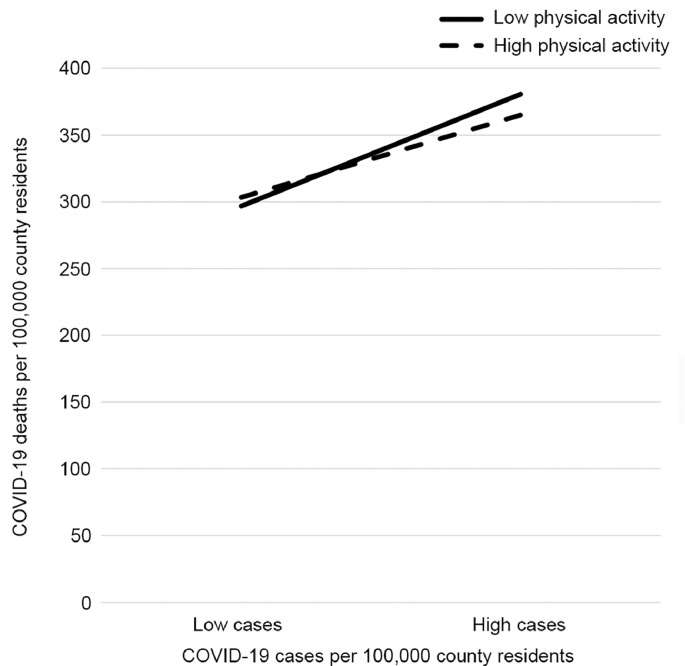
As shown in Table 3, results indicate that Cases held a significant, positive relationship with Deaths (estimate = 36.37, SE = 1.46, p < 0.001). The main effects of PA were not significant in this model (estimate = –2.26, SE = 1.40). However, these effects were qualified by a significant Cases × PA interaction (estimate = –5.50, SE = 1.12, p < 0.001). Simple slopes analysis was then computed,44 and an illustrative summary of the interaction is available in Fig. 1. The relationship between Cases and Deaths was stronger when PA was low (estimate = 23.29, SE = 1.79, p < 0.001) than when it was high (estimate = 30.87, SE = 1.88, p < 0.001).
Table 3.
Results of two-level random intercept models examining the moderating effects of county-level physical activity PA and COVID-19 cases on COVID-19 deaths.
| Variable | Unconditional model | Full model |
|---|---|---|
| Fixed effects | ||
| Intercept | 73.09⁎⁎⁎ (5.83) | 336.47⁎⁎ (108.71) |
| Cases | 36.37⁎⁎⁎ (1.46) | |
| PA | –2.26 (1.40) | |
| Cases × PA | –5.50⁎⁎⁎ (1.12) | |
| Covariates | ||
| Fair or poor health | –0.37 (0.63) | |
| Uninsured | –1.09* (0.43) | |
| Log income | –35.41⁎⁎⁎ (8.73) | |
| Unemployed | –0.31 (1.06) | |
| Female residents | 3.38⁎⁎⁎ (0.48) | |
| White residents | –0.91⁎⁎⁎ (0.11) | |
| 65 or older | 1.95⁎⁎⁎ (0.31) | |
| Rural | 0.15⁎⁎ (0.05) | |
| Variance components | ||
| Level 1 – county-level (σ2) | 3900.76⁎⁎⁎ (99.22) | 2863.53⁎⁎⁎ (73.09) |
| Level 2 – state-level (τ00) | 1575.82⁎⁎⁎ (344.84) | 832.63⁎⁎⁎ (193.86) |
| AIC | 35,044.45 | 33,954.72 |
| BIC | 35,056.56 | 33,966.82 |
Notes: The values show mixed effects regression coefficients and their standard errors (SEs). SEs are presented in parentheses.
Abbreviations: AIC = Akaike's information criterion; BIC = Schwarz's Bayesian criterion; COVID-19 = coronavirus disease 2019; PA = physical activity.
p < 0.05, ** p < 0.01, *** p < 0.001.
Fig 1.
Moderating effects of county-level physical activity and COVID-19 cases on COVID-19 deaths. COVID-19 = coronavirus disease 2019.
