Abstract
Purpose of Review
This review examines the current epidemiological evidence for the relationship between levels of food insecurity and cardiovascular disease (CVD) outcomes among US adults > 17 years.
Recent Findings
Review of recent literature revealed that reduced food security was associated with decreased likelihood of good self-reported cardiovascular health and higher odds of reporting CVD-related outcomes such as coronary heart disease, angina, heart attack, peripheral arterial disease, and hypertension.
Summary
Existing evidence suggests a compelling association between each level of reduced food security and CVD risk with a particularly strong association between very low food security and CVD risk. Policies and public health-based strategies are needed to identify the most vulnerable subgroups, strengthen and enhance access to food assistance programs, and promote awareness and access to healthful foods and beverages to improve food security, nutrition, and cardiovascular health.
Keywords: Food security, Cardiovascular disease, Heart disease, Health outcomes, Nutrition, Risk factor
Introduction
Cardiovascular disease (CVD) is the number one leading cause of death globally [1•]. In the USA, CVD death was primarily attributable to coronary heart disease (CHD, 42.6%), followed by stroke (17.0%), hypertension (10.5%), heart failure (9.4%), and diseases of arteries (2.9%); other minor CVD causes combined accounted for 17.6% in 2017 [2]. CVD poses a substantial health and economic burden in the USA. About 10.6% of US adults were living with CHD, heart failure, or stroke between 2013 and 2016 [3]. The estimated annual direct and indirect cost of CVD was $351.2 billion for 2014–2015, and the total cost is expected to reach $1.1 trillion in 2035 [1•]. Although estimates suggest that approximately 80% of CVD can be prevented by controlling risk factors and adopting a healthy lifestyle, currently in the USA, the prevalence of heart healthy behaviors is low, and substantial barriers to implementation exist including low socioeconomic status and food insecurity [1•, 4, 5].
Food insecurity is a major US public health concern, with 10.5% of households having limited access at all times to enough food for an active and healthy life in 2019 [6]. Due to the coronavirus disease 2019 (COVID-19) pandemic, food insecurity is estimated to have tripled to 38.3% and increased well beyond levels seen during the Great Recession, based on a representative national sample of US adults collected in March 2020 [7]. The prevalence of food insecurity was even higher (44%) for US adults with income below 250% of the federal poverty level [8]. Growing evidence reveals food insecurity to be a risk factor for poor health across the life course. Children and adults living in food insecure households may have increased risk for negative health outcomes such as poor development, overall poor health, adverse mental health conditions, chronic diseases, functional limits, and potentially shorter life expectancy compared with those living in food secure households [9–13]. To cope with food insecurity, households may rely on a low variety of nutritionally inadequate foods and have disordered eating patterns that contribute to poor overall dietary quality, and do not meet the recommendation for key food groups nor fulfill the average requirement for nutrients [5, 11, 14–19]. Indeed, the classification of food security defines ranges; in the most severe level, very low food security (VLFS), amount of food is reduced, and disrupted eating patterns are present [20]. Low food security (LFS) is comparatively less severe but defines a range where there is reduced quality or variety but not amount of food [20]. In marginal food security (MFS), anxiety of having enough food exists, but no changes in diet are present, and finally, in high food security (HFS), there are no indications of food access limits [20]. Compromised dietary intake present with LFS and VLFS combined with potential cycles of bingeing and fasting alongside the fluctuating nature of food insecurity may lead to adverse metabolic effects such as insulin resistance and poor weight management that heighten CVD risk [1•, 11, 21, 22]. Additionally, lower food security may affect CVD risk by activating the stress response and elevating depressive and anxiety symptoms that could potentially trigger unhealthful coping behaviors or limit one’s ability to manage disease [21, 22].
Dietary intake and other lifestyle factors associated with and independent from food insecurity are important to CVD risk. Research using comparable risk assessment methods and nationally representative data have shown that about 45% of cardiometabolic deaths were attributable to poor dietary habits [23]. The leading dietary risk factors for cardiometabolic deaths included low consumption of vegetables and fruits (15%), high sodium intake (10%), low consumption of nuts/seeds (9%), high consumption of processed meats (8%), low intake of seafood omega-3 fats (8%), and high consumption of sugar-sweetened beverages (7%) [23], many of which have been associated with food insecurity [5, 15, 24, 25]. Besides eating a healthy diet, the American Heart Association’s Life’s Simple 7 highlights three other health behaviors (non-smoking/non-smokeless tobacco use, physical activity, healthy body weight) and three CVD risk factors (blood glucose, total cholesterol, and blood pressure) important for heart health [1•]. Poor adherence to these modifiable risk factors has been associated with reduced food security, indicating the great potential of food insecurity to be associated with cardiovascular health [9, 11, 24, 26]. Therefore, a strong link between food insecurity and CVD risk is plausible. Several studies have evaluated this relationship, but there is a lack of synthesis of recent literature to determine how the severity or the range of food insecurity may be associated with CVD risk. Summarizing the comprehensive evidence for this relationship may inform specific intervention strategies targeting food insecure groups by food security level to reduce CVD risk. This review examines the current epidemiological evidence for the relationship between the range of food insecurity and CVD outcomes among US adults > 17 years of age and concentrates on papers that reflect the most recent work. An explanation of the proposed mechanisms and policy implications is also included in discussion of the findings.
