Abstract
Study objective:
We compare clinical management and outcomes of emergency department (ED) encounters by sex after implementation of a clinical care pathway in 15 community EDs that standardized recommendations based on patient risk, using the History, ECG, Age, Risk Factors, and Troponin (HEART) score.
Methods:
This was a retrospective analysis of adult ED encounters evaluated for suspected acute coronary syndrome with a documented HEART score from May 20, 2016, to December 1, 2017. The primary outcomes were hospitalization or 30-day stress testing. Secondary outcomes included 30-day acute myocardial infarction or all-cause death (major adverse cardiac event). A generalized estimating equation regression model was used to compare the odds of hospitalization or stress testing by sex; we report HEART scores (0 to 10) stratified by sex and describing major adverse cardiac events.
Results:
A total of 34,715 adult ED encounters met the inclusion criteria (56.0% women). A higher proportion of women were classified as low risk (60.5% versus 52.4%; odds ratio [OR] 1.39; 95% confidence interval [CI] 1.33 to 1.45). Women were hospitalized or received stress testing less frequently than men for low HEART scores (18.8% versus 22.8%; OR 0.79; 95% CI 0.73 to 0.84) and intermediate ones (46.7% versus 49.7%; OR 0.88; 95% CI 0.83 to 0.95), but similarly for high-risk ones (74.1% versus 74.4%; OR 0.99; 95% CI 0.77 to 1.28). Women had 18% lower odds of hospitalization or noninvasive cardiac testing (OR 0.82; 95% CI 0.78 to 0.86), even after adjusting for HEART score and comorbidities. Men had higher risks of major adverse cardiac events than women for all HEART score categories but was significantly higher among low-risk HEART scores (0.4% versus 0.1%).
Conclusion:
Women with low-risk HEART scores are hospitalized or stress tested less than men, which is likely appropriate, and women have better outcomes than men. Use of the HEART score has the potential to reduce sex disparities in acute coronary syndrome care.
INTRODUCTION
Background
Acute coronary syndrome is one of the most common health problems globally.1 It is the leading cause of morbidity and mortality and accounts for greater than 7 million emergency department (ED) encounters annually in the United States.2 Sex disparities in patient care for individuals presenting to the ED with suspected acute coronary syndrome have been well documented.3–5 For example, women are less likely to be admitted for hospitalization and revascularization and are less frequently referred for coronary angiography when presenting to the ED with chest pain.6–8 Women also present less frequently with elevations of troponin level, which can result in misdiagnosis or delayed treatment.9–12 It is known there are sex differences in risk factors and presenting symptoms for acute coronary syndrome,13,14 but whether these differences are associated with a disparity in risk stratification of acute coronary syndrome and differences in management and outcomes remains unclear.
Importance
Risk assessment can assist physicians in accurately estimating a patient’s cardiac risk. The History, ECG, Age, Risk Factors, and Troponin (HEART) score is a 0- to 10-point score derived from clinical assessment of a patient’s level of these factors. This simple risk-stratification tool can stratify patients into low-, moderate-, and high-risk groups based on estimates of short-term adverse cardiac outcomes. These risk scores have been proven to be effective in identifying patients who require further testing and hospitalization.15,16 A small European study reported sex differences in myocardial infarction, revascularization, and death rates between men and women in accordance with the HEART score, reporting higher cardiac events in men across every risk score category.17 Our previous work has found benefits to using the HEART score in evaluating a cohort that excludes acute myocardial infarction identified at the ED visit because HEART is not generally used to direct acute myocardial infarction care. Our reports have also discovered significant differences in the HEART score risks of a US population compared with a European one, with differences in HEART performance.18 However, little is known about whether standardizing suspected acute coronary syndrome risk assessment affects previously reported sex disparities in the acute management of patients.
Goals of This Investigation
This study used data collected from 15 community EDs that adopted a HEART care pathway to risk stratify adults with suspected acute coronary syndrome. We aimed to understand whether using a standardized risk score was associated with reduced sex disparities in management and outcomes. We compared rates of 30-day stress testing and hospitalization, as well as acute myocardial infarction and all-cause death between men and women, stratified by HEART scores to describe sex differences in acute chest pain management and outcomes.
