Abstract
Global processes, such as climate change, frequent and distant travelling and population growth, increase the risk of viral infection spread. Unfortunately, the number of effective and accessible medicines for the prevention and treatment of these infections is limited. Therefore, in recent years, efforts have been intensified to develop new antiviral medicines or vaccines. In this review article, the structure and activity of the most promising antiviral cyanobacterial products are presented. The antiviral cyanometabolites are mainly active against the human immunodeficiency virus (HIV) and other enveloped viruses such as herpes simplex virus (HSV), Ebola or the influenza viruses. The majority of the metabolites are classified as lectins, monomeric or dimeric proteins with unique amino acid sequences. They all show activity at the nanomolar range but differ in carbohydrate specificity and recognize a different epitope on high mannose oligosaccharides. The cyanobacterial lectins include cyanovirin-N (CV-N), scytovirin (SVN), microvirin (MVN), Microcystis viridis lectin (MVL), and Oscillatoria agardhii agglutinin (OAA). Cyanobacterial polysaccharides, peptides, and other metabolites also have potential to be used as antiviral drugs. The sulfated polysaccharide, calcium spirulan (CA-SP), inhibited infection by enveloped viruses, stimulated the immune system’s response, and showed antitumor activity. Microginins, the linear peptides, inhibit angiotensin-converting enzyme (ACE), therefore, their use in the treatment of COVID-19 patients with injury of the ACE2 expressing organs is considered. In addition, many cyanobacterial extracts were revealed to have antiviral activities, but the active agents have not been identified. This fact provides a good basis for further studies on the therapeutic potential of these microorganisms.
Keywords: cyanobacteria, antiviral metabolites, lectins, polysaccharides
1. Introduction
Viruses and Viral Infections—A Global Problem
Viruses are obligatory parasites composed of nucleic acids (DNA or RNA) packed in a protein capsid, in some cases enveloped with a lipid bilayer. The great diversity of viral species makes it difficult to unequivocally classify them into related groups. For that reason, several ‘general’ classification systems were introduced [1,2]. With respect to the genetic material, viruses can be classified as DNA, RNA, or RNA/DNA viruses. Other classifications are based on morphological features and include enveloped and non-enveloped viruses, e.g., the Baltimore classification sorts viruses into groups based on the RNA production manner [2,3].
In the 21st century, the emergence of several viral species has been observed in humans, including Ebola, Zika, Middle East respiratory syndrome (MERS), severe acute respiratory syndrome (SARS), influenza, and Nipah virus [4,5]. The majority of these species emerge in humans due to the zoonotic events, when animal viruses unknown to our immune system cross the species border and manage to adapt to the new host [6]. In some cases, the geographic distribution of these species is limited to restricted areas (e.g., MERS-CoV), while other infections (e.g., influenza) spread throughout the globe [6,7,8,9]. With global processes, such as climate change, frequent and distant travelling, rapid population growth, and substandard sanitation as well as interactions with animals and transfer of insect vectors into new areas, there is an increased risk for transmission of viral infections. For example, the Aedes mosquitoes played a key role in the spread of dengue virus (DENV) epidemic events in tropical and subtropical regions of Asia (70%), Africa, the Americas, and Oceania [10]. The number of DENV infections that occur annually was estimated to be 390 million [11]. The Aedes mosquito also transmits such infections as Chikungunya virus, Zika virus (ZIKV), Yellow Fever virus (YFV) and Rift Valley fever virus (RVFV) [12].
The management of viral infections, while lacking effective prevention or mitigation tools, generates costs and has serious impacts on the economy and social life. The recent COVID-19 pandemic affected all economic sectors, the health system, education, social mobility, sport, and many other areas of human activities [13]. Unfortunately, effective protection by vaccinations is available only for selected viral species [14,15]. Further, the development of effective drugs is a long and tedious process that frequently ends up being a failure. In 2016, the list of antiviral agents contained only 90 approved drugs for the treatment of 22 human infectious diseases [16]. The low number of developed drugs is linked with the aforementioned diversity of viral species, and consequent lack of broad-spectrum antivirals, as seen for the bacteria. The rapid generation of the escape mutants further hampers the process.
Existing antiviral therapies target different steps of viral infection, from adsorption and penetration of the host cell, through uncoating and replication of nucleic acids, to viral assembly and release [17]. Unfortunately, as viral machinery is tightly fitted to the cellular microenvironment, antiviral agents often not only inhibit the viral infection but also affect the host metabolic processes. There are many other issues to be overcome in the development of effective antiviral therapeutics. These include the variable nature of viral genomes (high rate of mutation and recombination of RNA viruses), yielding rapid development of resistance towards currently used antiviral agents [18].
The most effective way to rapidly identify antiviral compounds is a high-throughput screening of libraries containing existing drugs or random molecules. Such an analysis yields potential drug candidates, but may also provide valuable data for, e.g., QSAR (quantitative structure-activity relationship) lead optimization. However, these efforts are usually cost-ineffective and limited by the available compound or fragment libraries. In the search for new antivirals, the natural products, with their diverse and unique structures and mechanisms of action, have always constituted an important source of inspiration. The nucleoside spongouridine produced by the marine sponges Cryptotethya crypta is one of the examples [19]. A synthetic analogue of the compound, vidarabine, as an approved drug, inhibits the replication of viral DNA, and is effective in the treatment of herpes simplex virus (HSV-1 and HSV-2) and varicella zoster virus (VZV) [20]. Natural products, such as flavonoids, oligostibens, coumarins and diarylheptanoids, are active against influenza virus neuraminidase [21]. Inhibition of the enzyme prevents the release of virus from the host cell and stops the spread of viral infection. For numerous plant-derived metabolites, the HIV integrase and/or reverse transcriptase (RT) are the targets [22]. The sulfated polysaccharides produced by marine algae belong to the broad-spectrum antivirals (BSAs). They disrupt different phases of viral infection by inhibition of attachment, penetration, uncoating, transcription and translation processes [23]. Cyclosporine A, originally isolated from an ascomycete fungus Tolypocladium inflatum, is an approved immunosuppressive drug effective against different viruses. It interacts with cyclophillins and blocks the conformational changes of the viral protein [24,25]. Many other natural antiviral agents have been identified and efforts to discover new bioactive metabolites, increase their efficacy and develop the most cost-effective methods of antiviral drug production are continuing [26,27,28].
The aim of the current work was to review the existing knowledge on the antiviral compounds produced by cyanobacteria. These prokaryotic, photosynthesizing microorganisms occur in all types of environments, including seas and oceans, lakes, rivers, hot springs, soil, rocks and ice [29]. They can live in free form or in symbiotic associations with other organisms. Their success in survival and development in different conditions, sometimes at a life limit, can be attributed, among others, to their unique metabolic pathways [29]. According to the latest data, over 2000 cyanobacteria secondary metabolites have been discovered [30]. These include both acute toxins and metabolites that constitute a valuable starting material for the development of novel drugs against cancer, bacterial infections, or metabolic disorders [31,32]. Compared to other activities of cyanometabolites, the antiviral effects have been explored to a lesser extent [32]. Most of the studies were focused on lectins [33] and polysaccharides [34].
2. Cyanobacterial Lectins
Lectins are monomeric or oligomeric proteins that specifically and reversibly bind to carbohydrates, including those that constitute a component of viral envelope glycoproteins [35]. These compounds are produced by a variety of organisms: plants, animals, fungi and bacteria [36]. Despite some similarity in amino acid sequences, significant differences in their tertiary structure can be observed. The orientation of the carbohydrate-binding domain (CBD) in lectin affects the affinity of the proteins to sugars, mainly the high mannose oligosaccharides, and determines their specificity. The binding potency of lectins is enhanced by the multivalency of CBD [37]. As potent viral entry inhibitors, they can be used in prophylactics, but their role in the treatment of viral infections is also explored [35].
2.1. Cyanovirin-N
Cyanovirin-N (CV-N, 11-kDa) was isolated from the culture of the freshwater cyanobacterium Nostoc ellipsosporum. The lectin is composed of 101 amino acid residues with a sequence of low homology to other proteins [38,39,40]. In the CV-N structure, two internal repeats containing residues 1–50 and 51–101 of 32% sequence identity were distinguished (Figure 1).
Figure 1.
Amino acid sequence alignment of cyanobacterial lectins described in the work: cyanovirin (CV-N), microvirin (MVN), scytovirin (SVN), Microcystis viridis lectin (MVL) and Oscillatoria agardhii agglutinin (OAA). The structural domains (solid line) and disulfide bonds (dashed line) are marked. Identical residues are indicated in dark grey, and similar residues are in light grey. (The figure was based on the following references: [41] CV-N, [42] MVN, [43] SVN, [44] MVL and [45] OAA).
The fold of the protein is novel, with a three-stranded β sheet structure [40,46,47]. The two carbohydrate-binding domains, A and B, are linked with the four-residue sequence Gln-Pro-Ser-Asn [40,48]. Domain A contains both N- (residues 1–38) and C- (residues 90–101) termini and is stabilized by a disulfide bond that links Cys58 and Cys73. Domain B occupies the inner part of the protein (residues 39–89) and contains a disulfide bond between Cys8 and Cys22 [39,40] (Figure 1). In solution, CV-N occurs mainly as a monomer, while in crystal, a domain-swapped dimmer is formed [40,46,48]. In the dimmer, the identical (A) or similar (B) domains occur, but they are composed of the sequences derived from two different CV-N monomers [46,48]. CV-N is stable in a broad range of pH and temperature, it is also resistant to organic solvents and detergents [49].
