Abstract
Low uptake of women's cancer screening and its facilitating factors and barriers in Iran has been studied so far but no consensus on factors affecting this low uptake has been stated previously. Nevertheless, facilitating factors and barriers of breast cancer and cervical cancer have been reviewed. In this systematic review, Web of Science, PubMed, EMBASE, Scopus, and Google Scholar were the preferred search engines. In addition, the Persian database of Magiran and SIDs and ISC indexed journals were searched with different combinations of Persian keywords compatible with English search. A hand search of key Iranian journals was also accomplished. Through 964 primarily searched articles, finally, after duplicates being removed, the screen of records, and full-text articles assessed for eligibility, only 12 articles were included in the review. Barriers observed mostly were screening not advised by a physician, having no relevant problems or disease, having no knowledge about the procedure, fear from pain or cancer detection, shame from the procedure, and forget to have screening. Facilitators were less focused than barriers and frequently were identified as advised by healthcare professionals, the perceived necessity for screening, and the important identified risk of cancer acquire. Almost all studies focused on individual and interpersonal barriers and facilitators for screening instead of a holistic view on the utilization of screening programs. In future studies on women's cancer screening, facilitating factors and barriers of both supply (health system provision and policy implications) and demand-side (individual and interpersonal factors) of healthcare provision has been strongly recommended.
Keywords: Iran, mass screening, review, women
Introduction
In developing countries, breast cancer and cervical cancer account for 882,900 and 444,500 new cases, respectively and together accounted for 114,000 (97,000–131,000) deaths in the reproductive age women in 2010.[1,2]
In Iran, breast cancer is the first and cervical cancer is the fifth most common cancers (apart from skin cancer) of women.[3] The incidence of breast and cervical cancer in women is estimated to 22 per 100,000[4] and 6 per 100,000 in the order already mentioned.[5]
Using preventive modalities, in the era of increasing cancer incidence, is of utmost importance.[6,7,8] It is accepted in developed countries that cervical and breast cancer mortality could be prevented by screening programs. The screening program may be organized or opportunistic. The main difference between these two methods is that in organized screening, the manner in which the clients are invited is through centralized population registers while opportunistic screening depends on clients or on their health advisors to recommend screening. Organized screening includes timely call, recall, follow-up of early detected cases, and surveillance systems.[9]
Organized screening program which is implemented mostly in developed countries, often considers key factors for effective screening (quality assurance indicators, number of detected cases, number of false positive, etc). Organized breast cancer screening programs in 22 developed countries had coverage less than 25 to 100%[10] and for cervical cancer screening of European countries, there were differences in coverage from below 50 to 82%.[11] The effectiveness of opportunistic vs organized screening has been studied elsewhere. In Hong Kong, opportunistic cervical cancer screening in place was less effective and less efficient than expected organized screening and also there was some problem with over or under the screening of a minority of women.[12] As a result of limited healthcare resources in developing countries, there should be a context adopted screening program that is affordable.[13] Presently, most low-income countries have inefficient screening for breast cancer and low coverage documented (less than 5%) cervical cancer opportunistic screening.[14]
Currently, in Iran, breast and cervical cancer screening are not organized. There is only an opportunistic screening of breast and cervical cancer which is integrated into the SABA health service program (Iranian Women's Health Record) since 2012. In SABA, eligible women in primary healthcare settings undergo Pap smear and are referred to perform mammography. However, the uptake of SABA is not well documented until now. Health care providers of other settings, rather than primary healthcare settings, only may encourage patient to perform mammography or Pap smear. In some cases, clients demand mammography or Pap smear from their physicians.
The accomplishment of the mammography and report of Pap smear results in SABA is not free of charge. Moreover, the cost of breast and cervical cancer screening in other situations is not covered by all insurance (since there are various types of insurance with different coverage, cost of screening may differ) subsequently, no follow-up is defined for true or false, and for positive or negative screening results. Continuity of care is not defined due to a lack of surveillance systems.[15] To our knowledge, there is no documented evaluation for the effectiveness and quality of ongoing screening of breast and cervical cancer in Iran.
In the present situation of cervical and breast cancer screening, we have to identify the barriers and facilitators for performing screening which of course could help us have a better understanding of the need of clients. Factors affecting the uptake of these screening tests have been investigated in several single primary studies on Iranian women.[16,17,18,19,20,21,22,23,24,25,26,27,28] But there is no comprehensive view on the barriers and facilitators of screening tests in Iran.