MATERIALS AND METHODS
Study Design and Setting
We performed a retrospective analysis of data for all ED encounters at Kaiser Permanente Southern California hospitals between May 20, 2016, and December 1, 2017. Kaiser Permanente Southern California is an integrated health system providing health care for greater than 4 million members. These hospitals provide care to greater than 1 million ED patients per year (study sites range from ≈25,000 to 95,000 annual ED visits). Of these ED patients, approximately 80% are health plan members. All sites use the same troponin laboratory assay (Access AccuTnI+3; Beckman Coulter, Brea, CA), which currently uses a threshold of 0.5 ng/mL to rule in acute myocardial infarction for patients with suspected acute coronary syndrome. The study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Selection of Participants
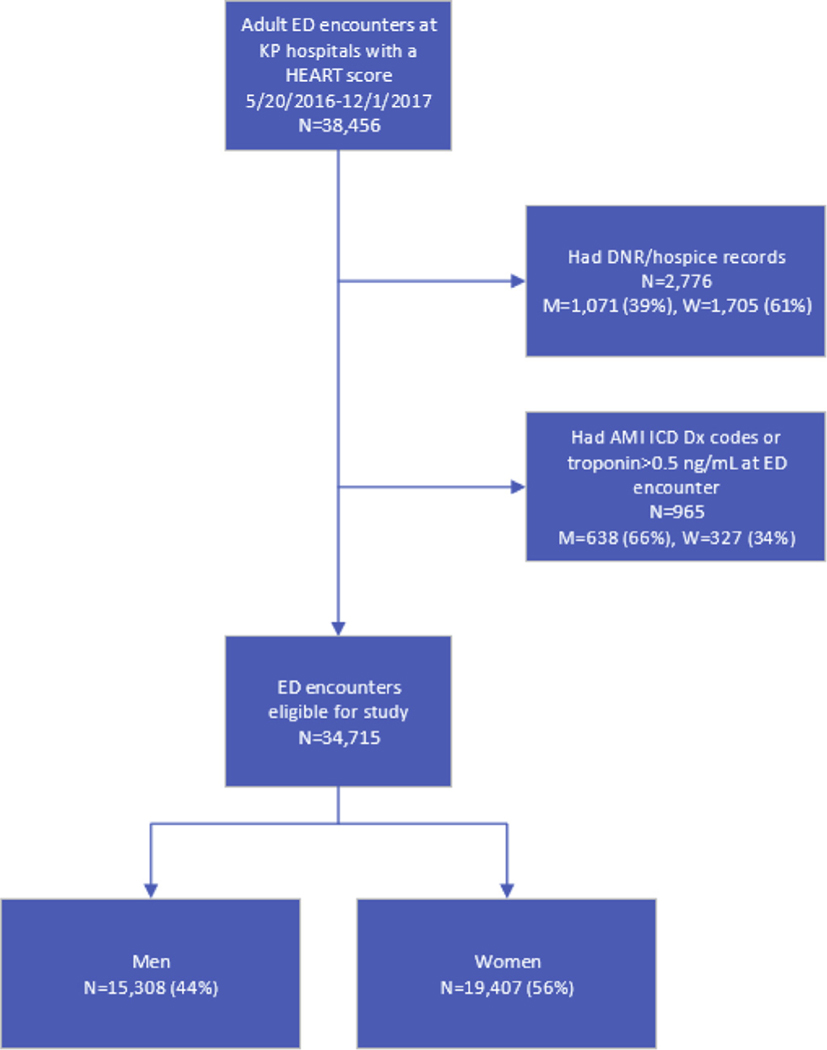
ED encounters were included for adult (≥18 years) Kaiser Permanente members with a physician-documented HEART score at 1 of 15 Kaiser Permanente Southern California hospitals. Of 224,177 ED encounters with a troponin-level test ordered from May 20, 2016, to December 1, 2017, 38,456 had a documented HEART score. Often, these tests are performed for vague symptoms (eg, generalized weakness, altered mental status, nausea) or for prognostic purposes (ischemic stroke or sepsis), but are unlikely to be conducted for primary evaluation of acute coronary syndrome. Among 60,497 encounters with a diagnosis of chest pain and a troponin-level test order, 23,202 (38%) had a documented HEART score. Patient encounters with non–health plan individuals were excluded because of inability to capture reliable outcome data. Patients who transferred from non-Kaiser hospitals or those who died at the ED were not included in the analysis. We excluded hospice patients and those with a do-not-resuscitate status. Patients who had an acute myocardial infarction identified in the ED (either troponin level >0.5 ng/mL or International Classification of Diseases [ICD] diagnosis codes 410.XX, I21.X, or I22.X) were also excluded from the analysis (Figure 1).
Figure 1.
Flow diagram of the patient cohort used for analysis. KP, Kaiser Permanente; DNR, do not resuscitate; M, men; W, women; Dx, diagnosis.
Interventions
Kaiser Permanente Southern California adopted a HEART care pathway to be used by emergency physicians during the clinical evaluation and management of patients with possible acute coronary syndrome. An online education module and multiple presentations disseminated information to all emergency physicians, summarizing current medical evidence related to the management of possible acute coronary syndrome. Decision support was embedded into the electronic health record (May 2016) and prompts alerted physicians to insert the history, ECG, and risk factors necessary to calculate a HEART score. The age and troponin values were automatically included to allow streamlined calculation of the HEART score. The details of this intervention, the clinical recommendations, and the effect of the intervention overall have been previously reported.18–20
Methods of Measurement
Patient demographic information, including age, sex, race, and ethnicity data, were obtained from administrative records, whereas education level was determined with population measures by home zip code. Clinical variables were obtained by querying the structured electronic medical records. Comorbidities such as coronary artery disease, diabetes, hypertension, and lipid disorder were identified in the medical record with ICD-9 and ICD-10 codes, as was history of coronary revascularization. Body mass index was measured from ED intake documentation or the most recently available visit, whereas smoking and family history of coronary artery disease were self-reported fields in electronic health records.