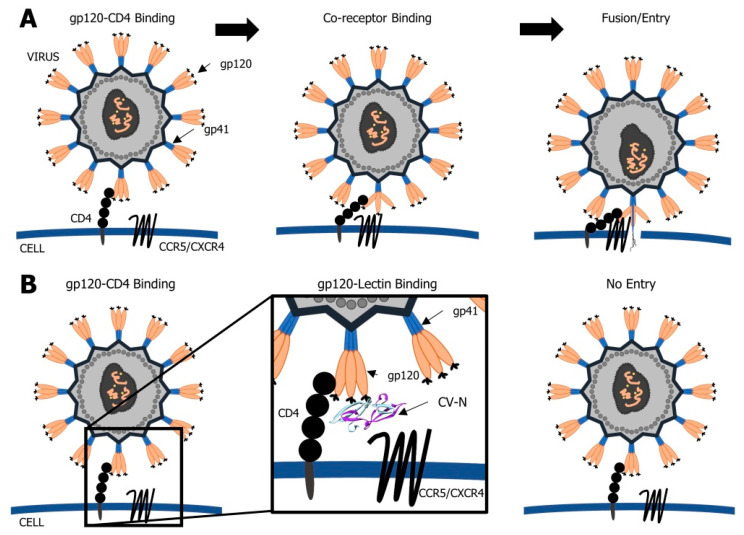
CV-N acts by blocking the interaction between the human immunodeficiency virus HIV gp120 and the CD4 T-cell receptor [48,50]. Binding to viral gp120 prevents the conformational changes of CD4 and interaction with the associated co-receptors CXCR4 and CCR5 (Figure 2). As a consequence, the virus cannot enter into the cell and its transmission from infected to a non-infected cell is blocked. CV-N specifically binds to the terminal Manα(1-2)Man unit of arms D1 and D3 on large high-mannose N-linked oligosaccharides (Man8GlcNAc2 (Man8) and Man9GlcNAc2 (Man9)) of HIV gp120 (an epitope of the 2G12 mAb) [38] (Figure 3). In the in vitro studies, the deactivation of HIV was observed at a nanomolar concentration of the lectin [38,51]. The two binding domains of CV-N enable the protein to cross-link the branched oligomannosides and the interaction with both domains is required for the activity of the lectin. However, domain B interacts with α(1-2) linked oligomannose with 10 times higher affinity than domain A. Monovalent mutants of CV-N are inactive [40]. The deletion of N-glycans in viral gp120 led to the development of resistance in CV-N exposed strains [52].
Figure 2.
Schematic representation of viral infection (A) and the role of cyanobacterial lectin, cyanovirin (CV-N), in inhibition of viral entry and fusion (B). CV-N blocks the interaction between the viral gp120 and the CD4 receptor on the host cell. It prevents the interaction with the associated co-receptors CXCR4/CCR5. As a consequence, the virus cannot enter into the cell.
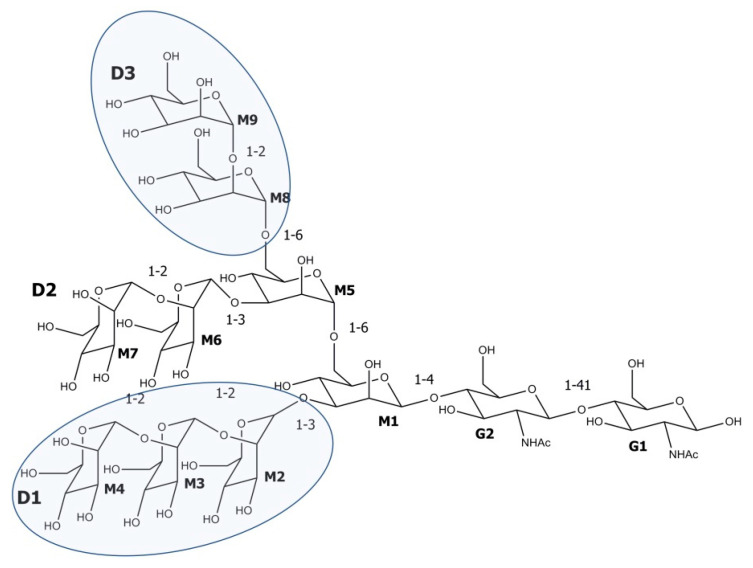
Figure 3.
Chemical structure of the high mannose oligosaccharide Man9GlcNAc2. The cyanovirin (CV-N) recognition sites, Manα(1-2)Man disaccharide units that terminate arms D1 and D3, are marked. Microvirin (MVN) has an affinity for Manα(1-2)Man terminating disaccharide. Scytovirin (SVN) binds to the Manα(1-2)Manα(1-6)Manα(1-6)Man tetrasaccharide core structure, Microcystis viridis lectin (MVL) binds to Manα(1-6)Manβ(1-4)GlcNAcβ(1-4)GlcNAc tetrasaccharide and Oscillatoria agardhii agglutinin (OAA) recognizes the pentasaccharide sequence Manα(1-3)Manα(1-6)Manβ(1-4)GlcNAcβ(1-4)GlcNAc. M stands for mannose, G for GlcNHAc.
The potential of CV-N to be developed as a topical microbicide has been extensively explored. Besides interaction with HIV gp120 and inhibition of HIV (type 1 and 2) infection, CV-N is active at a nanomolar level against other enveloped viruses such as simian immunodeficiency virus (SIV) and the chimeric SIV/HIV-1 virus (SHIV89.6P) [53], feline immunodeficiency virus (FIV), human herpes virus 6 (HHV-6), measles virus (MeV) [54], Ebola virus [55], hepatitis virus [56], and influenza virus [57], all with the N-linked high mannose oligosaccharides as glycoprotein components. To improve the drug-like properties of CV-N, the protein was modified by site-specific conjugation with polyethylene glycol in a reaction called PEGylation [58]. When administered intravenously, the PEGylated CV-N was significantly less immunogenic.
Due to a broad spectrum of activity against enveloped viruses, and high stability [49], CV-N represents great potential as a prevention measure against viral infections. Therefore, a need to develop alternative or improved methods of CV-N production occurred. Attempts were made to produce recombinant CV-N (rCV-N) at low costs and in amounts sufficient for drug development. The genes involved in CV-N production were expressed in bacterial hosts such as Streptococcus gordonii [59], Escherichia coli [60], Lactobacillus jensenii [61], and in transgenic plants, Pichia pastoris and Nicotiana tabacum [62,63], reaching the yield of 140 mg/40 g wet cell (40 mg/L) in E. coli [47,60].
The in vivo tests on simian/HIV (SHIV89.6P) virus-infected macaques (Macaca fascicularis), with a rectal and vaginal administration, proved recombinant cyanovirin to be effective in the prevention of sexual transmission of the virus [53]. For these tests, the lectin produced by E. coli, with the same activity as natural CV-N, was used. In another study, L. jensenii strain 1153-1666 was bioengineered to produce the protein [64]. Repeated vaginal administration of the bacteria in macaques led to a 63% reduction in transmission of SHIVSF162P3 and in the peak viral loads. Prolonged production of rCV-N by L. jensenii in the vagina did not cause any observable negative effects [64]. When macaques were fed with yoghurt containing the CV-N-producing commensal bacteria (50 mL/day) of the genus Lactobacillus (LAB-mCV-N), the lectin was detected in the rectal vault up to ten days after the treatment [65]. In the tests, the 20-fold lower peak of viral infection was observed. Further experiments on macaques showed a positive effect of LAB-mCV-N on the vaginal microbiome [66]. In the case of mice, subcutaneous injection of CV-N (approx. 5 mg/kg) reduced the titers of the Zaire strain of the Ebola virus, but the therapeutic index of the protein was found to be narrow [55].
Although the in vivo tests on macaques treated with CV-N did not reveal adverse effects of the lectin, some risk, especially with longer-term usage, still exists. The peripheral blood mononuclear cells (PBMCs) exposed to CV-N showed changes in morphology and were more susceptible to viral infection. In addition, an increase in mitogenic activity and level of chemokines occurred [52,67]. When applied at a 5-fold lower concentration than the antiviral activity range, CV-N enhanced the replication of HIV-1 in PBMCs [52]. CV-N (2 μg/mL) was also toxic to primary human keratinocytes (PHKs) [67].
2.2. Microvirin
Microvirin (MVN, 12.7 kDa) was isolated from Microcystis aeruginosa PCC7806 [42]. This monomeric protein is composed of 108 amino acids, which form two tandem repeats (residues 1–54 and 55–108) of 35% sequence identity (Figure 1). As in CV-N, these sequential repeats do not correspond to the two structural domains of the protein. Domain A is composed of residues 38–93 and its structure is stabilized by two disulfide bonds linking Cys-60 and Cys-80, and Cys-63 and Cys-78 (Figure 1). The domain contains the only carbohydrate-binding site of the lectin, which interacts with terminal Manα(1-2)Man of viral gp120 glycans [68] (Figure 3). As a monovalent protein, MVN does not cross-link with the branched oligomannosides. In domain B (residues 1–37 and 94–108), there is only one disulfide bond and it links Cys-8 and Cys-24 (Figure 1).
In vitro tests revealed potent activity of MVN against a wide range of laboratory-adapted, and clinical HIV-1 strains, and also in various cell types (IC50 = 2–12 nM) [68,69]. MVN was also found to inhibit syncytium formation between the T-cell line HUT-78 infected by HIV-1 and uninfected HUT-78 cells [69]. The lectin did not inhibit HIV-1 clinical isolates of group O, HIV-2, SIVmac251, MLV and the vesicular stomatitis virus (VSV) [47,48]. In contrast to other lectins, including CV-N, MVN had only minor cytotoxic and mitogenic activity; it also did not activate or enhance viral replication in pretreated cells [68,69]. At a dose of up to 7 µM, MVN was not toxic to T-cell line MT-4 and PBMCs. Therefore, it represents a better safety profile than CV-N [69]. In PBMCs, MVN induced the production of several pro-inflammatory cytokines, but with the exception of IL-1B and G-CSF, the effect was less pronounced than in the case of CV-N [69].
The MVN resistant virus with mutations in N-glycans of gp120 was obtained after 205-day (41 passages) exposure of HIV-1 NL-4.3 to the lectin [69]. The virus also became resistant to carbohydrate-specific human monoclonal antibody mAb 2G12, but was still found to be sensitive to lectins such as CV-N, HHA (Hippeastrum hybridum agglutinin), GNA (Galanthus nivalis agglutinin) and UDA (Urtica dioica agglutinin) [69].
