Abstract
Neuroinflammation constitutes a normal part of the brain immune response orchestrated by microglial cells. However, a sustained and uncontrolled production of proinflammatory factors together with microglial activation contribute to the onset of a chronic low-grade inflammation, leading to neuronal damage and cognitive as well as behavioral impairments. Hence, limiting brain inflammatory response and improving the resolution of inflammation could be particularly of interest to prevent these alterations. Dietary n-3 long chain polyunsaturated fatty acids (LC-PUFAs) and low molecular weight peptides are good candidates because of their immunomodulatory and proresolutive properties. These compounds are present in a fish hydrolysate derived from marine-derived byproducts. In this study, we compared the effect of an 18-day supplementation with this fish hydrolysate to a supplementation with docosahexaenoic acid (DHA) on lipopolysaccharide (LPS)-induced inflammation in mice. In response to peripherally injected LPS, the fish hydrolysate supplementation decreased the hippocampal mRNA expression of the proinflammatory cytokines IL-6 (p < 0.001), IL-1β (p = 0.0008) and TNF-α (p < 0.0001), whereas the DHA supplementation reduced only the expression of IL-6 (p = 0.004). This decline in proinflammatory cytokine expressions was associated with an increase in the protein expression of IκB (p = 0.014 and p = 0.0054 as compared to the DHA supplementation and control groups, respectively) and to a modulation of microglial activation markers in the hippocampus. The beneficial effects of the fish hydrolysate could be due in part to the switch of the hippocampal oxylipin profile towards a more anti-inflammatory profile as compared to the DHA supplementation. Thus, the valorization of fish byproducts seems very attractive to prevent and counteract neuroinflammation.
Keywords: low molecular weight peptides, docosahexaenoic acid (DHA), microglia, oxylipins, resolution of inflammation, fish byproducts
1. Introduction
Neuroinflammation constitutes a normal part of the brain immune response. It remains a crucial mechanism of defense against pathogens and is involved in response to injury as well as wound healing [1,2]. Microglial cells, the immune cells of the central nervous system (CNS), orchestrate the immune response. Once activated, they display an activated morphology, proliferate and produce pro- and anti-inflammatory cytokines, including interleukin (IL)-1β, IL-6, tumor necrosis factor (TNF)-α, as well as growth factors such as brain-derived neurotrophic factor (BDNF) to ensure the return to homeostasis [3,4,5,6,7,8]. However, a sustained and uncontrolled production of proinflammatory factors together with microglial activation contribute to the onset of chronic low-grade inflammation, leading to neuronal damage, as observed in neurodegenerative diseases and aging [9,10,11]. Indeed, it has been proposed that some diseases that are associated with chronic inflammation could be explained by dysregulated resolution of inflammation as much as by ongoing proinflammatory processes [12]. The functional consequences of dysregulated inflammation include cognitive impairment as well as behavioral alterations, notably depression [13] that could seriously impact the quality of life. Hence, limiting excessive brain inflammatory responses and improving the resolution of inflammation is of importance.
Nutrition appears as an innovative strategy to prevent neuroinflammation-related impairments. Notably, n-3 long chain polyunsaturated fatty acids (LC-PUFAs) and low molecular weight peptides are of interest for their immunomodulatory and proresolutive properties.
n-3 LC-PUFAs, including docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), display powerful anti-inflammatory and proresolutive properties. Indeed, they regulate the release of proinflammatory mediators as evidenced in clinical and preclinical studies, and in vitro [14,15,16] and are precursors of oxylipins called specialized proresolving mediators (SPMs) [15,17,18,19,20,21,22]. They also affect the synthesis of oxylipins derived from arachidonic acid (AA) that are mainly proinflammatory [20,23,24]. The level of oxylipins are regulated by external factors such as proinflammatory stimuli and dietary supply. Indeed, central and peripheral expression of oxylipins’ synthesis enzymes (cyclooxygenases, lipoxygenases, cytochrome P450) as well as oxylipins levels are tightly regulated by inflammatory stimuli [15,20,25,26,27,28,29]. In addition, n-3 LC-PUFA supplementations increase cerebral and peripheral oxylipins derived from DHA and EPA, decrease lipid mediators derived from AA and regulate oxylipins’ synthesis enzymes [20,23,24,28,30,31,32].
Low molecular weight peptides (<1000 Da) contained in protein hydrolysates are also nutrients of interest for their central and peripheral anti-inflammatory properties [33,34]. Indeed, bioactive peptides derived from various food sources inhibit the proinflammatory c-Jun N-terminal kinase/mitogen-activated protein kinase (JNK/MAPK) and nuclear factor kappa B (NF-κB) pathways in vivo and in vitro [35,36,37,38]. In mice, peptides from milk reduced the expression of inflammatory factors such as TNF-α, monocyte chemoattractant protein-1 (MCP-1/CCL2) or inducible nitric oxide synthase (iNOS) in the hippocampus in a model of Alzheimer’s disease [39]. In D-galactose-induced mice ageing, a hydrolysate obtained from lantern fish and containing active di- and tripeptides induced an increased level of BDNF [40]. In vitro, in human primary monocytes and murine macrophages, salmon and lupine-derived peptides inhibited the production of nitric oxide (NO), prostaglandin (PG) E2 and proinflammatory cytokines including TNF-α, IL-6 and IL-1β [41,42]. Moreover, peptides from soy and milk reduced the peripheral expression of proinflammatory factors such as TNF-α, IL-6, IL-1β, interferon-γ and IL-17 in mice colon and abdominal aorta [37,43].
Combining low molecular weight peptides and n-3 LC-PUFAs could be relevant to prevent neuroinflammation since we already demonstrated a beneficial effect of this association in age-related cognitive decline [44]. However, to our knowledge, no studies demonstrated its anti-inflammatory properties. Thus, we explored in mice the effect of a dietary supplementation with a fish hydrolysate, obtained by means of a sustainable developmental approach from marine-derived byproducts, on LPS-induced inflammation and compared it to a DHA supplementation whose anti-inflammatory properties have already been described in the literature.
2. Materials and Methods
2.1. Animals and Treatments
All experiments were performed with 7-week-old C57Bl/6J mice obtained from Janvier Labs (Le Genest-Saint-Isle, France). Mice were maintained under standard housing conditions, on cellulose litter, in a temperature (21 ± 2 °C) and humidity (40%) controlled environment with a 12 h light/dark cycle (9:00–21:00) and with ad libitum access to water and A04 food (Safe, Augy, France). A total of 33 animals were used in this study. This study was approved by the national ethical committee for the care and use of animals (approval ID A16320) and conducted in accordance with the EU Directive 2010/63/EU for animal experiments. Mice received by gavage via a gastric tube (Ecimed, Boissy-Saint-Léger, France) during 18 days 150 µL of supplement containing the fish hydrolysate (from the Brain Booster consortium, n = 10) or 10mg of DHA alone (Polaris, Quimper, France, n = 12) or peanut oil and water for control (n = 11). DHA and fish hydrolysate were diluted in peanut oil or water respectively. The fish hydrolysate was obtained from marine byproducts. The 150 µL fish hydrolysate supplement contained 5 mg of low molecular weight peptides (<1000 Da) and 143 µg of DHA (Table 1). This dose was determined by a literature review [45,46]. At the end of the supplementation period, a solution of LPS (lipopolysaccharide; Escherichia coli, 0127: B8, Sigma-Aldrich, Lyon, France) at a dose of 125 µg/kg (diluted in saline solution NaCl 0.9%) was intraperitoneally injected in 4 fish hydrolysate mice, 6 DHA mice and 6 control mice [20,47]. Six fish hydrolysate mice, 6 DHA mice and 5 control mice received an injection of saline solution.
Table 1.
Composition of the supplementations.
| Control | Hydrolysate | DHA | |
|---|---|---|---|
| Water (µL/day) | 100 | - | 100 |
| Peanut oil (µL/day) | 50 | 50 | - |
| Fish hydrolysate group (µL/day) | - | 100 | - |
| Peptides (mg/day) | - | 5 | - |
| DHA (mg/day) | - | 0.143 | - |
| DHA supplementation group (µL/day) | - | - | 50 |
| DHA (mg/day) | - | - | 10 |
DHA: docosahexaenoic acid.
Two hours after the injection, mice were anesthetized by isoflurane inhalation and euthanized. After transcardiac perfusion of phosphate buffered saline (PBS), brain structures of interest (hippocampus and whole brain cortex) were isolated and stored at −80 °C until analysis.
2.2. Quantitative Real Time PCR
mRNA expression was analyzed on hippocampus as described by Rey et al. (2019) [20]. Total RNAs were extracted using the extraction protocol of TRIzol (Invitrogen, Life Technologies, Villebon sur Yvette, France). The purity and the amount of RNA of each sample were determined using Nanodrop spectrophotometer (Nanodrop One, Life Technologies, France). Two micrograms of RNA were reverse transcribed to synthesize cDNA (complementary DNA) using Superscript III (Invitrogen, Life Technologies, France). As previously described, cDNAs were amplified by PCR using Taqman® primers specific to target genes studied [20,47]. We focused on IL-6 (Mm00446190_m1), IL-1β (Mm00434228_m1), TNF-α (Mm00443258_m1), cluster of differentiation 206 (CD206; Mm00485148_m1), Arginase 1 (Arg1; Mm00475988_m1), suppressor of cytokine signaling 3 (SOCS3; Mm00545913_s1), transforming growth factor β1 (TGF-β1; Mm01178820_m1), cluster of differentiation 68 (CD68; Mm03047343_m1), cluster of differentiation 86 (CD86; Mm00444540_m1), cluster of differentiation 36 (CD36; Mm00432403_m1), cluster of differentiation 11b (CD11b; Mm00434455_m1), toll-like receptor 4 (TLR4; Mm00434455_m1), C-C Motif Chemokine Ligand 2 (CCL2; Mm00441242_m1), BDNF (Mm04230607_s1), tyrosine receptor kinase B (TrkB; Mm00435422_m1), nerve growth factor (NGF; Mm00443039_m1), tyrosine receptor kinase A (TrkA; Mm01219406_m1), cyclooxygenase-2 (COX-2; Mm00478374_m1), 15-lipoxygenase (15-LOX; Mm00507789_m1), 5-lipoxygenase (5-LOX; Mm01182747_m1) and beta-2 microglobulin (B2m; Mm00437762_m1) as reference gene. These genes are involved as modulators of inflammatory response [7,16]. Fluorescence was measured using an ABI PRISM 7500-sequence detection system (Applied Biosystems, Villebon sur Yvette, France) and final quantification was analyzed by the comparative threshold cycle (Ct) method. Results are expressed as relative fold change [20,47] to control target mRNA expression.
2.3. Western Blot
Protein expression was evaluated on hippocampus. Proteins were extracted using the extraction protocol of Simões et al. (2013) [48]. Protein concentration was determined by bicinchoninic acid protein assay (Interchim, Montlucon, France) according to the protocol. For analysis, proteins were resolved on 12% sodium dodecyl sulfate-polyacrylamide gel and transferred to nitrocellulose membranes. Membranes were incubated with different primary antibodies: anti-BDNF (ab108319, rabbit, Abcam, Cambridge, UK), anti-TrkB (4603, rabbit, Cell Signaling, Leiden, The Netherlands), anti-NF-κB (14220-1-AP, rabbit, ProteinTECH, Manchester, UK), anti-IκB (51066-1-AP, rabbit, ProteinTECH, Manchester, UK) and anti-GAPDH as housekeeping protein (51745, rabbit, Cell Signaling, Leiden, The Netherlands). These primary antibodies were detected with appropriated donkey horseradish peroxidase-conjugated secondary antibodies (711-035-152, Jackson Immunoresearch, Westgrove, PA, USA). The membranes were incubated with a peroxidase revealing solution (SuperSignal West Dura, ThermoFisher, Waltham, MA, USA) and were revealed using ChemiDoc MP (Biorad, Hercules, CA, USA). Proteins of interest were normalized to GAPDH and results are expressed as relative expression.
2.4. Lipid Analysis
Lipids from the cortex were extracted and fatty acids were transmethylated as previously described [49,50,51]. Fatty acid methyl esters were analyzed using gas chromatography on a Hewlett Packard Model 5890 series II gas chromatograph (Palo Alto, CA, USA) equipped with a split/spitless injector, a flame ionization detector (Palo Alto, CA, USA), and a CPSIL-88 column (100 m × 0.25 mm internal diameter; film thickness, 0.20 µm; Varian, Les Ulis, France). The carrier gas was hydrogen (inlet pressure, 210 kPa). The oven temperature was held at 60 °C for 5 min, increased to 165 °C at 15 °C/min and held for 1 min, and then to 225 °C at 2 °C/min and finally held at 225 °C for 17 min. The injector and the detector were maintained at 250 °C and 280 °C, respectively. Fatty acid methyl esters were identified by comparison with commercial standards. Fatty acid composition is expressed as a percentage of total fatty acids.
2.5. Oxylipin Quantification
The different metabolites derived from LA, AA, DHA and EPA were extracted from hippocampus and analyzed by mass spectrometry (LC-MS/MS) at METATOUL platform (MetaboHUB, INSERM UMR 1048, I2MC, Toulouse, France) as previously described by Le Faouder et al. (2013) [52]. Results are expressed as pg/mg of protein.