Methods
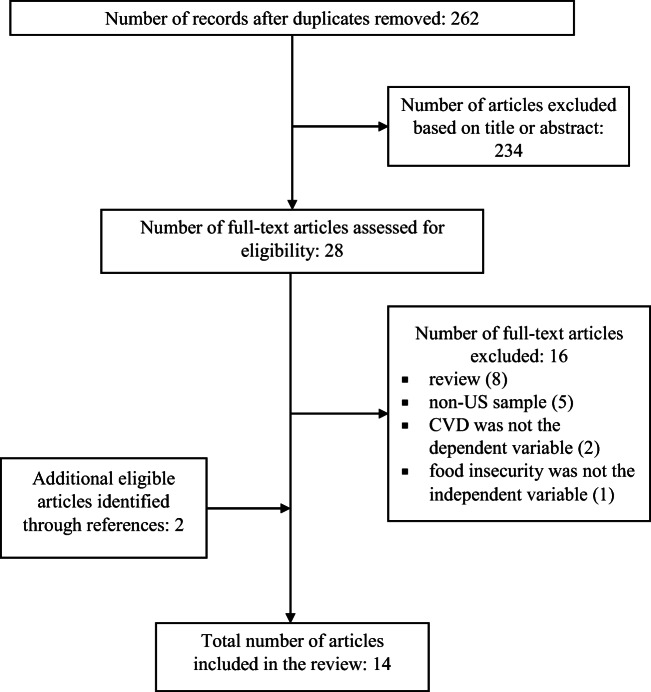
A PubMed search of the terms “food security” and “health outcomes” or “chronic disease” or “cardiovascular disease” or “heart disease” or “coronary heart disease” or “angina pectoris” or “myocardial infarction” or “heart attack” or “peripheral arterial disease” or “stroke” or “cerebrovascular disease” or “heart failure” or “arrhythmia” or “rheumatic heart disease” or “congenital heart disease” or “thrombosis” or “pulmonary embolism” yielded 262 peer-reviewed studies published between 2010 and 2020. Searches were limited to human studies published in the English language. First, the title and abstract were assessed for general relevance. Second, the full text of remaining articles was examined for accordance with eligibility criteria. Relevant articles were included in this review if they (1) used a sample drawn from the US population, (2) contained self-reported or measured CVD-related outcomes, and (3) classified food insecurity using the US Department of Agriculture (USDA) Household Food Security Survey Module or variants on this measure.
Results
After an examination of the title and abstract, 234 articles were excluded from further consideration (Fig. 1). Full texts of the remaining 28 articles were assessed in accordance with the eligibility criteria, and 12 articles were retained for inclusion. Two additional eligible articles were identified through review of article references. A total of 14 studies [27–29, 30••, 31–40] met all criteria and were included in the final review (Table 1).
Fig. 1.
Flowchart of the literature search and article selection process
Table 1.
Summary of research on food insecurity and cardiovascular disease among US adults during 2010–2020*
| Reference | Population | Data source | Design | Outcome measures | Key findings |
|---|---|---|---|---|---|
| Ford et al. [29] | 10455 US adults aged ≥ 20 years | NHANES (2003–2008) | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); 10-year CVD risk (calculated based on algorithm derived from Framingham data); diabetes, hypertension, dyslipidemia, C-reactive protein, urinary albumin-creatinine ratio (measured by biomarkers) |
• No significant association between food security status and 10-year CVD risk > 20% (p = 0.14). However, stratified analysis showed increased predicted 10-year CVD risk > 20% among VLFS participants aged 30–59 years compared with FS participants (adjusted prevalence ratio = 2.38, 95% CI 1.31–4.31, p = 0.03), but not among older adults aged 60–74 years (p = 0.43) • Food security status was significantly associated with several risk factors, including hemoglobin A1c ≥ 6.5% (p = 0.01), hypertension (p = 0.004), low high-density lipoprotein cholesterol (p = 0.002), BMI ≥ 30 kg/m2 (p = 0.03), current smoking (p < 0.001), cotinine > 10 ng/ml (p < 0.001), C-reactive protein >3 mg/l (p = 0.002), and urinary albumin-creatinine ratio ≥ 30 mg/g (p = 0.01) • Prevalence of food insecurity: HFS (83.9%), MFS (6.7%), LFS (5.8 %), VLFS (3.6%) |
| Gregory et al. [30••] | 41,854 working-age US adults (age 19-64 years) living ≤200% FPL | National Health Interview Survey (2011–2015) | Cross-sectional, random sample | Food security (10-item questionnaire); hypertension, CHD, hepatitis, stroke, cancer, asthma, diabetes, arthritis, chronic obstructive pulmonary disease, and kidney disease (self-reported) |
• As food insecurity worsens, the likelihood of having hypertension (MFS, β = 0.23, p < 0.01; LFS, β = 0.35, p < 0.01; VLFS, β = 0.64, p < 0.01), CHD (MFS, β = 0.35, p < 0.01; LFS, β = 0.43, p < 0.01; VLFS, β = 0.76, p < 0.01), stroke (LFS, β = 0.52, p < 0.01; VLFS, β = 0.78, p < 0.01), and diabetes (MFS, β = 0.25, p < 0.01; LFS, β = 0.36, p < 0.01; VLFS, β = 0.58, p < 0.01) increased relative to those in HFS households • Tests for difference between MFS and LFS was significant for stroke, number of chronic conditions, and self-assessed health (p < 0.05, respectively). Tests for difference between LFS and VLFS was significant for hypertension, CHD, stroke, diabetes, number of chronic conditions, and self-assessed health (p < 0.05, respectively). Tests for difference between MFS and VLFS were significant for hypertension, CHD, stroke, diabetes, number of chronic conditions, and self-assessed health (p < 0.01, respectively) • Covariates significantly associated with CHD and/or stroke included sex, age, race/ethnicity, education, employment, having insurance, household income-to-poverty ratio • Prevalence of food insecurity was not reported |
| Shiue et al. [35] | 4979 US adults aged ≥ 20 years | NHANES (2005–2006) | Cross-sectional, random sample | Food security (USDA 18-item HFSSM); heart failure, and other health outcomes (self-reported) |
• Household food security was not associated with heart failure, coronary heart disease, angina, heart attack, or stroke (p > 0.05) • Prevalence of food insecurity: HFS (77.9%), MFS (9.5%), LFS and VLFS combined (12.7 %) |
| Vercammen et al. [39] | 13,518 US adults aged 20–64 years | NHANES (2007–2014) | Cross-sectional, random sample | Food security (USDA 18-item HFSSM); calculated 10-year CVD risk (pooled cohort equations); BMI, waist circumference, blood pressure (physical exam); cholesterol, blood glucose (fasting metabolic panel) |
• VLFS adults had significantly greater odds of excess predicted CVD risk (≥ 20%) compared with food secure adults (OR = 2.36, 95% CI 1.25, 4.46) • Adults reduced food security had higher odds of current smoking (MFS, OR = 1.43, 95% CI 1.17, 1.75; LFS, OR = 1.47, 95% CI 1.22, 1.77; VLFS, OR = 1.95, 95% CI 1.60, 2.37) compared with FS adults • Prevalence of food insecurity: HFS (75.4%), MFS (9.9%), LFS (8.2%), VLFS (6.5%) |
| Palakshappa et al. [32] | 9203 US adults aged ≥ 20 years living with obesity | NHANES (2007–2014) | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); CVD outcomes (self-reported); other disease outcomes (self-reported or measured) |
