Abstract
Background:
Sexually transmitted infections (STIs) are dynamic and show a variable prevalence in different parts of the country. Moreover, the prevalence changes with time in the same geographical area. It is important to have the knowledge of current trend of STIs and partner notification (PN) rate in a particular area for the effective implementation of preventive and control measures.
Aims:
This study aimed to assess the changing demographic and clinical trends of STIs in the patients attending a tertiary care center in North India.
Materials and Methods:
This study was conducted at STI clinic located at a tertiary care center in North India. All the patients visiting STI clinic over a 5-year period from January 1, 2013, to December 31, 2017, were included in our study. Diseases were diagnosed on the basis of detailed history, clinical examination, and relevant investigations, and PN was done using the patient-oriented notification method.
Results:
The most common STI affected age group was 25–44 years (45.11%), and the most common STI noted was candidal balanoposthitis in males (19.49%) and candidal vaginal discharge in females (20.54%), followed by herpes genitalis (15.04%) and condylomata acuminata (14.66%) in both the genders. Bacterial STIs such as syphilis (1.58%), lymphogranuloma venereum (0.45%), and chancroid (0.39%) were less common. The average PN rate was 42.48%.
Conclusion:
In the present study, fungal and viral STIs showed an upward trend, whereas bacterial STIs such as syphilis and chancroid demonstrated a declining trend. The measures to improve PN are urgently required for both cure and the prevention of STIs.
Keywords: Changing trends, partner notification, sexually transmitted infections
INTRODUCTION
Sexually transmitted infections (STIs) are the most common among notifiable diseases.[1] STIs are more dynamic than other diseases prevailing in the community. Their epidemiological profile varies from country to country and from one region to another within a country, depending on ethnographic, demographic, socioeconomic, and health factors. The clinical pattern is also a result of the interaction among pathogens; the behaviors that mediate their transmission and the effectiveness of preventive and control interventions.[2]
HIV infection, a global pandemic has affected the approach to the treatment of STIs very significantly, as the most important mode of HIV transmission is sexual, and the STIs also play a facilitative role in the acquisition and transmission of HIV. Moreover, the natural history, manifestations, and treatment of classic sexually transmitted diseases may be altered by the concurrent HIV infection.[3]
Partner notification (PN) for STIs has been recommended as an important step in STI management to interrupt the transmission of infections and prevent potential reinfection and complications. PN provides an opportunity to make index patients aware of risk-reduction strategies for avoiding STIs, enables earlier diagnosis for partners, motivate behavior change in clients and partners, and reduce the burden of disease in communities.[4]
The present study was designed to identify the demographic and clinical changes at an STI clinic and to assess the trend of STI among HIV patients and PN rate in-clinic attendees.
MATERIALS AND METHODS
In this retrospective study conducted over a period of 5 years from January 1, 2013, to December 31, 2017, 7321 patients attending the STI clinic located at a tertiary care center in North India were clinically evaluated by trained physicians for STIs. The serological tests such as ELISA, rapid tests for HIV, and venereal disease research laboratory for syphilis and fasting blood sugar (to rule out diabetes) were done routinely. Specific on-site laboratory examinations for STIs (Gram's stain, culture, Tzanck smear, potassium hydroxide and wet mount preparations, and dark-ground microscopy) were performed wherever required.
The following data were collected on the clinical pro forma at the first visit: (1) demographic information – age, gender, and marital status, (2) sexual history – last sexual contact, single or multiple partners, (3) clinical information – complaints at the time of presentation (ulcers, discharge, growths on genitalia, pain, pruritus, fever, and swelling), duration, and history of previous treatment, and (4) clinical diagnosis and treatment.
PN was done using patient-oriented notification methods, in which index patient notifies their partner.
