Abstract
Background.
Maternal mortality is an issue of growing concern in the US, where incidence of death during pregnancy and postpartum appears to be increasing. The purpose of this analysis was to explore whether residing in a maternity care desert (defined as a county with no hospital offering obstetric care and no OB/GYN or certified nurse midwife providers) was associated with risk of death during pregnancy and up to 1 year postpartum among women in Louisiana from 2016–2017.
Methods.
Data provided by the March of Dimes were used to classify Louisiana parishes by level of access to maternity care. Using data on all pregnancy-associated deaths verified by the Louisiana Department of Health (n=112 from 2016–2017) and geocoded live births occurring in Louisiana during the same time period (n=101,484), we fit adjusted modified Poisson regression models with generalized estimating equations and exploratory spatial analysis to identify significant associations between place of residence and risk of death.
Results.
We found that risk of death during pregnancy and up to 1 year postpartum due to any cause (pregnancy-associated mortality) and in particular death due to obstetric causes (pregnancy-related mortality) was significantly elevated among women residing in maternity care deserts compared to women in areas with greater access (aRR for pregnancy-associated mortality=1.91, 95% CI=1.15–3.18; aRR for pregnancy-related mortality=3.37, 95% CI=1.71–6.65). A large racial inequity in risk persisted above and beyond differences in geographic access to maternity care (non-Hispanic Black vs. non-Hispanic White aRR for pregnancy-associated mortality=2.22, 95% CI=1.39, 3.56; aRR for pregnancy-related mortality=2.66, 95% CI=1.16, 6.12).
Conclusions.
Ensuring access to maternity care may be an important step towards maternal mortality prevention, but may alone be insufficient for achieving maternal health equity.
Maternal mortality is an issue of growing concern in the US, where incidence of death among women who are pregnant or up to 1 year postpartum continues to rise, in opposition to global trends (“Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015,” 2016). Reasons underlying maternal mortality in this country extend beyond clinical risk factors such as maternal age, and are rooted in the social, economic, and geographic conditions that shape uneven access to health-promoting resources and opportunities across the life course (Ruiz et al., 2015). In particular, the historical and ongoing oppression of Black people – structural racism established at time of the nation’s founding and upheld by present day policies and practices (Bailey et al., 2017) – is reflected in the vast and persistent racial inequity in maternal death. Maternal mortality ratios remain three to four-fold higher among Black women compared to White women (Benno, 2020; Petersen et al., 2019).
Access to continuous, high-quality maternal health care in the time surrounding pregnancy is key to preventing birth-related complications for women and their children. However, many women encounter barriers to care that prevent them from fully accessing the care that they need to maintain a healthy pregnancy (Derose, Gresenz, & Ringel, 2011). Geographic availability is an important aspect of access and availability of maternal healthcare, especially for rural women who are greatly affected by the increasing number of hospital closures in their communities (Balasubramanian & Jones, 2016; Hung, Henning-Smith, Casey, & Kozhimannil, 2017). Between 2004 and 2014, rural counties in the US saw hospital-based obstetric services decline from 54% to 45%, and this decline is predicted to continue. A recent study found that loss of hospital-based obstetric services in rural counties not adjacent to urban areas, compared with counties with continual services, is associated with increases in out-of-hospital and preterm births and births in hospitals without obstetric units in the following year (Kozhimannil, Hung, Henning-Smith, Casey, & Prasad, 2018). Concurrently, drawing on the findings from maternal mortality review committees in 13 states from 2013–2017, a recent report by the Centers for Disease Control and Prevention identified communities with limited access to clinical care and inadequate receipt of care/care coordination across systems as key factors contributing to rising incidence of maternal mortality and necessitating targeted prevention strategies (Petersen et al., 2019).
Lack of access to care due to unavailability of services may impact maternal health outcomes directly by delaying entry into prenatal care or increasing travel time to obtain care, both of which may increase risk for the woman and the neonate (Attar, Hanrahan, Lang, Gates, & Bratton, 2006; Grzybowski, Stoll, & Kornelsen, 2011). Additionally, communities located in areas with limited or no access to health care services may already be at elevated risk for adverse health consequences given the co-located burdens of economic hardship, lack of community resources including employment and health insurance coverage, and inadequate transportation and other public service systems (Probst, Moore, Glover, & Samuels, 2004). These factors in turn may be manifestations of structural racism and the intersection of racial and socioeconomic oppression (Williams & Collins, 2001) and therefore more likely to impact maternal morbidity and mortality among women of color and those with low incomes. Importantly, these issues are not exclusive to rural communities, but can occur in urban centers or adjacent areas when hospital closures disrupt continuity of care and exacerbate limitations of public transportation systems (March of Dimes, 2019). A Philadelphia study found that hospital obstetric care units that remained open after many surrounding closures over a nearly 20-year period faced more difficulties in providing complete and continuous maternal care due to resource strain, causing a brief increase in neonatal mortality (Lorch, Martin, Ranade, Srinivas, & Grande, 2014; Lorch, Srinivas, Ahlberg, & Small, 2013).
