Abstract
Objective: To evaluate the influence of conventional rehabilitation combined with virtual reality on improving quality of life related to post-stroke health. Design: Randomized controlled trial. Setting: Rehabilitation and neurology departments of a general hospital (Talavera de la Reina, Spain). Subjects: A total of 43 participants with subacute stroke. Intervention: Participants were randomized into experimental group (conventional treatment + virtual reality) and control (conventional treatment). Main measures: Health-related quality of life as measured by the EuroQoL-5 dimensions instrument (EQ-5D-5L) and EuroQoL visual analog scale (EQ-VAS). Results: A total of 23 patients in the experimental group (62.6 ± 13.5 years) and 20 in the control (63.6 ± 12.2 years) completed the study. In the experimental group, EQ-VAS score was 29.1 ± 12.8 at baseline, 86.5 ± 7.1 post-intervention, and 78.3 ± 10.3 at the three-month follow-up. The control group obtained scores of 25.5 ± 5.1, 57.0 ± 4.7, and 58.5 ± 5.9, respectively. We identified significant differences at the post-intervention and follow-up timepoints (p = 0.000) and a partial η2 of 0.647. In EQ-5D-5L, the severity of issues decreased after intervention in the experimental group, while pain and anxiety dimensions increased between post-intervention and follow-up. Conclusions: The conventional rehabilitative approach combined with virtual reality appears to be more effective for improving the perceived health-related quality of life in stroke survivors.
Keywords: stroke, virtual reality, quality of life, occupational therapy, randomized controlled trial
1. Introduction
Stroke is one of the world’s leading health problems and a major cause of acquired disability in adults [1,2]. Motor and sensory deficits are common in stroke patients, producing disorders of motor control, balance, and gait [3]. An estimated 80% of the survivors present motor difficulties in the upper extremities, affecting their execution of activities of daily living, performance in the community, and health-related quality of life (HRQoL) [4,5,6]. In addition, alterations in body alignment occur, requiring the incorporation of treatment strategies focused on improving the postural control and symmetry of weight bearing [7,8,9]. The multidimensional impact of the diagnosis on survivors is of vital importance for their functional recovery, and cannot be explained exclusively by clinical variables. Measures of perceived health status, social participation, and HRQoL are increasingly used as part of a person-centered assessment process, reflecting the interaction between health determinants and physical, social, and emotional functions [10,11]. HRQoL is an important factor, together with the increase in life expectancy, the chronification of pathologies, and the achievement of health policies focused on the patient’s subjective wellbeing and satisfaction after completing the intervention processes [2,12,13,14]. The EuroQoL-5 dimensions instrument (EQ-5D-5L) is useful for evaluating HRQoL over time, comparing the evolution between groups and calculating the cost-effectiveness and/or effectiveness of the administered interventions [15,16].
In recent years, the use of neurorehabilitation approaches based on technology and virtual reality (VR) has increased, allowing the creation of effective rehabilitation environments and providing multimodal, controllable, and customizable stimulation [17]. In these simulations, the recreation of virtual objects maximizes visual feedback [18], and a high intensity and high number of repetitions fundamentally influence neuroplasticity and functional improvement of the patients [19]. VR-based rehabilitation offers the possibility to individualize treatment needs and, at the same time, standardize assessment and training protocols [20,21]. In this sense, it should be noted that virtual reality technology, specifically for rehabilitation processes for people with neurological pathologies, makes it possible to work in a functional way and with specific intervention objectives, as well as to easily qualify and document the progress made during the session [22].
The present study aims to examine the effect of a combined treatment of conventional therapy with virtual reality on HRQoL of people diagnosed with stroke in the acute phase and its evolution after three months in the integrated health area of Talavera de la Reina.
2. Materials and Methods
2.1. Study Design
This study began in April 2018 and was completed by March 2020. It adhered to the standards of the Declaration of Helsinki and was approved by the Research Ethics and Medicines Committee (CEIm) of the integrated health area of Talavera de la Reina (12/2018). The study was registered in the trial registry ISRCTN (ISRCTN27760662) [23]. All participants received verbal and written information about the study and gave their written informed consent.
This randomized controlled trial compared conventional rehabilitation of physical therapy and occupational therapy (control group) and the combination of conventional rehabilitation with the use of virtual reality technology (experimental group), following the guidelines of the Consolidated Standards of Reporting Trials (CONSORT) [24]. The change in HRQoL (baseline, post-intervention, and three-month follow-up) was used as the primary outcome. The evaluation of the post-intervention variables was completed three weeks after the start of treatment in both groups (after receiving 15 treatment sessions).
The participants were recruited from the neurology and rehabilitation units of the University General Hospital of Talavera de la Reina, Spain. They were assigned randomly to the control or experimental group by an external researcher to the intervention and evaluation process (allocation ratio of 1:1). The conventional rehabilitation therapists were blinded to the study, but the intervention could not be blinded to the participants or to the therapist who applied the combined treatment.
2.2. Participant and Settings
The study included 46 patients (of whom 43 completed the intervention period and follow-up evaluation) who attended the hospital rehabilitation unit (mean age: 63.1; % of women: 18.6), who had been diagnosed with stroke and met the following inclusion criteria: (1) age: 18 to 85 years; (2) maximum evolution time of six months; (3) upper limb motor involvement; (4) dependence in activities of daily living (Stroke Impact Scale; version 3.0); (5) life expectancy greater than six months (absence of life-threatening diagnoses such as end-stage cancer); and (6) absence of other serious and disabling pathologies. Four exclusion criteria were defined: presence of other neurological diagnoses, severe hemineglect, psychiatric pathologies, and signed revocation of informed consent.