RESULTS
Among the total of 7321 patients with complaints of genital lesions attending the STI clinic included in this study, 5305 (72.46%) were male and 2016 (27.53%) were female with a ratio of 2.63 (M):1 (F). The most common age group involved was 25–45 years, including 3303 (45.11%) patients. In our study, 81.2% of attendees were married. Multiple sex partners were found in 37.5% of patients.
Our study showed an increasing number of patients attending the STI clinic over a period of 5 years. Nine hundred (12.29%) patients attended the STI clinic in 2013 and the number increased to 2627 (35.88%) by the year 2017 [Table 1].
Table 1.
Year-wise age and sex distribution of sexually transmitted infections clinic attendees
| <25 years | 25–45 years | >45 years | ||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| 2013 | 140 | 51 | 315 | 161 | 194 | 39 |
| 2014 | 140 | 46 | 301 | 177 | 272 | 59 |
| 2015 | 150 | 44 | 401 | 207 | 221 | 48 |
| 2016 | 323 | 79 | 607 | 291 | 342 | 86 |
| 2017 | 621 | 185 | 755 | 388 | 525 | 153 |
In males, the most common STI noted was candidal balanoposthitis followed by herpes genitalis, condylomata acuminata and least common STI was chancroid. In females, the most common STI was candidal vaginal discharge followed by genital herpes, condylomata acuminata and least common STI was chancroid [Table 2].
Table 2.
Sexually transmitted infections in males and females
| STI | Males | Females | Total (%) |
|---|---|---|---|
| Candidal balanoposthitis | 1292 | - | 1292 (19.49) |
| Vaginal discharge | |||
| Candidal | - | 1061 | 1361 (20.54) |
| Bacterial vaginosis | - | 153 | |
| Trichomoniasis | - | 47 | |
| Herpes genitalis | 729 | 268 | 997 (15.04) |
| Condylomata accuminata | 721 | 251 | 972 (14.66) |
| Genital scabies | 707 | 163 | 870 (13.13) |
| Molluscum contagiosum | 485 | 125 | 610 (9.20) |
| Nongonococcal urethritis | 246 | 111 | 357 (5.38) |
| Gonococcal urethritis | 83 | 23 | 106 (1.59) |
| Syphilis | 64 | 41 | 105 (1.58) |
| LGV | 25 | 5 | 30 (0.45) |
| Chancroid | 23 | 3 | 26 (0.39) |
| Total | 4375 | 2251 | 6626 |
STI=Sexually transmitted infections; LGV=Lymphogranuloma venereum
Many patients who attended the STI clinic were found to have non-STI conditions and psycho-sexual problems [Table 3].
Table 3.
Non-sexually transmitted infections conditions in sexually transmitted infection clinic attendees
| Non-STI condition | Males | Female |
|---|---|---|
| Intertrigo | 148 | 89 |
| Tinea cruris | 103 | 52 |
| Pearly penile papule | 126 | - |
| Scrotal dermatitis | 82 | - |
| Erectile dysfunction | 43 | - |
| Vulval pruritus | - | 33 |
| LSEA/BXO | 10 | 9 |
STIs=Sexually transmitted infections; LSEA=Lichen Sclerosus et atrophicus; BXO=Balanitis Xerotica Obliterans
A total of 438 clinic attendees were HIV positive. The most common STI noted in the HIV patients (both males and females) was herpes genitalis followed by condylomata acuminata [Table 4].
Table 4.
Sexually transmitted infections in HIV patients
| STIs | Males | Females |
|---|---|---|
| Genital herpes | 94 | 43 |
| Condylomata accuminata | 67 | 28 |
| Balanoposthitis | 59 | - |
| Genital molluscum | 45 | 16 |
| Syphilis | 25 | 11 |
| Vaginal discharge | - | 31 |
| Chancroid | 6 | 1 |
| LGV | 9 | 3 |
| Total | 305 | 133 |
LGV=Lymphogranuloma venereum; STIs=Sexually transmitted infections
A significant number of patients also attended the STI clinic with venereophobia (morbid fear of venereal disease), which was more common among the males 447 (5.68%) than the females 166 (2.11%).
