Abstract
Most cystic fibrosis (CF) patients referred for lung transplantation are chronically infected with Gram-negative opportunistic pathogens. It is well known that chronic infections in CF patients have a significant impact on lung-function decline and survival before transplantation. The rate and timing of re-colonization after transplantation have been described, but the impact on survival after stratification of bacteria is not well elucidated. We did a single-center retrospective analysis of 99 consecutive CF patients who underwent lung transplantation since the beginning of the Copenhagen Lung Transplant program in 1992 until October 2014. Two patients were excluded due to re-transplantation. From the time of CF diagnosis, patients had monthly sputum cultures. After transplantation, CF-patients had bronchoscopy with bronchoalveolar lavage at 2, 4, 6 and 12 weeks and 6, 12, 18 and 24 months after transplantation, as well as sputum samples if relevant. Selected culture results prior to and after transplantation were stored. We focused on colonization with the most frequent bacteria: Pseudomonas aeruginosa (PA), Stenotrophomonas maltophilia (SM), Achromobacter xylosoxidans (AX) and Burkholderia cepacia complex (BCC). Pulsed-field gel electrophoresis (PFGE) was used to identify clonality of bacterial isolates obtained before and after lung transplantation. Time to re-colonization was defined as the time from transplantation to the first positive culture with the same species. Seventy-three out of 97 (75%) had sufficient culture data for analyses with a median of 7 (1–91) cultures available before and after transplantation. Median colonization-free survival time was 23 days until the first positive culture after transplantation. After 2 years, 59 patients (81%) were re-colonized, 33 (48.5%) with PA, 7 (10.3%) with SM, 12 (17.6%) with AX, and 7 (10.3%) with BCC. No difference in survival was observed between the patients colonized within the first 2 years and those not colonized. Re-colonization of bacteria in the lower airways occurred at a median of 23 days after transplantation in our cohort. In our patient cohort, survival was not influenced by re-colonization or bacterial species.
Keywords: cystic fibrosis, lung transplantation, colonization
1. Introduction
Lung transplantation is a well-established treatment for selected patients with end-stage cystic fibrosis (CF). CF is the most common indication for transplantation among younger recipients [1]. A major challenge when transplanting CF patients is the presence of microbial pathogens at the time of transplant, increasing the risk for infectious complications in the early post-operative period as well as later recurrence in the transplanted lung in part due to immunosuppressants [2,3,4,5]. This has been shown for specific pathogens like Burkholderia cepacia complex (BCC) [6], which is a risk factor for developing pneumonia [7] and death in the early post-transplant period where immunosuppression is at maximum [8,9,10].
Chronic airway infection with pan-resistant Pseudomonas aeruginosa [10], non-epidemic Burkholderia cenocepacia, Burkholderia gladioli [11] and Mycobacterium abscessus prior to transplantation leads to a higher risk of re-colonization and a suggested increased risk of morbidity and mortality [8,12].
The primary cause of morbidity and mortality after lung transplantation is chronic lung allograft dysfunction (CLAD), affecting up to 50% of all patients after 5 years [13,14]. The rate of colonization and its association with CLAD and best-achieved pulmonary functions (FEV1, FVC and diffusion capacity) after transplantation is not well elucidated [15]. However, a link has been shown in a previous single-center study, which found that colonization after transplantation was independently associated with increased risk of CLAD [16]. The use of pulsed-field gel electrophoresis (PFGE) to investigate the relatedness of the bacteria found before and after lung transplantation has not previously been done.
The aim of this study was
-
(1)
to investigate the rate of re-colonization stratified by type of bacteria;
-
(2)
to demonstrate whether bacteria were genetically identical before and after lung transplantation by the use of PFGE;
-
(3)
to investigate the impact of infection on CLAD, pulmonary function and survival.
2. Materials and Methods
We did a single-center retrospective study of all double lung transplanted CF-patients in Denmark since the beginning of the lung transplant program in 1992 until October 2014. All Danish lung transplantations are centralized at Rigshospitalet, Copenhagen, Denmark.
The analysis focused on the most frequently cultured bacteria Pseudomonas aeruginosa [17,18] (PA), Stenotrophomonas maltophilia (SM), Achromobacter xylosoxidans (AX) and Burkholderia cepacia complex (BCC). All CF patients were followed before and after lung transplantation, at one of the two Danish Cystic Fibrosis Centers and at the national lung transplant center, and all clinical and microbiological cultures were collected from the CF-database and from the microbiology data system (MADS) at Department of Clinical Microbiology at Rigshospitalet.
2.1. Pharmacological Treatment after Lung Transplantation
All recipients received induction therapy with either ATG or Daclizumab at transplantation. Lifelong maintenance immunosuppression therapy was a combination of Cyclosporine, Azathioprine and steroid.
All patients received some combination of systemic antimicrobial treatment with at least two drugs for the first couple of weeks after the transplant procedure. This was combined with antifungal and antiviral prophylaxis, which was administered during the first 12 weeks.