2.3. Intervention
All study participants received 15 treatment sessions with a duration of 150 min per session over five consecutive days per week. In total, the intervention lasted three weeks per participant. The patients assigned to the experimental group combined conventional upper and lower limb strength and motor training (100 min; guided by the hospital’s physiotherapy and occupational therapy team) with the use of virtual reality technological devices (50 min), while the participants in the control group received conventional physiotherapy and occupational therapy of 75 min each.
The conventional intervention protocol consisted of receiving manual therapy techniques (massage); passive and active assisted mobilization of the upper and lower limbs; walking in parallel, on slope and stairs; exercises with and without resistance with balls, elastic bands, and dumbbells in therapeutic cage and trellises; active-assisted mobility exercises of the upper limb and fingers in a sitting position; moving objects horizontally on a table; elevation and superposition of objects in vertical plane; biomechanical tasks that simulate flexion–extension and abduction–adduction of the shoulder and flexion–extension of the wrist and fingers.
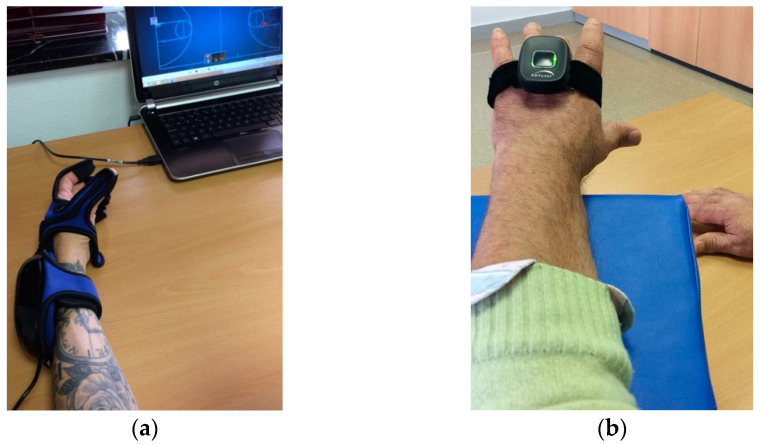
Motor training with virtual reality devices consisted of several systems: First, the HandTutor© glove (Figure 1a) [25,26] for hand rehabilitation and 3DTutor© (Figure 1b) for upper extremities [21]. Both systems are based on intensive and repetitive practice through movement and feedback instructions provided by the software with virtual environments and tasks that simulate movements that stroke survivors require for daily life [27,28,29]. The glove allows the blocking of compensatory joint movements and ensures a better adaptation to functional tasks (for example, active joint range movement can be limited). It focuses on flexion–extension of fingers and wrist [30]. The 3DTutor© allows the therapist to focus on training all movements of the head, trunk, shoulder, elbow, wrist, hip, knee, and ankle joints [31]. Second, the Rehametrics© software [32] + Microsoft Kinect sensor [33,34,35] was used for the recovery of the upper limb (elbow and shoulder), trunk, and lower body, which simulates activities of daily living and mobility in the community with virtual environments and in combination with the use of gamification. It monitors and captures the user’s movement in real time and allows the therapist to adjust and customize the difficulty, duration, range of motion, and the number of distracting or visual aids.
Figure 1.
(a) HandTutor© glove (flexion–extension of the fingers); (b) 3DTutor© (wrist extension).
The baseline and post-interventional assessments and the three-month follow-up were conducted by the same researcher in both groups.
2.4. Outcomes Measures
The primary outcome variable for this study was HRQoL. For its quantification, we applied the EQ-5D-5L instrument, which is widely used in the literature [36]. It is quick and easily applied, validated in Spanish, and reliable in both healthy and symptomatic populations [37,38]. It consists of five dimensions (descriptive system) that assess mobility, personal care, activities of daily living, pain/discomfort, and anxiety/depression, assigning to each dimension the following response categories (level of severity): no problems, mild/moderate problems, and severe problems/inability to perform the activity. In addition, it uses the EuroQoL visual analog scale (EQ-VAS) for self-assessment of the state of improvement and/or health condition, in which it scores from 0 (minimum) to 100 (maximum). The reliability of the EQ-5D-5L test was r = 0.90 and that of EQ-VAS r = 0.86 [39,40]. In addition, sociodemographic and clinical data were recorded, such as age, sex, time elapsed since diagnosis, location of the lesion, risk factors, dominance, pain, or mild hemispatial neglect syndrome. HRQoL was recorded before starting the treatment (baseline), three weeks after the start (post-intervention), and three months after its completion (follow-up).
2.5. Statistical Analysis
The sample size was calculated using the Epidat 4.2 program. An effectiveness ratio of 90% was estimated for the experimental group and 50% for the control group. Using a power of 80% and a confidence level of 95% (p < 0.05), a minimum sample size of 20 participants was obtained in each group. The data were analyzed with the IBM SPSS statistical package (version 24.0) (IBM, S.A., Madrid, Spain.). To compare the clinical and sociodemographic variables of the intervention groups, Student’s t and chi-square tests were used. Differences in baseline HRQoL, post-intervention, and three-month follow-up scores were analyzed with inter- and intragroup ANOVA, Student’s t test, and the chi-square test. The clinically relevant improvement was defined by Robinson et al. [41] as 0.05 points [42]. Statistical significance was set at a p-value below 0.05.