The degree to which geographic access to care and the geographic distribution of health-promoting resources may contribute to the current maternal mortality crisis in the US and exacerbate social inequities in mortality remains unclear. As independent jurisdictions within the US, states often make decisions about the distribution of such resources. This may, in part, contribute to the immense variation in risk of maternal death across US states, with Louisiana consistently ranking among those with the highest incidence. The purpose of this study was to explore the relationship between living in counties with limited or no access to maternity care (a maternity care desert) and risk of death during pregnancy and postpartum. We leveraged unique access to linked vital records, which overcome limitations of ecologic explorations of maternal mortality rates by allowing for the estimation of individual-level risk associated with place of residence in a retrospective cohort of pregnant and postpartum women in Louisiana from 2016–2017.
We hypothesized that women residing in areas with limited or no access to maternity care would be at increased risk of death during the pregnancy and postpartum period relative to those in counties with greater access. We explored this relationship with both pregnancy-associated mortality (death due to any cause during pregnancy or up to one year following the end of pregnancy) and within the subgroup of cases that constitute pregnancy-related mortality (death due to obstetric causes during pregnancy or up to one year since the end of pregnancy). Finally, we employed exploratory spatial analytic methods to assess spatial clustering of maternity care deserts within the state.
METHODS
Study population
Data on all verified cases of pregnancy-associated mortality from 2016–2017 (n=112) were provided by the Louisiana Department of Health. Deaths were verified as pregnancy-associated (death during pregnancy or up to 1 year postpartum from any cause) if a death record linked to a live birth or fetal death within 1 year and/or via the death record pregnancy checkbox indicating pregnancy status of the decedent. Pregnancy checkbox cases required additional review and verification by the Bureau of Family Health Regional Maternal and Child Health Coordinators. We created a retrospective analytic cohort of pregnant women in Louisiana from 2016–2017 by combining all live birth records issued to living women (n=125,537), live birth records with linked maternal death records (n=62), and unlinked maternal death records where no birth record was available because the decedent was pregnant at time of death (n=32) or linkage was not successful (n=18). Reasons for unsuccessful linkages may include data entry errors on the birth or death certificate variables used in the two-stage linkage procedure (maternal social security number, first and last name, and date of birth) or instances where the infant was put up for adoption.
For all records, address of residence was geocoded using ArcGIS software (ESRI Inc, Redlands, CA). We successfully identified geographic coordinates for all maternal deaths (n=112) and for over 80% of births (n=101,484). Those unable to be located included P.O. boxes (n=479), and records with missing or unknown errors in the house number, street name, or zip code variables (n=23,574). For records with missing or incorrect address data, we assigned parish of residence (county equivalent) based on the residential county Federal Information Processing System variable where available on the birth or death record (if discrepant, parish of residence on the birth record took precedence). The final analytic sample with georeferenced data was 124,197 (99% of records).
Among all cases of pregnancy-associated mortality we identified a subgroup of cases consisting of those that were pregnancy-related based on International Classification of Diseases 10th revision codes for underlying cause of death (Chapter XV: Pregnancy, childbirth, and the puerperium). We explored pregnancy-associated and pregnancy-related mortality separately in all analyses.
Maternity care deserts
A recent report by the March of Dimes (March of Dimes, 2019) used data from the 2016–2017 Area Health Resource File to describe availability of maternity care in every US county. Counties were classified by level of access to maternity care: those with access to maternity care, those with limited access to maternity care, and maternity care deserts. Maternity care deserts were counties with no hospitals offering obstetric care and no OB/GYN or certified nurse midwife providers. Counties with limited access to maternity care services had only 1 hospital providing obstetric services and fewer than 60 obstetric providers per 10,000 births. All other counties were classified as having access to maternity care. We extracted care level classification data from the March of Dimes report for every parish in Louisiana.
Individual-level covariates
In adjusted models we included individual-level sociodemographic characteristics known to be associated with reproductive health outcomes and available on the birth record: maternal age (<25, 25–29, 30–34, ≥35), race/ethnicity (non-Hispanic White; non-Hispanic Black; Hispanic, multiple, or other), and educational attainment as an indicator of socioeconomic position (less than high school, high school graduate, more than high school). In cases where only a maternal death record was available (n=55), decedent age, race, and educational attainment variables were coded to match birth record groupings described above. We additionally controlled for the delivery volume of the birth facility based on the number of births from 2016–2017, with >1000 deliveries considered high volume.