In this study, we reviewed the articles on the barriers and facilitators of breast and cervical cancer screening in Iran.
Materials and Method
This systematic review was conducted according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guideline statement.[29] The review protocol was written before the start of the study. The proposal was approved by the scientific review board of Shiraz University of Medical Sciences.
Search strategy
We employed a very broad search strategy to identify uptake barriers for performing mammography, self-breast exam (SBE), clinician breast exam (CBE), and Pap smear test in Iranian women. Medical subject headings (MeSH), free-text words, and Emtree thesaurus were used to detect the relevant terms. We searched through Web of Science, PubMed, EMBASE, and Scopus. To achieve the grey literature and unpublished findings, Google Scholar was searched manually through page 30. Also, the Persian database of Magiran and SIDs and ISC indexed journals were searched with different combinations of Persian keywords compatible with English search (supplementary material). A hand search of key Iranian journals including International Journal of Preventive Medicine (IJPM), Iranian Journal of Public Health (IJPH), The Iran Journal of Nursing (IJN), Iranian Quarterly Journal of Breast Diseases, Iranian Journal of Obstetrics, Gynecology, and Infertility (IJOGI) was also accomplished.
The time limit was set for publication after 2000 till the date of the last search (1st day of November 2019) and no language restrictions were applied.
We scanned reference lists of relevant references to retrieve as much relevant information as possible. In our search strategies, we believe that to combine indexing terms and text words can achieve high sensitivity and specificity. Databases were searched with the alternative keywords which could be found in the supplementary material of this article (supplementary material).
Eligibility criteria
We enrolled in quantitative observational studies which include women with compatible age for screening. However studies which include ever-married women of any age through 70 years for Pap smear, > =20 years for SBE and CBE and > =40 years for mammography were eligible for this review, mounting the sensitivity of findings, we accepted studies on facilitators and barriers of Pap smear of ever-married women through 65 years.[30] In this study, articles in which reported barriers and/or facilitators of breast and cervical cancer in Iran were included. Any impediments that directly prevent, or make participation in screening difficult for women and any factor that encourages or persuade women to perform screening regarded as barrier or facilitator of screening, respectively. Studies in which barriers and/or facilitators were found through statistical modeling or correlated to the practice or participation of screening were not included. Studies on barriers and facilitators for breast and cervical cancer screening in specified limited women's population (for example, healthcare workers, nurses, teachers, students, etc.) were excluded to decrease the risk of potential biases in selected articles.
Study selection
S. Ghahramani and H. Kasraei, independently identified which study to include based on the prespecified protocol. Disagreements were resolved by discussion or by consulting a third researcher (KBL). Duplicated articles from different databases were omitted and abstracts of the remaining articles were scanned. Full-text of articles assessed for eligibility. None relevant studies were excluded. Around 22 items STROBE checklist was used for assessment of the quality of the final included full texts (n = 12). The methodological criteria included description of study design, setting, participants and variables, data sources/measurement, bias, study size, quantitative variables, and statistical methods. Quality assessment was rated independently by the two abovementioned authors and inconsistencies were resolved by consensus or by consulting a third researcher.
Data collection process and Data items
S. Ghahramani and H. Kasraei independently extracted methodological and outcome data. Extracted data were entered in a data collecting form which included name of author and date of publication; province and study setting, language of study; number of studied women; mean (standard deviation) age of participants, design of study; type of screening (mammography, self-breast exam (SBE), clinician breast exam (CBE) or Pap smear); barriers and facilitating factors related to screening and details of questionnaire which was used for data collection. The data of main outcomes (barriers and facilitators of breast and cervical cancer screenings) in Iran was qualitative in essence, so we could not perform a meta-analysis on the results of included studies.
Results
Study selection
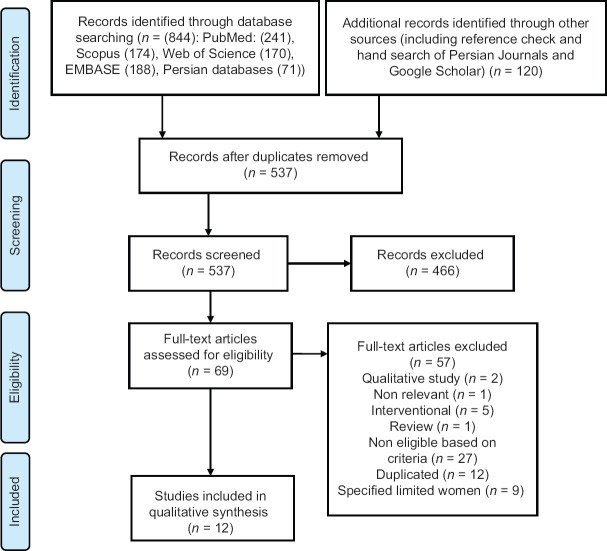
The process of the search and screening for the present systematic review is illustrated in the PRISMA flow diagram [Figure 1]. The initial search strategy resulted in a total number of 964 articles. After removing the duplicates, 537 studies were remained and screened. The screening was performed based on the title and abstract and 69 studies were selected for full-text assessment. Lastly, 12 cross-sectional studies were considered in the final assessment.