The analysis of missing data from the control group was carried out with multiple imputation in the analysis (expectation maximization and regression method), with a little’s chi-square statistic 14,247 (degree freedom = 19; p = 0.769).
The investigator who performed the statistical analysis was unaware of the random assignment of participants to the intervention groups.
3. Results
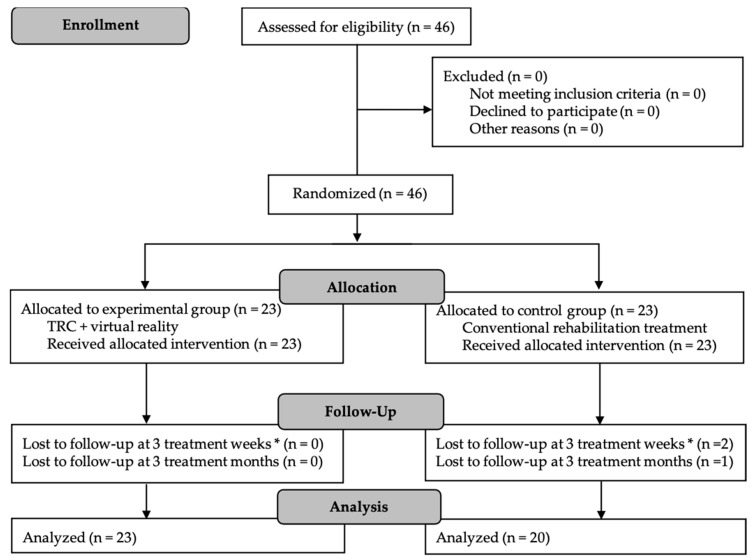
A total of 46 patients were selected for randomization, of whom 43 completed the intervention period and follow-up evaluation. A total of 23 participants were assigned to the experimental group and 23 to the control group. Three participants were lost in the control group, as a consequence of the start of the COVID-19 pandemic in Spain (Figure 2).
Figure 2.
CONSORT Flow Diagram for participant recruitment, allocation, follow-up and analysis. TRC: conventional rehabilitation treatment. * Post-intervention evaluation.
The sociodemographic and clinical characteristics of the participants are shown in Table 1. Significant differences are observed in the evolution of pain between both groups, which decreased considerably after the intervention in the experimental group. A total of 15.0% (n = 3) of the participants in the control group registered a change in dominance (from right to left) post-intervention, while the experimental group maintained baseline dominance. A total of 43.5% (n = 10) in the experimental group and 30.0% (n = 6) in the control group were diagnosed with arterial hypertension, which thus constituted the main risk factor.
Table 1.
Characteristics of the participants of both groups (n = 43).
| Study Variables | Experimental Group (n = 23) |
Control Group (n = 20) |
Difference of Mean between Groups (p-Value) |
|---|---|---|---|
| Age | |||
| Mean (SD) Below 55 years (%) 55 to 70 years (%) Above 70 years (%) |
62.6 (13.5) 26.1 30.4 43.5 |
63.6 (12.2) 25.0 45.0 30.0 |
−0.9 (0.812) 0.566 |
| Sex | |||
| Male Female |
78.3 21.7 |
85.0 15.0 |
0.571 |
| Main diagnostic | |||
| Ischemic/thrombotic Hemorrhagic |
91.3 8.7 |
90.0 10.0 |
0.883 |
| Middle cerebral artery lesion (%) | 60.9 | 55.0 | 0.697 |
| Time since diagnostic (days) * | |||
| Baseline (pre-intervention) Post-intervention (3 week follow-up) Follow-up (3 months) |
55.3 (34.3) 75.3 (34.3) 162.3 (36.9) |
54.2 (30.4) 74.2 (30.4) 157.2 (36.1) |
1.1 (0.909) 1.1 (0.909) 5.1 (0.650) |
| Hemispatial neglect syndrome (%) | 13.0 | 10.0 | 0.756 |
| Presence of pain in extremities | |||
| Baseline (pre-intervention) Post-intervention (3 week follow-up) Follow-up (3 months) |
43.5 21.7 82.6 |
50.0 80.0 100.0 |
0.669
0.000 0.050 |
| Location of the brain injury (%) | |||
| Right Left |
82.6 17.4 |
85.0 15.0 |
0.832 |
| Dominance (change baseline to post-intervention) | |||
| Right Left |
100.0/100.0 0 |
100.0/85.0 0/15.0 |
0.054 |
* Mean (SD). p-value: Student’s t-test for independent samples in continuous variables/Pearson’s chi-squared test.
