Abstract
(1) Background: China will provide free coronavirus disease 2019 (COVID-19) vaccinations for the entire population. This study analyzed the COVID-19 vaccination willingness rate (VWR) and its determinants under China’s free vaccination policy compared to a paid vaccine. (2) Methods: Data on 2377 respondents were collected through a nationwide questionnaire survey. Multivariate ordered logistic regression models were specified to explore the correlation between the VWR and its determinants. (3) Results: China’s free vaccination policy for COVID-19 increased the VWR from 73.62% to 82.25% of the respondents. Concerns about the safety and side-effects were the primary reason for participants’ unwillingness to be vaccinated against COVID-19. Age, medical insurance and vaccine safety were significant determinants of the COVID-19 VWR for both the paid and free vaccine. Income, occupation and vaccine effectiveness were significant determinants of the COVID-19 VWR for the free vaccine. (4) Conclusions: Free vaccinations increased the COVID-19 VWR significantly. People over the age of 58 and without medical insurance should be treated as the target intervention population for improving the COVID-19 VWR. Contrary to previous research, high-income groups and professional workers should be intervention targets to improve the COVID-19 VWR. Strengthening nationwide publicity and education on COVID-19 vaccine safety and effectiveness are recommended policies for decision-makers.
Keywords: COVID-19, vaccination willingness, free vaccination policy, determinant
1. Introduction
At the end of January 2021, the World Health Organization reported over 102.1 million infected cases, and over 2.2 million deaths, globally from the coronavirus disease 2019 (COVID-19) [1]. Vaccinations will be the most effective and economic way to prevent COVID-19 and control its spread [2], and people’s vaccination willingness will decide whether they will receive the COVID-19 vaccine. During 2021, China’s COVID-19 prevention and control policy [3] will provide free COVID-19 vaccinations for high-risk cohorts and then the general population. The government’s free vaccination program, and the successful management of COVID-19, will depend on people’s vaccination willingness. High vaccination rates protect both the vaccinated and unvaccinated, create herd immunity and reduce the risk of virus mutations. This study analyzed the determinants affecting people’s COVID-19 vaccination willingness under China’s free vaccination policy compared to the paid vaccine. The survey was conducted in May–June 2020 before the announcement on 9 January 2021 of China’s free vaccination program.
Previous vaccination studies have shown that many factors are responsible for the COVID-19 vaccination willingness rate (VWR), such as socio-economic factors, awareness of the severity and susceptibility to the disease and trust in the vaccine [4,5,6,7,8]. From a survey in Japan, Yoda and Katsuyama found that males, older age people, rural residents and chronic disease sufferers displayed the highest willingness toward COVID-19 vaccination [4]. Marital status and trust in the health service system were found to be key determinants of COVID-19 vaccination willingness in Saudi Arabia [9]. Using an online survey of American adults, Reiter et al. found that participants were more likely to get vaccinated when they perceived a higher likelihood of getting a COVID-19 infection in the future, perceived a heightened severity of COVID-19 infection and perceived greater effectiveness in a COVID-19 vaccine; they were less likely to get vaccinated when they perceived higher potential vaccine harm [5]. Several studies have also been carried out on special populations, such as healthcare workers, long-term care staff and caregivers, which found that concerns about vaccine safety, side effects and effectiveness were the primary reasons for vaccine hesitancy [7,10,11,12,13]. A Chinese national online survey found that participants that perceived the benefits and were unconcerned about the efficacy of COVID-19 vaccines had the highest intention to vaccinate [6]. Their willingness-to-pay (WTP) for COVID-19 vaccines was influenced by social and demographic factors, such as occupation and region. A number of discrete choice experiments revealed that a strong preference for the COVID-19 vaccine depended on its effectiveness, side-effects, protection duration and number of injections [14,15,16,17]. However, little is currently known about the effect of free vaccinations on the COVID-19 VWR in China. To address this lacuna, we surveyed participants’ (un)willingness to vaccinate when the vaccine was free; identified the reasons participants would get vaccinated or not; and recommend measures to improve the COVID-19 VWR.
2. Materials and Methods
2.1. Data Source and Sample
A questionnaire was designed to collect COVID-19 vaccination willingness and other variables. China’s 27 provinces were divided into three regions: eastern, central and western. The provinces in each region were stratified into low, medium and high economic levels according to their 2019 gross domestic product (GDP). Randomly, one province was chosen from each economic level in each region, yielding nine provinces. Next, according to their 2019 GDP rank, all the cities in each selected province were divided into low, medium and high economic levels. One city was randomly chosen from each GDP level, with 27 cities selected from the 9 provinces. One hundred participants were interviewed face-to-face, or by online video interviews in cities where participants were required to home quarantine, in each city, with equal numbers of men and women and three urban residents for every two rural residents, which reflected the nationwide urban–rural breakdown. All investigators recruited in the 27 cities received standardized training before the formal investigations. During 30 May to 10 June 2020, face-to-face interviews were conducted by interviewers. All participants were informed about the purpose of the survey and gave informed consent. We collected data on 2700 adults over the age of 18 years old, which yielded a sample of 2377 respondents after deleting cases with missing data, with a response rate of 88.04%.