Outcome Measures
The primary outcome was 30-day stress testing or hospitalization after assessment at the ED encounter. Hospitalization included patients admitted as inpatients or under observation status after the initial evaluation at the ED encounter, whereas a stress test was defined as either an ED referral to a cardiology department for a noninvasive stress test or a direct order for stress testing during the ED encounter. Stress testing outcomes were measured until 30 days after the index encounter. The secondary outcome was 30-day major adverse cardiac events, consisting of all-cause death or acute myocardial infarction. ICD-9 and ICD-10 codes (410.XX, I21.X, or I22.X) were used to identify acute myocardial infarctions at hospital encounters after ED admission, whereas deaths came from both KSPSC hospitals and California state vital records. The percentage of encounters resulting in 30-day major adverse cardiac events for men and women is reported stratified by HEART score.
Primary Data Analysis
Continuous patient and encounter characteristics are summarized in the demographics and results tables with means and SDs, whereas categoric characteristics are presented as frequencies and column percentages. The percentage of men and women with the secondary outcomes of 30-day mortality or acute myocardial infarction is reported by HEART score. All tables and figures show results at the encounter level. We fit a logistic regression model to compare the odds of hospitalization or 30-day stress testing among different subpopulations. Multiple encounters by the same individual were accounted for with an exchangeable correlation structure using generalized estimating equations to address within-patient correlation. Odds ratios (ORs) and 95% confidence intervals (CIs) from the generalized estimating equation models are presented without covariates unless otherwise indicated. We identified variables considered for inclusion in the model according to literature review and consensus among our clinical authors: HEART score (0 to 10), age (continuous), race/ethnicity (Alaska Native/Pacific Islander, Asian, black, Hispanic, other, and white), medical center, college education (continuous percentage by zip code), body mass index (<18, 18 to 25, 25 to 30, and >30 kg/m2, or missing), smoking status (never or passive, quit, active, or missing), diabetes, coronary artery disease, and stroke. We conducted variable selection with Elastic Net (which accounts for collinearity between model variables) and used race/ethnicity, medical center, college education, body mass index, smoking status, coronary artery disease, and medical center as covariates in the fully adjusted model.21 All analyses were conducted with SAS Enterprise Guide (version 7.1; SAS Institute, Inc., Cary, NC). All tests of statistical significance were 2 sided with α=.05. This study was approved by the Kaiser Permanente Southern California institutional review board.
RESULTS
Characteristics of Study Subjects
A total of 34,715 adult ED encounters with a documented HEART score were included in the analysis, including 19,407 women (56%) (Figure 1). The median age of the population was 61 years (Table 1). At baseline, a higher proportion of men had a history of smoking and coronary artery disease. Women were slightly older and had higher rates of family history of coronary artery disease and stroke. Compared with men, women were more likely to be categorized as low risk (HEART score 0 to 3; 60.5% versus 52.4%; OR 1.39; 95% CI 1.33 to 1.45) and less likely to be categorized as high risk (HEART score 7 to 10; 2.8% versus 4.9%; OR 0.55; 95% CI 0.49 to 0.62).
Table 1.
Patient demographics.
| Women, |
Men, |
|
|---|---|---|
| N=19,407 | N=15,308 | |
| HEART score | ||
| Median | 3.0 | 3.0 |
| Q1, Q3 | 2.0, 4.0 | 2.0, 5.0 |
| HEART score, No. (%) | ||
| Low (0–3) | 11,736 (60.5) | 802 8,021 (52.4) |
| Intermediate (4–6) | 7,134 (36.8) | 6,537 (42.7) |
| High (7–10) | 537 (2.8) | 750 (4.9) |
| Age, y | ||
| Median | 61.0 | 60.5 |
| Q1, Q3 | 50.7, 72.0 | 49.0, 71.0 |
| Education, college or higher (%) | ||
| Median | 56.7 | 58.3 |
| Q1, Q3 | 42.0, 71.4 | 43.5, 73.0 |
| Household median income, $ | ||
| Median | 63,200 | 65,500 |
| Q1, Q3 | 46,300, 84,200 | 47,900, 87,500 |
| Race, No. (%) | ||
| Alaska Native/Pacific Islander | 230 (1.2) | 216 (1.4) |
| Asian | 1,753 (9) | 1,332 (8.7) |
| Black | 3,535 (18.2) | 2,049 (13.4) |
| Hispanic | 7,094 (36.6) | 5,306 (34.7) |
| Other | 260 (1.3) | 280 (1.8) |
| White | 6,535 (33.7) | 6,125 (40) |
| BMI, No. (%), kg/m2 | 30.2 (7.53) | 30.2 (6.52) |
| Underweight, <18.5 | 348 (1.8) | 101 (0.7) |
| Normal, 18.5–24.9 | 4,520 (23.3) | 2,830 (18.5) |
| Overweight, 25–29.9 | 5,864 (30.2) | 5,481 (35.8) |
| Obese, ≥30 | 8,495 (43.8) | 6,627 (43.3) |
| Missing | 180 (0.9) | 269 (1.8) |
| Smoking, No. (%) | ||
| Never or passive | 13,289 (68.5) | 7,314 (47.8) |
| Quit | 4,807 (24.8) | 6,117 (40) |
| Active | 989 (5.1) | 1,363 (8.9) |
| Missing | 322 (1.7) | 514 (3.4) |
| Comorbidities (in year before), No. (%) | ||
| CAD | 2,844 (14.7) | 4,139 (27) |
| Diabetes | 5,777 (29.8) | 5,180 (33.8) |
| Hypertension | 11,303 (58.2) | 9,298 (60.7) |
| Lipid disorder | 11,885 (61.2) | 10,349 (67.6) |
| Stroke | 670 (3.5) | 586 (3.8) |
| CABG | 44 (0.2) | 121 (0.8) |
| PTCA | 141 (0.7) | 178 (1.2) |
| Family history of CAD | 7,099 (36.6) | 5,161 (33.7) |
| Family history of stroke | 3,997 (20.6) | 2,570 (16.8) |
BMI, Body mass index; CAD, coronary artery disease; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty.
