Abstract
Monochorionic monoamniotic pregnancy are considered high risk gestations and the fetal outcome is at times unpredictable. Correct diagnosis and counselling are extremely important, especially regarding the risk of unexpected fetal demise. We present the rare case of a monochorionic monoamniotic twin pregnancy with early identification of cord entanglement and the characteristic ultrasound findings in the first trimester of pregnancy.
Keywords: monochorionic monoamniotic twin pregnancy, cord entanglement, fetal demise
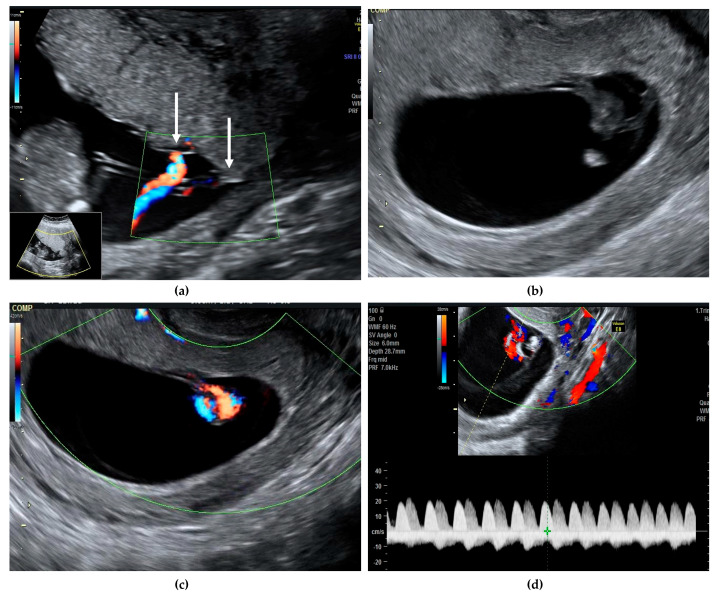
Monochorionic monoamniotic twin pregnancy is rare, with an estimated prevalence of about 1 in 10,000 pregnancies, representing 1–5% of all monochorionic twins [1]. Correct diagnosis and counselling of parents are extremely important, especially regarding the risk of unexpected fetal demise. Without major abnormalities, the rates of fetal loss before 24 weeks are 20% [2] and the risk of perinatal mortality after 24 weeks ranges between 10–20% [2,3]. More recent data reported a lower risk of unexpected fetal death, of about 5–10%, after excluding cases of discordant structural anomalies, spontaneous miscarriage, or complications related to monochorionicity such as twin-to-twin transfusion syndrome (TTTS) [4]. After 32 weeks, the risk of sudden fetal death is 4% and usually involves both twins [5]. Cord entanglement has been evoked as the main cause of sudden death, although other mechanisms such as acute exsanguination through large umbilical anastomoses are likely to be involved, as cord entanglement is present in almost all monoamniotic twins and most of them have a good prognosis after 20 weeks despite this finding [3]. Diagnosis of chorionicity and amnionicity is easily established in the first trimester of pregnancy, along with other major structural defects [6]. Cord entanglement can be identified early in the first trimester using color Doppler and pulsed-wave Doppler by the simultaneous recording of two different heart rates [7] (Figure 1).
Figure 1.
We present a case of a 30-year-old G2 P2 with a previous caesarean section, who presented in our unit at 11 weeks gestation for pregnancy confirmation after normal spontaneous conception. A viable monochorionic monoamniotic twin pregnancy was identified, and the common placenta and the cord insertions, very close to one another, were visualized (a, white arrows). The second ultrasound evaluation at 13 weeks did not reveal any structural abnormalities and the risk for aneuploidies was low (Supplementary Materials). Cord entanglement was suspected at this early gestational age, both in gray scale and color Doppler (b,c). Simultaneous registrations of two different heart rates also suggested the cord entanglement (d, represented by white and yellow arrows). The patient was counselled regarding the diagnosis, the possible complications, and the monitoring plan. The follow-up visit was planned for 16 weeks and both Doppler studies and growth were within normal ranges. From 16 weeks onwards, the follow-up scans were booked every second week. Unfortunately, the patient did not attend the 18 weeks scan, but she had a scan at 19 weeks. Sadly, double fetal demise was diagnosed. We acknowledge that this event was unpreventable and that routinely we recommend a scan every second week for reassurance. When fetal death occurs, this is an acute hemodynamic event, therefore previous scans are usually normal.
Legend
Supplementary Materials
The following are available online at https://www.mdpi.com/2075-4418/11/3/520/s1, Monochorionic monomaniotic pregnancy early cord entanglemnet demonstration by ultrasound. S1—with color doppler; S2—in B mode.
Author Contributions
Conceptualization, A.M.P. and A.V.; methodology, B.C and A.M.C.; investigation, A.M.P., A.V., N.G., and R.B.; data curation, R.B.; writing—original draft preparation, A.M.P. and A.M.C; writing—review and editing, B.C. and G.P.; visualization, N.G.; supervision, A.V. and G.P.; project administration, A.M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sebire N.J., Souka A., Skentou H., Geerts L., Nicolaides K.H. First trimester diagnosis of monoamniotic twin pregnancies. Ultrasound Obstet. Gynecol. 2000;16:223–225. doi: 10.1046/j.1469-0705.2000.00229.x. [DOI] [PubMed] [Google Scholar]
- 2.Litwinska E., Syngelaki A., Cimpoca B., Frei L., Nicolaides K.H. Outcome of twin pregnancies with two live fetuses at 11–13 weeks’ gestation. Ultrasound Obstet Gynecol. 2020;55:32–38. doi: 10.1002/uog.21892. [DOI] [PubMed] [Google Scholar]
- 3.Hack K.E., Derks J.B., Schaap A.H., Lopriore E., Elias S.G., Arabin B., Eggink A.J., Sollie K.M., Mol B.W.J., Duvekot H.J., et al. Perinatal Outcome of Monoamniotic Twin Pregnancies. Obstet. Gynecol. 2009;113:353–360. doi: 10.1097/AOG.0b013e318195bd57. [DOI] [PubMed] [Google Scholar]
- 4.Dias T., Mahsud-Dornan S., Bhide A., Papageorghiou A.T., Thilaganathan B. Cord entanglement and perinatal outcome in monoamniotic twin pregnancies. Ultrasound Obstet. Gynecol. 2010;35:201–204. doi: 10.1002/uog.7501. [DOI] [PubMed] [Google Scholar]
- 5.D’Antonio F., Odibo A., Berghella V., Khalil A., Hack K., Saccone G., Prefumo F., Buca D., Liberati M., Pagani G. Perinatal mortality, timing of delivery and prenatal management of monoam-niotic twin pregnancy: Systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019;53:166–174. doi: 10.1002/uog.20100. [DOI] [PubMed] [Google Scholar]
- 6.Vayna A.M., Veduta A., Duta S., Panaitescu A.M., Stoica S., Buinoiu N., Nedelea F., Peltecu G. Diagnosis of Fetal Structural Anomalies at 11 to 14 Weeks. J. Ultrasound Med. 2018;37:2063–2073. doi: 10.1002/jum.14561. [DOI] [PubMed] [Google Scholar]
- 7.Overton T.G., Denbow M.L., Duncan K.R., Fisk N.M. First-trimester cord entanglement in monoamniotic twins. Ultrasound Obstet. Gynecol. 1999;13:140–142. doi: 10.1046/j.1469-0705.1999.13020140.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.