2.6. Statistical Analysis
Statistical analyses were performed using GraphPad Prism 7 (GraphPadSotfware, San Diego, CA, USA). The 3 groups were compared using a 2-way ANOVA test (with LPS and supplementation as factors) followed by an LSD Fisher post hoc test comparison when appropriate.
Principal component analysis (PCA) was performed, using RStudio software (RStudio Desktop 1.3.1056, Boston, MA, USA). The number of components was selected using Cattell criterion. All the data were expressed as means ± SEM. Statistical significance was set at p < 0.05.
3. Results
3.1. Fish Hydrolysate Supplementation Decreases Proinflammatory Marker Expression and Prevents IκB Degradation in Response to LPS
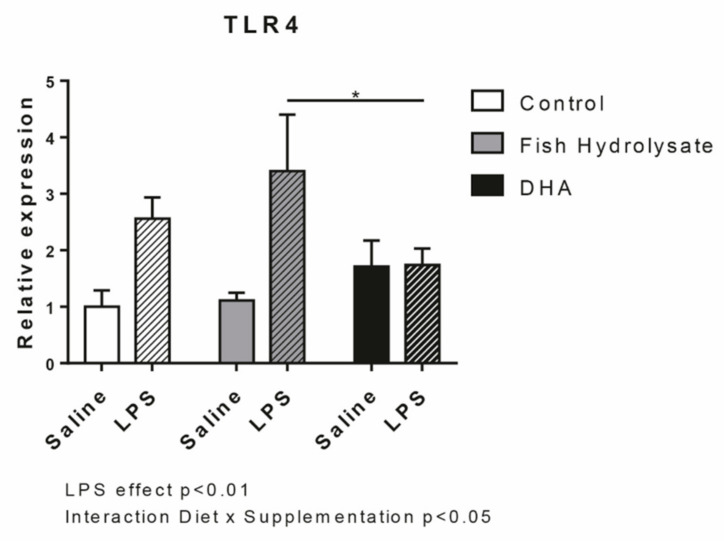
We first evaluated the expression of LPS receptor, TLR4. As expected, LPS increased TLR4 expression (F(1,27) = 13.36, p = 0.011) but no significant effect of both supplementations were observed. However, the interaction between LPS and supplementation was significant (F(2,27) = 3.61, p = 0.0407). DHA supplementation reduced the LPS-induced expression of TLR4 compared to the fish hydrolysate supplementation (p = 0.0163) (Figure 1).
Figure 1.
Expression of the lipopolysaccharide (LPS) receptor TLR4 in the hippocampus of mice fed orally with control solution (in white), fish hydrolysate (in grey) or DHA (in black) by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (hatched bars) (* p < 0.05 by 2-way ANOVA and Fisher’s LSD post hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
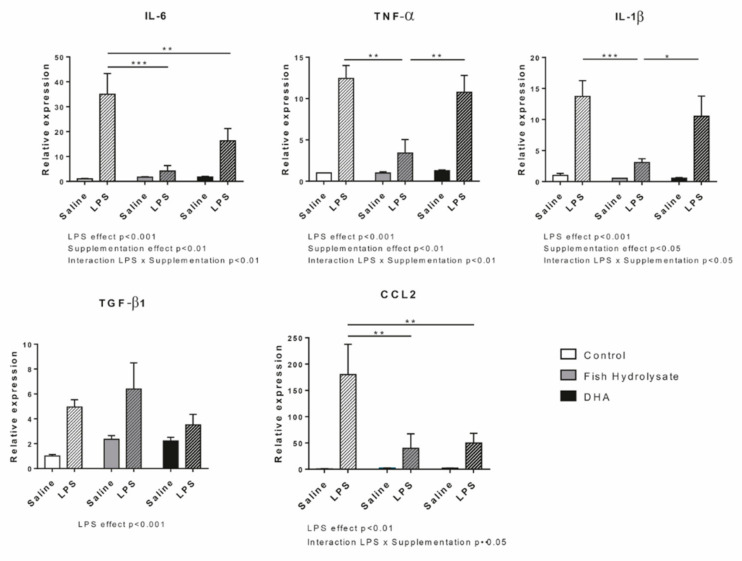
We then determined the impact of both supplementations on pro- and anti-inflammatory cytokine and chemokine expression in response to LPS (Figure 2). As expected, LPS significantly increased the mRNA expression of IL-6 (F(1,27) = 21.86, p < 0.0001), TNF-α (F(1,27) = 56.96, p < 0.0001), IL-1β (F(1,27) = 29.87, p < 0.0001), TGF-β1 (F(1,25) = 19.87, p = 0.0002) and CCL2 (F(1,25) = 12.16, p = 0.0018). Supplementations significantly modulated proinflammatory cytokine expression (IL-6: F(2,27) = 5.595, p = 0.0093; TNF-α: F(2,27) = 6.949, p = 0.0037 and IL-1β: F(2,27) = 4.239, p = 0.0251) and tended to decrease CCL2 expression (F(2,25) = 3.06, p = 0.065) but not the anti-inflammatory marker expression. Interestingly, the two-way ANOVA analysis revealed a significant interaction between LPS and supplementation factors for IL-6 (F(2,27) = 6.195, p = 0.0061), TNF-α (F(2,27) = 6.636, p = 0.0045), IL-1β (F(2,27) = 3.673, p = 0.0388) and CCL2 (F(2,25) = 3.18, p = 0.05) but not for TGF-β1. Indeed, IL-6 expression was significantly decreased by the fish hydrolysate and DHA supplementations (p < 0.001 and p = 0.0040, respectively) whereas TNF-α and IL-1β expression was only decreased by the fish hydrolysate supplementation (p < 0.0001 and p = 0.0008, respectively) in LPS-treated animals. Furthermore, LPS-induced IL-6 expression tended to be more decreased in animals supplemented with the fish hydrolysate as compared to animals treated by DHA (p = 0.0788). CCL2 expression was decreased by both fish hydrolysate (p = 0.0043) and DHA (p = 0.0032) supplementations in LPS-treated mice.
Figure 2.
Expression of pro- and anti-inflammatory cytokines (IL-6, TNF-α, IL-1β, TGF-β1) and chemokine (CCL2) in the hippocampus of mice fed orally with control solution (in white), fish hydrolysate (in grey) or DHA (in black) by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (hatched bars) (* p < 0.05, ** p < 0.01, *** p < 0.001 by 2-way ANOVA and Fisher’s LSD post-hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
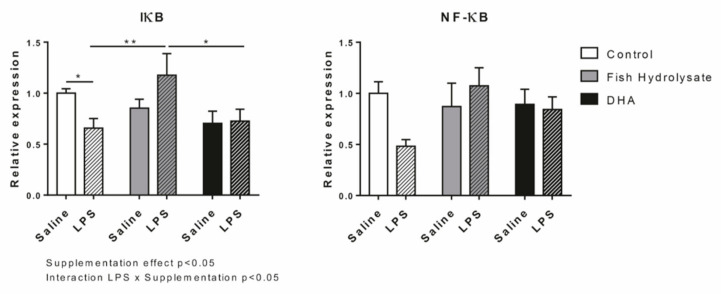
Finally, we examined protein expressions of IκB and NF-κB involved in the regulation of the expression of these inflammatory factors (Figure 3). No significant effect of LPS was observed on both factors. The supplementations affected the protein expression of IκB (F(2,27) = 3.41, p = 0.0479) and an interaction between supplementation and LPS was revealed only for IκB (F(2,27) = 4.03, p = 0.0293). Thus, in inflammatory condition, the protein expression of IκB was significantly increased by the fish hydrolysate supplementation as compared to the DHA supplementation (p = 0.0141) and to the control group (p = 0.0054).
Figure 3.
Protein expression of proinflammatory factors IκB and NF-κB in the hippocampus of mice fed orally with control solution (in white), fish hydrolysate (in grey) or DHA (in black) by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (hatched bars) (* p < 0.05, ** p < 0.01 by 2-way ANOVA and Fisher’s LSD post hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
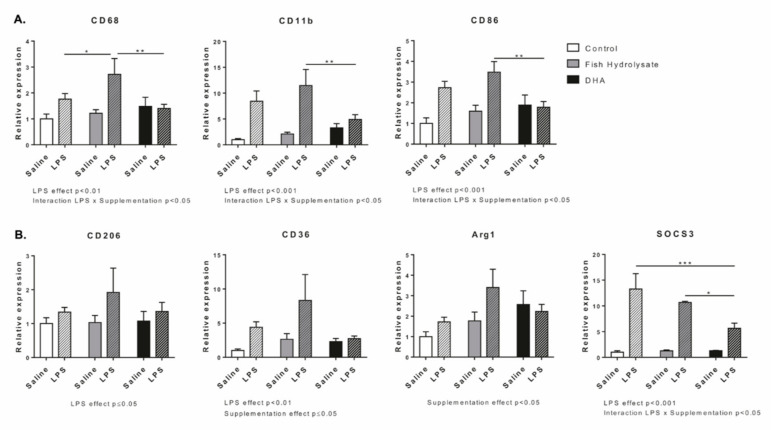
3.2. Fish Hydrolysate Supplementation Modulates Microglial Activation Markers in Response to LPS
We evaluated the expression of different markers of microglial activation (Figure 4A). LPS significantly increased the mRNA expression of CD68 (F(1,27) = 9.86, p = 0.0041), CD11b (F(1,25) = 25.58, p < 0.0001) and CD86 (F(1,27) = 15.28, p = 0.0006). Supplementation had no effect on CD68, CD11b and CD86. However, the two-way ANOVA analysis revealed a significant interaction between LPS and supplementation for CD68 (F(2,27) = 2.41, p = 0.0326), CD11b (F(2,25) = 3.84, p = 0.0351) and CD86 (F(2,27) = 4.83, p = 0.0161). Compared to DHA supplementation, the fish hydrolysate supplementation significantly increased CD68 (p = 0.0045), CD11b (p = 0.0052) and CD86 (p = 0.0045) expression in response to LPS.
Figure 4.
Expression of M1 (A) (CD68, CD11b and CD86) and M2 (B) (CD206, CD36, Arg1 and SOCS3) microglial markers in the hippocampus of mice fed orally with control solution (in white), fish hydrolysate (in grey) or DHA (in black) by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (hatched bars) (* p < 0.05, ** p < 0.01, *** p < 0.001 by 2-way ANOVA and Fisher’s LSD post hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
Then, we determined the expression of anti-inflammatory markers (Figure 4B). LPS significantly increased the mRNA expression of CD206 (F(1,27) = 4.19, p = 0.05), CD36 (F(1,26) = 9.23, p = 0.0054) and SOCS3 (F(1,24) = 42.15, p < 0.0001). Supplementation affected the mRNA expression of Arg1 (F(2,26) = 3.79, p < 0.0358) and CD36 (F(2,26) = 3.22, p = 0.05) and tended to modulate SOCS3 (F(2,24) = 3.003, p = 0.069). An interaction between LPS and supplementation was highlighted for SOCS3 (F(2,24) = 3.46, p = 0.0480). Indeed, DHA supplementation decreased SOCS3 expression in LPS-treated animals compared to control (p = 0.0011) and fish hydrolysate supplemented animals (p = 0.05).
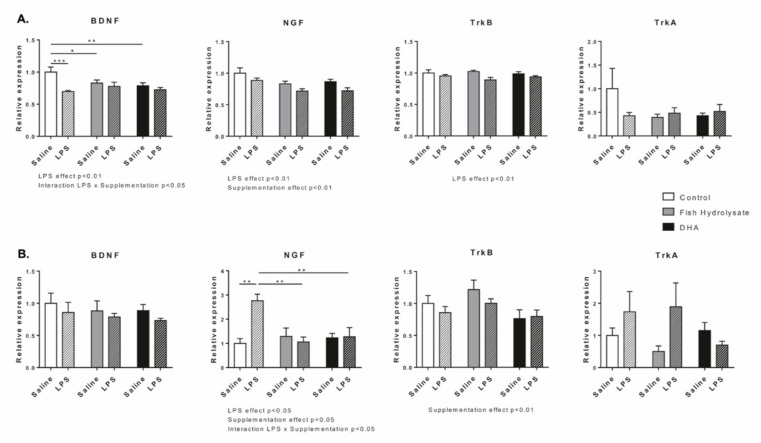
3.3. Fish Hydrolysate Supplementation Prevents LPS-Induced Changes in the Expression of Neurotrophins
We investigated the effect of supplementations on the mRNA expression of neurotrophins BDNF, NGF and their respective receptors TrkB and TrkA (Figure 5a). LPS significantly decreased the mRNA expression of BDNF (F(1,26) = 11.13, p = 0.0026), NGF (F(1,27) = 9.12, p = 0.0055) and TrkB (F(1,27) = 8.80, p = 0.0062) but had no effect on TrkA expression. Supplementations decreased mRNA expression of NGF (F(2,27) = 6.61, p = 0.0046). Interestingly, the basal mRNA expression of BDNF was decreased in fish hydrolysate (F(2,26) = 3.81, p = 0.0354, p = 0.0222) and DHA supplemented animals ((F(2,26) = 3.81, p = 0.0354), p = 0.0054). Moreover, in response to LPS, BDNF mRNA expression was blunted in animals fed with the fish hydrolysate or DHA (F(2,26) = 3.81, p = 0.0354).
Figure 5.