4. Discussion
Health behaviors and outcomes are a function of factors at multiple levels, including intrapersonal and interpersonal processes, institutional factors, community factors, and societal laws and statutes.9 With respect to COVID-19, most of the scholarship has focused on intrapersonal factors,1, 2, 3, 4, 5 but there is evidence that community and public policy factors can and do influence the incidence of COVID-19 cases and deaths.11, 12, 13,45 Nevertheless, scholars have yet to examine the association of PA with COVID-19 cases and deaths. Even though PA among community members is related to better health outcomes for the community as a whole22, 23, 24 and can reduce many of the comorbidities associated with COVID-19 risk,25,26 examination of PA’s relationship with COVID-19 cases and deaths is missing. The purpose of this study was to rectify that gap. Consistent with the 2 study hypotheses, PA at the county level was negatively associated with both COVID-19 cases and deaths per 100,000 county residents. Additional analyses showed that PA moderated the relationship between COVID-19 cases and deaths, such that the relationship was stronger when county-level PA was low. The latter findings suggest PA can have protective effects.
The patterns identified in this study likely manifest from several factors. First, researchers have demonstrated how PA is linked with improved immune markers in several diseases related to COVID-19, including cardiovascular disease, diabetes, and obesity.46, 47, 48 From this perspective, PA among community members might buffer them against disease. This was demonstrated in the current study, as county-level PA was negatively associated with COVID-19 cases. Importantly, the immune-related benefits of PA might protect county residents against serious illnesses and negative health outcomes associated with COVID-19. Simpson and Katsanis25 argued as much, noting the possibility that physically active people have “less severe symptoms, shorter recovery times, and may be less likely to infect others they come into contact with”.25 The results of this study offer empirical evidence for their argument: the relationship between cases and deaths decreased when PA levels were high.
From a different, more macro perspective, high county-wide PA levels might signal a culture of health and fitness concern. As a result of this culture of health and fitness, the county is likely to invest in parks, recreational facilities, and a built environment that encouragers active living.49,50 The county residents, in addition to being physically active, might also take other steps to promote their health and well-being.51 One outcome of a health and fitness culture particularly germane to this study is wearing a mask during the pandemic. Researchers have shown that masks can be an effective tool in combatting the spread of COVID-19;45,52 nonetheless, it remains a politicized issue that is shaped, in part, by where one lives.53 As such, it is possible that people living in counties where health and fitness are part of the culture or way of life might also be more willing to wear a mask.
This possibility was examined by drawing from the New York Times county-level dataset related to mask-wearinga and merging it with the current dataset. The Times provides county-level estimates of the percentage of county residents who never, rarely, sometimes, frequently, or always wear a mask when they are outside and within 6 feet of another person. Analysis of these data show that the percentage of county residents who always wore a mask was positively related to the percentage who are physically active—a pattern that is supportive of the culture of health and fitness hypothesis. Even more encouraging, the percentage of people who always wore a mask was negatively associated with COVID-19 cases and deaths per 100,000 residents.
The preceding discussion should also be couched within a discussion of intersectionality and existing inequalities.54 Counties with the highest percentage of residents who were at least minimally active also had higher incomes and lower unemployment rates (Table 1). In this way, some counties might have more opportunities to develop a culture of health and well-being than do others. This discussion also points to just one of the many ways in which the COVID-19 pandemic has exacerbated existing inequalities and health disparities.55,56
The results presented here offer empirical evidence of the benefits of county-level PA during a pandemic. Fortunately, with several vaccines developed and being administered as of December 2020, there appears to be a light at the end of the COVID-19 pandemic tunnel. However, other pandemics can and will occur. For their part, communities can engage in a number of steps to promote PA and related health benefits. Hood and colleagues51 offer a potential framework, showing how the physical environment, social and economic factors, clinical care, and health behaviors all combine to influence a host of health outcomes, including quality of life and mortality. Hood et al.’s51 work (a) demonstrates the importance of considering factors at multiple levels of analysis—consistent with a social ecological approach; and (b) identifies specific levers that public health officials can utilize in seeking to improve health.
