Abstract
To learn anatomy, medical students need to look at body structures and manipulate anatomical structures. Simulation-based education is a promising opportunity for the upgrade and sharing of knowledge. The purpose of this review is to investigate the evaluation of virtual technologies in teaching anatomy to medical students.
Methods: In this review, we searched PubMed, Web of Sciences, Scopus, and Embase for relevant articles in November 2018. Information retrieval was done without time limitation. The search was based on the following keywords: virtual reality, medical education, and anatomy.
Results: 2483 articles were identified by searching databases. Finally, the fulltext of 12 articles was reviewed. The results of the review showed that virtual technologies had been used to train internal human anatomy, ear anatomy, nose anatomy, temporal bone anatomy, surgical anatomy, neuroanatomy, and cardiac anatomy.
Conclusion: Virtual reality, augmented reality, and games can enhance students' anatomical learning skills and are proper alternatives to traditional methods in case of no access to the cadavers and mannequin.
Keywords: Anatomy education, Medical education, Virtual reality, Augmented reality, Mixed reality
↑ What is “already known” in this topic:
Given that medical education is very specialized and extensive, the necessity and importance of using effective new teaching methods is very significant. Improving the practical skills of medical students in the field of anatomy education requires new technologies. Virtual technologies have provided new opportunities for education, especially anatomy.
→ What this article adds:
This study focuses on the impact of virtual technology on anatomy education for medical students. The results of this study can be considered in order to use these technologies for education and its use in the students' curriculum.
Introduction
Simulation is a new method providing a safe and interactive environment for learning and teaching. It provides unique opportunities for understanding and transferring knowledge that improves performance, reduces errors, and better understanding concepts for individuals, especially students (1). Simulation-based education is a promising opportunity for the upgrade and sharing of knowledge (2, 3) that has a positive impact on learning (4, 5). Various forms of technology are available to simulate from 3D computer environments to virtual simulations using wearable sensors (6). Each simulation technology has a unique feature that can be effective. Virtual reality (VR) is an interactive educational tool that simulates the real world and creates a digital environment. Mixed reality (MR) is a combination of real situation and the virtual world. Augmented reality (AR) means that the real world is amplified, added, or enriched with virtual components (7). Simulation allows medical professionals to earn the competency in a non-threatening environment (3). Learning through simulation has been studied in previous studies and has promising results for the training of professionals, the development of surgical skills (3, 8, 9) and teaching anatomy (10-13). To learn anatomy in the medical education curricula, medical students need to look at body structures and manipulate anatomical structures and acquire widespread skills to become expert professionals (14). Anatomy training enables them to properly understand the correct organs, tissues and their exact location (15). Anatomy as the oldest medical science, is one of the essential requirements for medical education. Its learning is based on models and cadaversfor the acquisition of skills, but the lack of adequate infrastructure and equipment provides problems for educators and students (16). Reducing the use of cadaver dissection as an educational tool due to time and cost limitation has an adverse effect on anatomy knowledge (17) but can be improved by using the new educational tool. Technology provides learning environments for medical students more efficiently and easily (12). The use of simulation in the field of surgical anatomy training ensures planning and making decisions in a timely manner that requires proper skill and performance. Virtual simulation provides educational, efficient and effective training program throughout the learning process and reduces the dependence of education on the cadaver (9). The simulation application is a useful tool for medical education, but little information is available about the use of this tool for teaching clinical anatomy to medical students. The purpose of this paper is to investigate the impact of the use of virtual technologies in teaching anatomy to medical students.
Methods
This study is a review of the articles aiming at reviewing the papers and describing the designated features. So we went through this overview in a framework. This study was conducted to answer the question: Are virtual technologies effective in teaching anatomy to medical students?
