Abstract
Background: Measuring hospital efficiency is one of the tools for determining how to use resources. Considering the necessity of measuring the efficiency in hospitals, the current study was conducted to evaluate the efficiency and its determining factors in the Hospitals affiliated to medical universities in Tehran.
Methods: This was a descriptive-analytical and longitudinal study. In the first stage of the research, the variables affecting the efficiency of hospitals were extracted using the Delphi method. In the second stage, th. Efficiency of 29 public hospitals in Tehran from 2012 to 2016 was calculated using data envelopment analysis techniques. We performed a sensitivity analysis of the efficiency scores by running the DEA model several times using different combinations of input variables. At last, applying the Tobit regression, factors explaining the inefficiencies of hospitals were determined. Data analysis was done by STATA 12 and SPSS 16 software. Significance level of all the tests was set at .05.
Results: In the first stage, 10 input variables and 10 output variables necessary from the mangers' point of view were identified to test efficiency. In the second stage, the mean of hospital efficiency was ascending from 2012 to 2015, and then it descending after 2015. According to the results of sensitivity analysis, despite the variability of technical efficiency during the study period (p<0.0001), the difference between the mean performance scores among different scenarios was not significant (p=0.066). Based on the third stage results, the average length of stay (Beta=-1.60E-12, p=0.030) and educational status (Beta=-2.89E+00, p=0.001) had a significant negative effect on hospitals' efficiency.
Conclusion: The study results indicated that the efficiency changes during the years investigated were significant among Tehran public hospitals. The optimal use of inputs to produce hospital services should be on the agenda of health managers and policymakers.
Keywords: Efficiency, Data envelopment analysis, Tobit regression, Hospital
↑ What is “already known” in this topic:
According to sensitivity analysis approach, prioritized input indices are identified to attract the attention of Iran decision makers to suggest the various solutions for efficiency promotion. However, sensitivity analysis and effective factors on efficiency have been ignored among multiple studies in the field of hospital efficiency.
→ What this article adds:
According to the findings of this study, the average length of stay and the educational status of hospitals have a negative impact on their efficiency. Therefore, implementing policies, such as expanding outpatient services, home health services, paying attention to the needs of the area covered, educating medical students in the field of working efficiency methods, considering the efficiency of hospitals in accreditation measures, using efficiency ratings as performance indicators and designing accurate and integrated database of hospitals, seem necessary.
Introduction
Despite the ever-increasing demand for services in the section of health and medicine, governmental organizations are faced with many financial problems due to budget and resource limitations. Such condition makes these organizations encounter inevitable limitation in the use of financial resources (1). This problem is more important in developing nations like Iran, which have allocated less share of GDP to the health section (in Iran, 6.9%; the global mean, 8.5%) (2). Hospitals are one of the most important economic units in health system of each country (3), as the most share of health resources are consumed in them (2). According to the limited resources, it is necessary to design managerial decision-making strategies to maximize the efficiency and improvement of activities in hospitals to reduce costs (1). Therefore, health and medicine managers use performance studies to lead interferences to reduce rare resources waste (4, 5). It is possible to use accessible resources to offer more services or to develop and improve hospital services quality through preventing and reducing resource waste (6). However, ignoring how to use financial resources and lack of clarity in this field challenge hospital sustainability (7).
From an economic point of view, efficiency is the result of production optimization and resource allocation. To test it, the performance of economic units has to be compared with the potential efficiency of production. Farrell considers 3 types of efficiency: technical efficiency, allocative efficiency, and economic efficiency. Technical efficiency shows the institution's ability to obtain the maximum product from the determined value of inputs and using the minimum inputs to achieve the determined value of the output (8). To test the efficiency of economic institutions, various methods are suggested, which are divided into 2 general groups: parametric and nonparametric (1). The Data Envelopment Analysis (DEA) is a specific nonparametric method and a powerful instrument to measure hospitals' efficiency (9). In addition to comparing efficient units with inefficient ones, this method categorizes them and compares each unit with its best state. Thus, it is possible to suggest applied recommendations to increase the efficiency of each measuring unit (10). Therefore, many studies have used this method in hospitals, including the studies of Joshan et al, Mosaddegh Rad et al, Fazeli et al (11), Askari et al (12), Mohebbifar et al (13), and Esmaili et al (1). Based on the results of these investigations, the mean of technical efficiency is 0.961 and 0.955 in Tehran medical sciences university hospitals after and before evolution design, respectively; this was between 0.584 and 0.998 in Iran hospitals, 0.9 in Ilam medical sciences hospitals, 0.958 in Yazd medical sciences hospitals, 0.943 in Gilan medical sciences hospitals, and 0.924 in Iran social security hospitals. Most of the studies conducted in this field have measured hospitals' efficiency without separating the type of activity. However, it is not appropriate to compare the efficiency of public hospitals with private hospitals, as this comparison would not provide the researcher with a correct view. Therefore, this matter has to be considered in the studies that measure and compare efficiency.