Gene (A) and protein (B) expression of neurotrophins (BDNF, NGF) and their receptors (TrkB and TrkA) in the hippocampus of mice fed orally with control solution (in white), fish hydrolysate (in grey) or DHA (in black) by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (hatched bars) (* p < 0.05, ** p < 0.01, *** p < 0.001 by 2-way ANOVA and Fisher’s LSD post-hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
Then, we measured the protein expression of these factors (Figure 5b). LPS significantly impacted the expression of NGF (F(1,27) = 4.79, p = 0.0374) but had no effect on BDNF, TrkB and TrkA expression. Supplementations significantly affected protein expression of NGF (F(2,27) = 3.49, p = 0.0447) and TrkB (F(2,27) = 3.61, p = 0.0407) but not BDNF and TrkA. The two-way ANOVA showed that the protein expression of NGF significantly increased in the control group in response to LPS whereas it remained stable (compared to saline) in fish hydrolysate and DHA groups (F(2,27) = 6.73, p = 0.0043; p = 0.0026). Moreover, in LPS-treated animals, fish hydrolysate and DHA supplementations significantly decreased NGF expression as compared to the control group (F(2,27) = 6.73, p = 0.0043, p = 0.0073 and p = 0.0089, respectively).
3.4. Fish Hydrolysate and DHA Supplementations Affect Cortical Fatty Acid Composition
We measured the impact of both supplementations on fatty acid composition in the cortex (Table 2). Supplementations significantly modulated total n-6 and total n-3 PUFA levels (total n-6 PUFAs: F(2,27) = 17.22, p < 0.0001 and total n-3 PUFAs: F(2,27) = 5.48, p = 0.01). Almost all n-6 and n-3 long chain PUFAs were impacted: 20:3 n-6 (F(2,26) = 23.39, p < 0.0001), 20:4 n-6 (F(2,27) = 23.70, p < 0.0001), 22:4 n-6 (F(2,26) = 6.05, p = 0.0069), 22:5 n-6 (F(2,25) = 13.13, p = 0.0001), 20:5 n-3 (F(2,27) = 19.59, p < 0.0001), 22:5 n-3 (F(2,27) = 64.00, p < 0.0001) and 22:6 n-3 (F(2,27) = 4.72, p = 0.0175). These changes modulated the n-6/n-3 ratio (F(2,27) = 17.72, p < 0.0001). LPS treatment didn’t have any effect on total n-6 and n-3 PUFA content. However, LPS affected 4 fatty acids, among them three minor PUFAs: 22:4 n-6 (F(1,26) = 5.96, p = 0.0218), 20:2 n-6 (F(1,27) = 4.50, p = 0.0432) and 20:3 n-9 (F(1,27) = 8.68, p = 0.0066) and one major saturated fatty acid: 18:0 (F(1,27) = 19.93, p = 0.0001).
Table 2.
Cortical fatty acid composition of mice fed orally with control solution, fish hydrolysate or DHA by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg).
| Fatty Acid (% of Total Fatty Acids) | Control | Hydrolysate | DHA | Statistical Effect | |||||
|---|---|---|---|---|---|---|---|---|---|
| Saline | LPS | Saline | LPS | Saline | LPS | Supplementation | LPS | Supplementation × LPS | |
| 14:0 | 0.13 ± 0.00 | 0.13 ± 0.00 | 0.12 ± 0.00 | 0.13 ± 0.00 | 0.13 ± 0.00 | 0.13 ± 0.00 | - | - | - |
| 15:0 | 0.04 ± 0.00 | 0.05 ± 0.00 | 0.05 ± 0.00 | 0.05 ± 0.00 | 0.05 ± 0.01 | 0.04 ± 0.00 | - | - | - |
| 16:0 | 21.43 ± 0.22 | 21.36 ± 0.31 | 21.36 ± 0.15 | 21.49 ± 0.12 | 21.27 ± 0.07 | 21.10 ± 0.15 | - | - | - |
| 17:0 | 0.14 ± 0.00 | 0.16 ± 0.01 | 0.14 ± 0.00 | 0.14 ± 0.00 | 0.16 ± 0.02 | 0.14 ± 0.00 | - | - | - |
| 18:0 | 20.03 ± 0.06 a | 19.65 ± 0.04 b | 20.06 ± 0.08 a | 19.66 ± 0.17 b | 19.74 ± 0.05 b | 19.78 ± 0.09 b | - | p = 0.0001 | p = 0.0034 |
| 20:0 | 0.22 ± 0.01 | 0.21 ± 0.01 | 0.21 ± 0.01 | 0.21 ±0.01 | 0.22 ± 0.01 | 0.23 ± 0.01 | - | - | - |
| 22:0 | 0.15 ± 0.01 | 0.17 ± 0.02 | 0.16 ± 0.01 | 0.15 ± 0.01 | 0.15 ± 0.01 | 0.16 ± 0.00 | - | - | - |
| 24:0 | 0.17 ± 0.01 | 0.17 ± 0.01 | 0.17 ± 0.01 | 0.17 ± 0.00 | 0.17 ± 0.01 | 0.18 ± 0.01 | - | - | - |
| SFAs | 42.31 ± 0.21 | 41.89 ± 0.32 | 42.27 ± 0.19 | 42.00 ± 0.15 | 41.89 ± 0.08 | 41.76 ± 0.20 | - | - | - |
| 16:1n-9 | 0.15 ± 0.00 | 0.16 ± 0.00 | 0.16 ± 0.00 | 0.16 ± 0.00 | 0.15 ± 0.00 | 0.15 ± 0.00 | p = 0.0047 | - | - |
| 16:1n-7 | 0.51 ± 0.01 | 0.53 ± 0.01 | 0.52 ± 0.00 | 0.53 ± 0.01 | 0.52 ± 0.01 | 0.52 ± 0.01 | - | - | - |
| 18:1t | 0.03 ± 0.00 a | 0.03 ± 0.00 a | 0.04 ± 0.00 a | 0.04 ± 0.01 a | 0.04 ± 0.01 a | 0.07 ± 0.00 b | p = 0.0004 | - | p = 0.0114 |
| 18:1n-9 | 14.04 ± 0.11 | 14.17 ± 0.11 | 14.17 ± 0.11 | 14.12 ± 0.10 | 14.22 ± 0.18 | 14.42 ± 0.11 | - | - | - |
| 18:1n-7 | 3.51 ± 0.01 | 3.55 ± 0.04 | 3.53 ± 0.02 | 3.50 ± 0.02 | 3.49 ± 0.03 | 3.49 ± 0.01 | - | - | - |
| 20:1n-9 | 0.90 ± 0.03 | 0.94 ± 0.04 | 0.90 ± 0.03 | 0.90 ± 0.03 | 0.93 ± 0.06 | 0.96 ± 0.03 | - | - | - |
| 20:1n-7 | 0.24 ± 0.01 | 0.26 ± 0.01 | 0.25 ± 0.01 | 0.24 ± 0.01 | 0.26 ± 0.02 | 0.26 ± 0.01 | - | - | - |
| 22:1n-9 | 0.09 ± 0.01 | 0.11 ± 0.01 | 0.09 ± 0.00 | 0.10 ± 0.00 | 0.10 ± 0.01 | 0.10 ± 0.00 | - | - | - |
| 24:1n-9 | 0.20 ± 0.01 a,b,c | 0.18 ± 0.01 b,e | 0.22 ± 0.01 a,d | 0.20 ± 0.01 b,d,e | 0.20 ± 0.01 a,e | 0.23 ± 0.01 c,d | - | - | p = 0.0473 |
| MUFAs | 19.68 ± 0.15 | 19.93 ± 0.18 | 19.86 ± 0.16 | 19.79 ± 0.15 | 19.90 ± 0.28 | 20.19 ± 0.14 | - | - | - |
| 18:2n-6 | 0.52 ± 0.01 | 0.47 ± 0.02 | 0.51 ± 0.01 | 0.52 ± 0.01 | 0.54 ± 0.01 | 0.52 ± 0.01 | - | - | - |
| 20:2n-6 | 0.13 ± 0.00 a | 0.12 ± 0.00 b | 0.12 ± 0.00 b,c | 0.13 ± 0.00 a,b | 0.13 ± 0.00 a | 0.13 ± 0.00 a,c | - | p = 0.0432 | p = 0.0089 |
| 20:3n-6 | 0.41 ± 0.01 | 0.39 ± 0.01 | 0.42 ± 0.00 | 0.42 ± 0.01 | 0.47 ± 0.01 | 0.46 ± 0.01 | p < 0.0001 | - | - |
| 20:4n-6 | 9.98 ± 0.11 | 10.15 ± 0.08 | 9.96 ± 0.09 | 9.95 ± 0.06 | 9.34 ± 0.16 | 9.43 ± 0.09 | p < 0.0001 | - | - |
| 22:4n-6 | 2.05 ± 0.03 | 2.17 ± 0.07 | 2.05 ± 0.02 | 2.14 ± 0.04 | 1.93 ± 0.04 | 2.02 ± 0.04 | p = 0.0069 | p = 0.0218 | - |
| 22:5n-6 | 0.30 ± 0.01 | 0.32 ± 0.02 | 0.29 ± 0.01 | 0.30 ± 0.01 | 0.28 ± 0.02 | 0.27 ± 0.00 | p = 0.0001 | - | - |
| n-6 | 13.41 ± 0.13 | 13.61 ± 0.16 | 13.34 ± 0.08 | 13.45 ± 0.07 | 12.69 ± 0.19 | 12.81 ± 0.13 | p < 0.0001 | - | - |
| 20:5n-3 | 0.06 ± 0.01 | 0.06 ± 0.00 | 0.06 ± 0.00 | 0.06 ± 0.00 | 0.08 ± 0.00 | 0.08 ± 0.00 | p < 0.0001 | - | - |
| 22:5n-3 | 0.13 ± 0.00 | 0.14 ± 0.00 | 0.14 ± 0.00 | 0.14 ± 0.00 | 0.17 ± 0.00 | 0.17 ± 0.00 | p < 0.0001 | - | - |
| 22:6n-3 | 15.85 ± 0.29 | 15.67 ± 0.25 | 15.69 ± 0.24 | 16.09 ± 0.24 | 16.74 ± 0.28 | 16.19 ± 0.18 | p = 0.0175 | - | - |
| n-3 | 16.05 ± 0.29 | 15.87 ± 0.24 | 15.89 ± 0.24 | 16.29 ± 0.24 | 16.99 ± 0.28 | 16.43 ± 0.18 | p = 0.01 | - | - |
| 20:3n-9 | 0.13 ± 0.02 a,b | 0.09 ± 0.01 c,d | 0.17 ± 0.03 a | 0.08 ± 0.00 c,d | 0.10 ± 0.00 b,c | 0.12 ± 0.01 b,d | - | p = 0.0066 | p = 0.0122 |
| PUFAs | 29.59 ± 0.31 | 29.56 ± 0.28 | 29.40 ± 0.26 | 29.81 ± 0.20 | 29.78 ± 0.38 | 29.36 ± 0.13 | - | - | - |
| dma16:0 | 2.23 ± 0.03 | 2.36 ± 0.03 | 2.27 ± 0.03 | 2.27 ± 0.05 | 2.24 ± 0.05 | 2.28 ± 0.02 | - | - | - |
| dma18:0 | 3.99 ± 0.03 | 3.99 ± 0.03 | 3.98 ± 0.03 | 3.92 ± 0.03 | 3.97 ± 0.05 | 4.04 ± 0.03 | p = 0.0448 | - | - |
| dma18:1n-9 | 1.19 ± 0.02 | 1.22 ± 0.03 | 1.20 ± 0.03 | 1.19 ± 0.02 | 1.19 ± 0.03 | 1.24 ± 0.02 | - | - | - |
| dma18:1n-7 | 1.02 ± 0.02 | 1.05 ± 0.03 | 1.03 ± 0.02 | 1.03 ± 0.03 | 1.04 ± 0.03 | 1.08 ± 0.02 | - | - | - |
| DMA | 8.43 ± 0.08 | 8.62 ± 0.08 | 8.48 ± 0.06 | 8.41 ± 0.13 | 8.43 ± 0.15 | 8.64 ± 0.09 | - | - | - |
| n-6/n-3 | 0.84 ± 0.02 | 0.86 ± 0.02 | 0.84 ± 0.01 | 0.83 ± 0.01 | 0.75 ± 0.01 | 0.78 ± 0.01 | p < 0.0001 | - | - |
Values with superscripts (a, b, c, d, e) differ significantly, n = 4–6/group. Data are presented as mean ± SEM and are expressed as percentage of total fatty acids. DHA: docosahexaenoic acid; DMA: dimethylacetals; LPS: lipopolysaccharide; MUFAs: monounsaturated fatty acids; PUFAs: polyunsaturated fatty acids; SFAs: saturated fatty acids.
3.5. Fish Hydrolysate Supplementation Affects Hippocampal Oxylipin Concentration in LPS-Treated Animals
We evaluated the impact of the supplementations on the concentration of oxylipins derived from n-6 or n-3 PUFAs in the hippocampus in basal condition or in response to LPS (Table 3). Many oxylipins derived from AA were detected: thromboxanes and prostaglandins (TxB2, 6kPGF1α, PGF2-α, PGE2, PGD2, PGA1, 15dPGJ2, 8isoPGA2), lipoxins (LxA4 and LxB4), epoxy fatty acids (14,15-EET, 8,9-EET, 5,6-EET) and hydroxy fatty acids (15-HETE, 8-HETE, 12-HETE, 5-HETE, 5-oxoETE). We also detected hydroxy fatty acids derived from linoleic acid (LA) (13-HODE and 9-HODE) and hydroxy fatty acids derived from DHA (17-HDoHE, 14-HDoHE and 7-MaR1).
