Abstract
No-show appointments waste resources and decrease the sustainability of care. This study is an attempt to evaluate patient no-shows based on modes of appointment-making and types of appointments. We collected hospital information system data and appointment data including characteristics of patients, service providers, and clinical visits over a three-month period (1 September 2018 to 30 November 2018), at a large tertiary hospital in Seoul, Korea. We used multivariate logistic regression analyses to identify the factors associated with no-shows (Model 1). We further assessed no-shows by including the interaction term (“modes of appointment-making” X “type of appointment”) (Model 2). Among 1,252,127 appointments, the no-show rate was 6.12%. Among the modes of appointment-making, follow-up and online/telephone appointment were associated with higher odds of no-show compared to walk-in. Appointments for treatment and surgery had higher odds ratios of no-show compared to consultations. Tests for the interaction between the modes of appointment-making and type of appointment showed that follow-up for examination and online/telephone appointments for treatment and surgery had much higher odds ratios of no-shows. Other significant factors of no-shows include age, type of insurance, time of visit, lead time (time between scheduling and the appointment), type of visits, doctor’s position, and major diagnosis. Our results suggest that future approaches for predicting and addressing no-show should also consider and analyze the impact of modes of appointment-making and type of appointment on the model of prediction.
Keywords: no-show, health care resource planning, modes of appointment-making, types of appointment
1. Introduction
No-shows occur when a patient fails to attend a scheduled appointment with no prior notification to the hospital [1]. Terms identified as corresponding to “no-show” in existing literature included appointment breaking, nonattendance, dropping out, missed appointment, and appointment failures [2]. No-show appointments not only decrease the sustainability of care for individuals but also pose several challenges for health care systems, including wasted resources, longer wait times, and concomitant threats to future patient satisfaction [3,4]. It is a well-known fact that no-show decreases the service provider’s productivity and efficiency, increases healthcare costs, and limits the medical institution’s effective capacity [5]. Hence, from the perspectives of sustainable medical services and operational efficiencies, managing patients’ no-show behavior is essential [6].
The growing number of patients and limited service capacity have greatly increased the need for a hospital appointment system [7]. Although there are some differences based on size or type of medical institutions, on an average, 70–90% of all outpatient care cases are based on the appointment system in Korea [8]. From the perspective of patient experience management, the appointment system promotes the exchange of information between hospitals and patients by providing real-time information to allow patients to schedule appointments with their preferred doctors at a convenient time [6,9].
However, no-show rates range from 5% to 25% across different hospitals [10,11,12]. The literature suggests that socio-economic backgrounds, clinical environments, hospital characteristics, and types of appointment systems affect no-shows [10,12,13,14,15]. Past studies have found that no-shows occur in female, younger age, and Medical Aid I and II recipient patient groups [7,12,13,14,15]. Other factors shown to be associated with no-shows are region, day of the week and time of appointment, types of appointment (new or follow-up), and professional situation [12,16,17,18,19,20,21,22,23]. In addition, religious events and holidays, distance between the clinic and patients’ homes, remote area, lack of social support, and social deprivation had relevance to no-shows [24,25,26,27,28]. A study on the methodology of predicting no show utilized a hybrid probabilistic prediction framework based on the elastic net variable-selection methodology integrated with probabilistic Bayesian Belief Network [29].
In summary, several studies have been conducted to find important variables associated with no-shows. However, limited literature has examined whether the modes of appointment-making, types of appointment, and their interactions are associated with patient no-shows. There are several modes of appointment-making. To increase patient accessibility, many hospitals let patients schedule an appointment directly, either over the phone or online. Appointment types also matter in scheduling, provider efficiency, patient satisfaction, and maximizing patient revenues.
By identifying in which types of appointment patient no-shows occur most often and organizing appointments accordingly, hospitals can ensure more revenue, happy doctors, and satisfied patients. Furthermore, it has been reported that modes of appointment-making and occurrences of no-shows vary according to the types of appointment [12]. To our knowledge, no research in Korea has examined the factors of no-shows by considering the influence between modes of appointment-making and types of appointment.
This study aimed to identify the interactions between modes of appointment-making and types of appointment among factors related to no-shows. This study is significant in that it provides insight into important factors relative to no-shows and is the first study to exhibit interactions between modes of appointment-making and types of appointment.
This paper is organized as follows: In Section 2, Materials and Methods are summarized. Specifically, it addresses the subjects and data source, variables and measurement, and statistical analysis. Then, in Section 3, the results of this study are explained. In Section 4, demographic, appointment-related, and practice-related factors associated with no-shows are discussed, in addition to the limitations and strengths of this study. Finally, Section 5 concludes with the main findings of this study.
2. Materials and Methods
2.1. Subjects and Data Source
This study used data of patients who made an outpatient appointment at a tertiary hospital located in Seoul, Korea. The hospital is one of the largest general hospitals in Korea, operating 63 departments, and thus allowed a large number of and diverse patients to be included in the study sample. Data were collected from medical records and administration records of patients who had reserved outpatient care appointments from 1 September 2018 to 30 November 2018. In order to protect personal information, the patients’ personal identification number was used instead of the hospital registration number, which was also anonymized in the initial extraction stage. During this period, the total number of outpatients was 256,011, and the total number of appointments given was 1,252,127.
This study was reviewed by the Yonsei University Health System Institutional Review Board and was ruled exempt (IRB number: Y-2019-0097). Written informed consent from patients was waived as this was a secondary data analysis using de identified data.
2.2. Variables and Measurement
2.2.1. Dependent Variable
We examined the outpatient nursing department records for each patient to check the no-show status. All patients’ appointments were categorized as either “no-show” or “show-up.” No-show was defined as a patient who did not attend outpatient care on the day of the appointment [10].
2.2.2. Independent Variables
Demographic Characteristics
The demographic characteristics included were gender, age, region (based on the patient’s residence), and types of insurance. Patients were divided into seven groups based on their age (≤19, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69, and ≥70 years). We divided the regions of patient residence into three groups: Seoul, Incheon Gyeonggi, and other areas. This categorization was employed as the study hospital is located in Seoul, the largest city of Korea; the second group, Incheon and Gyeonggi, represents the two of the most populated regions in Korea following Seoul; lastly, the remaining 14 cities and do-provinces of Korea are categorized as other areas. We divided types of insurance into four groups: National Health Insurance, Medical Aid, Industrial Accident Compensation Insurance and Automobile Insurance, and International Insurance and Private Insurance.
Appointment Related Characteristics
Among the appointment related characteristics, we divided the modes of appointment-making into three groups: Follow-up, online or telephone, and walk-in. Follow-up appointments meant appointment for the next schedule after previous medical treatment in the hospital. Walk-in appointments indicate that a patient visited the hospital in person to make an appointment. We divided time of visit into six groups: before“ 9:00 a.m., 9:00 a.m.–11:00 a.m., 11:00 a.m.–13:00 p.m., 13:00 p.m.–15:00 p.m., 15:00 p.m.–17:00 p.m., and after 17:00 p.m. Days of a week were from Monday to Sunday, and Sundays included an examination reservation in addition to a treatment reservation. Lead time was the time between scheduling and the appointment and, in this study, was divided into less than 8 days, 8–14 days, 15–21 days, 22–28 days, 29–56 days, 57–84 days, and more than 85 days. Seven days represent one week; however, to avoid overlap among the periods, the weeks were indicated as days.
