Abstract
Background
Foot characteristics and mechanics are hypothesized to affect aetiology of several lower extremity musculoskeletal conditions, including knee osteoarthritis (KOA). The purpose of this systematic review was to identify the foot characteristics and mechanics of individuals with KOA.
Methods
Five databases were searched to identify relevant studies on foot characteristics and mechanics in people with KOA. Meta-analyses were performed where common measures were found across included studies. Included studies were evaluated for data reporting quality using the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) checklist.
Results
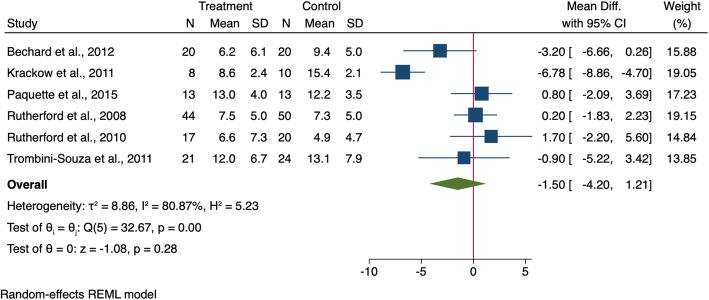
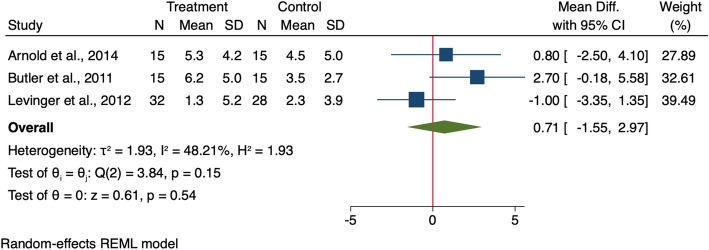
Thirty-nine studies were included in this systematic review. Two studies reported participants with KOA had statistically significantly (P < 0.05) more pronated foot postures than those without. Meta-analyses for foot progression angle (FPA) and peak rearfoot eversion angle found no difference between those with and without KOA (FPA mean difference:-1.50 [95% confidence interval − 4.20-1.21]; peak rearfoot eversion mean difference: 0.71 [1.55–2.97]).
Conclusion
A more pronated foot posture was noticed in those with KOA. However, it was not possible to establish a relationship between other foot characteristics or mechanics in people with KOA due to heterogeneity between the included study and limited number of studies with similar measurements. There is need for identifying common measurement techniques and reporting metrics when studying the foot in those with KOA.
Keywords: Foot posture, Foot mechanics, Foot characteristics, Knee osteoarthritis
Background
Knee osteoarthritis (KOA) is a degenerative progressive joint disease characterized by chronic joint pain and stiffness, leading to the limitation of daily living activities and physical function [1–3]. KOA is estimated to affect 18% of adults over 45 years of age [4] and is a leading cause of functional disability [5]. Aetiology of KOA includes traumatic injury [6], genetics [7], obesity [8], and poor joint biomechanics, with poor biomechanics a likely cause of primary progressive KOA [9].
Given the important role of the foot in receiving and distributing forces during walking, foot characteristics and mechanics, including static foot posture and dynamic foot function, may significantly contribute to musculoskeletal conditions of the lower limb [10]. However, the specific associations between foot characteristics and mechanics and KOA [11] have not yet been investigated. Therefore, the primary purpose of this systematic review is to evaluate foot characteristics and mechanics in individuals with KOA and compare them to people without KOA. There were two aims of the study: 1) to provide an overview of the foot characteristics and mechanics that have been evaluated in the extant literature in people with KOA, and 2) to investigate whether foot characteristics and mechanics vary between people with and without KOA.
Methods
This systematic review was submitted and approved through the PROSPERO registry of systematic reviews (CRD42015023946), and it followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12].
Search strategy and study selection
Five electronic databases were searched: MEDLINE, Web of Science, Current Nursing and Allied Health literature (CINAHL), Physical Education Index, and Physiotherapy Evidence Database (PEDro). The searches were conducted in May 2020, with no restrictions by language, year of publication or study design. The Medical Subject Headings (MeSH) search terms adopted were “foot” and “knee osteoarthritis” using the Boolean operator AND.
Studies were evaluated for relevance by applying specific inclusion and exclusion criteria (see Table 1). At the title stage, one reviewer (RA) eliminated publications, with a second reviewer (JLR) verifying the results. At the abstract stage, two reviewers (RA and JLR) independently reviewed abstracts for inclusion, and reference lists of prior KOA review articles were searched to include relevant studies. For manuscripts included following the abstract stage, full-text articles were obtained and independently reviewed for inclusion by reviewers (RA and JLR).
Table 1.
Study inclusion criteria
| Criteria | Description |
|---|---|
| Study design | Studies with cross-sectional data or intervention data if the baseline data were available. |
| Study participants | Studies were included if they recruited participants with KOA; where a control group was included, they had to be otherwise healthy and free from KOA. |
| Study outcome domains | Studies had to include objective measures of foot mechanics or foot characteristics to be eligible. Objective measures of foot mechanics or characteristics included, but were not limited to, foot progression angle, rearfoot eversion, Foot Posture Index and muscle activity. Further data could be obtained from participants in a barefoot or shod condition, provided the shod condition was without any foot orthoses. |
| Study results | Results had to provide quantitative data presented as mean and standard deviation or median and interquartile range clearly indicating if it was collected in a barefoot or shod condition. |
Data extraction
Data from the included manuscripts were extracted (RA) and checked (JLR). For each manuscript, the data extracted was as follows: the country, year of study, sample size, age, gender, body mass index (BMI), diagnostic and inclusion criteria for participants, footwear condition (i.e., barefoot, shod), foot-related outcome measures, and foot-related outcome data. For intervention studies, the baseline data were extracted for analysis. The level of agreement was determined using weighted kappa statistics for inclusion/exclusion.
Assessment of study quality
Study quality of the information reported in the included manuscripts were based on the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) checklist criteria [13], which is a reliable quality rating tool for observational studies [14]. Each criterion was scored “Yes”, “No”, or not applicable (NA). A criterion received a “Yes” if it was applicable and met in the study, “No” if it was applicable but not met, and “NA” if it was not relevant to the study. The number of “Yes” criterion divided by the number of applicable criterions per manuscript yielded a percentage of the applicable STROBE criteria. Articles were dichotomized by their rating scores, with ≥65% regarded as high-quality studies, and < 65% deemed low-quality. The 65% cut-off point is similar to work conducted by Andrews et al. [15] in dichotomizing high and low quality studies. The 65% cut-off point is lower than the recommended cut-off point of 80% [16] as the reported foot characteristics and mechanics were often not the study’s primary outcome measure.
Data analysis
Meta-analyses were performed to estimate the differences between the foot characteristics of participants, with and without KOA, for foot progression angle and peak rearfoot eversion angle. Mean differences (MD) with 95% confidence intervals (95% CI) were calculated. The standard deviation (SD) was extracted or estimated from the standard error of the mean, the 95% CI, P value, or other methods as recommended by the Cochrane Collaboration [17]. Meta-analyses were performed in STATA (16.1) using the ‘meta’ command. The effect sizes of the meta-analyses are reported in degrees.
Results
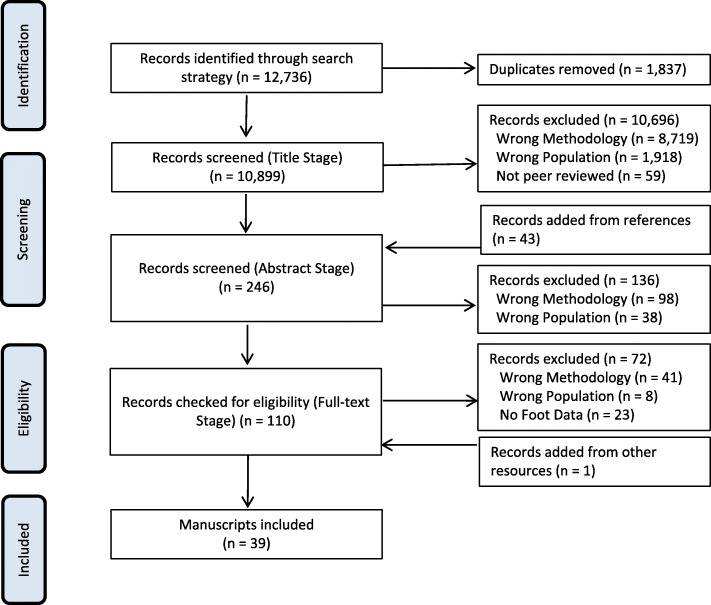
Following the implementation of the outlined search strategy, MeSH search yielded 12,736 articles, of which 1837 were duplicate publications (Fig. 1), leaving 10,899 articles for the title stage. Screening at the title stage excluded 10,696 of these articles, leaving 203 articles eligible for the abstract stage. At the abstract stage, 43 titles were added from reference lists and other sources, making a total of 246 articles eligible for the abstract stage, and 136 articles were excluded. A total of 110 articles were then reviewed at the full-text stage and 72 articles were excluded, while one article matching the eligibility criteria was added in the full-text stage from other sources, leaving 39 articles found to have evaluated foot characteristics and/or mechanics in individuals with KOA. Kappa agreement values between the reviewers were 0.79, 0.79, and 0.73 for the title, abstract, and full-text stage, respectively.
Fig. 1.
PRISMA flow chart diagram of the systematic review process
Study characteristics
The included studies were published between 2006 and 2020 (Table 2). There were 25 observational studies [18–22, 25, 27, 29, 32, 33, 37–41, 43, 45–52, 56] and 14 intervention studies [23, 24, 26, 28, 30, 31, 34–36, 42, 44, 53–55]. The 39 studies included a total of 2260 participants. In the KOA groups, the sample sizes ranged from eight [37] to 123 [42] participants, with a mean study sample size of 57 participants. Twenty-two studies included a control population [18–22, 25, 27, 29, 31, 37–41, 45–47, 49–51, 54, 56], with sample sizes ranging from ten [37] to 80 [18] participants, and a mean control sample size of 17 participants. Thirty-two studies included both genders [18, 19, 21–24, 26–30, 33–35, 37–53, 55], while four studies were limited to women [20, 32, 54, 56]. Three studies failed to report gender characteristics [25, 31, 36].
Table 2.