• Food insecurity (β = 0.09, 95% CI 0.02–0.15, p = 0.01) and VLFS (β = 0.17, 95% CI 0.07–0.28, p = 0.003) were associated with an increased number of obesity-related comorbidities. In secondary analyses, food insecurity was associated with increased odds of coronary artery disease (OR = 1.5, 95% CI 1.1–2.0), and the increased odds was primarily seen among VLFS adults (OR = 2.0, 95% CI 1.3–3.0) • Prevalence of food insecurity: LFS (9%), VLFS (6.6%) |
| Smith et al. [36] | 15499 working-age low-income immigrant adults (aged 18–64 years) living ≤ 300% FPL | NHANES (2011–2015) | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); CHD, angina pectoris, heart attack, obesity (self-reported), self-rated poor health (self-reported) |
• Both food insecurity and acculturation are strongly associated with CHD and related health outcomes. Food insecurity is associated with 57% higher odds of being diagnosed with CHD (p < 0.01), 81% higher odds of angina pectoris (p < 0.01), and more than doubled odds of heart attack (p < 0.01) • For all three heart outcomes, the relationship with food insecurity is stronger for women and not significant for men (p < 0.01) • LFS and VLFS are associated with CHD (β = 1.8, p < 0.01; β = 1.5, p < 0.1), angina pectoris (β = 2.0, p < 0.01; β = 2.5, p < 0.01), heart attack (β = 2.2, p < 0.01; β = 1.8, p < 0.05), self-reported poor health (β = 2.6, p < 0.01; β = 4.8, p < 0.01), and obesity (β = 1.3, p < 0.01; β = 1.3, p < 0.01). Food insecurity is associated more strongly with CHD and related outcomes for immigrants in the USA for < 5 years or those ≥ 15 years, than those for 5–14 years (p = 0.014) • Prevalence of food insecurity: 20.6% |
| Venci et al. [38] | 30,010 US adults aged ≥ 18 years | National Health Interview Survey 2011 | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); functional limitation, coronary heart disease and other chronic diseases (self-reported) |
• VLFS adults had higher odds for coronary heart disease (OR = 1.75, 95% CI 1.37–2.24), heart attack (OR = 1.40, 95% CI 1.08–1.81), hypertension (OR = 1.42, 95% CI 1.22–1.65), inflammatory disease or joint/muscular pain (OR = 1.74; 95% CI 1.49–2.04), and diabetes (OR = 1.23, 95% CI 1.02–1.48) compared with FS adults • LFS adults had higher odds for functional limitation (OR = 1.87, 95% CI 1.63–2.14), hypertension (OR = 1.18, 95% CI 1.04–1.35), inflammatory diseases or joint/muscular pain (OR = 1.42, 95% CI 1.21–1.68), and diabetes (OR = 1.26, 95% CI 1.06–1.51) when compared with FS adults • Prevalence of food insecurity: LFS (7.4%), VLFS (5.8%) |
| Banerjee et al. [27] | 9245 US adults aged ≥ 20 years, living below the 130% FPL | Participants were followed for mortality through 2011 using probabilistic matching between NHANES (1999–2010) and National Death Index death certificate records | Longitudinal, random sample | Food security (USDA 10-item HFSSM); cardiorenal syndrome (CVD was self-reported; chronic kidney disease was confirmed by a glomerular filtration rate < 60 ml/min per 1.73 m2 or a urine albumin-to-creatinine ratio < 30) |
• Food insecurity was associated with 28% higher mortality rate than food secure individuals • The adjusted HR was 2.81 (95% CI 1.57–5.05, p < 0.001) among food insecure individuals with cardiorenal syndrome, while the adjusted HR was 2.48 (95% CI 1.73–3.55, p < 0.001) among food secure individuals with cardiorenal syndrome, after controlling for obesity and diabetes status, gender, age, education level, and ethnicity • Prevalence of food insecurity: 37.8% |
| Fanelli Kuczmarski et al. [28] | 2066 US adults aged 30–64 years from urban Baltimore neighborhoods |
Healthy Aging in Neighborhoods of Diversity across the Life Span Study (wave 4) |
Cross-sectional, convenience sample | Food security (1-item question); 10-year atherosclerotic CVD risk (calculated using pooled cohort equations); mean adequacy ratio, DASH score, count, evenness, dissimilarity (calculated using the average of two 24-h recall intakes) |
• Being food secure was associated with higher 10-year atherosclerotic CVD risk (p < 0.001) • A micronutrient-rich diet assessed by the mean adequacy ratio was associated with lower atherosclerotic CVD risk (p < 0.001). Greater dissimilarity among foods (p < 0.04) and lower count (p < 0.03), but not DASH score, were associated with lower atherosclerotic CVD risk • Prevalence of food insecurity: 25.9% |
| Liu et al. [31] | 270 US adults aged 21–80 years recruited from food pantries in central Indiana | Food Finders Food Bank, West Lafayette, Indiana | Cross-sectional, convenience sample | Food security (USDA 18-item HFSSM); CVD and other disease outcomes (self-reported) |
• Household food insecurity was associated with higher odds of reporting heart disease (age- and sex-adjusted OR = 2.65; 95% CI 1.05–6.69) compared with household food security • Prevalence of food insecurity: 79% |
| Redmond et al. [33] | 2027 seniors (aged ≥ 60 years) with peripheral arterial disease | NHANES (1999–2004) | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); peripheral arterial disease (ankle brachial index score ≤ 90); other chronic diseases (self-reported) |
• Food insecure seniors had increased odds of having peripheral arterial disease (OR = 1.50, 95% CI 1.11–2.03) • Prevalence of food insecurity: 22.1% |
| Saiz et al. [34] | 2935 adults aged 21–74 years | Survey of the Health of Wisconsin (2008––2014 wave) | Cross-sectional, representative sample of Wisconsin residents | Food security (1-item question); cardiovascular health (self-reported, American Heart Association Life’s Simple 7 criteria) |
• Food insecurity was associated with a decreased likelihood of good cardiovascular health (OR = 0.53, 95% CI 0.31 to 0.92, p = 0.02) • Prevalence of food insecurity: 12% |
| Vaccaro et al. [37] | 3871 US adults aged ≥ 55 years | NHANES (2011–2014) | Cross-sectional, random sample | Food security (USDA 10-item HFSSM); CVD, cancer, diabetes, lung diseases (self-reported) |
• No significant association was observed between food insecurity and CVD (p = 0.48). But adults living in poverty had greater odds of CVD (OR = 1.56, 95% CI 1.10–2.20) compared with those living above the poverty level • Prevalence of food insecurity: 13% |