Generally, recognizing affective factors on efficiency- as a collection of rich data related to inputs and outputs- plays an important role in improving the effectiveness and hospital outcomes. It is possible to evaluate the efficiency and effectiveness factors in hospitals and represent a more comprehensive picture of hospitals' performance by identifying these factors (14). However, it is useful to find efficiency is more sensitive to which of these institutions and outputs, as it will help managers select better corrective strategies. Sensitivity analysis is the identification of influential key indices on hospitals' efficiency and investigating their sensitivity to these indices; according to this approach, prioritized input indices are identified to attract the attention of Iran decision makers to suggest the various solutions for efficiency promotion (15, 16). However, sensitivity analysis and effective factors on efficiency have been ignored among multiple studies in the field of hospital efficiency. Thus, it is necessary to conduct a study that measures the efficiency of homogenous hospitals and the 2 mentioned items in hospitals because it will provide policymakers with a broad view in determining strategies to promote efficiency. Therefore, the present study measures efficiency and determines effective factors on the inefficiency of Tehran public hospitals.
Methods
This is a descriptive-analytical and longitudinal study that was conducted in the 2012-2016 in 3 stages. The study population includes all 29 public hospitals in Tehran province, Iran.
Input and output variables were extracted through a Delphi method to measure the efficiency of hospitals. The variables were extracted from the literature review to reach a consensus on them and identify the native variables. Then, a Delphi technique was used in 3 rounds. The study was conducted in the hospitals of the Ministry of Health in Iran, and the participants consisted of 30 hospital managers- based on the classification of education hub in the Ministry of Health- from different cities, such as Alborz, Saveh, Qazvin, Qom, and Hamadan. The extracted hospital efficiency assessment variables were then submitted to the Delphi panel to identify input and output variables used for measuring the efficiency of the hospitals. In the next stage, the variables identified in the first stage were given to the members of the Delphi panel in the format of a questionnaire format to score them based on their importance. Finally, the Delphi panel received a questionnaire, which included questions and ratings by the researcher in the previous stages in order to be reviewed.
Data were analyzed by using interquartile range (IQR) and median. IQR was used to assess the agreement among the panel members. Then, data envelopment analysis (DEA) method was used to evaluate the efficiency of hospitals during 2012-2016. Moreover, the input-orientation approach and variable returns to scale (VRS) model were selected for data analysis.
Data envelopment analysis (DEA):
where: U0 = represents the convexity constant, and its sign shows the returns to scale. If U0 < 0, it specifies increasing returns to the scale; if U0 > 0, it refers to reducing returns to the scale, and if U0 = 0, it represents constant returns to the scale (4).
The number of inputs and outputs about DMUs can affect the efficiency scores.
If the number of DMUs, compared with the number of inputs, is relatively small or if it is very large in comparison with the number of inputs and outputs, the scores can be overestimated. Therefore, it is suggested that the number of DMUs be at least 3 times more of the inputs and outputs variables. In our model, the number of DMUs is more than 3 times greater than the number of inputs and outputs; therefore, it was not a binding constraint for the study. In addition, due to limited access to available information, 4 outputs (number of hospitalized patients, number of outpatients, bed occupancy rate, and number of surgeries) and 4 inputs (number of beds, number of doctors, number of nurses, and number of other staff) were included in the model.
Sensitivity analysis:
Multiple variables in the DEA model may lead to inconsistent results, such as inconsistent efficiency estimates. There is no test to assess the suitability of a particular model specification in DEA. Therefore, a sensitivity analysis of the efficiency scores was conducted by running the DEA model in 4 scenarios, ie, using different combinations of input variables. Besides, different specifications of the DEA models were considered for testing the sensitivity of our main model. Repeated-measures ANOVA was used to analyze the sensitivity and also measure the changes in technical efficiency scores for different scenarios.
Tobit regression: In the third stage, the panel data Tobit model was used to explore the factors affecting the efficiency of hospitals. In this study, the censored Tobit model was used because the dependent variable is censored at zero from below. In order to determine how these factors affect efficiency, DEA efficiency scores were analyzed by regressing them against some hospital characteristics.
In the regression models, when the change range of dependent variable is somehow restricted, the variables that take values on a limited scale are defined as “censored” or “truncated” data. If the observations outside the specified range are systematically excluded from the sample and ultimately lost, they are called “truncated” data. Even if the observations do not have any information on the dependent variable, at least the independent variables could be observed. They are called “censored” data (17). If the observations resulted from the analysis of DEA are >1, then they would not be excluded from the sample, as it was with the truncated data. Hence, they cannot take their values either, and they are censored to 1 (18). In this context, since the dependent variables correspond to 1 can be observed, they can have a censored structure.
Estimating a model with a censored dependent variable by the OLS method leads to biased and inconsistent results in parametric estimations (19). In addition, because DEA scores are a relative indicator and there is a correlation between efficiency scores within the DMUs, the OLS regression is invalid.
(20). Therefore, in this study Tobit regression, was used.
To estimate the parameters, the Maximum Likelihood Estimation (MLE) method is used in the Tobit model. Since the parameters obtained through MLE are nonlinear, the predictions of estimations are performed by iteration. Thus, the Newton-Raphson method was used, as it is less time-consuming and requires less iterations (20, 21).
The basic formula of the panel Tobit used in this study is expressed as follows:
| (1) |
| (2) |
Where subscript idefines the hospital, and subscript t defines the time. Xit is the explanatory variable in the dimension of 1×k, and β is the parameter vector on the dimension of k ×1 (20).