Practice-Related Characteristics
The practice-related characteristics included the types of visit, type of appointment, department, doctor’s positions, and patient’s major diagnosis. We divided type of visit into three groups: A (new patients at the study hospital), B (patients who had visited the clinical department before), and C (new patients at the clinical department, but those who had visited the study hospital before). There were three major appointment types: Consultation, examination, and treatment and surgery. We divided clinical departments into 10 groups: Internal medicine, surgery department, obstetrics and gynecology (OBGYN), pediatrics, ophthalmology, otolaryngology, dermatology, urology, neuropsychiatry, and others. The positions of the doctors were categorized into professional, fellow, and training positions. The categorization followed the progression of years and training required for a doctor to be specialized in a particular field in Korea as his or her seniority increases within the hospital. For instance, a doctor who is in a fellow position refers to a person who trains for 1–2 years at a department of his or her major after obtaining the license to become a resident doctor. Patients’ major diagnoses were classified according to the 22 major diagnoses based on the Korean standard classification of diseases-7 codes.
2.3. Statistical Analysis
A three-step analysis was performed. First, for all categorical variables, we used chi-square tests to calculate the distribution of patient characteristics according to no-show status. This test is commonly used to test association between two or more categorical variables. Second, multivariate logistic regression analysis was used to assess the factors associated with no-show (Model 1). Finally, the interaction term (“modes of appointment-making” x “types of appointment”) was included in Model 2. Multiple logistic regression was used for two main reasons. First, the no-show status, the dependent variable of this study, was a binary outcome (Show-up: 0; No-show: 1). Second, logistic regression is appropriate for handling relationships among outcome variables and independent variables. To control for multiple appointments by the same patient, we incorporated repeated measures by using the “repeated subject” option in the generalized estimating equation. Statistical significance was established at p < 0.05. SAS software (ver. 9.4; SAS Institute, Cary, NC, USA) was used for all calculations and analyses.
3. Results
3.1. Comparison of Characteristics between No-Shows and Show-Ups
Table 1 shows the comparison of characteristics between no-show and show-up. During the study period, the number of outpatient appointments was 1,252,127, and the no-show rate was 6.12%. Regarding demographic characteristics, the group of subjects who failed to show-up for their appointments comprised mostly men (6.4%), those ≤19 years (7.2%), patients residing in Seoul (6.5%), and recipients of Medical Aid (8.7%).
Table 1.
Comparison between no-shows and show-ups.
| Variables | Total | Show-Ups | No-Shows | p-Value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Demographic characteristics | |||||||
| Gender | |||||||
| Female | 667,734 | 53.3 | 628,559 | 94.1 | 39,175 | 5.9 | <0.0001 |
| Male | 584,393 | 46.7 | 546,895 | 93.6 | 37,498 | 6.4 | |
| Age | |||||||
| ≤19 | 173,825 | 13.9 | 161,291 | 92.8 | 12,534 | 7.2 | <0.0001 |
| 20–29 | 78,534 | 6.3 | 73,225 | 93.2 | 5309 | 6.8 | |
| 30–39 | 114,031 | 9.1 | 107,474 | 94.3 | 6557 | 5.8 | |
| 40–49 | 151,203 | 12.1 | 142,957 | 94.6 | 8246 | 5.5 | |
| 50–59 | 220,641 | 17.6 | 208,067 | 94.3 | 12,574 | 5.7 | |
| 60–69 | 249,549 | 19.9 | 235,529 | 94.4 | 14,020 | 5.6 | |
| ≥70 | 264,344 | 21.1 | 246,911 | 93.4 | 17,433 | 6.6 | |
| Region | |||||||
| Seoul | 721,492 | 57.6 | 674,846 | 93.5 | 46,646 | 6.5 | <0.0001 |
| Incheon·Gyeonggi area | 333,993 | 26.7 | 314,404 | 94.1 | 19,589 | 5.9 | |
| Other areas | 196,642 | 15.7 | 186,204 | 94.7 | 10,438 | 5.3 | |
| Types of insurance | |||||||
| National Health Insurance | 1,166,189 | 93.1 | 1,096,750 | 94.1 | 69,439 | 5.9 | <0.0001 |
| Medical Aid | 50,403 | 4.0 | 46,030 | 91.3 | 4373 | 8.7 | |
| Industrial Accident Compensation Insurance and Automobile Insurance |
10,929 | 0.9 | 10,164 | 93.0 | 765 | 7.0 | |
| International Insurance and Private Insurance |
24,606 | 2.0 | 22,510 | 91.5 | 2096 | 8.5 | |
| Appointment related characteristics | |||||||
| Modes of appointment-making | |||||||
| Walk-in | 59,187 | 4.7 | 52,922 | 89.4 | 6265 | 10.6 | <0.0001 |
| Follow-up | 1,178,836 | 94.1 | 1,109,091 | 94.1 | 69,745 | 5.9 | |
| Online/telephone | 14,104 | 1.1 | 13,441 | 95.3 | 663 | 4.7 | |
| Time of visit | |||||||
| 9:00–11:00 | 100,503 | 8.0 | 91,784 | 91.3 | 8719 | 8.7 | <0.0001 |
| <9:00 | 327,124 | 26.1 | 310,519 | 94.9 | 16,605 | 5.1 | |
| 11:00–13:00 | 269,994 | 21.6 | 253,514 | 93.9 | 16,480 | 6.1 | |
| 13:00–15:00 | 226,907 | 18.1 | 213,868 | 94.3 | 13,039 | 5.7 | |
| 15:00–17:00 | 236,243 | 18.9 | 221,798 | 93.9 | 14,445 | 6.1 | |
| ≥17:00 | 91,356 | 7.3 | 83,971 | 91.9 | 7385 | 8.1 | |
| Day of week | |||||||
| Monday | 255,286 | 20.4 | 240,098 | 94.1 | 15,188 | 5.9 | <0.0001 |
| Tuesday | 237,566 | 19.0 | 223,731 | 94.2 | 13,835 | 5.8 | |
| Wednesday | 226,738 | 18.1 | 213,466 | 94.2 | 13,272 | 5.8 | |