2.2. Bronchoscopy
The lung transplant surveillance program includes bronchoscopy with bronchoalveolar lavage (BAL) sampling at 2, 4, 6 and 12 weeks and at 6, 12, 18 and 24 months after transplantation as well as additional bronchoscopy if clinically relevant, e.g., in the case of acute unexplained drop in lung function.
BAL was performed with three aliquots of 50 mL with the bronchoscope wedged into the middle lobe or lingula. Samples were stored at room temperature before shipment to the department of clinical microbiology within six hours.
2.3. Microbiology
In the transplanted CF population, BAL fluid is routinely cultured for CF-bacteria and fungi at all time points. All BAL fluids and airway secretions were Gram-stained to ensure the origin from the lower airways and cultured on selective media in the clinical microbiological laboratory. These media included a Sabouraud plate, a 7% NaCl plate, a B. cepacia plate containing colistin and gentamicin and a “blueplate” (modified Conradi Drigalski’s medium) selective for Gram-negative rods and non-selective media including 5% Danish blood agar and chocolate agar (Statens Serum Institute, Copenhagen, Denmark). Before 2011, isolated bacteria were identified using biochemical profiling based on API 20NE (bioMérieux), and from 2011, MALDI-TOF MS (Bruker Daltronics, Bremen Germany) was used [19].
Date of colonization after transplantation was defined as the first positive BAL culture, out of at least two positive BAL cultures including the same micro-organism, respectively. Re-colonization was defined as colonization after lung transplantation with the same type of bacteria as before transplantation.
2.4. Bacteria Isolates
Since the beginning of the nineties, P. aeruginosa, and later on S. maltophilia, A. xylosoxidans, B. cepacia complex and P. apista isolates from sputum were collected and stored (−80 °C) 20 annually.
2.5. Pulsed-Field-Gel-Electrophoresis (PFGE)
PFGE was used for the identification of clonality of bacterial isolates obtained before and after lung transplantation. We used Spe I as a restriction enzyme for all typed isolates (P. aeruginosa, S. maltophilia, A. xylosoxidans, B. cepacia complex and P. apista) according to methods described previously [19,20,21]. PFGE patterns were compared visually and evaluated using the criteria previously described [21,22]. Isolates with differences in zero, one or two bands were considered identical; other isolates were considered unrelated.
2.6. Lung Function Tests
The patient’s lung function was closely monitored with per-protocol spirometry at least every third month at the lung transplantation clinic as well as body box plethysmography at 3, 6, and 12 months and yearly after the transplantation. If the patient experienced a decline in absolute FEV1, new pulmonary tests were made. The static lung volumes were measured using spirometry lung-function tests calculating the expiratory flow rates, and using body box plethysmography, dynamic and static lung volumes were measured.
2.7. Chronic Lung Allograft Dysfunction
Baseline FEV1 and forced vital capacity (FVC) post-transplant were defined as the average of the 2 best lung-function tests at least three weeks apart according to the standard criteria for International Society for Heart and Lung Transplantation (ISHLT) [23]. Baseline diffusion capacity for carbon monoxide (DLCO), residual volume (RV) and total lung capacity (TLC) was defined as the measured value at the same time or first after the baseline values for FEV1 and FVC, if patients did not reach the threshold for CLAD. CLAD was defined as a persistent decrease in FEV1 < 80% of baseline value with or without an associated decrease in TLC < 90% of baseline value, also conditional on 3 months survival according to standard ISHLT criteria.
Survival was calculated as the time of transplantation to the time of death or by censoring the patients when data were updated in October 2014.
2.8. Statistics
Statistical analysis was performed using IBM SPSS Statistics (version 22.0) software. Kaplan–Meier plots with Log-Rank tests were employed to demonstrate survival and CLAD-free survival, while stratifying for types of microbes. Continuous variables were described as mean ± standard deviation (±SD) and compared using ANOVA. A p-value ≤ 0.05 was considered statistically significant.
3. Results
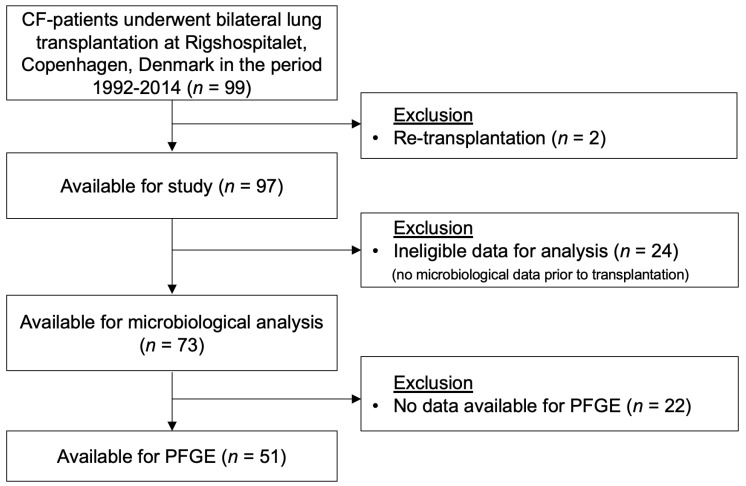
During the period from 1992 to 2014, 99 CF patients underwent bilateral lung transplantation at Rigshospitalet, Copenhagen, Denmark. As described in flowchart 1, two of the patients were excluded from the follow-up study due to re-transplantation. In total, 73 out of 97 patients (75%) had sufficient data for inclusion in the study. See Figure 1 for patient inclusion and exclusion. If there were no bacterial isolates prior to transplantation or frozen cultures available for PFGE, patients were excluded for these analyses; see Table 1 for demography.