As revealed using the HCVcc-Huh-7.5 (hepatitis C virus-human hepatoma 7.5) infection system, both the monomeric and its recombinantly engineered oligomeric MVN forms were active against hepatitis C virus (HCV) [70]. Moreover, the oligomeric variants, especially the trimmers and tetramers, were more potent in neutralizing HIV and HCV than the monomeric MVN. The activity increased with the length of the peptide linker connecting the monomers [70]. LUMS1, the engineered MVN variant composed of two identical domains and with two binding sites, specifically inhibited the infection of HIV-1 and HCV, but was not active against VSV. The potency of HIV-1 (EC50 = 37.2 nM) and HCV entry inhibition (EC50 = 45.3 nM) by LUMS1 was lower than by MVN (EC50 = 8.0 nM) [71]. However, this engineered lectin had a marginal cytotoxic effect on PBMCs, human hepatoma cell line Huh-7.5 and human liver cancer cell line HepG2. LUMS1 also had a negligible effect on the activation of B and T helper (Th) cells [71].
2.3. Scytovirin
Scytovirin (SVN, 9.71 kDa) was isolated from Scytonema varium strain HG-24-1 [43]. This single-chained 95-amino acid lectin is composed of two sequence repeats [43,72]. They form two 90% identical structural domains, SD1: 3-43 and SD2: 51-89, separated by a Pro-rich linker [72,73,74] (Figure 1). Each domain contains three aromatic amino acids involved in carbohydrate binding, and two intra-domain disulfide bonds. The fifth inter-domain disulfide bond links Cys-7 and Cys-55 (Figure 1). SVN represents a novel fold, with only short fragments of regular secondary structures and a high number of hydrogen bonds [72,73]. The primary structure of SVN is similar to a chitin-binding group of hevein-like proteins with two chitin-binding sites. However, the arrangements of disulfide bonds and the aromatic triad in the binding site of the proteins are different, which might explain the lack of chitin-binding ability of SVN. The lectin also does not bind to monosaccharides or common trisaccharides [43,72].
SVN binds to the Manα(1-2), Manα(1-6),Manα(1-6)Man tetrasaccharides of the viral enveloped glycoproteins, especially to gp120, but also gp160 and less effectively to gp41 [43]. The binding proceeds simultaneously at the two domains (SD1 and SD2), but domain SD1 has a higher affinity for oligosaccharides than SD2 [75,76]. The in silico studies showed that for the two domains the mechanism of the SVN–Man4 interactions was different [76].
SVN possesses potent activity against different HIV-1 isolates (EC50 = 0.3–22 nM). The lectin is also active against Zaire Ebola virus (ZEBOV) (EC50 41 nM), Marburg virus (MARV) and HCV (3.2–96 nmol) [77]. In experiments on BALB/c mice, the maximal antiviral protection was achieved when SVN was continually administered before the infection or during the earliest stages of the viral life cycle. Due to low stability in serum, SVN should be dosed every 6 h to be effective [77]. SVN was not toxic to the Huh-7.5.1 cell line at up to 2 µM [78].
The expression of the synthetic gene encoding SVN in E. coli yielded 5–10 mg/L of the lectin [75]. The engineered SVN was found to be equally active or showed an even higher affinity to viral glycans [79].
2.4. Microcystis Viridis Lectin
M. viridis lectin (MVL, 13 kDa), a homodimer lectin, was isolated from M. viridis NIES-02 [44]. The monomers are composed of 113 amino acid residues, which form two 50% identical domains, N-terminal domain (SD1: residues 1–54) and C-terminal domain (SD2: residues 60–113), separated by a five-amino acid linker (Figure 1) [80]. Each monomer contains two binding sites, which show affinity to N-linked oligomannosides with at least the Manα(1-6)Manβ(1-4)GlcNAcβ(1-4)GlcNAc tetrasaccharide core structure [80,81,82]. The lectin inhibits cell fusion of HIV-1 [81] and HCV [83] with an IC50 value of approx. 30 nM. Interestingly, one of the oligomannose binding sites of MVL exerts glucosidase activity and catalyzes the degradation of a chitotriose GlcNAcβ(1-4)GlcNAcβ(1-4)GlcNAcGlcAc3 to GlcNAc [82]. It was demonstrated that the antiviral activity of MVL and CV-N is complex and includes both binding of the lectins to the target cell surface and to the viral envelope gp120 [83]. As MVL interacts with cellular proteins, the cytotoxic effects of the lectin might occur. Indeed, the MTT assay revealed an inhibitory effect of the recombinant MVL on Hep-G2 (human hepatocellular liver carcinoma), HT-29 (human colon cancer), SGC-7901 (stomach cancer) and SK-OV-3 (human ovarian cancer) cell lines (IC50 40–53 μg/mL) [84]. This activity could be attributed to the expression of high mannose oligosaccharides during cancer progression [85].
2.5. Oscillatoria Agardhii Agglutinin
O. agardhii agglutinin (OAA; 13.9 kDa) was isolated from strain NIES-204. This monomeric protein consists of 132 amino acids, which form two 75% identical domains, N-terminal domain (SD1: residues 1–67) and C-terminal domain (SD2: residues 68–132) [45,86] (Figure 1). The primary structure of the protein was similar to the sequences of hemagglutinin MBHA produced by myxobacterium Myxococcus xanthus and the lectin ESA-2 from red algae Eucheuma serra, but distinct from lectins produced by M. aeruginosa [45,86].
OAA possesses two carbohydrate-binding sites located symmetrically at opposite ends of the compound. In contrast to other cyanobacterial lectins (e.g., CV-N, SVN and MVL), which bind to the end mannoses of Man-9, OAA recognizes the branched central core unit of Man-9, a pentasaccharide glycan, Manα(1-3)Manα(1-3)Manα(1-6)Manα(1-6)Man [87].
OAA inhibited HIV replication in MT-4 cells (EC50 = 44.5 nM) [45]. Genes encoding lectins and their products with structure, carbohydrate-binding specificity and antiviral activity similar to OAA were discovered in a number of prokaryotic and eukaryotic organisms [45,86,88,89]. This family of lectins was termed Oscillatoria agardhii agglutinin homologs (OAAH). They all showed potent antiviral activity against a wide range of HIV-1 and HIV-2 strains and clinical isolates, including HIV-1 group O isolates [90]. OAAH block the viral entry to the target cell and the replication of HIV [86,90]. They also bind to HIV-infected cells with expressed viral glycoproteins on their surface, preventing cell-to-cell transmission of the virus [90].
OAA is a stable protein; it preserved its activity even at 80 °C (30 min) and pH 4–11 [86]. The OAA genes were expressed in E. coli, and 48 mg/L of the recombinant protein (rOAA) were obtained [88]. Unfortunately, the development of an antiviral agent from OAA might be problematic, because, like CV-N, MVN and MVL, it exerts cytotoxic effects [45].
The production of antiviral lectins by cyanobacteria is probably a common feature of these microorganisms. The CV-N homologue, Cyt-CVNH, with approximately 4-fold stronger anti-HIV activity was identified in Cyanothece sp. PCC7424 from rice fields in Senegal [91]. Recently, an oscillatorial lectin with anticancer and antiviral activity has been isolated from Oscillatoria acuminate MHM-632MK014210 from Egyptian soil habitat [92]. In addition, the genomic screening of cyanobacteria isolated from a lake in the Amazon region led to the identification of new lectins and their homologues [93].
3. Cyanobacterial Polysaccharides
Polysaccharides, including chitin, cellulose, glycogen, starch, agar and carrageenan, are the most abundant natural polymers. They constitute structural elements of plants, animals and microorganisms, and play various other roles in their life. Polysaccharides also found wide application in the food industry, cosmetics production, agriculture and medicine [94]. Their anticancer, immunomodulatory, antimicrobial, anticoagulant and wound healing properties have been explored in traditional herbal and modern medicine [95,96]. Polysaccharides of antiviral activity frequently contain sulfate groups and have potent effects on a broad spectrum of viruses, including HIV, HSV, CMV, influenza virus, hepatitis virus and coronavirus [96,97,98,99].
Calcium Spirulan
Calcium spirulan (Ca-SP), a sulfated polysaccharide, was isolated from Arthrospira platensis (previous name Spirulina platensis). First, the inhibitory effect of Arthrospira water extract on the replication of HSV-1 in HeLa cells (human cervix epithelioid carcinoma) was observed [100,101]. The isolated active agent, Ca-SP, was found to be composed of rhamnose, 3-O-methyl-rhamnose, 2,3-di-O-methyl-rhamnose, 3-O-methylxylose, uronic acids, sulfate groups and calcium ions chelated with sulfate groups [102].
In vitro tests showed selective activity of Ca-SP against enveloped viruses, such as HSV-1, HCMV (human cytomegalovirus), MeV (measles virus), MuV (mumps virus), influenza A virus, HHV-6 [101,103], and Kaposi sarcoma-associated herpesvirus/human herpes virus 8 (KSHV/HHV-8) [104]. When added before the infection, Ca-SP reduced viral replication at ED50 0.92–23 µg/mL. In the same experiments, the cytotoxic effects were low; for different cell lines, the ID50 ranged from 2900 to 7900 µg/mL [101]. When the quantitative PCR method was applied, the inhibitory activity of Ca-SP against HSV-1 was found to be more potent (IC50 0.05–0.5 µg/mL) and comparable to other antiviral agents such as acyclovir [104].
Desulfation or the removal of Ca2+ led to the loss of Ca-SP activity. The replacement of the ion with Na+ and K+ had no significant effects, while the presence of other ions, e.g., Ag+ and Cd2+, decreased spirulan potency [101,102]. These effects were assigned to the loss of specific spirulan conformation, which was found to be critical for its activity [102].
It is pertinent to note that beside antiviral activity, Ca-SP also induced production of tissue-type plasminogen activator (t-PA) in human fetal lung fibroblasts, showed heparin cofactor II-dependent antithrombin activity [105], and inhibited the invasion and metastasis of tumor cells [106].