Study and participants’ characteristics (data reported as mean ± standard deviation)
| No. | Author | Year published | Country | Subjects subgroups | No. of subjects (Men/ Women) | Age (years) | BMI (kg/m2) |
|---|---|---|---|---|---|---|---|
| 1 | Abourazzak et al. [18] | 2014 | Morocco | KOA | 100 (21/79) | 59.68 ± 7.64 | 30.89 ± 4.94 |
| Healthy control | 80 (20/60) | 48.66 ± 9.30 | 28.00 ± 3.81 | ||||
| 2 | Al-Zahrani and Bakheit [19] | 2002 | UK | KOA | 58 (14/44) | 71 ± 8.40 | NR |
| Healthy control | 25 (10/15) | 69 ± 7.29 | NR | ||||
| 3 | Anan et al. [20] | 2015 | Japan | KOA | 20 (0/20) | 69 ± 4.4 | 24.4 ± 2.8 |
| Healthy control | 17 (0/17) | 69.8 ± 4.3 | 21.3 ± 2.7 | ||||
| 4 | Arnold et al. [21] | 2014 | Australia | KOA | 15 (7/8) | 67.0 ± 8.9 | 30.7 ± 6.2 |
| Healthy control | 15 (7/8) | 68.2 ± 9.7 | 25.5 ± 5.3 | ||||
| 5 | Bechard et al. [22] | 2012 | Canada | KOA | 20 (8/12) | 55 ± 8 | 28.9 ± 3.0 |
| Healthy control | 20 (12/8) | 51 ± 8 | 25.9 ± 3.2 | ||||
| 6 | Booij et al. [23] | 2020 | Netherlands | Medial KOA only | 30 (14/16) | 62.7 ± 5.9 | 25.5 ± 2.7 |
| 7 | Butler et al. [24] | 2009 | USA | KOA only | 30 (13/17) | 63.1 ± 6.8 | 33.8 ± 6.9 |
| 8 | Butler et al. [25] | 2011 | USA | Medial KOA | 15 (NR/NR) | 66.2 ± 7.8 | 32.2 ± 7.9 |
| Lateral KOA | 15 (NR/NR) | 65.3 ± 6.4 | 30.4 ± 7.5 | ||||
| Healthy control | 15 (NR/NR) | 56.3 ± 10.7 | 27.8 ± 5.7 | ||||
| 9 | Chapman et al. [26] | 2015 | UK | KOA only | 70 (43/27) | 60.3 ± 9.6 | 30.5 ± ± 4.9 |
| 10 | Chang et al. [27] | 2007 | USA | KOA only | 56 (23/33) | 66.6 ± 8.6 | 29.0 ± 4.2 |
| 11 | Charlton et al. [28] | 2018 | Canada | Medial KOA only | 16 (6/10) | 67.4 ± 9.3 | 24.6 ± 15.1 |
| 12 | Elbaz et al. [29] | 2017 | Israel | KOA | 63 (22/41) | 64.2 ± 8.1 | NR |
| Healthy control | 30 (21/9) | 67.9 ± 8.9 | NR | ||||
| 13 | Erhart-Hledik et al. [30] | 2017 | Canada | Medial KOA only | 10 (9/1) | 65.3 ± 9.8 | 27.8 ± 3.0 |
| 14 | Gardner et al. [31] | 2015 | USA | KOA | 13 (NR/NR) | 56.8 ± 5.2 | 26.6 ± 3.6 |
| Healthy control | 11 (NR/NR) | 50.0 ± 9.7 | 25.9 ± 5.4 | ||||
| 15 | Guler et al. [32] | 2009 | Turkey | KOA only | 115 (0/115) | 62.11 ± 8.72 | 32.91 ± 4.14 |
| 16 | Guo et al. [33] | 2007 | USA | KOA only | 10 (6/4) | 64 ± 8 | 29.0 ± 5.6 |
| 17 | Hinman et al. [34] | 2012 | Australia | KOA only | 73 (28/45) | 63.3 ± 8.4 | 27.7 ± 3.6 |
| 18 | Hinman et al., [35] | 2016 | Australia | KOA only | 81 (39/42) | 63.3 ± 7.9 | 29.7 ± 3.7 |
| 19 | Khan et al. [36] | 2019 | Malaysia | KOA only | 20 (NR) | 61.5 ± 8.63 | NR |
| 20 | Krackow et al. [37] | 2011 | USA | KOA | 8 (4/4) | 59 ± 11.34 | 33.84 ± 6.90 |
| Healthy control | 10 (5/5) | 62.50 ± 4.17 | 28.44 ± 4.23 | ||||
| 21 | Levinger et al. [38] | 2010 | Australia | KOA | 32 (16/16) | 65.84 ± 7.57 | 29.97 ± 5.26 |
| Healthy control | 28 (13/15) | 65.22 ± 11.41 | 25.56 ± 3.95 | ||||
| 22 | Levinger et al. [39] | 2012a | Australia | KOA | 50 (27/23) | 66.4 ± 7.6 | 29.6 ± 5.1 |
| Healthy control | 28 (13/15) | 65.1 ± 11.2 | 25.7 ± 3.9 | ||||
| 23 | Levinger et al. [40] | 2012b | Australia | KOA | 32 (16/16) | 65.8 ± 7.5 | 29.9 ± 5.2 |
| Healthy control | 28 (13/15) | 65.2 ± 11.4 | 25.5 ± 3.9 | ||||
| 24 | Lidtke et al. [41] | 2010 | USA | KOA | 25 (6/19) | 60.2 ± 10.6 | 29.2 ± 4.6 |
| Healthy control | 25 (12/13) | 58.5 ± 9.1 | 26.6 ± 3.3 | ||||
| 25 | Nigg et al. [42] | 2006 | Canada | KOA only | 123 (56/67) | 57.4 ± 2.2 | 29.5 ± 1.6 |
| 26 | Ohi et al. [43] | 2017 | Japan | KOA only | 88 (30/58) | 74.8 ± 7.58 | 24.3 ± 3.54 |
| 27 | Paquette et al. [44] | 2015 | USA | KOA | 13 (6/7) | 62.5 ± 9 | 28.3 ± 6.5 |
| Healthy control | 13 (5/8) | 58.9 ± 8.3 | 23.9 ± 2.6 | ||||
| 28 | Park et al. [45] | 2016 | Canada | KOA | 24 (7/17) | 54 ± 7.3 | 26.1 ± 3.4 |
| Healthy control | 24 (8/16) | 52.4 ± 10.6 | 24.7 ± 3.2 | ||||
| 29 | Reilly et al. [46] | 2006 | UK | KOA | 60 (25/35) | 67.80 ± 8.09 | NR |
| Healthy control | 60 (28/32) | 64.92 ± 12.18 | NR | ||||
| 30 | Reilly et al. [47] | 2009 | UK | Medial KOA | 20 (9/11) | 63 ± 8.7 | NR |
| Healthy control | 20 (4/16) | 56 ± 7.3 | NR | ||||
| 31 | Rutherford et al. [48] | 2008 | Canada | KOA asymptomatic | 50 (32/18) | 53 ± 10 | 26 ± 4 |
| KOA mild to moderate | 46 (20/26) | 60 ± 9 | 31 ± 5 | ||||
| KOA severe | 44 (20/24) | 67 ± 8 | 32 ± 5 | ||||
| 32 | Rutherford et al. [49] | 2010 | Canada | KOA | 17 (10/7) | 56 ± 8.8 | 29.8 ± 6.5 |
| Healthy control | 20 (7/13) | 46.5 ± 7.0 | 25.9 ± 4.8 | ||||
| 33 | Saito et al. [50] | 2013 | Japan | KOA | 50 (10/40) | 75 | NR |
| Elderly control | 44 (8/36) | 74 | NR | ||||
| 34 | Shakoor et al. [51] | 2008 | USA | KOA | 27 (5/22) | 54 ± 12 | 37.8 ± 8.6 |
| Healthy control | 14 (5/9) | 47 ± 14 | 29.8 ± 5.6 | ||||
| 35 | Simic et al. [52] | 2013 | Australia | KOA only | 22 (9/13) | 69.7 ± 9.0 | 28.4 ± 4.8 |
| 36 | Tan et al. [53] | 2020 | Australia | KOA only | 21 (7/14) | 58 ± 8 | 27.0 ± 4.8 |
| 37 | Trombini-Souza et al. [54] | 2011 | Brazil | KOA | 21 (0/21) | 6 5 ± 5 | NR |
| Healthy control | 24 (0/24) | 65 ± 4 | NR | ||||
| 38 | Van Tunen et al. [55] | 2018 | Australia | Medial KOA only | 21 (9/12) | 63.4 ± 7.0 | 29.8 ± 3.6 |
| 39 | Zhang et al. [56] | 2017 | China | KOA | 23 (0/23) | 64.2 ± 6.6 | 23.3 ± 1.9 |
| Healthy control | 23 (0/23) | 62.1 ± 2.4 | 22.6 ± 1.8 |
Abbreviations: KOA knee osteoarthritis, BMI Body Mass Index, NR not reported
Participant characteristics
Participant age
The mean age of the study participants was 61.5 years, ranging from 47 years [51] to 74 years [50] in the control groups, and 53 years [48] to 75 years [50] in KOA groups (Table 2).
Body mass index
In KOA groups, four studies reported a BMI mean of 18.5–24.9 kg/m2 (normal weight) [20, 28, 43, 56]; 19 studies reported participants’ mean BMI of 25–29.9 kg/m2 (overweight) [22, 23, 27, 30, 31, 33–35, 38–42, 44, 45, 49, 52, 53, 55]; eight studies reported the mean BMI of 30–34.9 kg/m2 (grade I obese) [18, 21, 24–26, 32, 37, 48]; and one study reported a mean BMI ≥35 kg/m2 [51] (grade II obese). Seven studies did not report the mean BMI of their participants [19, 29, 36, 46, 47, 50, 54]. In control groups, four studies reported a BMI mean of 18.5–24.9 kg/m2 (normal weight) [20, 44, 45, 56]; 12 studies reported participants’ mean BMI of 25–29.9 kg/m2 (overweight) [18, 21, 22, 25, 31, 37–41, 48, 51] and six studies did not report the mean BMI of their control participants [19, 29, 46, 47, 50, 54].
Participant eligibility criteria
The included studies evaluated foot characteristics and mechanics in those with KOA, yet four studies did not report the KOA diagnostic method used [19, 46, 47, 53]. Thirty-five studies diagnosed KOA severity using the Kellgren-Lawrence (KL) scoring system [18, 20–45, 48–52, 54–56].
