Abstract
Acinetobacter baumannii are bacteria that belong to the critical priority group due to their carbapenems and third generation cephalosporins resistance, which are last-chance antibiotics. The growing multi-drug resistance and the ability of these bacteria to form biofilms makes it difficult to treat infections caused by this species, which often affects people with immunodeficiency or intensive care unit patients. In addition, most of the infections are associated with catheterization of patients. These bacteria are causative agents, inter alia, of urinary tract infections (UTI) which can cause serious medical and social problems, because of treatment difficulties as well as the possibility of recurrence and thus severely decrease patients’ quality of life. Therefore, a promising alternative to standard antibiotic therapy can be bacteriophage therapy, which will generate lower costs and will be safer for the treated patients and has real potential to be much more effective. The aim of the review is to outline the important role of drug-resistant A. baumannii in the pathogenesis of UTI and highlight the potential for fighting these infections with bacteriophage therapy. Further studies on the use of bacteriophages in the treatment of UTIs in animal models may lead to the use of bacteriophage therapy in human urinary tract infections caused by A. baumannii in the future.
Keywords: bacteriophages, multidrug resistance (MDR), urinary tract infection (UTI), uropatogenic bacteria, critical priority group
1. Introduction
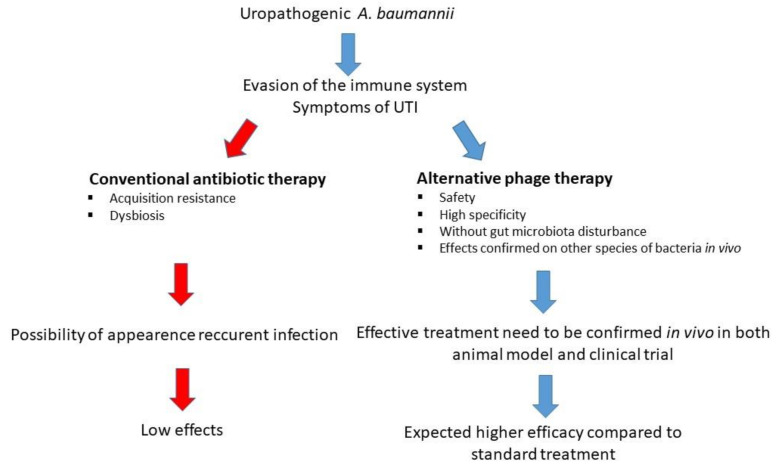
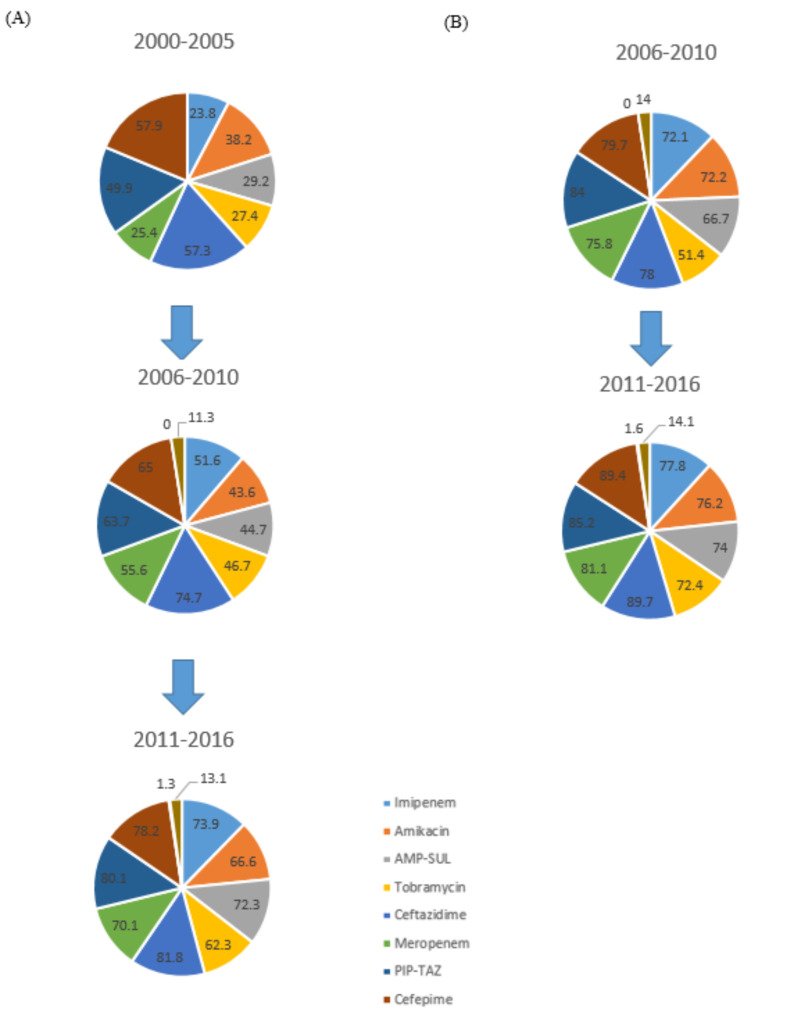
Each year, approximately 150 million people worldwide suffer from UTI [1]. They are caused by uropathogenic bacteria, such as Escherichia coli, Klebsiella, Staphylococcus, Enterococcus [2], and multi-drug resistant (MDR) Acinetobacter baumannii [3]. In addition to bacteria, urogenital infections can be caused by the sub-Saharan Africa endemic parasite Schistosoma haematobium [4] or by Candida species. Fungal infections of the urinary tract caused by Candida affect people with weakened immunity or those who are hospitalized [5]. Infection of the urinary tract causes many difficulties during treatment due to the increasing antibiotic resistance among bacterial strains [6]. Approximately 60% of women will experience a UTI at least once in their lifetime, and 20–30% of them will have had a recurrence within 6 months [6,7,8]. The costs incurred in the fight against UTI are related to the treatment, but also to the loss of productivity related to absence from work [6]. The common method of fighting UTI is antibiotic therapy. A huge problem arose when the widespread use of antibiotics resulted in the appearance of antibiotic-resistant bacterial strains all over the world. Therefore, other possibilities of treatments for UTI should be urgently considered [9]. One of the promising treatment methods is bacteriophage therapy (Figure 1), which can prove to be an effective method of combating this serious medical and social problem [10]. The increase in resistance among A. baumannii to currently used drugs is shown in Figure 2.
Figure 1.
Comparison of antibiotic therapy and the potential new alternative phage therapy in combating uropathogenic strains of A. baumannii.
Figure 2.
Resistance of A. baumannii strains in the world to available antibiotics in countries belonging to the Organization for Economic Co-operation and Development (OECD) (A) and non‑OECD (B). PIP-TAZ piperacillin-tazobactam, AMP-SUL ampicillin-sulbactam [11].
A. baumannii most often causes hospital bacteremia and lung infections. The presence of an endotracheal tube creates an ideal condition for the formation of bacterial biofilm, which results in infection [12]. Bloodstream infections caused by A. baumannii are related to the presence of the central venous catheter or as a consequence of extensive pneumonia. Additionally, A. baumannii causes infections of the urinary tract, usually associated with the presence of percutaneous nephrostomy tubes or urinary catheters. These pathogenic strains are also responsible for meningitis, osteomyelitis, endocarditis and wound infections. These infections occur mainly after an injury or surgery [13,14,15,16,17]. A. baumannii isolates are characterized by multi-drug resistance, therefore the treatment of infections caused by these bacteria is quite limited. Standard treatment of susceptible strains is based on the use of beta lactam antibiotics. In more difficult cases, carbapenems are applied [18,19,20]. The growing resistance among A. baumannii to currently used therapeutics has forced a search for a new effective, as well as safe method of fighting these infections, such as bacteriophage therapy [21]. Bacteriophages can be isolated from various environments [22,23,24]. Those specific to A. baumannii are most often isolated from water samples, especially from hospital sewage and almost every part of the human body [25,26,27,28,29]. When examining human samples, bacteriophages were detected in 11% of blood cultures, 14% of cerebrospinal fluid, 23% of urine samples, 28% of serum and 45% of ascitic fluid [30]. So far, rodent studies have shown that bacteriophages specific to a particular strain of A. baumannii can be helpful in combating infection (intraperitoneal sepsis, wound or lung infection) caused by this pathogen [31,32,33,34].
1.1. Global Problem of the Urinary Tract Infections Caused by A. baumannii
In recent years, all over the world, among nosocomial pathogens, an increasing number of infections have been caused by Gram-negative bacteria. Additionally, many of them are MDR strains [35]. MDR A. baumannii, formerly considered commensals, nowadays are associated with many dangerous hospital infections [36]. These strains can easily be isolated from intubated patients in the intensive care unit (ICU) [37]. Many of these strains are MDR; Lob et al. (2016) in their work described research on A. baumannii strains isolated from patients in 48 countries (453 hospitals) around the world under the Study for Monitoring Antimicrobial Resistance Trends (SMART) [38]. In this study from 2011 and 2014, 2337 A. baumannii isolates were collected. These strains were isolated from patients with intra-abdominal infections and UTIs, and for a group of 1011 isolates (2013–2014), sensitivity and multidrug resistance (resistant to at least three classes of drugs) were determined. Of these, 721 were from patients with intra-abdominal infections and 276 isolates were from patients with UTI. A total of 307 isolates came from intensive care units (ICU), and 615 from other hospital units.
Drug resistance was tested for the isolates of A. baumannii. Among the strains causing UTI in the Middle East, over 90% of the strains were MDR, similar to Europe 90% of A. baumannii strains were MDR. In Latin America, Africa, Asia and North America, approximately 85%, 80%, 70% and 50% of isolates were MDR, respectively. It is worth noting that in these regions of the world (except North America) over 90% of isolated A. baumannii strains in intensive care units were MDR. For North America, more than 60% of A. baumannii isolates were MDR, and this phenomenon remains unclear [38].