| Wang et al. [40] | US adults aged 20–64 years from 3142 counties across 50 states and Washington D.C. (2011–2017) | National Center for Health Statistics; Map the Meal Gap project | Ecological design (county-level longitudinal analysis) | Annual county-level food security rate (estimated by the Map the Meal Gap project using state-level food security data measured by the 18-item USDA HFSSM in the current population survey); annual county-level age-adjusted cardiovascular mortality rate (calculated using data from the National Center for Health Statistics) |
• An estimated 1% point increase in food insecurity was associated with a 0.83% (95% CI 0.43–1.25%, p < 0.001) increase in age-adjusted cardiovascular mortality. In stratified analysis by baseline food insecurity quartiles, this association was only significant in the third (0.92%, 95% CI 0.03–1.82%, p = 0.04) and fourth quartiles (0.76%, 95% CI 0.23–1.31%, p = 0.01) • Prevalence of food insecurity: not reported |
*NHANES National Health and Nutrition Examination Survey, USDA United States Department of Agriculture, HFSSM Household Food Security Survey Module, CVD cardiovascular disease, CHD coronary heart disease, BMI body mass index, HFS high food security, MFS marginal food security, LFS low food security, VLFS very low food security, FPL federal poverty level, DASH Dietary Approaches to Stop Hypertension
Most of the research examining food insecurity and its association with CVD concentrated on working-age adults or adults in general (Table 1), except for three studies that featured older adults [29, 33, 37]. Eleven studies used a nationally representative sample [27, 29, 30••, 32, 33, 35–40], while three studies used convenience samples [28, 31] or state-specific representative samples [34]. Twelve studies were cross-sectional [28, 29, 30••, 31–39], and one study was ecological [40], whereas one used longitudinal analysis [27]. Four studies focused on evaluating the relationship between food insecurity and CVD outcomes among low-income populations that fell below a certain percentage of the federal poverty level [27, 30••, 31, 36]. High prevalence of heart disease (18%) and stroke (12%) above the national average [41] were reported specifically in a food pantry user population (aged 21–80 years) where the majority lived below 100% federal poverty level [31]. Only one study used clinical measures to ascertain peripheral arterial disease [33], while the majority used self-reported data for CVD-related outcomes [27, 30••, 31, 32, 34–38]. Additionally, three studies calculated the 10-year risk for atherosclerotic CVD events [28, 29, 39] using the pooled cohort equations introduced by the American College of Cardiology/American Heart Association [42], based on risk factors such as age, total cholesterol, blood pressure, high-density lipoprotein cholesterol, type 1 or 2 diabetes status, and smoking status. Food security status was quantified by the 18-item or 10-item USDA’s Household Food Security Survey Module in 12 studies [27, 29, 30••, 31–33, 35–40], while two studies used a 1-item or 2-item screener to assess food security [28, 34]. The prevalence of food insecurity ranged from 9.4% [29] to 79% [31].
Four studies in this review classified food security into HFS, MFS, LFS, and VLFS [29, 30••, 35, 39], while three studies combined HFS and MFS as being food secure (FS) that was then examined along with LFS and VLFS [32, 36, 38]. These studies suggested a compelling association between each level of reduced food security and CVD risk, though evidence supporting a dose-dependent relationship was mixed. According to the USDA report conducted using data from the National Health Interview Survey of over 40,000 working-age adults living ≤ 200% federal poverty level, adults in households with MFS, LFS, and VLFS all had significantly increased risk of CHD, hypertension, diabetes, and four other chronic illnesses (asthma, arthritis, chronic obstructive pulmonary disease, kidney disease), compared to those in HFS households [30••]. As food insecurity worsened, the risk of chronic illness was progressively higher as suggested by the statistically significant differences between MFS, LFS, and VLFS groups [30••]. Findings from another study did not support a consistent dose-dependent relationship between food insecurity and CVD-related outcomes. Specifically, MFS, LFS, and VLFS were associated with higher odds of CHD (β = 1.5 ± 0.3, p < 0.1; β = 1.8 ± 0.3, p < 0.01; β = 1.5 ± 0.3, p < 0.1), angina pectoris (β = 2.2 ± 0.5, p < 0.01; β = 2.0 ± 0.4, p < 0.01; β = 2.5 ± 0.6, p < 0.01), and heart attack (β = 0.7 ± 0.2, p > 0.1; β = 2.2 ± 0.6, p < 0.01; β = 1.8 ± 0.5, p < 0.05) compared with HFS among low-income adults living ≤ 300% federal poverty level (n = 15,499) from the National Health and Nutrition Examination Survey (NHANES) [36]. Similar findings were reported in another study using NHANES data where only VLFS adults had significantly higher odds for CHD and heart attack and both LFS and VLFS adults had significantly higher odds for hypertension, diabetes, and inflammatory disease or joint/muscular pain, compared with FS adults [38]. Another study pointed out that the significantly greater odds of CHD (OR = 1.5, 95% CI 1.1–2.0) observed among food insecure adults was primarily seen among individuals living in VLFS households (OR = 2.0, 95% CI 1.3–3.0), compared to their FS counterparts based on NHANES data (n = 9,203) [32]. Using data from NHANES of over 13,000 adults aged 20–64 years, one study showed 2.4 times greater odds of excess predicted 10-year CVD risk (≥ 20%) among VLFS adults compared with FS adults [39]. Another study showed significantly increased predicted 10-year CVD risk (> 20 %) among VLFS adults aged 30–59 years compared with FS adults (adjusted prevalence ratio = 2.38, p = 0.03), but not among older adults aged 60–74 years [29]. Of these seven studies, only one reported no significant association between food insecurity and heart failure, CHD, angina, heart attack, or stroke [35].