Search strategy
PubMed, Web of Sciences, Scopus, and Embase were searched for key terms ((((((((((((((((((((Reality, Virtual) OR Virtual Reality, Educational) OR Educational Virtual Realities) OR Educational Virtual Reality) OR Reality, Educational Virtual) OR Virtual Realities, Educational) OR Virtual Reality, Instructional) OR Instructional Virtual Realities) OR Instructional Virtual Reality) OR Realities, Instructional Virtual) OR Reality, Instructional Virtual) OR hybrid reality) OR mixed reality) OR simulation) OR video game)) OR augmented reality)) AND Anatomy) AND Medical Education) and the researchers used the same search words. The search was conducted by the authors. The latest search date was on November 2018. In order to lose the minimum number of articles, the search was conducted without time limitation. We did not search other resources such as the web pages of the journals on anatomy and anatomy education.
Data Extraction
Inclusion criteria: In this review, we tried to study and retrieve the studies in an organized manner, due to the fact that this study is not a systematic review, but its features were used to investigate the information gap. We have included papers in this review that included the following criteria: 1) articles with full text; 2) articles published in English; 3) only articles related to using virtual technology for teaching anatomy to medical students.
Exclusion criteria: 1) Systematic review, review articles, letter, conference proceedings, discussion papers, commentaries, debates, and editorials papers, 2) papers in languages other than English and duplicate were excluded from the study, 3) articles related to medical education to dental and allied health courses, and veterinary medicine were excluded from the study.
Data were extracted from articles according to checklist designed that includes the following items: author, year, aim, application type, target population, education level, domain, and outcome. The review search identified 2483 articles. Duplicates were removed, and 2089 papers were screened by title and abstract. After reviewing the articles, 1995 papers were excluded. 94 full-text articles evaluated for eligibility. Finally, 12 articles were included in this review. The final list of articles was reviewed by two independent authors using full-text papers. In case of disagreement, they reached a consensus through a discussion session. Figure 1 shows the selection process of the studies. Data were analyzed based on descriptive statistics
Fig. 1.
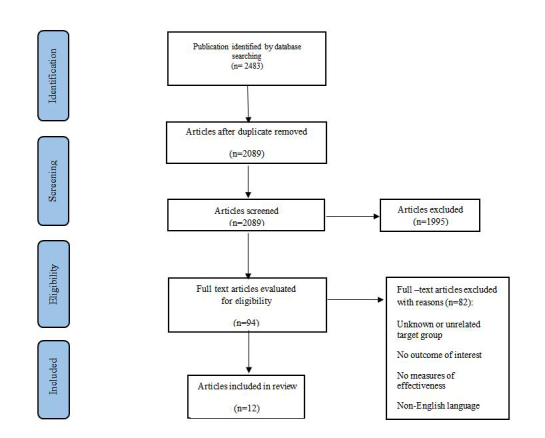
The flow chart of the article search process
Results
The programs used for teaching anatomy are classified as follows: virtual reality robotic surgical simulator, augmented reality, 3-dimensional haptic, virtual reality, 3-dimensional, virtual and augmented reality and 3D tablet, augmented reality magic mirror. As Table 1 shows, all papers point to the effectiveness of the use of virtual technologies for teaching anatomy. The results of the review showed that virtual technologies had been used to train internal human anatomy, ear anatomy, nose anatomy, temporal bone anatomy, surgical anatomy, neuroanatomy, and cardiac anatomy.
Table 1. Variables extracted from papers.