Assessment of study quality
Included studies were assessed for their reporting quality using the STROBE checklist criteria (Table 3). The percentages of STROBE criterion met ranged from 42% [19] to 84% [43]. Ten studies were categorized as high-quality studies [21, 25, 27, 35, 42–44, 47, 53, 55], while 29 studies scored less than 65% in relation to the applicable criteria on the STROBE checklist, and were therefore classified as low-quality studies [18–20, 22–24, 26, 28–34, 36–41, 45, 46, 48, 49, 51, 52, 54, 56].
Table 3.
Assessment of study quality using the STROBE checklist
| Item Number | Recommendations | Abourazzak et al., 2014 [18] | Al-zahrani amd Bakheit, 2002 [19] | Anan et al., 2015 [20] | Arnold et al., 2014 [21] | Bechard et al., 2012 [22] | Booij et al., 2020 [23] | Butler et al., 2009 [24] | Butler et al., 2011 [25] | Charlton et al. 2018 [28] | Chang et al., 2007 [27] | Chapman et al., 2015 [26] | Elbaz et al., 2017 [29] | Erhart-Hledik et al., 2017 [30] | Gardner et al., 2015 [31] | Guler et al., 2009 [32] | Guo et al., 2007 [33] | Hinman et al., 2012 [34] | Hinman et al., 2016 [35] | Khan et al., 2019 [36] | Krackow et al., 2011 [37] |
| 1a | Abstract: study’s design in the title or the abstract | No | No | No | Yes | No | No | No | Yes | No | No | No | No | No | No | No | No | No | Yes | Yes | No |
| 1b | Abstract: balanced summary | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2 | Introduction: background and rationale | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3 | Introduction: objectives, including hypotheses | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4 | Methods: study design early in the paper | Yes | No | No | Yes | No | Yes | No | Yes | No | No | No | Yes | Yes | No | No | No | No | Yes | Yes | No |
| 5 | Methods: setting, locations, and relevant dates, recruitment, data collection | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6a | Methods: cohort eligibility criteria, follow-up | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 6a | Methods: case-control: eligibility criteria of cases and controls | Yes | Yes | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 6a | Methods: cross-sectional: eligibility criteria and methods of participants’ selection | NA | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6b | Methods: cohort: number of exposed and unexposed | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | NA | NA |
| 6b | Methods: case-control: matching criteria | Yes | Yes | Yes | NA | Yes | NA | NA | NA | NA | NA | NA | Yes | NA | Yes | NA | NA | NA | NA | NA | NA |
| 7 | Methods: define outcomes, exposures, diagnostic criteria | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8 | Methods: sources of data, methods of assessment (measurement) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9 | Methods: how bias addressed | No | No | No | No | No | No | No | No | No | Yes | Yes | No | No | No | No | No | No | Yes | Yes | No |
| 10 | Methods: power analysis | No | No | No | No | Yes | No | Yes | Yes | No | No | No | No | Yes | No | No | No | No | No | Yes | No |
| 11 | Methods: quantitative variables addressed | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 12a | Methods: statistical methods | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 12b | Methods: statistical subgroups and interactions | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | Yes | Yes |
| 12c | Methods: how missing data addressed | NA | No | NA | No | No | No | NA | No | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 12d | Methods: cohort: how loss to follow-up addressed | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 12d | Methods: case-control: how matching of cases and controls addressed | No | No | No | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | NA | NA |
| 12d | Methods: cross-sectional: sampling strategy | NA | NA | NA | Yes | No | No | Yes | Yes | No | NA | Yes | Yes | No | No | No | Yes | No | NA | No | No |
| 12e | Methods: sensitivity analyses | No | No | No | Yes | No | Yes | No | Yes | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 13a | Results: numbers of individuals at each stage | Yes | No | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| 13b | Results: reasons for non-participation at each stage | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 13c | Results: use of a flow diagram | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 14a | Results: characteristics of study participants | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 14b | Results: number with missing data | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | Yes | No | No |
| 14c | Results: cohort: follow-up time | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 15 | Results: cohort: summary measures over time | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 15 | Results: case-control: summary measures of exposure | Yes | Yes | Yes | NA | NA | NA | NA | NA | NA | NA | NA | No | NA | NA | NA | NA | NA | Yes | NA | NA |
| 15 | Results: cross-sectional: numbers of events or measures | NA | NA | NA | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| 16a | Results: unadjusted estimates | Yes | No | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | No | Yes | No | No | Yes |
| 16b | Results: category boundaries | Yes | No | No | No | No | No | No | No | No | Yes | Yes | No | No | No | No | No | No | NA | No | No |
| 16c | Results: translating relative risk into absolute risk | NA | No | No | Yes | No | NA | No | No | No | No | No | NA | No | NA | NA | No | No | NA | No | No |
| 17 | Results: other analyses (subgroups and interactions, and sensitivity) | Yes | No | No | No | No | No | No | No | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | No | Yes |
| 18 | Discussion: summarise key results with reference to study objectives | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 19 | Discussion: limitations | No | No | Yes | Yes | No | Yes | No | Yes | Yes | No | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes |
| 20 | Discussion: overall interpretation of results considering other relevant evidence | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 21 | Discussion: generalisability of results | No | No | No | Yes | No | No | No | No | No | No | No | No | No | No | No | Yes | Yes | Yes | No | No |
| 22 | Funding: source of funding | No | No | No | No | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes | No |
| % | Total percentage of successfully reported criteria in each study | 61 | 42 | 58 | 72 | 58 | 58 | 53 | 72 | 50 | 66 | 63 | 64 | 59 | 63 | 48 | 53 | 61 | 94 | 61 | 56 |
| Item Number | Recommendations | Levinger et al., 2010 [38] | Levinger et al., 2012a [39] | Levinger et al., 2012 [40] | Lidtke et al., 2010 [41] | Nigg et al., 2006 [42] | Ohi et al., 2017 [43] | Paquette et al., 2015 [44] | Park et al., 2016 [45] | Reilly et al., 2006 [46] | Reilly et al., 2009 [47] | Rutherford et al., 2008 [48] | Rutherford et al., 2010 [49] | Saito et al., 2013 [50] | Shakoor et al., 2008 [51] | Simic et al., 2013 [52] | Tan et al., 2020 [53] | Trombini-Souza et al., 2011 [54] | Van Tunen et al., 2018 [55] | Zhang et al., 2017 [56] | |
| 1a | Abstract: study’s design in the title or the abstract | No | No | No | No | Yes | No | No | No | No | Yes | Yes | No | No | No | No | No | No | Yes | No | |
| 1b | Abstract: balanced summary | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2 | Introduction: background and rationale | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 3 | Introduction: objectives, including hypotheses | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 4 | Methods: study design early in the paper | No | No | No | No | Yes | Yes | No | No | Yes | Yes | Yes | No | No | Yes | No | Yes | No | Yes | No | |
| 5 | Methods: setting, locations, and relevant dates, recruitment, data collection | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 6a | Methods: cohort eligibility criteria, follow-up | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 6a | Methods: case-control: eligibility criteria of cases and controls | NA | Yes | Yes | Yes | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | |
| 6a | Methods: cross-sectional: eligibility criteria and methods of participants’ selection | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | |
| 6b | Methods: cohort: number of exposed and unexposed | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 6b | Methods: case-control: matching criteria | Yes | Yes | Yes | Yes | NA | NA | Yes | Yes | Yes | NA | NA | Yes | Yes | NA | NA | NA | NA | NA | Yes | |
| 7 | Methods: define outcomes, exposures, diagnostic criteria | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | |
| 8 | Methods: sources of data, methods of assessment (measurement) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 9 | Methods: how bias addressed | No | No | No | No | No | Yes | No | No | No | Yes | No | No | No | No | No | No | No | No | No | |
| 10 | Methods: power analysis | No | No | No | No | Yes | No | Yes | No | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | No | |
| 11 | Methods: quantitative variables addressed | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | |
| 12a | Methods: statistical methods | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 12b | Methods: statistical subgroups and interactions | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | |
| 12c | Methods: how missing data addressed | No | No | No | No | Yes | No | No | No | No | No | No | No | No | No | No | No | No | No | No | |
| 12d | Methods: cohort: how loss to follow-up addressed | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 12d | Methods: case-control: how matching of cases and controls addressed | NA | No | No | No | NA | NA | No | No | No | NA | NA | No | No | NA | NA | NA | NA | NA | No | |
| 12d | Methods: cross-sectional: sampling strategy | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | NA | Yes | No | NA | NA | No | NA | Yes | No | No | NA | |
| 12e | Methods: sensitivity analyses | No | No | No | No | No | Yes | Yes | No | Yes | Yes | No | No | No | No | No | Yes | No | Yes | No | |
| 13a | Results: numbers of individuals at each stage | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | |
| 13b | Results: reasons for non-participation at each stage | No | No | No | No | Yes | Yes | No | No | No | No | No | No | No | No | No | No | No | No | No | |
| 13c | Results: use of a flow diagram | No | No | No | No | Yes | Yes | No | No | No | No | No | No | No | No | No | No | No | No | No | |
| 14a | Results: characteristics of study participants | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 14b | Results: number with missing data | No | No | No | No | Yes | Yes | No | No | No | No | No | No | No | No | No | No | No | No | No | |
| 14c | Results: cohort: follow-up time | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 15 | Results: cohort: summary measures over time | NA | NA | NA | NA | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 15 | Results: case-control: summary measures of exposure | NA | NA | NA | NA | NA | NA | No | Yes | Yes | NA | NA | NA | NA | NA | NA | NA | NA | NA | Yes | |
| 15 | Results: cross-sectional: numbers of events or measures | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | |
| 16a | Results: unadjusted estimates | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | No | |
| 16b | Results: category boundaries | No | No | Yes | No | Yes | No | Yes | No | No | Yes | No | No | No | No | No | No | No | No | No | |
| 16c | Results: translating relative risk into absolute risk | NA | No | No | NA | No | NA | No | NA | No | No | No | No | No | No | No | No | No | No | No | |
| 17 | Results: other analyses (subgroups and interactions, and sensitivity) | No | No | No | No | Yes | Yes | No | No | Yes | Yes | Yes | NA | No | Yes | No | No | No | Yes | No | |
| 18 | Discussion: summarise key results with reference to study objectives | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 19 | Discussion: limitations | No | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | |
| 20 | Discussion: overall interpretation of results considering other relevant evidence | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 21 | Discussion: generalisability of results | No | No | No | No | Yes | Yes | Yes | No | Yes | Yes | No | No | No | No | No | No | No | Yes | Yes | |
| 22 | Funding: source of funding | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | |
| % | Total percentage of successfully reported criteria in each study | 56 | 60 | 63 | 62 | 83 | 84 | 69 | 58 | 61 | 81 | 63 | 63 | 52 | 63 | 60 | 69 | 50 | 69 | 48 | |
Abbreviation: NA not applicable
Among the common criterion not met included methods for addressing potential bias, with six meeting this criterion [26, 27, 35, 36, 43, 47]; study generalizability and external validity, with 11 meeting this criterion [27, 33–35, 42–44, 46, 47, 55, 56]; and sample size calculations provided, with 12 meeting this criterion [22, 24, 25, 30, 36, 42, 44, 46, 47, 52–54].