Table 3.
Hippocampal oxylipin concentration of mice fed orally with control solution, fish hydrolysate or DHA by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg).
| Oxylipin (pg /mg protein) | Control | Hydrolysate | DHA | Statistical Effect | |||||
|---|---|---|---|---|---|---|---|---|---|
| Saline | LPS | Saline | LPS | Saline | LPS | Supplementation | LPS | Supplementation × LPS | |
| AA-oxylipins | |||||||||
| Thromboxanes, prostaglandins | |||||||||
| TxB2 | 1584.36 ± 136.93 | 1739.60 ± 138.94 | 1729.72 ± 220.19 | 1495.16 ± 30.78 | 1781.36 ± 166.54 | 1747.47 ± 205.07 | - | - | - |
| 6kPGF1α | 151.68 ± 68.79 a | 505.96 ± 66.67 b | 246.65 ± 83.26 a | 78.59 ± 49.27 a | 210.93 ± 69.00 a | 226.75 ± 92.39 a | - | - | p = 0.0086 |
| PGF2α | 4429.79 ± 380.97 | 5550.45 ± 330.52 | 4582.04 ± 486.14 | 5708.87 ± 577.25 | 5656.33 ± 461.46 | 5155.75 ± 727.26 | - | - | - |
| PGE2 | 1428.02 ± 141.17 a | 2366.55 ± 121.53 b | 1410.87 ± 117.93 a | 2356.64 ± 224.38 b | 1883.66 ± 204.02 a,b | 1881.02 ± 257.90 a,b | - | p = 0.0003 | p = 0.0211 |
| PGD2 | 1741.08 ± 319.14 a | 3208.60 ± 445.99 b | 1639.05 ± 216.33 a | 3188.42 ± 282.95 b,c | 2301.83 ± 244.21 a,b | 2178.11 ± 411.06 a,c | - | p = 0.002 | p = 0.0314 |
| PGA1 | 0.00 ± 0.00 a | 28.65 ± 7.78 b | 0.00 ± 0.00 a | 34.75 ± 11.80 b | 0.00 ± 0.00 a | 0.00 ± 0.00 a | p = 0.0014 | p < 0.0001 | p = 0.0014 |
| 15dPGJ2 | 31.15 ± 19.37 | 71.23 ± 8.44 | 13.59 ± 13.59 | 89.69 ± 19.08 | 45.69 ± 23.73 | 53.66 ± 24.59 | - | p = 0.0145 | - |
| 8isoPGA2 | 464.81 ± 24.87 | 651.95 ± 76.86 | 500.41 ± 109.57 | 864.62 ± 133.33 | 682.20 ± 116.56 | 750.64 ± 92.68 | - | p = 0.0184 | - |
| Lipoxins | |||||||||
| LxA4 | 265.31 ± 31.85 a | 764.10 ± 117.00 c | 352.61 ± 37.66 a,b | 1126.31 ± 115.00 d | 631.05 ± 121.16 b,c | 614.25 ± 151.20 b,c | - | p < 0.0001 | p = 0.0041 |
| LxB4 | 119.60 ± 79.81 | 413.04 ± 100.91 | 488.09 ± 79.65 | 560.64 ± 67.12 | 342.60 ± 115.89 | 309.99 ± 112.83 | p = 0.0483 | - | - |
| Epoxy fatty acids | |||||||||
| 14,15-EET | 258.15 ± 55.32 | 218.68 ± 27.43 | 221.62 ± 44.03 | 339.82 ± 95.94 | 317.46 ± 68.49 | 321.12 ± 36.59 | - | - | - |
| 8,9-EET | 665.74 ± 86.14 | 717.35 ± 62.99 | 745.55 ± 88.82 | 1132.12 ± 251.53 | 984.20 ± 127.64 | 904.92 ± 119.39 | - | - | - |
| 5,6-EET | 510.40 ± 59.39 | 552.36 ± 22.88 | 607.26 ± 61.65 | 776.15 ± 152.98 | 730.88 ± 94.28 | 687.14 ± 90.15 | - | - | - |
| Hydroxy fatty acids | |||||||||
| 15-HETE | 5381.63 ± 491.85 a | 10236.55 ± 1133.60 b,c | 4986.08 ± 394. 85 a | 12370.92 ± 946.68 c | 8412.97 ± 1033.41 b | 8271.61 ± 1124.26 b | - | p < 0.0001 | p = 0.0014 |
| 8-HETE | 616.39 ± 59.62 a | 861.88 ± 71.18 b | 536.21 ± 32.63 a | 1094.93 ± 100.61 c | 825.45 ± 81.77 b | 823.81 ± 84.78 b | - | p = 0.0001 | p = 0.0033 |
| 12-HETE | 1496.97 ± 53.35 a,b | 2662.28 ± 394.98 c,d | 1188.01 ± 51.49 a | 3479.62 ± 252.58 d | 2076.89 ± 258.48 b,c | 2145.92 ± 439.72 b,c | - | p < 0.0001 | p = 0.0044 |
| 5-HETE | 5518.82 ± 671.54 | 6747.00 ± 403.13 | 5484.87 ± 486.33 | 8002.11 ± 382.00 | 7715.60 ± 1005.41 | 8939.82 ± 1212.00 | p = 0.0318 | p = 0.0262 | - |
| 5-oxoETE | 5524.57 ± 639.67 a | 6300.15 ± 474.39 a,c | 5286.41 ± 199.95 a | 9143.13 ± 785.06 b | 8623.43 ± 291.86 b | 7449.52 ± 981.74 b,c | p = 0.0072 | p = 0.0342 | p = 0.0022 |
| LA-oxylipins | |||||||||
| Hydroxy fatty acids | |||||||||
| 13-HODE | 1294.54 ± 41.33 a | 2091.36 ± 184.04 a | 1429.20 ± 192.49 a | 3655.32 ± 871.76 b | 2266.32 ± 315.64 a | 2212.73 ± 339.80 a | - | p = 0.0026 | p = 0.0134 |
| 9-HODE | 497.38 ± 19.99 a | 979.03 ± 109.81 b,c | 577.19 ± 76.69 a,b | 1628.82 ± 355.30 d | 967.76 ± 132.13 b,c | 950.78 ± 147.61 a,c | - | p = 0.0005 | p = 0.0066 |
| DHA-oxylipins | |||||||||
| Hydroxy fatty acids | |||||||||
| 17-HDoHE | 1208.83 ± 91.11 a,b | 2030.94 ± 216.72 c,d | 1002.70 ± 83.64 b | 2428.07 ± 154.48 c | 1717.12 ± 318.00 a,d | 1731.76 ± 194.06 a,d | - | p = 0.0001 | p = 0.0076 |
| 14-HDoHE | 819.92 ± 71.54 a,b | 1171.61 ± 168.81 b,c | 639.76 ± 45.18 a | 1683.52 ± 143.81 d | 1266.36 ± 167.27 c,d | 1290.20 ± 175.01 c,d | - | p = 0.0004 | p = 0.0056 |
| 7-MaR1 | 0.00 ± 0.00 a,b | 42.73 ± 11.82 b | 0.00 ± 0.00 a | 88.89 ± 50.81 c | 0.00 ± 0.00a | 0.00 ± 0.00a | p = 0.0289 | p = 0.0019 | p = 0.0289 |
Values with superscripts (a, b, c, d) differ significantly, n = 4–6/group. Data are presented as mean ± SEM and are expressed in pg/mg protein. 5-oxoETE: 5-oxo-eicosatetraenoic; 7-MaR1: 7(S)-maresin; AA: arachidonic acid; DHA: docosahexaenoic acid; EET: epoxy-eicosatrienoic acid; HDoHE: hydroxy-docosahexaenoic acid; HETE: hydroxy-eicosatetraenoic acid; HODE: hydroxy-octadecadienoic acid; LA: linoleic acid; LPS: lipopolysaccharide; Lx: lipoxin; PG: prostaglandin; TxB2: thromboxane B2.
The two-way ANOVA analysis revealed that most of the significant effects were due to LPS treatment. Indeed, LPS impacted the amounts of oxylipins derived from AA: PGE2 (F(1,27) = 16.76, p = 0.0003), PGD2 (F(1,27) = 11.75, p = 0.002), PGA1 (F(1,26) = 31.51, p < 0.0001), 15dPGJ2 (F(1,27) = 6.83, p = 0.0145), 8isoPGA2 (F(1,27) = 6.29, p < 0.0184), LxA4 (F(1,27) = 21.68, p < 0.0001), 15-HETE (F(1,27) = 27.48, p < 0.0001), 8-HETE (F(1,27) = 19.65, p = 0.0001), 12-HETE (F(1,27) = 22.45, p < 0.0001), 5-HETE (F(1,26) = 5.56, p = 0.0262), 5-oxoETE (F(1,26) = 4.99, p = 0.0342). The same results were found for those derived from LA: 13-HODE (F(1,26) = 11.09, p = 0.0026) and 9-HODE (F(1,26) = 15.84, p = 0.0005) and also for those derived from DHA: 17-HDoHE (F(1,27) = 19.85, p = 0.0001), 14-HDoHE (F(1,27) = 16.10, p = 0.0004) and 7-MaR1 (F(1,27) = 11.91, p = 0.0019). The supplementations modulated the amounts of oxylipins derived from AA: PGA1 (F(2,26) = 8.60, p = 0.0014), LxB4 (F(2,27) = 3.40, p = 0.0483), 5-HETE (F(2,26) = 3.95, p = 0.0318), 5-oxoETE (F(2,26) = 6.00, p = 0.0072) and of 7-MaR1 (F(2,27) = 4.05, p = 0.0289) derived from DHA.
However, an interaction LPS x supplementation was observed for these oxylipins: those derived from AA: PGE2 (F(2,27) = 4.46, p = 0.0211), PGD2 (F(2,27) = 3.95, p = 0.0314), PGA1 (F(2,26) = 8.60, p = 0.0014), LxA4 (F(2,27) = 6.77, p = 0.0041), 15-HETE (F(2,27) = 8.44, p = 0.0014), 8-HETE (F(2,27) = 7.13, p = 0.0033), 12-HETE (F(2,27) = 6.66, p = 0.0044) and 5-oxoETE (F(2,26) = 7.86, p = 0.0022); those derived from LA: 13-HODE (F(2,26) = 5.12, p = 0.0134) and 9-HODE (F(2,26) = 6.12, p = 0.0066); and those derived from DHA: 17-HDoHE (F(2,27) = 5.87, p = 0.0076), 14-HDoHE (F(2,27) = 6.32, p = 0.0056) and 7-MaR1 (F(2,27) = 4.05, p = 0.0289). Indeed, in saline conditions, the fish hydrolysate supplementation increased 17-HDoHE as compared to the DHA group (p = 0.0158). Moreover, DHA supplementation significantly increased 15-HETE, 8-HETE, 12-HETE, 5-oxoETE and 14-HDoHE levels as compared to the control (15-HETE: p = 0.0299, 14-HDoHE: p = 0.0363, 5-oxoETE: p = 0.0022) and fish hydrolysate supplementation (15-HETE: p = 0.0113, 12-HETE: p = 0.0376, 8-HETE: p = 0.0069, 14-HDoHE: p = 0.0031 and 5-oxoETE: p = 0.0007). In response to LPS, the fish hydrolysate supplementation increased PGE2 (p = 0.0023) and 12-HETE (p < 0.0001) as compared to saline-treated animals. It also increased PGA1, LxA4, 15-HETE, 8-HETE, 5-oxoETE, 13-HODE, 9-HODE, 14-HDoHE, 17-HDoHE and 7-MaR1 as compared to control (LxA4: p = 0.0366, 8-HETE: p = 0.0445, 14-HDoDE: p = 0.0252, 5-oxoETE: p = 0.0052, 13-HODE: p = 0.0069 and 9-HODE: p = 0.0084) and to DHA supplementation (LxA4: p = 0.0044, 8-HETE: p = 0.0210, 13-HODE: p = 0.0118, 17-HDoHE: p = 0.0332, 15-HETE: p = 0.0072, 9-HODE: p = 0.0062, PGA1: p < 0.0001 and 7-MaR1: p = 0.0007). Moreover, DHA supplementation decreased PGA1 (p = 0.0001), PGD2 (p = 0.0339) and 7-MaR1 (p = 0.05) levels as compared to control.