| Author (year) | Year | Aim | Application type | Target Population | Education level | Domain | Outcome measure |
| Nicholson et al. (32) | 2006 | Evaluating the effectiveness of the 3-dimensional anatomy model |
3-dimensional VR |
60 medical students | First-year medical students | Anatomical ear model | The results of the three-dimensional model evaluation in this study were positive and could enhance the learning of medical students. |
| Solyar et al. (33) | 2008 | Evaluation of sinus surgery simulator | Endoscopic sinus surgery simulator | 15 medical student | First-year | Nasal | The results of the study showed that the use of the simulator as a nasal and paranasal sinus anatomy learning tool is helpful. |
| Petersson et al. (20) | 2009 | Evaluation of the 3-dimensional method | Virtual reality | 137 medical student | Second and fifth-semester medical student | Anatomy | The results of the study show the positive effect of using virtual reality in learning anatomy. |
| Seixas-Mikelus et al. (34) | 2010 | Evaluating the use of virtual reality robotic surgical simulator | Virtual reality robotic surgical simulator | 10 medical students and residents | --- | Surgical anatomy | Virtual reality robotic surgical simulator has been reported as an effective tool for enhancing the ability to learn surgical anatomy. |
| Fang et al. (9) | 2014 | Evaluation of 3-dimensional, haptic, virtual reality simulator to teach temporal bone | 3-dimensional, haptic, virtual reality temporal bone simulator | 7 otolaryngology residents and 7 medical students |
Fifth-year of postgraduate & (MD) fifth through the seventh year |
Temporal bone | The results of the study indicated that the simulation technology would increase confidence level, efficiency and reduce educational errors. |
| Küçük et al. (10) | 2016 | Assessing the effectiveness of learning anatomy with mobile augmented reality (mAR) | Augmented reality | 70 medical students | Second-year undergraduate | Neuroanatomy | The success of the students using the mAR applications for learning anatomy was more than the control group and because of flexibility, it has a positive impact on learning. |
| Author (year) | Year | Aim | Application type | Target Population | Education level | Domain | Outcome measure |
| Ma et al. (21) | 2016 | Develop an augmented reality system to education | Augmented reality | 72 students and 7 clinicians | Anatomy student and first-year and final year undergraduate medical students | Human anatomy | The use of the augmented reality interactive system has been reported useful for anatomy education. |
| Moro et al. (12) | 2017 | Evaluating the effectiveness of using VR & AR compared to tablet-based apps for learning anatomy | VR & AR and 3D tablet | 50 Biomedical, health sciences, 5medical student and 4 other faculties | ---- | Skull anatomy | The results of this study revealed virtual reality and augmented reality as an effective learning tool for teaching anatomy content. |
| Rochlen et al. (22) | 2017 | The usability and feasibility assessment of augmented reality to teach needle placement | Augmented Reality | 40 medical students and anesthesiology residents | Third and fourth-year | Internal anatomy | Results of this study indicated augmented reality has been helpful in teaching internal anatomy. |
| Stepan et al. (13) | 2017 | Evaluating the effectiveness of virtual reality in teaching neuroanatomy | Virtual reality simulation | 66 medical students | First-year and 2nd year | Neuroanatomy. | Students' experience of virtual reality was positive in the field of neuroanatomy and increased their motivation for learning. |
| Kugelmann et al. (11) | 2018 | Evaluation of augmented reality magic mirror system for teaching anatomy | Augmented reality magic mirror system | 880 medical students | First-year | Human anatomy | Students in this study referred to the positive impact and potential of using augmented reality. |
| Maresky et al. (35) | 2018 | The effectiveness of VR for the education of cardiac anatomy | virtual reality | Forty-two undergraduate medical students | First-year medical students | Cardiac anatomy | The results of the study showed that virtual reality technology is considered as an effective tool for training anatomy of the heart. |
Figure 2 shows the outcome and effects of virtual technology on students. Sixty-six point six percent of the studies announced the use of virtual technology to increase students' learning ability. Sixteen point six percent of studies considered these technologies useful and fun. Twenty-five percent of the articles point to anatomical knowledge enhancement by virtual reality.
Fig. 2.

The outcome and effects of virtual technology on students
Table 2 shows the applications of virtual technology according to the type of study and field used. Virtual reality technology has been used as the most usable technology for teaching body anatomy, ear, neuroanatomy, and cardiac anatomy. This use of virtual reality technology has been approved by a clinical trial and experimental study. Figure 3 shows the frequency of virtual programs for teaching anatomy. On average, 123 students were trained simultaneously or gradually in each training project. The results of Table 3 show that 78% of the students trained with virtual technologies were the first year of medicine.