The efficiency score was used as a dependent variable and was run against the independent variables. As for panel analysis, random effects models were used from 2012 to 2016.
The results of DEA in this study were obtained through deep sensitivity analysis with SPSS 16 and the consequences of Panel data Tobit were obtained using STATA 12 programs.
Researchers are skeptical about not disclosing hospital information and maintaining confidentiality principles. Furthermore, the final report of the study was published after the approval and discretion of stakeholders.
Results
Selecting variables
After searching in selected databases and finding articles related to measuring efficiency in hospitals, and removing duplicate studies, and studying the full text of 35 selected articles in Persian and English, 20 potential indices that have been used in most studies were identified through DEA method. After running Delphi for the third time and analyzing the results, 10 variables as input (number of beds, number of intensive care beds, number of full-time staff, number of specialized physicians, number of clinics, hospital condition, and geographical location, value of hospitals capital properties, health medical services tariff, specialized equipment and hospital base) and 10 variables as output (number of hospitalization admittance, bed occupancy, bed circulation, average length of stay, death after 24h, patients satisfaction, number of outpatients admittance, number of urgency referents, the time mean of deciding the future of patients in urgency and patients re-admittance) were selected to measure Iranian Public hospital efficiency using the participants' consensus in Delphi panel.
Measuring efficiency
Four scenarios are considered for hospitals' technical efficiency. In the first scenario, 4 input and output variables were used to measure hospital efficiency based on the DEA model. Table 1 shows hospital efficiency changes during the study period based on the first scenario.
Table 1. The process of changing the technical efficiency of hospitals based on the first scenario.
| Hospital ID | 2012 | 2013 | 2014 | 2015 | 2016 |
| 1 | 0.619 | 0.573 | 0.591 | 0.754 | 0.684 |
| 2 | 0.734 | 0.721 | 0.61 | 0.708 | 0.528 |
| 3 | 0.355 | 0.326 | 0.364 | 0.468 | 0.474 |
| 4 | 0.659 | 0.766 | 0.853 | 1 | 1 |
| 5 | 0.48 | 0.511 | 0.557 | 0.673 | 0.542 |
| 6 | 0.438 | 0.436 | 0.495 | 0.619 | 0.58 |
| 7 | 0.829 | 0.796 | 0.884 | 0.91 | 1 |
| 8 | 1 | 1 | 1 | 1 | 1 |
| 9 | 0.462 | 0.431 | 0.442 | 1 | 0.667 |
| 10 | 0.576 | 0.564 | 0.521 | 0.525 | 0.641 |
| 11 | 0.966 | 1 | 1 | 0.768 | 0.599 |
| 12 | 0.665 | 0.869 | 0.921 | 0.807 | 1 |
| 13 | 0.521 | 0.515 | 0.488 | 0.567 | 0.354 |
| 14 | 0.869 | 0.847 | 0.893 | 1 | 0.928 |
| 15 | 0.453 | 0.549 | 0.576 | 0.591 | 0.474 |
| 16 | 0.398 | 0.432 | 0.45 | 0.571 | 1 |
| 17 | 0.517 | 0.525 | 0.524 | 0.532 | 0.304 |
| 18 | 1 | 1 | 1 | 1 | 1 |
| 19 | 0.386 | 0.51 | 0.604 | 0.87 | 1 |
| 20 | 0.363 | 0.657 | 0.675 | 1 | 1 |
| 21 | 0.81 | 0.797 | 0.662 | 0.746 | 0.814 |
| 22 | 0.944 | 0.91 | 0.553 | 0.621 | 0.429 |
| 23 | 0.863 | 0.845 | 0.772 | 0.858 | 1 |
| 24 | 0.181 | 0.21 | 0.488 | 0.538 | 0.508 |
| 25 | 1 | 1 | 1 | 1 | 1 |
| 26 | 1 | 1 | 0.5 | 0.68 | 0.475 |
| 27 | 0.548 | 0.533 | 0.575 | 0.695 | 0.574 |
| 28 | 0.436 | 0.387 | 1 | 1 | 1 |
| 29 | 0.526 | 0.585 | 0.573 | 1 | 0.56 |
| Mean | 0.641 | 0.665 | 0.675 | 0.776 | 0.729 |
| Standard Deviation | 0.240 | 0.230 | 0.205 | 0.185 | 0.246 |
In the second scenario, the number of outpatients and inpatients and bed occupancy percent were considered as output variables and the number of beds and physicians and nurses were considered as input variables. Based on this scenario, the mean and standard deviation of technical efficiency was 0.620 (0.327), 0.712 (0.181), 0.662 (0.208), 0.649 (0.233), 0.617 (0.241) during study years, respectively.
In the third scenario, the number of outpatients and inpatients and bed occupancy percent were considered as output variables and the number of beds and the number of physicians and other staff were considered as input variables. Based on this scenario, the mean and standard deviation of technical efficiency was 0.576 (0.289) , 0.700 (0.172) , 0.629 (0.203), 0.638 (0.233), and 0.618 (0.236) during study years, respectively.
At last, in the fourth scenario, the number of outpatients and inpatients and bed occupancy percent were considered as output variables and the number of beds and the number of nurses and other staff were considered as input variables. Based on this scenario, the mean and standard deviation of technical efficiency was 0.447 (0.282), 0.728 (0.174), 0.651 (0.204), 0.596 (0.229) ,0.569 (0.229) during study years, respectively.