Outcomes measures
Twenty-four studies included measures of participants taken while barefoot [18–21, 23, 27–29, 32, 36–41, 43, 44, 46–49, 51, 54, 55], while 14 were in shod conditions [22, 24–26, 30, 31, 33, 34, 42, 45, 50, 52, 53, 56] (Tables 4, 5 and 6). The majority of the studies (n = 24) used a three-dimensional (3D) motion analysis system and force platforms [19–28, 30, 31, 33, 34, 36, 37, 39, 40, 44, 48, 49, 52–54], whereas the rest (n = 14) used other measurement instruments including pressure plates [41], plantar pressure insoles [56], the Biodex system [42], static footprint [38], foot scanners [50], digital callipers [29], a dynamometer force system [45], a biothesiometer [51], and objective visual and manual measurements including foot posture index (FPI) [18, 47, 53, 55], goniometer [46], and lateral talometatarsal angle [32].
Table 4.
Common foot variables in participants with KOA (data reported as mean ± standard deviation)
| Foot variables | Study, year | Instrument- Shod condition | Results | P-value | |
|---|---|---|---|---|---|
| KOA | Controls | ||||
| Foot Progression Angle or toe-out degree (0) | Bechard et al., 2012 | 3D motion analysis system, force platform- Wearing lab shoes | 6.2 ± 6.1 | 9.4 ± 5.0 | 0.68 |
| Booij et al., 2020 | 3D motion analysis system, force platform- Barefoot | −40.12 ± 4.80 | No controls | NA | |
| Chang et al., 2007 | 3D motion analysis system, force platform- Barefoot | 18.1 ± 8.4 | No controls | NA | |
| Guo et al., 2007 | 3D motion analysis system, force platform- Wearing lab shoes | 2.0 ± 6.8 | No controls | NA | |
| Hinman et al., 2012 | 3D motion analysis system, force platform- Wearing lab shoes | −6.06 ± 5.56 | No controls | NA | |
| Khan et al., 2019 | 3D motion analysis system, force platform- Barefoot | 9.6 ± 3.7 | No controls | NA | |
| Krackow et al., 2011 | 3D motion analysis system, force platform- Barefoot | 8.58 ± 2.37 | 15.36 ± 2.12 | NR | |
| Paquette et al., 2015 | 3D motion analysis system, force platform- Barefoot | 13 ± 4 | 12.2 ± 3.5 | 0.82 | |
| Rutherford et al., 2008 | 3D motion analysis system, force platform- Barefoot | 7.5 ± 5 | 7.3 ± 5 | NA | |
| Rutherford et al., 2010 | 3D motion analysis system, force platform- Barefoot | 6.6 ± 7.3 | 4.9 ± 4.7 | 0.625 | |
| Simic et al., 2013 | 3D motion analysis system- Wearing lab shoes | −4.5 ± 1.5 | No controls | NA | |
| Trombini-Souza et al., 2011 | 3D motion analysis system, force platform- Barefoot | 12.2 ± 6.74 | 13.1 ± 7.90 | 0.71 | |
| Peak rearfoot eversion (0) | Arnold et al., 2014 | 3D motion analysis system, force platform – Barefoot | 5.3 ± 4.2 | 4.5 ± 5.0 | 0.850 |
| Butler et al., 2009 | 3D motion analysis system, force platform- Wearing lab shoes | 3.5 ± 4.3 | No controls | NA | |
| Butler et al., 2011 | 3D motion analysis system, force platform- Wearing lab shoes | 6.2 ± 5.0 | 3.5 ± 2.7 | 0.01* | |
| Chapman et al., 2015 | 3D motion analysis system, force platform- Wearing lab shoes | 3.51 ± 2.77 | No controls | NA | |
| Erhart-Hledik et al., 2017 | 3D motion analysis system, force platform- Wearing lab shoes | 13.9 ± 5.4 | No controls | NA | |
| Levinger et al., 2012 | 3D motion analysis system, force platform- Barefoot | 1.3 ± 5.2 | 2.3 ± 3.9 | NR | |
| Nigg et al., 2006 | Biodex system- Wearing lab shoes | 41.9 | No controls | NA | |
| Peak rearfoot inversion (0) | Arnold et al., 2014 | 3D motion analysis system, force platform- Barefoot | 1.4 ± 4.4 | 1.1 ± 4.2 | 0.708 |
| Levinger et al., 2012 | 3D motion analysis system, force platform- Barefoot | 11.6 ± 5.2 | 14.9 ± 5.0 | NR | |
| Nigg et al., 2006 | Biodex system- Wearing lab shoes | 45.1 | No controls | NA | |
| Pes planus prevalence (%) | Abourazzak et al., 2014 | Visual observation (FPI)- Barefoot | 42 | 22 | 0.03* |
| Guler et al., 2009 | Objective manual testing- Barefoot | 38.3 | No controls | NA | |
| Foot pronation (difference in FPI) | Abourazzak et al., 2014 | Visual observation (FPI)- Barefoot | 1.5 ± 2.68 | 0.72 ± 2.63 | 0.05* |
| Levinger et al., 2010 | Visual observation (FPI)- Barefoot | 2.46 ± 2.18 | 1.35 ± 1.43 | 0.022* | |
*Statistically significant p-value at 95% confidence interval
Abbreviations: 3D three dimensional, FPI foot posture index, KOA knee osteoarthritis, NA not applicable, NR not reported
Table 5.
Static foot variables in participants with KOA (data reported as mean ± standard deviation)
| Study, year of publish | Foot variable (outcome) | Instrument- Shod condition | Results | P-value | |
|---|---|---|---|---|---|
| KOA | Controls | ||||
| Abourazzak et al., 2014 [18] | Prevalence of pes cavus (%) | Visual observation (FPI)- Barefoot | 58 | 77 | 0.004* |
| Elbaz et al., 2017 [29] | Achilles tendon thickness (mm) | Digital caliper- Barefoot | 17.1 ± 3.4 | 15.1 ± 3.1 | 0.009 |
| Guler et al., 2009 [32] | Hallux valgus deformity (%) | Objective manual testing, radiography (x-ray)- Barefoot | 22.60 | No controls | NA |
| Hinman et al., 2016 [35] | FPI (n, %) | Visual observation (FPI)- Barefoot | |||
| Severely supinated | 1 (1) | No controls | NA | ||
| Supinated | 0 (0) | ||||
| Normal | 44 (54) | ||||
| Pronated | 30 (37) | ||||
| Severely pronated | 6 (7) | ||||
| Levinger et al., 2010 [38] | Vertical navicular height | Objective manual testing, static footprint- Barefoot | 0.23 ± 0.03 | 0.24 ± 0.03 | 0.542 |
| Navicular drop | 0.02 ± 0.01 | 0.03 ± 0.01 | 0.019* | ||
| Arch index | 0.26 ± 0.04 | 0.22 ± 0.04 | 0.04* | ||
| Ohi et al., 2017 [43] | Hallux valgus angle (°) | 3D footprint automatic (laser) measurement- Barefoot | 13.6 ± 7.22 | No controls | NA |
| Presence of hallux valgus (%) | 12.5 | ||||
| Navicular height (mm) | 30.1 ± 6.75 | ||||
| Calcaneus angle relative to floor (°) | 1.35 ± 5.09 | ||||
| Rear foot angle (°) | 6.01 ± 3.76 | ||||
| Reilly et al., 2006 [46] | Navicular height in sitting (cm) | Objective manual testing (goniometer)- Barefoot | 5.22 ± 0.94 | 5.28 ± 0.89 | 0.005* |
| Navicular height in standing (cm) | 4.69 ± 0.83 | 4.73 ± 0.98 | 0.003* | ||
| Reilly et al., 2009 [47] | FPI** | Visual observation (FPI)- Barefoot | 7.0 (−2 to 10)** | 1.0 (−4 to 8)** | < 0.001* |
| Ankle dorsiflexion during sitting (°)** | Objective manual testing using goniometer -Barefoot | 9.0 (0 to 32)** | 7.5 (0 to 15)** | < 0.001* | |
| Shakoor et al., 2008 [51] | VPT (volts) | Biothesiometer, AP radiography- Barefoot | |||
| First MTPJ | 15 ± 9.9 | 6.4 ± 3.3 | < 0.001* | ||
| Medial malleolus | 22 ± 11.7 | 12.3 ± 5.2 | 0.001* | ||
| Lateral malleolus | 22.3 ± 10.5 | 10.4 ± 3.2 | < 0.001* | ||
| Tan et al., 2020 [53] | FPI |
Visual observation (FPI)- Midfoot and arch height mobility/arch indices- Barefoot |
3 (1 to 7) | No controls | NA |
| Arch height difference (mm) | 8.8 ± 5.2 | ||||
| Midfoot width difference (mm) | 8.9 ± 3.1 | ||||
| Foot mobility magnitude (mm) | 14.8 ± 7.9 | ||||
| Van Tunen et al., 2018 [55] | FPI (n, %) |
Visual observation (FPI)- Barefoot Foot mobility magnitude calculation Navicular drop test |
|||
| Normal (scores 0 to + 5) | 9 (43) | No controls | NA | ||
| Pronated (scores + 6 to + 9) | 11 (52) | ||||
| Highly pronated (scores greater + 9) | 1 (5) | ||||
| Foot mobility magnitude (mm) | 9.6 ± 3.8 | ||||
| Navicular drop (mm) | 7.6 ± 3.1 | ||||
*Statistically significant p-value at 95% confidence interval
** Data reported as median (interquartile range)
Abbreviations: 3D three-dimensional, FPI foot posture index, KOA knee osteoarthritis, MTPJ metatarsophalangeal joint, NA not applicable, NR not reported, SAI Staheli arch index, VPT Vibratory perception threshold
Table 6.