1.2. Acinetobacter baumannii as an Uropathogenic Species
Jiménez-Guerra et al. (2018) described the evolution of A. baumannii resistance in UTIs [39]. Among the isolated strains of A. baumannii, the highest percentage value of resistance was demonstrated for fosfomycin, aztreonam, ciprofloxacin, ceftazidime and cefepime. In vitro studies showed that colistin turned out to be the most effective antibiotic against these bacteria. Additionally, in the years 2013–2016 an increase in the resistance of A. baumannii isolates to imipenem, piperacillin-tazobactam and meropenem was noted. In addition to antibiotic resistance, A. baumannii may be resistant to bacteriophages. However, bacteriophage resistance may become a desirable trait. In vitro studies on two strains of A. baumannii (AB900 and A9844) showed that with the acquisition of resistance to specific bacteriophages (ΦFG02 and ΦCO01, respectively) the bacteria lost their capsule on the bacterial surface. The loss of capsule was due to a defect in the overall production of capsule polysaccharides in bacteriophage-resistant bacteria. This defect contributed to a 2 × decrease in the minimum inhibitory concentration (MIC) for ciprofloxacin and as much as a 16 × decrease in the MIC for ceftazidime for the bacteriophage resistant AB900 strain compared to the wild strain. For bacteriophage resistant strain A9844, a 2 × decrease in MIC was observed for minocycline, meropenem, cefepime and ampicillin with sulbactam compared to the wild strain. Additionally, resistance to bacteriophages of A. baumannii strains contributed to their sensitivity to the action of human complement [40].
Natural physiological mechanisms, such as the physicochemical properties of urine (e.g., the correct pH), urination, or the structure of the urethra, prevent bacteria from entering the sterile parts of the urinary tract. Some virulent organisms, known as uropathogens, have the ability to overcome natural protective barriers. This may be favored by the presence of adhesive fimbriae, exemplified by the synergistically acting type P and type 1 fimbriae in uropathogenic E. coli, which significantly promotes colonization of renal tubules [41]. Another important virulence factor—proteases, have also been described in UTI-causing Acinetobacter strains [42,43]. Important enzymes encoded by bacteria and conducive to the development of infections, including UTIs, are haemolysins and aerobactins [44], which are involved in the acquisition of iron necessary for bacterial growth.
Another group of enzymes are phospholipases, which contribute to an increase in bacterial virulence by degrading the phospholipids of human cell membranes [45]. Although Acinetobacter is considered a non-motile bacterium, it has been shown to be capable of twitching motility, which may contribute to it spreading more easily [46]. A. baumannii is also characterized by an escape from the human immune system by removing zinc ions, thanks to which bacterial growth is not inhibited by one of the proteins of the immune system—calprotectin. High resistance to dryness and the ability to pump out antiseptics significantly contribute to the difficulties in fighting this pathogen [45].
Di Venanzio et al. (2019) conducted an analysis of Acinetobacter isolates identified in the BJC Healthcare System (BJC) in the period from January 2007 to August 2017 [43]. Among 2309 cases of Acinetobacter calcoaceticus-baumannii complex (Acbc), 22.2% Acbc was isolated from urinary sources; other sources of Acbc isolation were respirators (33.9%), soft tissue/musculoskeletal (31.9%) and endovascular (10.4%). The authors made an even broader analysis, reviewing clinical trials since 1995, which took into account the anatomical location of Acbc or A. baumannii isolates. An analysis of over 19,000 cases showed that the majority of isolates came from the respiratory tract (39.5%) and soft tissue/musculoskeletal (22.7%). The percentage share of uropathogenic isolates ranged from 6.1% to 29.3%, and the average was 17.1% of all isolates (3410 from 19,957). From the above analysis it can be concluded that A. baumannii strains constitute a significant percentage of pathogens infecting the urinary tract (Table 1).
Table 1.
Anatomical sites of isolation of A. baumannii clinical strains.
| Total Isolate Number | Anatomical Site of A. baumannii Isolation (%) | Region of the World | Collection Date | Reference | ||||
|---|---|---|---|---|---|---|---|---|
| Urinary Tract | Respiratory Tract | Soft Tissue/Musculoskeletal | Endovascular | Other | ||||
| 7046 | 20.4 | 38.7 | 26.3 | 6.2 | 8.5 | Hong Kong | 01.1990–11.1994 | [47] |
| 1532 | 28.7 | 28.3 | 21.2 | 12.7 | 9.1 | Spain | 1991–1996 | [48] |
| 4484 | 9.9 | 48.9 | 13.9 | 18.3 | 9.0 | USA | 1.1994–12.2011 | [49] |
| 826 | 9.0 | 36.2 | 4.2 | 46.0 | 4.6 | Latin America | 1.1997–12.2001 | [50] |
| 1444 | 18.0 | 35.0 | 18.0 | 25.0 | 4.0 | USA | 1.1998–12.2005 | [51] |
| 58 | 29.3 | 0.0 | 63.8 | 6.9 | 0.0 | Nigeria | 2001 | [52] |
| 66 | 6.1 | 33.3 | 7.6 | 53.0 | 0.0 | Canada | 2007–2009 | [53] |
| 2273 | 22.2 | 33.9 | 31.9 | 10.4 | 1.5 | USA | 1.2007–7.2017 | [43] |
| 167 | 10.2 | 32.3 | 44.3 | 6.0 | 7.2 | Malaysia | 10.2010–4.2011 | [54] |
| 1176 | 10.8 | 26.8 | 42.3 | 9.4 | 10.8 | Saudi Arabia | 1.2010–12.2013 | [55] |
| 140 | 13.6 | 0.0 | 37.1 | 22.9 | 26.4 | India | 8.2010–7.2011 | [56] |
| 645 | 8.8 | 77.2 | 5.3 | 2.0 | 1.0 | Japan | 10.2012–3.2013 | [57] |
| 100 | 13.0 | 59.0 | 15.0 | 12.0 | 1.0 | Iran | 5.2015–7.2016 | [58] |
| 19,957 | 17.1 | 39.5 | 22.7 | 13.2 | 7.5 | Total | ||
The analysis shows that on average, 17.1% of A. baumannii strains are isolated from urinary sources, but only 2% of UTIs are caused by these bacteria. However, A. baumannii is the main pathogen causing UTIs associated with the use of catheters in intensive care units [59,60]. More than half of A. baumannii strains isolated from urine come from catheterized patients. Moreover, other infections caused by A. baumannii are often associated with the use of medical equipment, such as central venous lines or endotracheal [61]. Di Venanzio et al. (2019), to investigate the uropathogenesis of A. baumannii, used the catheter-associated UTI mouse model [43]. This model is frequently used to study the uropathogenic methicillin-resistant Staphylococcus aureus (MRSA), Group B Streptococcus, Escherichia coli and Enterococcus faecalis [62,63,64]. Two strains of A. baumannii isolated from urine were used to test the ability to colonize the kidneys and bladder of mice: UPAB1 and ATCC19606. The isolated MDR UPAB1 strain came from a patient with uncomplicated UTI; the ATCC19606 strain is widely used to study the virulence of A. baumannii in murine models of sepsis and pneumonia [43,65]. The bacteria were administered through an implant (transurethrally by a small piece of silicone tube) placed in the animal’s urethra [43]. The results of the experiment show that infection with the UPAB1 strain caused a 5 log increase in bacterial count on the implants and in the bladders of mice 24 h after infection. A fluorescence microscope confirmed the presence of bacteria on the silicone implants and luminal urothelial surface, whereas the ATCC19606 strain was almost completely removed from the body of the mice 24 h after infection. This study showed that UPAB1 infects the urinary tract like other uropathogenic bacteria.
Sequencing of the UPAB1 genome indicated that this strain possesses the pAB5 plasmid, the presence of which affected uropathogenesis and was associated with a higher bacterial titer on the implant and urinary bladder of mice in the catheter-associated UTI (compared to the control without the plasmid). Completely different results were obtained for lung infection in mice caused by the UPAB1 strain. In the case of the wild-type strain (with the pAB5 plasmid), 36 h after intranasal administration, the bacterial titer was 1 to 4 logs lower in livers, lungs, kidneys, spleens and hearts compared to the infection with the strain without the plasmid. In addition, no deaths were reported among mice infected with the wild-type bacterial strain where infection with the strain without plasmid resulted in 40% mortality in the animals. The results suggest that A. baumannii strains show different survival rates depending on the anatomical location of the host, and additional studies are needed to thoroughly investigate their pathobiology [43].
In the United States, approximately 100,000 cases of catheter-UTIs are reported each year [66]. This may be due to the formation of a bacterial biofilm on the surface of the catheter [67]. Even more than 75% of A. baumannii strains are capable of producing biofilm, therefore the bacteria may contribute significantly to UTIs [68,69,70]. Braun and Vidotto (2004) isolated 13 strains of A. baumannii derived from urinary sources from patients aged 18 to 88 years. Six strains have been isolated from hospital patients and seven from outpatients. The susceptibility of these strains to selected antibiotics was tested, three strains from non-hospitalized patients were sensitive to the action of most of the antibiotics used. Interestingly, the remaining strains turned out to be resistant to amikacin, ceftriaxone, ciprofloxacin and trimethoprim-sulfamethoxazole. [71]. Pour et al. (2011) also described uropathogenic strains of A. baumannii. Researchers isolated 47 strains of A. baumannii and three strains of A. lwoffii from urinary tract and urinary catheter samples. The ability of the tested strains to produce biofilm was also assessed, and it turned out that biofilm forms better on polypropylene than on glass surfaces. Additionally, shaking promoted the formation of a bacterial biofilm. What is more, resistance to 27 different antibiotics was tested for six biofilm-forming strains of A. baumannii. These isolates were resistant to 97% of aminoglycosides, 94.4% of the cephalosporin group, 83.3% of β-lactams, 75% of quinolones, 66.6% of tetracycline and oxytetracycline, 33.3% of imipenem and 50% of the other antibiotics tested. Interestingly, all isolates were sensitive to colistin [72].