Sensitivity analysis
ANOVA with repeated measures is the generalized state of paired comparison, except that instead of comparing 1 group in 2 states, 1 group is compared in 2 or more states. When an item can be measured multiple times, this test has to be used to investigate and compare data mean among these several times of measurements. Results of various studies show that Pillai's Trace test is a more suitable test than other tests to measure intergroup effects. According to P values, only time influenced the multivariate model (p<0.001); that is, technical efficiency was changing during the study period. However, different scenarios which have contradictory impact on efficiency scores was not significant (p>0 .05).
After it was revealed that efficiency was changing over the study period, several questions were raised: “Between which times are these changes increase and decrease?” and “Are these differences significant or not?” According to Table 2, differences were significant at all times. For example, there was a significant difference between the mean of efficiency at the beginning of the period (2012) and 1 year after (2013) (p=0.001).
Table 2. Pairwise comparisons.
| (I) time | (J) time |
Mean Difference (I-J) |
Std. Error | Sig.a | 95% CI | |
| Lower Bound | Upper Bound | |||||
| 1 | 2 | -.026* | 0.007 | 0.001 | -0.04 | -0.011 |
| 3 | -.043* | 0.019 | 0.025 | -0.08 | -0.005 | |
| 4 | -.118* | 0.022 | 0 | -0.161 | -0.075 | |
| 5 | 0.018 | 0.031 | 0.55 | -0.042 | 0.079 | |
| 2 | 1 | .026* | 0.007 | 0.001 | 0.011 | 0.04 |
| 3 | -0.017 | 0.017 | 0.318 | -0.051 | 0.017 | |
| 4 | -.092* | 0.021 | 0 | -0.134 | -0.05 | |
| 5 | 0.044 | 0.027 | 0.109 | -0.01 | 0.098 | |
| 3 | 1 | .043* | 0.019 | 0.025 | 0.005 | 0.08 |
| 2 | 0.017 | 0.017 | 0.318 | -0.017 | 0.051 | |
| 4 | -.075* | 0.015 | 0 | -0.104 | -0.046 | |
| 5 | .061* | 0.024 | 0.012 | 0.013 | 0.109 | |
| 4 | 1 | .118* | 0.022 | 0 | 0.075 | 0.161 |
| 2 | .092* | 0.021 | 0 | 0.05 | 0.134 | |
| 3 | .075* | 0.015 | 0 | 0.046 | 0.104 | |
| 5 | .136* | 0.024 | 0 | 0.088 | 0.184 | |
| 5 | 1 | -0.018 | 0.031 | 0.55 | -0.079 | 0.042 |
| 2 | -0.044 | 0.027 | 0.109 | -0.098 | 0.01 | |
| 3 | -.061* | 0.024 | 0.012 | -0.109 | -0.013 | |
| 4 | -.136* | 0.024 | 0 | -0.184 | -0.088 | |
Figure 1 shows efficiency changes during the study period among different scenarios. Efficiency changes were identical and descending in all 4 scenarios.
Fig. 1.
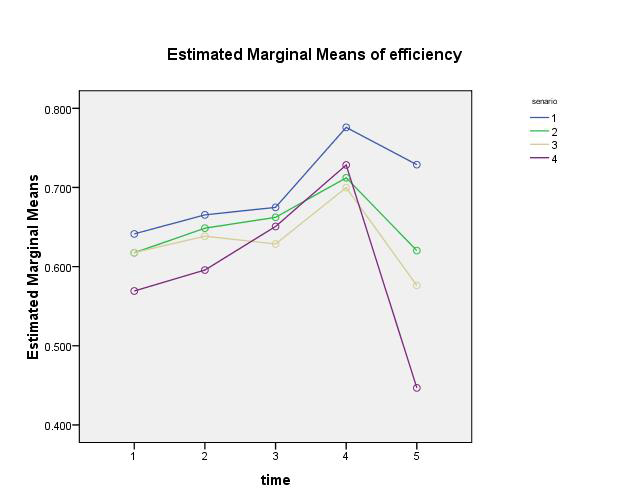
Efficiency changes in different time periods and scenarios
Tobit regression
Although many variables affect the efficiency of hospitals, the educational status of hospitals and the average length of stay were selected according to log-likelihood criteria as variables explaining the inefficiency of hospitals.
Tobit panel regression was employed to test influential factors on hospitals' inefficiency. In order to select between pool methods and panel methods in Tobit model, panel data methods were selected using Chav test and observing F Limer statistics. Then, using the Hasman test and observing the chi-square statistics, the random effect model was selected against the fixed effect. Table 3 shows the results of this investigation. According to the results of Tobit regression, the average length of stay and educational status has a negative and significant effect on hospitals' efficiency.
