Abstract
Background:
With the successful introduction of ART, the life expectancy of children living with HIV (CLHIV) is substantially increased. However, strict compliance is a necessary step to begin with as noncompliance is again associated with its own demerits of incomplete suppression and decreasing the overall survival of the patients.
Aims:
The aim of this study was to measure factors associated with adherence to ART among CLHIV.
Materials and Methods:
This is a 1-year follow-up study conducted from November 2012 to December 2013. A total of 171 children between 18 months and 15 years living with HIV and on ART attending the two ART centers of Delhi were enrolled in the study. Adherence and factors affecting adherence were obtained from the study participants using a semi-structured interview schedule.
Statistical Analysis Used:
Collected data were transformed into variables and analyzed into SPSS. All observations were in terms of mean, median, standard deviations, percentages, and proportions. Tests of significance such as Chi-square test and t-test were applied wherever required.
Results:
In nearly 89% of the study participants, adherence to ART was ≥95% at the end of the study. The most common reason for nonadherence was forgetfulness (59%), and 57% of the parents/caretakers were facing monetary problems. Long distance, greater duration to reach center, and unavailability of the parents/caretakers were also quoted as problems.
Conclusion:
Adherence is genesis to successful treatment outcome and is strongly associated with availability of support by their parents/caretakers. Professional help along with guidance and encouragement is required not only at the caretaker level but also to the family as a whole.
Keywords: Adherence, ART, children, highly active antiretroviral treatment, HIV, India
INTRODUCTION
Antiretroviral Treatment (ART) has substantially changed the face of HIV infection where it has been successfully introduced. Now, with the introduction of ART, many children are surviving to adolescence and even adulthood.[1]
The free antiretroviral therapy (ART) initiative, launched on April 1, 2004, by the National AIDS Control Programme (NACP) in India, was a turning point in HIV care which brought hopes to lives of people living with HIV (PLHIV) in India. The program adopted a public health approach for the provision of ART and provides comprehensive prevention, care, and treatment services, with a standardized, simplified combination of ART regimens, a regular secure supply of good quality antiretroviral (ARV) drugs, and a robust monitoring and evaluation system. Through efficient planning and rapid scale-up over the years, the number of ART centers has expanded almost logarithmically, and 512 ART centers and 1080 link ART centers were functioning in 2015. These centers provide ART to over 880,000 PLHIV, which is the second highest number anywhere in the world. Wider access to ART has led to a 29% reduction in estimated annual AIDS-related deaths between 2007 and 2011.[2] In 2016, there were an estimated 2.1 million (1.7 million–2.6 million) children (<15 years) living with HIV (CLHIV) who continue to experience persistent treatment gaps. HIV treatment coverage for children (43% [30%–54%]) is far less than coverage for adults (54% [40%–65%]) in 2016.[2] Thus, there is a crucial and significant need to provide ART for children who become infected regardless of all the attempts made to prevent the spread of HIV infection.[3]
Children differ from adults in that they have high rates of viral replication, high rates of CD4+ cell destruction, more chance of viral mutation, faster rate of disease progression, and good immunologic response to highly active ARV treatment (HAART). ARV drugs suppress viral replication and thus prevent mutant forms from developing. However, if ARVs are not taken/taken at low doses, then due to suboptimal level of ARVs, incomplete suppression occurs. Incomplete suppression leads to more replication, added opportunity for mutations to arise, and thus further chances that drug-resistant HIV strain will emerge and treatment failure occurs.[4,5] Failure refers to the loss of antiviral efficacy and triggers the switch of the entire regimen from first to more expensive, and often unavailable, second-line regimens.[6] It is identified by clinical and/or immunological and/or virological monitoring. The recurrence of severe malnutrition that is not caused by a lack of food in children receiving ART may indicate treatment failure and the need to switch therapy.[7] Other causes of treatment failure besides drug resistance can be nonadherence, impaired drug absorption, drug interactions, or altered drug pharmacokinetics.[7] Other than that, side effects can be mild or severe due to the toxicity profiles of the ARV drugs used in substitution and second-line ART regimens. Adherence is, therefore, a genesis of viral load suppression, a decrease in morbidity/mortality, and a backbone to successful ART treatment.[8,9,10,11,12,13,14,15,16,17]
Infants and children are dependent on adults for timely and correct doses of medicines. Each child must be directly observed to swallow the medicine (sometimes they spit it out or keep in the cheeks). Poor adherence can also be due to caretaker's issues, so caretakers must be counseled to see if they have other problems, for example, poor memory, workload, being busy, nonavailability of caretakers, migration, and problem taking ART themselves.[5,18,19,20] Distance, travel time, and costs remain the main constraints to access ART services and adherence to treatment, leading to poor drug adherence, lost to follow-up, and missed cases.