Average PN reported in our study was 42.48%. Among HIV patients, PN was high which was 89.72% (393/438) [Figure 1].
Figure 1.
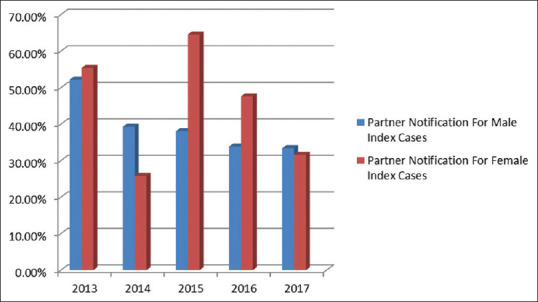
Partner notification in sexually transmitted infection cases
DISCUSSION
This study reports an increase in the number of patients attending our STI clinic, contrary to the data reported by Jaiswal et al., Ray et al., and Banger et al. in different parts of North India.[5,6,7] This is attributed to increasing health education coverage because of efforts from various governmental and nongovernmental organizations and referrals from peripheral STI centers. In the present study, males (72.46%) outnumbered the females (27.53%), which was in accordance with the earlier studies by Sharma et al., Saikia et al., and others but was contradictory to the studies done by Singh S et al. and Sharma A et al. where female patients were in majority.[1,8,9,10,11,12,13,14,15,16,17,18,19]
In our study, the total number of female patients increased over the 5-year period, as in recent years, married men have been encouraged to motivate their regular sexual partners (often the spouse) to receive STI testing and care. Male-to-female ratio did not change much, being 2.58:1 in 2013 and 2.61:1 in 2017.
The most common STI found was candidal infection (balanoposthitis in males and candidal vaginal discharge in females) followed by viral STIs (herpes genitalis and condylomata acuminata). Although contrary to the findings in most of the other studies where either viral or bacterial STI was common, this was in accordance with a study conducted by Arakkal et al.[20]
Behavioral risk factors that have been significantly associated with a higher incidence of vaginal candidiasis include frequent sexual intercourse and receptive oral sex as well as the use of high-estrogen (not low dose) oral contraceptives and spermicides. Host-related risk factors that have been significantly associated with candidiasis include antibiotic use, uncontrolled diabetes, conditions with high reproductive hormone levels, immunosuppression, and genetic predisposition. Being uncircumcised is an additional predisposing factors for candidal balanoposthitis.[21] Unless proved due to other medical causes such as diabetes, we considered candidal balanoposthitis and candidal vaginal discharge to be an STI.
The comparison with an earlier study from the same institute by Chopra et al. and other studies from North India by Ray et al. and Banger et al. is shown in Table 5.[6,7,22]
Table 5.
Comparison with other studies
| Sexually transmitted infection | Chopra et al.[22] | Ray et al.[6] (2002–2004) | Banger et al.[7] (2007–2014) | Present Study (2013–2017) | |
|---|---|---|---|---|---|
| 1983–1988 | 1990–1998 | ||||
| Syphilis (%) | 29.6 | 17.2 | 24.2 | 2.06 | 1.58 |
| Vaginal discharge (%) | 15 | 19.5 | 8.6 | 12.35 | 20.4 |
| Condyloma accuminata (%) | 12 | 5.1 | 18.1 | 10.61 | 14.66 |
| Genital herpes (%) | 11.6 | 5.5 | 22.4 | 21.75 | 15.04 |
| Gonorrhea (%) | 10 | 4.24 | 15.4 | 0.33 | 1.59 |
| Chancroid (%) | 8.8 | 1.6 | 5.4 | 1.10 | 0.39 |
| Balanoposthitis (%) | 5.4 | 9.4 | - | 24 | 19.49 |
| NGU (%) | 5.2 | 10.8 | 2.8 | 2.37 | 5.38 |
| LGV (%) | 0.2 | 0.15 | 0.2 | 0.17 | 0.45 |
NGU=Non-Gonococcal urethritis; LGV=Lymphogranuloma venereum
Declining the prevalence of bacterial infections may be due to the increasing sexual health awareness, indiscriminate use of antibiotics, and syndromic management of the infections by the physicians. Viral infections are more commonly seen because of their persistence and recurrences.