Figure 1.
This diagram shows how patients were included and excluded in this study.
Table 1.
Demography of the patients including lung function at baseline and at chronic lung allograft dysfunction (CLAD). Variables are presented as median and standard deviation.
| Burkholderia (n = 7) | Pseudomonas (n = 39) | Stenotrophamonas (n = 7) | Achromobachter (n = 12) | Non-Recolonization (n = 8) | p-Value | |
|---|---|---|---|---|---|---|
| Gender female (%) | 6/7 | 21/39 | 2/7 | 4/12 | 3/8 | 0.702 |
| Age at transplantation (years) | 28.7 (±7.8) | 31.2 (±7.4) | 39.1 (±10.7) | 27.3 (±9.9) | 22.3 (±9.2) | 0.162 |
| Donor Pulse (BPM) | 112 (±30.1) | 99.5 (±28.0) | 100 (±17.2) | 90 (±49.7) | 99.5 (±12.7) | 0.997 |
| Donor Systolic BP (mmHg) | 122 (±15.9) | 114 (±25.5) | 109 (±17.7) | 111 (±26.7) | 121 (±12.9) | 0.941 |
| Donor Diastolic BP (mmHg) | 71.5 (±18.8) | 65 (±16.3) | 71 (±15.8) | 62.5 (±14.0) | 81.5 (±13.9) | 0.575 |
| Donor Weight (Kg) | 65.0 (±7.4) | 65 (±12.5) | 67.5 (±18.9) | 76.5 (±12.5) | 69.0 (±8.12) | 0.542 |
| Donor Height (m) | 1.67 (±0.11) | 1.71 (±0.07) | 1.78 (±0.11) | 1.70 (±0.10) | 1.70 (±0.11) | 0.228 |
| Donor age (years) | 43.0 (±9.5) | 43.0 (±12.5) | 37.0 (±16.8) | 42.0 (±15.7) | 41.0 (±18.2) | 0.832 |
| Baseline FVC (L) | 3.23 (±0.81) | 3.40 (±0.67) | 4.08 (±1.34) | 3.74 (±1.38) | 3.9 (±0.95) | 0.215 |
| Baseline FEV1 (L) | 2.56 (±0.56) | 2.62 (±0.66) | 3.70 (±1.11) | 3.05 (±1.0) | 2.98 (±0.9) | 0.179 |
| Baseline RV (L) | 1.7 (±0.20) | 1.95 (±0.74) | 2.28 (±0.50) | 1.82 (±0.55) | 1.56 (±0.85) | 0.441 |
| Baseline TLC (L) | 5.1 (±0.84) | 5.42 (±1.43) | 6.35 (±1.72) | 4.86 (±1.97) | 5.49 1.80 | 0.364 |
| Baseline DLCO | 6.1 (±0.78) | 5.95 (±1.58) | 6.6 (±2.3) | 5.38 (±1.54) | 5.52 (±2.1) | 0.701 |
| Baseline DLCO alveolar | 1.1 (±0.23) | 1.26 (±0.20) | 1.16 (±0.16) | 1.12 (±0.21) | 1.11 (±0.29) | 0.640 |
3.1. Re-Colonization
The re-colonization after transplantation stratified by type of bacteria present in BAL fluid was investigated. We found that P. aeruginosa (n = 39), S. malthophilia (n = 7), A. xylosoxidans (n = 12) and B. cepacia complex (n = 7) were the most frequently cultured bacteria. Eight patients did not experience re-colonization during the study period. There was no significant difference in outcome between the patients stratified by re-colonization when comparing age at transplantation.
The median time passed to re-colonization after transplantation in all patients was 23 days. The colonization-free survival after transplantation stratified by bacteria is depicted in Figure 2. No difference in the rate of re-colonization was observed between all types of microbes using Log-Rank test (Mantel-Cox) (p = 0.46).
Figure 2.
Kaplan–Meyer plot showing time from transplantation to re-colonization.