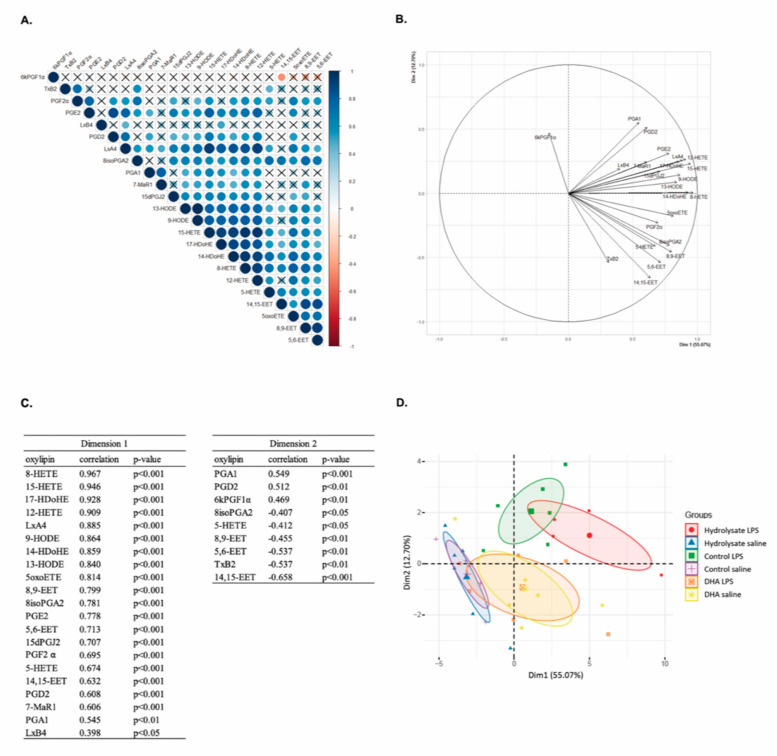
3.6. Multivariate Analysis Highlights the Separation of Oxylipin Profile in Function of the Supplementation in LPS-Treated Animals
We performed multivariate analysis to evaluate if our groups could be differentiated by an oxylipin pattern. The 23 variables corresponding to the 23 oxylipins detected in the mice hippocampus were analyzed. The correlation matrix revealed the most correlated variables. Significant correlations were highlighted (p < 0.05) (Figure 6A): except 6kPGF1α, TxB2 and LxB4, other oxylipins were mostly positively correlated together. According to the correlation matrix, PCA analysis revealed that the oxylipins were mostly grouped (Figure 6B). Indeed, the first component “dim 1” explained 55.07% of the total variance and it showed a positive score for all the oxylipins except 6kPGF1α and TxB2. The component 2 “dim 2” explained 12.70% of the variance and revealed a positive score for PGA1, PGD2 and 6kPGF1α and a negative score for 8isoPGA2, 5-HETE, TxB2, 8,9-EET, 5,6-EET and 14,15-EET (Figure 6C).
Figure 6.
Multivariate analysis of oxylipins in the hippocampus of mice fed orally with control solution, fish hydrolysate or DHA by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg). (A) Correlation matrix of the 23 oxylipins (blue: positive correlation, red: negative correlation, X: no significant correlation). (B) Correlation circle from PCA. (C) Correlation between each variable and the principal component score from PCA (dimension 1 or dimension 2). (D) Individual map of PCA. 5-oxoETE: 5-oxo-eicosatetraenoic; 7-MaR1: 7(S)-maresin; EET: epoxy-eicosatrienoic acid; HDoHE: hydroxy-docosahexaenoic acid; HETE: hydroxy-eicosatetraenoic acid; HODE: hydroxy-octadecadienoic acid; Lx: lipoxin; PCA: principal component analysis; PG: prostaglandin; TxB2: thromboxane B2.
PCA visualization of individuals revealed a separation between the different groups (Figure 6D). Indeed, in basal condition, the control and fish hydrolysate groups showed the same high and negative average score for component 1 whereas the DHA group revealed an average score close to 0. In response to LPS, the DHA group showed a similar profile to that in basal conditions whereas the control and fish hydrolysate groups revealed different profiles as compared to their basal condition but evolved in different ways. Indeed, the control group showed a higher positive average score for component 2 but a small positive average score for component 1 as compared to the fish hydrolysate group. Thus, according to the supplementations, LPS treatment caused a different oxylipin variation.
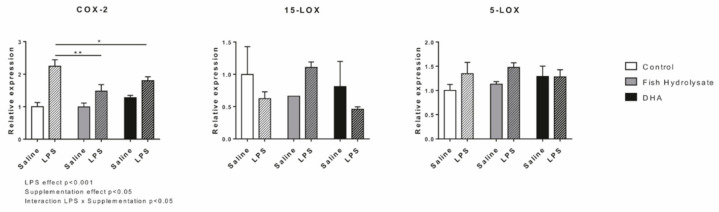
3.7. LPS-Induced Hippocampal Expression of Oxylipin Biosynthesis Enzymes Is Regulated by Supplementations
Oxylipins are mainly generated through the actions of COX-2, 5-LOX and 15-LOX. Hippocampal expression of these enzymes was measured 2 h following LPS injection. LPS significantly increased mRNA expression of COX-2 (F(1,27) = 40.6, p < 0.0001) but had no effect on 15-LOX and 5-LOX (15-LOX: F(1,14) = 0.235, p = 0.635; 5-LOX: F(1,25) = 2.289, p = 0.143). Both supplementations significantly decreased COX-2 expression (F(2,27) = 3.753, p = 0.0375) and the interaction LPS x supplementations was significant (F(2,27) = 4.432, p = 0.0217) (Figure 7). Indeed, the fish hydrolysate and DHA supplementations significantly reduced the LPS-induced expression of COX-2 (p = 0.0014 and p = 0.0294, respectively). No significant effects were found on 15-LOX and 5-LOX expressions.
Figure 7.
Expression of oxylipin biosynthesis enzymes (COX-2, 15-LOX and 5-LOX) in the hippocampus of mice fed orally with control solution, fish hydrolysate or DHA by daily gavage for 18 days, 2 h following LPS injection (125 µg/kg) (* p < 0.05, ** p < 0.01 by 2-way ANOVA and Fisher’s LSD post hoc test; n = 4–6 per group). Data are presented as mean ± SEM. DHA: docosahexaenoic acid; LPS: lipopolysaccharide.
4. Discussion
This work provides evidence that dietary supplementation with fish hydrolysate reduces the LPS-induced proinflammatory cytokine expression and switch hippocampal oxylipin profile, thus counteracting neuroinflammation.
Neuroinflammation is a normal part of the immune response against pathogen invasion or tissue injury [1,2]. The inflammatory response is an active process, limited in time and space, and programmed to re-establish tissue homeostasis [53,54,55]. However, a default in proresolving pathways can result in chronic low-grade inflammation, leading to long term excessive tissue damage and pathology [54,56]. Various mechanisms are involved in the resolution of inflammation, including the inhibition of proinflammatory markers, the increased production of anti-inflammatory cytokines and the generation of lipid metabolites called oxylipins [54,56]. We thus evaluated the effects of the fish hydrolysate on these mechanisms following systemic LPS injection.
Dietary supplementation with fish hydrolysate reduced the LPS-induced expression of proinflammatory cytokines IL-6, IL-1β and TNF-α. We previously showed that this fish hydrolysate reduced the LPS-induced expression of IL-6 and IL-1β in microglial-like cells [44]. This beneficial effect of the fish hydrolysate can be linked, in part, to the increased protein expression of IκB that inhibits NF-κB responsible for the production of proinflammatory cytokines [57]. This decrease in the expression of proinflammatory cytokines 2 h following LPS injection was also accompanied by the reduction in CCL2 expression, which is a chemokine highly expressed by microglia to attract monocytes from the periphery to the brain during neuroinflammation [58]. Thus, our results suggest that the anti-inflammatory properties of the fish hydrolysate were sufficient to limit the recruitment of peripheral monocytes 2 h post-LPS. The immune response is orchestrated by microglial cells, which shift their functional phenotype once stimulated by inflammatory factors [59,60]. Then we evaluated the effects of the fish hydrolysate supplementation on the expression of microglial phenotype markers. Although the fish hydrolysate supplementation had no effect on the expression of the M2 phenotype markers, our results showed a higher expression of the M1 microglial activation markers CD86, CD68 and CD11b 2 h post-LPS compared to control and DHA groups. Fish hydrolysate reduced gene expression of COX-2, another marker of the M1 phenotype, also responsible for the biosynthesis of the first lipid mediators synthesized following LPS injection, the proinflammatory oxylipins (prostaglandins and leukotrienes). COX-2 expression is rapidly increased under inflammatory conditions and is regulated by NF-κB [61,62,63,64,65]. Here, we can hypothesize that 2 h-post LPS, proinflammatory oxylipins have already been produced in the fish hydrolysate supplemented mice, and that there has been a switch in lipid mediator class towards the synthesis of anti-inflammatory mediators and proresolving mediators (lipoxins and SPMs), suggesting that the resolution of inflammation has begun.
Among the fish hydrolysate compounds, low molecular weight peptides and DHA can explain the effects described above since both have been reported to have beneficial effects on inflammation. Indeed, protein hydrolysates show strong immunomodulatory effects in animals. Oral administration of a bioactive milk tripeptide inhibits the expression of inflammatory factors such as TNF-α, CCL2 or iNOS in the hippocampus of the Alzheimer’s disease mice model [39]. In another study, milk-derived tripeptides decrease proinflammatory cytokines IL-1β, IL-6 as well as SOCS3 in the abdominal aorta of ApoE-deficient mice, thus reducing atherosclerosis development [37]. Moreover, egg-derived tripeptides significantly decrease the plasmatic expression of IL-6 and CCL2 in a model of hypertensive rats [36]. At the cellular level, peptides from salmon exerted anti-inflammatory activities by reducing TNF-α, IL-1β, IL-6 expressions and decreasing NO and PGE2 production in murine macrophages [41]. In human monocytes, an octapeptide from lupine reduces the LPS-induced expression of IL-6, TNF-α, IL-1β as well as CCL2 and increases the expression of the anti-inflammatory cytokine IL-10 [42].
The beneficial effect of DHA, the second compound of interest in the fish hydrolysate, has been demonstrated in vivo in numerous studies. DHA and/or EPA limit or prevent the LPS-induced increase in proinflammatory cytokines in the CNS [20,66,67,68,69]. Furthermore, mice fed with a diet enriched in α-linolenic acid, the precursor of DHA, have higher brain DHA levels and produce less cortical proinflammatory cytokines and CCL2 24h post traumatic brain injury [70]. These beneficial effects of DHA on the CNS or the brain could be direct or indirect. Indeed, DHA can act directly by downregulating the activation of NF-κB, p38 MAPK as well as JNK and consequently decreasing the production of proinflammatory cytokines and chemokines by microglia in vitro [67,71,72,73,74,75,76]. Moreover, DHA can reduce microglial activation and shift microglial polarization toward the M2 phenotype in vivo and in vitro under inflammatory conditions and in models of neurological diseases [66,77,78,79,80,81,82,83]. DHA can also act indirectly via the synthesis of SPMs, which reduce the intensity of inflammation [54]. SPMs include protectins, D-series resolvins, and maresins [54,84,85]. They display anti-inflammatory and proresolving properties as well as neuroprotective functions [19,68,86,87]. Dietary interventions with n-3 PUFAs, including DHA, have been shown to increase EPA- and DHA-derived oxylipins and decrease oxylipins derived from AA [20,23,24]. Conversely, Taha et al. [28] have shown that dietary n-6 PUFA supplementation increases AA-derived oxylipins and decreases EPA-derived oxylipins. Furthermore, Rey et al. [20] showed that a dietary supplementation with n-3 long chain PUFAs induces an anti-inflammatory oxylipin profile in mice 24h post-LPS. This oxylipin generation following LPS injection can explain, in part, the differential effect between fish hydrolysate and DHA supplementations. Indeed, as compared to DHA supplementation, the fish hydrolysate supplementation induced a higher production of oxylipins derived from DHA, Mar1, its precursor 14-HDoHE and 17-HDoHE, which are derived from the LOX pathway [17]. Mar1 was first identified in macrophages and is involved in the resolution of inflammation [88,89]. Mar1 has been shown to decrease proinflammatory signaling cascades and influence macrophages towards an M2 repair phenotype after cerebral ischemia or spinal cord injury [90,91,92]. The increase in 17-HDoHE and 14-HDoHE has been reported to down-regulate the inflammatory response in the CNS and in microglia in vitro [19,20,93]. In addition, 17R-HDHA and 17S-HDHA reduce the production of proinflammatory cytokines in the spinal cord and hippocampus [68,94]. Furthermore, the fish hydrolysate supplementation increased the production of LxA4, which is a lipid-mediator class switching between the acute inflammation phase and the resolution phase. It possesses anti-inflammatory properties through the ALX/Fpr2 receptor, which is particularly expressed in microglia [22,94,95,96,97]. LxA4 inhibits neutrophil infiltration, decreases proinflammatory cytokine expression via the inhibition of NF-κB, phosphorylation of p38 MAPK and JNK [98,99,100]. Furthermore, the fish hydrolysate induced an increased production of 12-HETE and 15-HETE. Despite the fact that 12- and 15-HETE are mostly described as proinflammatory, anti-inflammatory properties have also been highlighted [101]. Indeed, they can activate PPARγ, attenuate COX-2 and iNOS expression and inhibit the NF-κB pathway in ischemic rat brain [102]. Thus, our results suggest that the fish hydrolysate supplementation induced a faster transition from the acute inflammation phase to the resolution phase compared to control and DHA groups.