This study aimed to measure the prevalence and factors associated with adherence to ART among caregivers of HIV-infected children in tertiary care hospitals of Delhi.
MATERIALS AND METHODS
Study design
The study is a hospital-based study conducted in antiretroviral treatment (ART) centers of two tertiary care hospitals in New Delhi. The study was carried out from November 2012 to December 2013. Enrollment of the cases was done from November 2012 to December 2012; thereafter, quarterly follow-up was done for each child during the course of 12 months. The study population comprised all children between 18 months and <15 years of age living with HIV and on HAART attending the ART centers. One hundred and seventy-one CLHIV of 18 months to <15 years and residents of Delhi were recruited.
Data were collected after obtaining approval from the institutional protocol and ethical committee. During enrollment, information about the purpose of the study was conveyed to their parents/caretakers. Enrollment was voluntary. On consenting to participate in the study, written consent was taken from their parents/primary caretaker if literate; otherwise, the left thumb impression in front of a witness was taken. For children >7 years, assent was also taken. The confidentiality of enrolled children and their parents/primary caretakers was maintained. Interview of primary caretakers was taken for children <10 years of age, whereas in children ≥10 years, interview of children as well as primary caretakers was taken.
Information regarding sociodemographic profile and factors affecting response to HAART was obtained from the study participants using a semi-structured interview schedule. Details which might affect response to HAART, for example, age of the children, socioeconomic status, caretaker's education, duration of ART drug intake, method of reminder used to take medicines at home, adherence to ART drugs, and problems faced by the parents/caretakers in seeking services from the ART center or at home in giving medicines to the child were also assessed and compiled during the follow-up period. Adherence was recorded by a pill-counting method and was classified as optimal (95%) and suboptimal (<95% adherence). Mean adherence was calculated for the study period which was used for statistical analysis.
Data analysis
Collected data were transformed into variables, coded, and entered into SPSS version 17 SPSS Statistics for Windows, Version 17.0 (SPSS Inc. Chicago). Data were entered and analyzed using SPSS. All observations were in terms of mean, median, standard deviations, percentages, and proportions. Tests of significance such as Chi-square test and t-test were applied for comparisons wherever required. P <0.05 was considered statistically significant at 95% confidence level.
RESULTS
Nearly 67.8% of the study participants were boys. Socioeconomic status and type of family were assessed in 169 participants as 2 children were living in a nongovernmental organization (NGO). Approximately 74% of the study participants belonged to upper lower socioeconomic status, and 65.7% were living in a nuclear family. More than four-fifth of the study participants (86%) were taken care of by their biological parents. Other caretakers of the children included adopted parents (4), maternal/paternal uncle or aunt (8), elder brother (1), and NGO (2) [Table 1].
Table 1.
Distribution of study participants according to sociodemographic factors (n=171)
| Sociodemographic factors | Study participants, n (%) |
|---|---|
| Age | |
| 18 months-<5 years | 48 (28.1) |
| 5 years-<15 years | 123 (71.9) |
| Gender | |
| Boys | 116 (67.8) |
| Girls | 55 (32.2) |
| Socioeconomic status* (n=169)# | |
| Upper | 7 (4.1) |
| Upper middle | 14 (8.3) |
| Lower middle | 23 (13.6) |
| Upper lower** | 125 (74) |
| Type of family (n=169)# | |
| Nuclear family | 111 (65.7) |
| Joint family | 58 (34.3) |
| Schooling status (n=123) | |
| Going to school | 111 (90.2) |
| Not attending school | 12 (9.8) |
| Orphan status | |
| Both parents alive | 103 (60.2) |
| Single parent alive | 48 (28.1) |
| Both parents dead | 20 (11.7) |
| Primary caretakers of study participants | |
| Parents | 147 (86.0) |
| Grandparents | 9 (5.3) |
| Other relatives | 15 (8.8) |
| HIV status of parents | |
| Mother positive | 137 (80.1) |
| Father positive | 129 (75.4) |
| Both parents positive | 127 (74.3) |
| One parent positive | 12 (7.0) |
| None positive | 26 (15.2) |
| Unknown | 6 (3.5) |
*Modified Kuppuswamy scale; #One study participant lived in NGO; **Three study participants of lower socioeconomic status. NGO=Nongovernmental organization
The schooling status of 123 study participants was assessed as participants of <5 years were not considered to be eligible for going to primary school. Ninety percent of the eligible children were going to school, and only 12 were not attending school, reason being ill health (9/12 or 75%): prolonged sickness (5), optic atrophy and HIV encephalopathy (1), Down syndrome (1), mental retardation (1), and inability to speak and epilepsy (1). Other reasons were migration (1), not interested in studies (1), and planning for admission (1). Eleven percent of the study participants had lost both of their parents.