The other seven studies used binary comparisons of adults living in food insecure households with those living in FS households [27, 28, 31, 33, 34, 37, 40]. Overall, food insecurity was associated with significantly decreased likelihood of good self-reported cardiovascular health (OR = 0.53, 95% CI 0.31–0.92) [34], higher odds of reporting CVD-related outcomes such as peripheral arterial disease (OR = 1.50, 95% CI 1.11–2.03) [33] and heart disease (OR = 2.65, 95% CI 1.05–6.69) [31], and higher mortality rate among individuals with cardiorenal syndrome (HR = 2.81, 95% CI 1.57–5.05) [27]. The ecological study using county-level longitudinal analysis of data from 3142 US counties across 50 states and Washington DC (2011–2017) showed that a 1% point increase in food insecurity was associated with a 0.83% (95% CI 0.43–1.25%, p < 0.001) increase in age-adjusted cardiovascular mortality [40]. Surprisingly, one study using data from a convenience sample of 2066 US adults aged 30–64 years showed that living in FS households was associated with higher 10-year CVD risk (p < 0.001) relative to food insecure households, though the study used a single item question to assess food security status and thus may be subjected to misclassification bias [28]. Another study using NHANES data reported no association between food insecurity and self-reported CVD outcome among older adults aged ≥ 55 years; however, the study reported that adults living in poverty had greater odds of CVD (OR = 1.56, 95% CI 1.10–2.20) compared with those living above the poverty level [37].
Discussion
This review of the recent literature suggests a compelling association between reduced food security and CVD risk. The association between VLFS with CVD-related outcomes was particularly strong; however, each level of food insecurity and even MFS presented a unique risk for CVD. The full range of food insecurity classification to four levels captures important information about economic hardship translated to poor health outcomes, showing statistically significant differences between each level across the range of food insecurity in terms of likelihood of various chronic health outcomes [30••]. For most chronic health outcomes examined in the USDA report, MFS, LFS, and VLFS were strongly associated with increased risk and increased number of chronic conditions, relative to HFS [30••]. Specifically, there was a statistically significant increase in the prevalence of hypertension for adults as food security worsens (HFS, 20%; MFS, 24%; LFS, 28%; VLFS, 36%) [30••]. Another study supported the notion that MFS was associated with higher cumulative biological risk scores and MFS adults were more likely to have higher mean glycohemoglobin, C-reactive protein, and systolic blood pressure, relative to HFS [43]. Yet the relationship of MFS to CVD may not be observed when food security status is dichotomized [10]. LFS and VLFS were both associated with CVD-related outcomes [27, 29, 30••, 31–34, 36, 38–40]; in particular, VLFS adults had at least two times higher odds of having excess 10-year CVD risk (≥ 20%) and at least 1.4 times higher odds of having CHD, heart attack, and hypertension compared to FS adults [29, 30••, 32, 38, 39]. One study reported that VLFS adults had the highest likelihood of having CHD, hypertension, and stroke across the four levels of food insecurity [30••].
The mechanisms by which reduced food security may cause or heighten CVD risk remain unclear, but previous studies hypothesized several pathways by which reduced food security could lead to the development or worsening of chronic disease and health conditions. In addition to the mechanisms described in the introduction of this paper, previous life experiences of food insecurity may heighten CVD risk, yet these remain uninvestigated hypotheses. For example, the experience of food deprivation as a child may have lifelong influence on eating patterns, attitudes, and preference in adulthood; some adults who experienced food shortages in childhood described long-term disordered eating practice, such as bingeing when food was available or food hoarding [44, 45]. Food insecurity has also been associated with increased depressive symptoms and stress [13]. Stress activates the sympathetic-adrenal-medullary system and the hypothalamic-pituitary-adrenal axis, which trigger the fight-or-light responses and a surge in stress-mediator hormones that act on multiple biological systems [46]. Thus, stress has the potential to affect blood glucose level, serum lipids, and blood pressure, which have implications on CVD outcomes [46]. Chronic stress may lead to increased allostatic load, a concept referring to the excessive wear and tear on multiple physiological systems due to the chronic overuse and imbalance of the stress mediators [47, 48]. Based on the allostatic load framework, one study created a cumulative biological risk score using data from NHANES and found that food insecurity was associated with a 0.14-unit higher cumulative biological risk score (p = 0.003) and 1.2 times higher odds of elevated biological risk (p = 0.003), which indicated a potential role of food insecurity in influencing chronic health outcomes through chronic stress [43]. In addition, stress may further reduce cognitive bandwidth, motivation, and self-efficacy, which may undermine efforts at self-management or trigger unhealthful behaviors such as smoking [13, 14].
Reduced ability to manage complex chronic conditions may increase the risk of developing or worsening CVD among food insecure populations. Some researchers suggested a bidirectional relationship between food insecurity and cardiovascular health [39, 49]. Food insecure individuals were reported to have higher odds of delaying medication, postponing needed medical care, and hospitalization compared with food secure individuals [50, 51]. Cost-related medication underuse is a term used to describe reducing, skipping, or delaying use of medications or using lower-cost medications to compensate for lack of resources [52]. A significant dose-response relationship between cost-related medication underuse and food insecurity was reported among older adults, with increasing likelihood of cost-related medication underuse with increasing severity of food insecurity [52]. Studies have also associated food insecurity with impaired glucose self-monitoring and poor metabolic control among diabetic patients [9, 11, 49]. Conversely, it is also possible that worsening cardiovascular health may increase medical expenses and reduce capacity for maintaining employment, leading to lower income and increasing risk of food insecurity [39, 49]. One study suggested that individuals living with food insecurity incurred an additional $1863 annually in healthcare expenditure, $493 more for inpatient hospitalizations, and $779 more for prescription medications [49]. The estimated annual total healthcare expenditures were higher among food insecure individuals with heart disease ($5144.1, p < 0.0001), hypertension (+$2175.5, p = 0.003), and diabetes (+$4414.6, p = 0.004), compared with FS individuals with these conditions [49]. Another study also showed that food insecurity was associated with higher use of emergency visits, inpatient admissions, and having high healthcare costs [53].