Main Results
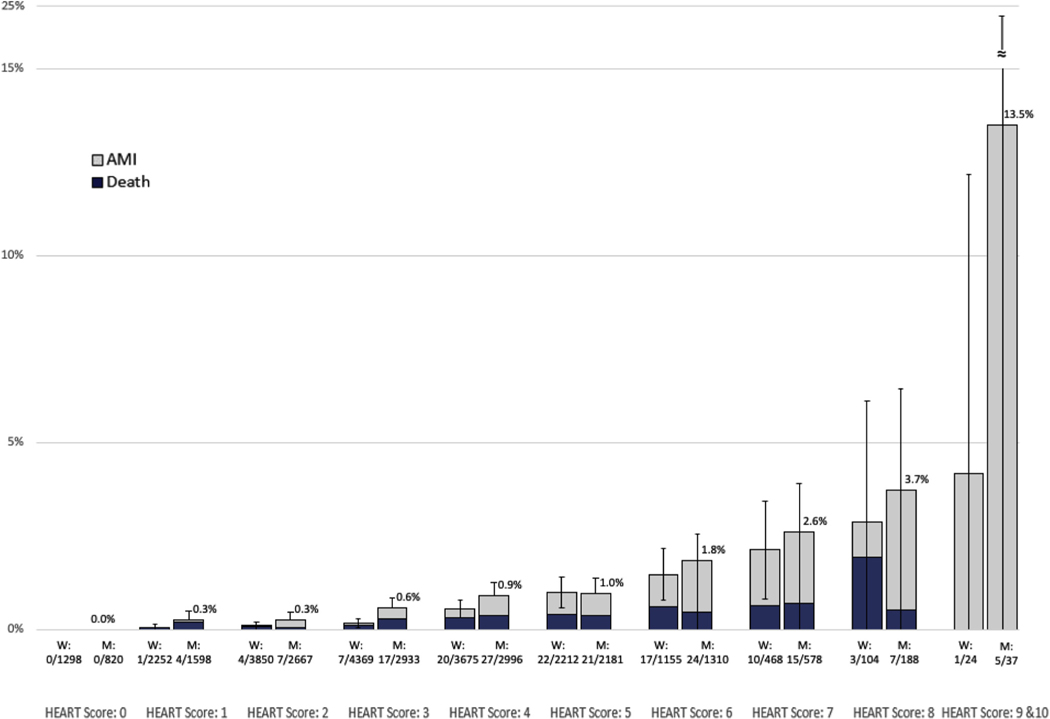
There were differences in 30-day stress testing and hospitalization between men and women. Clinicians referred more men for stress testing compared with women (23.6% versus 21.1%; OR 0.93; 95% CI 0.88 to 0.98). Women were discharged more often than men (84.4% versus 78.3%; OR 1.30; 95% CI 1.23 to 1.38). For men, there were 4,506 stress tests ordered and 3,776 completed (83.8%); women had 5,336 tests ordered and 4,338 completed (81.3%). The overall adjusted odds of hospitalization or 30-day stress testing were significantly lower for women compared with men (OR 0.82; 95% CI 0.78 to 0.86) (Table 2). Major adverse cardiac event outcomes stratified by HEART score for men and women showed that men had slightly higher rates of events than women (Figure 2). The outcomes by risk category for men and women varied, and regression analyses showed that women were less likely than men to be hospitalized or stress tested for low-risk categories (OR 0.77; 95% CI 0.71 to 0.82) and intermediate-risk ones (OR 0.86; 95%CI 0.80 to 0.92), but not high-risk ones (OR 0.96; 95% CI 0.74 to 1.23).
Table 2.