A. baumannii infections do not only affect humans, they also cause infections in animals. Kuzi et al. (2016) described UTIs in hospitalized dogs and cats caused by Acinetobacter calcoaceticus-baumannii complex (Acbc) [73]. A total of 19 dogs and four cats were hospitalized due to the primary disease. Twenty-two animals were treated in the intensive care unit and five of them were transferred to the general hospitalization ward after 1–3 days. The animals were hospitalized for 2 to 15 days. There were clinical signs among the animals (including: weakness 52%, fever 39%, urine turbidity 30%) indicative of a healthcare-associated secondary Acbc infection (pneumonia, UTI, sepsis, cellulitis and septic arthritis). In total, 10 hospitalized animals (two cats and eight dogs) were diagnosed with UTI and the Acbc was isolated from the urine in two cats and seven dogs. All animals diagnosed with secondary Acbc urinary tract infection were previously catheterized. Antibiotics were given to all animals diagnosed with Acbc infection. As a result of infection, all dogs with the infection survived and two cats died [73].
Bacterial strains isolated from animals are also characterized by a significant increase in MDR [74]. The Acbc strains were isolated from cats and dogs from urine, blood, bronchoalveolar lavage fluid, kidneys, lungs, heart, and liver, as well as fluid aspirated from subcutaneous tissues with cellulitis. For all isolated Acbc strains, the antibiotic resistance profile was investigated. All of them were resistant to most of the tested antibiotics commonly used in hospitals: amoxicillin-clavulanic acid, amikacin, ampicillin, fluoroquinolones, gentamycin, sulfamethoxazole/trimethoprim, polymyxin B, florfenicol, third generation cephalosporins, second generation cephalosporins, first generation cephalosporins, imipenem and ticarcillin. The isolated strains turned out to be sensitive only to polymyxin-B (96%), imipenem (74%), ticarcillin (59%) and amikacin (35%). The above study shows that veterinary MDR Acbc infections are characterized by high mortality up to 70% [73].
It is important to remember that there is a significant problem regarding the possibility of transmitting zoonotic pathogens to humans, including bacteria from the ESKAPE group, such as A. baumannii [75]. The role of animals, especially dogs, in helping in the treatment of hospitalized patients is clearly emphasized, and despite their many benefits, they can pose a serious threat as carriers of pathogens.
1.3. Bacteriophages as a Tool in the Fight against Uropathogenic Bacteria
Bacteriophages were discovered over 100 years ago, first by microbiologist Frederick Twort in 1915 [76]. Then, in 1917, Felix d’Herelle published a paper about bacteriophages, as invisible microbes that were present in the filtrate of feces of people suffering from dysentery. He showed that the titer of bacteriophages increases with the development of the disease and reaches its highest value during recovery. d’Herelle tested bacteriophage therapy on himself and his relatives, and then on patients with dysentery and cholera. It was then used to heal wounds, and the bacteriophages were tested for avian typhosis caused by Salmonella gallinarum. Bacteriophages have been used against Pasteurella multocida in the treatment of bovine hemorrhagic septicaemia. However, the first paper on bacteriophage therapy appeared in 1921, published by Bruynoghe and Maisin [76]. Due to the discovery of antibiotics, the use of bacteriophages has been limited to Poland and Georgia [77]. Nowadays however, because of problems with antibiotic inefficiency, this method of treating bacterial infections has gained renewed interest.
Bacteriophage therapy, unlike antibiotics, does not damage the natural microbiota of both the human and animal body. Because bacteriophages are able to be amplified only with the presence of susceptible bacteria causing lysis of their cells, they are named self-limiting “drugs”. What is more, bacteriophages may also be active against antibiotic-resistant strains of bacteria. Therefore, in people with bacterial infections, where antibiotics failed, it is possible to use lytic bacteriophages [10,28] that also proved to be safe and well-tolerated by immunocompromised patients as well as people allergic to antibiotics. This is likely due to their structure, which is composed of proteins and nucleic acids only and therefore are considered as non-toxic [78]. In contrast to antibiotics, bacterial viruses that are most abundant in the environment can thus be sought and isolated from places where bacteria are present [79,80,81]. Bacteriophages can be found in almost any environment, and thus the costs associated with the production of bacteriophage preparations are lower than in the case of antibiotics [82]. Interestingly, a particularly desirable feature of bacteriophages is their ability to combat bacterial biofilm, the structure of which is difficult to penetrate and destroy by antibiotics. In addition, the potential of bacteriophage therapy efficacy against pathogenic microorganisms has been confirmed by different studies on animal models [83,84,85,86]. Due to the features mentioned above, bacteriophage therapy has become a promising and effective alternative to standard therapy for the treatment of UTIs also caused by MDR bacteria.
In the case of UTI treatment, natural bacteriophage cocktails, bacteriophage lytic enzymes or proteins (natural or engineered form), genetically engineered bacteriophages, as well as bacteriophages in combination with antibiotics may be used. Thus, bacteriophages can be detected in the urine, and despite its alkaline pH, bacteriophages can remain active in the urine [22,87]. For example, UTIs by E. coli resulted in the appearance of bacteriophages specific for these bacteria in the urine [88,89]. Active bacteriophage particles specific to E. coli were detected in the urine after intravenous injection of purified preparation into the bloodstream [90]. Interestingly, specific bacteriophages in urine were also found in 30% of patients after oral administration of bacteriophage preparation [91].
Nowadays, bacteria are acquiring new and more sophisticated resistance mechanisms to the available antibiotics. Lytic bacteriophages are capable of destroying bacteria at the end of the infection cycle, and antibiotic resistance in the case of bacterial strains does not preclude effective bacteriophage therapy [78]. Therefore, bacteriophage therapy serves as a great tool to fight MDR bacterial infections [92], especially UTI caused by MDR A. baumannii.
UTIs are a serious social and economic problem. In the United States, as many as seven million medical visits and more than 100 thousand hospital admissions a year are caused by UTIs. A total of 15% of prescribed antibiotics are used to treat UTIs, at a cost of 1.6 billion dollars a year [93]. Pyelonephritis is a common case of patient UTIs and is associated with the patient’s catheterization [94]. Another problem in the fight against UTI is the widespread use of antibiotics and the increasing phenomenon of resistance acquisition among uropathogenic strains [95,96]. Bacteriophage therapy is recognized as safe and effective in the treatment of UTI, as confirmed by clinical trials for the treatment of UTI and diarrhea in children caused by enteropathogenic E. coli, uropathogenic E. coli, enterotoxigenic E. coli, and P. aeruginosa [97,98,99,100]. Therefore, bacteriophages may be a real alternative for treating UTI. Due to the bacteriophage preparations, it is possible to combat specific bacterial hosts. Compared to bacterial resistance to antibiotics, bacteriophage resistance is slight, but present among some bacterial strains [101]. Nevertheless, there are many readily available sources of searching for new bacteriophages [102,103], and the process leading to the discovery of a new bacteriophage is relatively inexpensive and fast, therefore it is quite easy to match specific bacteriophages to specific bacterial strains. The use of a bacteriophage cocktail instead of monotherapy reduces the likelihood of the emergence of bacteriophage resistance. Each of the bacteriophages can be attached to a different receptor in a bacterial cell, and different bacteriophages can also act synergistically, so using a cocktail of several bacteriophages increases the probability of therapeutic effectiveness [104,105].
Using an intravenous catheter, Nishikawa et al. (2008) transurethrally injected an uropathogenic E. coli strain ECU5 (5·109 CFU/mL) into the BALB/c mouse bladder [106]. Next, the purified T4 at multiplicities of infection (MOIs): 0.01–60 or KEP10: MOI = 60 bacteriophages were administered into the peritoneal cavity. For T4 bacteriophage at MOI 0.01, 0.1, 0.5, 1 and 60 survival rate after 3 days was 40%, 60%, 40%, 80% and 100% respectively. The administration of the KEP10 at MOI = 60 rescued 90% of infected animals compared to the untreated control where 100% of the mice died [106].
Subsequently, UTI bacteriophage therapy was applied in a mouse model through the transurethral application of Cronobacter turicensis (1011 CFU/mL). At the same time, specific bacteriophages were given intraperitoneal at a titer of 1011 PFU/mL. After 24 h, the bacterial count in the kidneys in mice treated with bacteriophage therapy reduced the bacterial count by 70% [107].
Sybesma et al. (2016) described the effect of commercial bacteriophage cocktails on uropathogenic clinical strains of K. pneumoniae and E. coli [108] in vitro. The results of a study of 41 clinical E. coli strains showed that the lytic activity of the Enko, Ses, Intesti, Pyo (before adaptation) and Pyo (after adaptation) bacteriophage cocktails was 92.7%, 90.2%, 82.9%, 65.9% and 92.7%, respectively. For nine clinical K. pneumoniae strains, the lytic activity of 10 bacteriophages from the Eliava collection ranged from 0% (vB_KlpR1, vB_KloxR2, vB_KlpR5 and vB_KlpR7 bacteriophage), 11% (vB_KlpR6 bacteriophage), 22% (vB_KlpR3, vB_KlpR4 and vB_KlpR8 bacteriophage), 56% (v_BRKpM9 bacteriophage) up to even 100% (v_BRKpS10 bacteriophage).