3.2. Pulsed-Field Gel Electrophoresis
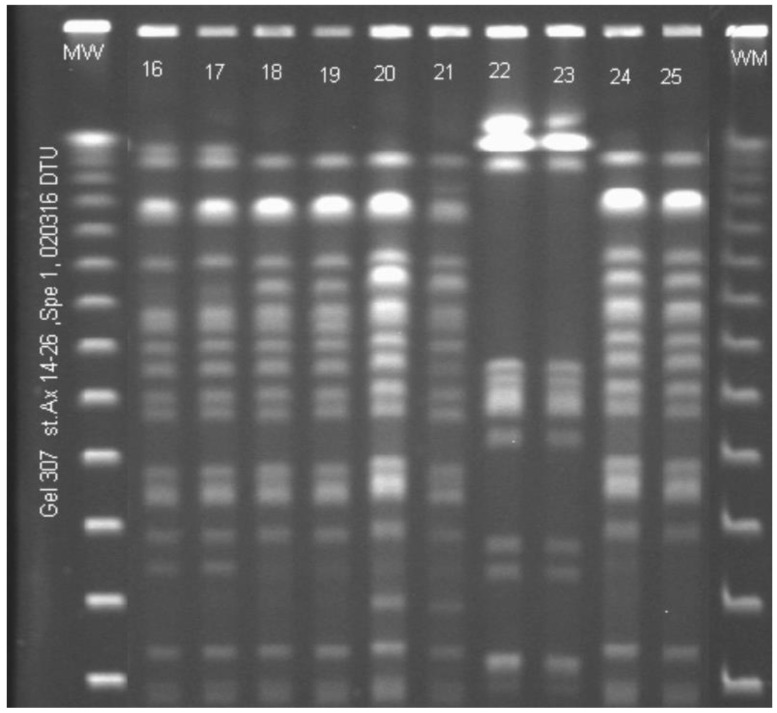
Out of 73 lung transplantation recipients, 51 patients had pre-transplant isolates available for PFGE and were colonized with the same bacteria after transplantation. These bacteria were distributed on the following pathogens: 38 patients colonized with P. aeruginosa, two with S. maltophilia, five with A. xylosoxidans (Figure 3), five with B. cepacia complex and one with P. apista.
Figure 3.
Pulsed-field-gel-electrophoresis pattern of 10 paired Achromobacter xylosoxidans isolates from bronchoalveolar lavage (BAL) fluid from five cystic fibrosis (CF) patients before and after lung transplantation (ltx). The Spe restriction enzyme was used. MW: molecular-weight standard. Lane 16 and 17: CF334 ML, before (lane16) and after ltx (lane 17). Lane 18 and 19: CF340 JP, before (lane 18) and after ltx (lane 19). Lane 20 and 21: CF353 ST, before (lane 20) and after ltx (lane 21). Lane 22 and 23: CF172 TN, before (lane 22) and after ltx (lane 23). Lane 24 and 25: CF347 HM, before (lane 24) and after ltx (lane 25).
We examined the PFGE pattern among these pre- and post-transplant isolates and found that twenty-four out of the 38 patients (63%) who had chronic P. aeruginosa infection had an identical PFGE pattern pre- and post-lung-transplantation. All bacterial isolates from patients with chronic S. maltophilia, A. xylosoxidans, B. cepacia complex and P. apista had the same PFGE pattern before and after lung transplantation.
The median time between isolates collected pre- and post-lung-transplantation was 2 years (range 1–16 years) in P. aeruginosa infected patients with bacteria having the same PFGE pattern compared to 3 years (range 1–12 years) in patients with different PFGE pattern.