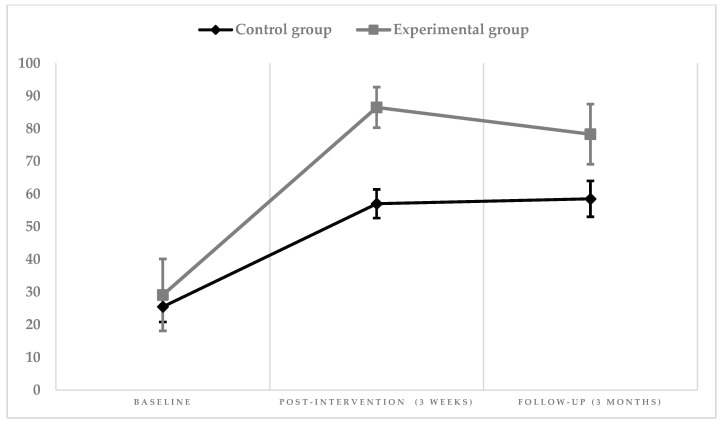
Table 2 shows the differences in the evolution of EQ-VAS results between groups. An increase of the score is observed in both groups; however, it was notably higher in the experimental group (mean score at baseline 29.1 to post-intervention 86.5). During follow-up, the mean score of the control group remained stable, whereas the score in the experimental group decreased slightly (post-intervention 86.5 to follow-up 78.3) (Figure 3).
Table 2.
Linear model. Effect of the intervention on EuroQoL visual analog scale (EQ-VAS) results.
| Intervention Group | Difference Follow-Up/Baseline | ||||||
|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) | Post-Intervention Mean (SD) | Follow-Up Mean (SD) | Mean (CI95%) | ANOVA | |||
| F | p | η2 Parcial | |||||
| EQ-VAS (T-score) | |||||||
| Experimental group | 29.1 (12.8) | 86.5 (7.1) | 78.3 (10.7) | 49.2 (42.2–56.0) * | |||
| Control group | 25.5 (5.1) | 57.0 (4.7) | 58.5 (5.9) | 33.0 (29.1–36.8) * | 75.2 | 0.000 | 0.647 |
| p | 0.241 | 0.000 | 0.000 | ||||
SD: Standard deviation. CI95%: 95% confidence interval. Partial η2: magnitude of effect. * The difference in means is significant at level 0.000. p-value: italics.
Figure 3.
Graphic representation of the intervention’s effect on EQ-VAS.
The magnitude of the effect of the experimental intervention is large and statistically significant.
The differences in the EQ-5D-5L HRQoL results between groups are shown in Table 3. We observed an effect of the experimental intervention on the frequency distribution in all dimensions, with statistically significant differences between baseline, post-intervention, and follow-up, except for pain/discomfort (baseline: 0.562; three-month follow-up: 0.147). Marked was the increased severity of issues of pain and anxiety dimensions of the experimental group between the post-intervention and the follow-up (pain: from 21.7 to 82.6; anxiety: from 8.7 to 65.2).
Table 3.
Difference in the EuroQoL-5 dimensions instrument (EQ-5D-5L) frequency distribution according to intervention group.
| EuroQoL-5 Dimensions Instrument | Baseline (n = 43) % |
Post-Intervention (n = 43) % |
Follow-Up (n = 43) % |
||||||
|---|---|---|---|---|---|---|---|---|---|
| CG (n) | EG (n) | p | CG (n) | EG (n) | p | CG (n) | EG (n) | p | |
| D1. Mobility | |||||||||
| (1) (2) (3) |
0 60.0 (12) 40.0 (8) |
0 21.7 (5) 78.3 (18) |
0.011 | 0 90.0 (18) 10.0 (2) |
43.5 (10) 56.5 (13) 0 |
0.002 | 0 90.0 (18) 10.0 (2) |
39.1 (9) 60.9 (14) 0 |
0.007 |
| D2. Selfcare | |||||||||
| (1) (2) (3) |
0 60.0 (12) 40.0 (8) |
0 21.7 (5) 78.3 (18) |
0.011 | 20.0 (4) 80.0 (16) 0 |
60.9 (14) 39.1 (9) 0 |
0.014 | 25.0 (5) 75.0 (15) 0 |
65.2 (15) 34.8 (8) 0 |
0.014 |
| D3. Daily activities | |||||||||
| (1) (2) (3) |
0 20.0 (4) 80.0 (16) |
0 21.7 (5) 78.3 (18) |
0.019 | 0 100.0 (20) 0 |
34.8 (8) 65.2 (15) 0 |
0.000 | 0 100.0 (20) 0 |
34.8 (8) 65.2 (15) 0 |
0.000 |
| D4. Pain/discomfort | |||||||||
| (1) (2) (3) |
50.0 (10)45.0 (9)5.0 (1) | 56.5 (13)26.2 (6)17.3 (4) | 0.562 | 0100.0 (20)0 | 78.3 (18) 21.7 (5) 0 |
0.000 | 0 95.0 (19) 5.0 (1) |
17.4 (4) 82.6 (19) 0 |
0.147 |
| D5. Anxiety/depression | |||||||||
| (1) (2) (3) |
0 85.0 (17) 15.0 (3) |
0 78.3 (18) 21.7 (5) |
0.090 | 0 100.0 (20) 0 |
91.3 (21) 8.7 (2) 0 |
0.000 | 0 65.0 (13) 35.0 (7) |
30.4 (7) 65.2 (15) 4.4 (1) |
0.005 |
CG: control group; EG: experimental group. (1) No problems; (2) mild and moderate problems; (3) severe, extreme problems and incapacity (15). EQ-5D-5L: descriptive system (5 dimensions). p-value: chi-squared test.