Many of the uropathogenic bacterial strains have the ability to produce biofilm, especially in urinary catheters, which hinders the therapeutic effects of antibiotics [67,109,110]. The antimicrobial activity of bacteriophages against biofilm-producing A. baumannii strains was demonstrated in vitro in the study conducted by Vukotic et al. [111]. Two bacteriophages, isolated from Belgrade wastewater samples, were tested against 103 A. baumannii isolates, resulting in a higher host range for the ISTD bacteriophage compared to NOVI bacteriophage (36% and 22%, respectively). Moreover, a reduction in bacterial cell count in the biofilm formed on porous glass beads was observed 6 h after ISTD bacteriophage application. However, after 24 h of observation, the number of bacterial cells did not differ between the biofilm on which the bacteriophages were applied and the control biofilm.
The action of bacteriophages combined with antibiotics on the reduction in biofilm produced by uropathogenic strains of A. baumannii was tested in vitro [112]. Among 25 clinical uropathogenic strains of A. baumannii, one was selected AB20, which was characterized by a strong biofilm formation capacity, sensitivity to the bacteriophage used (Aba-1–Aba-6) and resistance to antibiotics (ciprofloxacin, meropenem, levofloxacin, trimethoprim/sulfamethoxazole, netilmicin gentamicin, and imipenem). The bacterial biofilm produced after 24 h, immersed in human urine, was treated with 1/2 MIC and 1/4 MIC of antibiotics: ciprofloxacin (MIC = 8), levofloxacin (MIC = 16), trimethoprim/sulfamethoxazole (MIC = 64), amikacin (MIC = 32), tobramycin (MIC = 2), gentamicin (MIC = 64), colistin (MIC = 1), imipenem (MIC = 16), meropenem (MIC = 32). Then, a bacteriophage cocktail (Aba-1, Aba-2, Aba-3, Aba-4, and Aba-6) with a titer of 1·107 PFU/mL was added to each sample with an antibiotic. After 6 h of incubation, the highest level of biofilm biomass reduction was recorded for bacteriophages combined with trimethoprim/sulfamethoxazole 98.6% and 94.3% for ½ and ¼ MIC, respectively. The use of ciprofloxacin in combination with the bacteriophage cocktail resulted in a reduction of 93.3% and 87% for ½ and ¼ MIC, respectively. For the remaining antibiotics, the results were similar, only amikacin and levofloxacin did not act synergistically with bacteriophages. Additionally, the weakest result was recorded for the combination of the bacteriophage cocktail with colistin, where increased biofilm formation was noted. The bacteriophage cocktail alone reduced the biofilm biomass in 77%. These studies indicate that bacteriophage therapy in the future may be a useful tool in the fight against UTIs in humans. So far, no studies have been conducted on the use of bacteriophage therapy in the treatment of UTIs caused by A. baumannii in an animal model. However, other work on treating UTIs caused by uropathogenic strains (E. coli, P. aeruginosa, Cronobacter spp.) has shown positive results [97,98,99,100,107]. Due to the differences between the human body and the organisms of various animals, the results obtained in vivo studies with the use of animal models cannot be fully related to the human body, but they significantly help, e.g., in choosing the most advantageous route of bacteriophage administration or assessing the appropriate therapeutic dose [113].
The possibility of using bacteriophage-derived enzymes as effective tools to combat UTI is also emphasized [114]. Despite the satisfactory results of the action of bacteriophage lysins mainly on Gram-positive bacteria, promising studies of these enzymes in A. baumannii sepsis in a mouse model have been conducted [115].
Bacteriophages are capable of fighting bacterial biofilm that can form on the catheters. Additionally, bacteriophages can be used in conjunction with antibiotics. Grygorcewicz et al. (2020) in their work presented promising results of the fight against A. baumannii biofilm with the use of bacteriophage cocktail combined with antibiotics in a human urine model. The use of a bacteriophage cocktail (Aba-1, Aba-2, Aba-3, Aba-4, and Aba-6) in combination with ciprofloxacin, trimethoprim/sulfamethoxazole, gentamicin, tobramycin, imipenem and meropenem resulted in a significant reduction in the biofilm biomass of A. baumannii AB20. The best combination turned out to be the combination of the bacteriophage cocktail with trimethoprim/sulfamethoxazole, where the reduction in biofilm reached 94.3% and 98.6%, with ¼ and ½ MIC, respectively [112].
Studies have also been carried out using the Pyo bacteriophage in the treatment of patients with UTI [97]. Of 118 clinical uropathogens (P. aeruginosa, E. coli, Streptococcus spp., Proteus mirabilis, S. aureus), 41% of the strains were sensitive to the action of the Pyo bacteriophage, and after its four-fold adaptation, the sensitivity of the bacteria increased to 75%. In the second part of the study, urine samples were collected from nine patients after transurethral resection of the prostate. E. coli was detected in the samples of four patients, Streptococcus spp. in two, Enterococcus spp. in two and P. aeruginosa in one of the nine patients. The patients were administered the Pyo bacteriophage intravesically. The bacteriophage was administered twice a day for 7 days (starting from the first day after the treatment) at a volume of 20 mL. The bacteriophage-containing solution was in the bladder for 0.5–1 h. After treatment with bacteriophages, six of nine patients had a 1 to 5 log reduction in urine bacterial counts. Additionally, no side effects of bacteriophage therapy were noted. Other studies show that bacteriophage therapy in treating UTI has not been shown to be more effective than washing the bladder with a placebo solution and standard antibiotic therapy [116].
In addition to the positive aspects, bacteriophage therapy also has limitations. One of them is the possibility of pathogens acquiring bacteriophage resistance. Therefore, bacteriophage cocktails are used due to the lower probability of resistance to all bacteriophages present in the cocktail [101]. In addition, UTI can be caused by more than one bacterial strain, therefore monotherapy in comparison to bacteriophage cocktails may turn out to be unsuccessful [117]. Another limitation of bacteriophage therapy may be the limited access of bacteriophages to biofilm-building bacteria—due to the layers of extracellular polymeric substances (EPS) surrounding the bacteria [118]. A negative effect of bacteriophage therapy may be the adverse response of the immune system due to the sudden lysis of bacteria and the release of toxic lipopolysaccharides [119]. A serious limitation of bacteriophage therapy is that there is not much evidence that the use of bacteriophages alone (without antibiotics) is capable of combating UTIs [120].
Although bacteriophage therapy is not an approved method of treating UTI, further research will optimize this method and determine the role of bacteriophages in the fight against UTI [116]. The results suggest that bacteriophage therapy has great potential in treating UTIs, which needs confirmation in the case of UTI caused by A. baumannii strains.
2. Conclusions
The species Acinetobacter baumannii has been classified to the list of the ten most serious threats to public health and as a critical priority group. Currently, many bacteria, including A. baumannii [121], exhibit resistance to a wide spectrum of available antibiotics [122]. Consequently, antibiotics cannot be considered as a real and effective agent against bacterial infections caused by these pathogens. Moreover, in addition to being resistant to many antimicrobial agents, the Acinetobacter species has many characteristics that facilitate its spread and increase pathogenicity, such as the aforementioned ability to produce enzymes that allow more efficient acquisition of ingredients necessary for the survival of bacteria or the ability to escape from the human immune system.
An infection of the urinary tract is common and causes many difficulties during treatment due to the antibiotic resistance among bacterial strains and the side effects observed after and/or during antibiotic therapy, therefore other treatments for UTI should be considered [123,124,125,126,127]. Previous studies have shown that UTIs pose serious medical, social and economic problems [6,7,8]. One of the possibilities may be bacteriophage therapy, which can prove to be an effective method to solve this problem. Future studies on the treatment of UTIs caused by uropathogenic strains of A. baumannii may have a bearing on the use of this solution in humans in the future. Further research should focus on developing an animal model of UTI caused by A. baumannii. Appropriately selected bacteriophages may constitute the composition of a bacteriophage cocktail capable of fighting infections caused by A. baumannii [128]. Future studies in animal models may lead to the development of a treatment model for A. baumannii UTI in humans.
Author Contributions
N.B. drafted the main part of the manuscript, M.C. and E.J.-M. contributed to the parts of the manuscript, A.G. and E.J.-M. provided support and conceptual advice at all stages of manuscript preparation; all authors revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by statutory funds from Ludwik Hirszfeld Institute of Immunology and Experimental Therapy, Polish Academy of Science.