Table 2. The applications of virtual technology according to the type of study and field used.
| Domain | Type of study | Type of App | ||||||
|
Augmented reality Magic Mirror |
Virtual and augmented reality and 3D tablet | 3-dimensional virtual reality |
Virtual reality simulators |
3-dimensional, haptic |
Augmented Reality |
virtual reality robotic surgical simulator | ||
| Human anatomy | Experimental |
√ √ |
√ |
√ | ||||
| Skull | Experimental | √ | ||||||
| Anatomical ear model | Randomized controlled trials | √ | ||||||
| Nasal | Randomized controlled trials | √ | ||||||
| Temporal bone | Experimental | √ | ||||||
| Surgical anatomy | Randomized controlled trials | √ | ||||||
| Neuroanatomy | Randomized controlled trials | √ | √ | |||||
| Cardiac anatomy | Randomized controlled trials | √ | ||||||
Fig. 3.
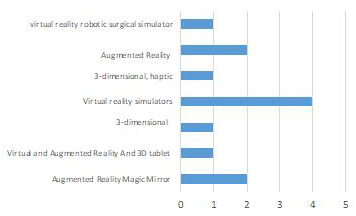
The frequency of virtual programs for teaching anatomy
Table 3. Target population and level of education based on the educational field of anatomy .
| Domain | Target Population | Level |
| Human anatomy | 880 medical students | First-year |
| Human anatomy | 72 students and 7 clinicians |
Anatomy student and first-year and final year undergraduate medical students |
| Skull anatomy | 50 biomedical, health sciences, 5 medical student and 4 other faculties | ---- |
| Anatomical | 60 medical students | First-year medical students |
| Ear model | 15 medical student | First-year |
| Nasal | 7 otolaryngology residents and 7 medical students |
Fifth-year of postgraduate (MD)fifth through seventh-year |
| Temporal bone | 40 medical students and anesthesiology residents | Third and fourth-year |
| Internal anatomy | 10 medical students and residents | --- |
| Surgical | 66 medical students | First-year and 2nd year |
| Anatomy | 70 medical students | Second-year undergraduate |
| Neuroanatomy | 137 medical student | Second and fifth-semester medical student |
| Cardiac anatomy | 42 undergraduate medical students | First-year medical students |
Discussion
Medical education is a continuous and active process that seeks the best way to flexible learn and improve performance. On the other hand, proper learning and teaching will have a positive effect on the quality of care in the future. This continuous cycle depends on effective teaching methods.
Moving to make anatomical information more practical for improving students' skills is one of the essential goals of education (18). The use of virtual technologies can be a promising tool and an effective technique for training in the field of education. Based on the results of Zweifach's study, given the high value of these technologies in medical education, their use is not high. Continuing education using these technologies provides students with similar experiences with less risk (19).
The initial focus of this article was to review studies related to the evaluation of virtual technologies, including virtual reality, augmented reality, mixed reality, simulation for medical anatomy education. The review included a methodological search of related literature databases. In general, 12 articles were evaluated on the use of virtual technologies in various educational fields, including the anatomy of the ears, nose, skull bone, anatomy of surgery, neurology, and cardiac anatomy. The results of the studies showed that medical students attitude towards interactive and simulation programs has been positive and satisfactory for learning anatomy (9, 11, 12, 20). In this study, medical students and residents were considered as target groups. In 50% of articles, the participants were the first-year students. Students who are less skilled needed more time to learn (21). The first-year students had less experience and knowledge about the anatomical structure and they were not aware of the potential damage that they might cause for the structure of anatomy; hence, simulation techniques can be helpful for students with low experience (9). This study showed that learning by simulation programs have a positive effect on the training of anatomy, and there was no difference in the learning quality for different levels of education.