Table 3. The results of estimating Tobit regression .
| Technical Efficiency | Coefficient | Standard Error | Z statistics | p |
| Educational Status | -2.89E+00 | 9.06E-01 | -3.187 | 0.001 |
| Average length of stay | -1.60E-12 | 7.74E-13 | -2.07 | 0.03 |
| y-intercept | 0.862 | 0.106 | 8.12 | 0 |
| loglikelihood | -22.996 | Hausman | 10.184 | |
| LM Test(F) | 40.064 | |||
| (0.000) | Chi-Square | -0.0702 |
Discussion
In the first stage, 10 variables were selected as input and 10 as output to measure Iran’s public hospitals’ efficiency using participants’ consensus in the Delphi panel. Kabaler et al analyzed Valencia's hospital efficiency. They considered input variables, including the number of physicians and the number of beds and output variables, including the number of consultations, number of successful consultations, and number of surgery interferences. This study has recommended using consumers' satisfaction qualitative variables as output (23). The findings of their study support those of the present study because hospital managers not only considered quantitative indices but also paid attention to qualitative indices, such as patients' satisfaction to measure efficiency. A reliable and common instrument among hospitals is needed to measure qualitative variables and to include these variables into measuring efficiency. Also, managers who have a managerial perspective and knowledge may influence the selection of variables and measure the efficiency of hospitals.
In the second stage, the study investigated different types of efficiency based on different inputs in different scenarios. According to the present study results in 2012, the mean of technical efficiency of hospitals under investigation in the first scenario, which was more complete respecting the number of inputs, was 0.641, and it was 0.665 in 2013, and 0.675 in 2014. In a study aiming at investigating the efficiency of Tehran medical science university hospitals, the technical efficiency was reported to be 0.961 and 0.955 in 2013 and 2014, respectively (24). Also, the value of 0.772 was reported for hospital efficiency in West Azerbaijan medical sciences hospitals in 2013, which was 0.886 in 2014 (25). The mean of technical efficiency in hospitals under investigation was reported to be 0.776 in 2015; the value 0.949 was reported for all Tehran medical sciences hospitals (public and private) in the study of Jafari Pouyan et al (5). This value was 0.919 in Tabriz medical sciences hospitals (26). In 2016, the mean of hospitals' technical efficiency was measured to be 0.726. This value was 0.91 for Tabriz medical sciences hospitals (26). The results of all the mentioned studies show their higher efficiency than the present study. Since the type of hospital's activity will cause a difference in their efficiency, the difference in results may be related to the studied hospitals' homogeneity (all public hospitals). Therefore, it may not be appropriate to compare the efficiency between public and private hospitals. However, the inefficiency of hospitals in the present study may be due to the large number of hospitals and competition in providing services to patients.
Based on the results of the present study, the mean of hospital efficiency under investigation was 0.697 from 2012 to 2016. Consistent with the present study, the review study conducted by Mosaddegh Rad et al reported the mean of 0.584 and 0.998 for Iran hospitals' efficiency until 2016 (27). On the other hand, Gannon (28) has reported the technical efficiency of Ireland public hospitals as 0.96 in his study, which is higher than Iran, and the challenges like expensive diagnostic equipment, location, and hospital type, were among the inefficiency factors in Iran hospitals.
The present study has investigated the effect of different inputs and time on efficiency in the sensitivity analysis of 4 different scenarios. Therefore, by removing other staff from input in the second scenario, the technical changes process turned from increasing to almost fixed trend. Even in the third scenario, after the removal of nurses from inputs, changes turned into a decreasing trend, and in the fourth scenario also by removing physicians from the input list, this trend reported a decrease from 2012 to 2016. But generally, according to the results of statistical tests, despite the variability of technical efficiency during the study (p<0.05), the difference of efficiency scores mean among different scenarios was not significant (p=0.198). The possible reason for the current finding is that physicians and nurses are considered as complementary inputs. As a result, efficiency will not change significantly after deleting or adding one of the inputs.
Findings showed that efficiency changes have been ascending in all 4 scenarios from 2012 to 2015. The study conducted by Hossein Barqazan and Javan also demonstrated that technical efficiency has a positive and weak correlation with evolution design (26). Dargahi et al (29) have shown that Tehran medical sciences university hospitals showed efficiency improvement after operating evolution design from 2012 to 2015. Hashemian’s study (30) reported that the number of efficient university centers has increased, and the number of inefficient centers has decreased after operating evolution design from 2014 to 2015. Nabilou et al have reported improved efficiency in West Azerbaijan medical science university hospitals in 2014 rather than 2013 (25). Some environmental changes can justify the reason for such fluctuation from 2012 to 2015, one of which is operating Health Evolution Design in 2014 was one of the important changes in the health system. This plan increased the number of patients admitted to public hospitals by reducing out-of-pocket payments and increasing service quality. However, 4 scenarios showed a decrease in the efficiency of hospitals in 2016 (0.729). In Joshan’s study, the mean of technical efficiency reduced from 0.961 to 0.955 after operating evolution design (24); efficiency reduction from 2015 to 2016 was due to operating evolution design, which occurred in the Iran Health System with the challenge of extreme costs increase (25). Therefore, university hospital efficiency decreased by continuing the evolution design and not supplying equipment and human force compatible with the referring load increase to hospitals, imposing extra costs resulting from bed occupancy increase, and patients' long hospital stay.