Other Arthrospira platensis metabolites are also active against enveloped viruses such as HIV, HSV and possibly SARS-CoV [107,108]. This microorganism and Arthrospira-based products (spirulina extracts) have been used for centuries as protein- and vitamin-rich health food supplements or nutraceuticals. They were shown to have antioxidant, antiviral activity and the ability to boost the immune system. The expanded use of spirulina extracts in food and beverages was approved by the Food and Drug Administration (FDA) [21CFR73.530]. In HIV-patients treated with spirulina extract, a significant decrease in viral load accompanied by an increase in the activity of macrophages, interferon production, NK cytotoxicity and other immune system responses was observed [108,109,110]. In enzymatic hydrolysate from the marine Spirulina sp., phycobilin-derived peptides with inhibitory activity against angiotensin-converting enzyme (ACE) were isolated [111,112]. The angiotensin-converting enzyme inhibitors (ACEIs) reduce the production of angiotensin II, responsible for blood vessel constriction. The inhibitors are used in patients with cardiovascular disorders and high blood pressure problems. The inhibition of ACE also enhances the activity of ACE2 (converting angiotensin II into angiotensin), which is downregulated in the SARS-CoV2 infected organs. In COVID-19 patients with severe injury of ACE2 expressing organs, mainly lungs, the therapeutic application of ACEIs has been studied [108]. On the other hand, SARS-CoV2 infection starts with the attachment of the viral spike protein (S-protein) to the host cell ACE2 [113]. Therefore, concerns were expressed that in patients treated with ACEIs, and suffering from cardiovascular disorders, a higher risk of viral infection can occur. Recently conducted clinical trials did not support this hypothesis [114,115].
Nostoflan, another antiviral polysaccharide, was isolated from a terrestrial cyanobacterium, Nostoc flagelliforme [116]. It contains glucose (42.8%), xylose (29.9%), galactose (20.7%), as well as mannose (6.6%) and glucuronic acid (13.3%) on the nonreducing ends. Unlike many sulfated polysaccharides, nostoflan did not show antithrombin activity [116]. It also has very low cytotoxicity and a wide spectrum of antiviral activity against enveloped viruses such as HSV-1, HSV-2, HCMV, and influenza A virus. When the compound was applied at the onset of the infection, the IC50 values for viral replication were 0.37–78 µg/mL [116]. Nostoflan prevented the binding of viral particles to host cells, but did not affect their penetration. Nostoflan also stimulated the response of the immune system in the infected organism [116].
4. Antiviral Cyanopeptides and Other Metabolites
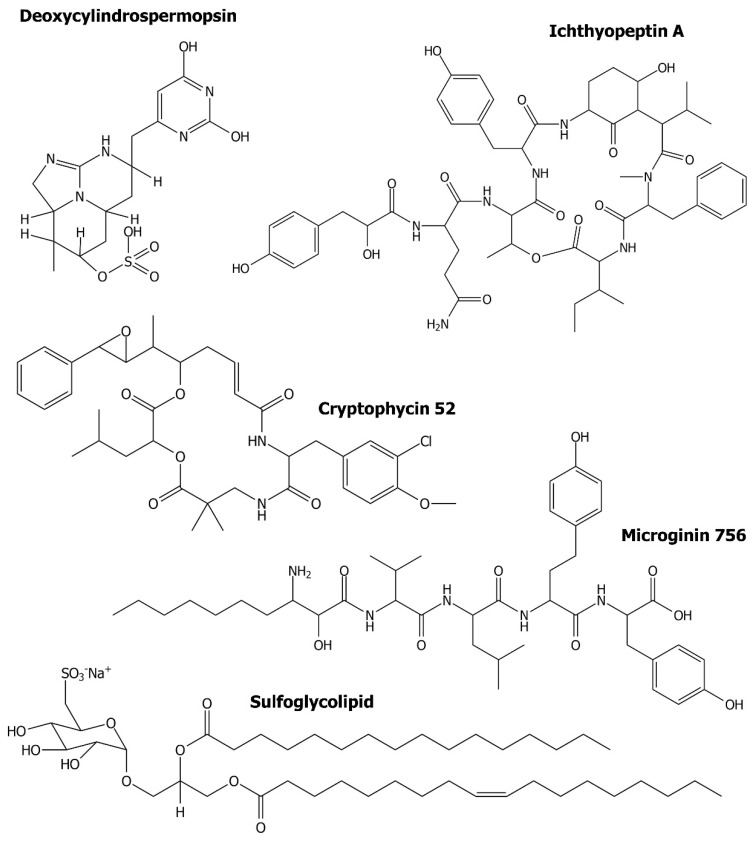
Peptides constitute another group of antiviral cyanometabolites. A chromatographic fraction containing a mixture of two ichthyopeptins, A and B, inhibited influenza A virus in infected Medin–Darby Canine Kidney cells (MDCK) (IC50 = 12.5 µg/mL) [117]. Ichthyopeptins (Figure 4) are cyclic depsipeptides with a unique residue, 3-amino-6-hydroxy-2-piperidone (Ahp), and the general structure PAA-Gln/Asn-[Thr-Tyr/Leu-Ahp-Val/Ile-MePhe-Ile/Val], where PAA is 2-hydroxy-3-(4′-hydroxyphenyl)acetic acid. These peptides were isolated from Microcystis ichthyoblabe strain BM Mi/13 [117].
Figure 4.
Chemical structure of cyanometabolites discussed in the work as potential antiviral agents.
The antiviral activity of microginins (MGs) (Figure 4), a class of non-ribosomal peptides produced mainly by the genus Microcystis, was not reported. However, their inhibitory activity against ACE [118,119,120] might indicate their potential to prevent SARS-CoV2 infections. MGs contain from 3 to 6 residues and are characterized by the presence of N-terminal β-amino-α-hydroxy-decanoic acid (Ahda) or its variants [121,122]. They are also active against aminopeptidases [123,124], but showed no effects against proteases: trypsin, thrombin, plasmin, chymotrypsin, elastase and papain [125].
Sulfoglycolipids (Figure 4) were among the first discovered cyanobacterial metabolites with antiviral activity [126]. In these microorganisms, sulfoglycolipids are present in the thylakoid membrane and cell wall of heterocysts. The compounds were isolated from several filamentous species, including Lyngbya lagerheimii, Phormidium tenue, Oscillatoria raoi, O. trichoides, O. limnetica and Scytonema sp. [126,127,128]. Sulfoglycolipids inhibited the DNA polymerase function of the HIV-1 RT with IC50 values in the range 24–2950 nM, but had no significant effects on the ribonuclease H [127,128]. The presence of a sulfate group in the sugar unit and the fatty acid ester side chains in the structure was critical for sulfoglycolipid’s activity against HIV RT [128].
The process of antiviral drug development includes both biological tests and in silico studies. The latter ones are performed with the application of structure-based or ligand-based approaches and enable the identification and better understanding of the ligand–target interactions [129]. These techniques reduce the time and costs spent on new drug development and also increase the chances for the design of safe and effective medicine. The in silico techniques were applied in the screening of 23 cyanobacterial metabolites with previously documented anticancer, antimicrobial or antiviral activity [130]. In the study, the molecular docking of the compounds at the binding pockets of two SARS-CoV2 proteases, the main protease Mpro and the papain-like protease PLpro, was analyzed. These proteases are important targets in antiviral drug development. Of the cyanometabolites, the depsipeptide cryptophycin 52 (Figure 4) and the alkaloid deoxycylindrospermopsin, showed promising effects on the two SARS-CoV2 proteases. The assessment of the physicochemical properties of the compounds performed based on Lipinski’s rule of five [131] led to the conclusion that deoxycylindrospermopsin has the best antiviral drug-like properties. According to Naidoo et al. [130], these results provide a good basis for the development of effective anti-COVID-19 therapy.
In some studies, the potent antiviral activity of crude cyanobacterial extracts was documented, however, the active agents were not identified [132,133,134]. At concentrations non-toxic to MDCK cells, the extracts from several Microcystis strains inhibited the replication of influenza A virus [132]. The observed activity was attributed to serine protease inhibitors produced by cyanobacteria [117,132]. The replication of influenza viruses in MDCK cells was also affected by Leptolyngbya extracts [133]. The samples inhibited viral neuraminidase, which is one of the antiviral therapy targets [133]. Five other cyanobacterial strains, Leptolyngbya boryana, Arthrospira platensis, Nostoc punctiforme, Oscillatoria sp. and Leptolyngbya sp., reduced the titers of coxsackievirus B3 (CVB3) in green monkey kidney cell culture and rotavirus (RV) SA-11 in Rhesus monkey kidney cell culture [134].
Antiviral activity was found in cyanobacteria representing different taxonomic groups and different metabolite profiles. This indicates that not only cyanobacterial lectins and polysaccharides can be used as starting material for antiviral drug development. Therefore, the efforts to identify the antiviral cyanobacterial products and to determine their pharmaceutical potential are continuing. This is especially important in view of the global and devastating consequences of the COVID-19 pandemic and its negative impact on different areas of our life. The expansion of infectious diseases caused by other viruses also indicates the urgent need for exploration of all potential sources of effective antiviral therapeutics. Considering the increasing threat of pandemic outbreaks caused by different types and strains of viruses as well as their mutation and expansion, the development of broad-spectrum antivirals that do not induce the development of resistance is the biggest challenge and priority.