Average PN was 42.48% of total index cases during the study period. Low PN can be because of the patient-oriented method used for PN. The use of alternative notification methods, including provider-oriented and mixed approach (both patient and provider-oriented) increases the rate of PN, but these are costly and require more advanced infrastructure. Stigmatization and discrimination against people with STI undermine their ability to seek care and their willingness to notify spouses or other partners of their STI infection status.[4]
PN was relatively higher (44.98%) when index cases were females and lower (39.36%) when index cases were males. This can be attributed to higher incidences of multiple sexual partners, paid sex, and risk-taking behavior in males as compared to females. The main barriers for women to notify partners included (1) their husband worked in a different town; (2) fear that their husband will accuse them of being the source of the STI; and (3) fear of divorce. Married men reported following barriers to notifying their wives: (1) the wife lived in a rural area, (2) embarrassment, (3) fear of loss of respect, and (4) fear of disharmony in the family.[4] The high rate of PN was seen among HIV patients, which can be because of fear of fatal disease in spouse and children.
CONCLUSION
STIs constitute a major public health problem and are responsible for significant morbidity in both men and women. At the same time, a number of STI patients are rising, with a shift in the type of STIs. The present study concluded that fungal STIs (candidal balanoposthitis and vulvovaginitis) and viral STIs (herpes genitalis and condylomata acuminata) are on the rise and bacterial STIs (syphilis and chancroid) are declining. The measures to improve PN are required for cure as well as the prevention of STI. Counseling of index STI patients is particularly useful in terms of raising the awareness of PN, eliminating stigma and fear related to STIs, and should be promoted in both public and private STD clinics. The main strategy aimed at achieving the effective management for people with established infections has been to integrate STD services into the existing health-care system and syndromic management recommended by the National AIDS Control Organization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Singh S, Badaya S, Agrawal D. Current socioclinical trend of sexually transmitted diseases and relevance of STD clinic: A comparative study from referral tertiary care center of Gwalior, India. Drug Dev Ther. 2014;5:134–8. [Google Scholar]
- 2.Thappa DM, Kaimal S. Sexually transmitted infections in India: Current status (except human immunodeficiency virus/acquired immunodeficiency syndrome) Indian J Dermatol. 2007;52:78–82. [Google Scholar]
- 3.Chopra D, Sandhu I, Bahl RK, Bhatia R, Goyal A. Prevalence of sexually transmitted infections in HIV positive and HIV negative females, in a tertiary care hospital-An observational study. Indian J Sex Transm Dis AIDS. 2015;36:59–63. doi: 10.4103/2589-0557.156730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alam N, Chamot E, Vermund SH, Streatfield K, Kristensen S. Partner notification for sexually transmitted infections in developing countries: A systematic review. BMC Public Health. 2010;10:19. doi: 10.1186/1471-2458-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaiswal AK, Banerjee S, Matety AR, Grover S. Changing trends in sexually transmitted diseases in North Eastern India. Indian J Dermatol Venereol Leprol. 2002;68:65–6. [PubMed] [Google Scholar]
- 6.Ray K, Bala M, Gupta SM, Khunger N, Puri P, Muralidhar S, et al. Changing trends in sexually transmitted infections at a Regional STD Centre in north India. Indian J Med Res. 2006;124:559–68. [PubMed] [Google Scholar]