4. Discussion
This randomized controlled trial examined the effects of treatment based on virtual reality combined with conventional rehabilitation for stroke patients. An objective and validated outcome measure was used for the assessment of HQRoL [43], compared to a control group. Our results show that the use of a virtual reality program combined with conventional therapy produces significant changes in HQRoL in stroke survivors in the subacute phase. However, the results of the present study cannot be extrapolated to stroke patients in other stages of the disease or to rehabilitation systems with less-intensive intervention programs or in which the start of treatment is delayed.
Regarding the HQRoL, our results indicate that the combination of conventional treatment with a virtual semi-immersive approach produces positive effects in reducing the severity of problems in the dimensions of the EQ-5D-5L and in improving subjectively perceived health status (EQ-VAS). We highlight the effectiveness of the experimental intervention in the perception of pain and in the sensation of anxiety or depression, coinciding with another study [44]. A recent meta-analysis correlated post-stroke depression with a significantly higher risk of mortality in stroke patients [9].
The significant improvements of the participants in the experimental group can be explained theoretically. Task-oriented repetitive practice may provide more effective motor relearning for post-stroke neuronal recovery [45]. In this sense, the virtual reality devices used for this randomized controlled trial focus on intensive hand and upper limb movements, forcing the patient to mobilize body segments in various directions and at different speeds. The virtual reality games simulate movements necessary for the execution of activities of daily life. The patients in the experimental group experienced changes in their lives before and after the virtual reality session. Intensive and repetitive mobilization increased the activation of the affected area, reducing disuse and allowing the patients to carry out tasks outside the hospital setting with greater independence. The improved execution of movement and the increased functional independence may explain the decrease or absence of pain in the most affected upper limb and the results obtained in the anxiety–depression dimension of the EQ-5D-5L instrument.
It would therefore seem beneficial to establish lines of research and treatment programs aimed at reducing anxiety and pain in these patients. Along these lines, the use of virtual reality can be an interesting tool to include in protocols adapted to stroke patients [21]. The differences observed in the subjective diminution of problems performing activities of daily living stand in contrast to the minimum number of sessions established in other studies for this type of intervention [46,47]; however, they coincide with experimental interventions based on the adjustment of the balance between challenge and skill [42], an implicit characteristic in the specific virtual reality devices used for randomized controlled trials. In this sense, it should be noted that most of the published studies use commercial games or video consoles [48].
Current findings indicate that structural changes occur in response to motor learning during adulthood. Rehabilitative approaches that involve a high intensity of practice, positive feedback between stimulus and response, and increased motivation [29] are associated with more positive changes, without implying more hours of training [49,50]. Understanding the mechanisms of brain plasticity after injury is key to optimizing survivor interventions, promoting adaptive structural plasticity from the outset [30,51,52,53]. Based on our results, we can affirm that the use of virtual reality can be an appropriate complement for the conventional rehabilitation of patients with stroke in the subacute phase. Preventing and reducing pain in the most affected body segments, increasing the feeling of wellbeing, and improving the perception of the quality of life of the people with whom we work can allow an optimal recovery of the stroke survivor and his family, having repercussions, in turn, in the reduction of health and community services after the end of the subacute phase.
This research supports the integration of virtual reality in clinical practice and in the improvement of HQRoL of stroke survivors in the subacute phase. These systems can be incorporated into conventional intervention programs in stroke patients as adjunctive treatment [54,55].
Limitations of this study were that it did not include a long-term follow-up to determine if the differences within and between groups are maintained after the completion of the subacute phase. This long-term follow-up has not been possible due to the start of the COVID-19 pandemic in Spain. The present study was limited to a single center which could increase the effect of treatment, compared to other multicenter randomized controlled trial designs. The participants could not be blinded because they coincided in the conventional rehabilitative treatment and transmitted the evolution and improvements due to the use of virtual reality systems in hand mobility, reduction of shoulder pain, and improvement in the performance of activities of daily living [56,57].
5. Conclusions
The conventional rehabilitative approach combined with virtual reality would appear to be more effective than conventional treatment alone for improving the evaluated and perceived health-related quality of life in stroke survivors. We highlight two clinical messages: (1) Virtual reality as complement to conventional rehabilitation treatment is associated with a perceived increase of HRQoL in stroke survivors, and (2) three months after finishing the treatment, the effect of the combined intervention is reduced, especially in the dimensions of pain, anxiety, and depression.
Author Contributions
Conceptualization: M.R.-H., B.P.-L., and J.-J.C.-Á.; methodology: M.R.-H. and J.-J.C.-Á.; software: M.R.-H. and J.-J.C.-Á.; validation: M.R.-H., B.P.-L., and J.-J.C.-Á.; formal analysis: M.R.-H. and J.-J.C.-Á.; investigation: M.R.-H.; writing—original draft preparation: M.R.-H., B.P.-L., and J.-J.C.-Á.; writing—review and editing: A.M.-M., A.-I.C.-S., and J.L.M.-C.; supervision: A.M.-M., A.-I.C.-S., and J.L.M.-C. All authors have read and agreed to the published version of the manuscript.