Author Contributions
All authors have participated in writing, review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Science Centre in Poland, grant number NCN2019/33/B/NZ9/02018 and by the Statutory Programme of the Institute of Oceanology, PAS, grant number II.3.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Knipe D.M., Howley P.M. Fields Virology. 6th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2013. [Google Scholar]
- 2.Gorbalenya A., Krupovic M., Mushegian A., Kropinski A.M., Siddell S.G., Varsani A., Adams M.J., Davison A.J., Dutilh B.E., Harrach B., et al. The new scope of virus taxonomy: Partitioning the virosphere into 15 hierarchical ranks. Nat. Microbiol. 2020;5:668–674. doi: 10.1038/s41564-020-0709-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahmoudabadi G., Phillips R. A comprehensive and quantitative exploration of thousands of viral genomes. Elife. 2018;7:e31955. doi: 10.7554/eLife.31955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloom D.E., Cadarette D. Infectious disease threats in the twenty-first century: Strengthening the global response. Front. Immunol. 2019;10:549. doi: 10.3389/fimmu.2019.00549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo G.D., Gao S.-J. Global health concerns stirred by emerging viral infections. Med. Virol. 2020;92:399–400. doi: 10.1002/jmv.25683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piret J., Boivin G. Pandemics Throughout History. Front. Microbiol. 2021;11:3594. doi: 10.3389/fmicb.2020.631736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muñoz L.S., Garcia M.A., Gordon-Lipkin E., Parra B., Pardo C.A. Emerging viral infections and their impact on the global burden of neurological disease. Semin. Neurol. 2018;38:163–175. doi: 10.1055/s-0038-1647247. [DOI] [PubMed] [Google Scholar]
- 8.Bleibtreu A., Bertine M., Bertin C., Houhou-Fidouh N., Visseaux B. Focus on Middle East respiratory syndrome coronavirus (MERS-CoV) Med. Mal. Infect. 2020;50:243–251. doi: 10.1016/j.medmal.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roychoudhury S., Das A., Sengupta P., Dutta S., Roychoudhury S., Choudhury A.P., Ahmed A.B.F., Bhattacharjee S., Slama P. Viral pandemics of the last four decades: Pathophysiology, health impacts and perspectives. Int. J. Environ. Res. Public Health. 2020;17:9411. doi: 10.3390/ijerph17249411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaefer T.J., Panda P.K., Wolford R.W. Dengue Fever. StatPearls Publishing; Treasure Island, FL, USA: 2021. [PubMed] [Google Scholar]
- 11.Bhatt S., Gething P.W., Brady O.J., Messina J.P., Farlow A.W., Moyes C.L., Drake J.M., Brownstein J.S., Hoen A.G., Sankoh O., et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Powell J.R., Human M.-B. Viral diseases: Why Aedes aegypti? Am. J. Trop Med. Hyg. 2018;8:1563–1565. doi: 10.4269/ajtmh.17-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trovato M., Sartorius R., D’Apice L., Manco R., De Berardinis P. Viral emerging diseases: Challenges in developing vaccination strategies. Front. Immunol. 2020;11:2130. doi: 10.3389/fimmu.2020.02130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tse L.V., Meganck R.M., Graham R.L., Baric R.S. The current and future state of vaccines, antivirals and gene therapies against emerging coronaviruses. Front. Microbiol. 2020;11:658. doi: 10.3389/fmicb.2020.00658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Clercq E., Li G. Approved antiviral drugs over the past 50 years. Clin. Microbiol. Rev. 2016;29:695–747. doi: 10.1128/CMR.00102-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pour P.M., Fakhri S., Asgary S., Farzaei M.H., Echeverría J. The signaling pathways, and therapeutic targets of antiviral agents: Focusing on the antiviral approaches and clinical perspectives of anthocyanins in the management of viral diseases. Front. Pharmacol. 2019;10:1207. doi: 10.3389/fphar.2019.01207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bryan-Marrugo O.L., Ramos-Jiménez J., Barrera-Saldaña H., Rojas-Martínez A., Vidaltamayo R., Rivas-Estilla A.M. History and progress of antiviral drugs: From acyclovir to direct-acting antiviral agents (DAAs) for hepatitis C. Med. Univ. 2015;17:165–174. doi: 10.1016/j.rmu.2015.05.003. [DOI] [Google Scholar]
- 19.Riccio G., Ruocco N., Mutalipassi M., Costantini M., Zupo V., Coppola D., de Pascale D., Lauritano D. Ten-year research update review: Antiviral activities from marine organisms. Biomolecules. 2020;10:1007. doi: 10.3390/biom10071007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzuki M., Okuda T., Shiraki K. Synergistic antiviral activity of acyclovir and vidarabine against herpes simplex virus types 1 and 2 and varicella-zoster virus. Antiviral. Res. 2006;72:157–161. doi: 10.1016/j.antiviral.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Grienke U., Schmidtke M., von Grafenstein S., Kirchmair J., Liedl K.R., Rollinger J.M. Influenza neuraminidase: A druggable target for natural products. Nat. Prod. Rep. 2012;29:11–36. doi: 10.1039/C1NP00053E. [DOI] [PubMed] [Google Scholar]
- 22.Mohan S., Taha M.M.E., Makeen H.A., Alhazmi H.A., Al Bratty M., Sultana S., Ahsan W., Najmi A., Khalid A. Bioactive natural antivirals: An updated review of the available plants and isolated molecules. Molecules. 2020;25:4878. doi: 10.3390/molecules25214878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hans N., Malik A., Naik S. Antiviral activity of sulfated polysaccharides from marine algae and its application in combating COVID-19: Mini review. Bioresour. Technol. Rep. 2021;13:100623. doi: 10.1016/j.biteb.2020.100623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell G., Graveley R., Seid J., Al-Humidan A., Skjødt H. Mechanisms of action of cyclosporine and effects on connective tissues. Semin. Arthritis Rheum. 1992;21:16–22. doi: 10.1016/0049-0172(92)90009-3. [DOI] [PubMed] [Google Scholar]
- 25.Matsuda S., Koyasu S. Mechanisms of action of cyclosporine. Immunopharmacology. 2000;47:119–125. doi: 10.1016/S0162-3109(00)00192-2. [DOI] [PubMed] [Google Scholar]
- 26.Martinez J.P., Sasse F., Brönstrup M., Diez J. A meyerhans antiviral drug discovery: Broad-spectrum drugs from nature. Prod. Rep. 2015;32:29–48. doi: 10.1039/C4NP00085D. [DOI] [PubMed] [Google Scholar]
- 27.Newman D.J., Cragg G.M. Natural products as sources of new drugs from 1981 to 2014. J. Nat. Prod. 2016;79:629–661. doi: 10.1021/acs.jnatprod.5b01055. [DOI] [PubMed] [Google Scholar]
- 28.Ma J., Gu Y., Xu P. A roadmap to engineering antiviral natural products synthesis in microbes. Curr. Opin. Biotechnol. 2020;66:140–149. doi: 10.1016/j.copbio.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whitton B.A. The Ecology of Cyanobacteria II: Their Diversity in Space and Time. Springer; Dordrecht, The Netherlands: 2012. [Google Scholar]
- 30.Jones M.R., Pinto E., Torres M.A., Dörr F., Mazur-Marzec H., Szubert K., Tartaglione L., Dell’Aversano C., Miles C.O., Beach D.G., et al. CyanoMetDB, a comprehensive public database of secondary metabolites from cyanobacteria. Water Res. 2021 doi: 10.1016/j.watres.2021.117017. in press. [DOI] [PubMed] [Google Scholar]
- 31.Dittmann E., Gugger M., Sivonen K., Fewer D.P. Natural product biosynthetic diversity and comparative genomics of the cyanobacteria. Trends Microbiol. 2015;23:642–652. doi: 10.1016/j.tim.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 32.Demay J., Bernard C., Reinhardt A., Marie B. Natural products from cyanobacteria: Focus on beneficial activities. Mar. Drugs. 2019;17:320. doi: 10.3390/md17060320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh R.S., Walia A.K., Khattar J.S., Singh D.P., Kennedy J.F. Cyanobacterial lectins characteristics and their role as antiviral agents. Int. J. Biol. Macromol. 2017;102:475–496. doi: 10.1016/j.ijbiomac.2017.04.041. [DOI] [PubMed] [Google Scholar]
- 34.Lee J.B., Srisomporn P., Hayashi K., Tanaka T., Sankawa U., Hayashi T. Effects of structural modification of calcium spirulan, a sulfated polysaccharide from Spirulina platensis, on antiviral activity. Chem. Pharm. Bull. 2001;49:108–110. doi: 10.1248/cpb.49.108. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell C.A., Ramessar K., O’Keefe B.R. Antiviral lectins: Selective inhibitors of viral entry. Antiviral. Res. 2017;142:37–54. doi: 10.1016/j.antiviral.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lam S.K., Ng T.B. Lectins: Production and practical applications. Appl. Microbiol. Biotechnol. 2011;89:45–55. doi: 10.1007/s00253-010-2892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee R.T., Lee Y.C. Affinity enhancement by multivalent lectin-carbohydrate interaction. Glycoconj. J. 2000;17:543–551. doi: 10.1023/A:1011070425430. [DOI] [PubMed] [Google Scholar]
- 38.Boyd M.R., Gustafson K.R., McMahon J.B., Shoemaker R.H., O’Keefe B.R., Mori T., Gulakowski R.J., Wu L., Rivera M.I., Laurencot C.M., et al. Discovery of cyanovirin-N, a novel human immunodeficiency virus-inactivating protein that binds viral surface envelope glycoprotein gp120: Potential applications to microbicide development. Antimicrob. Agents Chemother. 1997;41:1521–1530. doi: 10.1128/AAC.41.7.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gustafson K.R., Sowder R.C., 2nd, Henderson L.E., Cardellina J.H., 2nd, McMahon J.B., Rajamani U., Pannell L.K., Boyd M.R. Isolation, primary sequence determination, and disulfide bond structure of cyanovirin-N, an anti-HIV (human immunodeficiency virus) protein from the cyanobacterium Nostoc ellipsosporum. Biochem. Biophys. Res. Commun. 1997;238:223–228. doi: 10.1006/bbrc.1997.7203. [DOI] [PubMed] [Google Scholar]