Interestingly, we also demonstrated that the differential effect between the fish hydrolysate and DHA supplementation could be due to the greater attenuation of LPS-induced expression of proinflammatory cytokines of the fish hydrolysate supplementation as compared to DHA supplementation. Indeed, 2 h following LPS injection, DHA supplementation only reduced the expression of IL-6 whereas the fish hydrolysate supplementation decreased the expression of IL-6, IL-1β and TNF-α. We hypothesized that the effect on proinflammatory cytokines could be due to peptides alone or to the potentiation of DHA present in low amount in the fish hydrolysate by the low molecular weight peptides. To answer this point, we have to isolate and test separately the low molecular weight peptides. Another hypothesis would be that the fish hydrolysate modified the kinetic of the resolution of inflammation by shifting microglia polarization into a more reactive phenotype, as shown by the increase in microglial activation, which could be in accordance with a faster immune response and beneficial during acute inflammation. Altogether, our results showed that the fish hydrolysate supplementation induced an earlier immune response 2 h post-LPS as compared to DHA supplementation. Indeed, the shift of microglia into a more reactive phenotype allowed a lower inflammatory response which was associated to the decrease in proinflammatory markers and to the production of anti-inflammatory and proresolutive oxylipins. These changes could explain the different hippocampal oxylipin profile compared to control and DHA groups, and thus the modulation of the immune response observed.
5. Conclusions
These results are particularly of interest since the fish hydrolysate allowed a faster immune response compared to a supplementation with 100 times more DHA, described as the efficient dose in the literature. Furthermore, this fish hydrolysate was obtained through the valorization of marine byproducts in a context of sustainable development. Thus, it remains an innovative and good candidate for the prevention of inflammation and notably in the case of neurodegenerative pathologies, which are characterized by a chronic low-grade inflammation. Nevertheless, in this work we did not evaluate the impact of hydrolysate supplementation on LPS-injected mice outcome as fever, food intake and sickness behavior. Further investigations are still needed to decipher the individual role of low molecular weight peptides and DHA by realizing a time course of inflammatory markers expression after LPS injection to better understand the mechanisms of action at the cerebral level and to characterize the peptides contained in this hydrolysate.
Acknowledgments
This work is part of the Brain Booster project selected for Fonds Unique Interministériel (FUI) projects (2016–2020). Every partner of the Brain Booster Consortium is acknowledged. The authors would also like to thank the animal technicians for the animal care and Blandine Gendre for the realization of the multivariate analysis. VP, SL, EB, AM, ALD and CJ devised the project, the main conceptual ideas and the proof outline. MC, VP, ALD and CJ conceived and designed the experiments. MC, MM and CL conducted the research, analyzed the data and performed the statistical analysis. MC wrote the manuscript with support from ALD and CJ. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Abbreviations
| 5-oxoETE | 5-oxo-eicosatetraenoic acid |
| AA | arachidonic acid |
| ALA | α-linolenic acid |
| Arg1 | arginase 1 |
| BDNF | brain-derived neurotrophic factor |
| CD | cluster of differentiation |
| CNS | central nervous system |
| COX | cyclooxygenase |
| DHA | docosahexaenoic acid |
| EET | epoxy eicosatrienoic acid |
| EPA | eicosapentaenoic acid |
| HDoHE | hydroxy-docosahexaenoic acid |
| HETE | hydroxy-eicosatetraenoic acid |
| HODE | hydroxy-octadecadienoic acid |
| IL | interleukin |
| iNOS | inducible nitric oxide synthase |
| JNK | c-Jun N-terminal kinase |
| LA | linoleic acid |
| LC-PUFAs | long chain polyunsaturated fatty acids |
| LOX | lipoxygenase |
| LPS | lipopolysaccharide |
| Lx | lipoxin |
| MAPK | mitogen-activated protein kinase |
| MaR | maresin |
| MCP-1/CCL2 | monocyte chemoattractant protein-1 |
| NF-κB | nuclear factor kappa B |
| NGF | nerve growth factor |
| NO | nitric oxide |
| PG | prostaglandin |
| PUFAs | polyunsaturated fatty acids |
| SPMs | specialized proresolving mediators |
| SOCS | Suppressor of cytokine signalling |
| TGF | transforming growth factor |
| TLR | toll-like receptor |
| TNF | tumor necrosis factor |
| Trk | tyrosine receptor kinase |
| Tx | thromboxane |
Author Contributions
V.P., S.L., A.M., E.B.; A.-L.D. and C.J. devised the project, the main conceptual ideas and proof outline. M.C., V.P., S.L., A.-L.D. and C.J. conceived and designed experiments. M.C., M.M. and C.L. conducted research, analyzed data and performed statistical analysis. M.C. wrote the manuscript with support of A.-L.D. and C.J. All authors have read and agreed to the published version of the manuscript.
Funding
This work is part of the Brain Booster project which has been funded by Bpifrance and the Région Bretagne (DOS0049628/00).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Bordeaux (France) (protocol code A16320, date of approval 9/18/2018).
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Calder P.C., Albers R., Antoine J.-M., Blum S., Bourdet-Sicard R., Ferns G.A., Folkerts G., Friedmann P.S., Frost G.S., Guarner F., et al. Inflammatory Disease Processes and Interactions with Nutrition. Br. J. Nutr. 2009;101(Suppl. S1):S1–S45. doi: 10.1017/S0007114509377867. [DOI] [PubMed] [Google Scholar]
- 2.Calder P.C. Long Chain Fatty Acids and Gene Expression in Inflammation and Immunity. Curr. Opin. Clin. Nutr. Metab. Care. 2013;16:425–433. doi: 10.1097/MCO.0b013e3283620616. [DOI] [PubMed] [Google Scholar]
- 3.Aloisi F. Immune Function of Microglia. Glia. 2001;36:165–179. doi: 10.1002/glia.1106. [DOI] [PubMed] [Google Scholar]
- 4.Dantzer R., O’Connor J.C., Freund G.G., Johnson R.W., Kelley K.W. From Inflammation to Sickness and Depression: When the Immune System Subjugates the Brain. Nat. Rev. Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dinel A.-L., André C., Aubert A., Ferreira G., Layé S., Castanon N. Lipopolysaccharide-Induced Brain Activation of the Indoleamine 2,3-Dioxygenase and Depressive-like Behavior Are Impaired in a Mouse Model of Metabolic Syndrome. Psychoneuroendocrinology. 2014;40:48–59. doi: 10.1016/j.psyneuen.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Heneka M.T., Carson M.J., El Khoury J., Landreth G.E., Brosseron F., Feinstein D.L., Jacobs A.H., Wyss-Coray T., Vitorica J., Ransohoff R.M., et al. Neuroinflammation in Alzheimer’s Disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Layé S., Parnet P., Goujon E., Dantzer R. Peripheral Administration of Lipopolysaccharide Induces the Expression of Cytokine Transcripts in the Brain and Pituitary of Mice. Brain Res. Mol. Brain Res. 1994;27:157–162. doi: 10.1016/0169-328X(94)90197-X. [DOI] [PubMed] [Google Scholar]
- 8.Nimmerjahn A., Kirchhoff F., Helmchen F. Resting Microglial Cells Are Highly Dynamic Surveillants of Brain Parenchyma in Vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 9.Layé S. Polyunsaturated Fatty Acids, Neuroinflammation and Well Being. Prostaglandins Leukot. Essent. Fatty Acids. 2010;82:295–303. doi: 10.1016/j.plefa.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Rothwell N.J., Luheshi G.N. Interleukin 1 in the Brain: Biology, Pathology and Therapeutic Target. Trends Neurosci. 2000;23:618–625. doi: 10.1016/S0166-2236(00)01661-1. [DOI] [PubMed] [Google Scholar]
- 11.Venters H.D., Dantzer R., Kelley K.W. A New Concept in Neurodegeneration: TNFalpha Is a Silencer of Survival Signals. Trends Neurosci. 2000;23:175–180. doi: 10.1016/S0166-2236(99)01533-7. [DOI] [PubMed] [Google Scholar]
- 12.Fullerton J.N., Gilroy D.W. Resolution of Inflammation: A New Therapeutic Frontier. Nat. Rev. Drug Discov. 2016;15:551–567. doi: 10.1038/nrd.2016.39. [DOI] [PubMed] [Google Scholar]
- 13.Capuron L., Dantzer R. Cytokines and Depression: The Need for a New Paradigm. Brain Behav. Immun. 2003;17(Suppl. S1):S119–S124. doi: 10.1016/S0889-1591(02)00078-8. [DOI] [PubMed] [Google Scholar]
- 14.Calder P.C. Polyunsaturated Fatty Acids and Inflammation. Biochem. Soc. Trans. 2005;33:423–427. doi: 10.1042/BST0330423. [DOI] [PubMed] [Google Scholar]
- 15.Joffre C., Rey C., Layé S. N-3 Polyunsaturated Fatty Acids and the Resolution of Neuroinflammation. Front. Pharmacol. 2019;10 doi: 10.3389/fphar.2019.01022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Layé S., Nadjar A., Joffre C., Bazinet R.P. Anti-Inflammatory Effects of Omega-3 Fatty Acids in the Brain: Physiological Mechanisms and Relevance to Pharmacology. Pharmacol. Rev. 2018;70:12–38. doi: 10.1124/pr.117.014092. [DOI] [PubMed] [Google Scholar]
- 17.Hong S., Gronert K., Devchand P.R., Moussignac R.-L., Serhan C.N. Novel Docosatrienes and 17S-Resolvins Generated from Docosahexaenoic Acid in Murine Brain, Human Blood, and Glial Cells. Autacoids in Anti-Inflammation. J. Biol. Chem. 2003;278:14677–14687. doi: 10.1074/jbc.M300218200. [DOI] [PubMed] [Google Scholar]
- 18.Levy B.D., Clish C.B., Schmidt B., Gronert K., Serhan C.N. Lipid Mediator Class Switching during Acute Inflammation: Signals in Resolution. Nat. Immunol. 2001;2:612–619. doi: 10.1038/89759. [DOI] [PubMed] [Google Scholar]
- 19.Rey C., Nadjar A., Buaud B., Vaysse C., Aubert A., Pallet V., Layé S., Joffre C. Resolvin D1 and E1 Promote Resolution of Inflammation in Microglial Cells in Vitro. Brain Behav. Immun. 2016;55:249–259. doi: 10.1016/j.bbi.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Rey C., Delpech J.C., Madore C., Nadjar A., Greenhalgh A.D., Amadieu C., Aubert A., Pallet V., Vaysse C., Layé S., et al. Dietary N-3 Long Chain PUFA Supplementation Promotes a pro-Resolving Oxylipin Profile in the Brain. Brain Behav. Immun. 2019;76:17–27. doi: 10.1016/j.bbi.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 21.Serhan C.N., Clish C.B., Brannon J., Colgan S.P., Chiang N., Gronert K. Novel Functional Sets of Lipid-Derived Mediators with Antiinflammatory Actions Generated from Omega-3 Fatty Acids via Cyclooxygenase 2–Nonsteroidal Antiinflammatory Drugs and Transcellular Processing. J. Exp. Med. 2000;192:1197–1204. doi: 10.1084/jem.192.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serhan C.N., Dalli J., Colas R.A., Winkler J.W., Chiang N. Protectins and Maresins: New pro-Resolving Families of Mediators in Acute Inflammation and Resolution Bioactive Metabolome. Biochim. Biophys. Acta. 2015;1851:397–413. doi: 10.1016/j.bbalip.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balvers M.G.J., Verhoeckx K.C.M., Bijlsma S., Rubingh C.M., Meijerink J., Wortelboer H.M., Witkamp R.F. Fish Oil and Inflammatory Status Alter the N-3 to n-6 Balance of the Endocannabinoid and Oxylipin Metabolomes in Mouse Plasma and Tissues. Metabolomics. 2012;8:1130–1147. doi: 10.1007/s11306-012-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hashimoto M., Katakura M., Tanabe Y., Al Mamun A., Inoue T., Hossain S., Arita M., Shido O. N-3 Fatty Acids Effectively Improve the Reference Memory-Related Learning Ability Associated with Increased Brain Docosahexaenoic Acid-Derived Docosanoids in Aged Rats. Biochim. Biophys. Acta BBA Mol. Cell Biol. Lipids. 2015;1851:203–209. doi: 10.1016/j.bbalip.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 25.Balvers M.G.J., Verhoeckx K.C.M., Meijerink J., Bijlsma S., Rubingh C.M., Wortelboer H.M., Witkamp R.F. Time-Dependent Effect of in Vivo Inflammation on Eicosanoid and Endocannabinoid Levels in Plasma, Liver, Ileum and Adipose Tissue in C57BL/6 Mice Fed a Fish-Oil Diet. Int. Immunopharmacol. 2012;13:204–214. doi: 10.1016/j.intimp.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 26.Birnie M., Morrison R., Camara R., Strauss K.I. Temporal Changes of Cytochrome P450 (Cyp) and Eicosanoid-Related Gene Expression in the Rat Brain after Traumatic Brain Injury. BMC Genom. 2013;14:303. doi: 10.1186/1471-2164-14-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenberger T.A., Villacreses N.E., Hovda J.T., Bosetti F., Weerasinghe G., Wine R.N., Harry G.J., Rapoport S.I. Rat Brain Arachidonic Acid Metabolism Is Increased by a 6-Day Intracerebral Ventricular Infusion of Bacterial Lipopolysaccharide. J. Neurochem. 2004;88:1168–1178. doi: 10.1046/j.1471-4159.2003.02246.x. [DOI] [PubMed] [Google Scholar]