- 7.Banger HS, Sethi A, Malhotra S, Malhotra SK, Kaur T. Clinico-epidemiological profile of patients attending Suraksha clinic of Tertiary care hospital of North India. Indian J Sex Transm Dis AIDS. 2017;38:54–9. doi: 10.4103/2589-0557.203436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma S, Tiwari S, Paliwal V, Mathur DK, Bhargava P. Study of patterns of sexually transmitted diseases using a syndromic approach in the era of human immunodeficiency virus from a tertiary care hospital of the Northern India. Indian J Sex Transm Dis AIDS. 2015;36:158–61. doi: 10.4103/2589-0557.167157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saikia L, Nath R, Deuori T, Mahanta J. Sexually transmitted diseases in Assam: An experience in a tertiary care referral hospital. Indian J Dermatol Venereol Leprol. 2009;75:329. doi: 10.4103/0378-6323.51245. [DOI] [PubMed] [Google Scholar]
- 10.Zamzachin G, Singh NB, Devi TB. STD trends in regional institute of medical sciences, Manipur. Indian J Dermatol Venereol Leprol. 2003;69:151–3. [PubMed] [Google Scholar]
- 11.Krishnamurthy VR, Ramachandran V. STD trends in Chengalpattu hospital. Indian J Dermatol Venereol Leprol. 1996;62:3–12. [PubMed] [Google Scholar]
- 12.Kumar B, Sharma VK, Malhotra S, Bakaya V. Pattern of sexually transmitted diseases in Chandigarh. Indian J Dermatol Venereol Leprol. 1987;53:286–91. [PubMed] [Google Scholar]
- 13.Nair TG, Asha LK, Leelakumari PV. An epidemiological study of sexually transmitted diseases. Indian J Dermatol Venereol Leprol. 2000;66:69–72. [PubMed] [Google Scholar]
- 14.Jain VK, Dayal S, Aggarwal K, Jain S. Changing trends of sexually transmitted diseases at Rohtak. Indian J Sex Transm Dis. 2008;29:23–5. [Google Scholar]
- 15.Choudhry S, Ramachandran VG, Das S, Bhattacharya SN, Mogha NS. Pattern of sexually transmitted infections and performance of syndromic management against etiological diagnosis in patients attending the sexually transmitted infection clinic of a tertiary care hospital. Indian J Sex Transm Dis AIDS. 2010;31:104–8. doi: 10.4103/2589-0557.74998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Devi SA, Vetrichevvel TP, Pise GA, Thappa DM. Pattern of sexually transmitted infections in a tertiary care centre at Puducherry. Indian J Dermatol. 2009;54:347–9. doi: 10.4103/0019-5154.57611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vora R, Anjaneyan G, Doctor C, Gupta R. Clinicoepidemiological study of sexually transmitted infections in males at a rural-based tertiary care center. Indian J Sex Transm Dis. 2011;32:86–9. doi: 10.4103/2589-0557.85410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hassan I, Anwar P, Rather S, Sameem F, Majid I, Jabeen Y, et al. Pattern of sexually transmitted infections in a Muslim majority region of North India. Indian J Sex Transm Dis AIDS. 2015;36:30–4. doi: 10.4103/2589-0557.156697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma A, Rattan R, Sood A. Pattern of sexually transmitted infections in a district hospital from Himachal Pradesh. Int J Community Med Public Health. 2017;4:1028–31. [Google Scholar]
- 20.Arakkal GK, Damarla SV, Kasetty HK, Chintagunta SR. Changing trends in sexually transmitted infection (STI) clinic attendees – Current scenario. Int J Med Sci Public Health. 2014;3:1215–8. [Google Scholar]
- 21.Achkar JM, Fries BC. Candida infections of the genitourinary tract. Clin Microbiol Rev. 2010;23:253–73. doi: 10.1128/CMR.00076-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chopra A, Mittal RR, Singh P, Sharma P. Pattern of sexually transmitted diseases at Patiala. Indian J Sex Transm Dis. 1990;11:43–5. [PubMed] [Google Scholar]