- 40.Bewley C.A. Solution structure of a cyanovirin-N:Manα1-2Manα complex: Structural basis for high-affinity carbohydrate-mediated binding to gp120. Structure. 2001;9:931–940. doi: 10.1016/S0969-2126(01)00653-0. [DOI] [PubMed] [Google Scholar]
- 41.Mori T., Shoemaker R.H., Gulakowski R.J., Krepps B.L., McMahon J.B., Gustafson K.R., Pannell L.K., Boyd M.R. Analysis of sequence requirements for biological activity of cyanovirin-N, a potent HIV (human immunodeficiency virus)-inactivating protein. Biochem. Biophys. Res. Commun. 1997;238:218–222. doi: 10.1006/bbrc.1997.7202. [DOI] [PubMed] [Google Scholar]
- 42.Kehr J.-C., Zilliges Y., Springer A., Disney M.D., Ratner D.D., Bouchier C., Seeberger P.H., de Marsac N.T., Dittmann E. A mannan binding lectin is involved in cell-cell attachment in a toxic strain of Microcystis aeruginosa. Mol. Microbiol. 2006;59:893–906. doi: 10.1111/j.1365-2958.2005.05001.x. [DOI] [PubMed] [Google Scholar]
- 43.Bokesch H.R., O’Keefe B.R., McKee T.C., Pannell L.K., Patterson G.M.L., Gardella R.S., Sowder R.C., 2nd, Turpin J., Watson K., Buckheit R.W., Jr., et al. A potent novel anti-HIV protein from the cultured cyanobacterium Scytonema varium. Biochemistry. 2003;42:2578–2584. doi: 10.1021/bi0205698. [DOI] [PubMed] [Google Scholar]
- 44.Yamaguchi M., Ogawa T., Muramoto K., Kamio Y., Jimbo M., Kamiya H. Isolation and characterization of a mannan-binding lectin from the freshwater cyanobacterium (blue-green algae) Microcystis viridis. Biochem. Biophys. Res. Commun. 1999;265:703–708. doi: 10.1006/bbrc.1999.1749. [DOI] [PubMed] [Google Scholar]
- 45.Sato Y., Okuyama S., Hori K. Primary structure and carbohydrate binding specificity of a potent anti-HIV lectin isolated from the filamentous cyanobacterium Oscillatoria agardhii. J. Biol. Chem. 2007;282:11021–11029. doi: 10.1074/jbc.M701252200. [DOI] [PubMed] [Google Scholar]
- 46.Yang F., Bewley C.A., Louis J.M., Gustafson K.R., Boyd M.R., Gronenborn A.M., Clore G.M., Wlodawer A. Crystal structure of cyanovirin-N, a potent HIV-inactivating protein, shows unexpected domain swapping. J. Mol. Biol. 1999;288:403–412. doi: 10.1006/jmbi.1999.2693. [DOI] [PubMed] [Google Scholar]
- 47.Botos I., Wlodawer A. Cyanovirin-N: A sugar-binding antiviral protein with a new twist. Cell Mol. Life Sci. 2003;60:277–287. doi: 10.1007/s000180300023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barrientos L.G., Gronenborn A.M. The highly specific carbohydrate-binding protein cyanovirin-N: Structure, anti-HIV/Ebola activity and possibilities for therapy. Mini Rev. Med. Chem. 2005;5:21–31. doi: 10.2174/1389557053402783. [DOI] [PubMed] [Google Scholar]
- 49.Lotfi H., Sheervalilou R., Zarghami N. An update of the recombinant protein expression systems of cyanovirin-N and challenges of preclinical development. Bioimpacts. 2018;8:139–151. doi: 10.15171/bi.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu Y., Carrol J.R., Holt L.A., McMahon J., Giomarelli B., Ghirlanda G. Multivalent interactions with gp120 are required for the anti-HIV activity of Cyanovirin. Biopolymers. 2009;92:194–200. doi: 10.1002/bip.21173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Keeffe J.R., Gnanapragasam P.N.P., Gillespie S.K., Yong J., Bjorkman P.J., Mayo S.L. Designed oligomers of cyanovirin-N show enhanced HIV neutralization. Proc. Natl. Acad. Sci. USA. 2011;108:14079–14084. doi: 10.1073/pnas.1108777108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Balzarini J., Van Laethem K., Peumans W.J., Van Damme E.J.M., Bolmstedt A., Gago F., Schols D. Mutational pathways, resistance profile, and side effects of cyanovirin relative to human immunodeficiency virus type 1 strains with N-glycan deletions in their gp120 envelopes. J. Virol. 2006;80:8411–8421. doi: 10.1128/JVI.00369-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tsai C.-C., Emau P., Jiang Y., Tian B., Morton W.R., Gustafson K.R., Boyd M.R. Cyanovirin-N gel as a topical microbicide prevents rectal transmission of SHIV89.6P in macaques. AIDS Res. Hum. Retroviruses. 2003;19:535–541. doi: 10.1089/088922203322230897. [DOI] [PubMed] [Google Scholar]
- 54.Dey B., Lerner D.L., Lusso P., Boyd M.R., Elder J.H., Berger E.A. Multiple antiviral activities of cyanovirin-N: Blocking of human immunodeficiency virus type 1 gp120 interaction with CD4 and coreceptor and inhibition of diverse enveloped viruses. J. Virol. 2000;74:4562–4569. doi: 10.1128/JVI.74.10.4562-4569.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barrientos L.G., O’Keefe B.R., Bray M., Sanchez A., Gronenborn A.M., Boyd M.R. Cyanovirin-N binds to the viral surface glycoprotein, GP1,2 and inhibits infectivity of Ebola virus. Antiviral Res. 2003;58:47–56. doi: 10.1016/S0166-3542(02)00183-3. [DOI] [PubMed] [Google Scholar]
- 56.Helle F., Wychowski C., Vu-Dac N., Gustafson K.R., Voisset C., Dubuisson J. Cyanovirin-N inhibits hepatitis C virus entry by binding to envelope protein glycans. J. Biol. Chem. 2006;281:25177–25183. doi: 10.1074/jbc.M602431200. [DOI] [PubMed] [Google Scholar]
- 57.O’Keefe B.R., Smee D.F., Turpin J.A., Saucedo C.J., Gustafson K.R., Mori T., Blakeslee D., Buckheit R., Boyd M.R. Potent anti-influenza activity of cyanovirin-N and interactions with viral hemagglutinin. Antimicrob. Agents Chemother. 2003;47:2518–2525. doi: 10.1128/AAC.47.8.2518-2525.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zappe H., Snell M.E., Bossard M.J. PEGylation of cyanovirin-N, an entry inhibitor of HIV. Adv. Drug Deliv. Rev. 2008;60:79–87. doi: 10.1016/j.addr.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 59.Giomarelli B., Provvedi R., Meacci F., Maggi T., Medaglini D., Pozzi G., Mori T., McMahon J.B., Gardella G., Boyd M.R. The microbicide cyanovirin-N expressed on the surface of commensal bacterium Streptococcus gordonii captures HIV-1. AIDS. 2002;16:1351–1356. doi: 10.1097/00002030-200207050-00006. [DOI] [PubMed] [Google Scholar]
- 60.Colleluori D.M., Tien D., Kang F., Pagliei T., Kuss R., McCormick T., Watson K., McFadden K., Chaiken I., Buckheit R.W., Jr., et al. Expression, purification, and characterization of recombinant cyanovirin-N for vaginal anti-HIV microbicide development. Protein Expr. Purif. 2005;39:229–236. doi: 10.1016/j.pep.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 61.Liu X., Lagenaur L.A., Simpson D.A., Essenmacher K.P., Frazier-Parker C.L., Liu Y., Tsai D., Rao S.S., Hamer D.H., Parks T.P., et al. Engineered vaginal lactobacillus strain for mucosal delivery of the human immunodeficiency virus inhibitor cyanovirin-N. Antimicrob. Agents Chemother. 2006;50:3250–3259. doi: 10.1128/AAC.00493-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mori T., Barrientos L.G., Han Z., Gronenborn A.M., Turpin J.A., Boyda M.R. Functional homologs of cyanovirin-N amenable to mass production in prokaryotic and eukaryotic hosts. Protein Expr. Purif. 2002;26:42–49. doi: 10.1016/S1046-5928(02)00513-2. [DOI] [PubMed] [Google Scholar]
- 63.Sexton A., Drake P.M., Mahmood N., Harman S.J., Shattock R.J., Ma J.K.-C. Transgenic plant production of Cyanovirin-N, an HIV microbicide. FASEB J. 2006;20:356–358. doi: 10.1096/fj.05-4742fje. [DOI] [PubMed] [Google Scholar]
- 64.Lagenaur L.A., Sanders-Beer B.E., Brichacek B., Pal R., Liu X., Liu Y., Yu R., Venzon D., Lee P.P., Hamer D.H. Prevention of vaginal SHIV transmission in macaques by a live recombinant Lactobacillus. Mucosal. Immunol. 2011;4:648–657. doi: 10.1038/mi.2011.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li M., Patton D.L., Cosgrove-Sweeney Y., Ratner D., Rohan L.C., Cole A.M., Tarwater P.M., Gupta P., Ramratnam B. Incorporation of the HIV-1 microbicide cyanovirin-N in a food product. J. Acquir. Immune Defic. Syndr. 2011;58:379–384. doi: 10.1097/QAI.0b013e31823643fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brichacek B., Lagenaur L.A., Lee P.P., Venzon D., Hamer D.H. In vivo evaluation of safety and toxicity of a Lactobacillus jensenii producing modified cyanovirin-N in a rhesus macaque vaginal challenge model. PLoS ONE. 2013;8:e78817. doi: 10.1371/journal.pone.0078817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huskens D., Vermeire K., Vandemeulebroucke E., Balzarini J., Schols D. Safety concerns for the potential use of cyanovirin-N as a microbicidal anti-HIV agent. Int. J. Biochem. Cell Biol. 2008;40:2802–2814. doi: 10.1016/j.biocel.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 68.Shahzad-ul-Hussan S., Gustchina E., Ghirlando R., Clore G.M., Bewley C.A. Solution structure of the monovalent lectin microvirin in complex with Manα(1-2)Man provides a basis for anti-HIV activity with low toxicity. J. Biol. Chem. 2011;286:20788–20796. doi: 10.1074/jbc.M111.232678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Huskens D., Férir G., Vermeire K., Kehr J.-K., Balzarini J., Dittmann E., Schols D. Microvirin, a novel α(1,2)-mannose-specific lectin isolated from Microcystis aeruginosa, has anti-HIV-1 activity comparable with that of cyanovirin-N but a much higher safety profile. J. Biol. Chem. 2010;285:24845–24854. doi: 10.1074/jbc.M110.128546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Min Y.