Conflicts of Interest
A. Górski is a co-inventor of patents owned by L. Hirszfeld Institute and covered bacteriophage preparations. Other authors declared that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Öztürk R., Murt A. Epidemiology of urological infections: A global burden. World J. Urol. 2020;38:2669–2679. doi: 10.1007/s00345-019-03071-4. [DOI] [PubMed] [Google Scholar]
- 2.Flores-Mireles A.L., Walker J.N., Caparon M., Hultgren S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015;13:269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fournier P.E., Richet H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin. Infect. Dis. 2006;42:692–699. doi: 10.1086/500202. [DOI] [PubMed] [Google Scholar]
- 4.Odegaard J.I., Hsieh M.H. Immune responses to Schistosoma haematobium infection. Parasite Immunol. 2014;36:428–438. doi: 10.1111/pim.12084. [DOI] [PubMed] [Google Scholar]
- 5.Sobel J.D., Fisher J.F., Kauffman C.A., Newman C.A. Candida urinary tract infections—Epidemiology. Clin. Infect. Dis. 2011;52:S433–S436. doi: 10.1093/cid/cir109. [DOI] [PubMed] [Google Scholar]
- 6.Foxman B., Barlow R., D’Arcy H., Gillespie B., Sobel J.D. Urinary tract infection: Self-reported incidence and associated costs. Ann. Epidemiol. 2000;10:509–515. doi: 10.1016/S1047-2797(00)00072-7. [DOI] [PubMed] [Google Scholar]
- 7.Foxman B. Urinary tract infection syndromes: Occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect. Dis. Clin. N. Am. 2014;28:1–13. doi: 10.1016/j.idc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Wang C.H., Fang C.C., Chen N.C., Liu S.S., Yu P.H., Wu T.Y., Chen W.T., Lee C.C., Chen S.C. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: A systematic review and meta-analysis of randomized controlled trials. Arch. Intern. Med. 2012;172:988–996. doi: 10.1001/archinternmed.2012.3004. [DOI] [PubMed] [Google Scholar]
- 9.Foxman B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010;7:653–660. doi: 10.1038/nrurol.2010.190. [DOI] [PubMed] [Google Scholar]
- 10.Górski A., Międzybrodzki R., Łobocka M., Głowacka-Rutkowska A., Bednarek A., Borysowski J., Jończyk-Matysiak E., Łusiak-Szelachowska M., Weber-Dąbrowska B., Bagińska N., et al. Bacteriophage Therapy: What Have We Learned? Viruses. 2018;10:288. doi: 10.3390/v10060288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie R., Zhang X.D., Zhao Q., Peng B., Zheng J. Analysis of global prevalence of antibiotic resistance in Acinetobacter baumannii infections disclosed a faster increase in OECD countries. Emerg. Microbes Infect. 2018;7:31. doi: 10.1038/s41426-018-0038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raad I.I., Mohamed J.A., Reitzel R.A., Jiang Y., Dvorak T.L., Ghannoum M.A., Hachem R.Y., Chaftari A.M. The prevention of biofilm colonization by multidrug-resistant pathogens that cause ventilator-associated pneumonia with antimicrobial-coated endotracheal tubes. Biomaterials. 2011;32:2689–2694. doi: 10.1016/j.biomaterials.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 13.Joly-Guillou M.L. Clinical impact and pathogenicity of Acinetobacter. Clin. Microbiol. Infect. 2005;11:868–873. doi: 10.1111/j.1469-0691.2005.01227.x. [DOI] [PubMed] [Google Scholar]
- 14.Sievert D.M., Ricks P., Edwards J.R., Schneider A., Patel J., Srinivasan A., Kallen A., Limbago B., Fridkin S. National Healthcare Safety Network (NHSN) Team and Participating NHSN Facilities. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect. Control. Hosp. Epidemiol. 2013;34:1–14. doi: 10.1086/668770. [DOI] [PubMed] [Google Scholar]
- 15.Davis K.A., Moran K.A., McAllister C.K., Gray P.J. Multidrug-resistant Acinetobacter extremity infections in soldiers. Emerg. Infect. Dis. 2005;11:1218–1224. doi: 10.3201/1108.050103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yun H.C., Branstetter J.G., Murray C.K. Osteomyelitis in military personnel wounded in Iraq and Afghanistan. J. Trauma. 2008;64:S163–S168. doi: 10.1097/TA.0b013e318160868c. [DOI] [PubMed] [Google Scholar]
- 17.Carvalho V.C., Oliveira P.R., Dal-Paz K., Paula A.P., Félix Cda S., Lima A.L. Gram-negative osteomyelitis: Clinical and microbiological profile. Braz. J. Infect. Dis. 2012;16:63–67. doi: 10.1590/S1413-86702012000100011. [DOI] [PubMed] [Google Scholar]
- 18.Saballs M., Pujol M., Tubau F., Peña C., Montero A., Domínguez M.A., Gudiol F., Ariza J. Rifampicin/imipenem combination in the treatment of carbapenem-resistant Acinetobacter baumannii infections. J. Antimicrob. Chemother. 2006;58:697–700. doi: 10.1093/jac/dkl274. [DOI] [PubMed] [Google Scholar]
- 19.Fraenkel C.J., Ullberg M., Bernander S., Ericson E., Larsson P., Rydberg J., Törnqvist E., Melhus A. In vitro activities of three carbapenems against recent bacterial isolates from severely ill patients at Swedish hospitals. Scand. J. Infect. Dis. 2006;38:853–859. doi: 10.1080/00365540600684371. [DOI] [PubMed] [Google Scholar]
- 20.Scott P., Deye G., Srinivasan A., Murray C., Moran K., Hulten E., Fishbain J., Craft D., Riddell S., Lindler L., et al. An outbreak of multidrug-resistant Acinetobacter baumannii-calcoaceticus complex infection in the US military health care system associated with military operations in Iraq. Clin. Infect. Dis. 2007;44:1577–1584. doi: 10.1086/518170. [DOI] [PubMed] [Google Scholar]
- 21.LaVergne S., Hamilton T., Biswas B., Kumaraswamy M., Schooley R.T., Wooten D. Bacteriophage Therapy for a Multidrug-Resistant Acinetobacter baumannii Craniectomy Site Infection. Open Forum Infect. Dis. 2018;5:ofy064. doi: 10.1093/ofid/ofy064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jończyk E., Kłak M., Międzybrodzki R., Górski A. The influence of external factors on bacteriobacteriophages—Review. Folia Microbiol. 2011;56:191–200. doi: 10.1007/s12223-011-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucena F., Ribas F., Duran A.E., Skraber S., Gantzer C., Campos C., Morón A., Calderón E., Jofre J. Occurrence of bacterial indicators and bacteriobacteriophages infecting enteric bacteria in groundwater in different geographical areas. J. Appl. Microbiol. 2006;101:96–102. doi: 10.1111/j.1365-2672.2006.02907.x. [DOI] [PubMed] [Google Scholar]
- 24.Gantzer C., Henny J., Schwartzbrod L. Bacteroides fragilis and Escherichia coli bacteriobacteriophages in human faeces. Int. J. Hyg. Environ. Health. 2002;205:325–328. doi: 10.1078/1438-4639-00152. [DOI] [PubMed] [Google Scholar]
- 25.Yang H., Liang L., Lin S., Jia S. Isolation and characterization of a virulent bacteriobacteriophage AB1 of Acinetobacter baumannii. BMC Microbiol. 2010;10:131. doi: 10.1186/1471-2180-10-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin N.T., Chiou P.Y., Chang K.C., Chen L.K., Lai M.J. Isolation and characterization of phi AB2: A novel bacteriobacteriophage of Acinetobacter baumannii. Res. Microbiol. 2010;161:308–314. doi: 10.1016/j.resmic.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Ghajavand H., Esfahani B.N., Havaei A., Fazeli H., Jafari R., Moghim S. Isolation of bacteriobacteriophages against multidrug resistant Acinetobacter baumannii. Res. Pharm. Sci. 2017;12:373–380. doi: 10.4103/1735-5362.213982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Górski A., Wazna E., Dabrowska B.W., Dabrowska K., Switała-Jeleń K., Miedzybrodzki R. Bacteriobacteriophage translocation. FEMS Immunol. Med. Microbiol. 2006;46:313–319. doi: 10.1111/j.1574-695X.2006.00044.x. [DOI] [PubMed] [Google Scholar]
- 29.Żaczek M., Weber-Dąbrowska B., Międzybrodzki R., Górski A. Bacteriophage Prevalence in the Human Urinary Tract-Current Knowledge and Therapeutic Implications. Microorganisms. 2020;8:1802. doi: 10.3390/microorganisms8111802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blanco-Picazo P., Fernández-Orth D., Brown-Jaque M., Miró E., Espinal P., Rodríguez-Rubio L., Muniesa M., Navarro F. Unravelling the consequences of the bacteriobacteriophages in human samples. Sci. Rep. 2020;10:6737. doi: 10.1038/s41598-020-63432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.García-Quintanilla M., Pulido M.R., López-Rojas R., Pachón J., McConnell M.J. Emerging therapies for multidrug resistant Acinetobacter baumannii. Trends Microbiol. 2013;21:157–163. doi: 10.1016/j.tim.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Jeon J., Ryu C.M., Lee J.Y., Park J.H., Yong D., Lee K. In Vivo Application of Bacteriobacteriophage as a Potential Therapeutic Agent To Control OXA-66-Like Carbapenemase-Producing Acinetobacter baumannii Strains Belonging to Sequence Type 357. Appl. Environ. Microbiol. 2016;82:4200–4208. doi: 10.1128/AEM.00526-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y., Mi Z., Niu W., An X., Yuan X., Liu H., Li P., Liu Y., Feng Y., Huang Y., et al. Intranasal treatment with bacteriobacteriophage rescues mice from Acinetobacter baumannii-mediated pneumonia. Future Microbiol. 2016;11:631–641. doi: 10.2217/fmb.16.11. [DOI] [PubMed] [Google Scholar]