Dynamic foot variables in participants with KOA (data reported as mean ± standard deviation)
| Study, year of publish | Foot variable (outcome) | Instrument- Shod condition | Results | P-value | |
|---|---|---|---|---|---|
| KOA | Controls | ||||
| Al-Zahrani and Bakheit 2002 [19] | Ankle plantar flexion in stance (°)** | 3D motion analysis system, force platform- Barefoot | 19.01 (15.90 to 22.70)** | 30.88 (23.50 to 35.60)** | < 0.12 |
| Ankle plantar flexion in swing (°)** | 27.76 (17.70 to 26.40)** | 22.74 (15.90 to 22.70)** | < 0.02* | ||
| Ankle moment (pre-swing) (Nm/kg)** | 0.57 (0.36 to 0.78)** | 0.79 (0.61 to 0.91)** | < 0.002* | ||
| Ankle power (pre-swing) (Watt/k.)** | 1.46 (0.53 to 2.31)** | 3.86 (2.91 to 4.58)** | < 0.000* | ||
| Anan et al., 2015 [20] | Maximum ankle plantar flexion moment during STS (Nm/kg) |
3D motion analysis system, force platform- Barefoot |
0.36 ± 0.07 | 0.34 ± 0.07 | 0.343 |
| Mean ankle plantar flexion moment during STS (Nm/kg) | 0.23 ± 0.06 | 0.24 ± 0.08 | 0.685 | ||
| Ankle planter flexion moment impulse during STS (Nms/kg) | 0.47 ± 0.16 | 0.38 ± 0.15 | 0.072 | ||
| Arnold et al., 2014 [21] | Hindfoot conronal plane ROM (o) | 3D motion analysis system, force platform- Barefoot | 10.9 ± 3.4 | 10.9 ± 4.3 | 0.562 |
| Butler et al., 2009 [24] | Rearfoot eversion excursion (o) | 3D motion analysis system, force platform- Wearing lab shoes | 10.1 ± 2.8 | No controls | NA |
| −0.030 ± 0.034 | |||||
| Peak rearfoot eversion moment (Nm/kg*m) | |||||
| Butler et al., 2011 [25] | Peak rearfoot inversion moment (Nm/kg*m) | 3D motion analysis system, force platform- Wearing lab shoes | −0.050 ± | − 0.062 ± | 0.38 |
| Rearfoot eversion excursion (o) | 0.045 | 0.03 | 0.96 | ||
| 10.6 ± 5.6 | 10.2 ± 3.7 | ||||
| Charlton et al. 2018 [28] | Foot rotation angle during natural walking: | 3D motion analysis system- Barefoot | |||
| Ipsilateral foot (°) | −7.8 ± 7.9 | No controls | NA | ||
| Contralateral foot (°) | −8.4 ± 5.7 | ||||
| Gardner et al., 2007 [31] | Planter flexion angle during cycling (o) | 3D motion analysis system, force platform- Wearing lab shoes | −6.0 ± 8.5 | − 8.9 ± 10.7 | 0.834 |
| Ankle eversion during cycling (o) | −6.8 ± 8.5 | −13.2 ± 8.4 | 0.015* | ||
| Internal rotation angle (o) | 8.1 ± 7.1 | 9.2 ± 7.6 | 0.849 | ||
| Guo et al., 2007 [33] | FPA during stair ascent (o) | 3D motion analysis system, force platform- Wearing lab shoes | 2.5 ± 6.6 | No controls | NA |
| FPA during stair descent (o) | 11.3 ± 8.9 | ||||
| Hinman et al., 2012 [34] | COP offset (mm) | 3D motion analysis system, force platform- Wearing lab shoes | −5.6 ± 4.3 | No controls | NA |
| Levinger et al.,2012a [39] | Ankle dorsiflexion (o) | 3D motion analysis system, force platform-Barefoot | 3.6 ± 3.3 | 2.4 ± 2.8 | 0.08 |
| Ankle adduction (0) | 2.8 ± 1.9 | 4.2 ± 2.1 | 0.01* | ||
| Toe clearance sensitivity in ankle (mm/degrees) | −0.1 ± 3.5 | 1.1 ± 4.5 | 0.05* | ||
| Levinger et al., 2012b [40] | Rearfoot frontal plane ROM (o) | 3D motion analysis system, force platform- Barefoot | 10.2 ± 3.3 | 12.5 ± 3.1 | NR |
| Rearfoot transverse plane ROM (o) | 8.8 ± 4.7 | 10.0 ± 4.9 | NR | ||
| Internal rotation (o) | 11.7 ± 6.3 | 15.4 ± 7.9 | NR | ||
| External rotation (o) | 2.9 ± 5.8 | 5.4 ± 6.1 | NR | ||
| Lidtke et al., 2010 [41] | COP index | Plantar pressure plate- Barefoot | −5.87 ± 5.6 | −0.45 ± 3.45 | < 0.001* |
| Nigg et al., 2006 [42] | Ankle plantar flexion (o) | Biodex system- Wearing lab shoes | 50.6 | No controls | NA |
| Ankle dorsiflexion (o) | 22.2 | ||||
| Park et al., 2016 [45] | MVIC of ankle inversion muscle group (N/kg) | Force dynamometer- Wearing lab shoes | 0.62 ± 0.26 | 0.86 ± 0.31 | 0.007* |
| Reilly et al., 2006 [46] | Ankle Plantar flexion in sitting (°) | Objective manual testing (goniometer)- Barefoot | 50.72 ± 11.49 | 52.13 ± 10.94 | 0.788 |
| Ankle dorsiflexion in sitting (°) | 10.07 ± 4.29 | 8.4 ± 3.71 | 0.000* | ||
| Calcaneal angle in sitting (°) | 2.02 ± 2.04 | −0.25 ± 2.93 | 0.000* | ||
| Saito et al., 2013 [50] | Partial foot pressure per body weight (%) | Plantar pressure sensor insoles during walking- Wearing lab shoes | |||
| Heel | 27.1 ± 11.2 | 41.7 ± 8.5 | < 0.001* | ||
| Central | 33.1 ± 11.2 | 16.5 ± 13.8 | < 0.001* | ||
| Metatarsal | 12.4 ± 7.9 | 12.1 ± 6.7 | > 0.001 | ||
| Hallux | 1.5 ± 2.2 | 3.5 ± 3.0 | < 0.001* | ||
| Lateral toes | 1.2 ± 1.7 | 2.5 ± 2.1 | > 0.001 | ||
| Tan et al., 2020 [53] | Peak dorsiflexion angle in stance (°) during walking | 3D motion analysis system, force platform-Wearing lab shoes | 14.9 ± 3.2 | No controls | NA |
| Peak dorsiflexion moment (Nm/kg) during walking | 0.15 ± 0.27 | ||||
| Peak dorsiflexion angle in stance (°) stair ascent / descent. | 9.7 ± 4.4 | ||||
| Peak dorsiflexion moment (Nm/kg) stair ascent / descent. | 1.08 ± 0.22 | ||||
| Weight bearing ankle joint dorsiflexion ROM (cm) | Knee to wall test | 9.1 ± 3.2 | |||
| Zhang et al., 2017 [56] | Contact area (cm2) | Plantar pressure sensor insoles during walking- Wearing lab shoes | |||
| Heel | 28.9 ± 2.9 | 28.6 ± 1.7 | 0.982 | ||
| Midfoot | 41.5 ± 5.8 | 36.5 ± 7.3 | 0.043* | ||
| 1st MTPJ | 13.8 ± 1.6 | 13.1 ± 1.3 | 0.875 | ||
| 2nd MTPJ | 13.6 ± 0.8 | 13.2 ± 1.3 | 0.922 | ||
| 3rd-5th MTPJ | 12.7 ± 0.6 | 12.8 ± 0.3 | 0.986 | ||
| Hallux | 7.1 ± 1.7 | 6.6 ± 1.6 | 0.684 | ||
| Lesser toes | 10.3 ± 1.1 | 10.8 ± 0.4 | 0.988 | ||
| Maximum force (%BW) | |||||
| Heel | 69.5 ± 15.2 | 67.1 ± 11.3 | 0.817 | ||
| Midfoot | 30.3 ± 7.1 | 23.6 ± 7.4 | 0.43 | ||
| 1st MTPJ | 32.3 ± 7.1 | 26.5 ± 6.2 | 0.037* | ||
| 2nd MTPJ | 35.2 ± 9.1 | 30.3 ± 5.1 | 0.041* | ||
| 3rd-5th MTPJ | 17.7 ± 5.4 | 16.7 ± 4.9 | 0.843 | ||
| Hallux | 14.3 ± 6.5 | 13.5 ± 5.6 | 0.901 | ||
| Lesser toes | 12.0 ± 4.7 | 12.6 ± 3.2 | 0.973 | ||
| Plantar pressure (kPa) | |||||
| Heel | 252.9 ± 52.5 | 243.7 ± 52.5 | 0.581 | ||
| Midfoot | 132.8 ± 28.3 | 116.5 ± 30.0 | 0.031* | ||
| 1st MTPJ | 295.1 ± 100.4 | 224.3 ± 62.4 | 0.024* | ||
| 2nd MTPJ | 273.8 ± 103.9 | 244.6 ± 56.1 | 0.183 | ||
| 3rd-5th MTPJ | 156.1 ± 43.1 | 157.9 ± 49.3 | 0.981 | ||
| Hallux | 231.9 ± 77.6 | 219.6 ± 79.4 | 0.531 | ||
| Lesser toes | 139.4 ± 49.4 | 142.9 ± 44.9 | 0.801 | ||
*Statistically significant p-value at 95% confidence interval
** Data reported as median (interquartile range)
Abbreviations: 3D three-dimensional, %BW percent bodyweight, AP anteroposterior, COP centre of pressure, KOA knee osteoarthritis, NA not applicable, NR not reported, MVIC maximum voluntary isometric contraction, MTPJ metatarsophalangeal joint, ROM range of motion, STS sit-to-stand
A wide range of foot characteristics and mechanics were reported in the included studies. The most common foot-related outcomes investigated and reported were foot progression angle (FPA) or toe-out degree (n = 12) [22, 23, 27, 33, 34, 36, 37, 44, 48, 49, 52, 54], and peak rearfoot eversion angle (n = 7) [21, 24–26, 30, 40, 42]. Other outcome measures included the prevalence of pes planus among participants with KOA measured with reference to the medial arch index and the lateral talometatarsal angle [18, 32], and foot pronation measured by foot posture index (FPI) [18, 38]. One study measured partial foot pressure percentage by body weight [50], and another measured plantar load during walking [56].