2.2. Definition and Measurement of Dependent Variables
The categorical dependent variable, COVID-19 vaccination willingness, was assessed by two questions: “Would you pay for the COVID-19 vaccination?” and “Would you get the COVID-19 vaccination if the vaccine were free?” There were three answers (“no” (0), “it depends” (1) and “yes” (2)) for each question, representing COVID-19 vaccination willingness being low, medium and high.
2.3. Definition and Measurement of Independent Variables
As shown in Table 1, the independent variables comprised sex (male–female), age groups, three average monthly income groups (low (<RMB4000), medium (≥RMB4000–<RMB8000) and high (≥RMB8000)), education level (below high school, and high school and above), occupation, medical insurance (yes/no), urban–rural residence, self-rated health, residence in east–west–central region, and awareness of COVID-19 vaccine effectiveness, safety and risk of infection. Three urban residents were interviewed for every two rural participants. Occupations were categorized into professionals (including physicians, teachers and civil servants), farmers, students, self-employed, unemployed, migrant workers and other. Self-rated health was categorized into, “bad”, “medium” and “good”, based on the question: “How is your health status compared to your peers?” Participant’s awareness of COVID-19 vaccine effectiveness and safety was measured by the questions: “Do you believe that the COVID-19 vaccine is effective?”/“Do you believe that the COVID-19 vaccine is safe?”, and coded into a three-item Linkert scale (“don’t agree—low effectiveness/safety”, “neutral attitude--medium effectiveness/safety” and “agree—high effectiveness/safety”). The respondents’ risk of infection was measured by asking participants whether they would be infected by COVID-19 in the future according to “low–neutral–high” measure of risk.
Table 1.
Characteristic of respondents.
| Variables | N | % | |
|---|---|---|---|
| Sex | Male | 1154 | 48.55 |
| Female | 1223 | 51.45 | |
| Age | 18–27 | 915 | 38.49 |
| 28–37 | 340 | 14.30 | |
| 38–47 | 460 | 19.35 | |
| 48–57 | 426 | 17.92 | |
| 58+ | 236 | 9.93 | |
| Income | High (≥RMB8000) | 813 | 34.20 |
| Medium (≥RMB4000–<RMB8000) | 796 | 33.49 | |
| Low (<RMB4000) | 768 | 32.31 | |
| Education level | Below high school | 1472 | 61.93 |
| High school and above | 905 | 38.07 | |
| Occupation | Professional | 708 | 29.79 |
| Farmer | 278 | 11.70 | |
| Migrant worker | 289 | 12.16 | |
| Self-employed | 221 | 9.30 | |
| Unemployed | 103 | 4.33 | |
| Student | 639 | 26.88 | |
| Retired | 86 | 3.62 | |
| Other | 53 | 2.23 | |
| Medical insurance | Yes | 2289 | 96.30 |
| No | 88 | 3.70 | |
| Residence | Urban | 1462 | 61.51 |
| Rural | 915 | 38.49 | |
| Self-rated health | Bad | 73 | 3.07 |
| Medium | 564 | 23.73 | |
| Good | 1740 | 73.20 | |
| Region | Eastern | 748 | 31.47 |
| Central | 686 | 28.86 | |
| Western | 943 | 39.67 | |
| Vaccine effectiveness | Low | 17 | 0.72 |
| Medium | 301 | 12.66 | |
| High | 2059 | 86.62 | |
| Vaccine safety | Low | 40 | 1.68 |
| Medium | 378 | 15.90 | |
| High | 1959 | 82.41 | |
| Risk of infection | Low | 1107 | 46.57 |
| Medium | 670 | 28.19 | |
| High | 600 | 25.24 | |
2.4. Statistical Analyses
All data were double-entered using EpiData 3.1 and checked for consistency. Statistical analyses were performed using STATA 12.0. The Pearson chi-square test was used to compare the differences in VWRs among different subgroups and the VWR differences between the paid and free vaccine. Multivariate ordered logistic regression models and odds ratio (OR) were used to assess the associations between each independent variable and the VWRs of the paid and free COVID-19 vaccines.
3. Results
3.1. Characteristics of Respondents
Table 1 shows the characteristics of 2377 survey respondents, with the male (49%) and female (51%) sex ratio broadly even and the urban (62%)–rural (38%) split close to the 3:2 national urban–rural ratio; the median age was 35; the median monthly income was RMB5000 and the three low-, medium- and high-income groups were roughly equal. In terms of education, 38.07% respondents had a high school and above education level. Professionals (29.79%) accounted for the highest occupational group, followed by students (26.88%), migrant workers (12.16%) and farmers (11.70%). Only 3.07% reported their self-assessed health as “bad” and 96% had one or more type of medical insurance. There was a broadly equal number of respondents from the eastern (31.47%), central (28.86%) and western (39.67%) regions. Respondents mainly believed that the COVID-19 vaccine was effective (86.62%); 82.41% believed that the vaccine was safe and 53.43% thought they were at medium or high risk of COVID-19 infection.