-Q., Duan X.-C., Zhou Y.-D., Kulinich A., Meng W., Cai Z.-P., Ma H.-Y., Liu L., Zhang X.-L., Voglmeir J. Effects of microvirin monomers and oligomers on hepatitis C virus. Biosci. Rep. 2017;37:BSR20170015. doi: 10.1042/BSR20170015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shahid M., Qadir A., Yang J., Ahmad I., Zahid H., Mirza S., Windisch M.P., Shahzad-ul-Hussan S. An engineered microvirin variant with identical structural domains potently inhibits human immunodeficiency virus and hepatitis C virus cellular entry. Viruses. 2020;12:199. doi: 10.3390/v12020199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McFeeters R.L., Xiong C., O’Keefe B.R., Bokesch H.R., McMahon J.B., Ratner D.M., Castelli R., Seeberger P.H., Byrd R.A. The novel fold of scytovirin reveals a new twist for antiviral entry inhibitors. J. Mol. Biol. 2007;369:451–561. doi: 10.1016/j.jmb.2007.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moulaei T., Botos I., Ziółkowska N.E., Bokesch H.R., Krumpe L.R., McKee T.C., O’Keefe B.R., Dauter Z., Wlodawer A. Atomic-resolution crystal structure of the antiviral lectin scytovirin. Protein. Sci. 2007;16:2756–2760. doi: 10.1110/ps.073157507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moulaei T., Stuchlik O., Reed M., Yuan W., Pohl J., Lu W., Haugh-Krumpe L., O’Keefe B.R., Wlodawer A. Topology of the disulfide bonds in the antiviral lectin scytovirin. Protein. Sci. 2010;19:1649–1661. doi: 10.1002/pro.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xiong C., O’Keefe B.R., Botos I., Wlodawer A., McMahon J.B. Overexpression and purification of scytovirin, a potent, novel anti-HIV protein from the cultured cyanobacterium Scytonema varium. Protein. Expr. Purif. 2006;46:233–239. doi: 10.1016/j.pep.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 76.Siqueira A.S., Lima A.R.J., de Souza R.C., Santos A.S., Vianez Júnior J.L.D.S.G., Gonçalves E.C. In silico analysis of the cyanobacterial lectin scytovirin: New insights into binding properties. Mol. Biol. Rep. 2017;44:353–358. doi: 10.1007/s11033-017-4116-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Garrison A.R., Giomarelli B.G., Lear-Rooney C.M., Saucedo C.J., Yellayi S., Krumpe L.R.H., Rose M., Paragas J., Bray M., Olinger G.G., Jr., et al. The cyanobacterial lectin scytovirin displays potent in vitro and in vivo activity against Zaire Ebola virus. Antiviral Res. 2014;112:1–7. doi: 10.1016/j.antiviral.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Takebe Y., Saucedo C.J., Lund G., Uenishi R., Hase S., Tsuchiura T., Kneteman N., Ramessar K., Tyrrell D.L.J., Shirakura M., et al. Antiviral lectins from red and blue-green algae show potent in vitro and in vivo activity against hepatitis C virus. PLoS ONE. 2013;8:e64449. doi: 10.1371/journal.pone.0064449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McFeeters H., Gilbert H.J., Wood A.M., Haggenmaker C.B., Jones J., Kutsch O., McFeeters R.L. Scytovirin engineering improves carbohydrate affinity and HIV-1 entry inhibition. Biochem. Physiol. 2013;S2 doi: 10.4172/2168-9652.S2-003. [DOI] [Google Scholar]
- 80.Williams D.C., Jr., Lee J.Y., Cai M., Bewley C.A., Clore G.M. Crystal structures of the HIV-1 inhibitory cyanobacterial protein MVL free and bound to Man3GlcNAc2: Structural basis for specificity and high-affinity binding to the core pentasaccharide from n-linked oligomannoside. J. Biol. Chem. 2005;280:29269–29276. doi: 10.1074/jbc.M504642200. [DOI] [PubMed] [Google Scholar]
- 81.Bewley C.A., Cai M., Ray S., Ghirlando R., Yamaguchi M., Muramoto K. New carbohydrate specificity and HIV-1 fusion blocking activity of the cyanobacterial protein MVL: NMR, ITC and sedimentation equilibrium studies. J. Mol. Biol. 2004;339:901–914. doi: 10.1016/j.jmb.2004.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shahzad-ul-Hussan S., Cai M., Bewley C.A. Unprecedented glycosidase activity at a lectin carbohydrate-binding site exemplified by the cyanobacterial lectin MVL. J. Am. Chem. Soc. 2009;131:16500–16508. doi: 10.1021/ja905929c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kachko A., Loesgen S., Shahzad-ul-Hussan S., Tan W., Zubkova I., Takeda K., Wells F., Rubin S., Bewley C.A., Major M.E. Inhibition of hepatitis C virus by the cyanobacterial protein Microcystis viridis lectin: Mechanistic differences between the high-mannose specific lectins MVL, CV-N, and GNA. Mol. Pharm. 2013;10:4590–4602. doi: 10.1021/mp400399b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li Y., Zhang X. Recombinant Microcystis viridis lectin as a potential anticancer agent. Pharmazie. 2010;65:922–923. doi: 10.1691/ph.2010.0713. [DOI] [PubMed] [Google Scholar]
- 85.Stowell S.R., Ju T., Cummings R.D. Protein glycosylation in cancer. Annu. Rev. Pathol. 2015;10:473–510. doi: 10.1146/annurev-pathol-012414-040438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sato Y., Murakami M., Miyazawa K., Hori K. Purification and characterization of a novel lectin from a freshwater cyanobacterium, Oscillatoria agardhii. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2000;125:169–177. doi: 10.1016/S0305-0491(99)00164-9. [DOI] [PubMed] [Google Scholar]
- 87.Koharudin L.M.I., Gronenborn A.M. Structural basis of the anti-HIV activity of the cyanobacterial Oscillatoria agardhii agglutinin. Structure. 2011;19:1170–1181. doi: 10.1016/j.str.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sato T., Hori K. Cloning, expression, and characterization of a novel anti-HIV lectin from the cultured cyanobacterium, Oscillatoria agardhii. Fish. Sci. 2009;75:743–753. doi: 10.1007/s12562-009-0074-4. [DOI] [Google Scholar]
- 89.Koharudin L.M.I., Kollipara S., Aiken C., Gronenborn A.M. Structural insights into the anti-HIV activity of the Oscillatoria agardhii agglutinin homolog lectin family. J. Biol. Chem. 2012;287:33796–33811. doi: 10.1074/jbc.M112.388579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Férir G., Huskens D., Noppen S., Koharudin L.M.I., Gronenborn A.M., Schols D. Broad anti-HIV activity of the Oscillatoria agardhii agglutinin homologue lectin family. J. Antimicrob. Chemother. 2014;69:2746–2758. doi: 10.1093/jac/dku220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Matei E., Basu R., Furey E., Shi J., Calnan C., Aiken C., Gronenborn A.M. Structure and glycan binding of a new cyanovirin-N homolog. J. Biol. Chem. 2016;291:18967–18976. doi: 10.1074/jbc.M116.740415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Saad M.H., El-Fakharany E.M., Salem M.S., Sidkey N.M. In vitro assessment of dual (antiviral and antitumor) activity of a novel lectin produced by the newly cyanobacterium isolate, Oscillatoria acuminate MHM-632 MK014210.1. J. Biomol. Struct. Dyn. 2020;17:1–21. doi: 10.1080/07391102.2020.1848632. [DOI] [PubMed] [Google Scholar]
- 93.Siqueira A.S., Lima A.R.J., Aguiar D.C.F., Santos A.S., Vianez Júnior J.L.D.S.G., Gonçalves E.C. Genomic screening of new putative antiviral lectins from Amazonian cyanobacteria based on a bioinformatics approach. Proteins. 2018;86:1047–1054. doi: 10.1002/prot.25577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.van Dam J.E.G., van den Broek L.A.M., Boeriu C.G. Polysaccharides in human health care. Nat. Prod. Commun. 2017;12:821–830. doi: 10.1177/1934578X1701200604. [DOI] [Google Scholar]
- 95.Lee Y.-E., Kim H., Seo C., Park T., Lee K.B., Yoo S.-Y., Hong S.-C., Kim J.T., Lee J. Marine polysaccharides: Therapeutic efficacy and biomedical applications. Arch. Pharm Res. 2017;40:1006–1020. doi: 10.1007/s12272-017-0958-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen X., Han W., Wang G., Zhaoa X. Application prospect of polysaccharides in the development of anti-novel coronavirus drugs and vaccines. Int. J. Biol. Macromol. 2020;164:331–343. doi: 10.1016/j.ijbiomac.2020.07.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang W., Wang S.-X., Guan H.-S. The antiviral activities and mechanisms of marine polysaccharides: An overview. Mar. Drugs. 2012;10:2795–2816. doi: 10.3390/md10122795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shi Q., Wang A., Lu Z., Qin C., Hu J., Yin J. Overview on the antiviral activities and mechanisms of marine polysaccharides from seaweeds. Carbohydr. Res. 2017;453–454:1–9. doi: 10.1016/j.carres.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 99.Chen L., Huang G. The antiviral activity of polysaccharides and their derivatives. Int. J. Biol. Macromol. 2018;115:77–82. doi: 10.1016/j.ijbiomac.2018.04.056. [DOI] [PubMed] [Google Scholar]
- 100.Hayashi K., Hayashi T., Morita N. An extract from Spirulina platensis is a selective inhibitor of herpes simplex virus type 1 penetration into HeLa Cells. Phytother. Res. 1993;7:76–80. doi: 10.1002/ptr.2650070118. [DOI] [Google Scholar]
- 101.Hayashi K., Hayashi T., Kojima I. A natural sulfated polysaccharide, calcium spirulan, isolated from Spirulina platensis: In vitro and ex vivo evaluation of anti-herpes simplex virus and anti-human immunodeficiency virus activities. AIDS Res. Hum. Retroviruses. 1996;12:1463–1471. doi: 10.1089/aid.1996.12.1463. [DOI] [PubMed] [Google Scholar]