Foot progression angle (toe-out degree)
Twelve studies measured and reported FPA [22, 23, 27, 33, 34, 36, 37, 44, 48, 49, 52, 54]. Six studies recruited both KOA and control groups and compared the findings between them [22, 37, 44, 48, 49, 54]. The FPA meta-analysis showed no difference between participants with and without KOA (MD: -1.50, 95% CI − 4.20 to 1.21) (Fig. 2). Six other studies recruited KOA participants without a control group [23, 27, 33, 34, 36, 52], and three of these reported negative values for FPA [23, 34, 52], meaning that KOA participants walked with in-toeing gait, while the other three studies reported positive values of FPA [27, 33, 36] [27, 33, 36], meaning that KOA participants tended to walked with a toe-out gait.
Fig. 2.
Forest plot for the differenuihjhjce in FPA during walking between KOA people and healthy controls. 95% CI = 95% Confidence Interval, SD = standard deviation
Peak rearfoot eversion angle
Seven studies measured peak rearfoot eversion angle in individuals with KOA [21, 24–26, 30, 40, 42] using 3D motion analysis systems (in weight bearing position during walking) [21, 24–26, 30, 40], and Biodex (non-weight bearing, in sitting position) [42]. Four studies recruited a KOA group only [24, 26, 30, 42], while three studies compared data to those without KOA [21, 25, 40] (Table 4). A meta-analysis of these studies showed no significant difference in peak rearfoot eversion angle during walking between groups (MD: 0.71, 95%CI − 1.55 to 2.97) (Fig. 3).
Fig. 3.
Forest plot for the difference in peak rearfoot eversion angle during walking between KOA people and healthy controls. 95% CI = 95% Confidence Interval, SD = standard deviation
Foot posture
FPI was reported in six studies [18, 35, 38, 47, 53, 55]. However, the study outcomes were not presented comparably between these studies, limiting the possibilities of meta-analysis. Two studies measured differences in foot posture using FPI in KOA and non-KOA populations [18, 38]. Both of them noted that participants with KOA had statistically significant (P < 0.05) highly pronated foot postures, with a difference of 0.78 [18] and 0.61 [38] between the groups (Table 4). Four additional studies measured FPI in individuals with KOA [35, 47, 53, 55], with the results reported here in Table 5 as they were measured differently, with two reporting results as median and interquartile ranges [47, 53] and two categorising and reporting the prevalence of individuals into categories. The first study categorised individuals into three categories: normal, pronated, or highly (severely) pronated [55], while the other study added two categories: supinated, and severely supinated [35]. The highest prevalence in both studies was in the pronated foot posture category, with 52% of participants (N = 11) in one study [55] and 37% (N = 30) in the other [35] (Table 5).
Pes planus
Two studies reported on the prevalence of pes planus in individuals with KOA. Pes planus was measured with reference to the medial arch index in one study, and it showed a statistically significant greater prevalence of pes planus in participants with KOA (42% vs. 22%) [18]. Another study measured pes planus by the lateral talometatarsal angle, where it was defined as an angle > 4°, and reported that 38.3% of participants with KOA had pes planus [32].
Other outcomes
Other foot characteristics and mechanics measured in individuals with KOA were divided into two categories and reported in two different tables: static foot variables (Table 5) and dynamic foot variables (Table 6). The medial arch of the foot was assessed and reported in four studies using different methods (vertical navicular height, navicular drop, and arch index), with different tools (arch index, static footprint, goniometer, and navicular drop test). Of those four studies, two studies compared the results of the KOA group to a control group [38, 46]. When participants with KOA were compared to those without, they were found to have a more significant navicular drop (0.03 ± 0.01 vs 0.02 ± 0.01), a significantly greater arch index (0.26 ± 0.04 vs 0.22 ± 0.04) [38], and significantly lower navicular height in sitting (5.22 ± 0.94 cm vs 5.28 ± 0.89 cm) [46] and standing (4.69 ± 0.83 cm vs. 4.73 ± 0.98 cm) [46].
Plantar pressure was measured during walking while wearing plantar pressure sensor insoles embedded inside lab shoes in two studies [50, 56]. One study [50] assessed and reported the percentage of partial foot pressure per body part, and reported that plantar pressure was statistically lower in participants with KOA compared to those without KOA in the heel (27.1 ± 11.2% vs. 41.7 ± 8.5%), and hallux (1.5 ± 2.2% vs. 3.5 ± 3.0%), and statistically greater at the midfoot (central) (33.1 ± 11.2% vs. 16.5 ± 13.8%) [50]. In the other study [56], a significantly greater plantar pressure was reported in the midfoot (132.8 ± 28.3 kPa vs. 116.5 ± 30.0 kPa), and the first metatarsophalangeal joint (295.1 ± 100.4 kPa vs. 224.3 ± 62.4 kPa) when compared to a control population [56].
One study [51] investigated the vibratory perception threshold (VPT) in specific foot areas and reported significant deficits in vibratory sensation in participants with KOA. Compared to participants without KOA, those with KOA demonstrated significantly greater VPT in the first metatarsophalangeal joint (15 ± 9.9 V vs. 6.4 ± 3.3 V), medial malleolus (22 ± 11.7 V vs. 12.3 ± 5.2 V), and lateral malleolus (22.3 ± 10.5 V vs. 10.4 ± 3.2 V) [51]. Another study which explored Achilles tendon thickness reported significantly thicker tendons in the KOA group compared to the control [29] (17.1 mm vs. 15.1 mm), with thickness associated positively with KOA severity.
Discussion
The purpose of this review was to evaluate foot characteristics and mechanics in individuals with KOA and compare them to people without KOA where possible. Variations in foot characteristics and mechanics in people with KOA were found in the included studies. These variations included differences in FPA, peak rearfoot eversion angle, pronated foot posture, and incidence of pes planus in people with KOA. Several studies compared foot characteristics and mechanics in individuals with KOA to those without KOA; however measurement techniques and outcome measures were not homogenous across studies. Therefore, meta-analyses were conducted on two foot variables only, FPA and peak rearfoot eversion angle. However, these revealed no statistical difference in FPA or peak rearfoot eversion angle. The results across the included studies were inconsistent, a situation which can be attributed to three main reasons: 1) several studies had no control group without KOA, limiting the ability to report between group differences; 2) studies employed different measurement techniques or methods of reporting, limiting the ability to combine data in meta-analyses; and 3) foot characteristics or mechanics were reported by only one study (e.g., VPT, prevalence of hallux valgus deformity, Achilles tendon thickness), making it impossible to draw robust conclusions. Therefore, further work is needed to fully understand the differences in foot characteristics and mechanics in individuals with KOA.
Results of the present work suggest that the prevalence of pes planus and pronated foot posture is higher among participants with KOA. Zhang et al. (2017) reported significantly greater plantar pressure in the midfoot in those with KOA compared to those without. The increase of midfoot and central plantar pressure aligns with the increased incidence of pes planus [18, 32] and greater foot pronation [18, 38] associated with KOA. Further, the positive association noted between pes planus and lower vertical navicular height [38] may explain the high pressure in the midfoot area and the absence of a medial longitudinal arch in the foot [50]. The greater peak rearfoot eversion angles evident in individuals with KOA [21, 25, 31] also align with the reported FPA differences between those with and without KOA [22, 34, 37, 52, 54], as these measurements are hypothesised to influence each other biomechanically.
As the included studies measured foot characteristics and mechanics in those with KOA at a single time point, it is unclear if foot posture or incidence of pes planus is a cause or effect of KOA. Nonetheless, the presence of the biomechanical foot differences (pronated foot posture, greater peak rearfoot eversion angle, and incidence of pes planus) associated with KOA highlight the importance of the kinetic chain and biomechanical influence of one joint on another, which may indicate that foot characteristics may be related to KOA progression. However, further longitudinal studies are required to confirm this. As foot posture and foot function have previously been associated with knee joint loading [38, 57], a cause of primary progressive KOA [9], it is possible that changing the foot posture or function may be an appropriate intervention for KOA.
Conservative interventions targeting a biomechanical change to address KOA have included foot-related interventions [58, 59]. The most common foot-related interventions used to manage KOA are gait modifications and lateral wedge insoles [58]. Toe-out gait has been widely deployed as a conservative intervention in order to reduce knee adduction moment (KAM) and symptoms in people with KOA [59]. Walking with a greater toe-out angle as a mechanical intervention changes the knee joint load in individuals with KOA, shifting the KAM into a flexion moment and reducing knee pain [60]. Furthermore, a greater toe-out degree during walking has been associated with a reduced likelihood of disease progression in participants with KOA for over 18 months [27]. Therefore, this intervention can be limited to targeting people with KOA who walk with a toe-in gait pattern. However, the findings of this systematic review also revealed a diversity in walking patterns among people with KOA (toe-in vs. toe-out gait); thus, this intervention cannot be applied widely in people with KOA.
Lateral wedge orthoses are another common foot-related intervention for KOA [58]. A recent systematic review and meta-analysis demonstrated a reduction in knee joint load, reported as a significant small reduction in first peak of external KAM (standardized mean difference [SMD]: − 0.19; 95% confidence interval [95% CI] -0.23, − 0.15) and second peak external KAM (SMD -0.25; 95% CI -0.32, − 0.19) with a low level of heterogeneity (I2 = 5 and 30%, respectively) and small but favourable reduction in knee adduction angular impulse during walking in people with KOA (SMD = − 0.14; 95% CI -0.21, − 0.07, I2 = 31%) [58]. However, the biomechanical changes reported as resulting from lateral wedge orthoses were considered minimal, thus limiting the efficacy of this intervention [58]. Furthermore, the impact of this intervention is still unknown for people with KOA who have pronated foot posture as lateral wedge orthoses were reported to significantly increase subtalar joint valgus moment [61]. Therefore, defining foot characteristics and mechanics in individuals with KOA is extremely important, as doing so can play an essential role in selecting the most appropriate foot-related interventions to fit the individual’s own foot characteristics and mechanics.
This systematic review has identified several gaps and areas where future research is needed. Intrinsic foot muscle strength, which affects gait and balance [62], remains an unknown characteristic in the KOA population. Future work evaluating the association between foot muscle strength and KOA may prove beneficial in determining if foot strength or its improvement may be an effective KOA intervention. Further, only one study [51] to date has investigated and reported a loss of vibratory sensation in the foot and ankle with KOA, a measure also affecting gait [63]. Understanding if there is a loss in vibratory sense loss or proprioception as well as how it affects those with KOA may also inform the type of rehabilitation deemed appropriate for this population. It has been suggested that poor neuromuscular control affects injury risk and prevention [64], and neuromuscular control has been associated with KOA severity [65]. Therefore, improving foot neuromuscular control may potentially lessen the risk of knee injury and decrease the impact of KOA.