Funding
Sponsored by the University of Castilla La Mancha (grant # 2020-GRIN-29192).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Research Ethics and Medicines Committee (CEIm) of the integrated health area of Talavera de la Reina (protocol code: 12/2018 and date of approval: 17/04/2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mendis S. Stroke Disability and Rehabilitation of Stroke: World Health Organization Perspective. Int. J. Stroke. 2013;8:3–4. doi: 10.1111/j.1747-4949.2012.00969.x. [DOI] [PubMed] [Google Scholar]
- 2.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oliveira C.B., Medeiros I.R.T., Greters M.G., Frota N.A.F., Tavares L., Scaff M., Conforto A.B. Abnormal sensory integration affects balance control in hemiparetic patients within the first year after stroke. Clinics. 2011;66:2043–2048. doi: 10.1590/S1807-59322011001200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duncan J., Van Wijck F., Pollock A., Ali M. Outcome measures in post-stroke arm rehabilitation trials: Do existing measures capture outcomes that are important to stroke survivors, carers, and clinicians? Clin. Rehabil. 2019;33:737–749. doi: 10.1177/0269215518823248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosomworth H., Rodgers H., Shaw L., Smith L., Aird L., Howel D., Wilson N., Alvarado N., Andole S., Cohen D.L., et al. Evaluation of the enhanced upper limb therapy programme within the Robot-Assisted Training for the Upper Limb after Stroke trial: Descriptive analysis of intervention fidelity, goal selection and goal achievement. Clin. Rehabil. 2020;35:119–134. doi: 10.1177/0269215520953833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schnabel S., Van Wijck F., Bain B., Barber M., Dall P., Fleming A., Kerr A., Langhorne P., McConnachie A., Molloy K., et al. Experiences of augmented arm rehabilitation including supported self-management after stroke: A qualitative investigation. Clin. Rehabil. 2020;35:288–301. doi: 10.1177/0269215520956388. [DOI] [PubMed] [Google Scholar]
- 7.Tyson S.F., Hanley M., Chillala J., Selley A., Tallis R.C. Balance Disability after Stroke. Phys. Ther. 2006;86:30–38. doi: 10.1093/ptj/86.1.30. [DOI] [PubMed] [Google Scholar]
- 8.Tessem S., Hagstrøm N., Fallang B. Weight distribution in standing and sitting positions, and weight transfer during reaching tasks, in seated stroke subjects and healthy subjects. Physiother. Res. Int. 2007;12:82–94. doi: 10.1002/pri.362. [DOI] [PubMed] [Google Scholar]
- 9.Cano-Mañas M.J., Collado-Vázquez S., Rodríguez J., Muñoz A.J., Cano-de-la-Cuerda R. Effects of Video-Game Based Therapy on Balance, Postural Control, Functionality, and Quality of Life of Patients with Subacute Stroke: A Randomized Controlled Trial. J. Healthc. Eng. 2020;2020:5480315. doi: 10.1155/2020/5480315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris J.H., Van Wijck F., Joice S., Donaghy M. Predicting health related quality of life 6 months after stroke: The role of anxiety and upper limb dysfunction. Disabil. Rehabil. 2013;35:291–299. doi: 10.3109/09638288.2012.691942. [DOI] [PubMed] [Google Scholar]
- 11.Salter K.L., Moses M.B., Foley N.C., Teasell R.W. Health-related quality of life after stroke: What are we measuring? Int. J. Rehabil. Res. 2008;31:111–117. doi: 10.1097/MRR.0b013e3282fc0f33. [DOI] [PubMed] [Google Scholar]
- 12.Testa M.A., Simonson D.C. Assessment of Quality-of-Life Outcomes. N. Engl. J. Med. 1996;334:835–840. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 13.Barrera Y.M., Concepción O.F., Hernández T.E. Calidad de vida en pacientes post-ictus: Factores determinantes desde la fase aguda. Rev. Haban. Cienc. Med. 2016;15:508–524. [Google Scholar]
- 14.García-Moriche N., Rodríguez-Gonzalo A., Muñoz-Lobo M.J., Parra-Cordero S., Fernández-De Pablos A. Quality of life in stroke patients. A phenomenological study. Enferm. Clin. 2010;20:80–87. doi: 10.1016/j.enfcli.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Aceituno-Gómez J., García-Madero V.M., Blázquez-Gamallo R., Harto-Martínez A.M., Mohedano A., Viñuela A., Avendaño-Coy J., Gómez-Soriano J., Muñoz-González A., González-González J., et al. Health-related quality of life in patients diagnosed with subacromial syndrome in the Talavera Integrated Area. Rev. Esp. Salud Publica. 2019;93:e201910094. [PubMed] [Google Scholar]
- 16.Ayis S., Wellwood I., Rudd A.G., McKevitt C., Parkin D., Wolfe C.D.A. Variations in Health-Related Quality of Life (HRQoL) and survival 1 year after stroke: Five European population-based registers. BMJ Open. 2015;5:e007101. doi: 10.1136/bmjopen-2014-007101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devlin N.J., Parkin D., Browne J. Patient-reported outcome measures in the NHS: New methods for analysing and reporting EQ-5D data. Health Econ. 2010;19:886–905. doi: 10.1002/hec.1608. [DOI] [PubMed] [Google Scholar]
- 18.Da Silva M., Bermúdez S., Duarte E., Verschure P.F.M.J. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: A randomized controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor. Neurol. Neurosci. 2011;29:287–298. doi: 10.3233/RNN-2011-0599. [DOI] [PubMed] [Google Scholar]
- 19.Mekbib D.B., Han J., Zhang L., Fang S., Jiang H., Zhu J., Roe A.W., Xu D. Virtual reality therapy for upper limb rehabilitation in patients with stroke: A meta-analysis of randomized clinical trials. Brain Inj. 2020;34:456–465. doi: 10.1080/02699052.2020.1725126. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad M.A., Singh D.K.A., Mohd N.A., Hooi K., Ibrahim N. Virtual Reality Games as an Adjunct in Improving Upper Limb Function and General Health among Stroke Survivors. Int. J. Environ. Res. Public Health. 2019;16:5144. doi: 10.3390/ijerph16245144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akinladejo F.O. Virtual Environments in Physical Therapy. In: Sík Lányi C., editor. Virtual Reality and Environments. IntechOpen; University of Pannonia, Veszprém, Hungary: 2012. pp. 1–10. [DOI] [Google Scholar]
- 22.Sveistrup H. Motor rehabilitation using virtual reality. J. Neuroeng. Rehabil. 2004;1:10. doi: 10.1186/1743-0003-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ISRCTN—ISRCTN27760662: Effectiveness of Virtual Reality Devices in the Rehabilitation of Adults with Stroke. [(accessed on 8 January 2021)]; Available online: http://www.isrctn.com/ISRCTN27760662.