3.2. COVID-19 Vaccination Willingness Rate
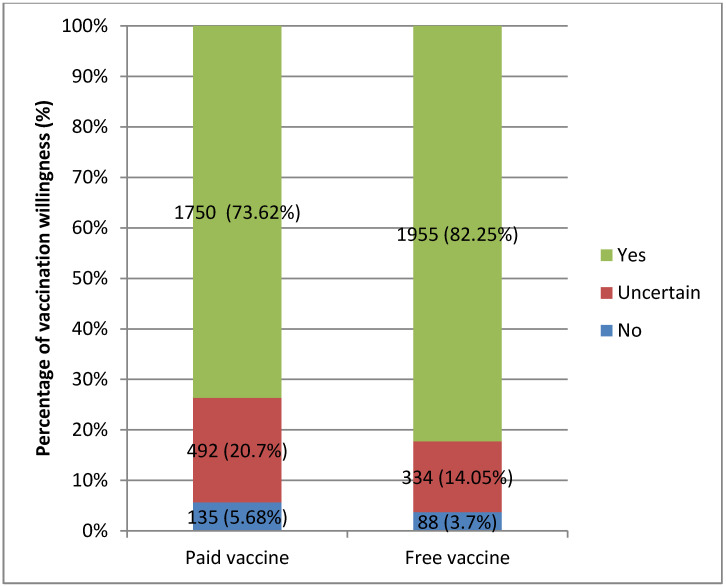
Figure 1 shows that the COVID-19 VWR increased from 73.62% to 82.25% when vaccination changed from paid to free, and the uncertain group fell from 20.7% to 14.05% (Chi2 = 827.89, p < 0.001). For the paid vaccine, only 5.7% were unwilling to vaccinate: first, because of concerns about the safety and side-effects of the COVID-19 vaccine (32.99%); second, because there was no perceived need for vaccination because the COVID-19 outbreak had been controlled in China (23.71%); and third, because of the expense of the vaccine (15.46%). For the free vaccine, only 3.7% were unwilling to vaccinate, with 51.32% worried about the safety and side-effects of COVID-19 vaccines; 13.16% did not believe that the vaccine was effective and 9.21% believed that they would not be infected in the future and that it was unnecessary to vaccinate against COVID-19.
Figure 1.
Comparison of COVID-19 vaccination willingness rates (VWRs) between paid and free vaccine.
3.3. Results of Chi-Square Test
Table 2 shows that the COVID-19 VWR for the free vaccine was higher than that of the paid vaccine in all subgroups (p < 0.05), except for the low vaccine effectiveness group, the VWR of which was 47.06% for the paid vaccine and 41.18% for the free vaccine (p = 0.005). For both the paid and free vaccine, the COVID-19 VWRs of the below high school education group was higher than the high school and above group (p < 0.05); farmers retained the highest VWR among all occupations, with a 76.62% VWR for the paid vaccine and 88.85% VWR for the free vaccine (p = 0.001); the VWR of respondents who had medical insurance was higher than that of non-insured respondents (p < 0.05); and the VWR increased with participants’ increased awareness of vaccine effectiveness and safety (p < 0.001). The VWR of the 28–37 age group was the highest, and the VWR of the over-58 age group was the lowest for the paid vaccine group, with a VWR of 69.49% (p < 0.001), but it rose to 83.9% for the free vaccine (p = 0.001). There were no differences among income groups for the paid vaccine, but the VWR decreased with income when the vaccine was free (p = 0.004), with the highest VWR for the low-income group (86.2%). The central region had the highest VWR (83.53%), followed by the western area (82.61%) and the eastern area (80.61%), for the free vaccine (p = 0.034). The participants with the highest awareness of a COVID-19 infection risk were most willing to get vaccinated, with a VWR of 84.33% for the free vaccine (p = 0.013).
Table 2.
Comparison of COVID-19 vaccination willingness for paid and free vaccination with independent variables.