Strengths and limitations
As with any study, the systematic review and meta-analyses presented here should be evaluated with respect to their strengths and limitations. This review set out a wide range of foot characteristics and mechanics in people with KOA. However, most of the measures were only reported in one or two studies with a small sample of participants, which may limit their generalisability to the wider KOA population. Further, this study has evaluated foot characteristics and mechanics in individuals with KOA and suggested a potential relationship between some of the foot measures and KOA. However, the potential cause and effect relationship of foot characteristics and mechanics outcome measures to KOA is still unknown, as this work has reported foot- related data collected at one time point from observational studies, or data at baseline from intervention studies. Future researchers are advised to investigate the relationship between KOA and foot characteristics and mechanics in more depth via longitudinal studies.
One strength of this study is its robust design, which allowed for the breadth of foot characteristics published to be included in the systematic review and meta-analysis, providing a strong background for researchers to develop longitudinal and intervention studies. However, the wide variety of techniques used to measure similar outcomes prevented the possibility of conducting multiple meta-analyses. Therefore, future studies are advised to develop and follow standardized techniques with which to measure foot characteristics and mechanics in order to facilitate further meta-analyses.
The foot characteristics and mechanics reported in this systematic review were assessed and measured using a range of specific measurements. These could be divided into two categories: 1) laboratory-based measurement (e.g., 3D motion capture, static footprint, force platform, and Biodex); and 2) visual observation and objective manual measurements (e.g., navicular drop test, knee to wall test, FPI, Staheli arch index, and digital caliper). Many of the included studies omitted to provide sufficient details on how the measurements were taken. Moreover, due to the heterogeneity in measurement methods used to investigate foot characteristics and mechanics between the included studies, the process of pooling results for comparison was limited.
One of the limitations identified during this review was the lack of quality in the included studies, as only ten studies attained 65% on the STROBE checklist and could thus be considered high-quality studies. A lower cut-off point of 65% was utilized during the assessment of study quality because foot characteristics and mechanics were not generally the primary outcome measure in the included studies; thus, a cut-off point higher than 65% would not have been achievable by the included studies.
Conclusion
In conclusion, despite the large body of prior research investigating foot characteristics and mechanics in individuals with KOA, many studies lacked a comparison group without KOA. Five foot characteristics and mechanics measures were commonly reported in the included studies (FPA, rearfoot peak eversion angle, peak rearfoot inversion angle, foot posture, and prevalence of pes planus). A more pronated foot posture was noticed in the presence of KOA. Further, of these five common foot characteristics and mechanics, two were of similar design, enabling a meta-analysis to be conducted - FPA and peak rearfoot eversion angle. Meta-analysis of these two variables demonstrated no significant differences between participants with and without KOA. Thus, the implications of the present work suggest a need to adopt and adhere to unified measurement techniques of common foot characteristics and mechanics to make meta-analyses more viable. Lastly, longitudinal studies are needed to identify the potential causal relationship between foot characteristics and mechanics and KOA in people with KOA.
Acknowledgements
The first author (RA) would like to express her great appreciation to all co-authors for their valuable contributions to this work.
Abbreviations
- 3D
Three-dimensional
- BMI
Body mass index
- FPA
Foot progression angle
- FPI
Foot posture index
- KAM
Knee adduction moment
- KL
Kellgren-Lawrence scoring system
- KOA
Knee osteoarthritis
- MD
Mean difference
- mm
Millimetre
- SD
Standard deviation
- SMD
Standardized mean difference
- STROBE
Strengthening the reporting of observational studies in epidemiology
- ROM
Range of motion
- VPT
Vibratory perception threshold
Authors’ contributions
RA received the funds to this work as part of PhD work. RA, JLR, RB, MS contributed to study conception and design. RA, JLR collected the data, applied the eligibility criteria in full-texts stage and extracted the data from the included studies, assessed the included studies for quality (STROBE checklist). AB conducted the meta-analysis. All authors contributed to drafting the manuscript of this work. All authors have read and approved the final manuscript.
Funding
This work was funded by Royal Embassy of Saudi Arabia Cultural Bureau - London, UK.
Availability of data and materials
Dataset generated and analysed during the current study are available from the corresponding author on request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rania N. Almeheyawi, Email: ralmeheyawi@tu.edu.sa
Alessio Bricca, Email: abricca@health.sdu.dk.
Jody L. Riskowski, Email: jlriskowski@gmail.com
Ruth Barn, Email: ruth.barn@gcu.ac.uk.
Martijn Steultjens, Email: martijn.steultjens@gcu.ac.uk.
References
- 1.Cho Y, Kim M, Lee W. Effect of proprioceptive training on foot posture, lower limb alignment, and knee adduction moment in patients with degenerative knee osteoarthritis: a randomized controlled trial. J Phys Ther Sci. 2015;27:4. doi: 10.1589/jpts.272.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the Prevalence of Arthritis and Selected Musculoskeletal Disorders in the United States. Arthritis Rheum. 1998;41(5):778–99. [DOI] [PubMed]
- 3.Sharma L, Dunlop D, Cahue S, Song J, Hayes KW. Quadriceps Strength and Osteoarthritis progression in Malaligned and Lax Knees. Ann Internal Med. 2003;138(8):613–9. [DOI] [PubMed]
- 4.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, Fang F, Schwartz TA, Abbate LM, Callahan LF, Kalsbeek WD, Hochberg MC. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County osteoarthritis project. J Rheumatol. 2007;34(1):172–180. [PubMed] [Google Scholar]
- 5.Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145–1153. doi: 10.1016/j.joca.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthr Cartil. 1995;3(4):261–267. doi: 10.1016/S1063-4584(05)80017-2. [DOI] [PubMed] [Google Scholar]
- 7.Spector TD, Cicuttini F, Baker J, Loughlin J, Hart D. Genetic influences on osteoarthritis in women: a twin study. BMJ (Clinical research ed) 1996;312(7036):940–943. doi: 10.1136/bmj.312.7036.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toivanen AT, Heliövaara M, Impivaara O, Arokoski JP, Knekt P, Lauren H, et al. Obesity, physically demanding work and traumatic knee injury are major risk factors for knee osteoarthritis--a population-based study with a follow-up of 22 years. Rheumatology (Oxford) 2010;49(2):308–314. doi: 10.1093/rheumatology/kep388. [DOI] [PubMed] [Google Scholar]
- 9.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama. 2001;286(2):188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 10.Riskowski J, Dufour AB, Hannan MT. Arthritis, foot pain and shoe wear: current musculoskeletal research on feet. Curr Opin Rheumatol. 2011;23(2):148–155. doi: 10.1097/BOR.0b013e3283422cf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gross KD, Felson DT, Niu J, Hunter DJ, Guermazi A, Roemer FW, Dufour AB, Gensure RH, Hannan MT. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care Res (Hoboken). 2011;63(7):937–944. doi: 10.1002/acr.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):6. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cevallos M, Egger M, Moher D. STROBE (STrengthening the Reporting of OBservational studies in Epidemiology). Guidelines for reporting health research: a user's manual. 2014. p. 169–79.
- 14.Tate RL, Douglas J. Use of reporting guidelines in scientific writing: PRISMA, CONSORT, STROBE. STARD and Other Resources Brain Impairment. 2012;12(1):1–21. [Google Scholar]
- 15.Andrews P, Steultjens M, Riskowski J. Chronic widespread pain prevalence in the general population: a systematic review. Eur J Pain. 2018;22(1):5–18. doi: 10.1002/ejp.1090. [DOI] [PubMed] [Google Scholar]
- 16.Slavin RE. Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol. 1995;48(1):9–18. doi: 10.1016/0895-4356(94)00097-A. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JP, Green S. The Cochrane Collaboration, 2011. 2011. [Google Scholar]
- 18.Abourazzak FE, Kadi N, Azzouzi H, Lazrak F, Najdi A, Nejjari C, et al. A positive association between foot posture index and medial compartment knee osteoarthritis in Moroccan people. Open Rheumatol J. 2014;8:4. doi: 10.2174/1874312901408010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Zahrani K, Bakheit A. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disabil Rehabil. 2002;24(5):275–280. doi: 10.1080/09638280110087098. [DOI] [PubMed] [Google Scholar]
- 20.Anan M, Shinkoda K, Suzuki K, Yagi M, Ibara T, Kito N. Do patients with knee osteoarthritis perform sit-to-stand motion efficiently? Gait & Posture. 2015;41(2):488–492. doi: 10.1016/j.gaitpost.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Arnold J, Mackintosh S, Jones S, Thewlis D. Altered dynamic foot kinematics in people with medial knee osteoarthritis during walking: a cross-sectional study. Knee. 2014;21(6):1101–1106. doi: 10.1016/j.knee.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Bechard DJ, Birmingham TB, Zecevic AA, Jones IC, Giffin JR, Jenkyn TR. Toe-out, lateral trunk lean, and pelvic obliquity during prolonged walking in patients with medial compartment knee osteoarthritis and healthy controls. Arthritis Care Res (Hoboken) 2012;64(4):525–532. doi: 10.1002/acr.21584. [DOI] [PubMed] [Google Scholar]
- 23.Booij MJ, Richards R, Harlaar J, van den Noort JC. Effect of walking with a modified gait on activation patterns of the knee spanning muscles in people with medial knee osteoarthritis. Knee. 2020;27(1):198–206. doi: 10.1016/j.knee.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Butler RJ, Barrios JA, Royer T, Davis IS. Effect of laterally wedged foot orthoses on rearfoot and hip mechanics in patients with medial knee osteoarthritis. Prosthetics Orthot Int. 2009;33(2):107–116. doi: 10.1080/03093640802613237. [DOI] [PubMed] [Google Scholar]