Discharge disposition and stress testing by sex.
| Women, No. (%), |
Men, No. (%), |
OR (95% CI), |
|
|---|---|---|---|
| N=19,407 | N=15,308 | N=34,715 | |
| ED discharge disposition | |||
| Inpatient admission* | 566 (2.9) | 656 (4.3) | 0.77 (0.68–0.86) |
| Low (0–3) | 174 (1.5) | 150 (1.9) | 0.79 (0.63–0.98) |
| Intermediate (4–6) | 327 (4.6) | 388 (5.9) | 0.76 (0.65–0.89) |
| High (7–10) | 65 (12.1) | 118 (15.7) | 0.74 (0.54–1.03) |
| Observation* | 2,210 (11.4) | 2,337 (15.3) | 0.84 (0.78–0.89) |
| Low (0–3) | 438 (3.7) | 379 (4.7) | 0.78 (0.68–0.90) |
| Intermediate (4–6) | 1,483 (20.8) | 1,567 (24) | 0.83 (0.76–0.90) |
| High (7–10) | 289 (53.8) | 391 (52.1) | 1.07 (0.86–1.33) |
| Operating room | 11 (0.1) | 19 (0.1) | 0.46 (0.22–0.96) |
| Home* | 16,370 (84.4) | 11,984 (78.3) | 1.30 (1.23–1.38) |
| Low (0–3) | 11,000 (93.7) | 7,392 (92.2) | 1.27 (1.14–1.42) |
| Intermediate (4–6) | 5,196 (72.8) | 4,386 (67.1) | 1.32 (1.23–1.42) |
| High (7–10) | 174 (32.4) | 206 (27.5) | 1.26 (0.99–1.60) |
| Other | 250 (1.3) | 312 (2) | 0.63 (0.53–0.74) |
| 30-day stress test* | 4,092 (21.1) | 3,608 (23.6) | 0.93 (0.88–0.98) |
| Low (0–3) | 1,693 (14.4) | 1,388 (17.3) | 0.81 (0.75–0.87) |
| Intermediate (4–6) | 2,213 (31) | 2,012 (30.8) | 1.01 (0.94–1.09) |
| High (7–10) | 186 (34.6) | 208 (27.7) | 1.38 (1.09–1.75) |
| Hospitalization or 30-day stress test* | 5,936 (30.6) | 5,635 (36.8) | 0.84 (0.80–0.88) |
| Low (0–3) | 2,205 (18.8) | 1,828 (22.8) | 0.79 (0.73–0.84) |
| Intermediate (4–6) | 3,333 (46.7) | 3,249 (49.7) | 0.88 (0.83–0.95) |
| High (7–10) | 398 (74.1) | 558 (74.4) | 0.99 (0.77–1.28) |
| Hospitalization or 30-day stress test† (fully adjusted) | 0.82 (0.78–0.86) | ||
| Low (0–3) | 0.77 (0.71–0.82) | ||
| Intermediate (4–6) | 0.86 (0.80–0.92) | ||
| High (7–10) | 0.96 (0.74–1.23) |
Adjusting for HEART category (low 0 to 3, intermediate 4 to 6, and high 7 to 10).
Adjusting for race/ethnicity (Alaska Native, Pacific Islander, Asian, black, Hispanic, other, and white), college education (continuous percentage by zip code), body mass index (<18, 18 to 25, 25 to 30, and >30 kg/m2, and missing), smoking status (never or passive, quit, active, and missing), coronary artery disease, and medical center.
Figure 2.
Percentage of 30-day mortality or acute myocardial infarction risk by sex. The x axis is the documented HEART score 1 to 10 for men and women. The y axis is the percentage of acute myocardial infarction and death. The proportions listed under each bar represent the number of acute myocardial infarctions for men and women and each indicated HEART score. For better interpretation of the graph, HEART scores 9 and 10 were combined and the percentage bar for men was minimized at 5%, with the actual percentage listed above.
Difference in acute myocardial infarction and all cause-mortality showed that women had a significantly lower risk of major adverse cardiac events than men for the low-risk HEART score group (OR 0.31; 95% CI 0.15 to 0.61), but not for intermediate-risk (OR 0.82; 95% CI 0.56 to 1.19) or high-risk HEART scores (OR 0.76; 95% CI 0.38 to 1.52). Women who were hospitalized or stress tested had significantly lower odds of having major adverse cardiac events compared with men (OR 0.63; 95% CI 0.43 to 0.94), and this was especially true among patients with a low-risk HEART score (OR 0.10; 95% CI 0.01 to 0.83) (Table 3).
Table 3.
Outcomes of HEART score risk categories, stratified by sex.