Using more input and output variables for hospital efficiency increases the value of study results (31), so the first scenario was considered as the basis of result analysis in the third stage. Most of the efficiency studies in Iran have followed a specific cognitional method with common errors, and it is possible to apply "group error," and not investigating hospitals’ inefficiency is one of these errors (32). Thus, the present study measured the reasons of hospitals inefficiency using the Tobit panel regression. Also, Campanella et al (33) and Wasim et al (34) have used the Tobit regression to explain the inefficiency of 50 public hospitals in Italy and to identify the reasons influencing Palestine public hospitals' inefficiency. The findings of the current study showed that the average of residence duration and teaching state have negative and significant effects on hospitals' efficiency; therefore, by the increase of patient residence average, hospital inefficiency has increased, and teaching hospitals suffered more from inefficiency. The probable reason for the above result is the low percentage of hospital beds occupancy, which leads to the increase of the average residence of nonurgent patients in hospitals, which increases not only clinical errors on patients but also increases medical costs and imposes high financial pressure on patients and insurance companies. Amir Esmaili et al also reported the average of patients' residence as the second influential factor on the increase of hospital efficiency (35), as Mosaddegh Rad and others considered nonurgent residence among the factors of hospitals’ low efficiency in Iran (13). According to the present study results and other similar studies, developing outpatient services and efficient modeling hospitals is among approaches to increase Iran hospitals’ efficiency.
In contrast to the present study, in the survey conducted by Askari et al (12), the efficiency difference was not statistically significant between teaching and medical hospitals. Although the study by Pourreza et al (12) and another study by Moradali et al (36) showed that teaching hospitals have a positive effect on hospitals' inefficiency, this finding may explain that teaching hospitals are suitable places to obtain knowledge and skill through practical teaching (37), so medical hospitals offer more services than teaching hospitals. As a result, their number of discharge and efficiency in noneducational hospitals will be higher. Moreover, the excessive use of consumables and inexperienced apprentice are possible reasons for the decline in efficiency in teaching hospitals. Therefore, students in medical sciences universities have to be taught in different fields of efficiency, increasing method and health, and medical organizations' productivity. On the other hand, the high average length of stay can be due to the induced demand of providers, limited diagnostic and medical equipment of the hospital (including inadequate specialized services, lack of facilities, broken diagnostic devices), unfavorable economic situation of the patient that prevents the proper use of beds and facilities and as a result increase inefficiency. In addition, improving the quality of services and preventing nosocomial infections can be considered as tools to reduce the average length of stay.
Also, complementary investigations of the present study showed that y-intercept, including some variables which explain hospital inefficiency and have not been included in the model, are significantly influential. Some studies confirm this finding. For example, a study considers active beds as an influential factor in the hospitals' efficiency index. However, comprehensive attention to other inputs such as the number of physicians, number of nurses, bed occupancy day, and management factor and its related issues are necessary to obtain hospital efficiency to the desired level (38). Amir Esmaili et al (35) considered that bed occupancy rate, average patient residence, day bed cost, and bed circulation have the most effect on the increase of hospitals efficiency, respectively; accordingly teaching personnel, employing skilled, and committed human forces, using experienced managers are among important suggestions in efficiency increasing studies. In a review study, items such as the ratio of nurse to patient, physician and trained nurse, patient discharge process, physician presence in the ward, number of paraclinical requests, interdepartmental coordination, and time of first treatment after patient admission as factors affecting average length of stay were identified. These factors were classified into 4 groups: process, service, manpower, and organizational regulation. It seems that the process factor can be controlled and the efficiency of hospitals can be increased by implementing policy interventions. He has categorized these factors into 4 procedural, service, human force, and organizational regulation groups, among which procedural and managerial factors is controllable, and it is possible to promote hospital service quality and to increase hospital efficiency through operating policy-making interferences (38).
Limitations
The main limitation of this study is its environment (its small geographic area), which is limited to hospitals just in one of the cities of Iran.
In addition, there are limitations to using DEA. The limitation of the DEA method is that it works in a definite way, meaning that the results depend entirely on the numerical values of the data set. As the DEA approach compares DMUs, the number and nature of DMUs in the data set can significantly change the results. Another important limitation of this study is the availability of hospital data. Studied hospitals did not have integrated hospital information system; therefore, it could lead to an increase in the number of errors in data collection and analysis.
Conclusion
Hospitals' efficiency was divided into 2 periods: before and after 2014. Based on this study, hospitals' efficiency has an ascending trend before the mentioned year. Hospitals' efficiency has had a significant increasing trend in 2014 and 2015, as the early years of operating evolution design. Then, Health Evolution Design faced had a descending trend after the outbreak of economic problems. The average of inputs has increased in the years studied; and according to hospital efficiency scores, there was an extra increase in optimal inputs from 2012 to 2016. Also, the findings of the current study showed that the average residence duration and teaching state might explain some part of lack of hospital efficiency.
According to the results of this study regarding the negative effect of long patient stay and hospitals’ teaching state, it is recommended to operate offering services policies, such as expanding outpatient services, health services at home, and different classes access to hospitalization medical services, considering the need of the covered region, patients referring system, extra beds in units and developing units. Also, considering the importance of hospitals efficiency as one of the accreditation purposes, it is recommended to measure and consider hospitals’ efficiency in the evaluation process and their accreditation standards and criteria and to use efficiency rate as the hospitals' performance index for their budget and accreditation. However, executing all of this needs designing specialized informational bank to access hospital statistics and information easily to measure Iran hospitals’ efficiency and performance.