- 25.Butler RJ, Barrios JA, Royer T, Davis IS. Frontal-plane gait mechanics in people with medial knee osteoarthritis are different from those in people with lateral knee osteoarthritis. Phys Ther. 2011;91(8):1235–1243. doi: 10.2522/ptj.20100324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chapman GJ, Parkes MJ, Forsythe L, Felson DT, Jones RK. Ankle motion influences the external knee adduction moment and may predict who will respond to lateral wedge insoles?: an ancillary analysis from the SILK trial. Osteoarthr Cartil. 2015;23(8):1316–1322. doi: 10.1016/j.joca.2015.02.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang A, Hurwitz D, Dunlop D, Song J, Cahue S, Hayes K, Sharma L. The relationship between toe-out angle during gait and progression of medial tibiofemoral osteoarthritis. Ann Rheum Dis. 2007;66(10):1271–1275. doi: 10.1136/ard.2006.062927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charlton JM, Krowchuk NM, Hatfield GL, Guenette JA, Hunt MA. Contralateral limb foot rotation during unilateral toe-in or toe-out walking in people with knee osteoarthritis. Gait & posture. 2018;62:132–134. doi: 10.1016/j.gaitpost.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 29.Elbaz A, Magram-Flohr I, Segal G, Mor A, Debi R, Kalichman L. Association between knee osteoarthritis and functional changes in ankle joint and achilles tendon. The Journal of Foot and Ankle Surgery. 2017;56(2):238–241. doi: 10.1053/j.jfas.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 30.Erhart-Hledik JC, Asay JL, Clancy C, Chu CR, Andriacchi TP. Effects of active feedback gait retraining to produce a medial weight transfer at the foot in subjects with symptomatic medial knee osteoarthritis. J Orthopaedic Res. 2017;35(10):2251–2259. doi: 10.1002/jor.23527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gardner JK, Zhang S, Liu H, Klipple G, Stewart C, Milner CE, et al. Effects of toe-in angles on knee biomechanics in cycling of patients with medial knee osteoarthritis. Clin Biomech (Bristol, Avon) 2015;30(3):276–282. doi: 10.1016/j.clinbiomech.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 32.Guler H, Karazincir S, Turhanoglu AD, Sahin G, Balci A, Ozer C. Effect of coexisting foot deformity on disability in women with knee osteoarthritis. J Am Podiatr Med Assoc. 2009;99(1):23–27. doi: 10.7547/0980023. [DOI] [PubMed] [Google Scholar]
- 33.Guo M, Axe MJ, Manal K. The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait Posture. 2007;26(3):436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 34.Hinman RS, Bowles KA, Metcalf BB, Wrigley TV, Bennell KL. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin Biomech (Bristol, Avon) 2012;27(1):27–33. doi: 10.1016/j.clinbiomech.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 35.Hinman RS, Wrigley TV, Metcalf BR, Campbell PK, Paterson KL, Hunter DJ, Kasza J, Forbes A, Bennell KL. Unloading shoes for self-management of knee osteoarthritis: a randomized trial. Ann Intern Med. 2016;165(6):381–389. doi: 10.7326/M16-0453. [DOI] [PubMed] [Google Scholar]
- 36.Khan SJ, Khan SS, Usman J, Mokhtar AH, Abu Osman NA. Combined effects of knee brace, laterally wedged insoles, and toe-out gait on knee adduction moment and fall risk in moderate medial knee osteoarthritis patients. Prosthetics Orthot Int. 2019;43(2):148–157. doi: 10.1177/0309364618796849. [DOI] [PubMed] [Google Scholar]
- 37.Krackow KA, Mandeville DS, Rachala SR, Bayers-Thering M, Osternig LR. Torsion deformity and joint loading for medial knee osteoarthritis. Gait Posture. 2011;33(4):625–629. doi: 10.1016/j.gaitpost.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 38.Levinger P, Menz HB, Fotoohabadi MR, Feller JA, Bartlett JR, Bergman NR. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res. 2010;3(1):29. doi: 10.1186/1757-1146-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levinger P, Lai DT, Menz HB, Morrow AD, Feller JA, Bartlett JR, et al. Swing limb mechanics and minimum toe clearance in people with knee osteoarthritis. Gait Posture. 2012;35(2):277–281. doi: 10.1016/j.gaitpost.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 40.Levinger P, Menz HB, Morrow AD, Feller JA, Bartlett JR, Bergman NR. Foot kinematics in people with medial compartment knee osteoarthritis. Rheumatology (Oxford) 2012;51(12):2191–2198. doi: 10.1093/rheumatology/kes222. [DOI] [PubMed] [Google Scholar]
- 41.Lidtke RH, Muehleman C, Kwasny M, Block JA. Foot Center of Pressure and Medial Knee Osteoarthritis. J Am Podiatric Med Assoc. 2010;100(3):178–84. [DOI] [PubMed]
- 42.Nigg BM, Emery C, Hiemstra LA. Unstable shoe construction and reduction of pain in osteoarthritis patients. Med Sci Sports and Exercise. 2006;38(10):1701–1708. doi: 10.1249/01.mss.0000228364.93703.53. [DOI] [PubMed] [Google Scholar]
- 43.Ohi H, Iijima H, Aoyama T, Kaneda E, Ohi K, Abe K. Association of frontal plane knee alignment with foot posture in patients with medial knee osteoarthritis. BMC Musculoskelet Disord. 2017;18(1):246. doi: 10.1186/s12891-017-1588-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paquette MR, Klipple G, Zhang S. Greater step widths reduce internal knee abduction moments in medial compartment knee osteoarthritis patients during stair ascent. J Appl Biomech. 2015;31(4):229–236. doi: 10.1123/jab.2014-0166. [DOI] [PubMed] [Google Scholar]
- 45.Park S-K, Kobsar D, Ferber R. Relationship between lower limb muscle strength, self-reported pain and function, and frontal plane gait kinematics in knee osteoarthritis. Clin Biomech. 2016;38:68–74. doi: 10.1016/j.clinbiomech.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 46.Reilly KA, Barker KL, Shamley D, Sandall S. Influence of foot characteristics on the site of lower limb osteoarthritis. Foot Ankle Int. 2006;27(3):206–211. doi: 10.1177/107110070602700310. [DOI] [PubMed] [Google Scholar]
- 47.Reilly K, Barker K, Shamley D, Newman M, Oskrochi GR, Sandall S. The role of foot and ankle assessment of patients with lower limb osteoarthritis. Physiotherapy. 2009;95(3):164–169. doi: 10.1016/j.physio.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 48.Rutherford DJ, Hubley-Kozey CL, Deluzio KJ, Stanish WD, Dunbar M. Foot progression angle and the knee adduction moment: a cross-sectional investigation in knee osteoarthritis. Osteoarthr Cartil. 2008;16(8):883–889. doi: 10.1016/j.joca.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 49.Rutherford DJ, Hubley-Kozey CL, Stanish WD. The neuromuscular demands of altering foot progression angle during gait in asymptomatic individuals and those with knee osteoarthritis. Osteoarthr Cartil. 2010;18(5):654–661. doi: 10.1016/j.joca.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Saito I, Okada K, Nishi T, Wakasa M, Saito A, Sugawara K, Takahashi Y, Kinoshita K. Foot pressure pattern and its correlation with knee range of motion limitations for individuals with medial knee osteoarthritis. Arch Phys Med Rehabil. 2013;94(12):2502–2508. doi: 10.1016/j.apmr.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 51.Shakoor N, Agrawal A, Block JA. Reduced lower extremity vibratory perception in osteoarthritis of the knee. Arthritis Care & Research. 2008;59(1):117–121. doi: 10.1002/art.23241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simic M, Wrigley TV, Hinman RS, Hunt MA, Bennell KL. Altering foot progression angle in people with medial knee osteoarthritis: the effects of varying toe-in and toe-out angles are mediated by pain and malalignment. Osteoarthr Cartil. 2013;21(9):1272–1280. doi: 10.1016/j.joca.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 53.Tan JM, Middleton KJ, Hart HF, Menz HB, Crossley KM, Munteanu SE, Collins NJ. Immediate effects of foot orthoses on lower limb biomechanics, pain, and confidence in individuals with patellofemoral osteoarthritis. Gait & Posture. 2020;76:51–57. doi: 10.1016/j.gaitpost.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 54.Trombini-Souza F, Kimura A, Ribeiro AP, Butugan M, Akashi P, Passaro AC, et al. Inexpensive footwear decreases joint loading in elderly women with knee osteoarthritis. Gait Posture. 2011;34(1):126–130. doi: 10.1016/j.gaitpost.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 55.van Tunen JAC, Paterson KL, Wrigley TV, Metcalf BR, Thorlund JB, Hinman RS. Effect of knee unloading shoes on regional plantar forces in people with symptomatic knee osteoarthritis - an exploratory study. J Foot Ankle Res. 2018;11(1):34. doi: 10.1186/s13047-018-0278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang Z, Wang L, Hu K, Liu Y. Characteristics of plantar loads during walking in patients with knee osteoarthritis. Med Sci Monitor. 2017;23:5714–5719. doi: 10.12659/MSM.905136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Levinger P, Menz HB, Morrow AD, Bartlett JR, Feller JA, Bergman NR. Relationship between foot function and medial knee joint loading in people with medial compartment knee osteoarthritis. J Foot Ankle Res. 2013;6(1):33. doi: 10.1186/1757-1146-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arnold JB, Wong DX, Jones RK, Hill CL, Thewlis D. Lateral wedge insoles for reducing biomechanical risk factors for medial knee osteoarthritis progression: a systematic review and Meta-analysis. Arthritis Care & Research. 2016;68(7):936–951. doi: 10.1002/acr.22797. [DOI] [PubMed] [Google Scholar]
- 59.Simic M, Hinman RS, Wrigley TV, Bennell KL, Hunt MA. Gait modification strategies for altering medial knee joint load: a systematic review. Arthritis care & research. 2011;63(3):405–426. doi: 10.1002/acr.20380. [DOI] [PubMed] [Google Scholar]
- 60.Jenkyn TR, Hunt MA, Jones IC, Giffin JR, Birmingham TB. Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism. J Biomech. 2008;41(2):276–283. doi: 10.1016/j.jbiomech.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 61.Kakihana W, Akai M, Nakazawa K, Takashima T, Naito K, Torii S. Effects of laterally wedged insoles on knee and Subtalar joint moments. Arch Phys Med Rehabil. 2005;86(7):1465–1471. doi: 10.1016/j.apmr.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 62.Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol Ser A Biol Med Sci. 2006;61(8):866–870. doi: 10.1093/gerona/61.8.866. [DOI] [PubMed] [Google Scholar]
- 63.Alfuth M, Rosenbaum D. Effects of changes in plantar sensory feedback on human gait characteristics: a systematic review. Footwear Sci. 2012;4(1):1–22. doi: 10.1080/19424280.2011.653990. [DOI] [Google Scholar]
- 64.Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, et al. Biomechanical measures of neuromuscular control and Valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):10. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 65.Astephen Wilson JL, Deluzio KJ, Dunbar MJ, Caldwell GE, Hubley-Kozey CL. The association between knee joint biomechanics and neuromuscular control and moderate knee osteoarthritis radiographic and pain severity. Osteoarthr Cartil. 2011;19(2):186–193. doi: 10.1016/j.joca.2010.10.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Dataset generated and analysed during the current study are available from the corresponding author on request.