The results of the study showed that five articles used augmented reality technology for teaching anatomy. There was positive feedback for applying this technology for anatomy learning purposes (10-12, 21, 22). Augmented reality can combine the physical environment with the simulation environment, which covers all-round interaction and experience. It has a high potential in influencing health care and the success of medical education and reduces errors in high-risk situations; thus, it has been distinguished from virtual reality application (23). However, the limited experience of using augmented reality in medical education is notable. None of the articles used mixed reality technology for teaching anatomy. It should be noted that this method, along with other virtual methods, may revolutionize medical education and support the learning environment (24). Most of the reviewed articles showed that the use of virtual technologies increases students ability to learn and it is introduced as a useful tool for medical education; in addition, it increases students practical skills in various educational areas (2, 25) as well as reduces their stress level in high-risk situations, such as surgery (26). According to Moro et al., the use of virtual reality and augmented reality technologies were effective in teaching anatomy and raised the level of student satisfaction (12). Furthermore, the use of virtual technologies in medical education enhanced the safety of students allowing them to evaluate their performance. The growth of this technology may lead to real education at various levels of training. On the other hand, the use of cadavers in education put up ethical issues and difficulties in obtaining these materials for training, which should be properly considered (27). Al-Elq's study also showed that simulation-based medical education is hopeful of reducing risks, promoting self-confidence, and patient safety (1). Based on the reviewed works, in each training project, on average, 130 students were trained either simultaneously or gradually. Planning to hold classes and groups for training through virtual technologies can influence educational progress and development. The use of group instructional methods increases students' motivation for learning and, through content simulation, improves their participation and increases the knowledge and learning of anatomy (28). Simulation can be considered as a self-directed learning skill (SDL). SDL skills are more effective in acquiring knowledge than traditional learning methods (29) and are considered as an essential component of critical thinking for learners (30). Although the number of articles studied in this study was small, there were some interesting results showing that the benefits of virtual technologies in achieving educational goals are greater than the traditional methods. According to McGaghie et al. (31), simulation methods are superior to traditional methods for medical education to acquire professional skills and knowledge. Virtual reality enables participants to visualize the internal analytical structure successfully and benefit from the manipulation and interaction of the virtual environment (14).
The few publications associated with the teaching of anatomy through the use of virtual technologies and its types were the limitations of this study. Future works are required to explore the educational aspects of simulation in the field of medical education.
Conclusion
Virtual technology tools in the curriculum can be used without limitations of the clinical program for teaching the anatomy of students of all levels. The practicing and educational conditions created through the virtual world may improve student clinical performance. Our findings suggest that virtual technologies are effective means of teaching anatomy. Medical students and residents, with a variety of experiences and levels of education, found the virtual technologies to be real, enjoyable and satisfying. Virtual reality, augmented reality and games can enhance students' anatomical learning skills and are proper alternatives to traditional methods in case of no access to the cadavers and mannequin. These findings promise the use of virtual technologies as an effective and powerful tool in medical education. A systematic review of the literature on the use of virtual technologies for medical education in various fields such as dentistry, veterinary medicine, and allied health courses is recommended for future research.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Karbasi Z, Niakan Kalhori ShR. Application and evaluation of virtual technologies for anatomy education to medical students: A review. Med J Islam Repub Iran. 2020 (3 Dec);34:163. https://doi.org/10.47176/mjiri.34.163
Footnotes
Conflicts of Interest: None declared
Funding: None
References
- 1.Al-Elq AH. Simulation-based medical teaching and learning. J Fam Commun Med. 2010;17(1):35. doi: 10.4103/1319-1683.68787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alverson DC, Saiki Jr SM, Kalishman S, Lindberg M, Mennin S, Mines J. et al. Medical students learn over distance using virtual reality simulation. Simul Healthc. 2008;3(1):10–5. doi: 10.1097/SIH.0b013e31815f0d51. [DOI] [PubMed] [Google Scholar]
- 3.Vanderbilt AA, Grover AC, Pastis NJ, Feldman M, Granados DD, Murithi LK. et al. Randomized controlled trials: a systematic review of laparoscopic surgery and simulation-based training. Glob J Health Sci. 2015;7(2):310. doi: 10.5539/gjhs.v7n2p310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keri Z, Sydor D, Ungi T, Holden MS, McGraw R, Mousavi P. et al. Computerized training system for ultrasound-guided lumbar puncture on abnormal spine models: a randomized controlled trial. Can J Anaesth. 2015;62(7):777–84. doi: 10.1007/s12630-015-0367-2. [DOI] [PubMed] [Google Scholar]
- 5.Saidin NF, Halim NDA, Yahaya N. A review of research on augmented reality in education: advantages and applications. J Stud Int Educ. 2015;8(13):1. [Google Scholar]
- 6.Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment in medical education. J Gen Intern Med. 2008;23(1):46–9. doi: 10.1007/s11606-007-0283-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gutierrez M, Vexo F, Thalmann D. Stepping into Virtual Reality: Springer-Verlag TELOS; 2008.