| Variables | VWR of Paid Vaccine | VWR of Free Vaccine | Comparison between Paid and Free Vaccination | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | χ2 | p | N | % | χ2 | p | χ2 | p | ||
| Sex | Male | 862 | 74.70 | 1.50 | 0.471 | 953 | 82.58 | 0.72 | 0.698 | 498.37 | <0.001 |
| Female | 888 | 72.61 | 1002 | 81.93 | 346.51 | <0.001 | |||||
| Age | 18–27 | 670 | 73.22 | 63.75 | <0.001 | 755 | 82.51 | 25.12 | 0.001 | 244.42 | <0.001 |
| 28–37 | 266 | 78.24 | 291 | 85.59 | 93.89 | <0.001 | |||||
| 38–47 | 321 | 69.78 | 362 | 78.70 | 185.32 | <0.001 | |||||
| 48–57 | 329 | 77.23 | 349 | 81.92 | 208.45 | <0.001 | |||||
| 58+ | 164 | 69.49 | 198 | 83.90 | 66.22 | <0.001 | |||||
| Income | High | 602 | 74.05 | 2.95 | 0.565 | 642 | 78.97 | 15.35 | 0.004 | 339.79 | <0.001 |
| Medium | 584 | 73.37 | 651 | 81.78 | 271.24 | <0.001 | |||||
| Low | 564 | 73.44 | 662 | 86.20 | 235.30 | <0.001 | |||||
| Education level | Below high school | 1093 | 74.25 | 22.71 | <0.001 | 1228 | 83.42 | 7.68 | 0.021 | 536.48 | <0.001 |
| High school and above | 657 | 72.60 | 727 | 80.33 | 280.16 | <0.001 | |||||
| Occupation | Professional | 525 | 74.15 | 36.93 | 0.001 | 559 | 78.95 | 35.57 | 0.001 | 290.55 | <0.001 |
| Farmer | 213 | 76.62 | 247 | 88.85 | 99.27 | <0.001 | |||||
| Migrant worker | 220 | 76.12 | 239 | 82.70 | 104.51 | <0.001 | |||||
| Self-employed | 152 | 68.78 | 180 | 81.45 | 78.91 | <0.001 | |||||
| Unemployed | 71 | 68.93 | 89 | 86.41 | 29.02 | <0.001 | |||||
| Student | 468 | 73.24 | 525 | 82.16 | 184.11 | <0.001 | |||||
| Retired | 63 | 73.26 | 73 | 84.88 | 43.66 | <0.001 | |||||
| Other | 38 | 71.70 | 43 | 81.13 | 13.47 | 0.009 | |||||
| Medical insurance | Yes | 1700 | 74.27 | 13.66 | 0.001 | 1892 | 82.66 | 8.39 | 0.015 | 786.92 | <0.001 |
| No | 50 | 56.82 | 63 | 71.59 | 36.37 | <0.001 | |||||
| Residence | Urban | 1080 | 73.87 | 0.84 | 0.657 | 1197 | 81.87 | 0.39 | 0.821 | 582.10 | <0.001 |
| Rural | 670 | 73.22 | 758 | 82.84 | 258.51 | <0.001 | |||||
| Self-rated health | Bad | 50 | 68.49 | 7.79 | 0.100 | 60 | 82.19 | 1.17 | 0.883 | 11.14 | 0.025 |
| Medium | 400 | 70.92 | 466 | 82.62 | 161.68 | <0.001 | |||||
| Good | 1300 | 74.71 | 1429 | 82.13 | 680.67 | <0.001 | |||||
| Region | Eastern | 546 | 72.99 | 6.80 | 0.147 | 603 | 80.61 | 10.40 | 0.034 | 265.17 | <0.001 |
| Central | 505 | 73.62 | 573 | 83.53 | 386.46 | <0.001 | |||||
| Western | 699 | 74.13 | 779 | 82.61 | 188.60 | <0.001 | |||||
| Vaccine effectiveness | Low | 8 | 47.06 | 124.14 | <0.001 | 7 | 41.18 | 245.71 | <0.001 | 14.85 | 0.005 |
| Medium | 147 | 48.84 | 162 | 53.82 | 138.87 | <0.001 | |||||
| High | 1595 | 77.46 | 1786 | 86.74 | 529.37 | <0.001 | |||||
| Vaccine safety | Low | 18 | 45.00 | 167.88 | <0.001 | 21 | 52.50 | 279.62 | <0.001 | 25.40 | <0.001 |
| Medium | 194 | 51.32 | 214 | 56.61 | 199.46 | <0.001 | |||||
| High | 1538 | 78.51 | 1720 | 87.80 | 421.77 | <0.001 | |||||
| Risk of infection | Low | 802 | 72.45 | 9.22 | 0.056 | 914 | 82.57 | 12.69 | 0.013 | 394.98 | <0.001 |
| Medium | 485 | 72.39 | 535 | 79.85 | 250.14 | <0.001 | |||||
| High | 463 | 77.17 | 506 | 84.33 | 206.12 | <0.001 | |||||
3.4. Results of Multiple Ordered Logistic Regressions
Table 3 shows the results of two multivariate ordered logistic regression models specified to analyze the relationship between the VWR and the independent variables for the paid and free vaccine. Sex, education level, urban–rural residence, self-rated health, region and awareness of infection risk had no influence on VWR for both paid and free vaccines. The COVID-19 VWR of respondents aged above 58 was significantly lower than the 18–27 age group (OR = 0.581, p = 0.019 for the paid vaccine; OR = 0.456, p = 0.006 for the free vaccine) and respondents without medical insurance had a lower COVID-19 VWR than respondents who had medical insurance (OR = 0.496, p = 0.002 for the paid vaccine; OR = 0.513, p = 0.011 for the free vaccine). The COVID-19 VWR increased with vaccine safety for both the paid (OR = 2.061, p = 0.037 (medium group); OR = 4.692, p < 0.001 (high group)) and free (OR = 2.071, p = 0.046 (medium group); OR = 6.641, p < 0.001 (high group)) vaccine. There was no difference in VWR among different income groups for the paid vaccine, but the COVID-19 VWR for the low-income group was higher than for high-income group for the free vaccine (OR = 1.536, p = 0.009). There was no statistical difference between the VWRs of famers and professionals for the paid vaccine, while the farmers had a higher VWR than professionals when the vaccine was free (OR = 2.016, p = 0.008). Self-employed respondents had a lower VWR than professional participants for the paid vaccine (OR = 0.695, p = 0.046), but there was no difference between the self-employed and professionals in the free vaccine model in Table 3. For the paid vaccine, there was no difference in the COVID-19 VWRs among respondents with different awareness levels of vaccine effectiveness; however, the VWR of people with a high awareness level of vaccine effectiveness was higher than the low awareness group (OR = 5.49, p = 0.002).