In addition, public health experts can promote PA during the pandemic. Certainly, physical distancing requirements and lockdowns curtail many activities, but other options exist. Examples include exercising more at home, using home fitness machines, walking and running outdoors in open spaces, and practicing yoga in open spaces such as parks, among other options.20,57
Although the study makes several contributions, there are potential limitations. First, the study is cross-sectional, so results are discussed in terms of associations instead of causation. Second, the PA data measured the percentage of county residents who were physically active. However, the measure does not capture the amount or type of PA and, thus, represents the lowest threshold of activity. The data likely capture some people who were minimally active but not at levels that could provide health benefits. If this is the case, then the results underestimate the associations among PA and COVID-19 outcomes. That is, the reported associations are likely conservative. Related to this point, and recognizing that some activity is better than no activity,58 it is also possible that the benefits identified in this study could vary based on the type, intensity, and duration of the PA. Future researchers should explore these possibilities. Third, though there is value in considering health and PA data at the county level, there is also variability within counties.59,60 As data become available, more fine-grained analyses are warranted. In addition, some health officials believe COVID-19 cases and deaths are under-reported.61 Though such under-reporting would not necessarily change the pattern of findings reported here, the reader should remain mindful that the COVID-19-related mean scores might be less than those in society at large. Finally, the analyses did not include mitigation efforts occurring at county or state levels, and it is possible that the pattern of results would differ were such variables included.
Finally, there are a number of future research possibilities. As previously noted, a more fine-grained analysis of the type and nature of the county-level PA might yield fruitful insights. Second, in drawing from the social ecological perspective, researchers have identified a host of community and societal factors associated with COVID-19 cases and deaths, but additional possibilities exist. Hood et al.’s51 framework offers a model from which researchers could draw. Finally, though the benefits of community-level PA are demonstrated here and in previous research, there is considerable variability among counties. More work is needed to understand how to promote and sustain PA among community residents.
Competing interests
The author declares that he has no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
The New York Times provided county-level estimates for mask usage, with the data publicly available on GitHub: https://github.com/nytimes/covid-19-data/tree/bde13b021e99c6b4a63fb66a6144e889cc635e31/mask-use. The estimates were based on a survey of 250,000 individuals between July 2 and July 14, 2020. Participants responded to the question: “How often do you wear a mask in public when you expect to be within 6 feet of another person?” The Times then generated estimates for the percentage of people in each county who never, rarely, sometimes, frequently, or always wear a mask in those conditions. These data were merged with the current dataset to explore the influence of physical activity on mask wearing. Bivariate correlations showed that the percentage of county residents who always wore a mask was positively related to the percentage who are physically active (r = 0.23), and negatively associated with COVID-19 cases (r = −0.44) and deaths (r = −0.06) per 100,000 residents.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.03.008.
Appendix. Supplementary materials
References
- 1.Clerkin K.J., Fried J.A., Raikhelkar J. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 2.Cutler D.M., Summers L.H. The COVID-19 pandemic and the $16 trillion virus. JAMA. 2020;324:1495–1496. doi: 10.1001/jama.2020.19759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92:552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang H.Y., Li X.L., Yan Z.R., Sun X.P., Han J., Zhang B.W. Potential neurological symptoms of COVID-19. Ther Adv Neurol Disord. 2020;13 doi: 10.1177/1756286420917830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiong J., Lipsitz O., Nasri F. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J., Zheng Y., Gou X. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallis J.F., Owen N., Fisher E. In: Health behavior: Theory, research, and practice. Vol 5. Glanz K., Rimer B.K., Viswanath K., editors. Jossey-Bass; San Francisco, CA: 2015. Ecological models of health behavior; pp. 465–485. [Google Scholar]