Figure 1.
PRISMA flowchart of the selection process
Description of studies
Detailed characteristics of the included studies are described in Table 1. All included studies were cross-sectional. Studies were performed in 8 provinces out of 31 provinces of Iran. Kashan, Tehran, Hormozgan, and Hamadan provinces each one with two eligible studies[20,22,31,32,33,34,35,36] and Kerman, Chaharmahal and Bakhtiari, West Azarbayjan, and Isfahan provinces,[37,38,39,40] each comprise one study. The publication date of the included studies ranged from 2006 to 2018. The mean age of participants in each study ranged from 29.2 to 54.9 years. In these studies, a total of 14975 subjects participated. Regarding the type of screening, six studies were focused on breast cancer screening methods, four studies Pap smear, and two studies considered both cancer screenings. Three studies were in the English language[20,22,32] and other studies were in Persian. Except for three studies[32,35,39] which used the Champion's health belief model scale (CHBMS) questionnaire, the other one used researcher-made questionnaires. Quality assessment is described in detail in supplementary Table 1. Almost all of the included studies had “Good” and “Fair” quality. Only one study had “poor” quality.[36]
Table 1.
Studies characteristics
| Article number | Author (Year) | Province | Population, Setting | Questionnaire | Sample size | Mean (SDa) age of participants | Type of screening | Adherence to screeningb (percent/total) |
|---|---|---|---|---|---|---|---|---|
| 1 | Soltanahmadi (2010) | Kerman | Ever married women, referred to selected healthcare centers of Kerman | Researcher-made questionnaire | 200 | 30.6 (7.9) | SBEc, CBEd and Pap smear | 22.5 (SBE) 21.5 (CBE) 27 (Pap smear) |
| 2 | Sadatjediarani (2015) | Kashan | Ever married women, referred to selected urban and rural healthcare centers of Kashan | Researcher-made questionnaire | 851 | Was not reported | SBE, Mammography and Pap smear | 22.2 (SBE) 5.9 (Mammography) 43.7 (Pap smear) |
| 3 | Ghaoomi (2016) | Tehran | Ever married women, 20 to 65 years old , referred to Firoozgar Hospital, Tehran | Researcher-made questionnaire | 90 | Was not reported | Pap smear | - |
| 4 | Hajializadeh (2013) | Hormozgan, Bandar Abbas | Ever married women referred to selected healthcare centers of Bandar Abbas | Prepared by the researcher, using the valid questionnaires | 727 | 34 (-) | Pap smear | 31.8 |
| 5 | Jalilian (2011) | Hamadan | Married women 20 to 70 years old , referred to selected healthcare centers of Hamadan | Researcher-made using a standard questionnaire | 400 | 32.3 (-) | Pap smear | 28.3 |
| 6 | Saberi (2012) | Kashan | Ever married women, 15 to 75 years old , referred to selected healthcare centers of Kashan | Researcher-made questionnaire | 1000 | 36.3 (10.4) | Pap smear | 11.3 |
| 7 | Allahverdipour (2011) | Hamadan | women, 40 to 73 years old, selected healthcare centers of Hamadan | Champion’s revised HBM Scale (HBMS) and Champion’s Health Belief Model Scale (CHBMS) | 414 | 45.7 (SD 5.6) | Mammography and SBE | - |
| 8 | Banaeian (2006) | Chaharmahal and Bakhtiari | Women more than 20 years old referred to healthcare centers of Borujen | Researcher-made questionnaire | 400 | 31.1 (SD 8.6) | Mammography, CBE, and SBE | 4.5 (SBE) |
| 9 | Hasani (2011) | Hormozgan, | Women referred to selected healthcare centers of Bandar Abbas | Champion’s Health Belief Model Scale (CHBMS) | 240 | 37.2 (6.1) | SBE | 7.1 (SBE) |
| 10 | Mokhtari (2014) | West Azarbayjan | Women, more than 20 years old referred to selected healthcare centers of Khoy | Champion’s Health Belief Model Scale (CHBMS) | 162 | 29.2 (7.5) | Mammography and SBE | 8.6 (SBE) |
| 11 | Rejali (2018) | Isfahan | Door to door interview with women of 20 to 65 years old in both rural and urban area of Isfahan | Researcher-made questionnaire | 9591 | 37.6 (11.7) | Mammography, CBEd, and SBE | 63.4 (SBE) |
| 12 | Rezaee Ghazdehi (2013) | Tehran | women aged ≥40 referred to selected clinics of Tehran University of Medical Sciences, never had mammography | Researcher-made questionnaire | 900 | 54.9 (9.9) | Mammography | - |
aSD: Standard deviation, bbased on individual study definition, cSelf-breast exam, dclinician breast exam
Outcomes
Out of 12 included studies, two studies focused on barriers and facilitators of both cervical and breast cancer screening, six and four studies focused on barriers and facilitators of breast and cervical cancer screenings, respectively.