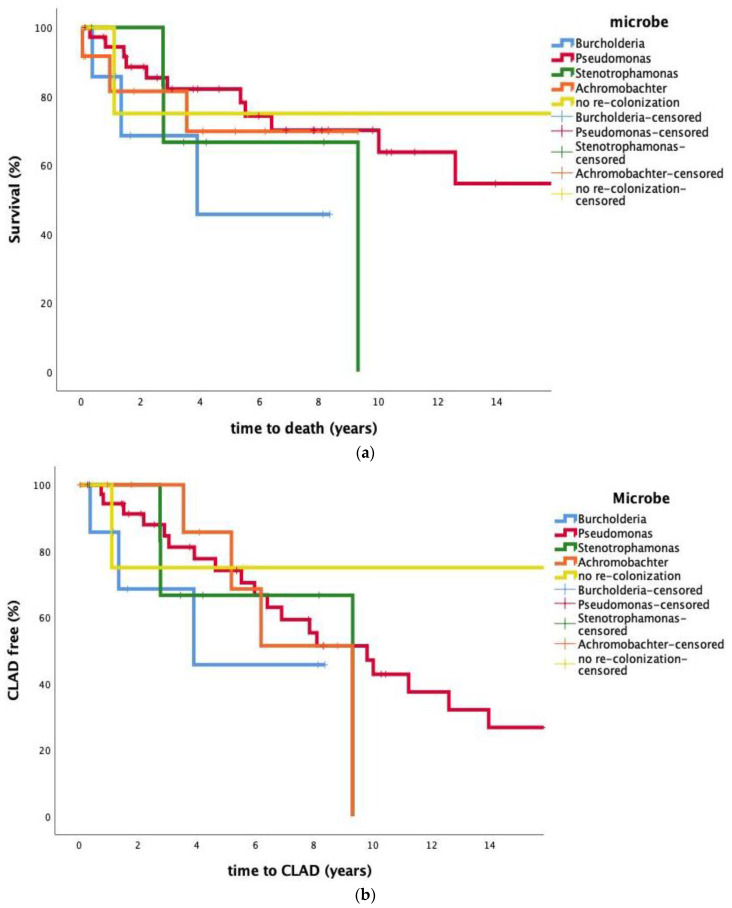
3.3. Impact of Colonization on Mortality
The impact of re-colonization on survival was analyzed, stratifying for bacterial species colonization of the patients. Median survival times were 13.7 years for P. aeruginosa, 7.1 years for S. maltophilia, 7.0 years for A. xylosoxidans and 5.0 years for B. cepacia complex. Kaplan–Meier plots are shown in Figure 4a. No statistically significant difference in survival was observed within the four bacterial subgroups of colonized patients; however, a statistically significant difference was present when comparing non-colonized patients to B. cepacia complex Log-Rank (p = 0.029), P. aeruginosa Log-Rank (p < 0.001) and A. xylosoxidans Log-Rank (p = 0.007) but not when comparing the non-colonized to S. maltophilia Log-Rank (p = 0.106).
Figure 4.
(a,b) demonstrate the time CLAD and death after transplantation stratified for different bacteria.
3.4. Impact of Colonization on CLAD
The impact of re-colonization on CLAD-free survival was investigated and stratified by bacteria. We found an estimated median CLAD free survival time of 10.0 years for P. aeruginosa, 7.1 years for S. maltophilia and 7.2 years for A. xylosoxidans. Two out of six patients who were re-colonized with B. cepacia complex encountered CLAD. A Kaplan–Meier plot showing CLAD-free survival is depicted in Figure 4b. No statistically significant difference in CLAD free survival was observed when comparing the four colonized groups’ Log-Rank (Mantel-Cox) (p = 0.752). Estimation was limited to the largest follow-up time if it was censored.
4. Discussion
Re-colonization of the lower airways after lung transplantation in CF patients is a well-known problem, and it is a major contributor to increased hospitalizations and the use of antibiotics [7]. The finding that the time to re-colonization was only 23 days post-transplantation corroborates findings from the early days of lung transplantation, where P. aeruginosa was found merely 15 days post-transplantation in a CF population 18.
The rate of colonization and its impact on survival in patients infected with, P. aeruginosa, S. maltophilia [24] A. xylosoxidans [25] and B. cepacia complex [25,26] has been described earlier, but its influence on post-transplant outcomes such as survival free of CLAD and impact on absolute values of baseline pulmonary function is not well described. One study found de novo and persistent colonization with P. aeruginosa to correlate with development of CLAD [27] compared to non-colonization.
Using Log Rank-test (Mantel-Cox), we found no difference in the rate of re-colonization between the different bacteria. The early re-colonization is likely due to aspiration from the upper airways, and it has previously been shown that most CF patients chronically infected with P. aeruginosa have the clone type in the upper and lower airways because of bi-directional communication [28,29].
The use of PFGE typing to investigate the relatedness of the bacteria found before and after lung transplantation has not previously been done. With our analysis, we found that all patients infected with S. maltophilia, A. xylosoxidans, B. cepacia complex and P. apista had the same PFGE pattern before and after lung transplantation. However, only 63% of the patients chronically infected with P. aeruginosa had the same PFGE pattern as before transplantation.
When looking at the impact of re-colonization on CLAD and mortality, we found no significant difference in CLAD-free survival when stratified for bacteria, and indeed some patients with early-onset CLAD were not re-colonized.
When we looked at re-colonization and its impact on survival stratifying for colonization status of the patients, we found no significant difference in survival within the four subgroups of colonized patients; however, a statistically significant difference was present when comparing non-colonized patients to B. cepacia complex, P. aeruginosa and A. xylosoxidans. This result could be caused by non-colonized patients that die before a potential re-colonization is detected. Our results are consistent with the results by Srour N et al. [30], who investigated pre-transplantation colonization of the lower airways with transmissible strains of P. aeruginosa in CF patients and its impact on morbidity and mortality post-transplantation. The study found that pre-transplant colonization was not associated with CLAD-free survival, frequency of acute rejection, frequency of post-transplant respiratory infection or post-transplant decline in FEV1.
The results of our study suggest that re-colonization after lung-transplantation in CF patients has no impact on the patient’s post-transplant morbidity and mortality. As nearly all patients were re-colonized early, it was not possible to determine the effect of recolonization per se.