- 24.Schulz K.F., Altman D.G., Moher D., CONSORT Group CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carmeli E., Peleg S., Bartur G., Elbo E., Vatine J.J. HandTutorTM enhanced hand rehabilitation after stroke—A pilot study. Physiother. Res. Int. 2011;16:191–200. doi: 10.1002/pri.485. [DOI] [PubMed] [Google Scholar]
- 26.Rodríguez-Hernández M., Fernández-Panadero C., López-Martín O., Polonio-López B. Hand Rehabilitation after Chronic Brain Damage: Effectiveness, Usability and Acceptance of Technological Devices: A Pilot Study. In: Tan U., editor. Physical Disabilities—Therapeutic Implications. IntechOpen; Cukurova University, Sarıçam/Adana, Turkey: 2017. pp. 57–72. [DOI] [Google Scholar]
- 27.Chua K.S.G., Kuah C.W.K. Innovating With Rehabilitation Technology in the Real World: Promises, Potentials, and Perspectives. Am. J. Phys. Med. Rehabil. 2017;96:S150–S156. doi: 10.1097/PHM.0000000000000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grefkes C., Fink G.R. Connectivity-based approaches in stroke and recovery of function. Lancet Neurol. 2014;13:206–216. doi: 10.1016/S1474-4422(13)70264-3. [DOI] [PubMed] [Google Scholar]
- 29.Saposnik G., Cohen L.G., Mamdani M., Pooyania S., Ploughman M., Cheung D., Shaw J., Hall J., Nord P., Dukelow S., et al. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): A randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016;15:1019–1027. doi: 10.1016/S1474-4422(16)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sampaio-Baptista C., Sanders Z.B., Johansen-Berg H. Structural Plasticity in Adulthood with Motor Learning and Stroke Rehabilitation. Annu. Rev. Neurosci. 2018;41:25–40. doi: 10.1146/annurev-neuro-080317-062015. [DOI] [PubMed] [Google Scholar]
- 31.Handtutor MediTouch. [(accessed on 9 January 2021)]; Available online: https://meditouch.co.il/products/handtutor/
- 32.3DTutor MediTouch. [(accessed on 9 January 2021)]; Available online: https://meditouch.co.il/products/3dtutor/
- 33.Rehametrics|Cuantificando la Rehabilitación Física y Cognitiva. [(accessed on 9 January 2021)]; Available online: https://rehametrics.com/
- 34.Martínez M.C., Parejo M.T., Laiz N.M. Valoración del uso de las nuevas tecnologías en personas con esclerosis múltiple. REDIS. 2018;6:149–171. doi: 10.5569/2340-5104.06.02.08. [DOI] [Google Scholar]
- 35.Abreu J., Rebelo S., Paredes H., Barroso J., Martins P., Reis A., EuricoVasco A. Assessment of Microsoft Kinect in the Monitoring and Rehabilitation of Stroke Patients. In: Rocha Á., Correia A.M., Adeli H., Reis L.P., Costanzo S., editors. Recent Advances in Information Systems and Technologies. Springer International Publishing; Berlin/Heidelberg, Germany: 2017. pp. 167–174. [DOI] [Google Scholar]
- 36.Ashwini K., Amutha R., Nagarajan K.K., Raj S.A. Kinect based Upper Limb Performance Assessment in Daily Life Activities; Proceedings of the International Conference on Wireless Communications Signal Processing and Networking (WiSPNET); Chennai, India. 21–23 March 2019; pp. 201–205. [DOI] [Google Scholar]
- 37.Mousavi H., Khademi M. A Review on Technical and Clinical Impact of Microsoft Kinect on Physical Therapy and Rehabilitation. J. Med. Eng. 2014;2014:846514. doi: 10.1155/2014/846514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.EuroQol Group EuroQol—A new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 39.Badia X., Roset M., Montserrat S., Herdman M., Segura A. [The Spanish version of EuroQol: A description and its applications. European Quality of Life scale] Med. Clin. 1999;112:79–85. [PubMed] [Google Scholar]
- 40.Herdman M., Badia X., Berra S. El EuroQol-5D: Una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Aten. Primaria. 2001;28:425–429. doi: 10.1016/S0212-6567(01)70406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Räsänen P., Roine E., Sintonen H., Semberg-Konttinen V., Ryynänen O.P., Roine R. Use of quality-adjusted life years for the estimation of effectiveness of health care: A systematic literature review. Int. J. Technol. Assess. Health Care. 2006;22:235–241. doi: 10.1017/S0266462306051051. [DOI] [PubMed] [Google Scholar]