In studies by Soltanahmadi et al.[37] and Sadatjediarani et al.[31] were focused on barriers and facilitators of both breast and cervical cancer screening in Iran. Adherence to screening was reported as SBE: 22.5%, CBE: 21.5%, and Pap smear: 27%[26] and SBE: 22.2%, mammography: 5.5% and Pap smear: 43.7%, although only Soltanahmadi et al.[26] clearly provided a definition for the adherence to screening. Soltanahmadi et al. stated that the main barriers for SBE, CBE, and mammography screening were lack of screening recommendation by a physician, lack of knowledge about the procedure, and negative history of previous related disease. Whereas Sadatjediarani et al. found that besides the negative history of the previous related disease and lack of knowledge about the probability of acquiring cancer; fear from cancer occurrence was a barrier for women's cancer screening in their study population.
In six studies in which evaluated the barriers and facilitators of breast cancer screening methods in Iran, adherence to screening only was reported for SBE by 4 studies and ranged between 4.5 to 63.4%. One study[32] reported both facilitators and barriers for breast cancer screening and other studies focused on barriers. The main facilitator of breast cancer screening was identified as recommendation from a healthcare professional (cue to action)[32] barriers of breast cancer screening though differed for different screening method but in brief include: have no problem or pain in breasts, fear of pain, trouble remembering to get a mammography, lack of knowledge about procedure, and shame. Detailed information is provided in Tables 2 and 3.
Table 2.
Barriers and facilitators for breast cancer, breast cancer, and cervical cancer screening (both cancers ) in eligible articles of Iran
| Author (Year) | Barriers | Facilitators |
|---|---|---|
| Soltanahmadi (2010) | For SBE, CBEa: | For SBE, CBEa: |
| -Was not recommended by a physician | - Informed about the necessity of performing the screening | |
| - Have no knowledge about the procedure | ||
| - No history of previous breast disease | - Early detection of cancer | |
| -Neglect | - Advised by midwife | |
| For Pap smear: | -Presence of disease in relatives | |
| - Was not recommended by a physician | For Pap smear: | |
| - Have no knowledge about the procedure | - Early detection of cancer | |
| - No history of genital disease previously | - Informed about the necessity of performing the screening | |
| - Shame | - Advised by midwife | |
| - presence of previous genital disease | ||
| Sadatjediarani (2015) | For SBE, Pap smear and Mammography | For SBE, Pap smear and Mammography |
| -Have no problem or disease | -the seriousness of the risk of cancer occurrence | |
| - Have no knowledge about the probability to have cancer | - advised by healthcare providers | |
| - Fear from cancer occurrence | - access to the healthcare left | |
| Allahverdipour (2011) | - Fear of pain | -recommendation from a health care professional (cue to action) |
| - Trouble remembering to get a mammography | ||
| - Lack of time to get a mammogram | ||
| Banaeian (2006) | -Don’t know how to perform SBE | |
| - Have no problem | ||
| Hasani (2011) | -Shame | |
| - The procedure is time-consuming | ||
| - Forget | ||
| - No suitable place for SBE | ||
| - Process of SBE is difficult | ||
| Mokhtari (2014) | For SBE: | |
| - No suitable place for SBE | ||
| For mammography: | ||
| - Trouble remembering the time to get a mammography | ||
| Rejali (2018) | For SBE: | |
| -Have no problem or pain in breasts | ||
| - Don’t know how to perform SBE | ||
| For CBE: | ||
| -Have no problem in breasts, | ||
| For mammography: | ||
| - Have no problem in breasts | ||
| - High cost | ||
| - Fear of pain | ||
| Rezaee Ghazdehi (2013) | -Have no symptom of breast cancer | |
| - Not concerned about breast cancer | ||
| - Not concerned about breast cancer because of no family history | ||
| -Feeling no necessity for performing mammography | ||
| - Not concerned about health status | ||
| - Believe in fate | ||
| - None of the friends had mammograms |
aSBE and CBE, Self-breast exam and clinician breast exam respectively
Table 3.