- 9.McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 10.Lyu W., Wehby G.L. Community use of face masks and COVID-19: Evidence from a natural experiment of state mandates in the US. Health Aff (Millwood) 2020;39:1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 11.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cunningham G.B., Wigfall L.T. Race, explicit racial attitudes, implicit racial attitudes, and COVID-19 cases and deaths: An analysis of counties in the United States. PloS One. 2020;15 doi: 10.1371/journal.pone.0242044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wadhera R.K., Wadhera P., Gaba P. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caputo E.L., Reichert F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J Phys Act Health. 2020;3:1–10. doi: 10.1123/jpah.2020-0406. [DOI] [PubMed] [Google Scholar]
- 15.Cheval B., Sivaramakrishnan H., Maltagliati S. Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland. J Sports Sci. 2020;39:699–704. doi: 10.1080/02640414.2020.1841396. [DOI] [PubMed] [Google Scholar]
- 16.Maugeri G., Castrogiovanni P., Battaglia G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. 2020;6:e04315. doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tison G.H., Avram R., Kuhar P. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann Intern Med. 2020;173:767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woods J.A., Hutchinson N.T., Powers S.K. The COVID-19 pandemic and physical activity. Sports Med Health Sci. 2020;2:55–64. doi: 10.1016/j.smhs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hammami A., Harrabi B., Mohr M., Krustrup P. Physical activity and coronavirus disease 2019 (COVID-19): Specific recommendations for home-based physical training. Manag Sport Leis. 2020 doi: 10.1080/23750472.2020.1757494. [DOI] [Google Scholar]
- 21.Dixon M.A., Cunningham G.B. Data aggregation in multilevel analysis: A review of conceptual and statistical issues. Meas Phys Educ Exerc Sci. 2006;10:85–107. [Google Scholar]
- 22.Ewing R., Schmid T., Killingsworth R., Zlot A., Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18:47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- 23.Michimi A., Wimberly M.C. Natural environments, obesity, and physical activity in nonmetropolitan areas of the united states. J Rural Health. 2012;28:398–407. doi: 10.1111/j.1748-0361.2012.00413.x. [DOI] [PubMed] [Google Scholar]
- 24.Sato M., Du J., Inoue Y. Rate of physical activity and community health: Evidence from U.S. counties. J Phys Act Health. 2016;13:640–648. doi: 10.1123/jpah.2015-0399. [DOI] [PubMed] [Google Scholar]
- 25.Simpson R.J., Katsanis E. The immunological case for staying active during the COVID-19 pandemic. Brain Behav Immun. 2020;87:6–7. doi: 10.1016/j.bbi.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dwyer M.J., Pasini M., De Dominicis S., Righi E. Physical activity: Benefits and challenges during the COVID-19 pandemic. Scand J Med Sci Sports. 2020;30:1291–1294. doi: 10.1111/sms.13710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Census Bureau. Terms and definitions. Available at: https://www.census.gov/programs-surveys/popest/guidance-geographies/terms-and-definitions.html. [accessed 02.01.2021]
- 28.Lasry A., Kidder D., Hast M. Timing of community mitigation and changes in reported COVID-19 and community mobility―Four U.S. metropolitan areas. MMWR Morb Mortal Wkly Rep. 2020;69:451–457. doi: 10.15585/mmwr.mm6915e2. February 26–April 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adhikari S., Pantaleo N.P., Feldman J.M., Ogedegbe O., Thorpe L., Troxel A.B. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Adult physical inactivity prevalence maps by race/ethnicity. Available at: https://www.cdc.gov/physicalactivity/data/inactivity-prevalence-maps/index.html. [accessed 03.01.2021]
- 31.Ssentongo P., Ssentongo A.E., Heilbrunn E.S., Ba D.M., Chinchilli V.M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PloS One. 2020;15 doi: 10.1371/journal.pone.0238215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunningham G.B., Wicker P., McCullough B.P. Pollution, health, and the moderating role of physical activity opportunities. Int J Environ Res Public Health. 2020;17:6272. doi: 10.3390/ijerph17176272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu J., Rozelle S., Xu Q., Yu N., Zhou T. Social engagement and elderly health in China: Evidence from the China health and retirement longitudinal survey (CHARLS) Int J Environ Res Public Health. 2019;16:278. doi: 10.3390/ijerph16020278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woolhandler S., Himmelstein D.U. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173:63–64. doi: 10.7326/M20-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen E., Miller G.E. Socioeconomic status and health: Mediating and moderating factors. Annu Rev Clin Psychol. 2013;9:723–749. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- 36.Wenham C., Smith J., Morgan R. Gender and COVID-19 Working Group. COVID-19: The gendered impacts of the outbreak. The Lancet. 2020;395:846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80:e14–e18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jilcott Pitts S.B., Edwards M.B., Moore J.B., Shores K.A., DuBose K.D., McGranahan D. Obesity is inversely associated with natural amenities and recreation facilities per capita. J Phys Act Health. 2013;10:1032–1038. doi: 10.1123/jpah.10.7.1032. [DOI] [PubMed] [Google Scholar]