Parish-level covariates
In order to control for sociodemographic and geographic differences between parishes that may be associated with both the level of maternity care and other health-promoting resources available to parish residents, we obtained data from the American Community Survey (2017 5-year estimates) on parish poverty level and the percentage of the population with health insurance. We additionally controlled for the proportion of births 2016–2017 that were covered by Medicaid (data aggregated across birth records) to capture socioeconomic variation among the maternal population in particular. In order to characterize distance to neighboring parishes that may differ in level of maternity care or other health-promoting resources we included the geographic area of the parish in square miles (estimates based on the 2010 Census Redistricting Data Summary File)(Bureau, 2011). We controlled for whether the parish was mostly urban, mostly rural, or completely rural (classifications defined by the 2010 Census Urban and Rural Classification and Urban Area Criteria)(Bureau, 2012) given evidence of health care shortages in rural areas (beyond maternity care) and other structural and social barriers to health (Probst et al., 2004).
Statistical analyses
Descriptive statistics characterized the study population and the parishes in which they lived. To preserve confidentiality, we merged maternal characteristic subgroups with less than 10 pregnancy-associated deaths into larger categories prior to estimating crude mortality ratios and 95% confidence intervals. In order to estimate the relative risk of death (and 95% confidence interval) associated with living in a maternity care desert, we fit modified Poisson regression models with generalized estimating equations to account for the correlation between women residing in the same parish. We adjusted estimates for both individual- and parish-level covariates.
Finally, we applied exploratory spatial analysis to detect the presence of spatial clustering of maternity care deserts in order to identify broader regions of the state that may warrant additional concern. A global indicator of spatial autocorrelation (univariate Moran’s I) was used to detect the presence of spatial clustering of maternity care deserts. Where the global indicator revealed significant autocorrelation, we ran Local Indicators of Spatial Autocorrelation (LISA) tests to further identify parishes of limited or no access to maternity care that were surrounded by neighboring parishes with limited or no access to maternity care (i.e., high-high clusters). We used first-order queen contiguity spatial weights and 999 permutations for statistical inference in the Moran’s I analysis, conducted in Geoda 1.12.1.161. This study was approved by the Tulane University Institutional Review Board.
RESULTS
The vast majority of women in this study resided in urban parishes (84%), one third (33%) were under age 25 at the time of live birth or maternal death prior to delivery, and most were non-Hispanic White (51.6%) or non-Hispanic Black (36.6%), reflective of the state’s overall racial/ethnic composition (Table 1). Approximately one in four women (24%) resided in a county with limited or no access to maternity care, with 9% residing in a maternity care desert. Among the 112 verified cases of death, pregnancy-associated mortality ratios (per 100,000 live births) were highest among women in both ends of the age distribution, non-Hispanic Black women, those with less than a high school education, those residing in completely rural parishes, and those residing in maternity care deserts, although wide confidence intervals around ratio estimates reflect the small number of deaths occurring at each stratification. The unadjusted pregnancy-associated mortality ratio among non-Hispanic Black women was 2.9 times the mortality ratio among women of all other race/ethnicities (164.9 vs. 56.0 deaths per 100,000 live births, respectively). Fifty-four of the 112 total pregnancy-associated deaths (48.2%) were pregnancy-related.
Table 1.
Descriptive Characteristics of Live Births and Maternal Deaths Due to Any Cause in Louisiana, 2016–2017 (n=124,179).
| Total population | Maternal deaths | ||
|---|---|---|---|
| N (%) | Pregnancy-associated mortality ratio per 100,000 live births (95 % confidence interval) | ||
| Maternal age | |||
| <25 | 41,364 (33.3) | 104.0 (72.9, 135.0) | |
| 25–29 | 38,324 (30.9) | 67.8 (41.8, 93.9) | |
| 30–34 | 29,128 (23.5) | 92.7 (57.7, 127.6) | |
| 35+ | 15,363 (12.4) | 104.1 (53.1, 155.2) | |
| Race/ethnicity | |||
| Non-Hispanic White | 64,073 (51.6) | a | |
| Non-Hispanic Black | 45,496 (36.6) | 147.3 (112.0, 182.5) | |
| Hispanic, multiple, or other | 14,610 (11.8) | a | |
| Non-Hispanic White, Hispanic, multiple, or other | 57.2 (40.5, 73.9) | ||
| Educational attainment | |||
| Less than high school | 19,060 (15.4) | 157 (101.1–213.7) | |
| High school graduate | 39,412 (31.9) | 99.0 (67.9–130.0) | |
| Some college or associates degree | 64,994 (52.6) | 66.2 (46.4–85.9) | |
| Level of access to maternity care | |||
| Access to maternity care | 94,436 (76.1) | 90.0 (70.9, 109.1) | |
| Limited access to maternity care | 18,950 (15.3) | 79.2 (39.1–119.2) | |
| Maternity care desert | 10,793 (8.7) | 111.2 (48.3, 174.1) | |
| Residential parish urbanicity | |||
| Mostly urban | 104,080 (83.8) | 95.1 (76.4, 113.8) | |
| Mostly rural | 18,045 (14.5) | a | |
| Completely rural | 2,054 (1.7) | a | |
| Mostly or completely rural | 64.7 (29.5, 99.8) | ||
| Delivery facility volume | |||
| High (>1000 births) | 114,662 (92.3) | ||
| Low (≤1000 births) | 9,517 (7.7) | ||
| Mean (SD) | Mean (SD) | ||
| Percentage of residential parish population with health insurance | 87.6 (2.0) | 87.7 (1.8) | |
| Percentage of residential parish families living below the federal poverty level | 15.0 (4.1) | 14.7 (3.8) | |
| Residential parish geographic area (square miles) | 816.4 (406.4) | 796.5 (405.7) | |
| Percentage of residential parish 2016–2017 births covered by Medicaid | 62.1 (10.2) | 62.8 (9.5) | |
In order to preserve confidentiality, cells with small numbers of deaths (<10) were combined with larger categories prior to mortality ratio estimation (mostly rural combined with completely rural; non-Hispanic White combined with Hispanic, multiple, or other race/ethnicities).