Acknowledgement
This study was funded by the Health Management and Economics Research Center at Iran University of Medical Sciences. Thus, the authors gratefully acknowledge the financial support of Health Management and Economics Research Center.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Sarabi Asiabar A, Sharifi T, Rezapour A, Khatami Firouzabadi SMA, Haghighat-Fard P, Mohammad-pour S. Technical eefficiency and its affecting factors in Tehran’s public hospitals: DEA approach and Tobit regression. Med J Islam Repub Iran. 2020 (29 Dec);34:176.
Footnotes
Conflicts of Interest: None declared
Funding: Health Management and Economics Research Center at Iran University of Medical Sciences. (Ethics code: IR. IUMS.REC1396.32011)
References
- 1.Esmaili F, Mehrolhassani M, Barooni M, Goudarzi R. Measurement of Efficiency of Direct Medical Services Affiliated with Iranian Social Security Organization using Data Envelopment Analysis in 2014. Iran J Epid. 2017;12(0):32–9. [Google Scholar]
- 2.Yaghoubi M, Soltani Zarandi M, Rahmati -Najarkolaei F. Factors Affecting Bed Occupancy Rate Based on Multiple-Criteria Decision Analysis (Hierarchical Analysis) in a Military Hospital. J Mil Med. 2017;19(4):344–50. [Google Scholar]
- 3.Ghasemi S, Rajabi Gilan N, Soofi M, Goodarzi G. Measurement of technical efficiency of hospitals of Kermanshah University of medical Science by using non-parametric method of data envelopment analysis. J Rafsanjan Univ Med Sci. 2015;13(9) [Google Scholar]
- 4.Ali M, Debela M, Bamud T. Technical efficiency of selected hospitals in Eastern Ethiopia. Health Econ Rev. 2017;7(1):24. doi: 10.1186/s13561-017-0161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaafaripooyan E, Sharifi T, Emamgholi poor S, Yekani Nejad M, Esmaeili S. Relationship between Accreditation Rank and Technical Efficiency of Hospitals Affiliated to Tehran University of Medical Sciences. J Hosp. 2018;17(2):49–57. [Google Scholar]
- 6.Salehzade R, Ketabi S. Evaluation of relative efficiency of Qom hospitals using data envelopment analysis approach Analytical Hierarchy Process. Health Inf Manag. 2012;8(4):479–89. [Google Scholar]
- 7.Najafi Ghezeljeh T, Rezapour A, Sharifi T, Soleymani Movahed M, Teimourizad A, Yousefi Y. et al. Analysis of the Education Costs of Nursing and Midwifery Students in the Autonomous Hospitals Affiliated to Iran University of Medical Sciences. Iran J Nurs. 2019;32(121):13–25. [Google Scholar]
- 8. Askari A, Charkhkar M. The determination and assessment of the relational efficiency indicators of tehran city and province tax affairs general directorates with data envelopment analysis approach (dea). J Tax res 2015;New Series- 23(26 (75)).
- 9.Rahmani N, Tabatabayee S, Kalhor R. Assessing the role of ownership on changes in total factors using indicators Malm Quist and data envelopment analysis method in Qazvin hospitals. J Paramed Sci. 2013;6(4):300–10. [Google Scholar]
- 10.Nikokar S, Ketabi S, Moazam E. Provide a combined model of data envelopment analysis and a spatial analysis for evaluating the performance of hospital managers. Health Inf Manag. 2011;(Special Issue):601–11. [Google Scholar]
- 11.Fazeli E, Vafaei F, Jamshidi Navid B. Investigation on efficacy of the hospitals affiliated to Ilam University of Medical Sciences by DEA method. J Ilam Univ Med Sci. 2015;23(1):89–97. [Google Scholar]
- 12.Askari R, Goudarzi R, Fallahzadeh H, Zarei B, Dehqani Tafti A. Efficiency Appraisal Of Yazd University Of Medical Science Hospitals By Quantitative Approach Data Envelopment Analysis (DEA) Payavard. 2012;6(3):215–24. [Google Scholar]
- 13.Mosadeghrad A, Esfahani P, Nikafshar M. Hospitals’ Efficiency in Iran: A Systematic Review and Meta-Analysis of Two Decades of Research. Payavard. 2017;11(3):318–31. [Google Scholar]
- 14.Leleu H, Al-Amin M, Rosko M, Valdmanis VG. A robust analysis of hospital efficiency and factors affecting variability. Health Serv Manag Res. 2018;31(1):33–42. doi: 10.1177/0951484817730537. [DOI] [PubMed] [Google Scholar]
- 15.Shahtahmasbi E, Shamsollahi S, Heidary T. Investigation on relative efficiency cargo and passenger transportation of provinces during third development plan and primary years of fourth development plan. J Trans Eng. 2011;2(2) [Google Scholar]
- 16. Issazadeh Roshan Y, Khosravi B. Ranking the telecommunication company of provinces by assessment of data envelopment analysis (dea). J Appl Math 2011;8(3 (30)).
- 17. Davidson R, MacKinnon JG. Econometric theory and methods: Oxford University Press New York; 2004.