| Women, No. (%) | Men, No. (%) | OR (95% CI) | |
|---|---|---|---|
| Low risk (HEART score 0–3) | |||
| Hospitalized or stress tested | N=2,221 | N=1,835 | |
| MACE | 1 (0.05) | 8 (0.44) | 0.10 (0.01–0.83) |
| AMI | 0 | 6 (0.33) | NA |
| Death | 1 (0.05) | 2 (0.11) | 0.41 (0.04–4.57) |
| Hospitalized | N=615 | N=535 | |
| MACE | 1 (0.16) | 4 (0.74) | 0.22 (0.02–1.93) |
| AMI | 0 | 2 (0.37) | NA |
| Death | 1 (0.16) | 2 (0.37) | 0.43 (0.04–4.78) |
| Stress tested | N=1,717 | N=1,399 | |
| MACE | 0 | 5 (0.36) | NA |
| AMI | 0 | 5 (0.36) | NA |
| Death | 0 | 0 | NA |
| All HEART scores (0–10) | |||
| Hospitalized or stress tested | N=5,936 | N=5,635 | |
| MACE | 43 (0.72) | 63 (1.12) | 0.63 (0.43–0.94) |
| AMI | 23 (0.39) | 45 (0.80) | 0.47 (0.28–0.78) |
| Death | 21 (0.35) | 20 (0.35) | 1.00 (0.54–1.84) |
| Hospitalized | N=2,787 | N=3,012 | |
| MACE | 41 (1.47) | 55 (1.83) | 0.80 (0.53–1.20) |
| AMI | 22 (0.79) | 37 (1.23) | 0.63 (0.36–1.08) |
| Death | 20 (0.72) | 19 (0.63) | 1.14 (0.61–2.14) |
| Stress tested | N=4,092 | N =3,608 | |
| MACE | 8 (0.20) | 22 (0.61) | 0.32 (0.14–0.72) |
| AMI | 6 (0.15) | 20 (0.55) | 0.26 (0.11–0.66) |
| Death | 2 (0.05) | 3 (0.08) | 0.59 (0.10–3.52) |
MACE, Major adverse cardiac event; AMI, acute myocardial infarction.
LIMITATIONS
This study was performed in an integrated health system that may offer better coordinated care in comparison with other health care models in the United States. Additionally, the study population had low rates of major adverse cardiac events overall, and outcomes may not be similar in other populations that have higher rates of them, which may include tertiary or quaternary care centers. Our study was conducted in community hospital EDs and other levels of care may yield different results. We investigated all patients with suspected acute coronary syndrome, which led to low mortality rates, whereas examining those with confirmed acute coronary syndrome may yield different results. The HEART score has a few limitations in that it does not account for autoimmune diseases or history of adverse pregnancy outcomes, which can lead to greater cardiac risk among women. It is possible that physicians attribute the risk of the patient history differently for men and women; this bias cannot be measured in accordance with our data and study results. It is also possible that physicians document HEART scores differently between men or women, which was not specifically accounted for in our study. Among ED encounters with troponin testing ordered, 57% had a documented HEART score. There are exceptions to HEART score risks, and clinical judgment should always be added to clinical pathways to provide safe patient-centered care. Last, the study included patients with a documented HEART score, and this could have missed those in whom acute coronary syndrome was suspected but for whom a HEART score was not documented by the physician. Also, this can miss patients with atypical symptoms for whom there was a misdiagnosis by the physician.
DISCUSSION
Our study found that women with low-risk HEART scores received guideline-concordant care more often than men by avoiding hospitalization or noninvasive cardiac testing and having better 30-day outcomes than low-risk men. Women had similar hospitalization or testing and outcomes comparable to those of men in the high-risk group. These results indicate that use of HEART score and standardized care pathways may be associated with more appropriate care for women, whereas overtesting may be more common in men.
Our results are consistent with those of other studies that reported more hospitalizations or stress testing for men than women.7,8,22 However, we found this to be most pronounced for patients at low risk according to HEART score, the largest group with suspected acute coronary syndrome. Our findings that women had fewer hospitalizations or less noninvasive testing may be consistent with recent reports suggesting such care is not of benefit for many ED patients with suspected acute coronary syndrome.23–25 Unlike previous studies describing higher rates of misdiagnosis or adverse events among women, we did not find this to be true among those at low risk.26,27 This finding raises the question of whether all low-risk patients would be better off with less noninvasive testing. We found that men in the low-risk score category were more likely to undergo testing or be admitted for hospitalization, but still had higher adverse events at 30 days. This may indicate that testing or admission in low-risk men did not have a beneficial influence on 30-day major adverse cardiac events. Early discharge of low-risk patients appears to be safe for both men and women. These results indicate far more perceived than actual risk for men with suspected acute coronary syndrome. In contrast, low-risk women were less likely to undergo unnecessary tests. Disparities in management of men and women may have unintended benefits to women by avoiding low-value or unnecessary care.
Some have suggested that sex-based differences in the management of suspected acute coronary syndrome are appropriate for the probability of disease for each sex.8 Although it is true men have a higher baseline risk for acute coronary syndrome, results demonstrated that among low- and intermediate-risk men, there was a 0.2% to 0.3% higher major adverse cardiac event rate. This does not account for the 14% lower likelihood for hospitalization and cardiac testing for women. The slightly higher risk in men at baseline should be considered when the HEART score is used, but in a way that recognizes sex-adjusted risk prediction.28 The American Heart Association has evidence-based guidelines for women, but they are not routinely incorporated into practice.29 Future research should determine whether sex-specific elements should be added into prediction tools such as HEART. For example, sex-specific thresholds for diagnostic tests, such as the new high-sensitivity troponin assays, may help improve sex-specific diagnostic performance.30,31
Within the high-risk group, women and men were admitted or observed at similar rates. Women in low- and moderate-risk groups receive less testing, which may be optimal because major adverse cardiac event outcomes remain similar to those of men and relatively low. Furthermore, the HEART score performed overall well in men and women, with only small differences (one tenth of a percent) in the lower-risk groups, which may have questionable clinical relevance. Men appear to have much higher risk than women in the higher-risk subgroups, which may warrant the differences in observation and inpatient status that was observed.