Table 3.
Results of multiple ordered logistic regressions.
| Variables | Paid Vaccine | Free Vaccine | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | S.E. | p | OR (95% CI) | β | S.E. | p | OR (95% CI) | ||
| Sex | Male | (Reference group) | (Reference group) | ||||||
| Female | −0.09 | 0.10 | 0.335 | 0.910 (0.752, 1.102) | −0.11 | 0.12 | 0.353 | 0.898 (0.715, 1.127) | |
| Age | 18–27 | (Reference group) | (Reference group) | ||||||
| 28–37 | 0.28 | 0.19 | 0.146 | 1.325 (0.907, 1.937) | 0.15 | 0.24 | 0.521 | 1.164 (0.732, 1.849) | |
| 38–47 | −0.14 | 0.18 | 0.426 | 0.869 (0.614, 1.229) | −0.32 | 0.21 | 0.130 | 0.724 (0.476, 1.100) | |
| 48–57 | 0.07 | 0.19 | 0.706 | 1.075 (0.739, 1.562) | −0.37 | 0.23 | 0.101 | 0.691 (0.445, 1.075) | |
| 58+ | −0.54 | 0.23 | 0.019 | 0.581 (0.370, 0.913) | −0.79 | 0.29 | 0.006 | 0.456 (0.260, 0.799) | |
| Income | High | (Reference group) | (Reference group) | ||||||
| Medium | −0.06 | 0.12 | 0.645 | 0.945 (0.743, 1.202) | 0.17 | 0.14 | 0.223 | 1.187 (0.901, 1.565) | |
| Low | −0.06 | 0.14 | 0.661 | 0.942 (0.723, 1.229) | 0.43 | 0.16 | 0.009 | 1.536 (1.113, 2.118) | |
| Education level | Below high school | (Reference group) | (Reference group) | ||||||
| High school and above | −0.16 | 0.12 | 0.197 | 0.855 (0.673, 1.085) | −0.21 | 0.14 | 0.146 | 0.814 (0.617, 1.074) | |
| Occupation | Professional | (Reference group) | (Reference group) | ||||||
| Farmer | 0.22 | 0.21 | 0.283 | 1.247 (0.833, 1.865) | 0.70 | 0.26 | 0.008 | 2.016 (1.205, 3.373) | |
| Migrant worker | 0.08 | 0.18 | 0.649 | 1.086 (0.761, 1.550) | 0.10 | 0.21 | 0.616 | 1.111 (0.737, 1.673) | |
| Self-employed | −0.36 | 0.18 | 0.046 | 0.695 (0.486, 0.993) | 0.03 | 0.22 | 0.887 | 1.032 (0.672, 1.584) | |
| Unemployed | −0.07 | 0.26 | 0.793 | 0.933 (0.556, 1.566) | 0.62 | 0.35 | 0.077 | 1.859 (0.936, 3.693) | |
| Student | −0.04 | 0.18 | 0.800 | 0.956 (0.676, 1.353) | −0.11 | 0.21 | 0.610 | 0.897 (0.591, 1.361) | |
| Retired | 0.13 | 0.29 | 0.663 | 1.137 (0.638, 2.024) | 0.58 | 0.37 | 0.111 | 1.789 (0.875, 3.659) | |
| Other | −0.16 | 0.33 | 0.637 | 0.854 (0.445, 1.641) | 0.05 | 0.40 | 0.901 | 1.050 (0.483, 2.284) | |
| Medical insurance | Yes | (Reference group) | (Reference group) | ||||||
| No | −0.70 | 0.22 | 0.002 | 0.496 (0.321, 0.766) | −0.67 | 0.26 | 0.011 | 0.513 (0.306, 0.858) | |
| Residence | Urban | (Reference group) | (Reference group) | ||||||
| Rural | −0.05 | 0.11 | 0.666 | 0.955 (0.773, 1.178) | −0.09 | 0.13 | 0.477 | 0.913 (0.711, 1.173) | |
| Self-rated health | Bad | (Reference group) | (Reference group) | ||||||
| Medium | 0.23 | 0.28 | 0.413 | 1.262 (0.723, 2.204) | 0.34 | 0.36 | 0.333 | 1.411 (0.703, 2.834) | |
| Good | 0.34 | 0.28 | 0.230 | 1.399 (0.808, 2.422) | 0.27 | 0.35 | 0.443 | 1.306 (0.660, 2.584) | |
| Region | Eastern | (Reference group) | (Reference group) | ||||||
| Central | 0.03 | 0.13 | 0.823 | 1.029 (0.800, 1.325) | 0.08 | 0.15 | 0.593 | 1.085 (0.804, 1.464) | |
| Western | 0.08 | 0.12 | 0.485 | 1.088 (0.859, 1.378) | −0.03 | 0.14 | 0.850 | 0.974 (0.738, 1.284) | |
| Vaccine effectiveness | Low | (Reference group) | (Reference group) | ||||||
| Medium | −0.05 | 0.52 | 0.920 | 0.950 (0.344, 2.622) | 0.80 | 0.54 | 0.138 | 2.229 (0.773, 6.430) | |
| High | 0.66 | 0.52 | 0.202 | 1.931 (0.703, 5.303) | 1.70 | 0.54 | 0.002 | 5.490 (1.910, 15.785) | |
| Vaccine safety | Low | (Reference group) | (Reference group) | ||||||
| Medium | 0.72 | 0.35 | 0.037 | 2.061 (1.044, 4.068) | 0.73 | 0.36 | 0.046 | 2.071 (1.013, 4.234) | |
| High | 1.55 | 0.34 | <0.001 | 4.692 (2.411, 9.131) | 1.89 | 0.36 | <0.001 | 6.641 (3.279, 13.450) | |
| Risk of infection | Low | (Reference group) | (Reference group) | ||||||
| Medium | 0.17 | 0.11 | 0.146 | 1.181 (0.944, 1.478) | 0.06 | 0.14 | 0.657 | 1.062 (0.814, 1.386) | |