- 34.Shivaswamy V.C., Kalasuramath S.B., Sadanand C.K., Basavaraju A.K., Ginnavaram V., Bille S., Ukken S.S., Pushparaj U.N. Ability of bacteriobacteriophage in resolving wound infection caused by multidrug-resistant Acinetobacter baumannii in uncontrolled diabetic rats. Microb. Drug Resist. 2015;21:171–177. doi: 10.1089/mdr.2014.0120. [DOI] [PubMed] [Google Scholar]
- 35.Livermore D.M. Current epidemiology and growing resistance of gram-negative pathogens. Korean J. Intern. Med. 2012;27:128–142. doi: 10.3904/kjim.2012.27.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falagas M.E., Karveli E.A., Siempos I.I., Vardakas K.Z. Acinetobacter infections: A growing threat for critically ill patients. Epidemiol. Infect. 2008;136:1009–1019. doi: 10.1017/S0950268807009478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmed N.H., Hussain T., Biswal I. Antimicrobial resistance of bacterial isolates from respiratory secretions of ventilated patients in a multi-specialty hospital. Avicenna J. Med. 2015;5:74–78. doi: 10.4103/2231-0770.160233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lob S.H., Hoban D.J., Sahm D.F., Badal R.E. Regional differences and trends in antimicrobial susceptibility of Acinetobacter baumannii. Int. J. Antimicrob. Agents. 2016;47:317–323. doi: 10.1016/j.ijantimicag.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 39.Jiménez-Guerra G., Heras-Cañas V., Gutiérrez-Soto M., Del Pilar Aznarte-Padial M., Expósito-Ruiz M., Navarro-Marí J.M., Gutiérrez-Fernández J. Urinary tract infection by Acinetobacter baumannii and Pseudomonas aeruginosa: Evolution of antimicrobial resistance and therapeutic alternatives. J. Med. Microbiol. 2018;67:790–797. doi: 10.1099/jmm.0.000742. [DOI] [PubMed] [Google Scholar]
- 40.Gordillo Altamirano F., Forsyth J.H., Patwa R., Kostoulias X., Trim M., Subedi D., Archer S.K., Morris F.C., Oliveira C., Kielty L., et al. Bacteriobacteriophage-resistant Acinetobacter baumannii are resensitized to antimicrobials. Nat. Microbiol. 2021;6:157–161. doi: 10.1038/s41564-020-00830-7. [DOI] [PubMed] [Google Scholar]
- 41.Melican K., Sandoval R.M., Kader A., Josefsson L., Tanner G.A., Molitoris B.A., Richter-Dahlfors A. Uropathogenic Escherichia coli P and Type 1 fimbriae act in synergy in a living host to facilitate renal colonization leading to nephron obstruction. PLoS Pathog. 2011;7:e1001298. doi: 10.1371/journal.ppat.1001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinsella R.L., Lopez J., Palmer L.D., Salinas N.D., Skaar E.P., Tolia N.H., Feldman M.F. Defining the interaction of the protease CpaA with its type II secretion chaperone CpaB and its contribution to virulence in Acinetobacter species. J. Biol. Chem. 2017;292:19628–19638. doi: 10.1074/jbc.M117.808394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Venanzio G., Flores-Mireles A.L., Calix J.J., Haurat M.F., Scott N.E., Palmer L.D., Potter R.F., Hibbing M.E., Friedman L., Wang B., et al. Urinary tract colonization is enhanced by a plasmid that regulates uropathogenic Acinetobacter baumannii chromosomal genes. Nat. Commun. 2019;10:2763. doi: 10.1038/s41467-019-10706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raeispour M., Ranjbar R. Antibiotic resistance, virulence factors and genotyping of Uropathogenic Escherichia coli strains. Antimicrob. Resist. Infect. Control. 2018;7:118. doi: 10.1186/s13756-018-0411-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ayoub Moubareck C., Hammoudi Halat D. Insights into Acinetobacter baumannii: A Review of Microbiological, Virulence, and Resistance Traits in a Threatening Nosocomial Pathogen. Antibiotics. 2020;9:119. doi: 10.3390/antibiotics9030119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harding C.M., Tracy E.N., Carruthers M.D., Rather P.N., Actis L.A., Munson R.S., Jr. Acinetobacter baumannii strain M2 produces type IV pili which play a role in natural transformation and twitching motility but not surface-associated motility. mBio. 2013;4:e00360. doi: 10.1128/mBio.00360-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siau H., Yuen K.Y., Wong S.S., Ho P.L., Luk W.K. The epidemiology of acinetobacter infections in Hong Kong. J. Med. Microbiol. 1996;44:340–347. doi: 10.1099/00222615-44-5-340. [DOI] [PubMed] [Google Scholar]
- 48.Ruiz J., Núñez M.L., Pérez J., Simarro E., Martínez-Campos L., Gómez J. Evolution of resistance among clinical isolates of Acinetobacter over a 6-year period. Eur. J. Clin. Microbiol. Infect. Dis. 1999;18:292–295. doi: 10.1007/s100960050280. [DOI] [PubMed] [Google Scholar]
- 49.Munoz-Price L.S., Arheart K., Nordmann P., Boulanger A.E., Cleary T., Alvarez R., Pizano L., Namias N., Kett D.H., Poirel L. Eighteen years of experience with Acinetobacter baumannii in a tertiary care hospital. Crit. Care Med. 2013;41:2733–2742. doi: 10.1097/CCM.0b013e318298a541. [DOI] [PubMed] [Google Scholar]
- 50.Tognim M.C., Andrade S.S., Silbert S., Gales A.C., Jones R.N., Sader H.S. Resistance trends of Acinetobacter spp. in Latin America and characterization of international dissemination of multi-drug resistant strains: Five-year report of the SENTRY Antimicrobial Surveillance Program. Int. J. Infect. Dis. 2004;8:284–291. doi: 10.1016/j.ijid.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 51.Perencevich E.N., McGregor J.C., Shardell M., Furuno J.P., Harris A.D., Morris J.G., Jr., Fisman D.N., Johnson J.A. Summer Peaks in the Incidences of Gram-Negative Bacterial Infection Among Hospitalized Patients. Infect. Control Hosp. Epidemiol. 2008;29:1124–1131. doi: 10.1086/592698. [DOI] [PubMed] [Google Scholar]
- 52.Iregbu K.C., Ogunsola F.T., Odugbemi T.O. Infections caused by Acinetobacter species and their susceptibility to 14 antibiotics in Lagos University Teaching Hospital, Lagos. West. Afr. J. Med. 2002;21:226–229. doi: 10.4314/wajm.v21i3.28036. [DOI] [PubMed] [Google Scholar]
- 53.McCracken M., Mataseje L.F., Loo V., Walkty A., Adam H.J., Hoban D.J., Zhanel G.G., Mulvey M.R. Canadian Antimicrobial Resistance Alliance (CARA). Characterization of Acinetobacter baumannii and meropenem-resistant Pseudomonas aeruginosa in Canada: Results of the CANWARD 2007–2009 study. Diagn. Microbiol. Infect. Dis. 2011;69:335–341. doi: 10.1016/j.diagmicrobio.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 54.Biglari S., Hanafiah A., Mohd Puzi S., Ramli R., Rahman M., Lopes B.S. Antimicrobial Resistance Mechanisms and Genetic Diversity of Multidrug-Resistant Acinetobacter baumannii Isolated from a Teaching Hospital in Malaysia. Microb. Drug Resist. 2017;23:545–555. doi: 10.1089/mdr.2016.0130. [DOI] [PubMed] [Google Scholar]
- 55.Al Mobarak M.F., Matbuli R.M., Meir H., Al Gehani N., ElToukhy A.A.M., Al Qureshey K.F., Mutwalli A.H., Abdulaziz A.M., Hadhoud A. Antimicrobial resistance patterns among Acinetobacter baumannii isolated from King Abdulaziz Hospital, Jeddah, Saudi Arabia, Four-Year Surveillance Study (2010–2013) Egypt J. Med. Microbiol. 2014;23:53–60. doi: 10.12816/0025920. [DOI] [Google Scholar]
- 56.Sinha N., Agarwal J., Srivastava S., Singh M. Analysis of carbapenem-resistant Acinetobacter from a tertiary care setting in North India. Indian J. Med. Microbiol. 2013;31:60–63. doi: 10.4103/0255-0857.108724. [DOI] [PubMed] [Google Scholar]
- 57.Matsui M., Suzuki M., Suzuki M., Yatsuyanagi J., Watahiki M., Hiraki Y., Kawano F., Tsutsui A., Shibayama K., Suzuki S. Distribution and Molecular Characterization of Acinetobacter baumannii International Clone II Lineage in Japan. Antimicrob. Agents Chemother. 2018;62:e02190. doi: 10.1128/AAC.02190-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fallah A., Rezaee M.A., Hasani A., Barhaghi M.H.S., Kafil H.S. Frequency of bap and cpaA virulence genes in drug resistant clinical isolates of Acinetobacter baumannii and their role in biofilm formation. Iran. J. Basic Med. Sci. 2017;20:849–855. doi: 10.22038/IJBMS.2017.9105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kumar S., Sen P., Gaind R., Verma P.K., Gupta P., Suri P.R., Nagpal S., Rai A.K. Prospective surveillance of device-associated health care-associated infection in an intensive care unit of a tertiary care hospital in New Delhi, India. Am. J. Infect. Control. 2018;46:202–206. doi: 10.1016/j.ajic.2017.08.037. [DOI] [PubMed] [Google Scholar]
- 60.Ding R., Li X., Zhang X., Zhang Z., Ma X. The Epidemiology of Symptomatic Catheter-associated Urinary Tract Infections in the Intensive Care Unit: A 4-year Single Center Retrospective Study. Urol. J. 2019;16:312–317. doi: 10.22037/uj.v0i0.4256. [DOI] [PubMed] [Google Scholar]
- 61.Cisneros J.M., Reyes M.J., Pachón J., Becerril B., Caballero F.J., García-Garmendía J.L., Ortiz C., Cobacho A.R. Bacteremia due to Acinetobacter baumannii: Epidemiology, clinical findings, and prognostic features. Clin. Infect. Dis. 1996;22:1026–1032. doi: 10.1093/clinids/22.6.1026. [DOI] [PubMed] [Google Scholar]