- 28.Taha A.Y., Blanchard H.C., Cheon Y., Ramadan E., Chen M., Chang L., Rapoport S.I. Dietary Linoleic Acid Lowering Reduces Lipopolysaccharide-Induced Increase in Brain Arachidonic Acid Metabolism. Mol. Neurobiol. 2017;54:4303–4315. doi: 10.1007/s12035-016-9968-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Willenberg I., Rund K., Rong S., Shushakova N., Gueler F., Schebb N.H. Characterization of Changes in Plasma and Tissue Oxylipin Levels in LPS and CLP Induced Murine Sepsis. Inflamm. Res. 2016;65:133–142. doi: 10.1007/s00011-015-0897-7. [DOI] [PubMed] [Google Scholar]
- 30.Kim H.-W., Rao J.S., Rapoport S.I., Igarashi M. Dietary N-6 PUFA Deprivation Downregulates Arachidonate but Upregulates Docosahexaenoate Metabolizing Enzymes in Rat Brain. Biochim. Biophys. Acta BBA Mol. Cell Biol. Lipids. 2011;1811:111–117. doi: 10.1016/j.bbalip.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leng S., Winter T., Aukema H.M. Dietary ALA, EPA and DHA Have Distinct Effects on Oxylipin Profiles in Female and Male Rat Kidney, Liver and Serum. J. Nutr. Biochem. 2018;57:228–237. doi: 10.1016/j.jnutbio.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 32.Rao J.S., Ertley R.N., DeMar J.C., Rapoport S.I., Bazinet R.P., Lee H.-J. Dietary N-3 PUFA Deprivation Alters Expression of Enzymes of the Arachidonic and Docosahexaenoic Acid Cascades in Rat Frontal Cortex. Mol. Psychiatry. 2007;12:151–157. doi: 10.1038/sj.mp.4001887. [DOI] [PubMed] [Google Scholar]
- 33.Lee S.Y., Hur S.J. Mechanisms of Neuroprotective Effects of Peptides Derived from Natural Materials and Their Production and Assessment. Compr. Rev. Food Sci. Food Saf. 2019;18:923–935. doi: 10.1111/1541-4337.12451. [DOI] [PubMed] [Google Scholar]
- 34.Majumder K., Mine Y., Wu J. The Potential of Food Protein-Derived Anti-Inflammatory Peptides against Various Chronic Inflammatory Diseases. J. Sci. Food Agric. 2016;96:2303–2311. doi: 10.1002/jsfa.7600. [DOI] [PubMed] [Google Scholar]
- 35.Aihara K., Ishii H., Yoshida M. Casein-Derived Tripeptide, Val-Pro-Pro (VPP), Modulates Monocyte Adhesion to Vascular Endothelium. J. Atheroscler. Thromb. 2009;16:594–603. doi: 10.5551/jat.729. [DOI] [PubMed] [Google Scholar]
- 36.Majumder K., Chakrabarti S., Davidge S.T., Wu J. Structure and Activity Study of Egg Protein Ovotransferrin Derived Peptides (IRW and IQW) on Endothelial Inflammatory Response and Oxidative Stress. J. Agric. Food Chem. 2013;61:2120–2129. doi: 10.1021/jf3046076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakamura T., Hirota T., Mizushima K., Ohki K., Naito Y., Yamamoto N., Yoshikawa T. Milk-Derived Peptides, Val-Pro-Pro and Ile-Pro-Pro, Attenuate Atherosclerosis Development in Apolipoprotein E–Deficient Mice: A Preliminary Study. J. Med. Food. 2013;16:396–403. doi: 10.1089/jmf.2012.2541. [DOI] [PubMed] [Google Scholar]
- 38.Zhang H., Kovacs-Nolan J., Kodera T., Eto Y., Mine Y. γ-Glutamyl Cysteine and γ-Glutamyl Valine Inhibit TNF-α Signaling in Intestinal Epithelial Cells and Reduce Inflammation in a Mouse Model of Colitis via Allosteric Activation of the Calcium-Sensing Receptor. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2015;1852:792–804. doi: 10.1016/j.bbadis.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 39.Min L.-J., Kobayashi Y., Mogi M., Tsukuda K., Yamada A., Yamauchi K., Abe F., Iwanami J., Xiao J.-Z., Horiuchi M. Administration of Bovine Casein-Derived Peptide Prevents Cognitive Decline in Alzheimer Disease Model Mice. PLoS ONE. 2017;12:e0171515. doi: 10.1371/journal.pone.0171515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chai H.-J., Wu C.-J., Yang S.-H., Li T.-L., Pan B.-S. Peptides from Hydrolysate of Lantern Fish (Benthosema Pterotum) Proved Neuroprotective In Vitro and In Vivo. J. Funct. Foods. 2016;24:438–449. doi: 10.1016/j.jff.2016.04.009. [DOI] [Google Scholar]
- 41.Ahn C.-B., Cho Y.-S., Je J.-Y. Purification and Anti-Inflammatory Action of Tripeptide from Salmon Pectoral Fin Byproduct Protein Hydrolysate. Food Chem. 2015;168:151–156. doi: 10.1016/j.foodchem.2014.05.112. [DOI] [PubMed] [Google Scholar]
- 42.Montserrat de la Paz S., Lemus-Conejo A., Toscano R., Pedroche J., Millan F., Millan-Linares M.C. GPETAFLR, an Octapeptide Isolated from Lupinus Angustifolius L. Protein Hydrolysate, Promotes the Skewing to the M2 Phenotype in Human Primary Monocytes. Food Funct. 2019;10:3303–3311. doi: 10.1039/C9FO00115H. [DOI] [PubMed] [Google Scholar]
- 43.Kovacs-Nolan J., Zhang H., Ibuki M., Nakamori T., Yoshiura K., Turner P.V., Matsui T., Mine Y. The PepT1-Transportable Soy Tripeptide VPY Reduces Intestinal Inflammation. Biochim. Biophys. Acta BBA Gen. Subj. 2012;1820:1753–1763. doi: 10.1016/j.bbagen.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 44.Chataigner M., Mortessagne P., Lucas C., Pallet V., Layé S., Mehaignerie A., Bouvret E., Dinel A.L., Joffre C. Dietary Fish Hydrolysate Supplementation Containing N-3 LC-PUFAs and Peptides Prevents Short-Term Memory and Stress Response Deficits in Aged Mice. Brain Behav. Immun. 2020;91:716–730. doi: 10.1016/j.bbi.2020.09.022. [DOI] [PubMed] [Google Scholar]
- 45.Belhaj N., Desor F., Gleizes C., Denis F.M., Arab-Tehrany E., Soulimani R., Linder M. Anxiolytic-like Effect of a Salmon Phospholipopeptidic Complex Composed of Polyunsaturated Fatty Acids and Bioactive Peptides. Mar. Drugs. 2013;11:4294–4317. doi: 10.3390/md11114294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Poncin-Séac’h M., Le Poncin-Lafitte C. Effets Sur Les Fonctions Cognitives et Mnésiques de Sujets Sains d’un Hydrolysat de Protéines Xde Poisson (FPHD!Àà): Étude Comparative Avec Le Ginkgo Biloba (EGB 761®) Méd. Longév. 2010;2:57–67. doi: 10.1016/j.mlong.2010.04.004. [DOI] [Google Scholar]
- 47.Mingam R., Moranis A., Bluthé R.-M., De Smedt-Peyrusse V., Kelley K.W., Guesnet P., Lavialle M., Dantzer R., Layé S. Uncoupling of Interleukin-6 from Its Signalling Pathway by Dietary n-3-Polyunsaturated Fatty Acid Deprivation Alters Sickness Behaviour in Mice. Eur. J. Neurosci. 2008;28:1877–1886. doi: 10.1111/j.1460-9568.2008.06470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simões A.E., Pereira D.M., Amaral J.D., Nunes A.F., Gomes S.E., Rodrigues P.M., Lo A.C., D’Hooge R., Steer C.J., Thibodeau S.N., et al. Efficient Recovery of Proteins from Multiple Source Samples after Trizol® or Trizol®LS RNA Extraction and Long-Term Storage. BMC Genom. 2013;14:181. doi: 10.1186/1471-2164-14-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Labrousse V.F., Nadjar A., Joffre C., Costes L., Aubert A., Grégoire S., Bretillon L., Layé S. Short-Term Long Chain Omega3 Diet Protects from Neuroinflammatory Processes and Memory Impairment in Aged Mice. PLoS ONE. 2012;7:e36861. doi: 10.1371/journal.pone.0036861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lafourcade M., Larrieu T., Mato S., Duffaud A., Sepers M., Matias I., De Smedt-Peyrusse V., Labrousse V.F., Bretillon L., Matute C., et al. Nutritional Omega-3 Deficiency Abolishes Endocannabinoid-Mediated Neuronal Functions. Nat. Neurosci. 2011;14:345–350. doi: 10.1038/nn.2736. [DOI] [PubMed] [Google Scholar]
- 51.Larrieu T., Madore C., Joffre C., Layé S. Nutritional N-3 Polyunsaturated Fatty Acids Deficiency Alters Cannabinoid Receptor Signaling Pathway in the Brain and Associated Anxiety-like Behavior in Mice. J. Physiol. Biochem. 2012;68:671–681. doi: 10.1007/s13105-012-0179-6. [DOI] [PubMed] [Google Scholar]
- 52.Le Faouder P., Baillif V., Spreadbury I., Motta J.-P., Rousset P., Chêne G., Guigné C., Tercé F., Vanner S., Vergnolle N., et al. LC-MS/MS Method for Rapid and Concomitant Quantification of pro-Inflammatory and pro-Resolving Polyunsaturated Fatty Acid Metabolites. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2013;932:123–133. doi: 10.1016/j.jchromb.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 53.Bara O., Day J., Djouadi S.M. Nonlinear State Estimation for Complex Immune Responses; Proceedings of the 52nd IEEE Conference on Decision and Control; Florence, Italy. 10–13 December 2013; pp. 3373–3378. [Google Scholar]
- 54.Serhan C.N. Pro-Resolving Lipid Mediators Are Leads for Resolution Physiology. Nature. 2014;510:92–101. doi: 10.1038/nature13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Serhan C.N., Savill J. Resolution of Inflammation: The Beginning Programs the End. Nat. Immunol. 2005;6:1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- 56.Barnig C., Bezema T., Calder P.C., Charloux A., Frossard N., Garssen J., Haworth O., Dilevskaya K., Levi-Schaffer F., Lonsdorfer E., et al. Activation of Resolution Pathways to Prevent and Fight Chronic Inflammation: Lessons from Asthma and Inflammatory Bowel Disease. Front. Immunol. 2019;10:1699. doi: 10.3389/fimmu.2019.01699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Doyle S.L., O’Neill L.A.J. Toll-like Receptors: From the Discovery of NFkappaB to New Insights into Transcriptional Regulations in Innate Immunity. Biochem. Pharmacol. 2006;72:1102–1113. doi: 10.1016/j.bcp.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 58.Butovsky O., Weiner H.L. Microglial Signatures and Their Role in Health and Disease. Nat. Rev. Neurosci. 2018;19:622–635. doi: 10.1038/s41583-018-0057-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cherry J.D., Olschowka J.A., O’Banion M.K. Neuroinflammation and M2 Microglia: The Good, the Bad, and the Inflamed. J. Neuroinflamm. 2014;11:98. doi: 10.1186/1742-2094-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hanisch U.-K. Functional Diversity of Microglia—How Heterogeneous Are They to Begin With? Front. Cell Neurosci. 2013;7:65. doi: 10.3389/fncel.2013.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Czapski G.A., Gajkowska B., Strosznajder J.B. Systemic Administration of Lipopolysaccharide Induces Molecular and Morphological Alterations in the Hippocampus. Brain Res. 2010;1356:85–94. doi: 10.1016/j.brainres.2010.07.096. [DOI] [PubMed] [Google Scholar]
- 62.Farooqui A.A., Horrocks L.A., Farooqui T. Modulation of Inflammation in Brain: A Matter of Fat. J. Neurochem. 2007;101:577–599. doi: 10.1111/j.1471-4159.2006.04371.x. [DOI] [PubMed] [Google Scholar]
- 63.Nadjar A., Tridon V., May M.J., Ghosh S., Dantzer R., Amédée T., Parnet P. NFkappaB Activates in Vivo the Synthesis of Inducible Cox-2 in the Brain. J. Cereb. Blood Flow Metab. 2005;25:1047–1059. doi: 10.1038/sj.jcbfm.9600106. [DOI] [PubMed] [Google Scholar]
- 64.Rivest S. Activation of the Nuclear Factor Kappa B (NF-KappaB) and Cyclooxygenase-2 (COX-2) Genes in Cerebral Blood Vessels in Response to Systemic Inflammation. Mol. Psychiatry. 1999;4:500. doi: 10.1038/sj.mp.4000679. [DOI] [PubMed] [Google Scholar]
- 65.Yamamoto S., Yamamoto K., Kurobe H., Yamashita R., Yamaguchi H., Ueda N. Transcriptional Regulation of Fatty Acid Cyclooxygenases-1 and -2. Int. J. Tissue React. 1998;20:17–22. [PubMed] [Google Scholar]