Across Louisiana’s 64 parishes, 86% of the population, on average, had health insurance coverage, 17% of families were living below the federal poverty level, and 65% of births in 2016–2017 were covered by Medicaid (Table 2). The average size of a parish was 815 square miles, ranging from 203 to 2,429. Figure 1 panel A shows Louisiana parishes by level of access to care, with care deserts appearing predominantly—although not exclusively—outside of urban metropolitan areas. While most of the parishes with access to care were urban (61%), 23% of maternity care deserts (n=7) were also urban parishes (Table 2).
Table 2.
Descriptive Characteristics of Louisiana Parishes (n=64).
| Total (n=64) | Access to maternity care (n=28) | Limited access to maternity care (n=12) | Maternity care desert (n=24) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | |
| Percent of the population with health insurance | 86.3 (3.7) | 73.7–93.4 | 87.4 (1.3) | 85.2–90.0 | 88.0 (1.9) | 84.6–91.5 | 84.2 (5.1) | 20.3–88.3 |
| Percentage of families living below the federal poverty level | 17.0 (5.8) | 7.1–41.8 | 16.2 (4.1) | 8.2–25.1 | 14.4 (3.7) | 9.3–20.4 | 19.3 (7.4) | 7.1–41.8 |
| Parish geographic area (square miles) | 815.0 (444.6) | 203.0–2429.0 | 817.9 (417.7) | 203.0–2080.0 | 761.7 (360.5) | 303.0–1538.0 | 838.4 (521.9) | 258.0–2429.0 |
| Percentage of 2016–2017 births covered by Medicaid | 65.0 (12.8) | 20.3–88.3 | 66.1 (9.5) | 47.1–82.4 | 60.7 (13.9) | 34.7–78.0 | 66.0 (15.5) | 20.3–88.3 |
| N (%) | N (%) | N (%) | N (%) | |||||
| Urban/Rural | ||||||||
| classification | ||||||||
| Mostly urban | 31 (48.4) | 19 (61.3) | 5 (16.1) | 7 (22.6) | ||||
| Mostly rural | 24 (37.5) | 8 (33.3) | 6 (25.0) | 10 (41.7) | ||||
| Completely rural | 9 (14.1) | 1 (11.1) | 1 (11.1) | 7 (77.8) | ||||
Figure 1.
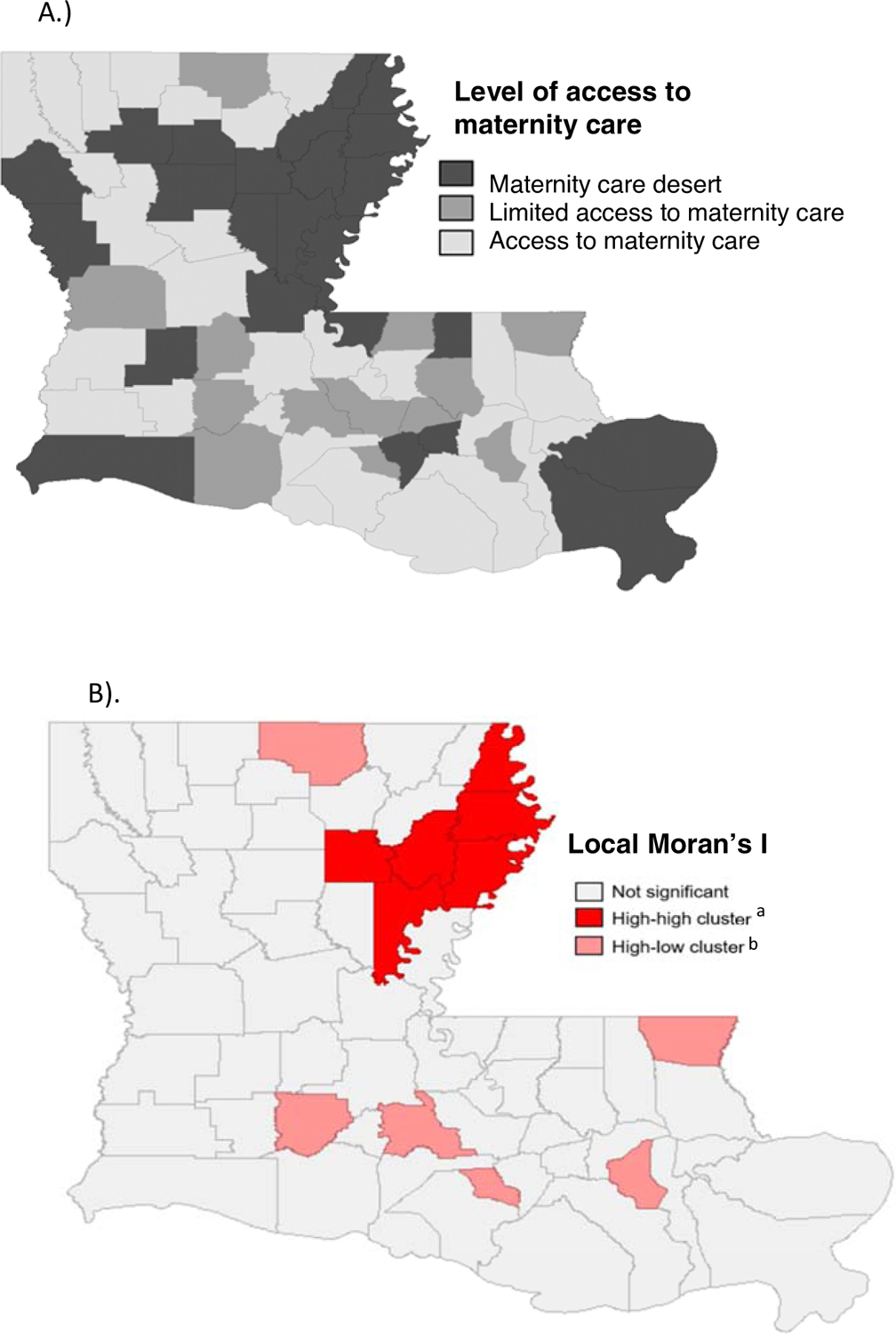
Maternity Care Access by Louisiana Parish and Local Moran’s I (LISA) Test for Spatial Autocorrelation of Maternity Care Deserts, 2016–2017.
A.) Level of maternity care access by Louisiana parish, 2016–2017.
B.) Local Moran’s I (LISA) test for spatial autocorrelation of maternity care deserts, Louisiana 2016–2017.
aHigh-high indicates parishes with limited or no access to maternity care surrounded by other parishes with limited or no access to maternity care.
bHigh-low indicates parishes with limit or no access to maternity care surrounded by parishes with access to maternity care.