Most studies included in this review were cross-sectional and focused on working-age adults or adults in general, while the senior population received little attention. According to a Feeding America report, food insecure seniors were 19% more likely to have hypertension, 57% more likely to have congestive heart failure, 66% more likely to have experienced a heart attack, 65% more likely to be diabetic, twice as likely to report fair or poor general health, 2.3 times more likely to suffer from depression, and over 30% more likely to report at least one limitation in activities of daily living compared with food secure seniors [26]. A subgroup of concern is food insecure seniors with income below 200% of the federal poverty level. Food insecurity rate was highest among seniors with incomes below the poverty line (30%), compared to those with incomes between 100 and 200% of the federal poverty level (18%) or those with income above 200% of the federal poverty level (4%) [26]. Food insecure seniors with income below 200% of the federal poverty level were more likely to have CHD, congestive heart failure, heart attack, chest pain, hypertension, high cholesterol, diabetes, depression, and other negative health outcomes compared with their food secure counterparts [26]. Additionally, seniors living with limitation in activities of daily living experience difficulty in performing daily functions such as going to the grocery store to purchase food, eating, or bathing [26]. Future research is warranted to assess how levels of food insecurity affect CVD-related outcomes among older adults, especially those living with functional limits and below 200% of the federal poverty level.
Food insecurity and its association with CVD present challenges to policy-makers, program administrators, and healthcare providers in the USA. With the COVID-19 pandemic causing a never-before-seen food insecurity crisis and economic downturn in the USA, existing disparities related to food insecurity are exacerbated and may continue to exert acute and long-lasting health consequences disproportionately felt by low-income populations [54, 55]. The summarized evidence supports the need for strengthening existing successful strategies such as federal nutrition assistance, nutrition education, and implementation of potentially new strategies to improve food security. For example, the Supplemental Nutrition Assistance Program (SNAP) has been established since 1964 and shown to successfully improve household food security [56–58]. Expansion of the SNAP program may contribute to further reduction in food insecurity, which in turn may lead to the potential reduction in CVD burden [59, 60]. Many people who are eligible for SNAP do not participate in this entitlement program as suggested by a national average participation rate of 84% in 2017 [61]. Especially among seniors, over 60% of those eligible do not receive benefits, suggesting room for improvement in reach of the current SNAP program [9]. Nutrition education has also been shown to improve food security [62, 63]. Education through the Supplemental Nutrition Assistance Program-Education (SNAP-Ed) combines nutrition and budgeting education for those who qualify for SNAP; SNAP-Ed improved food security by 25% over a 1-year timeframe in an intervention compared with a control group that was independent of participation in SNAP or other food assistance [62, 63]. Yet SNAP-Ed is even more restricted as a non-entitlement program serving approximately 5% of US adults who used SNAP in 2018 [64, 65]. With food insecurity incurring an additional $77.5 billion in healthcare expenditure annually, the “return on investment” potential of expanding food insecurity reduction programs like SNAP and SNAP-Ed may be significant [49].
Understanding the extent to which food insecure populations achieve dietary recommendations is the foundation for tailoring powerful public health-based strategies to “meet people where they are” to help them make small and positive shifts [66]. Interventions that integrate food insecurity screening into routine care (at clinics or dietitian’s office) may be an important step to identify individuals experiencing food insecurity and subsequently improve chronic health conditions and patient care for vulnerable populations [67–70]. Emergency food pantries have been increasingly used as a dependable food source over the last decade and chronic use may continue to increase with guidelines that further restrict SNAP eligibility [71, 72]. Programs that link patients to emergency food pantries and other community resources to help support unmet need for food assistance may also be helpful [73]. Lastly, supporting access to healthful foods and beverages in food environments such as federal food assistance programs and emergency food assistance network may be particularly relevant for disadvantaged subgroups to improve diet, health, and wellness [74].
Conclusions
This review suggests a compelling association between reduced food security and CVD risk with a particularly strong link between VLFS with CVD risk and evidence that each range of food security presents a unique risk for CVD. Future research using longitudinal individual-level data focusing on CVD outcomes will likely allow researchers to examine how different factors mediate the observed relationships between reduced food security and CVD risk over time, with appropriate adjustment of covariates such as cigarette smoking and physical activity. Policies and public health-based interventions are needed to identify the most vulnerable subgroups experiencing food insecurity, strengthen and enhance access to food assistance programs, and promote awareness and access to healthful foods and beverages to improve nutrition, food security, and cardiovascular health.
Compliance with Ethical Standards
Conflict of Interest
Yibin Liu declares no conflict of interest. Heather A. Eicher-Miller reports grants from the United States Department of Agriculture, National Institute of Food and Agriculture, Hatch Project 1019736; personal fees from Mead Johnson, National Dairy Council, and American Egg Board; and grants from Eli Lilly and Company.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Nutrition
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yibin Liu, Email: yibinliu@buffalo.edu.
Heather A. Eicher-Miller, Email: heicherm@purdue.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Blackwell DL, Villarroel MA. Tables of summary health statistics for US adults: 2017 National Health Interview Survey. Atlanta: Centers for Disease Control and Prevention; 2019. [Google Scholar]
- 3.National Center for Health Statistics . National Health and Nutrition Examination Survey (NHANES) public use data files. Atlanta: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 4.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 6.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the US in 2019. Alexandria: US Department of Agriculture Economic Research Service; 2020. [Google Scholar]
- 7.Fitzpatrick K, Harris C, Drawve G. Assessing US food insecurity in the United States during COVID-19 pandemic. Fayetteville: AR Community and Family Institute, University of Arkansas; 2020. [Google Scholar]