- 102.Lee J.B., Hayashi T., Hayashi K., Sankawa U. Structural analysis of calcium spirulan (Ca-SP)-derived oligosaccharides using electrospray ionization mass spectrometry. J. Nat. Prod. 2000;63:136–138. doi: 10.1021/np990348b. [DOI] [PubMed] [Google Scholar]
- 103.Rechter S., König T., Auerochs S., Thulke S., Walter H., Dörnenburg H., Walter C., Marschall M. Antiviral activity of Arthrospira-derived spirulan-like substances. Antiviral Res. 2006;72:197–206. doi: 10.1016/j.antiviral.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 104.Mader J., Gallo A., Schommartz T., Handke W., Nagel C.-H., Günther P., Brune W., Reich K. Calcium spirulan derived from Spirulina platensis inhibits herpes simplex virus 1 attachment to human keratinocytes and protects against herpes labialis. J. Allergy Clin. Immunol. 2016;137:197–203.e3. doi: 10.1016/j.jaci.2015.07.027. [DOI] [PubMed] [Google Scholar]
- 105.Hayakawa Y., Hayashi T., Hayashi K., Ozawa T., Niiya K., Sakuragawa N. Calcium spirulan as an inducer of tissue-type plasminogen activator in human fetal lung fibroblasts. Biochim Biophys Acta. 1997;1355:241–247. doi: 10.1016/S0167-4889(96)00137-1. [DOI] [PubMed] [Google Scholar]
- 106.Mishima T., Murata J., Toyoshima M., Fujii H., Nakajima M., Hayashi T., Kato T., Saiki I. Inhibition of tumor invasion and metastasis by calcium spirulan (Ca-SP), a novel sulfated polysaccharide derived from a blue-green alga, Spirulina platensis. Clin. Exp. Metastasis. 1998;16:541–550. doi: 10.1023/A:1006594318633. [DOI] [PubMed] [Google Scholar]
- 107.Chen Y.-H., Chang G.-K., Kuo S.-M., Huang S.-Y., Hu I.C., Lo Y.-L., Shih S.-R. Well-tolerated Spirulina extract inhibits influenza virus replication and reduces virus-induced mortality. Sci. Rep. 2016;6:24253. doi: 10.1038/srep24253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ratha S.K., Renuka N., Rawat I., Tech M., Bux F. Prospective options of algae-derived nutraceuticals as supplements to combat COVID-19 and human coronavirus diseases. Nutrition. 2021;83:111089. doi: 10.1016/j.nut.2020.111089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hirahashi T., Matsumoto M., Hazeki K., Saeki Y., Ui M., Seya T. Activation of the human innate immune system by Spirulina: Augmentation of interferon production and NK cytotoxicity by oral administration of hot water extract of Spirulina platensis. Int. Immunopharmacol. 2002;2:423–434. doi: 10.1016/S1567-5769(01)00166-7. [DOI] [PubMed] [Google Scholar]
- 110.Ngo-Matip M.-E., Pieme C.A., Azabji-Kenfack M., Moukette B.M., Korosky E., Stefanini P., Ngogang J.Y., Mbofung C.M. Impact of daily supplementation of Spirulina platensis on the immune system of naïve HIV-1 patients in Cameroon: A 12-months single blind, randomized, multicenter trial. Nutr. J. 2015;14:70. doi: 10.1186/s12937-015-0058-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Heo S.-Y., Ko S.-C., Kim C.S., Oh G.-W., Ryu B., Qian Z.-J., Kim G., Park W.S., Choi I.-W., Phan T.T.V., et al. A heptameric peptide purified from Spirulina sp. gastrointestinal hydrolysate inhibits angiotensin I-converting enzyme- and angiotensin II-induced vascular dysfunction in human endothelial cells. Int. J. Mol. Med. 2017;39:1072–1082. doi: 10.3892/ijmm.2017.2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Anekthanakul K., Senachak J., Hongsthong A., Charoonratana T., Ruengjitchatchawalya M. Natural ACE inhibitory peptides discovery from Spirulina (Arthrospira platensis) strain C1. Peptides. 2019;118:170107. doi: 10.1016/j.peptides.2019.170107. [DOI] [PubMed] [Google Scholar]
- 113.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Christiansen C.F., Pottegård A., Heide-Jørgensen U., Bodilsen J., Søgaard O.S., Maeng M., Vistisen S.T., Schmidt M., Lund L.C., Reilev M., et al. SARS-CoV-2 infection and adverse outcomes in users of ACE inhibitors and angiotensin-receptor blockers: A nationwide case-control and cohort analysis. Thorax. 2020:1–10. doi: 10.1136/thoraxjnl-2020-215768. [DOI] [PubMed] [Google Scholar]
- 115.Cohen J.B., Hanff T.C., William P., Sweitzer N., Rosado-Santander N.R., Medina C., Rodriguez-Mori J.E., Renna N., Chang T.I., Corrales-Medina V., et al. Continuation versus discontinuation of renin–angiotensin system inhibitors in patients admitted to hospital with COVID-19: A prospective, randomised, open-label trial. Lancet Respir. Med. 2021 doi: 10.1016/S2213-2600(20)30558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kanekiyo K., Lee J.-B., Hayashi K., Takenaka H., Hayakawa Y., Endo S., Hayashi T. Isolation of an antiviral polysaccharide, nostoflan, from a terrestrial cyanobacterium, Nostoc flagelliforme. J. Nat. Prod. 2005;68:1037–1041. doi: 10.1021/np050056c. [DOI] [PubMed] [Google Scholar]
- 117.Zainuddin E.N., Mentel R., Wray V., Jansen R., Nimtz M., Lalk M., Mundt S. Cyclic depsipeptides, ichthyopeptins A and B, from Microcystis ichthyoblabe. J. Nat. Prod. 2007;70:1084–1088. doi: 10.1021/np060303s. [DOI] [PubMed] [Google Scholar]
- 118.Neumann U., Forchert A., Flury T., Weckesser J. Microginin FR1, a linear peptide from a water bloom of Microcystis species. FEMS Microbiol Lett. 1997;153:475–478. doi: 10.1111/j.1574-6968.1997.tb12612.x. [DOI] [Google Scholar]
- 119.Kodani S., Suzuki S., Ishida K., Murakami M. Five new cyanobacterial peptides from water bloom materials of lake Teganuma (Japan) FEMS Microbiol. Lett. 1999;178:343–348. doi: 10.1111/j.1574-6968.1999.tb08697.x. [DOI] [Google Scholar]
- 120.Paiva F.C.R., Ferreira G.M., Trossini G.H.G., Pinto E. Identification, in vitro testing and molecular docking studies of microginins’ mechanism of angiotensin-converting enzyme inhibition. Molecules. 2017;22:1884. doi: 10.3390/molecules22121884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Okino T., Matsuda H., Murakami M., Yamaguchi K. Microginin, an angiotensin-converting enzyme inhibitor from the blue-green alga Microcystis aeruginosa. Tetrahedron. Lett. 1993;34:501–504. doi: 10.1016/0040-4039(93)85112-A. [DOI] [Google Scholar]
- 122.Zervou S.K., Gkelis S., Kaloudis T., Hiskia A., Mazur-Marzec H. New microginins from cyanobacteria of Greek freshwaters. Chemosphere. 2020;248:125961. doi: 10.1016/j.chemosphere.2020.125961. [DOI] [PubMed] [Google Scholar]
- 123.Lodin-Friedman A., Carmeli S. Microginins from a Microcystis sp. bloom material collected from the Kishon Reservoir, Israel. Mar. Drugs. 2018;16:78. doi: 10.3390/md16030078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ferreira G.M., Kronenberger T., de Almeida E.C., Sampaio J., Terra C.F., Pinto E., Trossini G.H.G. Inhibition of porcine aminopeptidase M (pAMP) by the pentapeptide microginins. Molecules. 2019;24:4369. doi: 10.3390/molecules24234369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ishida K., Kato T., Murakami M., Watanabe M., Watanabe M.F. Microginins, zinc metalloproteases inhibitors from the cyanobacterium Microcystis aeruginosa. Tetrahedron. 2000;56:8643–8656. doi: 10.1016/S0040-4020(00)00770-5. [DOI] [Google Scholar]
- 126.Gustafson K.R., Cardellina J.H., 2nd, Fuller R.W., Weislow O.S., Kiser R.F., Snader K.M., Patterson G.M., Boyd M.R. AIDS-antiviral sulfolipids from cyanobacteria (blue-green algae) J. Natl. Cancer Inst. 1989;81:1254–1258. doi: 10.1093/jnci/81.16.1254. [DOI] [PubMed] [Google Scholar]
- 127.Reshef V., Mizrachi E., Maretzki T., Silberstein C., Loya S., Hizi A., Carmeli S. New acylated sulfoglycolipids and digalactolipids and related known glycolipids from cyanobacteria with a potential to inhibit the reverse transcriptase of HIV-1. J. Nat. Prod. 1997;60:1251–1260. doi: 10.1021/np970327m. [DOI] [PubMed] [Google Scholar]
- 128.Loya S., Reshef V., Mizrachi E., Silberstein C., Rachamim Y., Carmeli S., Hizi A. The inhibition of the reverse transcriptase of HIV-1 by the natural sulfoglycolipids from cyanobacteria: Contribution of different moieties to their high potency. J. Nat. Prod. 1998;61:891–895. doi: 10.1021/np970585j. [DOI] [PubMed] [Google Scholar]
- 129.Pinzi L., Rastelli G. Molecular docking: Shifting paradigms in drug discovery. Int. J. Mol. Sci. 2019;20:4331. doi: 10.3390/ijms20184331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Naidoo D., Roy A., Kar P., Mutanda T., Anandraj A. Cyanobacterial metabolites as promising drug leads against the Mpro and PLpro of SARS-CoV-2: An in silico analysis. J. Biomol. Struct. Dyn. 2020:1–13. doi: 10.1080/07391102.2020.1794972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lipinski C.A. Lead- and drug-like compounds: The rule-of-five revolution. Drug Discov. Today Technol. 2004;1:337–341. doi: 10.1016/j.ddtec.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 132.Zainuddin E.N., Mundt S., Wegner U., Mentel R. Cyanobacteria a potential source of antiviral substances against influenza virus. Med. Microbiol. Immunol. 2002;191:181–182. doi: 10.1007/s00430-002-0142-1. [DOI] [PubMed] [Google Scholar]
- 133.Silva T., Salomon P.S., Hamerski L., Walter J., Menezes R.B., Siqueira J.A., Santos A., Santos J.A.M., Ferme N., Guimarães T., et al. Inhibitory effect of microalgae and cyanobacteria extracts on influenza virus replication and neuraminidase activity. PeerJ. 2018;6:e5716. doi: 10.7717/peerj.5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Deyab M., Mofeed J., El-Bilawy E., Ward F. Antiviral activity of five filamentous cyanobacteria against coxsackievirus B3 and rotavirus. Arch. Microbiol. 2020;202:213–223. doi: 10.1007/s00203-019-01734-9. [DOI] [PubMed] [Google Scholar]