- 18.Chilingerian J. Evaluating physician efficiency in hospitals: A multivariate analysis of best practices. Eur J Oper Res. 1995;80(3):548–74. [Google Scholar]
- 19. Greene W. Econometric analysis 5th ed. 2003 Prentice Hall Upper Saddle River. New Jersey.
- 20.Atkinson S, Wilson P. Comparing mean efficiency and productivity scores from small samples: a bootstrap methodology. J Prod Anal. 1995;6(2):137–52. [Google Scholar]
- 21.Ravangard R, Nahid H, Teimourizad A, Jafari A. Factors affecting the technical efficiency of health systems: A case study of Economic Cooperation Organization (ECO) countries (2004–10) Inter J Helth Policy Manag. 2014;3(2):63–69. doi: 10.15171/ijhpm.2014.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goudarzi R. Determining and Investigating the Effective Factors Affecting the Technical Efficiency of Hospitals of Iran University of Medical Sciences Using Data Envelopment Analysis (DEA) and Randomized Frontier Analysis (SFA) during 1997-1999: Iran university of Medical Science. J Health Manag. 2007;9(26):39–44. [Google Scholar]
- 23.Caballer-Tarazona M, Moya-Clemente I, Vivas-Consuelo D, Barrachina-Martínez I. A model to measure the efficiency of hospital performance. Math Comput Model. 2010;52(7-8):1095–102. [Google Scholar]
- 24.Joshan Joshan, shahhoseini R, Ferres Ferres. Technical efficiency of Educational Hospitals Covered by Tehran University of Medical Sciences Using Data Envelopment Analysis Before and After Implementation of Health Transformation Plan. Teb Va Tazkiye. 2017;25(1):37–48. [Google Scholar]
- 25.Nabi-loo B, Salem-safi P, Yousef-zadeh H. Performance Evaluation of Health System Transformation Plan in Hospitals Covered by West Azarbaijan University of Medical Sciences. J Urmia Nurs Midwif Fac. 2017;14(11):905–896. [Google Scholar]
- 26. Hosseini-Barghazan S, Javan A. Evaluation of Technical efficiency of Tabriz University of Medical Sciences Hospitals Before and After Implementation of Health System Development Plan Using Data Envelopment Analysis and Malmquist Index. 11th Student Conference on Health Sciences; Shahid Beheshti University of Medical Sciences, Tehran, Iran2018.
- 27.Mosadeghrad A, Esfahani P, Afshari M. Strategies to improve hospital efficiency in Iran: A scoping review. Payesh. 2019;18(1):7–21. [Google Scholar]
- 28.Gannon B. Testing for variation in technical efficiency of hospitals in Ireland. Econ Soc Rev. 2005;36(3):273–294. [Google Scholar]
- 29.Dargahi H, Darroudi S, Abgoli M. The Study of the Impact of Health System Transformation Plan on Performance Indicators of Hospitals of Tehran University of Medical Sciences: A Case Study Using the Pabon Lasso Model. J Sch Pub Health. 2018;16(3):228–39. [Google Scholar]
- 30.Hashemian M, Mehri M, Ferdousi M, Moeini-pour M, Fatah H. Evaluation and Comparison of Isfahan Province Hospitals Performance in the Years Before and After Implementation of Health System Development Plan (1394-1394) Using Pabon-Lasso Model. J Ilam Univ Med Sci. 2017;25(3):186–200. [Google Scholar]
- 31. Mosadeghrad A, Dehnavi H. Performance Evaluation of Iranian Hospitals: A Systematic Review and Meta-Analysis of Two Decades of Research. Payesh. 2020:603-6015.
- 32.Emam-rezayee A, Barooni M. Hospitals efficiency Analysis in Iran: A Systematic Review. Payesh. 2017;16(1):7–16. [Google Scholar]
- 33.Campanella P, Azzolini E, Izzi A, Pelone F, De Meo C, La Milia D. et al. Hospital efficiency: how to spend less maintaining quality? Ann Ist Super Sanita. 2017;53(1):46–53. doi: 10.4415/ANN_17_01_10. [DOI] [PubMed] [Google Scholar]
- 34.Sultan W, Crispim J. Measuring the efficiency of Palestinian public hospitals during 2010–2015: an application of a two-stage DEA method. BMC Health Serv Res. 2018;18(1):381. doi: 10.1186/s12913-018-3228-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Amir-esmaeili M, Mosleh A, Isfahani P, Emami M. Factors Influencing Hospital efficiency Improvement From the Perspective of Zabul Hospital Managers. J Health Dev. 2012;1(1):56–66. [Google Scholar]
- 36.Ardestani A, Asiabar A, Azar F, Abtahi S. The relationship between hospital managers' leadership style and effectiveness with passing managerial training courses. Med J Islam Repub Iran. 2016;30:465. [PMC free article] [PubMed] [Google Scholar]
- 37.Hatam N, Pourmohammadi K, Bastani P, Javanbakht M. The survey of hospital size effect on technical efficiency in social security hospitals. Razi J Med Sci. 2013;20(108):61–9. [Google Scholar]
- 38.Sadeghian H, Zaboli A. Organizational Factors Affecting Average Patient Stay in Hospital: A Systematic Review of Studies. J Mil Med. 2019;20(6):577–88. [Google Scholar]