| Thursday | 266,325 | 21.3 | 250,448 | 94.0 | 15,877 | 6.0 | |
| Friday | 222,594 | 17.8 | 208,281 | 93.6 | 14,313 | 6.4 | |
| Weekend (Saturday and Sunday) | 43,618 | 3.5 | 39,430 | 90.4 | 4188 | 9.6 | |
| Lead time | |||||||
| Less than 8 days | 231,134 | 18.5 | 212,432 | 91.9 | 18,702 | 8.1 | <0.0001 |
| 8–14 days | 158,800 | 12.7 | 147,811 | 93.1 | 10,989 | 6.9 | |
| 15–21 days | 108,705 | 8.7 | 102,969 | 94.7 | 5736 | 5.3 | |
| 22–28 days | 74,548 | 6.0 | 70,371 | 94.4 | 4177 | 5.6 | |
| 29–56 days | 200,341 | 16.0 | 187,479 | 93.6 | 12,862 | 6.4 | |
| 57–84 days | 102,606 | 8.2 | 95,705 | 93.3 | 6901 | 6.7 | |
| More than 85 days | 375,993 | 30.0 | 358,687 | 95.4 | 17,306 | 4.6 | |
| Practice-related characteristics | |||||||
| Types of visit * | |||||||
| A | 79,990 | 6.4 | 78,914 | 98.7 | 1076 | 1.3 | <0.0001 |
| B | 1,015,836 | 81.1 | 949,339 | 93.5 | 66,497 | 6.5 | |
| C | 156,301 | 12.5 | 147,201 | 94.2 | 9100 | 5.8 | |
| Types of appointment | |||||||
| Consultation | 1,098,863 | 87.8 | 1,049,756 | 95.5 | 49,107 | 4.5 | <0.0001 |
| Examination | 15,831 | 1.3 | 11,059 | 69.9 | 4772 | 30.1 | |
| Treatment and surgery | 137,433 | 11.0 | 114,639 | 83.4 | 22,794 | 16.6 | |
| Department | |||||||
| Internal medicine | 437,833 | 35.0 | 413,638 | 94.5 | 24,195 | 5.5 | <0.0001 |
| Surgery department | 200,870 | 16.0 | 188,408 | 93.8 | 12,462 | 6.2 | |
| OBGYN | 64,137 | 5.1 | 61,235 | 95.5 | 2902 | 4.5 | |
| Pediatrics | 117,329 | 9.4 | 110,659 | 94.3 | 6670 | 5.7 | |
| Ophthalmology | 61,496 | 4.9 | 58,192 | 94.6 | 3304 | 5.4 | |
| Otolaryngology | 40,031 | 3.2 | 37,329 | 93.3 | 2702 | 6.7 | |
| Dermatology | 35,508 | 2.8 | 32,918 | 92.7 | 2590 | 7.3 | |
| Urology | 50,391 | 4.0 | 47,252 | 93.8 | 3139 | 6.2 | |
| Neuropsychiatry | 33,436 | 2.7 | 31,927 | 95.5 | 1509 | 4.5 | |
| Others | 211,096 | 16.9 | 193,896 | 91.9 | 17,200 | 8.1 | |
| Doctor’s position | |||||||
| Professional position | 1,142,108 | 91.2 | 1,072,506 | 93.9 | 69,602 | 6.1 | <0.0001 |
| Training position | 82,800 | 6.6 | 77,488 | 93.6 | 5312 | 6.4 | |
| Fellow position | 27,219 | 2.2 | 25,460 | 93.5 | 1759 | 6.5 | |
| Major diagnosis | |||||||
| A00-B99 | 12,821 | 1.0 | 11,866 | 92.6 | 955 | 7.4 | <0.0001 |
| C00-D48 | 159,483 | 12.7 | 146,806 | 92.1 | 12,677 | 7.9 | |
| D50-D89 | 38,148 | 3.0 | 35,573 | 93.3 | 2575 | 6.7 | |
| E00-E90 | 48,549 | 3.9 | 45,619 | 94.0 | 2930 | 6.0 | |
| F00-F99 | 26,763 | 2.1 | 25,757 | 96.2 | 1006 | 3.8 | |
| G00-G99 | 56,838 | 4.5 | 50,395 | 88.7 | 6443 | 11.3 | |
| H00-H59 | 41,301 | 3.3 | 38,061 | 92.2 | 3240 | 7.8 | |
| I00-I99 | 81,548 | 6.5 | 76,575 | 93.9 | 4973 | 6.1 | |
| J00-J99 | 24,509 | 2.0 | 22,515 | 91.9 | 1994 | 8.1 | |
| K00-K93 | 34,537 | 2.8 | 31,887 | 92.3 | 2650 | 7.7 | |
| L00-L99 | 19,304 | 1.5 | 18,148 | 94.0 | 1156 | 6.0 | |
| M00-M99 | 54,041 | 4.3 | 49,662 | 91.9 | 4379 | 8.1 | |
| N00-N99 | 46,461 | 3.7 | 41,779 | 89.9 | 4682 | 10.1 | |
| O00-P96 | 7025 | 0.6 | 6339 | 90.2 | 686 | 9.8 | |
| Q00-Q99 | 17,635 | 1.4 | 16,263 | 92.2 | 1372 | 7.8 | |
| R00-R99 | 56,723 | 4.5 | 51,220 | 90.3 | 5503 | 9.7 | |
| S00-T98 | 19,544 | 1.6 | 17,546 | 89.8 | 1998 | 10.2 | |
| U00-Z99 | 47,544 | 3.8 | 44,906 | 94.5 | 2638 | 5.5 | |
| No diagnosis | 459,353 | 36.7 | 444,537 | 96.8 | 14,816 | 3.2 | |
Note: * A: New patients at the study hospital; B: Patients who had visited the clinical department before; C: New patients at the clinical department, but those who had visited the study hospital before. Abbreviations: OBGYN, obstetrics and gynecology.
For appointment-related characteristics, regarding the modes of appointment-making, the no-show rate was higher for walk-in appointments (10.6%). In terms of the time of the visit, the no-show rate was higher for 9:00–11:00 a.m. category (8.7%) than at other times. Regarding the day of week, the no-show rate was higher on weekends (9.6%) than on the other days. Regarding, on lead time, the following groups had the highest no-show rates: Less than 8 days (8.1%), 8–14 days (6.9%), and 57–84 days (6.7%).
For practice-related characteristics, regarding types of visits, the no-show rate was the highest for re-visits (6.5%). Based on types of appointment, the following groups had the highest no-show rates: Examination (30.1%), treatment and surgery (16.6%), and consultation (4.5%). The department category others had the highest no-show rate of 8.1%, followed by dermatology (7.3%) and otolaryngology (6.7%). With regard to doctor’s position, the no-show rate was the highest for the fellow position (6.5%). Regarding patient’s diagnosis, diseases of the nervous system (G00-G99) had the highest no-show rate at 11.3%, followed by injury, poisoning, and certain other consequences of external causes (S00-T98) (10.2%), and diseases of the genitourinary system (N00-N99) (10.1%).
3.2. Factors Associated with No-Shows
Table 2 shows the results of the multivariate logistic regression (Model 1) identifying the factors associated with no-shows. Regarding the modes of appointment-making, follow-ups had a lower odds ratio of no-shows (OR = 0.86) than walk-in. The odds ratio for online/telephone-based appointments was not statistically significant. Patients who underwent planned examination, treatment, and surgery had a much higher odds ratio of no-shows than those with planned consultation (examination OR = 9.09; treatment and surgery OR = 4.51).
Table 2.