Nearly four-fifth of the study participants had HIV-positive mother and three-fourth had HIV-positive father [Table 2]. Both parents were found to be HIV positive in almost three-fourth (127) of the study participants, whereas only 15% (26) of the study participants had both parents HIV negative. The HIV status of a few parents was unknown as these parents had expired. Mothers and fathers of nearly 21% and 29% of children, respectively, had expired [Figure 1]. In nearly 89% of the study participants, adherence to ART was ≥95% at the end of the study ranging from 86.4% to 89.8% from enrollment till the end of the study [Table 3].
Table 2.
HIV status of parents
| n (%) | |
|---|---|
| Mother positive | 137 (80.1) |
| Father positive | 129 (75.4) |
| Both parents positive | 127 (74.3) |
| One parent positive | 12 (7.0) |
| None positive | 26 (15.2) |
| Unknown | 6 (3.5) |
Figure 1.
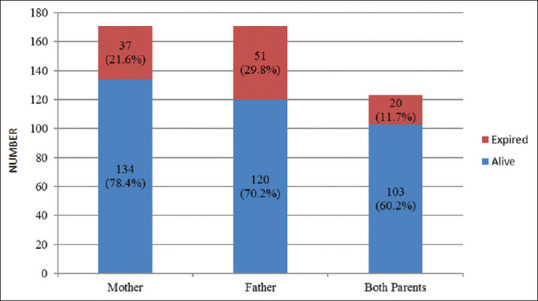
Living status of parents (n = 171)
Table 3.
Adherence of study participants to highly active antiretroviral treatment
| Adherence (%) | Period of study | ||||
|---|---|---|---|---|---|
| Enrollment (n=171), n (%) | First follow-up (n=169)*, n (%) | Second follow-up (n=166)**, n (%) | Third follow-up (n=168)#, n (%) | At the end of study (n=168)†, n (%) | |
| ≥95 | 149 (87.1) | 153 (90.5) | 144 (86.7) | 145 (86.3) | 150 (89.3) |
| <95 | 22 (12.9) | 16 (9.5) | 22 (13.2) | 23 (13.7) | 18 (10.7) |
Losses to follow-up were *2, **5, #3, †2, and 1 transferred out in the last month
More than half of the parents/caretakers felt that though medicines were given free, they were facing monetary problems in collecting medicines from ART centers mainly due to expenses incurred on traveling. Time to reach center and long distances were also quoted as problems. At home, the most common problems felt by a caretaker who missed the pill was forgetfulness in approximately three-fifth of the participants, followed by times when the caretaker was not available at home [Table 4].
Table 4.
Problem faced by parents/caretakers in seeking services from the antiretroviral treatment center and/or in giving medicines to the child at home (n=171)
| Problem faced by parents/caretakers | Study participants, n (%) |
|---|---|
| In seeking services from the art center | |
| Monetary problem | 98 (57.3) |
| Takes time to reach center | 79 (46.1) |
| Traveling long distance from home to center | 65 (38.0) |
| Migration | 15 (8.8) |
| Others | 2 (1.2) |
| At home | |
| Forgetfulness | 101 (59.1) |
| Caretaker was not available | 47 (27.5) |
| Caretaker was busy | 34 (19.9) |
| Child was sick | 27 (15.8) |
| Went to village | 17 (9.9) |
| Child refusal | 15 (8.8) |
| Others* | 19 (11.1) |
Multiple responses. *Child slept early, too many pills
There was a statistically significant association between adherence to HAART and socioeconomic status (P = 0.03) [Table 5], educational level of caretaker (P = 0.04), duration of ART (P = 0.04), and problems faced by the parents/caretakers in giving medicines to the child at home (P = 0.01). A statistical significant association was not seen between adherence to HAART and gender of the study participants (P = 0.56) and problems faced by the parents/caretakers in seeking services from the ART center (P = 0.16).