Limitations
A major limitation is the retrospective study design and small number of patients and available data, thus yielding low statistical power. This is because of a limited number of CF patients in Denmark and a similarly limited need for transplantation. Because of the long inclusion period of 22 years, changes in the choice of therapy and patient care could have biased our findings, specifically when comparing newer patients with historical groups. Donor organ quality in the entire era has been investigated and published previously [31,32].
We used PFGE as a way of assessing the epidemiological relationship between most common bacterial infections. Even though PFGE is a gold standard method, it has its limitations. The method cannot detect every genetic change; however, it is estimated that the average bacterial PGFE pattern represents more than 90% of the total genome [33].
5. Conclusions
In conclusion, we demonstrated that re-colonization of CF patients with the same bacterial strain is very common and happens early after transplantation, with a median time of 23 days. The rate of re-colonization with B. cepacia complex, P. aeruginosa, S. maltophilia and A. xylosoxidans was similar, and it did not seem to impact survival or CLAD-free survival, although numbers were small. The absolute values of pulmonary function both at baseline and at CLAD were not influenced by colonization. As this was a single-center study, with only a few patients included, our results should be investigated in future and larger clinical prospective studies. However, the results from this single-center study has resulted in a change in the post-transplant procedure for CF patients at our institution. The rate of re-colonization was earlier than expected, and even though the study found no impact on survival, other studies have found a higher risk for infectious complications in the early post-operative period as well as later recurrence in the transplanted lung, in part due to immunosuppressants [2,3,4,5]. The new standard practice includes a functional endoscopic sinus surgery 2–3 weeks after transplantation under wide antibiotic cover.
Acknowledgments
We thank Ulla Rydahl Johansen for excellent technical assistance.
Author Contributions
Conceptualization, A.E.H., H.H.L.S. and M.I.; Data curation, A.E.H. and H.H.L.S.; Formal analysis, A.E.H., H.H.L.S. and H.K.J.; Funding acquisition, H.H.L.S. and M.I.; Investigation, A.E.H. and H.H.L.S.; Methodology, A.E.H., H.H.L.S., H.K.J., T.P., T.K.L., M.I. and M.P.; Project administration, H.H.L.S.; Software, H.H.L.S. and H.K.J.; Validation, A.E.H.; Writing—original draft, A.E.H. and H.H.L.S.; Writing—review and editing, A.E.H., H.H.L.S., H.K.J., T.P., T.K.L., M.I. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
HKJ was funded by a clinical research stipend from The Novo Nordisk Foundation (NNF12OC1015920) and Rigshospitalet Rammebevilling 2015-17 and Lundbeckfonden Grant R167-2013-15229.
Institutional Review Board Statement
The local ethics committee at the Capital Region of Denmark Region Hovedstaden approved the use of the stored bacterial isolates: registration number H-4-2015-FSP.
Informed Consent Statement
Patient consent was waived due to this study being a historical cohort study, and the dansih legislation does not require an informed consent.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Orens J.B., Estenne M., Arcasoy S., Conte J.V., Corris P., Egan J.J., Egan T., Keshavjee S., Knoop C., Kotloff R., et al. International guidelines for the selection of lung transplant candidates: 2006 update—A consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2006;25:745–755. doi: 10.1016/j.healun.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Bonvillain R.W., Valentine V.G., Lombard G., LaPlace S., Dhillon G., Wang G. Post-operative infections in cystic fibrosis and non-cystic fibrosis patients after lung transplantation. J. Heart Lung Transplant. 2007;26:890–897. doi: 10.1016/j.healun.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Meachery G., De Soyza A., Nicholson A., Parry G., Hasan A., Tocewicz K., Pillay T., Clark S., Lordan J.L., Schueler S., et al. Outcomes of lung transplantation for cystic fibrosis in a large UK cohort. Thorax. 2008;63:725–731. doi: 10.1136/thx.2007.092056. [DOI] [PubMed] [Google Scholar]
- 4.Kanj S.S., Tapson V., Davis R.D., Madden J., Browning I. Infections in patients with cystic fibrosis following lung transplantation. Chest. 1997;112:924–930. doi: 10.1378/chest.112.4.924. [DOI] [PubMed] [Google Scholar]