- 8.Bharathan R, Vali S, Setchell T, Miskry T, Darzi A, Aggarwal R. Psychomotor skills and cognitive load training on a virtual reality laparoscopic simulator for tubal surgery is effective. Eur J Obstet Gynecol Reprod Biol. 2013;169(2):347–52. doi: 10.1016/j.ejogrb.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Fang TY, Wang PC, Liu CH, Su MC, Yeh SC. Evaluation of a haptics-based virtual reality temporal bone simulator for anatomy and surgery training. Comput Methods Programs Biomed. 2014;113(2):674–81. doi: 10.1016/j.cmpb.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Küçük S, Kapakin S, Göktaş Y. Learning anatomy via mobile augmented reality: effects on achievement and cognitive load. Anat Sci Educ. 2016;9(5):411–21. doi: 10.1002/ase.1603. [DOI] [PubMed] [Google Scholar]
- 11.Kugelmann D, Stratmann L, Nühlen N, Bork F, Hoffmann S, Samarbarksh G. et al. An augmented reality magic mirror as additive teaching device for gross anatomy. Ann Anat. 2018;215:71–7. doi: 10.1016/j.aanat.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ. 2017;10(6):549–59. doi: 10.1002/ase.1696. [DOI] [PubMed] [Google Scholar]
- 13.Stepan K, Zeiger J, Hanchuk S, Del Signore A, Shrivastava R, Govindaraj S. et al. Immersive virtual reality as a teaching tool for neuroanatomy. Int Forum Allergy Rhinol. 2017;7(10):1006–13. doi: 10.1002/alr.21986. [DOI] [PubMed] [Google Scholar]
- 14.Jang S, Vitale JM, Jyung RW, Black JB. Direct manipulation is better than passive viewing for learning anatomy in a three-dimensional virtual reality environment. Comput Educ. 2017;106:150–65. [Google Scholar]
- 15.Singh R, Tubbs RS, Gupta K, Singh M, Jones DG, Kumar R. Is the decline of human anatomy hazardous to medical education/profession?—A review. Surg Radiol Anat. 2015;37(10):1257–65. doi: 10.1007/s00276-015-1507-7. [DOI] [PubMed] [Google Scholar]
- 16.Ocak MA, Topal AD. Blended learning in anatomy education: a study investigating medical students' perceptions. Eurasia J Math Sci Technol Educ. 2015;11(3) [Google Scholar]
- 17.Bergman EM, Verheijen IW, Scherpbier AJ, Van der Vleuten CP, De Bruin AB. Influences on anatomical knowledge: The complete arguments. Clin Anat. 2014;27(3):296–303. doi: 10.1002/ca.22341. [DOI] [PubMed] [Google Scholar]
- 18.Yaghoubi M, Charkhat Gorgich EA, Karimi E, Hosseini ZS, Sabeti N, Dehghan AR. et al. The viewpoint of Medical Students on the Importance of Clinical Anatomy Education. Future Med Educ J. 2019;9(3):49–54. [Google Scholar]
- 19.Zweifach SM, Triola MM. Extended Reality in Medical Education: Driving Adoption through Provider-Centered Design. Digit Biomark. 2019;3(1):14–21. doi: 10.1159/000498923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petersson H, Sinkvist D, Wang C, Smedby Ö. Web‐based interactive 3D visualization as a tool for improved anatomy learning. Anat Sci Educ. 2009;2(2):61–8. doi: 10.1002/ase.76. [DOI] [PubMed] [Google Scholar]
- 21.Ma M, Fallavollita P, Seelbach I, Von Der Heide AM, Euler E, Waschke J. et al. Personalized augmented reality for anatomy education. Clin Anat. 2016;29(4):446–53. doi: 10.1002/ca.22675. [DOI] [PubMed] [Google Scholar]
- 22.Rochlen LR, Levine R, Tait AR. First person point of view augmented reality for central line insertion training: A usability and feasibility study. Simul Healthc. 2017;12(1):57. doi: 10.1097/SIH.0000000000000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barsom E, Graafland M, Schijven M. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016;30(10):4174–83. doi: 10.1007/s00464-016-4800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Antoniou PE, Dafli E, Arfaras G, Bamidis PD, editors. Versatile mixed reality educational spaces-a medical education implementation case. 2016 15th International Conference on Ubiquitous Computing and Communications and 2016 International Symposium on Cyberspace and Security (IUCC-CSS); 2016: IEEE.