Table 5.
Factors affecting adherence to highly active antiretroviral treatment (n=168)
| Number of study participants | χ2, P | |||
|---|---|---|---|---|
| Mean adherence | Total (n=168), n (%) | |||
| ≥95 (n=145), n (%) | <95 (n=23), n (%) | |||
| Gender | ||||
| Boy | 99 | 16 | 115 | 0.01, 0.56 |
| Girl | 46 | 7 | 53 | |
| Socioeconomic status (n=166)* | ||||
| Upper + upper middle | 21 | 0 | 21 | 3.87, 0.03 |
| Lower middle + upper lower + lower | 122 | 23 | 145 | |
| Caretaker education | ||||
| Middle school and lower | 97 | 20 | 117 | 3.78, 0.04 |
| High school and above | 48 | 3 | 51 | |
| Duration of ART (months) | ||||
| ≤24 | 24 | 8 | 32 | 4.27, 0.04 |
| >24 | 121 | 15 | 136 | |
| Problems faced by the parents/caretakers in seeking services from the ART center | ||||
| No problem | 28 | 4 | 32 | 0.05, 0.54 |
| Problem faced | 117 | 19 | 136 | |
| Problems faced by the parents/caretakers in giving medicines to the child at home | ||||
| No problem | 89 | 20 | 109 | 5.69, 0.01 |
| Problem faced | 56 | 3 | 59 | |
*=2 children are living in NGO so their Socioeconomic Status is not calculated, ART=Antiretroviral treatment
DISCUSSION
In the present study, three-fourth (74%) of the study participants belonged to upper lower socioeconomic status. An important finding was a high proportion of infected children (90.9%) older than 5 years who were going to school. This shows that perhaps stigma toward HIV has reduced, and parents as well as school authorities have shown a high level of acceptance in providing education to CLHIV. In a study conducted in Ethiopia[21] on HIV-infected 1–14-year-old children, comparatively, a higher percentage of children (25.2%) were reported as not attending school, which can be due to inclusion of all children in their assessment.
Four-fifth of the study participants had HIV-positive mothers, which is similar to other Indian studies.[22] In nearly three-fourth of the study participants, both parents were HIV positive, whereas Chennai study[23] and African study[24] show a relatively lower percentage of HIV-infected parents, indicating that mode of transmission may vary from place to place.
At the time of the study, both parents were alive in almost 60.2% of the study participants, whereas approximately 11.7% of children had lost both parents, which is almost similar to another study in Delhi.[22] However, in a study conducted by Patel et al.[8] (Gujarat, 2012), both parents were alive in 40.8% of the cases, whereas one-quarter of children had lost both parents. In another study by Pol et al.[25] (Karnataka, 2007), 42% of children had a single parent and 12.67% had lost both parents. Such differences can be attributed to the availability, accessibility, and utilization of ART services in different study settings. The increased life expectancy of CLHIV with ART could also be one of the reasons for these findings. Loss of parents means not only the loss of social security and additional financial burden for the family but also adversely affects the physical, mental, and emotional upbringing of these children. Nearly a third of children (29.8%) had lost their fathers, affecting the family economically which may influence medical treatment and regular follow-up. These statistics emphasize the family dimensions of the HIV pandemic. The increasing number of children orphaned due to HIV/AIDS is an emerging crisis in many developing countries.[8,22,24,25]
Caretakers used different mechanisms as reminders to dispense medications on time. Nearly 70% of the caretakers gave the pill on fixed time by watch, whereas 30% coordinated with activities of daily living and rest (11.1%) used an alarm as a reminder to give pill to the child. Almost similar findings were seen in a study conducted in Ethiopia,[21] where the most common reminder was a watch/clock system (62.4%). Another cross-sectional study by Biadgilign et al.[26] reported that watches/clocks were used as a reminder in 46.4% and cellular phone alarm systems was used in 25.4%. In a study done by Davies et al.[27] in Cape Town, maximum (74.7%) caregivers used at least one method to assist in remembering and giving medication, and the most commonly used aids were activities of daily living (40%).