Barriers and facilitators for cervical cancer screening in eligible articles of Iran
| Author (Year) | Barriers | Facilitators |
|---|---|---|
| Ghaoomi (2016) | -Shame | - Information provided by a physician |
| - Fear from cancer occurrence (detection) | ||
| Jalilian (2011) | - physicians’ recommendation | |
| Saberi (2012) | -Lack of information about the necessity of performing the screening | |
| - Shame | ||
| - performing the test makes me anxious | ||
| Hajializadeh (2013) | -Fear of the test | |
| -Painful Pap smear test | ||
| - Forgetting | ||
| - Time-consuming, have no time | ||
| - Inadequate knowledge | ||
| - Shame | ||
| -Lack of physician recommendation and health personnel |
Adherence to cervical cancer screening (by means of Pap smear) in Iran ranged between 11.3 to 31.8%. Information provided by physicians and recommendation of the physician were main facilitators of Pap smear in reviewed studies and barriers briefly include shame, fear (from the pain of Pap smear, cancer detection), and inadequate knowledge and information about the necessity of performing screening.
Details of barriers and facilitators of Pap smear in Iran are provided in Table 3.
Discussion
This study aimed to find facilitating factors for uptake and barriers of adherence to a screening of cervical and breast cancer in Iran. To our knowledge, this is the first comprehensive systematic review on this issue in Iran.
Through reviewed studies, main barriers for women's cancer screening in Iran include failure of physician to recommend for screening, lack of knowledge of participants about the screening procedure and the probability of acquiring cancer, negative history of previous related disease, fear from pain or cancer detection, shame from the procedure, and forget to have screening. Most of these barriers were stated in a systematic review of barriers of breast cancer screening behavior on Persian language articles published in 2015[41] however, the present systematic review had a broader view on both cervical and breast cancer screening with no language limit.
Adherence to women's cancer screening in Iran was reported to be less than 50% by most studies. Low adherence to screening has been reported in Iran, previously[42,43,44] however, there are two common flaws in this regard. Firstly, the adherence to screening should be clearly defined[37] and secondly, it is better to adjust the adherence to mammography and Pap smear screening based on the age of the participants.[44] In included articles of this review, facilitators were less focused than barriers and frequently were identified as advice by healthcare professionals, the perceived necessity for screening, important identified risk of cancer acquire, early detection of cancer, and presence of cancer in relatives. The essence of identified facilitators beside unacceptable percentages of adherence to screening program and recommendations of primary studies for improving uptake of screening motivate researchers for future interventional studies. It seems reasonable that future investigation should concentrate on the effect of increased awareness and knowledge of women and more educational and counseling efforts by healthcare professionals to facilitate screening uptake.[42,45,46,47,48,49,50] In the situation of no organized screening method for cancer screening of women in Iran, more competence of healthcare professionals combined with increase women awareness by socioculturally acceptable messages could be a good suggestion.[51,52]
Because of the diversity of barriers and facilitators, we can categorize them for a better understanding of four socioecological factors including individual, interpersonal, health system, and policy factors. The first two factors could be attributed to demand for healthcare, while the latter is identified as the supply of healthcare. Results showed more focus on barriers and facilitators in individual and interpersonal levels and limited geographic distribution in primary studies of breast and cervical cancer screening in Iran.
Focus on individual and interpersonal (the demand side for receiving service) factors lead to a lack of comprehensive and holistic view (both demand and supply side) on facilitating factors and barriers for the utility of screening of breast and cervical cancer. Healthcare provision may be introduced through developing a surveillance system and national policy and guidelines for full coverage of women's cancer in Iran.[15]
It is recommended in the situation of suffering from scarcity of resources,[50,51] health system has to implement the screening program in a small geographical area on the high-risk group with a sensitive program and attempt should be made to study if the program is effective or not. Resources should be sought to prepare the infrastructures, adequate trained human resources, and planned surveillance that cares about the follow-up of positive and negative cases before the expansion of the program.[13]
This study reviewed the studies on facilitating factors and barriers for the uptake of women's cancer in Iran but the possibility of the presence of facilitating factors and barriers for screening that are not stated in these primary studies should be kept in mind. Besides holistic view studies, research on the effectiveness of the current screening in places in Iran is also recommended.