- 62.Walker J.N., Flores-Mireles A.L., Pinkner C.L., Schreiber H.L., IV, Joens M.S., Park A.M., Potretzke A.M., Bauman T.M., Pinkner J.S., Fitzpatrick J.A.J., et al. Catheterization alters bladder ecology to potentiate Staphylococcus aureus infection of the urinary tract. Proc. Natl. Acad. Sci. USA. 2017;114:E8721–E8730. doi: 10.1073/pnas.1707572114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu W., Flores-Mireles A.L., Cusumano Z.T., Takagi E., Hultgren S.J., Caparon M.G. Host and bacterial proteases influence biofilm formation and virulence in a murine model of enterococcal catheter-associated urinary tract infection. NPJ Biofilms Microbiom. 2017;3:28. doi: 10.1038/s41522-017-0036-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hopkins W.J., Gendron-Fitzpatrick A., Balish E., Uehling D.T. Time course and host responses to Escherichia coli urinary tract infection in genetically distinct mouse strains. Infect. Immun. 1998;66:2798–2802. doi: 10.1128/IAI.66.6.2798-2802.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gaddy J.A., Arivett B.A., McConnell M.J., López-Rojas R., Pachón J., Actis L.A. Role of acinetobactin-mediated iron acquisition functions in the interaction of Acinetobacter baumannii strain ATCC 19606T with human lung epithelial cells, Galleria mellonella caterpillars, and mice. Infect. Immun. 2012;80:1015–1024. doi: 10.1128/IAI.06279-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zarb P., Coignard B., Griskeviciene J., Muller A., Vankerckhoven V., Weist K., Goossens M.M., Vaerenberg S., Hopkins S., Catry B., et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Euro. Surveill. 2012;17:20316. doi: 10.2807/ese.17.46.20316-en. [DOI] [PubMed] [Google Scholar]
- 67.Stickler D.J. Bacterial biofilms in patients with indwelling urinary catheters. Nat. Clin. Pract. Urol. 2008;5:598–608. doi: 10.1038/ncpuro1231. [DOI] [PubMed] [Google Scholar]
- 68.Abdi-Ali A., Hendiani S., Mohammadi P., Gharavi S. Assessment of biofilm formation and resistance to imipenem and ciprofloxacin among clinical isolates of Acinetobacter baumannii in Tehran. Jundishapur J. Microbiol. 2014;7:e8606. doi: 10.5812/jjm.8606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Azizi O., Shahcheraghi F., Salimizand H., Modarresi F., Shakibaie M.R., Mansouri S., Ramazanzadeh R., Badmasti F., Nikbin V. Molecular analysis and expression of bap gene in biofilm-forming multi-drug-resistant Acinetobacter baumannii. Rep. Biochem. Mol. Biol. 2016;5:62–72. [PMC free article] [PubMed] [Google Scholar]
- 70.Thummeepak R., Kongthai P., Leungtongkam U., Sitthisak S. Distribution of virulence genes involved in biofilm formation in multi-drug resistant Acinetobacter baumannii clinical isolates. Int. Microbiol. 2016;19:121–129. doi: 10.2436/20.1501.01.270. [DOI] [PubMed] [Google Scholar]
- 71.Braun G., Vidotto M.C. Evaluation of adherence, hemagglutination, and presence of genes codifying for virulence factors of Acinetobacter baumannii causing urinary tract infection. Mem. Inst Oswaldo Cruz. 2004;99:839–844. doi: 10.1590/S0074-02762004000800010. [DOI] [PubMed] [Google Scholar]
- 72.Pour N.K., Dusane D.H., Dhakephalkar P.K., Zamin F.R., Zinjarde S.S., Chopade B.A. Biofilm formation by Acinetobacter baumannii strains isolated from urinary tract infection and urinary catheters. FEMS Immunol. Med. Microbiol. 2011;62:328–338. doi: 10.1111/j.1574-695X.2011.00818.x. [DOI] [PubMed] [Google Scholar]
- 73.Kuzi S., Blum S.E., Kahane N., Adler A., Hussein O., Segev G., Aroch I. Multi-drug-resistant Acinetobacter calcoaceticus-Acinetobacter baumannii complex infection outbreak in dogs and cats in a veterinary hospital. J. Small Anim. Pract. 2016;57:617–625. doi: 10.1111/jsap.12555. [DOI] [PubMed] [Google Scholar]
- 74.Zordan S., Prenger-Berninghoff E., Weiss R., van der Reijden T., van den Broek P., Baljer G., Dijkshoorn L. Multidrug-resistant Acinetobacter baumannii in veterinary clinics, Germany. Emerg. Infect. Dis. 2011;17:1751–1754. doi: 10.3201/eid1709.101931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Santaniello A., Sansone M., Fioretti A., Menna L.F. Systematic Review and Meta-Analysis of the Occurrence of ESKAPE Bacteria Group in Dogs, and the Related Zoonotic Risk in Animal-Assisted Therapy, and in Animal-Assisted Activity in the Health Context. Int. J. Environ. Res. Public Health. 2020;17:3278. doi: 10.3390/ijerph17093278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abedon S.T., Kuhl S.J., Blasdel B.G., Kutter E.M. Bacteriobacteriophage. 2011 Mar; 1:66–85; Bacteriobacteriophage therapy. Summers WC. Annu. Rev. Microbiol. 2001;55:437–451. [Google Scholar]
- 77.Reardon S. Bacteriophage therapy gets revitalized. Nature. 2014;510:15–16. doi: 10.1038/510015a. [DOI] [PubMed] [Google Scholar]
- 78.Loc-Carrillo C., Abedon S.T. Pros and cons of bacteriophage therapy. Bacteriobacteriophage. 2011;1:111–114. doi: 10.4161/bact.1.2.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Broudy T.B., Fischetti V.A. In vivo lysogenic conversion of Tox(-) Streptococcus pyogenes to Tox(+) with Lysogenic Streptococci or free bacteriophage. Infect. Immun. 2003;71:3782–3786. doi: 10.1128/IAI.71.7.3782-3786.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brüssow H., Kutter E. Bacteriophage Ecology. In: Kutter E., Sulakvelidze A., editors. Bacteriobacteriophages Biology and Applications. 1st ed. CRC Press; Boca Raton, FL, USA: 2005. pp. 129–163. [Google Scholar]
- 81.Hanlon G.W. Bacteriobacteriophages: An appraisal of their role in the treatment of bacterial infections. Int. J. Antimicrob. Agents. 2007;30:118–128. doi: 10.1016/j.ijantimicag.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 82.Gordillo Altamirano F.L., Barr J.J. Bacteriophage Therapy in the Postantibiotic Era. Clin. Microbiol. Rev. 2019;32:e00066. doi: 10.1128/CMR.00066-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Capparelli R., Ventimiglia I., Roperto S., Fenizia D., Iannelli D. Selection of an Escherichia coli O157:H7 bacteriobacteriophage for persistence in the circulatory system of mice infected experimentally. Clin. Microbiol. Infect. 2006;12:248–253. doi: 10.1111/j.1469-0691.2005.01340.x. [DOI] [PubMed] [Google Scholar]
- 84.Watanabe R., Matsumoto T., Sano G., Ishii Y., Tateda K., Sumiyama Y., Uchiyama J., Sakurai S., Matsuzaki S., Imai S., et al. Efficacy of bacteriobacteriophage therapy against gut-derived sepsis caused by Pseudomonas aeruginosa in mice. Antimicrob. Agents Chemother. 2007;51:446–452. doi: 10.1128/AAC.00635-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gu J., Liu X., Li Y., Han W., Lei L., Yang Y., Zhao H., Gao Y., Song J., Lu R., et al. A method for generation bacteriophage cocktail with great therapeutic potential. PLoS ONE. 2012;7:1–8. doi: 10.1371/journal.pone.0031698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yen M., Cairns L.S., Camilli A. A cocktail of three virulent bacteriobacteriophages prevents Vibrio cholerae infection in animal models. Nat. Commun. 2017;8:1–7. doi: 10.1038/ncomms14187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.D’Herelle F. On an invisible microbe antagonistic toward dysenteric bacilli: Brief note by Mr. F. D’Herelle, presented by Mr. Roux. 1917. Res. Microbiol. 2007;158:553–554. doi: 10.1016/j.resmic.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 88.Larkum N.W. Bacteriophagy in urinary infection part I. The incidence of bacteriobacteriophage and of bacillus coli susceptible to dissolution by the bacteriobacteriophage in urines. Presentation of cases of renal infection in which bacteriobacteriophage was used therapeutically. J. Bacteriol. 1925;12:203–223. doi: 10.1128/jb.12.3.203-223.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Larkum N.W. Bacteriophagy in urinary infection part II. Bacteriophagy in the bladder. J. Bacteriol. 1926;12:225–242. doi: 10.1128/JB.12.3.225-242.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schultz I., Neva F.A. Relationship between blood clearance and viruria after intravenous injection of mice and rats with bacteriobacteriophage and polioviruses. J. Immunol. 1965;94:833–841. [PubMed] [Google Scholar]
- 91.Weber-Dabrowska B., Dabrowski M., Slopek S. Studies on bacteriobacteriophage penetration in patients subjected to bacteriophage therapy. Arch. Immunol. Ther. Exp. 1987;35:563–568. [PubMed] [Google Scholar]
- 92.Woźnica W.M., Bigos J., Łobocka M.B. Liza komórek bakteryjnych w procesie uwalniania bakteriofagów—Kanoniczne i nowo poznane mechanizmy [Lysis of bacterial cells in the process of bacteriobacteriophage release--canonical and newly discovered mechanisms] Postepy Hig. Med. Dosw. 2015;69:114–126. (In Polish) [PubMed] [Google Scholar]
- 93.Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am. J. Med. 2002;113:5S–13S. doi: 10.1016/S0002-9343(02)01054-9. [DOI] [PubMed] [Google Scholar]
- 94.Jacobsen S.M., Stickler D.J., Mobley H.L., Shirtliff M.E. Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin. Microbiol. Rev. 2008;21:26–59. doi: 10.1128/CMR.00019-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Carlet J., Collignon P., Goldmann D., Goossens H., Gyssens I.C., Harbarth S., Jarlier V., Levy S.B., N’Doye B., Pittet D., et al. Society’s failure to protect a precious resource: Antibiotics. Lancet. 2011;378:369–371. doi: 10.1016/S0140-6736(11)60401-7. [DOI] [PubMed] [Google Scholar]