- 8.Wolfson JA, Leung CW. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. 2020;12(6):1648. doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood) 2015;34(11):1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 10.Lee JS, Gundersen C, Cook J, Laraia B, Johnson MA. Food insecurity and health across the lifespan. Adv Nutr. 2012;3(5):744–745. doi: 10.3945/an.112.002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holben DH, Marshall MB. Position of the academy of nutrition and dietetics: food insecurity in the US. J Acad Nutr Diet. 2017;117(12):1991–2002. doi: 10.1016/j.jand.2017.09.027. [DOI] [PubMed] [Google Scholar]
- 12.Ke J, Ford-Jones EL. Food insecurity and hunger: a review of the effects on children's health and behaviour. Paediatr Child Health. 2015;20(2):89–91. doi: 10.1093/pch/20.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pourmotabbed A, Moradi S, Babaei A, et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutr. 2020;23(10):1778–1790. doi: 10.1017/S136898001900435X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the US. Annu Rev Public Health. 2019;40:319–337. doi: 10.1146/annurev-publhealth-040218-044132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Tooze JA, Zhang Y, et al. Breakfast consumption is positively associated with usual nutrient intakes among food pantry clients living in rural communities. J Nutr. 2019;150(3):546–553. doi: 10.1093/jn/nxz258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cowan AE, Jun S, Tooze JA, et al. Total usual micronutrient intakes compared to the dietary reference intakes among US adults by food security status. Nutrients. 2019;12(1):38. doi: 10.3390/nu12010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rivera RL, Zhang Y, Wang Q, et al. Diet quality and associations with food security among women eligible for Indiana Supplemental Nutrition Assistance Program-Education. J Nutr. 2020;150(8):2191–2198. doi: 10.1093/jn/nxaa171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright BN, Tooze JA, Bailey RL, et al. Dietary quality and usual intake of underconsumed nutrients and related food groups differ by food security status for rural, Midwestern food pantry clients. J Acad Nutr Diet. 2020;120(9):1457–1468. doi: 10.1016/j.jand.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weinfield NS, Mills G, Borger C, et al. Hunger in America 2014 national report. Chicago: Feeding America; 2014. [Google Scholar]
- 20.Bickel G, Nord M, Hamilton W. United States Household Food Security Survey Module: three-stage design with screeners. Alexandria: US Department of Agriculture, Economic Research Service; 2006. [Google Scholar]
- 21.Laraia BA. Food insecurity and chronic disease. Adv Nutr. 2013;4(2):203–212. doi: 10.3945/an.112.003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6–9. doi: 10.1056/NEJMp1000072. [DOI] [PubMed] [Google Scholar]
- 23.Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the US. JAMA. 2017;317(9):912–924. doi: 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eicher-Miller HA. A review of the food security, diet and health outcomes of food pantry clients and the potential for their improvement through food pantry interventions in the US. Physiol Behav. 2020;220:112871. doi: 10.1016/j.physbeh.2020.112871. [DOI] [PubMed] [Google Scholar]
- 25.Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–53.e2. doi: 10.1016/j.jand.2014.06.353. [DOI] [PubMed] [Google Scholar]
- 26.Gundersen C, Ziliak J. The health consequences of senior hunger in the US: evidence from the 1999-2014 NHANES. Alexandria: Feeding America and the National Foundation to End Senior Hunger; 2017. [Google Scholar]
- 27.Banerjee S, Radak T. Association between food insecurity, cardiorenal syndrome and all-cause mortality among low-income adults. Nutr Health. 2019;25(4):245–252. doi: 10.1177/0260106019869069. [DOI] [PubMed] [Google Scholar]
- 28.Fanelli Kuczmarski M, Brewer BC, Rawal R, Pohlig RT, Zonderman AB, Evans MK. Aspects of dietary diversity differ in their association with atherosclerotic cardiovascular risk in a racially diverse US adult population. Nutrients. 2019;11(5):1034–1048. doi: 10.3390/nu11051034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ford ES. Food security and cardiovascular disease risk among adults in the US: findings from the National Health and Nutrition Examination Survey, 2003-2008. Prev Chronic Dis. 2013;10:E202. doi: 10.5888/pcd10.130244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.•• Gregory CA, Coleman-Jensen A. Food insecurity, chronic disease, and health among working-age adults. Washington: Economic Research Service, US Department of Agriculture; 2017. https://www.ers.usda.gov/publications/pub-details/?pubid=84466. Accessed 16 Oct 2020. Findings from this report suggested a strong association between lower food security with higher probability of three cardiovascular disease related outcomes and seven other chronic diseases examined among working-age US adults at or below 200% of the federal poverty level.
- 31.Liu Y, Zhang Y, Remley DT, Eicher-Miller HA. Frequency of food pantry use is associated with diet quality among Indiana food pantry clients. J Acad Nutr Diet. 2019;119(10):1703–1712. doi: 10.1016/j.jand.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 32.Palakshappa D, Speiser JL, Rosenthal GE, Vitolins MZ. Food insecurity is associated with an increased prevalence of comorbid medical conditions in obese adults: NHANES 2007-2014. J Gen Intern Med. 2019;34(8):1486–1493. doi: 10.1007/s11606-019-05081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Redmond ML, Dong F, Goetz J, Jacobson LT, Collins TC. Food insecurity and peripheral arterial disease in older adult populations. J Nutr Health Aging. 2016;20(10):989–995. doi: 10.1007/s12603-015-0639-0. [DOI] [PubMed] [Google Scholar]
- 34.Saiz AM, Jr, Aul AM, Malecki KM, et al. Food insecurity and cardiovascular health: findings from a statewide population health survey in Wisconsin. Prev Med. 2016;93:1–6. doi: 10.1016/j.ypmed.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shiue I. People with diabetes, respiratory, liver or mental disorders, higher urinary antimony, bisphenol A, or pesticides had higher food insecurity: USA NHANES, 2005-2006. Environ Sci Pollut Res Int. 2016;23(1):198–205. doi: 10.1007/s11356-015-5677-y. [DOI] [PubMed] [Google Scholar]
- 36.Smith MD, Coleman-Jensen A. Food insecurity, acculturation and diagnosis of CHD and related health outcomes among immigrant adults in the USA. Public Health Nutr. 2020;23(3):416–431. doi: 10.1017/S1368980019001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaccaro JA, Huffman FG. Sex and race/ethnic disparities in food security and chronic diseases in US older adults. Gerontol Geriatr Med. 2017;3:2333721417718344. doi: 10.1177/2333721417718344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venci BJ, Lee SY. Functional limitation and chronic diseases are associated with food insecurity among US adults. Ann Epidemiol. 2018;28(3):182–188. doi: 10.1016/j.annepidem.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 39.Vercammen KA, Moran AJ, McClain AC, Thorndike AN, Fulay AP, Rimm EB. Food security and 10-year cardiovascular disease risk among US adults. Am J Prev Med. 2019;56(5):689–697. doi: 10.1016/j.amepre.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang SY, Eberly LA, Roberto CA, Venkataramani AS, Groeneveld PW, Khatana SAM. Food insecurity and cardiovascular mortality for non-elderly adults in the US from 2011 to 2017: a county-level longitudinal analysis. Circ Cardiovasc Qual Outcomes. 2021;14(1):e007473. [DOI] [PMC free article] [PubMed]