Conclusion
Barriers of women's cancer screening in Iran mostly were failure of the physician to recommend for screening, lack of knowledge of participants about the screening procedure and the probability of acquiring cancer, negative history of the previous related disease, fear from pain or cancer detection, shame from the procedure, and forget to have screening. Facilitators were less focused than barriers and frequently were identified as advice by healthcare professionals, the perceived necessity for screening, important identified risk of cancer acquire. Almost all studies focused on demand-side barriers for screening service with a telescopic view on individual and interpersonal factors instead of a holistic view on the utilization of screening programs. In future studies on the women's cancer screening, facilitating factors and barriers of both supply (health system provision and policy implications) and demand-side (individual and interpersonal factors) of healthcare provision is strongly recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the authors of primary studies.
References
- 1.Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: A systematic analysis. Lancet. 2011;378:1461–84. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Radmard AR. Five common cancers in Iran. Arch Iran Med. 2010;13:143–6. [PubMed] [Google Scholar]
- 4.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 5.Khorasanizadeh F, Hassanloo J, Khaksar N, Mohammad Taheri S, Marzaban M H, Rashidi B, et al. Epidemiology of cervical cancer and human papilloma virus infection among Iranian women — Analyses of national data and systematic review of the literature. Gynecol Oncol. 2013;128:277–81. doi: 10.1016/j.ygyno.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 6.Ahmadi A, Salehi F, Ahmadimirghaed Z. Cancer trends in a province of Southwest of Iran, 2003-2016. J Res Med Sci. 2018;23:80. doi: 10.4103/jrms.JRMS_68_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rafiemanesh H, Maleki F, Mohammadian-Hafshejani A, Salemi M, Salehiniya H. The trend in histological changes and the incidence of esophagus cancer in Iran (2003-2008) Int J Prev Med. 2016;7:31. doi: 10.4103/2008-7802.175990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeinalian M, Eshaghi M, Sharbafchi MR, Naji H, Marandi SM, Asgary S. A comparative study on cancer prevention principles between Iranian traditional medicine and classic medicine. Int J Prev Med. 2016;7:61. doi: 10.4103/2008-7802.179508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miles A, Cockburn J, Smith RA, Wardle J. A perspective from countries using organized screening programs. Cancer. 2004;101:1201–13. doi: 10.1002/cncr.20505. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro S, Coleman EA, Broeders M, Codd M, de Koning H, Fracheboud J, et al. Breast cancer screening programmes in 22 countries: Current policies, administration and guidelines. Int J Epidemiol. 1998;27:735–42. doi: 10.1093/ije/27.5.735. [DOI] [PubMed] [Google Scholar]
- 11.van Ballegooijen M, Van Den Akker-van Marle E, Patnick J, Lynge E, Arbyn M, Anttila A, et al. Overview of important cervical cancer screening process values in European Union (EU) countries, and tentative predictions of the corresponding effectiveness and cost-effectiveness. Eur J Cancer. 2000;36:2177–88. doi: 10.1016/s0959-8049(00)00330-0. [DOI] [PubMed] [Google Scholar]
- 12.Adab P, McGhee SM, Yanova J, Wong CM, Hedley AJ. Effectiveness and efficiency of opportunistic cervical cancer screening: Comparison with organized screening. Medical Care. 2004;42:600–9. doi: 10.1097/01.mlr.0000128007.04494.29. [DOI] [PubMed] [Google Scholar]
- 13.Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low-and middle-income developing countries. Bull World Health Organ. 2001;79:954–62. [PMC free article] [PubMed] [Google Scholar]
- 14.Pontén J, Adami HO, Bergström R, Dillner J, Friberg LG, Gustafsson L, et al. Strategies for global control of cervical cancer. Int J Cancer. 1995;60:1–26. doi: 10.1002/ijc.2910600102. [DOI] [PubMed] [Google Scholar]