- 25.Grantcharov TP, Kristiansen V, Bendix J, Bardram L, Rosenberg J, Funch‐Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91(2):146–50. doi: 10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- 26.Bernardo A. Virtual reality and simulation in neurosurgical training. World Neurosurg. 2017;106:1015–29. doi: 10.1016/j.wneu.2017.06.140. [DOI] [PubMed] [Google Scholar]
- 27.Corrêa CG, Machado MAdAM, Ranzini E, Tori R, Nunes FdLS. Virtual Reality simulator for dental anesthesia training in the inferior alveolar nerve block. J Appl Oral Sci. 2017;25(4):357–66. doi: 10.1590/1678-7757-2016-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burgess AW, Ramsey‐Stewart G, May J, Mellis C. Team‐based learning methods in teaching topographical anatomy by dissection. ANZ J Surg. 2012;82(6):457–60. doi: 10.1111/j.1445-2197.2012.06077.x. [DOI] [PubMed] [Google Scholar]
- 29.Murad MH, Coto‐Yglesias F, Varkey P, Prokop LJ, Murad AL. The effectiveness of self‐directed learning in health professions education: a systematic review. Med Educ. 2010;44(11):1057–68. doi: 10.1111/j.1365-2923.2010.03750.x. [DOI] [PubMed] [Google Scholar]
- 30.Benedict N, Schonder K, McGee J. Promotion of self-directed learning using virtual patient cases. Am J Pharm Educ. 2013;77(7):151. doi: 10.5688/ajpe777151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGaghie WC, Issenberg SB, Cohen MER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicholson DT, Chalk C, Funnell WRJ, Daniel SJ. Can virtual reality improve anatomy education? A randomised controlled study of a computer‐generated three‐dimensional anatomical ear model. Med Educ. 2006;40(11):1081–7. doi: 10.1111/j.1365-2929.2006.02611.x. [DOI] [PubMed] [Google Scholar]
- 33.Solyar A, Cuellar H, Sadoughi B, Olson TR, Fried MP. Endoscopic Sinus Surgery Simulator as a teaching tool for anatomy education. Am J Surg. 2008;196(1):120–4. doi: 10.1016/j.amjsurg.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 34.Seixas-Mikelus SA, Adal A, Kesavadas T, Baheti A, Srimathveeravalli G, Hussain A. et al. Can image-based virtual reality help teach anatomy? J Endourol. 2010;24(4):629–34. doi: 10.1089/end.2009.0556. [DOI] [PubMed] [Google Scholar]
- 35.Maresky HS, Oikonomou A, Ali I, Ditkofsky N, Pakkal M, Ballyk B. Virtual reality and cardiac anatomy: Exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin Anat. 2019;32(2):238–43. doi: 10.1002/ca.23292. [DOI] [PubMed] [Google Scholar]