- 66.Delpech J.-C., Thomazeau A., Madore C., Bosch-Bouju C., Larrieu T., Lacabanne C., Remus-Borel J., Aubert A., Joffre C., Nadjar A., et al. Dietary N-3 PUFAs Deficiency Increases Vulnerability to Inflammation-Induced Spatial Memory Impairment. Neuropsychopharmacology. 2015;40:2774–2787. doi: 10.1038/npp.2015.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Marcheselli V.L., Hong S., Lukiw W.J., Tian X.H., Gronert K., Musto A., Hardy M., Gimenez J.M., Chiang N., Serhan C.N., et al. Novel Docosanoids Inhibit Brain Ischemia-Reperfusion-Mediated Leukocyte Infiltration and Pro-Inflammatory Gene Expression. J. Biol. Chem. 2003;278:43807–43817. doi: 10.1074/jbc.M305841200. [DOI] [PubMed] [Google Scholar]
- 68.Orr S.K., Palumbo S., Bosetti F., Mount H.T., Kang J.X., Greenwood C.E., Ma D.W.L., Serhan C.N., Bazinet R.P. Unesterified Docosahexaenoic Acid Is Protective in Neuroinflammation. J. Neurochem. 2013;127:378–393. doi: 10.1111/jnc.12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shi Z., Ren H., Huang Z., Peng Y., He B., Yao X., Yuan T.-F., Su H. Fish Oil Prevents Lipopolysaccharide-Induced Depressive-Like Behavior by Inhibiting Neuroinflammation. Mol. Neurobiol. 2017;54:7327–7334. doi: 10.1007/s12035-016-0212-9. [DOI] [PubMed] [Google Scholar]
- 70.Desai A., Park T., Barnes J., Kevala K., Chen H., Kim H.-Y. Reduced Acute Neuroinflammation and Improved Functional Recovery after Traumatic Brain Injury by α-Linolenic Acid Supplementation in Mice. J. Neuroinflamm. 2016;13:253. doi: 10.1186/s12974-016-0714-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ajmone-Cat M.A., Salvatori M.L., Simone R.D., Mancini M., Biagioni S., Bernardo A., Cacci E., Minghetti L. Docosahexaenoic Acid Modulates Inflammatory and Antineurogenic Functions of Activated Microglial Cells. J. Neurosci. Res. 2012;90:575–587. doi: 10.1002/jnr.22783. [DOI] [PubMed] [Google Scholar]
- 72.Chang P.K.-Y., Khatchadourian A., McKinney R.A., Maysinger D. Docosahexaenoic Acid (DHA): A Modulator of Microglia Activity and Dendritic Spine Morphology. J. Neuroinflamm. 2015;12:34. doi: 10.1186/s12974-015-0244-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen J., Wei Y., Chen X., Jiao J., Zhang Y. Polyunsaturated Fatty Acids Ameliorate Aging via Redox-Telomere-Antioncogene Axis. Oncotarget. 2017;8:7301–7314. doi: 10.18632/oncotarget.14236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.De Smedt-Peyrusse V.D., Sargueil F., Moranis A., Harizi H., Mongrand S., Layé S. Docosahexaenoic Acid Prevents Lipopolysaccharide-Induced Cytokine Production in Microglial Cells by Inhibiting Lipopolysaccharide Receptor Presentation but Not Its Membrane Subdomain Localization. J. Neurochem. 2008;105:296–307. doi: 10.1111/j.1471-4159.2007.05129.x. [DOI] [PubMed] [Google Scholar]
- 75.Lu Y., Zhao L.-X., Cao D.-L., Gao Y.-J. Spinal Injection of Docosahexaenoic Acid Attenuates Carrageenan-Induced Inflammatory Pain through Inhibition of Microglia-Mediated Neuroinflammation in the Spinal Cord. Neuroscience. 2013;241:22–31. doi: 10.1016/j.neuroscience.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 76.Ma Q.-L., Yang F., Rosario E.R., Ubeda O.J., Beech W., Gant D.J., Chen P.P., Hudspeth B., Chen C., Zhao Y., et al. Beta-Amyloid Oligomers Induce Phosphorylation of Tau and Inactivation of Insulin Receptor Substrate via c-Jun N-Terminal Kinase Signaling: Suppression by Omega-3 Fatty Acids and Curcumin. J. Neurosci. 2009;29:9078–9089. doi: 10.1523/JNEUROSCI.1071-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Belayev L., Khoutorova L., Atkins K.D., Eady T.N., Hong S., Lu Y., Obenaus A., Bazan N.G. Docosahexaenoic Acid Therapy of Experimental Ischemic Stroke. Transl. Stroke Res. 2011;2:33–41. doi: 10.1007/s12975-010-0046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chang C.-Y., Kuan Y.-H., Li J.-R., Chen W.-Y., Ou Y.-C., Pan H.-C., Liao S.-L., Raung S.-L., Chang C.-J., Chen C.-J. Docosahexaenoic Acid Reduces Cellular Inflammatory Response Following Permanent Focal Cerebral Ischemia in Rats. J. Nutr. Biochem. 2013;24:2127–2137. doi: 10.1016/j.jnutbio.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 79.Chen S., Zhang H., Pu H., Wang G., Li W., Leak R.K., Chen J., Liou A.K., Hu X. N-3 PUFA Supplementation Benefits Microglial Responses to Myelin Pathology. Sci. Rep. 2014;4:7458. doi: 10.1038/srep07458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eady T.N., Belayev L., Khoutorova L., Atkins K.D., Zhang C., Bazan N.G. Docosahexaenoic Acid Signaling Modulates Cell Survival in Experimental Ischemic Stroke Penumbra and Initiates Long-Term Repair in Young and Aged Rats. PLoS ONE. 2012;7:e46151. doi: 10.1371/journal.pone.0046151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Eady T.N., Khoutorova L., Atkins K.D., Bazan N.G., Belayev L. Docosahexaenoic Acid Complexed to Human Albumin in Experimental Stroke: Neuroprotective Efficacy with a Wide Therapeutic Window. Exp. Transl. Stroke Med. 2012;4:19. doi: 10.1186/2040-7378-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hjorth E., Zhu M., Toro V.C., Vedin I., Palmblad J., Cederholm T., Freund-Levi Y., Faxen-Irving G., Wahlund L.-O., Basun H., et al. Omega-3 Fatty Acids Enhance Phagocytosis of Alzheimer’s Disease-Related Amyloid-β 42 by Human Microglia and Decrease Inflammatory Markers. J. Alzheimer’s Dis. 2013;35:697–713. doi: 10.3233/JAD-130131. [DOI] [PubMed] [Google Scholar]
- 83.Manzhulo O., Tyrtyshnaia A., Kipryushina Y., Dyuizen I., Manzhulo I. Docosahexaenoic Acid Induces Changes in Microglia/Macrophage Polarization after Spinal Cord Injury in Rats. Acta Histochem. 2018;120:741–747. doi: 10.1016/j.acthis.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 84.Serhan C.N., Hong S., Gronert K., Colgan S.P., Devchand P.R., Mirick G., Moussignac R.-L. Resolvins: A Family of Bioactive Products of Omega-3 Fatty Acid Transformation Circuits Initiated by Aspirin Treatment that Counter Proinflammation Signals. J. Exp. Med. 2002;196:1025–1037. doi: 10.1084/jem.20020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Serhan C.N., Yacoubian S., Yang R. Anti-Inflammatory and Proresolving Lipid Mediators. Annu. Rev. Pathol. 2008;3:279–312. doi: 10.1146/annurev.pathmechdis.3.121806.151409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lukiw W.J., Cui J.-G., Marcheselli V.L., Bodker M., Botkjaer A., Gotlinger K., Serhan C.N., Bazan N.G. A Role for Docosahexaenoic Acid-Derived Neuroprotectin D1 in Neural Cell Survival and Alzheimer Disease. J. Clin. Investig. 2005;115:2774–2783. doi: 10.1172/JCI25420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Orr S.K., Bazinet R.P. The Emerging Role of Docosahexaenoic Acid in Neuroinflammation. Curr. Opin. Investig. Drugs. 2008;9:735–743. [PubMed] [Google Scholar]
- 88.Dalli J., Zhu M., Vlasenko N.A., Deng B., Haeggström J.Z., Petasis N.A., Serhan C.N. The Novel 13S,14S-Epoxy-Maresin Is Converted by Human Macrophages to Maresin 1 (MaR1), Inhibits Leukotriene A4 Hydrolase (LTA4H), and Shifts Macrophage Phenotype. FASEB J. 2013;27:2573–2583. doi: 10.1096/fj.13-227728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Serhan C.N., Yang R., Martinod K., Kasuga K., Pillai P.S., Porter T.F., Oh S.F., Spite M. Maresins: Novel Macrophage Mediators with Potent Antiinflammatory and Proresolving Actions. J. Exp. Med. 2009;206:15–23. doi: 10.1084/jem.20081880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Francos-Quijorna I., Santos-Nogueira E., Gronert K., Sullivan A.B., Kopp M.A., Brommer B., David S., Schwab J.M., López-Vales R. Maresin 1 Promotes Inflammatory Resolution, Neuroprotection, and Functional Neurological Recovery After Spinal Cord Injury. J. Neurosci. 2017;37:11731–11743. doi: 10.1523/JNEUROSCI.1395-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xian W., Wu Y., Xiong W., Li L., Li T., Pan S., Song L., Hu L., Pei L., Yao S., et al. The Pro-Resolving Lipid Mediator Maresin 1 Protects against Cerebral Ischemia/Reperfusion Injury by Attenuating the pro-Inflammatory Response. Biochem. Biophys. Res. Commun. 2016;472:175–181. doi: 10.1016/j.bbrc.2016.02.090. [DOI] [PubMed] [Google Scholar]
- 92.Xian W., Li T., Li L., Hu L., Cao J. Maresin 1 Attenuates the Inflammatory Response and Mitochondrial Damage in Mice with Cerebral Ischemia/Reperfusion in a SIRT1-Dependent Manner. Brain Res. 2019;1711:83–90. doi: 10.1016/j.brainres.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 93.Zhao Y., Calon F., Julien C., Winkler J.W., Petasis N.A., Lukiw W.J., Bazan N.G. Docosahexaenoic Acid-Derived Neuroprotectin D1 Induces Neuronal Survival via Secretase- and PPARγ-Mediated Mechanisms in Alzheimer’s Disease Models. PLoS ONE. 2011;6:e15816. doi: 10.1371/journal.pone.0015816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Abdelmoaty S., Wigerblad G., Bas D.B., Codeluppi S., Fernandez-Zafra T., El-Awady E.-S., Moustafa Y., Abdelhamid A.E.S., Brodin E., Svensson C.I. Spinal Actions of Lipoxin A4 and 17(R)-Resolvin D1 Attenuate Inflammation-Induced Mechanical Hypersensitivity and Spinal TNF Release. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0075543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Luo C.-L., Li Q.-Q., Chen X.-P., Zhang X.-M., Li L.-L., Li B.-X., Zhao Z.-Q., Tao L.-Y. Lipoxin A4 Attenuates Brain Damage and Downregulates the Production of Pro-Inflammatory Cytokines and Phosphorylated Mitogen-Activated Protein Kinases in a Mouse Model of Traumatic Brain Injury. Brain Res. 2013;1502:1–10. doi: 10.1016/j.brainres.2013.01.037. [DOI] [PubMed] [Google Scholar]
- 96.Medeiros R., Kitazawa M., Passos G.F., Baglietto-Vargas D., Cheng D., Cribbs D.H., LaFerla F.M. Aspirin-Triggered Lipoxin A4 Stimulates Alternative Activation of Microglia and Reduces Alzheimer Disease-Like Pathology in Mice. Am. J. Pathol. 2013;182:1780–1789. doi: 10.1016/j.ajpath.2013.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Walker J., Dichter E., Lacorte G., Kerner D., Spur B., Rodriguez A., Yin K. Lipoxin A4 Increases Survival by Decreasing Systemic Inflammation and Bacterial Load in Sepsis. Shock. 2011;36:410–416. doi: 10.1097/SHK.0b013e31822798c1. [DOI] [PubMed] [Google Scholar]
- 98.Guo Z., Hu Q., Xu L., Guo Z.-N., Ou Y., He Y., Yin C., Sun X., Tang J., Zhang J.H. Lipoxin A4 Reduces Inflammation through Formyl Peptide Receptor 2/P38 MAPK Signaling Pathway in Subarachnoid Hemorrhage Rats. Stroke. 2016;47:490–497. doi: 10.1161/STROKEAHA.115.011223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Martini A.C., Berta T., Forner S., Chen G., Bento A.F., Ji R.-R., Rae G.A. Lipoxin A4 Inhibits Microglial Activation and Reduces Neuroinflammation and Neuropathic Pain after Spinal Cord Hemisection. J. Neuroinflamm. 2016;13:75. doi: 10.1186/s12974-016-0540-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang Y.-P., Wu Y., Li L.-Y., Zheng J., Liu R.-G., Zhou J.-P., Yuan S.-Y., Shang Y., Yao S.-L. Aspirin-Triggered Lipoxin A4 Attenuates LPS-Induced pro-Inflammatory Responses by Inhibiting Activation of NF-ΚB and MAPKs in BV-2 Microglial Cells. J. Neuroinflamm. 2011;8:95. doi: 10.1186/1742-2094-8-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hampson A.J., Grimaldi M. 12-Hydroxyeicosatetrenoate (12-HETE) Attenuates AMPA Receptor-Mediated Neurotoxicity: Evidence for a G-Protein-Coupled HETE Receptor. J. Neurosci. 2002;22:257–264. doi: 10.1523/JNEUROSCI.22-01-00257.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sun L., Xu Y.-W., Han J., Liang H., Wang N., Cheng Y. 12/15-Lipoxygenase Metabolites of Arachidonic Acid Activate PPARγ: A Possible Neuroprotective Effect in Ischemic Brain. J. Lipid Res. 2015;56:502–514. doi: 10.1194/jlr.M053058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.