Multivariate logistic regression identifying the factors associated with no-shows.
| Variables | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||
| Demographic characteristics | ||||||||
| Gender | ||||||||
| Female | ref | |||||||
| Male | 1.05 | 1.03 | 1.08 | <.0001 | 1.05 | 1.03 | 1.08 | <0.0001 |
| Age | ||||||||
| ≤19 | ref | |||||||
| 20–29 | 1.05 | 0.99 | 1.11 | 0.1055 | 0.98 | 0.93 | 1.04 | 0.5295 |
| 30–39 | 0.91 | 0.86 | 0.97 | 0.0021 | 0.84 | 0.80 | 0.90 | <0.0001 |
| 40–49 | 0.81 | 0.76 | 0.85 | <.0001 | 0.74 | 0.70 | 0.79 | <0.0001 |
| 50–59 | 0.80 | 0.76 | 0.84 | <.0001 | 0.73 | 0.69 | 0.77 | <0.0001 |
| 60–69 | 0.78 | 0.74 | 0.82 | <.0001 | 0.71 | 0.67 | 0.75 | <0.0001 |
| ≥70 | 0.92 | 0.87 | 0.97 | 0.0026 | 0.84 | 0.79 | 0.89 | <0.0001 |
| Region | ||||||||
| Seoul | ref | |||||||
| Incheon·Gyeonggi area | 0.97 | 0.94 | 0.99 | 0.0136 | 0.97 | 0.94 | 1.00 | 0.0359 |
| Other areas | 0.97 | 0.94 | 1.00 | 0.0701 | 0.98 | 0.95 | 1.01 | 0.1947 |
| Types of insurance | ||||||||
| National Health Insurance | ref | |||||||
| Medical Aid | 1.29 | 1.21 | 1.37 | <.0001 | 1.29 | 1.21 | 1.37 | <0.0001 |
| Industrial Accident Compensation Insurance and Automobile Insurance | 0.96 | 0.82 | 1.13 | 0.6450 | 0.95 | 0.82 | 1.11 | 0.5459 |
| International Insurance and Private Insurance |
1.45 | 1.35 | 1.55 | <.0001 | 1.35 | 1.26 | 1.45 | <0.0001 |
| Appointment related characteristics | ||||||||
| Time of visit | ||||||||
| 9:00–11:00 | ref | |||||||
| <9:00 | 1.00 | 0.95 | 1.06 | 0.9182 | 0.98 | 0.93 | 1.04 | 0.5394 |
| 11:00–13:00 | 1.16 | 1.12 | 1.20 | <.0001 | 1.15 | 1.12 | 1.19 | <0.0001 |
| 13:00–15:00 | 1.10 | 1.06 | 1.14 | <.0001 | 1.09 | 1.05 | 1.13 | <0.0001 |
| 15:00–17:00 | 1.18 | 1.14 | 1.22 | <.0001 | 1.17 | 1.13 | 1.21 | <0.0001 |
| ≥17:00 | 1.33 | 1.27 | 1.39 | <.0001 | 1.31 | 1.25 | 1.37 | <0.0001 |
| Day of week | ||||||||
| Monday | ref | |||||||
| Tuesday | 0.96 | 0.92 | 0.99 | 0.0121 | 0.96 | 0.93 | 0.99 | 0.0236 |
| Wednesday | 0.97 | 0.94 | 1.01 | 0.1394 | 0.97 | 0.94 | 1.01 | 0.1742 |
| Thursday | 0.98 | 0.95 | 1.02 | 0.3351 | 0.99 | 0.95 | 1.02 | 0.4626 |
| Friday | 1.03 | 0.99 | 1.07 | 0.0963 | 1.03 | 1.00 | 1.07 | 0.0773 |
| Weekend (Saturday and Sunday) | 1.43 | 1.35 | 1.53 | <.0001 | 1.45 | 1.36 | 1.54 | <0.0001 |
| Lead time | ||||||||
| Less than 8 days | ref | |||||||
| 8–14 days | 0.88 | 0.85 | 0.92 | <.0001 | 0.88 | 0.85 | 0.92 | <0.0001 |
| 15–21 days | 0.81 | 0.78 | 0.85 | <.0001 | 0.80 | 0.77 | 0.84 | <0.0001 |
| 22–28 days | 0.88 | 0.84 | 0.93 | <.0001 | 0.88 | 0.83 | 0.92 | <0.0001 |
| 29–56 days | 1.04 | 1.00 | 1.09 | 0.0445 | 1.04 | 1.00 | 1.09 | 0.0470 |
| 57–84 days | 1.05 | 1.00 | 1.10 | 0.0447 | 1.05 | 1.00 | 1.11 | 0.0411 |
| More than 85 days | 0.98 | 0.94 | 1.02 | 0.2422 | 0.96 | 0.92 | 1.00 | 0.0358 |
| Practice-related characteristics | ||||||||
| Types of visit * | ||||||||
| A | ref | |||||||
| B | 1.01 | 0.98 | 1.04 | 0.4891 | 0.95 | 0.93 | 0.98 | 0.0019 |
| C | 0.30 | 0.28 | 0.32 | <.0001 | 0.29 | 0.27 | 0.32 | <0.0001 |
| Department | ||||||||
| Internal medicine | ref | |||||||
| Surgery department | 1.46 | 1.42 | 1.51 | <.0001 | 1.39 | 1.35 | 1.44 | <0.0001 |
| OBGYN | 0.99 | 0.93 | 1.04 | 0.6083 | 0.94 | 0.89 | 0.99 | 0.0312 |
| Pediatrics | 1.14 | 1.07 | 1.21 | <.0001 | 1.02 | 0.96 | 1.08 | 0.5791 |
| Ophthalmology | 1.21 | 1.14 | 1.29 | <.0001 | 1.15 | 1.09 | 1.23 | <0.0001 |
| Otolaryngology | 1.40 | 1.32 | 1.48 | <.0001 | 1.35 | 1.28 | 1.43 | <0.0001 |
| Dermatology | 2.21 | 2.08 | 2.36 | <.0001 | 2.15 | 2.01 | 2.29 | <0.0001 |
| Urology | 1.30 | 1.23 | 1.37 | <.0001 | 1.27 | 1.20 | 1.34 | <0.0001 |
| Neuropsychiatry | 1.59 | 1.45 | 1.74 | <.0001 | 1.58 | 1.44 | 1.73 | <0.0001 |
| Others | 0.67 | 0.64 | 0.71 | <.0001 | 0.71 | 0.68 | 0.74 | <0.0001 |
| Doctor’s position | ||||||||
| Professional position | ref | |||||||
| Training position | 1.24 | 1.19 | 1.29 | <.0001 | 1.26 | 1.21 | 1.31 | <0.0001 |
| Fellow position | 1.16 | 1.09 | 1.24 | <.0001 | 1.18 | 1.11 | 1.26 | <0.0001 |
| Major diagnosis | ||||||||
| C00-D48 | ref | |||||||
| A00-B99 | 0.96 | 0.89 | 1.03 | 0.2576 | 0.94 | 0.87 | 1.01 | 0.0912 |
| D50- D89 | 0.95 | 0.91 | 1.00 | 0.0405 | 0.95 | 0.90 | 0.99 | 0.026 |
| E00-E90 | 0.91 | 0.86 | 0.95 | 0.0001 | 0.88 | 0.84 | 0.93 | <0.0001 |
| F00-F99 | 0.40 | 0.36 | 0.45 | <.0001 | 0.39 | 0.35 | 0.43 | <0.0001 |
| G00-G99 | 1.15 | 1.10 | 1.21 | <.0001 | 1.13 | 1.08 | 1.18 | <0.0001 |
| H00-H59 | 1.14 | 1.08 | 1.21 | <.0001 | 1.13 | 1.07 | 1.19 | <0.0001 |
| I00-I99 | 0.92 | 0.88 | 0.96 | 0.0002 | 0.89 | 0.86 | 0.93 | <0.0001 |
| J00-J99 | 1.11 | 1.05 | 1.18 | 0.0002 | 1.08 | 1.02 | 1.15 | 0.0057 |
| K00-K93 | 1.12 | 1.06 | 1.18 | <.0001 | 1.11 | 1.05 | 1.17 | <0.0001 |
| L00-L99 | 0.39 | 0.36 | 0.43 | <.0001 | 0.39 | 0.35 | 0.43 | <0.0001 |
| M00-M99 | 0.93 | 0.88 | 0.98 | 0.0044 | 0.91 | 0.86 | 0.96 | 0.0002 |