In the fully adjusted model, residing in a maternity care desert was associated with a 91% increase in risk of pregnancy-associated death relative to parishes with access to maternity care, independent of parish size, urbanicity, sociodemographic levels, and individual characteristics (aRR=1.91, 95% CI: 1.15, 3.18). Residence in a maternity care desert was associated with a three-fold risk of pregnancy-related mortality, although imprecision of this estimate due to fewer cases is evident in the broad confidence interval (aRR=3.37, 95% CI: 1.71, 6.65). Controlling for access to maternity care and all other parish- and individual-level factors did little to reduce the racial disparity in mortality, with a persistent 2.2-fold greater risk among non-Hispanic Black women compared to White women (aRR for pregnancy-associated mortality=2.22, 95% CI: 1.39, 3.56).
Global Moran’s I for parish-level access to care was 0.16 (P=0.02) indicating significant spatial clustering of maternity care deserts. The tests for Local Spatial Autocorrelation (LISA map) revealed 6 limited or no access parishes surrounded by other limited or no access parishes (high-high spatial clusters) and 5 limited or no access parishes surrounded by parishes with access (high-low spatial outliers) (Figure 1 panel B).
DISCUSSION
The results from this analysis of all verified pregnancy-associated deaths in Louisiana from 2016–2017 highlight the importance of place as a significant contributor to risk of death among pregnant and postpartum women. We find that women living in parishes that lack access to maternal care experience a 91% increase in risk of death during pregnancy and up to 1 year postpartum, independent of her age, race/ethnicity, socioeconomic position, and whether she lived in a parish that was urban or rural, impoverished or underinsured. The association was larger in magnitude for pregnancy-related mortality compared to pregnancy-associated mortality, likely reflecting the importance of timely clinical treatment and care in obstetric emergencies. However, the significant albeit smaller magnitude of association with pregnancy-associated mortality suggests the importance of maternity care throughout pregnancy as a critical window of opportunity for prevention of non-obstetric causes of death as well. For many women who may not otherwise be in contact with services, maternity care visits may represent a rare opportunity to receive intimate partner violence screening and prevention, mental health and substance use screening and treatment, or education on healthy behaviors and practices (seat belt use, for example). These are critically important components of care encounters as homicide, suicide, and transport accidents remain leading causes of pregnancy-associated mortality in the US (Palladino, Singh, Campbell, Flynn, & Gold, 2011; Wallace, Crear-Perry, Mehta, & Theall, 2020; Wallace, Hoyert, Williams, & Mendola, 2016).