- 5.Lobo L.J., Noone P.G. Respiratory infections in patients with cystic fibrosis undergoing lung transplantation. Lancet Respir. Med. 2014;2:73–82. doi: 10.1016/S2213-2600(13)70162-0. [DOI] [PubMed] [Google Scholar]
- 6.de Souza Carraro D., Carraro R.M., Campos S.V., Iuamoto L.R., Braga K.A.D.O., Oliveira L.C.D., Sabino E.C., Rossi F., Pêgo-Fernandes P.M. Burkholderia cepacia, cystic fibrosis and outcomes following lung transplantation: Experiences from a single center in Brazil. Clinics. 2018;73:e166. doi: 10.6061/clinics/2018/e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung M.-K., Rachakonda L., Weill D., Hwang P.H. Effects of sinus surgery on lung transplantation outcomes in cystic fibrosis. Am. J. Rhinol. 2008;22:192–196. doi: 10.2500/ajr.2008.22.3146. [DOI] [PubMed] [Google Scholar]
- 8.Alexander B.D., Petzold E.W., Reller L.B., Palmer S.M., Davis R.D., Woods C.W., Lipuma J.J. Survival after Lung Transplantation of Cystic Fibrosis Patients Infected with Burkholderia cepacia Complex. Am. J. Transplant. 2008;8:1025–1030. doi: 10.1111/j.1600-6143.2008.02186.x. [DOI] [PubMed] [Google Scholar]
- 9.De Soyza A., Meachery G., Hester K.L., Nicholson A., Parry G., Tocewicz K., Pillay T., Clark S., Lordan J.L., Schueler S., et al. Lung transplantation for patients with cystic fibrosis and Burkholderia cepacia complex infection: A single-center experience. J. Heart Lung Transplant. 2010;29:1395–1404. doi: 10.1016/j.healun.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Hadjiliadis D., Steele M.P., Chaparro C., Singer L.G., Waddell T.K., Hutcheon M.A., Davis R.D., Tullis D.E., Palmer S.M., Keshavjee S. Survival of lung transplant patients with cystic fibrosis harboring panresistant bacteria other than Burkholderia cepacia, compared with patients harboring sensitive bacteria. J. Heart Lung Transplant. 2007;26:834–838. doi: 10.1016/j.healun.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Murray S., Charbeneau J., Marshall B.C., LiPuma J.J. Impact of Burkholderia Infection on Lung Transplantation in Cystic Fibrosis. Am. J. Respir. Crit. Care Med. 2008;178:363–371. doi: 10.1164/rccm.200712-1834OC. [DOI] [PubMed] [Google Scholar]
- 12.Snell G., Reed A., Stern M., Hadjiliadis D. The evolution of lung transplantation for cystic fibrosis: A 2017 update. J. Cyst. Fibros. 2017;16:553–564. doi: 10.1016/j.jcf.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Knoop C., Estenne M. Chronic Allograft Dysfunction. Clin. Chest Med. 2011;32:311–326. doi: 10.1016/j.ccm.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sato M. Chronic lung allograft dysfunction after lung transplantation: The moving target. Gen. Thorac. Cardiovasc. Surg. 2013;61:67–78. doi: 10.1007/s11748-012-0167-3. [DOI] [PubMed] [Google Scholar]
- 15.Christie J.D., Edwards L.B., Kucheryavaya A.Y., Aurora P., Christie J.D., Kirk R., Dobbels F., Rahmel A.O., Hertz M. The Registry of the International Society for Heart and Lung Transplantation: Twenty-seventh official adult lung and heart-lung transplant report—2010. J. Heart Lung Transplant. 2010;29:1104–1118. doi: 10.1016/j.healun.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Gottlieb J., Mattner F., Weissbrodt H., Dierich M., Fuehner T., Strueber M., Simon A., Welte T. Impact of graft colonization with gram-negative bacteria after lung transplantation on the development of bronchiolitis obliterans syndrome in recipients with cystic fibrosis. Respir. Med. 2009;103:743–749. doi: 10.1016/j.rmed.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 17.Botha P., Archer L., Anderson R.L., Lordan J., Dark J.H., Corris P.A., Gould K., Fisher A.J. Pseudomonas aeruginosa colonization of the allograft after lung transplantation and the risk of bronchiolitis obliterans syndrome. Transplantation. 2008;85:771–774. doi: 10.1097/TP.0b013e31816651de. [DOI] [PubMed] [Google Scholar]
- 18.Nunley D.R., Grgurich W., Iacono A.T., Yousem S., Ohori N.P., Keenan R.J., Dauber J.H. Allograft colonization and infections with pseudomonas in cystic fibrosis lung transplant recipients. Chest. 1998;113:1235–1243. doi: 10.1378/chest.113.5.1235. [DOI] [PubMed] [Google Scholar]
- 19.Johansen H.K., Moskowitz S.M., Ciofu O., Pressler T., Hoiby N. Spread of colistin resistant non-mucoid Pseudomonas aeruginosa among chronically infected Danish cystic fibrosis patients. J. Cyst. Fibros. 2008;7:391–397. doi: 10.1016/j.jcf.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Johansen H.K., Norregaard L., Gotzsche P.C., Pressler T., Koch C., Hoiby N. Antibody response to Pseudomonas aeruginosa in cystic fibrosis patients: A marker of therapeutic success?—A 30-year cohort study of survival in Danish CF patients after onset of chronic P. aeruginosa lung infection. Pediatr. Pulmonol. 2004;37:427–432. doi: 10.1002/ppul.10457. [DOI] [PubMed] [Google Scholar]