| N00-N99 | 1.07 | 1.02 | 1.13 | 0.0037 | 1.06 | 1.01 | 1.11 | 0.0263 |
| O00-P96 | 1.11 | 1.01 | 1.22 | 0.0370 | 1.06 | 0.96 | 1.16 | 0.2732 |
| Q00-Q99 | 0.92 | 0.86 | 0.98 | 0.0115 | 0.92 | 0.87 | 0.98 | 0.0143 |
| R00-R99 | 1.23 | 1.18 | 1.28 | <.0001 | 1.20 | 1.15 | 1.24 | <0.0001 |
| S00-T98 | 1.06 | 0.99 | 1.13 | 0.1003 | 1.04 | 0.97 | 1.11 | 0.2939 |
| U00-Z99 | 0.88 | 0.85 | 0.92 | <.0001 | 0.88 | 0.84 | 0.92 | <0.0001 |
| No diagnosis | 0.44 | 0.43 | 0.46 | <.0001 | 0.42 | 0.41 | 0.43 | <0.0001 |
| Modes of appointment-making | ||||||||
| Walk-in | ref | ref | ||||||
| Follow-up | 0.86 | 0.82 | 0.91 | <.0001 | 1.36 | 1.24 | 1.49 | <0.0001 |
| Online/telephone | 1.11 | 0.99 | 1.24 | 0.0619 | 1.36 | 1.18 | 1.57 | <0.0001 |
| Types of appointment | ||||||||
| Consultation | ref | ref | ||||||
| Examination | 9.09 | 8.66 | 9.54 | <.0001 | 0.77 | 0.53 | 1.11 | 0.1610 |
| Treatment and surgery | 4.51 | 4.31 | 4.72 | <.0001 | 9.38 | 8.47 | 10.39 | <0.0001 |
|
Modes of appointment-making
× Types of appointment |
||||||||
| Follow-up × Examination | 12.59 | 8.67 | 18.27 | <0.0001 | ||||
| Follow-up × Treatment and Surgery | 0.39 | 0.35 | 0.44 | <0.0001 | ||||
| Online/telephone × Treatment and Surgery | 11.89 | 7.45 | 18.99 | <0.0001 | ||||
Note: * A: New patients at the study hospital; B: Patients who had visited the clinical department before; C: New patients at the clinical department, but those who had visited the study hospital before. Abbreviations: OR, odds ratio; CI, confidence interval; OBGYN, obstetrics and gynecology.
In the demographic characteristics of Model 1, for gender, the odds ratio was higher in males (OR = 1.05). Based on age, the odds ratio for other age groups was lower than for the group aged ≤19 years (30–39 OR = 0.91; 40–49 OR = 0.81; 50–59 OR = 0.80; 60–69 OR = 0.78; ≥70 OR = 0.92). The odds ratio for 20–29 groups was not statistically significant. For region, the odds ratio for patients residing in the Incheon·Gyeonggi area (OR = 1.07) was lower than that for patients residing in Seoul. Based on the type of insurance, the odds ratio for Medical Aid (OR = 1.29) and International Insurance and Private Insurance (OR = 1.45) were higher than those for National Health Insurance.
In terms of appointment related characteristics of Model 1, based on the time of visit, the odds ratio for other times was higher than that for 9:00–11:00 a.m. (11:00 a.m.–13:00 p.m. OR = 1.16; 13:00 p.m.–15:00 p.m. OR = 1.10; 15:00 p.m.–17:00 p.m. OR = 1.18; ≥17:00 p.m. OR = 1.33). Weekends (Saturday, Sunday) had a higher odds ratio than Monday (OR = 1.43), but the odds ratio for Tuesday was lower (OR = 0.96). Based on the lead time, the odds ratios for 8–14 days (OR = 0.88), 15–21 days (OR = 0.81), and 22–28 days (OR = 0.88) were lower than that for less than 8 days. However, the odds ratios for 29–56 days (OR = 1.04) and 57–84 days (OR = 1.05) were higher.
From practice-related characteristics, based on the type of visits, the odds ratio for C (new patients at the clinical department, but those who had visited the study hospital before) (OR = 0.30) was lower than that for A (new patients at the study hospital). Based on the department, the odds ratios for surgery, ophthalmology, otolaryngology, dermatology, urology, and neuropsychiatry (OR = 1.15 to 2.15) were higher than that for internal medicine, however the odds ratios for OBGYN and others (OBGYN OR = 0.94; others OR = 0.71) were lower. For the doctor’s position, the odds ratios for training position (OR=1.24) and fellow position (OR = 1.16) were higher than for professional position. From the diagnosis point of view, compared to neoplasms (C00-D48), diseases of the nervous system (G00-G99) (OR = 1.15), diseases of the ear and mastoid process (H00-H59) (OR = 1.12), diseases of the respiratory system (J00-J99) (OR = 1.11), diseases of the digestive system (K00-K93) (OR = 1.12), diseases of the genitourinary system (N00-N99) (OR = 1.07), pregnancy, childbirth, the puerperium, and certain conditions originating in the perinatal period (O00-P96) (OR = 1.11), and symptoms, signs, and abnormal clinical and laboratory findings, NEC (R00-R99) (OR = 1.23) had higher odds ratios of no-shows. While several diseases had lower odds ratios than neoplasms (C00-D48), no diagnosis (OR = 0.44) was the lowest.
3.3. The Interaction Term
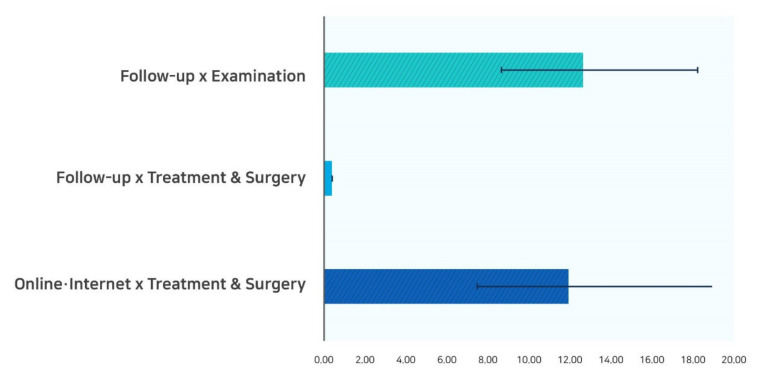
The interaction term is shown in Table 2. The interaction term between the modes of appointment-making and types of appointment was positive and statistically significant. As shown in Figure 1, for a follow-up patient, examination had a higher odds ratio of no-shows (OR = 12.59); however, treatment and surgery had a lower odds ratio (OR = 0.39). Patients with online telephone, treatment, and surgery had the highest odds ratio of no-shows (OR = 11.89).