- 39.Swierzy P., Wicker P., Breuer C. Usefulness of multilevel modeling in sport management research: The case of voluntary roles in nonprofit sports clubs. Meas Phys Educ Exerc Sci. 2019;23:325–336. [Google Scholar]
- 40.Garson G.D. In: Hierarchical linear modeling: Guide and applications. Garson G.D., editor. Sage; Thousand Oaks, CA: 2013. Fundamentals of hierarchical linear and multilevel modeling; pp. 3–25. editor. [Google Scholar]
- 41.Heck R.H., Thomas S.L., Tabata L.N. Routledge; New York, NY: 2013. Multilevel and longitudinal modeling with IBM SPSS. [Google Scholar]
- 42.Vallejo G., Tuero-Herrero E., Núñez J.C., Rosário P. Performance evaluation of recent information criteria for selecting multilevel models in behavioral and social sciences. Int J Clin Health Psychol. 2014;14:48–57. [Google Scholar]
- 43.Cunningham G.B., Ahn N.Y. Moderation in sport management research: Room for growth. Meas Phys Educ Exerc Sci. 2019;23:301–313. [Google Scholar]
- 44.Cohen J., Cohen P., West S.G., Aiken L.S. Erlbaum; Mahwah, NJ: 2013. Applied multiple regression/correlation analysis for the behavioral sciences. [Google Scholar]
- 45.Lyu W., Wehby G.L. Community use of face masks and COVID-19: Evidence from a natural experiment of state mandates in the US. Health Aff (Millwood) 2020;39:1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 46.Amanat S., Ghahri S., Dianatinasab A., Fararouei M., Dianatinasab M. In: Physical exercise for human health. Xiao J., editor. Springer; Singapore: 2020. Exercise and type 2 diabetes; pp. 91–105. [Google Scholar]
- 47.Duggal N.A., Niemiro G., Harridge S.D.R., Simpson R.J., Lord J.M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat Rev Immunol. 2019;19:563–572. doi: 10.1038/s41577-019-0177-9. [DOI] [PubMed] [Google Scholar]
- 48.Ozemek C., Erlandson K.M., Jankowski C.M. Physical activity and exercise to improve cardiovascular health for adults living with HIV. Prog Cardiovasc Dis. 2020;63:178–183. doi: 10.1016/j.pcad.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 49.Sato M., Inoue Y., Du J., Funk D.C. Access to parks and recreational facilities, physical activity, and health care costs for older adults: Evidence from U.S. counties. J Leisure Res. 2019;50:220–238. [Google Scholar]
- 50.Evenson K.R., Porter A.K., Day K.L. Developing the active communities tool to implement the community guide's built environment recommendation for increasing physical activity. Prev Chronic Dis. 2020;17:E142. doi: 10.5888/pcd17.200118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hood C.M., Gennuso K.P., Swain G.R., Catlin B.B. County health rankings: Relationships between determinant factors and health outcomes. Am J Prev Med. 2016;50:129–135. doi: 10.1016/j.amepre.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 52.Gandhi M., Beyrer C., Goosby E. Masks do more than protect others during COVID-19: Reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;35:3063–3066. doi: 10.1007/s11606-020-06067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haischer M.H., Beilfuss R., Hart M.R. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PloS One. 2020;15 doi: 10.1371/journal.pone.0240785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kapilashrami A., Hankivsky O. Intersectionality and why it matters to global health. The Lancet. 2018;391:2589–2591. doi: 10.1016/S0140-6736(18)31431-4. [DOI] [PubMed] [Google Scholar]
- 55.Kim E.J., Marrast L., Conigliaro J. COVID-19: Magnifying the effect of health disparities. J Gen Intern Med. 2020;35:2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74:964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nyenhuis S.M., Greiwe J., Zeiger J.S., Nanda A., Cooke A. Exercise and fitness in the age of social distancing during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:2152–2155. doi: 10.1016/j.jaip.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Powell K.E., Paluch A.E., Blair S.N. Physical activity for health: What kind? How much? How intense? On top of what? Annu Rev Public Health. 2011;32:349–365. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 59.Chen JT, Waterman PD, Krieger N. COVID-19 and the unequal surge in mortality rates in Massachusetts, by city/town and ZIP code measures of poverty, household crowding, race/ethnicity, and racialized economic segregation. HCPDS Working Paper Vol. 19, No. 1 (Harvard Center for Population and Development Studies, 2020). Boston, MA: HCPDS; 2020.
- 60.Khairat S., Haithcoat T., Liu S. Advancing health equity and access using telemedicine: A geospatial assessment. J Am Med Inform Assoc. 2019;26:796–805. doi: 10.1093/jamia/ocz108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Krantz S.G., Rao A.S.R.S. Level of underreporting including underdiagnosis before the first peak of COVID-19 in various countries: Preliminary retrospective results based on wavelets and deterministic modeling. Infect Control Hosp Epidemiol. 2020;41:857–859. doi: 10.1017/ice.2020.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.