- 41.National Center for Health Statistics . Heart disease. Atlanta: Center for Disease Control and Prevention; 2020. [Google Scholar]
- 42.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 43.Leung CW, Zhou MS. Household food insecurity and the association with cumulative biological risk among lower-income adults: results from the National Health and Nutrition Examination Surveys 2007-2010. Nutrients. 2020;12(5):1517. doi: 10.3390/nu12051517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olson CM, Bove CF, Miller EO. Growing up poor: long-term implications for eating patterns and body weight. Appetite. 2007;49(1):198–207. doi: 10.1016/j.appet.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 45.Eicher-Miller HA, Zhao Y. Evidence for the age-specific relationship of food insecurity and key dietary outcomes among US children and adolescents. Nutr Res Rev. 2018;31(1):98–113. doi: 10.1017/S0954422417000245. [DOI] [PubMed] [Google Scholar]
- 46.O'Connor DB, Thayer JF, Vedhara K. Stress and health: a review of psychobiological processes. Annu Rev Psychol. 2021;72:4.1–4.26. doi: 10.1146/annurev-psych-062520-122331. [DOI] [PubMed] [Google Scholar]
- 47.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 48.McEwen BS. Redefining neuroendocrinology: epigenetics of brain-body communication over the life course. Front Neuroendocrinol. 2018;49:8–30. doi: 10.1016/j.yfrne.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 49.Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food insecurity and health care expenditures in the US, 2011-2013. Health Serv Res. 2018;53(3):1600–1620. doi: 10.1111/1475-6773.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sullivan AF, Clark S, Pallin DJ, Camargo CA., Jr Food security, health, and medication expenditures of emergency department patients. J Emerg Med. 2010;38(4):524–528. doi: 10.1016/j.jemermed.2008.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Afulani P, Herman D, Coleman-Jensen A, Harrison GG. Food insecurity and health outcomes among older adults: the role of cost-related medication underuse. J Nutr Gerontol Geriatr. 2015;34(3):319–342. doi: 10.1080/21551197.2015.1054575. [DOI] [PubMed] [Google Scholar]
- 53.Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399–404. [PMC free article] [PubMed] [Google Scholar]
- 54.Leddy AM, Weiser SD, Palar K, Seligman H. A conceptual model for understanding the rapid COVID-19-related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr. 2020;112:1162–1169. doi: 10.1093/ajcn/nqaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. 2020;110(12):1763–1765. doi: 10.2105/AJPH.2020.305953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Food and Nutrition Service . A short history of SNAP. Alexandria: US Department of Agriculture; 2018. [Google Scholar]
- 57.Gundersen C, Kreider B, Pepper JV. Partial identification methods for evaluating food assistance programs: a case study of the causal impact of SNAP on food insecurity. Am J Agric Econ. 2017;99(4):875–893. doi: 10.1093/ajae/aax026. [DOI] [Google Scholar]
- 58.Swann CAJFP. Household history, SNAP participation, and food insecurity. Food Policy. 2017;73:1–9. doi: 10.1016/j.foodpol.2017.08.006. [DOI] [Google Scholar]
- 59.Carlson S. More adequate SNAP benefits would help millions of participants better afford food. Washington: Center on Budget and Policy Priorities; 2019. [Google Scholar]
- 60.Keith-Jennings B, Llobrera J, Dean S. Links of the Supplemental Nutrition Assistance Program with food insecurity, poverty, and health: evidence and potential. Am J Public Health. 2019;109(12):1636–1640. doi: 10.2105/AJPH.2019.305325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cunnyngham K. Estimates of state Supplemental Nutrition Assistance Program participation rates in 2017. Alexandria: US Department of Agriculture; 2020. [Google Scholar]
- 62.Eicher-Miller HA, Rivera RL, Sun H, Zhang Y, Maulding MK, Abbott AR. Supplemental Nutrition Assistance Program-Education improves food security independent of food assistance and program characteristics. Nutrients. 2020;12(9):2636. doi: 10.3390/nu12092636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rivera RL, Maulding MK, Eicher-Miller HA. Effect of Supplemental Nutrition Assistance Program-Education (SNAP-Ed) on food security and dietary outcomes. Nutr Rev. 2019;77(12):903–921. doi: 10.1093/nutrit/nuz013. [DOI] [PubMed] [Google Scholar]
- 64.National Institute of Food and Agriculture. SNAP-Ed budget allocation, FY 1992-2018. Washington, DC: US Department of Agriculture. https://snaped.fns.usda.gov/sites/default/files/documents/SNAP-Ed_Final_Allocations_for_FY_2018.pdf. Accessed 20 Nov 2020
- 65.Food and Nutrition Service. SNAP data tables. In. Alexandria, VA: US Department of Agriculture. https://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap. Accessed 20 Nov 2020
- 66.Dietary Guidelines Advisory Committee . Scientific report of the 2020 Dietary Guidelines Advisory Committee: advisory report to the secretary of Agriculture and the secretary of Health and Human Services. Washington: US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 67.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177(2):244–252. doi: 10.1001/jamainternmed.2016.7691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dzau VJ, McClellan MB, McGinnis JM, et al. Vital directions for health and health care: priorities from a National Academy of Medicine initiative. JAMA. 2017;317(14):1461–1470. doi: 10.1001/jama.2017.1964. [DOI] [PubMed] [Google Scholar]
- 69.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. doi: 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 71.Food and Nutrition Service . Supplemental nutrition assistance program: requirements for able-bodied adults without dependents. Alexandria: US Department of Agriculture; 2019. [Google Scholar]
- 72.Lowe ET, Poubelle A, Thomas G, Batko S, Layton J. The US Conference of Mayors’ report on hunger and homelessness: a status report on homelessness and hunger in America’s cities. Washington: National Alliance to End Homelessness; 2016. [Google Scholar]
- 73.Wright BN, MacDermid Wadsworth S, Wellnitz A, Eicher-Miller HA. Reaching rural veterans: a new mechanism to connect rural, low-income US Veterans with resources and improve food security. J Public Health (Oxf) 2019;41(4):714–723. doi: 10.1093/pubmed/fdy203. [DOI] [PubMed] [Google Scholar]
- 74.Stluka S, Moore L, Eicher-Miller HA, et al. Voices for food: methodologies for implementing a multi-state community-based intervention in rural, high poverty communities. BMC Public Health. 2018;18(1):1055–1063. doi: 10.1186/s12889-018-5957-9. [DOI] [PMC free article] [PubMed] [Google Scholar]