Figure 1.
Multivariable logistic regression showing significant interaction between the modes of appointment-making and types of appointment.
4. Discussion
Identifying factors based on outpatient no-shows represents an important potential win–win for patients and hospitals by improving the sustainability of care and reducing wastage of resources. Our study demonstrates that demographic, appointment-related, and practice-related characteristics, which are factors readily available in the HIS data, can be successfully used to evaluate no-shows. Our study examined various factors associated with no-shows, focusing on the modes of appointment-making and types of appointment. The no-show rate in the study, 6.12%, is within the reported range of 5–25% according to the literature [10,11,12]. However, these studies had different timing of examination, examination period, and analysis perspective. Thus, it is difficult to directly compare the results of these studies with those of this study.
Several factors found to be influential for no-shows based on the literature review were also confirmed to be important factors in this study. The summary of the comparison between the factors associated with no-shows in this study and those in existing studies is as follows. First, our study showed that the odds ratio of no-shows for follow-up appointments in Model 2 considering interaction term. This finding might be related to how their needs are not addressed properly. Follow-up appointments are often scheduled after a patient has received a treatment, but it is scheduled to fit the department’s availability rather than the patients. However, in cases where patients themselves with medical conditions made online, telephone, or in-person appointments, the no-show ratio was lower because the appointment compliance was carried out actively by the patients according to their situation. Hospitals may need to prioritize appointment and medical service management with utmost consideration because high no-show ratio of follow-up patients has a direct and detrimental effect on their health [30,31,32].
Further, our study identified various factors including gender, age, region, types of insurance, time of visit, day of week, lead time, types of visit, types of appointment, department, doctor position, and major diagnosis as potential factors associated with no-shows.
In examining types of insurance, our study showed that the odds ratios for no-show for Medical Aid and International Insurance and Private Insurance were higher than that for National Health Insurance. This is similar to previous studies that showed that low-income patients covered by public assistance programs had higher odds of no-show [12,33,34], and patients with International Insurance and Private Insurance had higher odds of no-shows [12]. Medical institutions of Korea are categorized into three tiers: (1) Tertiary hospitals that provide specialized medical services, (2) primary medical institutions for basic medical services, and (3) clinics that have general practitioners for providing outpatient services [33]. A medical referral form issued by a sub-tier institution is required for patients to visit a tertiary hospital [35]. It is not difficult to obtain a referral at most medical institutions [35]. Patients with National Health Insurance visiting tertiary hospitals must pay 60% out-of-pocket expenses, while those with Medical Aid I pay a fixed amount of KRW 2000 and Medical Aid II pay 15% out-of-pocket expenses [36]. Thus, because Medical Aid patients can easily access high-tier medical institutions by paying relatively lower out-of-pocket expenses, they prefer tertiary hospitals that provide specialized medical services [35]. This phenomenon causes problems as the no-show rate increases. Moreover, owing to having no penalties—either financial or concerning future reservations—for no-shows, most patients are not watchful of no-shows. A no-show problem by Medical Aid patients has been brought up consistently as a major operative challenge for hospitals, suggesting the necessity of Medical Aid patient management.
Odds ratios for no-show were higher during Friday and weekends (Saturdays and Sundays), a finding similar to previous results that no-shows were most frequent on Fridays and Saturdays [37,38,39]. This result can be explained with the existing study that found more likelihood of no-shows in Friday reservations due to various events. On the contrary, some studies identified no-show were more likely to occur for Monday reservations than for weekend reservations. According to a study by Kwon et al. (2015) [12], which was conducted in the same study hospital, the days and likelihood of no-shows differed according to the types of appointment. In the case of consultation appointment, no-show was most frequent on Mondays, while Saturdays experienced the highest number of no-shows for a test, treatment, and surgery appointment. In the case of the study hospital, during weekends, especially on Sundays, most reservations are for diagnostic examinations, such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and Positron Emission Tomography (PET), other than a consultation. Accordingly, contradictory results between this study and the existing study can be explained by differences in the type of appointment according to the days of the week. Moreover, this may occur partially because such time slots (i.e., Sunday) are generally less used. Thus, further studies should be conducted considering different days of the week.
Increase in lead time, which is the time between the booking of the appointment to the actual day of the appointment, seems to raise the odds ratio of no-shows. The further the date of appointment, the more likely the patient is to not show up. It is possible that with increased lead time, patients are more likely to forget their appointment, have a scheduling conflict, or visit another hospital or physician’s office that gives them a closer appointment date [10,33]. According to Athenahealth, “an analysis of 4.2 million appointments scheduled in 2016 by 13,000 providers found that shorter appointment lead times can be critical to getting new patients in the door” [40]. Specifically, Athenahealth found that “on average, a new patient who waits more than a month for a first appointment is more than twice as likely to cancel and not reschedule as a new patient who is scheduled within a week.” [40].
Lower odds ratios for established patients compared to new patients also have important implications. Established patients may have a reason to be attached to a specific hospital. They may have experienced the warmth of the staff, care of the nurses, and insightfulness of the physicians. However, to a new patient, a hospital clinic may still be just a name on a page. This is not unique to healthcare; it is a concept well studied in behavioral economics called the endowment effect [41].
In terms of departments, odds ratios of no-shows were higher for surgery department, pediatrics, ophthalmology, otolaryngology, dermatology, urology, and neuropsychiatry. This implies that tertiary hospitals, in managing ambulatory care, should invest greater efforts to improve patient compliance.
Furthermore, this study also proved that other major diagnoses had a higher no-show rate compared to neoplasms (C00-D48) along with their higher no-show ratio of examination, and treatment, and surgery appointments. This result could be related to patients’ needs. Tertiary care requires patients to have a medical referral form issued by primary or secondary care facilities, and these documents are issued quite easily by most medical institutions. Therefore, easy access to top medical institutions has resulted in more options for patients, which then leads to them favoring tertiary hospitals that provide specialized medical services [34,35]. Inevitably, this creates a problem of higher no-show rates for subordinate medical institutions as patients flock to tertiary medical institutions [33]. Considering the long waiting period in tertiary hospitals, patients with mild medical conditions who do not require immediate care tend to make appointments at several hospitals simultaneously [33]. This finding is important as any intervention aimed at reducing no-shows should include the effects of the patient’s diagnosis.
Our variables of key interest were modes of appointment-making, types of appointments, and their interactions. The finding that both follow-up and online/telephone appointments had higher odds ratios compared to walk-in appointments may suggest that relatively easier modes of appointment-making increase the likelihood of no-shows. Among the types of appointments, treatment and surgery had a much higher odds ratio of no-show compared to consultation. Missed treatment or surgery disrupts schedules, and potentially leaves doctors and nurses with gaps during the workday. When examining the interaction between the modes of appointment-making and types of appointment, follow-up and examination appointment had a higher odds ratio of no-shows while treatment and surgery had a lower odds ratio.