Majority (89.8%) of the study participants had ≥95% adherence to HAART at the end of the study which can be attributed to the adherence counseling session given to the study participants/caretakers at each visit and the clinical benefits apparent to caretakers, motivating them to adhere to the treatment. Adherence to treatment was good and comparable to that reported in other studies (range: 73%–97%) conducted in India and abroad.[7],21,27,[28,29,30,31,32,33,34]
One of the reasons for good adherence could be free ART treatment under NACP. Good relationship and open communication between caretakers and health-care service providers may also contribute to better adherence. Using a reminder to take medicine may also lead to increase in adherence, as shown in some studies.[21,27]
It is critical to focus on maximizing pediatric ART adherence to 100% to ensure the maximum effectiveness of ARV regimens. For better adherence, more counseling tools need to be used to inform the caretakers/patients about the advantages and benefits of high level of drug adherence. Monitoring and evaluation of adherence strategies are important components of any ART program and are useful in determining rates and identifying the key factors that influence adherence.
There are many barriers to ART adherence though children/caretakers do not perceive them consistently. In taking services from the ART center, more than half (57.3%) of the caretakers felt that although medicines were given free, they were facing monetary problems in collecting medicines mainly due to expenses spent on traveling. Time to reach center (46.1%) and long distances to travel from home to ART center (38%) were also some of the problems reported by caretakers. The strategy of the government is to open more link ART centers which can address these problems and reduce out-of-pocket expenses and time to seek ART services.
At home, the most common problem felt by caretakers to miss the pill was forgetfulness (59.1%). Almost similar findings were reported by Ugwu and Eneh,[28] Bhattacharya and Dubey,[29] Buchanan et al.,[35] and White et al.[36] Other issues were caretaker not available at home (26.5%), caretaker was busy (19.6%), and child was sick (16.4%). Other studies also reported similar issues.[29,35,36]
There was a significant association between drug adherence and socioeconomic status of the study participants. Similarly, there was a statistically significant association between adherence to HAART and educational level of caretaker, and this finding was similarly reported by other authors.[27,29,36] Furthermore, it was seen in this study that adherence to HAART significantly increases with increasing duration of ART drugs, as shown in another Indian study.[29] Problems faced by the parents/caretakers in giving medicines to the child at home also significantly affect adherence, which was also reported by Buchanan et al.[35] in the United States.
Although a study by Bhattacharya and Dubey[29] showed that lower adherence is associated with female gender, our study shows no association between drug adherence and gender of the children as seen in some other studies.[35,37]
CONCLUSION
Adherence is a crucial step for utmost effectiveness of ART among pediatric age group and they indirectly rely on their parents/caretakers for their medicine intake. For better adherence consistent counseling and motivation is required at the parents/caretakers end. Counselors should also try to find out the reasons for non-adherence in others. They should also try to fill gaps to maximize adherence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.WHO. Antiretroviral Therapy of HIV Infection in Infants and Children in Resource-Limited Settings: Towards Universal Access: Recommendations for a Public Health Approach. Geneva: WHO; 2006. [PubMed] [Google Scholar]
- 2.UNAIDS. Fact Sheet Geneva, Switzerland: World Health Organization; c2017. [[Last accessed on 2018 Apr 27]]. Available from: http://wwwunaidsorg/sites/default/files/media_asset/UNAIDS FactSheet_enpdf . [Google Scholar]
- 3.Ministry of Health and Family Welfare National AIDS Control Organization. Assessment of ART Centres of India National Report: Government of India New Delhi. [[Last accessed on 2018 Apr 27]]. Available from: http://nacogovin/sites/default/files/ART%20Assessment%20National%20Report-Final%2028092015pdf .