- 15.Joulaei H, Zarei N. Women's cancer care in Iran. Cancer Control. 2019;26:1073274819848432. doi: 10.1177/1073274819848432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akbari F, Shakibazadeh E, Pourreza A, Tavafian S. Barriers and facilitating factors for cervical cancer screening: A qualitative study from Iran. Iran J Cancer Prev. 2010;3:178–84. [Google Scholar]
- 17.Allahverdipour H, Asghari-Jafarabadi M, Emami A. Breast cancer risk perception, benefits of and barriers to mammography adherence among a group of Iranian women. Women Health. 2011;51:204–19. doi: 10.1080/03630242.2011.564273. [DOI] [PubMed] [Google Scholar]
- 18.Allahverdipour H, Emami A. Perceptions of cervical cancer threat, benefits, and barriers of Papanicolaou smear screening programs for women in Iran. Women Health. 2008;47:23–37. doi: 10.1080/03630240802132302. [DOI] [PubMed] [Google Scholar]
- 19.Ghourchaei A, Charkazi A, RazzaqNejad A. Knowledge, practice and perceived threat toward breast cancer in the women living in Gorgan, Iran. J Res Dev Nurs Midwifery. 2013;10:25–32. [Google Scholar]
- 20.Hajializadeh K, Ahadi H, Jomehri F, Rahgozar M. Health beliefs and screening behavior of cervical cancer among the women of Bandar Abbas. Life Sci J. 2013;10:545–51. [Google Scholar]
- 21.Hasani L, Aghamolaei T, Tavafian S, Zare S. Constructs of the health belief model as predicting factors in breast self-examination. Hayat. 2011;17:62–9. [Google Scholar]
- 22.Jalilian F, Emdadi S. Factors related to regular undergoing Pap-smear test: Application of theory of planned behavior. J Res Health Sci. 2011;11:103–8. [PubMed] [Google Scholar]
- 23.Montazeri A, Haji-Mahmoodi M, Jarvandi S. Breast self-examination: Do religious beliefs matter.A descriptive study? J Public Health. 2003;25:154–5. doi: 10.1093/pubmed/fdg031. [DOI] [PubMed] [Google Scholar]
- 24.Moodi M, Rezaeian M, Mostafavi F, Sharifirad GR. Determinants of mammography screening behavior in Iranian women: A population-based study. J Res Med Sci. 2012;17:750–9. [PMC free article] [PubMed] [Google Scholar]
- 25.Rezaee Ghazdehi M, Amini L, Parvizi S, Hoseyni AF. Attitudinal barriers to mammography screening among women in Tehran. J Mazandaran Univ Med Sci. 2013;23:69–75. [Google Scholar]
- 26.Sadatjediarani T, Akbari H, Hasanbeigi O, Askari Z. The study of preventive and impeller factors of prevalent cancers screening tests in women in Kashan during 2013. SJIMU. 2015;22:56–66. [Google Scholar]
- 27.Soltan Ahmadi Z, AbbasZadeh A, Tirgari B. Survey on the rate and causes of women's participation or nonparticipation in breast and cervical cancers screening program. IJOGI. 2010;13:37–46. [Google Scholar]
- 28.Teymoori P, Habibi S. Application of a health belief model for explaining mammography behavior by using structural equation model in women in Sanandaj. SJKU. 2014;19:103–15. [Google Scholar]
- 29.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zoorob R, Anderson R, Cefalu C, Sidani M. Cancer screening guidelines. Am Family Phys. 2001;63:1101–12. [PubMed] [Google Scholar]
- 31.Akbari H, Arani TJ, Gilasi H, Moazami A, Gharlipour Z, Gholinpour AA, et al. Study of motivational factors and causes of nonparticipation to breast and cervical cancer screening tests among women attending health centers in Kashan city. Ilam Univ Med Sci. 2014;22:137–48. [Google Scholar]
- 32.Allahverdipour H, Emami A. Perceptions of cervical cancer threat, benefits, and barriers of Papanicolaou smear screening programs for women in Iran. Women Health. 2008;47:23–37. doi: 10.1080/03630240802132302. [DOI] [PubMed] [Google Scholar]
- 33.Ghaoomi M, Aminimoghaddam S, Safari H, Mahmoudzadeh A. Awareness and practice of cervical cancer and Pap smear testing in a teaching hospital in Tehran. Tehran Univ Med J. 2016;74:183–9. [Google Scholar]
- 34.Ghazdehi MR, Amini L, Parvizi S, Hoseyni AF. Attitudinal barriers to mammography screening among women in Tehran. J Mazandaran Univ Med Sci. 2013;23:69–75. [Google Scholar]
- 35.Hasani L, Aghamolaei T, Tavafian SS, Zare S. Constructs of the health belief model as predicting factors in breast self-examination. HAYAT. 2011;17:84. [Google Scholar]