Outcomes for acute coronary syndrome in women have improved and mortality rates are now similar to those of men.32,33 We find that women presenting to the ED with suspected acute coronary syndrome are less likely to be hospitalized or tested, yet they still outperform men and experience less acute myocardial infarction and mortality. Standard risk assessment is one tool that can be used to measure performance and mitigate sex disparities among men and women with similar risk. Clinicians and guidelines should consider these results to implement practice changes to improve health outcomes by testing only patients most likely to benefit and avoiding low-value, potentially harmful care for those at low risk.
In conclusion, women at low risk were hospitalized less or received less testing than men, which is consistent with current clinical recommendations and results in better outcomes than those of men in this group. Men and women at high risk for acute coronary syndrome received similar testing and had comparable outcomes. Sex disparities of the intermediate-risk group were limited. Risk stratification (by HEART score) of ED patients with suspected acute coronary syndrome may be a useful tool to improve the care of women and minimize sex disparities. Future interventions to address overtesting and hospitalization among men at low risk are warranted.
Editor’s Capsule Summary.
What is already known on this topic
Women are evaluated differently from men when presenting to emergency departments (EDs) with suspected acute coronary syndrome.
What question this study addressed
The authors measured hospitalizations or 30-day stress testing among women and men evaluated for suspected acute coronary syndrome after History, ECG, Age, Risk Factors, and Troponin pathway implementation in 15 community EDs.
What this study adds to our knowledge
Adjusting for History, ECG, Age, Risk Factors, and Troponin scores and comorbidities, low-risk women had fewer hospitalizations, stress tests, and 30-day major adverse cardiac events. Low-risk men may be receiving unnecessary medical evaluations.
How this is relevant to clinical practice
Patients with suspected acute coronary syndrome should receive a diagnosis and be treated according to their acute coronary syndrome risk irrespective of sex. This article supports that most low-risk patients do not benefit from hospitalization or stress testing.
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). Dr. Sun was a consultant for Medtronic. Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) under award R01HL134647. Dr. Ferencik was supported by the American Heart Association Fellow-to-Faculty Award (13FTF16450001).
The authors acknowledge the patients of Kaiser Permanente for helping to improve care with information collected through the electronic health record systems, and acknowledge the time and dedication of the project management team, Visanee (“Vicky”) Musigdilok and Rani Pallegadda.
Footnotes
Supervising editor: Tyler W. Barrett, MD, MSCI. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Trial registration number: XXXXXXXX
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Salena M. Preciado, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Adam L. Sharp, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Benjamin C. Sun, Department of Emergency Medicine, University of Pennsylvania, Leonard Davis Institute, Philadelphia, PA.
Aileen Baecker, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Yi-Lin Wu, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Ming-Sum Lee, Division of Cardiology, Kaiser Permanente Southern California, Los Angeles Medical Center, Los Angeles, CA.
Ernest Shen, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Maros Ferencik, Knight Cardiovascular Institute, Oregon Health & Science University, Portland, OR.
Shaw Natsui, New York City Health + Hospitals, New York, NY.
Aniket A. Kawatkar, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Stacy J. Park, Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA.
Rita F. Redberg, Division of Cardiology, University of California–San Francisco, San Francisco, CA.