Of concern, we did not find a substantial reduction in the large racial inequity in maternal death between Black and White women after controlling for level of access to maternity care, parish- and individual-level sociodemographic characteristics. Previous research found that counties with larger numbers of non-Hispanic Black women had higher odds of losing all hospital obstetric services (Hung et al., 2017). This is alarming as the loss of hospital-based delivery services in communities already experiencing multiple forms of oppression are likely to aggravate persisting racial disparities in obstetric care and subsequently contribute to already severe racial inequities in maternal and birth outcomes (Grobman et al., 2015). Our finding of a persistent 2-fold greater risk experienced by Black women independent of their residential status (whether living in a maternity care desert or not) further implicates differential quality of care issues increasingly noted in the literature (Creanga et al., 2014; Fiscella & Sanders, 2016; Howell, Egorova, Balbierz, Zeitlin, & Hebert, 2016; Novick, 2009). Historically-embedded racism acting across multiple levels—individual health care provider bias, systemic racism within health care delivery systems, and structural racism within US society that engenders racially-segregated hospitals, the distribution of resources they receive and the quality of care they deliver—may be the most fundamental cause of this inequity (Prather, Fuller, Marshall, & Jeffries, 2016; Rosenthal & Lobel, 2011). Advancing our understanding of why the persistence of racial inequity in pregnancy-associated death extends beyond access to health care will require qualitative approaches to reveal the lived experiences of Black women, with particular attention to the complex and contextually-dependent barriers to their achieving optimal health before, during, and after pregnancy (Lawson & Marsh, 2017). Equally urgent is the need for research that identifies the ways in which structural racism continues to exclude Black people from access to power and resources, engendering population health inequities.
Through the conduct of exploratory spatial analysis, we identified a cluster of maternity care deserts within the northern region of the state that warrants further investigation. Longitudinal trends in maternal mortality in the northern region, or an exploration of severe maternal morbidity (which occurs at substantially greater incidence than mortality), may reveal significant maternal population health harms associated with living in this cluster of maternity care deserts.
This analysis has a number of limitations. First, this study is cross-sectional, and prohibits drawing causal conclusions or exploring the impact of changes in the health care access landscape on trends in maternal mortality over time. We have attempted to rule out alternative explanations for the apparent association between maternity care deserts and maternal death by adjusting estimates for differences between parishes that may be common causes of both. Still, we acknowledge the possibility of residual confounding by factors we are unable to measure (chronic disease prevalence or maternal social support, for example). Second, we used a single address of residence based on location at time of live birth (or death where no live birth record was available), and therefore we cannot explore or account for mobility and the possibility that women may have moved residences during the course of their pregnancy and postpartum periods. Because our data is limited to the state of Louisiana, we are also unable to spatially diagnose and account for the influence of surrounding counties located in other states, an issue that may be particularly important in the Mississippi delta region where a number of limited or no access Louisiana parishes share borders with counties in Mississippi. Finally, given the rarity of pregnancy-associated death in the study’s two-year period, we had limited power to explore sub-groups of death by cause or by sociodemographic characteristics. Even grouping those that were pregnancy-related yielded imprecise estimates. Additional years of data would increase analytic power, although would require careful consideration of the rapidly changing health care access landscape (hospital closures, insurance program expansions) that may occur when combining multiple years of data to yield more stable rates.
IMPLICATIONS FOR POLICY AND PRACTICE
Unequal geographic access to maternity care is an issue of concern not only for Louisiana, but for states across the US. Our findings support increased access to maternity care in the time surrounding pregnancy for prevention of pregnancy-related mortality and, although to a lesser extent, pregnancy-associated mortality. This may require greater coordination and resource sharing across hospital systems and settings to ensure complete geographic coverage; initiatives that provide logistical and financial support for women needing to travel for care; innovative interventions that incorporate technology, telemedicine, and novel models of supportive and preventive care delivery; and increased access to affordable, high-quality health care for women before, during, and after pregnancy. In 2018, the state’s perinatal regionalization system—a hospital classification system to ensure provision of risk-appropriate maternal care—began identifying obstetric levels of care specifically, while previously neonatal intensive care and maternal care were jointly considered. This system should help to facilitate transfer of women with high-risk conditions to facilities that are equipped to provide the appropriate levels of specialty care regardless of where they may be living (“Levels of Maternal Care: Obstetric Care Consensus No, 9,” 2019). Concurrently, improved access to care alone may be insufficient to reduce the deep and persistent racial inequity in maternal death. Future work should explore how additional health care system factors such a quality of care and respectful care interactions, continuity of care, and implementation of patient safety protocols may prevent future deaths. Moreover, broader examination of context beyond health care systems may continue to reveal social, structural and policy determinants that may be at play. Critically needed are interventions that begin to dismantle structural racism and remediate the harmful social contexts underlying pregnancy-associated mortality in the US.