- 21.Ojeniyi B., Hoiby N., Rosdahl V.T. Genome fingerprinting as a typing method used on polyagglutinable Pseudomonas aeruginosa isolates from cystic fibrosis patients. APMIS. 1991;99:492–498. doi: 10.1111/j.1699-0463.1991.tb05181.x. [DOI] [PubMed] [Google Scholar]
- 22.Qvist T., Taylor-Robinson D., Waldmann E., Olesen H.V., Mathiesen I.H., Høiby N., Katzenstein T.L., Smyth R.L., Diggle P.J., Pressler T. Comparing the harmful effects of nontuberculous mycobacteria and Gram negative bacteria on lung function in patients with cystic fibrosis. J. Cyst. Fibros. 2016;15:380–385. doi: 10.1016/j.jcf.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyer K.C., Raghu G., Verleden G.M., Corris P.A., Aurora P., Wilson K.C., Brozek J., Glanville A.R. An international ISHLT/ATS/ERS clinical practice guideline: Diagnosis and management of bronchiolitis obliterans syndrome. Eur. Respir. J. 2014;44:1479–1503. doi: 10.1183/09031936.00107514. [DOI] [PubMed] [Google Scholar]
- 24.Esposito A., Pompilio A., Bettua C., Crocetta V., Giacobazzi E., Fiscarelli E., Jousson O., Di Bonaventura G. Evolution of Stenotrophomonas maltophilia in Cystic Fibrosis Lung over Chronic Infection: A Genomic and Phenotypic Population Study. Front. Microbiol. 2017;8:1590. doi: 10.3389/fmicb.2017.01590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi K.J., Cheng T.Z., Honeybrook A.L., Gray A.L., Snyder L.D., Palmer S.M., Abi Hachem R., Jang D.W. Correlation between sinus and lung cultures in lung transplant patients with cystic fibrosis. Int. Forum Allergy Rhinol. 2018;8:389–393. doi: 10.1002/alr.22067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boussaud V., Guillemain R., Grenet D., Coley N., Souilamas R., Bonnette P., Stern M. Clinical outcome following lung transplantation in patients with cystic fibrosis colonised with Burkholderia cepacia complex: Results from two French centres. Thorax. 2008;63:732–737. doi: 10.1136/thx.2007.089458. [DOI] [PubMed] [Google Scholar]
- 27.Vos R., Vanaudenaerde B.M., De Vleeschauwer S.I., Van Raemdonck D.E., Dupont L.J., Verleden G.M. De Novo or Persistent Pseudomonal Airway Colonization After Lung Transplantation: Importance for Bronchiolitis Obliterans Syndrome? Transplantation. 2008;86:624–625. doi: 10.1097/TP.0b013e318182295d. [DOI] [PubMed] [Google Scholar]
- 28.Mainz J.G., Naehrlich L., Schien M., Käding M., Schiller I., Mayr S., Schneider G., Wiedemann B., Wiehlmann L., Cramer N., et al. Concordant genotype of upper and lower airways P aeruginosa and S aureus isolates in cystic fibrosis. Thorax. 2009;64:535–540. doi: 10.1136/thx.2008.104711. [DOI] [PubMed] [Google Scholar]
- 29.Johansen H.K., Aanaes K., Pressler T., Nielsen K.G., Fisker J., Skov M., Høiby N., von Buchwald C. Colonisation and infection of the paranasal sinuses in cystic fibrosis patients is accompanied by a reduced PMN response. J. Cyst. Fibros. 2012;11:525–531. doi: 10.1016/j.jcf.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Srour N., Chaparro C., Vandemheen K., Singer L.G., Keshavjee S., Aaron S.D. Effect of infection with transmissible strains of Pseudomonas aeruginosa on lung transplantation outcomes in patients with cystic fibrosis. J. Heart Lung Transplant. 2015;34:588–593. doi: 10.1016/j.healun.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 31.Schultz H.H., Møller C.H., Zemtsovski M., Ravn J., Perch M., Martinussen T., Carlsen J., Iversen M. Donor Smoking and Older Age Increases Morbidity and Mortality after Lung Transplantation. Transplant. Proc. 2017;49:2161–2168. doi: 10.1016/j.transproceed.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 32.Auråen H., Durheim M.T., Dellgren G., Hämmäinen P., Larsson H., Geiran O., Schultz H.H.L., Leuckfeld I., Iversen M., Fiane A., et al. Effect of Donor Age on Outcome of Lung Transplantation Stratified by Recipient Diagnosis. Transplantation. 2019;103:807–814. doi: 10.1097/TP.0000000000002402. [DOI] [PubMed] [Google Scholar]
- 33.Goering R.V. Pulsed field gel electrophoresis: A review of application and interpretation in the molecular epidemiology of infectious disease. Infect. Genet. Evol. 2010;10:866–875. doi: 10.1016/j.meegid.2010.07.023. [DOI] [PubMed] [Google Scholar]