REFERENCES
- 1.Vedanthan R, Seligman B, Fuster V. Global perspective on acute coronary syndrome: a burden on the young and poor. Circ Res. 2014;114:1959–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. National Hospital Ambulatory Medical Care Survey: 2010 emergency department summary tables. The Ambulatory and Hospital Care Statistics Branch. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf. Published 2010. Accessed. [Google Scholar]
- 3.Sörensen NA, Neumann JT, Ojeda F, et al. Relations of sex to diagnosis and outcomes in acute coronary syndrome 2018;7:e007297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Humphries KH, Izadnegahdar M, Sedlak T, et al. Sex differences in cardiovascular disease: impact on care and outcomes. Front Neuroendocrinol. 2017;46:46–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Humphries KH, Lee MK, Izadnegahdar M, et al. Sex differences in diagnoses, treatment, and outcomes for emergency department patients with chest pain and elevated cardiac troponin. Acad Emerg Med. 2018;25:413–424. [DOI] [PubMed] [Google Scholar]
- 6.Stähli BE, Gebhard C, Yonekawa K, et al. Gender-related differences in patients presenting with suspected acute coronary syndromes: clinical presentation, biomarkers and diagnosis. Cardiology. 2015;132:189–198. [DOI] [PubMed] [Google Scholar]
- 7.Ruane L, J HG, Parsonage W, et al. Differences in presentation, management and outcomes in women and men presenting to an emergency department with possible cardiac chest pain. Heart Lung Circ. 2017;26:1282–1290. [DOI] [PubMed] [Google Scholar]
- 8.Hess EP, Perry JJ, Calder LA, et al. Sex differences in clinical presentation, management and outcome in emergency department patients with chest pain. CJEM. 2010;12:405–413. [DOI] [PubMed] [Google Scholar]
- 9.Wiviott SD, Cannon CP, Morrow DA, et al. Differential expression of cardiac biomarkers by gender in patients with unstable angina/non-ST-elevation myocardial infarction: a TACTICS-TIMI 18 (Treat Angina With Aggrastat and Determine Cost of Therapy With an Invasive or Conservative Strategy–Thrombolysis in Myocardial Infarction 18) substudy. Circulation. 2004;109:580–586. [DOI] [PubMed] [Google Scholar]
- 10.Rosenfeld AG, Knight EP, Steffen A, et al. Symptom clusters in patients presenting to the emergency department with possible acute coronary syndrome differ by sex, age, and discharge diagnosis. Heart Lung. 2015;44:368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah AS, Griffiths M, Lee KK, et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ. 2015;350:g7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Humphries KH, Gao M, Lee MK, et al. Sex differences in cardiac troponin testing in patients presenting to the emergency department with chest pain. J Womens Health (Larchmt). 2018;27:1327–1334. [DOI] [PubMed] [Google Scholar]
- 13.Araújo C, Laszczynska O, Viana M, et al. Sex differences in presenting symptoms of acute coronary syndrome: the EPIHeart cohort study. BMJ Open. 2018;8:e018798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Appelman Y, van Rijn BB, Ten Haaf ME, et al. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis. 2015;241:211–218. [DOI] [PubMed] [Google Scholar]
- 15.Fanaroff AC, Rymer JA, Goldstein SA, et al. Does this patient with chest pain have acute coronary syndrome? the Rational Clinical Examination systematic review. JAMA. 2015;314:1955–1965. [DOI] [PubMed] [Google Scholar]
- 16.Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168:2153–2158. [DOI] [PubMed] [Google Scholar]
- 17.Bank IEM, de Hoog VC, de Kleijn DPV, et al. Sex-based differences in the performance of the HEART score in patients presenting to the emergency department with acute chest pain. J Am Heart Assoc. 2017;6:e005373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharp AL, Baecker AS, Shen E, et al. Effect of a HEART care pathway on chest pain management within an integrated health system. Ann Emerg Med. 2019;74:171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharp AL, Wu Y-L, Shen E, et al. The HEART score for suspected acute coronary syndrome in US emergency departments. J Am Coll Cardiol. 2018;72:1875–1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharp AL, Broder B, Sun BC. Improving emergency department care for low-risk chest pain. NEJM Catal. 2018;2018. [Google Scholar]
- 21.Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc Series B Stat Methodol. 2005;67:301–320. [Google Scholar]
- 22.Graham G Acute coronary syndromes in women: recent treatment trends and outcomes. Clin Med Insights Cardiol. 2016;10:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandhu AT, Heidenreich PA, Bhattacharya J, et al. Cardiovascular testing and clinical outcomes in emergency department patients with chest pain. JAMA Intern Med. 2017;177:1175–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foy AJ, Liu G, Davidson WR Jr, et al. Comparative effectiveness of diagnostic testing strategies in emergency department patients with chest pain: an analysis of downstream testing, interventions, and outcomes. JAMA Intern Med. 2015;175:428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinstock MB, Weingart S, Orth F, et al. Risk for clinically relevant adverse cardiac events in patients with chest pain at hospital admission. JAMA Intern Med. 2015;175:1207–1212. [DOI] [PubMed] [Google Scholar]
- 26.Wilkinson C, Bebb O, Dondo TB, et al. Sex differences in quality indicator attainment for myocardial infarction: a nationwide cohort study. Heart. 2019;105:516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davidson PM, Mitchell JA, DiGiacomo M, et al. Cardiovascular disease in women: implications for improving health outcomes. Collegian. 2012;19:5–13. [DOI] [PubMed] [Google Scholar]
- 28.McGregor AJ, Beauchamp GA, Wira CR 3rd, et al. Sex as a biological variable in emergency medicine research and clinical practice: a brief narrative review. West J Emerg Med. 2017;18:1079–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells M, Kalman M. Women and heart disease: symptoms and treatment guidelines. Nurse Pract. 2011;36:22–27. [DOI] [PubMed] [Google Scholar]
- 30.Ljung L, Lindahl B, Eggers KM, et al. A rule-out strategy based on high-sensitivity troponin and HEART score reduces hospital admissions. Ann Emerg Med. 2019;73:491–499. [DOI] [PubMed] [Google Scholar]
- 31.Januzzi JL Jr, Mahler SA, Christenson RH, et al. Recommendations for institutions transitioning to high-sensitivity troponin testing: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;73:1059–1077. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Underlying Cause of Death, 1999–2017. National Center for Health Statistics. [PubMed] [Google Scholar]
- 33.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics 2019 update: a report from the. American Heart Association. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]