- 4.Ballif M, Ledergerber B, Battegay M, Cavassini M, Bernasconi E, Schmid P, et al. Impact of previous virological treatment failures and adherence on the outcome of antiretroviral therapy in 2007. PLoS One. 2009;4:e8275. doi: 10.1371/journal.pone.0008275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eticha T, Berhane L. Caregiver-reported adherence to antiretroviral therapy among HIV infected children in Mekelle, Ethiopia. BMC Pediatr. 2014;14:114. doi: 10.1186/1471-2431-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chadwick EG, Rodman JH, Britto P, Powell C, Palumbo P, Luzuriaga K, et al. Ritonavir-based highly active antiretroviral therapy in human immunodeficiency virus type 1-infected infants younger than 24 months of age. Pediatr Infect Dis J. 2005;24:793–800. doi: 10.1097/01.inf.0000177281.93658.df. [DOI] [PubMed] [Google Scholar]
- 7.Barlow-Mosha LN, Bagenda DS, Mudiope PK, Mubiru MC, Butler LM, Fowler MG, et al. The long-term effectiveness of generic adult fixed-dose combination antiretroviral therapy for HIV-infected Ugandan children. Afr Health Sci. 2012;12:249–58. doi: 10.4314/ahs.v12i3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel A, Trivedi SS, Chudasama RK, Patel PK. Effect of antiretroviral therapy on clinical and immunologic disease progression in HIV positive children: One-year follow-up study. J Family Community Med. 2012;19:178–83. doi: 10.4103/2230-8229.102318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kabue MM, Buck WC, Wanless SR, Cox CM, McCollum ED, Caviness AC, et al. Mortality and clinical outcomes in HIV-infected children on antiretroviral therapy in Malawi, Lesotho, and Swaziland. Pediatrics. 2012;130:e591–9. doi: 10.1542/peds.2011-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nyesigire Ruhinda E, Bajunirwe F, Kiwanuka J. Anaemia in HIV-infected children: Severity, types and effect on response to HAART. BMC Pediatr. 2012;12:170. doi: 10.1186/1471-2431-12-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biressaw S, Abegaz WE, Abebe M, Taye WA, Belay M. Adherence to antiretroviral therapy and associated factors among HIV infected children in ethiopia: Unannounced home-based pill count versus caregivers' report. BMC Pediatr. 2013;13:132. doi: 10.1186/1471-2431-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolton-Moore C, Mubiana-Mbewe M, Cantrell RA, Chintu N, Stringer EM, Chi BH, et al. Clinical outcomes and CD4 cell response in children receiving antiretroviral therapy at primary health care facilities in Zambia. JAMA. 2007;298:1888–99. doi: 10.1001/jama.298.16.1888. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Guidelines on HIV and Infant Feeding 2010. Geneva: World Health Organization; 2011. [[Last accessed on 2018 Apr 27]]. p. 58. Available from: http://whqlibdocwhoint/publications/2010/9789241599535_engpdf . [Google Scholar]
- 14.Brady MT, Oleske JM, Williams PL, Elgie C, Mofenson LM, Dankner WM, et al. Declines in mortality rates and changes in causes of death in HIV-1-infected children during the HAART era. J Acquir Immune Defic Syndr. 2010;53:86–94. doi: 10.1097/QAI.0b013e3181b9869f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sutcliffe CG, van Dijk JH, Bolton C, Persaud D, Moss WJ. Effectiveness of antiretroviral therapy among HIV-infected children in sub-Saharan Africa. Lancet Infect Dis. 2008;8:477–89. doi: 10.1016/S1473-3099(08)70180-4. [DOI] [PubMed] [Google Scholar]
- 16.Harrigan PR, Hogg RS, Dong WW, Yip B, Wynhoven B, Woodward J, et al. Predictors of HIV drug-resistance mutations in a large antiretroviral-naive cohort initiating triple antiretroviral therapy. J Infect Dis. 2005;191:339–47. doi: 10.1086/427192. [DOI] [PubMed] [Google Scholar]
- 17.Lindsey JC, Malee KM, Brouwers P, Hughes MD PACTG 219C Study Team. Neurodevelopmental functioning in HIV-infected infants and young children before and after the introduction of protease inhibitor-based highly active antiretroviral therapy. Pediatrics. 2007;119:e681–93. doi: 10.1542/peds.2006-1145. [DOI] [PubMed] [Google Scholar]
- 18.Panel on Antiretroviral Therapy and Medical Management of HIV-Infected Children: Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. [[Last accessed on 2018 Apr 27]]. Available from: http://aidsinfonihgov/contentfiles/lvguidelines/pediatricguidelinespdf .