- 42.Yoshida I., Hirao K., Kobayashi R. The effect on subjective quality of life of occupational therapy based on adjusting the challenge–skill balance: A randomized controlled trial. Clin. Rehabil. 2019;33:1732–1746. doi: 10.1177/0269215519858713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robinson A., Gyrd-Hansen D., Bacon P., Baker R., Pennington M., Donaldson C. Estimating a WTP-based value of a QALY: The ‘chained’ approach. Soc. Sci. Med. 2013;92:92–104. doi: 10.1016/j.socscimed.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 44.Yoshida I., Hirao K., Nonaka T. Adjusting Challenge-Skill Balance to Improve Quality of Life in Older Adults: A Randomized Controlled Trial. Am. J. Occup. Ther. 2018;72:7201205030p1–7201205030p8. doi: 10.5014/ajot.2018.020982. [DOI] [PubMed] [Google Scholar]
- 45.Cai W., Mueller C., Li Y.J., Shen W.D., Stewart R. Post stroke depression and risk of stroke recurrence and mortality: A systematic review and meta-analysis. Ageing Res. Rev. 2019;50:102–109. doi: 10.1016/j.arr.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 46.Chen M.H., Huang L.L., Lee C.F., Hsieh C.L., Lin Y.C., Liu H., Chen M.-I., Lu W.-S. A controlled pilot trial of two commercial video games for rehabilitation of arm function after stroke. Clin. Rehabil. 2015;29:674–682. doi: 10.1177/0269215514554115. [DOI] [PubMed] [Google Scholar]
- 47.Dos Santos L.R.A., Carregosa A.A., Masruha M.R., Dos Santos P.A., Da Silveira M.L., Ferraz D.D., Ribeiro N.M.D.S. The Use of Nintendo Wii in the Rehabilitation of Poststroke Patients: A Systematic Review. J. Stroke Cerebrovasc. Dis. 2015;24:2298–2305. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 48.Cheok G., Tan D., Low A., Hewitt J. Is Nintendo Wii an Effective Intervention for Individuals With Stroke? A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015;16:923–932. doi: 10.1016/j.jamda.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 49.Maier M., Rubio B., Duff A., Duarte E., Verschure P.F.M.J. Effect of Specific Over Nonspecific VR-Based Rehabilitation on Poststroke Motor Recovery: A Systematic Meta-analysis. Neurorehabil. Neural Repair. 2019;33:112–129. doi: 10.1177/1545968318820169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laver K.E., George S., Thomas S., Deutsch J.E., Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2015;2015:CD008349. doi: 10.1002/14651858.CD008349.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laver K.E., Lange B., George S., Deutsch J.E., Saposnik G., Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017;11:CD008349. doi: 10.1002/14651858.CD008349.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burke E., Dodakian L., See J., McKenzie A., Le V., Wojnowicz M., Shahbaba B., Cramer S.C. Neural function, injury, and stroke subtype predict treatment gains after stroke. Ann. Neurol. 2015;77:132–145. doi: 10.1002/ana.24309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fan Y., Lin K., Liu H., Chen Y., Wu C. Changes in structural integrity are correlated with motor and functional recovery after post-stroke rehabilitation. Restor. Neurol. Neurosci. 2015;33:835–844. doi: 10.3233/RNN-150523. [DOI] [PubMed] [Google Scholar]
- 54.Fan Y.T., Wu C.Y., Liu H.L., Lin K.C., Wai Y.Y., Chen Y.L. Neuroplastic changes in resting-state functional connectivity after stroke rehabilitation. Front. Hum. Neurosci. 2015;9:546. doi: 10.3389/fnhum.2015.00546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Luque-Moreno C., Ferragut-Garcías A., Rodríguez-Blanco C., Heredia-Rizo A.M., Oliva-Pascual-Vaca J., Kiper P., Oliva-Pascual-Vaca Á. A Decade of Progress Using Virtual Reality for Poststroke Lower Extremity Rehabilitation: Systematic Review of the Intervention Methods. BioMed Res. Int. 2015;2015:342529. doi: 10.1155/2015/342529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Colomer C., Llorens R., Noé E., Alcañiz M. Effect of a mixed reality-based intervention on arm, hand, and finger function on chronic stroke. J. Neuroeng. Rehabil. 2016;13:45. doi: 10.1186/s12984-016-0153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ho T.H., Yang F.C., Lin R.C., Chien W.C., Chung C.H., Chiang S.L., Chou C.-H., Tsai C.-K., Lin Y.-K., Lee J.-T. Impact of virtual reality-based rehabilitation on functional outcomes in patients with acute stroke: A retrospective case-matched study. J. Neurol. 2019;266:589–597. doi: 10.1007/s00415-018-09171-2. [DOI] [PubMed] [Google Scholar]