- 36.Saberi F, Sadat Z, Abedzadeh M. Factors associated with cervical cancer screening and its barriers among women: Kashan, Iran. Payesh. 2012;11:365–70. [Google Scholar]
- 37.Soltanahmadi Z, Abbaszadeh A, Tirgari B. A survey on the rate and causes of women's participation or nonparticipation in breast and cervical cancers screening programs. Iran J Obstet Gynecol Infertil. 2010;13:37–46. [Google Scholar]
- 38.Banaeian S, Kazemian A, Kheiri S. Knowledge, attitude and practice about breast cancer screening and related factors among women referred to health care centers in Boroujen in 2005. J Shahrekord Univ Med Sci. 2006;7:28–34. [Google Scholar]
- 39.Mokhtari L, Khorami Markani A, Habibpoor Z. Correlation between health beliefs and breast cancer early detection behaviors among females referring to health centers in Khoy city, Iran. J Health Promotion Manag. 2014;3:56–64. [Google Scholar]
- 40.Rejali M, Yadegarfar G, Mostajeran M, Aghdak P, Fadaei R, Ansari R. Evaluation of the status of breast cancer screening in women in isfahan province, Iran. J Health Syst Res. 2018;13:415–21. [Google Scholar]
- 41.Naghibi SA, Shojaizadeh D, Yazdani Cherati J, Montazeri A. Breast cancer preventive Behaviors among Iranian women: A systematic review. Payesh. 2015;14:181–91. [Google Scholar]
- 42.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moghaddam Tabrizi F, Vahdati S, Khanahmadi S, Barjasteh S. Determinants of breast cancer screening by mammography in women referred to health centers of Urmia, Iran. Asian Pac J Cancer Prev. 2018;19:997–1003. doi: 10.22034/APJCP.2018.19.4.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmadipour H, Sheikhizade S. Breast and cervical cancer screening in women referred to urban healthcare centers in Kerman, Iran, 2015. Asian Pac J Cancer Prev. 2016;17:143–7. doi: 10.7314/apjcp.2016.17.s3.143. [DOI] [PubMed] [Google Scholar]
- 45.Parsa P, Mirmohammadi A, Khodakarami B, Roshanaiee G, Soltani F. Effects of breast self-examination consultation based on the health belief model on knowledge and performance of Iranian women aged over 40 years. Asian Pac J Cancer Prev. 2016;17:3849–54. [PubMed] [Google Scholar]
- 46.Parsa P, Sharifi F, Shobeiri F, Karami M. Effects of group counseling based on health belief model on cervical cancer screening beliefs and performance of rural women in Kaboudrahang, Iran. Asian Pac J Cancer Prev. 2017;18:1525–30. doi: 10.22034/APJCP.2017.18.6.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghahramani M, Alami A, Moghaddam HM, Moodi M. Screening for cervical cancer: An educational intervention based on transtheoretical models and health belief in women of Gonabad, Iran. Iran J Obstet Gynecol Infertil. 2018;21:22–32. [Google Scholar]
- 48.Rezaeian M, Sharifirad G, Mostafavi F, Moodi M, Abbasi MH. The effects of breast cancer educational intervention on knowledge and health beliefs of women 40 years and older, Isfahan, Iran. J Educ Health Promot. 2014;3:43. doi: 10.4103/2277-9531.131929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Termeh Zonouzy V, Niknami S, Ghofranipour F, Montazeri A. An educational intervention based on the extended parallel process model to improve attitude, behavioral intention, and early breast cancer diagnosis: A randomized trial. Int J Women's Health. 2019;11:1–10. doi: 10.2147/IJWH.S182146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mousavi SM, Harirchi I, Ebrahimi M, Mohagheghi MA, Montazeri A, Jarrahi AM, et al. Screening for breast cancer in Iran: A challenge for health policy makers. Breast J. 2008;14:605–6. doi: 10.1111/j.1524-4741.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 51.Asadzadeh VF, Broeders M, Kiemeney L, Verbeek A. Opportunity for breast cancer screening in limited resource countries: A literature review and implications for Iran. Asian Pac J Cancer Prev. 2011;12:2467–75. [PubMed] [Google Scholar]
- 52.Shrivastava SR, Shrivastava PS, Ramasamy J. Screening of cervical cancer: Barriers and facilitators. Iran J Cancer Prev. 2013;6:177. [PMC free article] [PubMed] [Google Scholar]