Not every examination will lead to an operation or admission, but doctors could lose out on service time for other patients when patients miss potentially critical examination appointments. Hospitals faced with a patient who does not show up for an examination may lose revenue, but the greater financial impact could be the possible necessary service that never occurs.
Another interaction term indicates that for patients who made appointments for treatment or surgery online or by phone had much higher odds of no-show. One might assume that providing direct or easy scheduling will result in better patient access, and thus, a reduction in no-shows. However, we could not find results that indicate that direct or easy scheduling improves patient access. Rather, the results suggest that direct or telephone scheduling decreases patients’ frequency of access to care.
Our study suggests that it is important for hospital managers to manage no-show with a focus on two aspects. First, we recommend that hospitals design interventions to reduce no-shows of follow-up patients who visit for examination. In addition, it is helpful for hospitals to decrease no-shows of online or telephone appointment patients who visit for treatment and surgery. Second, hospital managers must treat the issue seriously and design effective interventions for managing no-shows. In addition to satisfying the basic requirements of fundamental medical services, hospitals can provide other supportive services, for example, more comfortable waiting rooms and personalized accompanying services for patients.
This study has several limitations. First, this study was based on data on outpatient reservations at a single tertiary hospital for three months. Thus, the research results cannot be generalized to all tertiary hospitals. Second, restrictions on data extraction may have led to exclusion of certain variables that may be a factor in no-shows. In addition, the analysis did not include medical expenses, history of no-shows, and reason for no-shows, which were found to be associated with no-shows in the previous study. Therefore, to overcome the limitations of existing studies and this study, future studies need to include multiple medical institutions, as well as variables such as past no-show history and reservation change history. Despite these limitations, our study is unique in that it considered the modes of appointment-making and types of appointments simultaneously to examine no-shows and established the need to address patients’ medical needs. In addition, the target hospital responsible for this study is one of the largest tertiary hospitals in South Korea, which made it possible to analyze multiple and large groups of patients’ medical cases.
5. Conclusions
No-shows contribute to reduced scheduling efficiency and lowered effectiveness of the medical services delivered [42]. Sustainability of care is essential to ensure maximum health benefits for patients [43]. There is a need to develop interventions that will improve clinic attendance among clients [43]. Our results suggest that future approaches for predicting and addressing no-shows should also consider and analyze the impact of the modes of appointment-making and types of appointment on the model of prediction. Still, because no-shows constitute a complex issue and are affected by cultural differences and varying hospital systems, it is desirable to consider a conservative approach when applying the intervention, considering the limited generalizability of the present findings.
Author Contributions
Conceptualization, M.Y.S. and T.H.K.; formal analysis, B.K. and C.H.Y.; writing—original draft preparation, M.Y.S. and B.K.; writing—review and editing, S.G.L. and T.H.K.; supervision, T.H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Yonsei University Health System Institutional Review Board, South Korea (IRB approval no. Y-2019-0097).
Informed Consent Statement
Patient consent was waived as this was a secondary data analysis using de identified data.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang Y., Hanauer D.A. Patient no-show predictive model development using multiple data sources for an effective overbooking approach. Appl. Clin. Inform. 2014;5:836–860. doi: 10.4338/ACI-2014-04-RA-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turkcan A., Nuti L., DeLaurentis P.C., Tian Z., Daggy J., Zhang L., Lawley M., Sands L. No-show modeling for adult ambulatory clinics. In: Denton B.T., editor. Handbook of Healthcare Operations Management. Volume 184. Springer; New York, NY, USA: 2013. pp. 251–288. [Google Scholar]
- 3.DuMontier C., Rindfleisch K., Pruszynski J., Frey J.J., 3rd A multi-method intervention to reduce no-shows in an urban residency clinic. Fam. Med. 2013;45:634–641. [PubMed] [Google Scholar]
- 4.Partin M.R., Burgess D.J., Burgess J.F., Jr., Gravely A., Haggstrom D., Lillie S.E., Nugent S., Powell A.A., Shaukat A., Walter L.C., et al. Organizational predictors of colonoscopy follow-up for positive fecal occult blood test results: An observational study. Cancer Epidemiol. Biomark. Prev. 2015;24:422–434. doi: 10.1158/1055-9965.EPI-14-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W.-Y., Gupta D. Adaptive appointment systems with patient preferences. Manuf. Serv. Oper. Manag. 2011;13:373–389. doi: 10.1287/msom.1110.0332. [DOI] [Google Scholar]
- 6.Hu M., Xu X., Li X., Che T. Managing patients’ no-show behaviour to improve the sustainability of hospital appointment systems: Exploring the conscious and unconscious determinants of no-show behaviour. J. Clean Prod. 2020;269:122318. doi: 10.1016/j.jclepro.2020.122318. [DOI] [Google Scholar]
- 7.Min D., Koo H. No-Show Related Factors for Outpatients at a Hospital. J. Soc. e-Bus. Stu. 2017;22:37–49. doi: 10.7838/jsebs.2017.22.1.037. [DOI] [Google Scholar]
- 8.Ko Y.K. The Relationships among Waiting Time, Patient’s Satisfaction, and Revisiting Intention of Outpatients in General Hospital. J. Korean Acad. Nurs. Adm. 2010;16:219–228. doi: 10.11111/jkana.2010.16.3.219. [DOI] [Google Scholar]
- 9.Hashim M.J., Franks P., Fiscella K. Effectiveness of telephone reminders in improving rate of appointments kept at an outpatient clinic: A randomized controlled trial. J. Am. Board Fam. Pract. 2001;14:193–196. [PubMed] [Google Scholar]
- 10.Daggy J., Lawley M., Willis D., Thayer D., Suelzer C., DeLaurentis P.C., Turkcan A., Chakraborty S., Sands L. Using no-show modeling to improve clinic performance. Health Inform. J. 2010;16:246–259. doi: 10.1177/1460458210380521. [DOI] [PubMed] [Google Scholar]
- 11.Guzek L.M., Fadel W.F., Golomb M.R. A Pilot Study of Reasons and Risk Factors for “No-Shows” in a Pediatric Neurology Clinic. J. Child Neurol. 2015;30:1295–1299. doi: 10.1177/0883073814559098. [DOI] [PubMed] [Google Scholar]
- 12.Kwon S.T., Lee Y.S., Han E., Kim T.H. Factors Associated with No-show in an Academic Medical Center. Korean Public Health Res. 2015;41:29–46. doi: 10.22900/kphr.2015.41.2.003. [DOI] [Google Scholar]