- 96.Verbeken G., Huys I., Pirnay J.P., Jennes S., Chanishvili N., Scheres J., Górski A., De Vos D., Ceulemans C. Taking bacteriobacteriophage therapy seriously: A moral argument. Biomed. Res. Int. 2014;2014:621316. doi: 10.1155/2014/621316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ujmajuridze A., Chanishvili N., Goderdzishvili M., Leitner L., Mehnert U., Chkhotua A., Kessler T.M., Sybesma W. Adapted Bacteriobacteriophages for Treating Urinary Tract Infections. Front. Microbiol. 2018;9:1832. doi: 10.3389/fmicb.2018.01832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Furfaro L.L., Payne M.S., Chang B.J. Bacteriobacteriophage Therapy: Clinical Trials and Regulatory Hurdles. Front. Cell Infect. Microbiol. 2018;8:376. doi: 10.3389/fcimb.2018.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Abdelkader K., Gerstmans H., Saafan A., Dishisha T., Briers Y. The Preclinical and Clinical Progress of Bacteriobacteriophages and Their Lytic Enzymes: The Parts are Easier than the Whole. Viruses. 2019;11:96. doi: 10.3390/v11020096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zalewska-Piątek B., Piątek R. Bacteriophage Therapy as a Novel Strategy in the Treatment of Urinary Tract Infections Caused by E. coli. Antibiotics. 2020;9:304. doi: 10.3390/antibiotics9060304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Oechslin F. Resistance Development to Bacteriobacteriophages Occurring during Bacteriobacteriophage Therapy. Viruses. 2018;10:351. doi: 10.3390/v10070351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hyman P. Bacteriophages for Bacteriophage Therapy: Isolation, Characterization, and Host Range Breadth. Pharmaceuticals. 2019;12:35. doi: 10.3390/ph12010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Batinovic S., Wassef F., Knowler S.A., Rice D., Stanton C.R., Rose J., Tucci J., Nittami T., Vinh A., Drummond G.R., et al. Bacteriobacteriophages in Natural and Artificial Environments. Pathogens. 2019;8:100. doi: 10.3390/pathogens8030100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nilsson A.S. Pharmacological limitations of bacteriophage therapy. Ups. J. Med. Sci. 2019;124:218–227. doi: 10.1080/03009734.2019.1688433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schmerer M., Molineux I.J., Bull J.J. Synergy as a rationale for bacteriophage therapy using bacteriophage cocktails. Peer J. 2014;2:e590. doi: 10.7717/peerj.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nishikawa H., Yasuda M., Uchiyama J., Rashel M., Maeda Y., Takemura I., Sugihara S., Ujihara T., Shimizu Y., Shuin T., et al. T-even-related bacteriobacteriophages as candidates for treatment of Escherichia coli UTIs. Arch. Virol. 2008;153:507–515. doi: 10.1007/s00705-007-0031-4. [DOI] [PubMed] [Google Scholar]
- 107.Tóthová L., Celec P., Bábíčková J., Gajdošová J., Al-Alami H., Kamodyova N., Drahovská H., Liptáková A., Turňa J., Hodosy J. Bacteriophage therapy of Cronobacter-induced urinary tract infection in mice. Med. Sci. Monit. 2011;17:BR173–BR178. doi: 10.12659/MSM.881844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sybesma W., Zbinden R., Chanishvili N., Kutateladze M., Chkhotua A., Ujmajuridze A., Mehnert U., Kessler T.M. Bacteriobacteriophages as Potential Treatment for Urinary Tract Infections. Front. Microbiol. 2016;7:465. doi: 10.3389/fmicb.2016.00465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Soto S.M. Importance of Biofilms in Urinary Tract Infections: New Therapeutic Approaches. Adv. Biol. 2014;13:543974. doi: 10.1155/2014/543974. [DOI] [Google Scholar]
- 110.Djeribi R., Bouchloukh W., Jouenne T., Menaa B. Characterization of bacterial biofilms formed on urinary catheters. Am. J. Infect. Control. 2012;40:854–859. doi: 10.1016/j.ajic.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 111.Vukotic G., Obradovic M., Novovic K., Di Luca M., Jovcic B., Fira D., Neve H., Kojic M., McAuliffe O. Characterization, Antibiofilm, and Depolymerizing Activity of Two Bacteriophages Active on Carbapenem-Resistant Acinetobacter baumannii. Front. Med. 2020;7:426. doi: 10.3389/fmed.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Grygorcewicz B., Wojciuk B., Roszak M., Łubowska N., Błażejczak P., Jursa-Kulesza J., Rakoczy R., Masiuk H., Dołęgowska B. Environmental Bacteriophage-Based Cocktail and Antibiotic Combination Effects on Acinetobacter baumannii Biofilm in a Human Urine Model. Microb. Drug Resist. 2021;27:25–35. doi: 10.1089/mdr.2020.0083. [DOI] [PubMed] [Google Scholar]
- 113.Cieślik M., Bagińska N., Górski A., Jończyk-Matysiak E. Animal Models in the Evaluation of the Effectiveness of Bacteriophage Therapy for Infections Caused by Gram-Negative Bacteria from the ESKAPE Group and the Reliability of Its Use in Humans. Microorganisms. 2021;9:206. doi: 10.3390/microorganisms9020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.De Miguel T., Rama J., Sieiro C., Sánchez S., Villa T.G. Bacteriobacteriophages and Lysins as Possible Alternatives to Treat Antibiotic-Resistant Urinary Tract Infections. Antibiotics. 2020;9:466. doi: 10.3390/antibiotics9080466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lood R., Winer B.Y., Pelzek A.J., Diez-Martinez R., Thandar M., Euler C.W., Schuch R., Fischetti V.A. Novel bacteriophage lysin capable of killing the multidrug-resistant gram-negative bacterium Acinetobacter baumannii in a mouse bacteremia model. Antimicrob. Agents Chemother. 2015;59:1983–1991. doi: 10.1128/AAC.04641-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Leitner L., Ujmajuridze A., Chanishvili N., Goderdzishvili M., Chkonia I., Rigvava S., Chkhotua A., Changashvili G., McCallin S., Schneider M.P., et al. Intravesical bacteriobacteriophages for treating UTIs in patients undergoing transurethral resection of the prostate: A randomised, placebo-controlled, double-blind clinical trial. Lancet Infect. Dis. 2020;16:S1473. doi: 10.1016/S1473-309930330-3. [DOI] [PubMed] [Google Scholar]
- 117.Goodridge L.D. Designing bacteriophage therapeutics. Curr. Pharm. Biotechnol. 2010;11:15–27. doi: 10.2174/138920110790725348. [DOI] [PubMed] [Google Scholar]
- 118.Azeredo J., Sutherland I.W. The use of bacteriophages for the removal of infectious biofilms. Curr. Pharm. Biotechnol. 2008;9:261–266. doi: 10.2174/138920108785161604. [DOI] [PubMed] [Google Scholar]
- 119.Górski A., Międzybrodzki R., Borysowski J., Dabrowska K., Wierzbicki P., Ohams M., Korczak-Kowalska G., Olszowska-Zaremba N., Lusiak-Szelachowska M., Klak M., et al. Bacteriophage as a modulator of immune responses: Practical implications for bacteriophage therapy. Adv. Virus Res. 2012;83:41–71. doi: 10.1016/B978-0-12-394438-2.00002-5. [DOI] [PubMed] [Google Scholar]
- 120.Rostkowska O.M., Międzybrodzki R., Miszewska-Szyszkowska D., Górski A., Durlik M. Treatment of recurrent urinary tract infections in a 60-year-old kidney transplant recipient. The use of bacteriophage therapy. Transpl. Infect. Dis. 2020;29:e13391. doi: 10.1111/tid.13391. [DOI] [PubMed] [Google Scholar]
- 121.World Health Organization (WHO) [(accessed on 14 January 2021)];2018 Available online: http://www.who.int/mediacentre/news/releases/2017/bacteria-antibiotics-needed/en.
- 122.Coelho J., Woodford N., Turton J., Livermore D.M. Multiresistant Acinetobacter in the UK: How big a threat? J. Hosp. Infect. 2004;58:167–169. doi: 10.1016/j.jhin.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 123.Gupta K. Emerging antibiotic resistance in urinary tract pathogens. Infect. Dis Clin. N. Am. 2003;17:243–259. doi: 10.1016/S0891-5520(03)00006-0. [DOI] [PubMed] [Google Scholar]
- 124.World Health Organization (WHO) [(accessed on 14 January 2021)];2014 Available online: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf.
- 125.Cai T., Nesi G., Mazzoli S., Meacci F., Lanzafame P., Caciagli P., Mereu L., Tateo S., Malossini G., Selli C., et al. Asymptomatic bacteriuria treatment is associated with a higher prevalence of antibiotic resistant strains in women with urinary tract infections. Clin. Infect. Dis. 2015;61:1655–1661. doi: 10.1093/cid/civ696. [DOI] [PubMed] [Google Scholar]
- 126.Wagenlehner F.M., Naber K.G. Editorial commentary: Treatment of asymptomatic bacteriuria might be harmful. Clin. Infect. Dis. 2015;61:1662–1663. doi: 10.1093/cid/civ698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Jasim H.N., Hafidh R.R., Abdulamir A.S. Formation of therapeutic bacteriophage cocktail and endolysin to highly multi-drug resistant Acinetobacter baumannii: In vitro and in vivo study. Iran. J. Basic Med. Sci. 2018;21:1100–1108. doi: 10.22038/IJBMS.2018.27307.6665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Malik S., Sidhu P.K., Rana J.S., Nehra K. Managing urinary tract infections through bacteriophage therapy: A novel approach. Folia Microbiol. 2020;65:217–231. doi: 10.1007/s12223-019-00750-y. [DOI] [PubMed] [Google Scholar]