| High | 0.20 | 0.12 | 0.101 | 1.221 (0.962, 1.550) | 0.03 | 0.15 | 0.819 | 1.034 (0.778, 1.374) | |
4. Discussion
The COVID-19 VWR and its influencing factors among Chinese adults were analyzed for a paid and a free vaccine. The outcomes can be used to guide projections of future COVID-19 vaccine uptake and shape vaccination policy. The COVID-19 VWR was 82.25% for the free vaccine, significantly higher than 73.62% for the paid vaccine, increasing the COVID-19 VWR by 11.72%. For the paid vaccine, the VWR in this study was higher than in similar studies in Japan (65.7%) [4], France (62%), Germany (70%) [18] and the United States (69%) [5], but roughly the same as the Netherlands (73%), Italy (74%) and Portugal (75%); the VWR for the free vaccine was similar to Denmark (80%) [18] and Australia (85.8%) [19].
Age, medical insurance and vaccine safety were significant influencing factors in both the paid and free vaccine regression models; sex, education level, urban–rural residence, self-rated health, region and awareness of infection risk were not significant factors in VWR. Although free vaccinations raised COVID-19 VWR from 69.49% to 83.9% for respondents aged over 58 years old, their VWR remained lower than the 18–27 age group for both paid (OR = 0.581) and free vaccinations (OR = 0.456). This finding was counter to previous studies in Japan and the United States, which showed that the elderly had a higher COVID-19 vaccination willingness [4,20]. The COVID-19 VWR of people who had no medical insurance was only half that of those who had medical insurance (OR = 0.496 for the paid vaccine, OR = 0.513 for the free vaccine) even through the COVID-19 VWR of people without medical insurance increased from 56.82% to 71.59% when the vaccine was free. This finding is similar to past research, which found the COVID-19 vaccine acceptance of people with private or public health insurance was higher than people without health insurance [5]. One recommendation from our study is that special measures should be taken among people aged over 58 years old and without medical insurance to enhance their VWR.
Vaccine safety had the greatest impact on COVID-19 VWR, with the biggest OR = 6.63 for the high vaccine safety group in the free vaccine model. The COVID-19 VWR increased when respondents’ awareness of vaccine safety increased, consistent with a U.S. study that found that perceptions of the potential harm of a COVID-19 vaccine decreased people’s willingness to get vaccinated. However, the U.S. study also found that perceiving a risk of getting a COVID-19 infection in the future increased the VWR, which was different from the result in our study [5]. A study in Kuwait also showed that the respondents were less willing to accept COVID-19 vaccination when they viewed vaccines in general to have health-related risks [21]. We suggest that improving people’s awareness of vaccine safety will help to increase the COVID-19 VWR.
Income had no influence on COVID-19 VWR in the paid vaccine model, but the low-income group had a higher COVID-19 VWR than the high-income group in the free vaccine model (86.2% vs. 78.97%, OR = 1.536), which was different from previous research [5,6,22,23,24,25]. The VWR growth rate of free vaccinations for the low-income group was 17.37% (from 73.44% to 86.2%), but that for the high-income group was only 6.64% (from 74.05% to 78.97%). Free vaccinations had the greatest effect on the COVID-19 VWR of low-income people among all income groups. Surprisingly, one recommendation from our study is that new interventions should target the high-income group because their COVID-19 VWR was lower than the low-income group when vaccinations were free.