- 13.Gatrad A.R. Comparison of Asian and English non-attenders at a hospital outpatient department. Arch. Dis. Child. 1997;77:423–426. doi: 10.1136/adc.77.5.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neal R.D., Lawlor D.A., Allgar V., Colledge M., Ali S., Hassey A., Portz C., Wilson A. Missed appointments in general practice: Retrospective data analysis from four practices. Br. J. Gen. Pract. 2001;51:830–832. [PMC free article] [PubMed] [Google Scholar]
- 15.Weingarten N., Meyer D.L., Schneid J.A. Failed appointments in residency practices: Who misses them and what providers are most affected? J. Am. Board Fam. Pract. 1997;10:407–411. [PubMed] [Google Scholar]
- 16.Alaeddini A., Yang K., Reddy C., Yu S. A probabilistic model for predicting the probability of no-show in hospital appointments. Health Care Manag. Sci. 2011;14:146–157. doi: 10.1007/s10729-011-9148-9. [DOI] [PubMed] [Google Scholar]
- 17.Blumenthal D.M., Singal G., Mangla S.S., Macklin E.A., Chung D.C. Predicting Non-Adherence with Outpatient Colonoscopy Using a Novel Electronic Tool that Measures Prior Non-Adherence. J. Gen. Intern. Med. 2015;30:724–731. doi: 10.1007/s11606-014-3165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kopach R., DeLaurentis P.C., Lawley M., Muthuraman K., Ozsen L., Rardin R., Wan H., Intrevado P., Qu X., Willis D. Effects of clinical characteristics on successful open access scheduling. Health Care Manag. Sci. 2007;10:111–124. doi: 10.1007/s10729-007-9008-9. [DOI] [PubMed] [Google Scholar]
- 19.Lee V.J., Earnest A., Chen M.I., Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. BMC Health Serv. Res. 2005;5:51. doi: 10.1186/1472-6963-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norris J.B., Kumar C., Chand S., Moskowitz H., Shade S.A., Willis D.R. An empirical investigation into factors affecting patient cancellations and no-shows at outpatient clinics. Dec. Support Syst. 2014;57:428–443. doi: 10.1016/j.dss.2012.10.048. [DOI] [Google Scholar]
- 21.Pesata V., Pallija G., Webb A.A. A descriptive study of missed appointments: Families’ perceptions of barriers to care. J. Pediatr. Health Care. 1999;13:178–182. doi: 10.1016/S0891-5245(99)90037-8. [DOI] [PubMed] [Google Scholar]
- 22.Starkenburg R.J., Rosner F., Crowley K. Missed appointments among patients new to a general medical clinic. N. Y. State J. Med. 1988;88:473–475. [PubMed] [Google Scholar]
- 23.Vikander T., Parnicky K., Demers R., Frisof K., Demers P., Chase N. New-patient no-shows in an urban family practice center: Analysis and intervention. J. Fam. Pract. 1986;22:263–268. [PubMed] [Google Scholar]
- 24.Graber A., Davidson P., Brown A., McRae J., Woolridge K. Dropout and relapse during diabetes care. Diabetes Care. 1992;15:1477–1483. doi: 10.2337/diacare.15.11.1477. [DOI] [PubMed] [Google Scholar]
- 25.Johnson J., Weinert C., Richardson J. Rural residents’ use of cardiac rehabilitation programs. Public Health Nurs. 1998;15:288–296. doi: 10.1111/j.1525-1446.1998.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 26.Gucciardi E. A systematic review of attrition from diabetes education services: Strategies to improve attrition and retention research. Can. J. Diabetes. 2008;32:53–65. doi: 10.1016/S1499-2671(08)21011-7. [DOI] [Google Scholar]
- 27.Gatrad A.R. A completed audit to reduce hospital outpatients non-attendance rates. Arch. Dis. Child. 2000;82:59–61. doi: 10.1136/adc.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharp D.J., Hamilton W. Non-attendance at general practices and outpatient clinics. BMJ. 2001;323:1081–1082. doi: 10.1136/bmj.323.7321.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Topuz K., Uner H., Oztekin A., Yildirim M.B. Predicting pediatric clinic no-shows: A decision analytic framework using elastic net and Bayesian belief network. Ann. Oper. Res. 2018;263:479–499. doi: 10.1007/s10479-017-2489-0. [DOI] [Google Scholar]
- 30.Harvey H.B., Liu C., Ai J., Jaworsky C., Guerrier C.E., Flores E., Pianykh O. Predicting No-Shows in Radiology Using Regression Modeling of Data Available in the Electronic Medical Record. J. Am. Coll. Radiol. 2017;14:1303–1309. doi: 10.1016/j.jacr.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 31.Hwang A.S., Atlas S.J., Cronin P., Ashburner J.M., Shah S.J., He W., Hong C.S. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J. Gen. Intern. Med. 2015;30:1426–1433. doi: 10.1007/s11606-015-3252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaplan-Lewis E., Percac-Lima S. No-show to primary care appointments: Why patients do not come. J. Prim. Care Community Health. 2013;4:251–255. doi: 10.1177/2150131913498513. [DOI] [PubMed] [Google Scholar]
- 33.Lee Y.S., Kim T.H., Kim J. Association between missed appointment and related factors of patients with cancer in a tertiary hospital. Int. J. Health Plan. Manag. 2018 doi: 10.1002/hpm.2551. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization . Regional Office for the Western, P. Republic of Korea Health System Review. WHO Regional Office for the Western Pacific; Manila, Philippines: 2015. [Google Scholar]
- 35.Song Y.J. The South Korean health care system. JMAJ. 2009;52:206–209. [Google Scholar]
- 36.Ministry of Health and Welfare . 2018 Welfare Services Guidelines. Ministry of Health and Welfare; Sejong, Korea: 2018. p. 37. [Google Scholar]
- 37.Horsley B.P., Lindauer S.J., Shroff B., Tüfekçi E., Abubaker A.O., Fowler C.E., Maxfield B.J. Appointment keeping behavior of Medicaid vs non-Medicaid orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2007;132:49–53. doi: 10.1016/j.ajodo.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 38.Iben P., Kanellis M.J., Warren J. Appointment-keeping behavior of Medicaid-enrolled pediatric dental patients in eastern Iowa. Pediatr. Dent. 2000;22:325–329. [PubMed] [Google Scholar]
- 39.Kim K.H., Han S.T., Kang H., Sohn B. A preventive model to cancel reservation of new patients using the health information data base. JKDAS. 2004;6:1817–1827. [Google Scholar]
- 40.Hayhurst C. To Retain New Patients, Give Them an Appointment Stat. [(accessed on 12 November 2020)]; Available online: https://www.athenahealth.com/knowledge-hub/financial-performance/retain-new-patients-give-them-appointment-stat.
- 41.Rice T. The behavioral economics of health and health care. Annu. Rev. Public Health. 2013;34:431–447. doi: 10.1146/annurev-publhealth-031912-114353. [DOI] [PubMed] [Google Scholar]
- 42.DeFife J.A., Conklin C.Z., Smith J.M., Poole J. Psychotherapy appointment no-shows: Rates and reasons. Psychotherapy. 2010;47:413–417. doi: 10.1037/a0021168. [DOI] [PubMed] [Google Scholar]
- 43.Kunutsor S., Walley J., Katabira E., Muchuro S., Balidawa H., Namagala E., Ikoona E. Clinic Attendance for Medication Refills and Medication Adherence amongst an Antiretroviral Treatment Cohort in Uganda: A Prospective Study. AIDS Res. Treat. 2010;2010:872396. doi: 10.1155/2010/872396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.