- 19.Haberer J, Mellins C. Pediatric adherence to HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2009;6:194–200. doi: 10.1007/s11904-009-0026-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 2):S171–6. doi: 10.1086/313849. [DOI] [PubMed] [Google Scholar]
- 21.Zegeye S. Antiretroviral therapy adherence among pediatric patients attending ART clinics in harar and dire dawa ethiopia. Harar Bull Health Sci. 2012;96:152–70. [Google Scholar]
- 22.Arun S, Singh AK, Lodha R, Kabra SK. Disclosure of the HIV infection status in children. Indian J Pediatr. 2009;76:805–8. doi: 10.1007/s12098-009-0177-z. [DOI] [PubMed] [Google Scholar]
- 23.Rajasekaran S, Jeyaseelan L, Raja K, Ravichandran N. Demographic and clinical profile of HIV infected children accessing care at Tambaram, Chennai, India. Indian J Med Res. 2009;129:42–9. [PubMed] [Google Scholar]
- 24.Okomo U, Togun T, Oko F, Peterson K, Townend J, Peterson I, et al. Treatment outcomes among HIV-1 and HIV-2 infected children initiating antiretroviral therapy in a concentrated low prevalence setting in West Africa. BMC Pediatr. 2012;12:95. doi: 10.1186/1471-2431-12-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pol RR, Shepur TA, Ratageri VH. Clinico-laboratory profile of pediatric HIV in Karnataka. Indian J Pediatr. 2007;74:1071–5. doi: 10.1007/s12098-007-0199-3. [DOI] [PubMed] [Google Scholar]
- 26.Biadgilign S, Deribew A, Amberbir A, Deribe K. Adherence to highly active antiretroviral therapy and its correlates among HIV infected pediatric patients in Ethiopia. BMC Pediatr. 2008;8:53. doi: 10.1186/1471-2431-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davies MA, Boulle A, Fakir T, Nuttall J, Eley B. Adherence to antiretroviral therapy in young children in Cape Town, South Africa, measured by medication return and caregiver self-report: A prospective cohort study. BMC Pediatr. 2008;8:34. doi: 10.1186/1471-2431-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ugwu R, Eneh A. Factors influencing adherence to paediatric antiretroviral therapy in Portharcourt, South- South Nigeria. Pan Afr Med J. 2013;16:30. doi: 10.11604/pamj.2013.16.30.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhattacharya M, Dubey AP. Adherence to antiretroviral therapy and its correlates among HIV-infected children at an HIV clinic in New Delhi. Ann Trop Paediatr. 2011;31:331–7. doi: 10.1179/1465328111Y.0000000031. [DOI] [PubMed] [Google Scholar]
- 30.Bhattacharya M, Dubey AP, Sharma M. Patterns of diagnosis disclosure and its correlates in HIV-Infected North Indian children. J Trop Pediatr. 2011;57:405–11. doi: 10.1093/tropej/fmq115. [DOI] [PubMed] [Google Scholar]
- 31.Puthanakit T, Oberdorfer A, Akarathum N, Kanjanavanit S, Wannarit P, Sirisanthana T, et al. Efficacy of highly active antiretroviral therapy in HIV-infected children participating in Thailand's National Access to Antiretroviral Program. Clin Infect Dis. 2005;41:100–7. doi: 10.1086/430714. [DOI] [PubMed] [Google Scholar]
- 32.Haberer JE, Kiwanuka J, Nansera D, Ragland K, Mellins C, Bangsberg DR. Multiple measures reveal antiretroviral adherence successes and challenges in HIV-infected Ugandan children. PLoS One. 2012;7:e36737. doi: 10.1371/journal.pone.0036737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haberer JE, Cook A, Walker AS, Ngambi M, Ferrier A, Mulenga V, et al. Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects. PLoS One. 2011;6:e18505. doi: 10.1371/journal.pone.0018505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nabukeera-Barungi N, Kalyesubula I, Kekitiinwa A, Byakika-Tusiime J, Musoke P. Adherence to antiretroviral therapy in children attending Mulago Hospital, Kampala. Ann Trop Paediatr. 2007;27:123–31. doi: 10.1179/146532807X192499. [DOI] [PubMed] [Google Scholar]
- 35.Buchanan AL, Montepiedra G, Sirois PA, Kammerer B, Garvie PA, Storm DS, et al. Barriers to medication adherence in HIV-infected children and youth based on self- and caregiver report. Pediatrics. 2012;129:e1244–51. doi: 10.1542/peds.2011-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White YR, Pierre RB, Steel-Duncan J, Palmer P, Evans-Gilbert T, Moore J, et al. Adherence to antiretroviral drug therapy in children with HIV/AIDS in Jamaica. West Indian Med J. 2008;57:231–7. [PubMed] [Google Scholar]
- 37.Puthanakit T, Aurpibul L, Oberdorfer P, Akarathum N, Kanjananit S, Wannarit P, et al. Hospitalization and mortality among HIV-infected children after receiving highly active antiretroviral therapy. Clin Infect Dis. 2007;44:599–604. doi: 10.1086/510489. [DOI] [PMC free article] [PubMed] [Google Scholar]