The COVID-19 VWR of self-employed people was lower than professionals for the paid vaccine. Famers’ COVID-19 VWR increased from 76.62% to 88.85% with a growth rate of 15.96%, and that of self-employed people increased from 68.78% to 81.45% when the vaccine was free. The COVID-19 VWR of professionals only increased from 74.15% to 78.95%, with a growth rate of 6.47%, and their VWR was also lower than famers’ VWR for the free vaccine. While the self-employed should be a key intervention target for the paid vaccine, professionals are a key intervention group for free vaccinations.
For the paid vaccine, people’s COVID-19 VWR was only affected by vaccine safety, without any influence from vaccine effectiveness in the regression analysis. For the free vaccine, people cared not only about vaccine safety, but also about vaccine effectiveness. These results are similar to previous studies that showed that the perceived effectiveness of a COVID-19 vaccine improved the VWR [5,6,14,15,26]. Worrying about the safety and side-effects was also a main reason for people’s unwillingness to be vaccinated for both the paid vaccine (32.99%) and free vaccine (51.32%). Suspecting the effectiveness of vaccines was the second reason for unwillingness to take up the free vaccine (13.16%) in this study. For both the paid and free vaccines, information and education campaigns should be launched to reassure the public that listed COVID-19 vaccines are safe and effective and thus enhance the public’s trust in the COVID-19 vaccines [18,27,28,29,30]. Since urban–rural residence and regional location were not significant determinants of the VWR, information and education campaigns can be national.
Strengths and Limitations
This study has several strengths. First, this was the first study to assess the effect of a COVID-19 free vaccination policy on the COVID-19 VWR among Chinese adults. Second, the dataset came from a nationwide questionnaire survey, covering both rural and urban areas, and three (eastern, central and western) regions in China. Third, face-to-face or online video interviews were conducted to collect the data in contrast to most past research, which relied on online questionnaire surveys.
There were two major limitations. First, we used only one question to evaluate respondents’ COVID-19 vaccination willingness; a more complex vaccination willingness scale should be developed in further studies. Second, the sample was limited to only 100 respondents in each city across three regions in China.
5. Conclusions
Free vaccinations increased COVID-19 VWR by 11.72%, increasing the willingness to vaccinate from 73.62% for the paid vaccine to 82.25% for the free vaccine. Given the negative health and economic impact of the COVID-19 virus, increased vaccination rates promotes herd immunity and China’s return to pre-COVDI-19 normality. For both the paid and free vaccine, vaccine safety was the most significant concern among the study participants. The COVID-19 VWR for the free vaccine for respondents aged over 58 years old and without medical insurance was lower than the reference groups. Our results suggest that intervention measures should be directed towards people aged over 58 years old and without medical insurance to improve their COVID-19 VWR. For the free vaccine, the COVID-19 VWR of the high-income group was lower than the low-income group and that of professionals lower than farmers. Surprisingly, our results suggest that high-income groups and professionals should be special COVID-19 VWR intervention targets for the free vaccine. Strengthening COVID-19 vaccine knowledge through public information and education campaigns on vaccine safety would improve VWR, whether the vaccine is free or not. Vaccine effectiveness should be included in a nationwide COVID-19 education campaign, especially for the free vaccine.
Acknowledgments
The authors thank reviewers for their constructive comments and thank all interviewers from the nine sample provinces for their contribution to the survey.
Author Contributions
Conceptualization, R.L. and A.L. and J.W.; methodology, R.L. and Y.Z.; software, R.L. and Y.Z.; validation, S.N. and J.W. and R.L.; formal analysis, R.L. and Y.Z.; investigation, R.L. and A.L. and Y.Z.; resources, J.W. and A.L. and R.L.; data curation, R.L. and Y.Z.; writing—original draft preparation, R.L. and J.W. and Y.Z.; writing—review and editing, S.N. and E.M. and J.W.; supervision, J.W.; project administration, J.W. and A.L. and R.L.; funding acquisition, R.L. and A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Natural Science Foundation of China, grant number 71904089; the NHC Key Laboratory of Health Economics and Policy Research (Shandong University), grant number: NHC-HEPR2019006; the China Postdoctoral Science Foundation, grant number 2019M662392; and the Qingdao Postdoctoral Foundation.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Nanjing Medical University (protocol code Nanjing Medical University Ethical Audit (2020) Number 565 and 16 June 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to multi-cooperation with Wuhan University, Shandong University and Nanjing Medical University. The corresponding author will facilitate a discussion with these three universities for data access on a reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Coronavirus Disease (COVID-2019) Situation Reports. [(accessed on 4 February 2021)]; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.DRAFT Landscape of COVID-19 Candidate Vaccines—30 April 2020. [(accessed on 16 March 2021)]; Available online: https://www.who.int/whodocuments-detail/draft-landscape-of-COVID-19-candidate-vaccines.