Table 3.
Adjusted Relative Risks and 95% Confidence Intervals (CI) for Maternal Death in Association with Residence in a Maternity Care Desert,Louisiana 2016–2017.
| Pregnancy-associated mortality | Pregnancy-related mortality | |||
|---|---|---|---|---|
| Relative Risk | (95% CI) | Relative Risk | (95% CI) | |
| Level of access to maternity care | ||||
| Access to maternity care | Reference | |||
| Limited access to maternity care | 1.37 | (0.83–2.28) | 0.79 | (0.28–2.24) |
| Maternity care desert | 1.91 | (1.15–3.18) | 3.37 | (1.71–6.65) |
| Residential parish urbanicity | ||||
| Mostly urban | Reference | Reference | ||
| Mostly rural | 0.40 | (0.21–0.74) | 0.60 | (0.24–1.49) |
| Completely rural | 1.36 | (0.49–3.74) | 0.41 | (0.14–1.19) |
| Maternal age | ||||
| <25 | Reference | Reference | ||
| 25–29 | 0.81 | (0.50–1.32) | 1.80 | (0.84–3.83) |
| 30–34 | 1.25 | (0.73–2.12) | 2.17 | (0.95–4.92) |
| 35+ | 1.48 | (0.91–2.41) | 4.03 | (1.79–9.08) |
| Race/ethnicity | ||||
| Non-Hispanic White, | Reference | Reference | ||
| Non-Hispanic Black | 2.22 | (1.39–3.56) | 2.66 | (1.16–6.12) |
| Hispanic, multiple, or other | 0.52 | (0.22–1.22) | 0.64 | (0.19–1.50) |
| Educational attainment | ||||
| Less than high school | 2.39 | (1.50–3.81) | 2.90 | (1.35–6.21) |
| High school graduate/GED | 1.43 | (0.92–2.22) | 1.83 | (0.86–3.90) |
| More than high school | Reference | Reference | ||
| Percent of the population with health insurancea | 1.06 | (0.96–1.17) | 1.29 | (1.05–1.60) |
| Percentage of families living below the poverty levela | 0.93 | (0.88–0.97) | 0.84 | (0.78–0.91) |
| Parish geographic area (risk per 100 square miles) | 0.99 | (0.96–1.04) | 1.00 | (0.96–1.06) |
| Percentage of births covered by Medicaida | 1.04 | (1.01–1.07) | 1.07 | (1.02–1.13) |
| Delivery facility volume | ||||
| Low | Reference | |||
| High | 1.22 | (0.70–2.31) | 1.14 | (0.36–3.64) |
per 1-unit increase
Financial support:
This work was supported by the National Institute of Child Health and Human Development grant numbers R01HD092653 and R01HD096070. The funding source had no involvement in the conduct of the research or preparation of the article. Its contents are solely the responsibility of the authors and do not necessarily represent the official position of the National Institutes of Health or the Louisiana Department of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Attar MA, Hanrahan K, Lang SW, Gates MR, & Bratton SL (2006). Pregnant mothers out of the perinatal regionalization’s reach. J Perinatol, 26(4), 210–214. doi: 10.1038/sj.jp.7211488 [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: evidence and interventions. Lancet, 389(10077), 1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Balasubramanian SS, & Jones EC (2016). Hospital closures and the current healthcare climate: the future of rural hospitals in the USA. Rural Remote Health, 16(3), 3935. [PubMed] [Google Scholar]
- Benno J, Trichilo R, Gillispie-Bell V, Lake C. (2020). Louisiana Pregnancy-Associated Mortality Review 2017 Report. Retrieved from https://ldh.la.gov/assets/oph/Center-PHCH/Center-PH/maternal/2017_PAMR_Report_FINAL.pdf
- US Census Bureau. (2011). 2010 Census Redistricting Data (Public Law 94–171) Summary File. Retrieved from https://www.census.gov/prod/cen2010/doc/pl94-171.pdf
- US Census Bureau. (2012). 2010 Census Urban and Rural Classfication and Urban Area Criteria. Retrieved from https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
- Clayton D, & Kaldor J (1987). Empirical Bayes estimates of age-standardized relative risks for use in disease mapping. Biometrics, 43(3), 671–681. [PubMed] [Google Scholar]
- Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, & Callaghan WM (2014). Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol, 211(6), 647 e641–616. doi: 10.1016/j.ajog.2014.06.006 [DOI] [PubMed] [Google Scholar]
- Derose KP, Gresenz CR, & Ringel JS (2011). Understanding disparities in health care access--and reducing them--through a focus on public health. Health Aff (Millwood), 30(10), 1844–1851. doi: 10.1377/hlthaff.2011.0644 [DOI] [PubMed] [Google Scholar]
- March of Dimes. (2019). No Where to Go: Maternity Care Deserts Across the US. Retrieved from https://www.marchofdimes.org/materials/Nowhere_to_Go_Final.pdf
- Fiscella K, & Sanders MR (2016). Racial and Ethnic Disparities in the Quality of Health Care. Annu Rev Public Health, 37, 375–394. doi: 10.1146/annurev-publhealth-032315-021439 [DOI] [PubMed] [Google Scholar]
- Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. (2016). Lancet, 388(10053), 1775–1812. doi: 10.1016/S0140-6736(16)31470-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, … Human Development Maternal-Fetal Medicine Units, N. (2015). Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol, 125(6), 1460–1467. doi: 10.1097/AOG.0000000000000735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzybowski S, Stoll K, & Kornelsen J (2011). Distance matters: a population based study examining access to maternity services for rural women. BMC Health Serv Res, 11, 147. doi: 10.1186/1472-6963-11-147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Egorova N, Balbierz A, Zeitlin J, & Hebert PL (2016). Black-White differences in severe maternal morbidity and site of care. Am J Obstet Gynecol, 214(1), 122 e121–127. doi: 10.1016/j.ajog.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung P, Henning-Smith CE, Casey MM, & Kozhimannil KB (2017). Access To Obstetric Services In Rural Counties Still Declining, With 9 Percent Losing Services, 2004–14. Health Aff (Millwood), 36(9), 1663–1671. doi: 10.1377/hlthaff.2017.0338 [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, & Prasad S (2018). Association Between Loss of Hospital-Based Obstetric Services and Birth Outcomes in Rural Counties in the United States. JAMA, 319(12), 1239–1247. doi: 10.1001/jama.2018.1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson AK, & Marsh EE (2017). Hearing the Silenced Voices of Underserved Women: The Role of Qualitative Research in Gynecologic and Reproductive Care. Obstet Gynecol Clin North Am, 44(1), 109–120. doi: 10.1016/j.ogc.2016.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levels of Maternal Care: Obstetric Care Consensus No, 9. (2019). Obstet Gynecol, 134(2), e41–e55. doi: 10.1097/AOG.0000000000003383 [DOI] [PubMed] [Google Scholar]
- Lorch SA, Martin AE, Ranade R, Srinivas SK, & Grande D (2014). Lessons for providers and hospitals from Philadelphia’s obstetric services closures and consolidations, 1997–2012. Health Aff (Millwood), 33(12), 2162–2169. doi: 10.1377/hlthaff.2014.0136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorch SA, Srinivas SK, Ahlberg C, & Small DS (2013). The impact of obstetric unit closures on maternal and infant pregnancy outcomes. Health Serv Res, 48(2 Pt 1), 455–475. doi: 10.1111/j.1475-6773.2012.01455.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall RJ (1991). Mapping disease and mortality rates using empirical Bayes estimators. J R Stat Soc Ser C Appl Stat, 40(2), 283–294. [PubMed] [Google Scholar]
- Novick G (2009). Women’s Experience of Prenatal Care: An Integrative Review. Journal of Midwifery & Womens Health, 54(3), 226–237. doi: 10.1016/j.jmwh.2009.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palladino CL, Singh V, Campbell J, Flynn H, & Gold KJ (2011). Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstet Gynecol, 118(5), 1056–1063. doi: 10.1097/AOG.0b013e31823294da [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, … Barfield W (2019). Vital Signs: Pregnancy-Related Deaths, United States, 2011–2015, and Strategies for Prevention, 13 States, 2013–2017. MMWR Morb Mortal Wkly Rep, 68(18), 423–429. doi: 10.15585/mmwr.mm6818e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather C, Fuller TR, Marshall KJ, & Jeffries WL (2016). The Impact of Racism on the Sexual and Reproductive Health of African American Women. Journal of Womens Health, 25(7), 664–671. doi: 10.1089/jwh.2015.5637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst JC, Moore CG, Glover SH, & Samuels ME (2004). Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health, 94(10), 1695–1703. doi: 10.2105/ajph.94.10.1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L, & Lobel M (2011). Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med, 72(6), 977–983. doi: 10.1016/j.socscimed.2011.01.013 [DOI] [PubMed] [Google Scholar]
- Ruiz JI, Nuhu K, McDaniel JT, Popoff F, Izcovich A, & Criniti JM (2015). Inequality as a Powerful Predictor of Infant and Maternal Mortality around the World. Plos One, 10(10). doi:ARTN e0140796 10.1371/journal.pone.0140796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace ME, Crear-Perry J, Mehta P, & Theall KP (2020). Homicide During Pregnancy and the Postpartum Period in Louisiana, 2016–2017. JAMA Pediatr. doi: 10.1001/jamapediatrics.2019.5853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace ME, Hoyert D, Williams C, & Mendola P (2016). Pregnancy-associated homicide and suicide in 37 US states with enhanced pregnancy surveillance. Am J Obstet Gynecol, 215(3), 364 e361–364 e310. doi: 10.1016/j.ajog.2016.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C (2001). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports, 116(5), 404–416. doi:Doi 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]