- 3.COVID-19 Vaccination Free to Chinese Residents: Official. [(accessed on 5 February 2021)]; Available online: http://www.ecns.cn/news/2021-01-09/detail-ihafqmaz1834647.shtml.
- 4.Yoda T., Katsuyama H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines. 2021;9:48. doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020;14:e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nzaji M.K., Ngombe L.K., Mwamba G.N., Ndala D.B.B., Miema J.M., Lungoyo C.L., Mwimba B.L., Bene A.C.M., Musenga E.M. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragm. Observ. Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Graffigna G., Palamenghi L., Boccia S., Barello S. Relationship between Citizens’ Health Engagement and Intention to Take the COVID-19 Vaccine in Italy: A Mediation Analysis. Vaccines. 2020;8:576. doi: 10.3390/vaccines8040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohammed A.-M., Kumar P.B. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J. Multidiscip. Healthc. 2020;13:1657–1663. doi: 10.2147/jmdh.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldman R.D., Yan T.D., Seiler M., Cotanda C.P., Brown J.C., Klein E.J., Hoeffe J., Gelernter R., Hall J.E., Davis A.L., et al. International COVID-19 Parental Attitude Study Group Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine. 2020 doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., Gagneur A., Dubé E. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surv. Bull. Eur. Mal. Trans. Eur. Commun. Dis. Bull. 2021;26 doi: 10.2807/1560-7917.Es.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Unroe K.T., Evans R., Weaver L., Rusyniak D., Blackburn J. Willingness of long-term care staff to receive a COVID-19 vaccine: A single state survey. J. Am. Geriat. Soc. 2020 doi: 10.1111/jgs.17022. [DOI] [PubMed] [Google Scholar]
- 13.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020 doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leng A., Maitland E., Wang S., Nicholas S., Liu R., Wang J. Individual preferences for COVID-19 vaccination in China. Vaccine. 2021;39:247–254. doi: 10.1016/j.vaccine.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dong D., Xu R.H., Wong E.L.-Y., Hung C.-T., Feng D., Feng Z., Yeoh E.-K., Wong S.Y.-S. Public preference for COVID-19 vaccines in China: A discrete choice experiment. Health Expect. Int. J. Public Particip. Health Care Health Policy. 2020 doi: 10.1111/hex.13140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borriello A., Master D., Pellegrini A., Rose J.M. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2020;39:473–479. doi: 10.1016/j.vaccine.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.García L.Y., Cerda A.A. Contingent assessment of the COVID-19 vaccine. Vaccine. 2020;38:5424–5429. doi: 10.1016/j.vaccine.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., Exel J.v., Schreyögg J., Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dodd R.H., Cvejic E., Bonner C., Pickles K., McCaffery K.J. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinMed. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alqudeimat Y., Alenezi D., AlHajri B., Alfouzan H., Almokhaizeem Z., Altamimi S., Almansouri W., Alzalzalah S., Ziyab A. Acceptance of a COVID-19 Vaccine and its Related Determinants among the General Adult Population in Kuwait. Med. Princ. Pract. Int. J. Kuwait Univ. Health Sci. Cent. 2021 doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarasty O., Carpio C.E., Hudson D., Guerrero-Ochoa P.A., Borja I. The demand for a COVID-19 vaccine in Ecuador. Vaccine. 2020;38:8090–8098. doi: 10.1016/j.vaccine.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willingness to pay for a COVID-19 vaccine high in Chile. Pharm. Econ. Outcomes News. 2020;858:35. doi: 10.1007/s40274-020-7008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., Setiawan A.M., Rajamoorthy Y., Sofyan H., Vo T.Q., et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum. Vaccines Immunother. 2020;16:3074–3080. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong L.P., Alias H., Wong P.F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020;16:2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., Ryan M., Fuemmeler B.F., Carlyle K.E. Willingness to get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control. 2020;49:137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang S. Don’t rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020 doi: 10.1038/d41586-020-00751-9. [DOI] [PubMed] [Google Scholar]
- 28.Ehde D.M., Roberts M.K., Herring T.E., Alschuler K.N. Willingness to obtain COVID-19 vaccination in adults with multiple sclerosis in the United States. Mult. Scler. Relat. Disord. 2021;49:102788. doi: 10.1016/j.msard.2021.102788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miyachi T., Takita M., Senoo Y., Yamamoto K. Lower trust in national government links to no history of vaccination. Lancet. 2020;395:31–32. doi: 10.1016/S0140-6736(19)32686-8. [DOI] [PubMed] [Google Scholar]
- 30.Liu Z., Yang J.Z. In the Wake of Scandals: How Media Use and Social Trust Influence Risk Perception and Vaccination Intention among Chinese Parents. Health Commun. 2020:1–12. doi: 10.1080/10410236.2020.1748834. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to multi-cooperation with Wuhan University, Shandong University and Nanjing Medical University. The corresponding author will facilitate a discussion with these three universities for data access on a reasonable request.