Abstract
Objectives:
To determine the factors that shape utilization of social media based online support communities (OSC) and study the influence of these communities on medical decision making in patients with Idiopathic Subglottic Stenosis (iSGS).
Methods:
A survey investigating OSC use was sent to the 1056 members of the North American Airway Collaborative (NoAAC) iSGS1000 cohort in January 2018. Responses were merged with the existing NoAAC dataset containing extensive demographic data, disease specific history, and responses to validated patient reported outcome measures.
Results:
A total of 755 individuals with iSGS and mean age of 51.8±11.6 years were included (99% female, 98% white, 63% college educated) and 58% were OSC users. Younger age, female gender, and college education were each associated with OSC use (p<0.05). Users spent 2.5±3.3 hours per week on the platforms. Time spent on OSC was not associated with total number of prior treatments. Higher disease anxiety (FoP-Q, R=0.26, p<0.001), lower social support (MOS, R=−0.12, p=0.037) and lower level of shared-decision-making with the treating physician (SDM-Q9, R=−0.16, p=0.007) were weakly associated with more hours spent engaging an OSC. OSC use influenced treatment and physician choice in 35% and 26% of users, respectively. Increased time spent on OSC use was associated with increased influence on patient medical decisions regarding treatment, surgery, and physician choice (p<0.05).
Conclusion:
OSC engagement is common in patients with iSGS. Disease anxiety, social support, and relationship with the physician may influence OSC utilization. More OSC engagement weakly associated with greater OSC influence on patient medical decision-making.
Keywords: Online support group, online support communities, idiopathic subglottic stenosis, patient empowerment, medical decision-making, internet, Facebook
Introduction
The internet is a powerful tool that allows geographically separated persons the ability to learn, share information and connect with one another. Serving many roles, the internet is an influential source of health information for patients. In 2010 over 80% of internet users searched online for health related information1; that number has undoubtedly risen over the last ten years, especially during the current COVID-19 era which has potentially pushed most people further into the digital world. Not only are patients able to access professional resources, they are able to engage with content directed at consumers and communicate with individuals facing similar medical challenges. Medical online support communities (OSCs), established primarily through social media platforms such as Facebook and Twitter, have evolved into a significant healthcare resource.2,3 The commonality of social media allows people with similar medical conditions to easily find one another and share their experiences. These OSCs, present for only the last fifteen years, have dramatically changed the ways in which individuals interact, and potentially how they manage their disease.
Previous work suggested that OSCs might primarily generate value through sharing of emotional experiences rather than medical information.4 Content analysis has been undertaken to better understand what experiences individuals are sharing,5,6 but large gaps in knowledge still remain. The only two reports investigating OSCs influence on medical decision-making are in the fields of breast and prostate cancer.7,8 While the internet is unquestionably a powerful source of health information, the emerging social aspects of digital technology have dramatically lowered the barriers to exchange information, solidarity, and support between patients. In the process, they offer new insights on how patients experience their disease and care to non-patients. Yet the impact of OSCs on the disease experience and medical decision-making process has yet to be evaluated.9
Idiopathic subglottic stenosis (iSGS) is a rare inflammatory airway disease of unknown cause and without a defined cure.10 Despite disease rarity, active OSCs connecting thousands of individuals with this condition have emerged over the last 10 years. In a previous observational study by our group, the posts of a large Facebook group dedicated to iSGS were thematically analyzed to gain insight into the type of information exchanged.11 The current study furthers this inquiry to more fully understand how that information influences medical decision making by coupling data from the prospectively collected NoAAC iSGS1000 cohort with patient information pertaining to OSC utilization. The aim of this study is to assess iSGS patient motivation for OSC membership, patient factors impacting the frequency of OSCs use, and the influence of OSC engagement on medical decision making.
Methods
This study was approved by Vanderbilt University (#150917) and University of California Irvine (#2016–3209) Institutional Review Boards. Online surveys were distributed to patients actively enrolled in the North American Airway collaborative (NoAAC) Idiopathic subglottic stenosis patient group (iSGS1000) sponsored by the Patient-Centered Outcomes Research Institute. The survey was supported by secure and information-protected REDCap website (Nashville, Tennessee) and administrated to patients via email. Multiple reminders were sent, and the survey was online for 45 days in January-February 2018. The comprehensive survey, comprised of both standardized and original questionnaires, was designed by three fellowship-trained laryngologists (SV, AG, DF) and was implemented with with extensive input from a patient advocate (administrator of the Living with iSGS Facebook group). The survey queried patient demographics, clinical characteristics, treatment history and decision-making process, and level or type of OSC engagement. Moreover, three standardized questionnaires were administered: 9-Item Shared Decision-Making Questionnaire (SDM-Q9), Medical Outcomes Study Social Support Survey (MOS), and fear of progression in chronic disease questionnaire (FoP). The FoP had two components: 1) FoP-affective which evaluated disease-specific anxiety levels, and 2) FoP-coping which evaluated level of coping with disease anxiety.
The collected surveys were de-identified prior to analysis and summarized using parametric and non-parametric approaches. Important outcome variables included frequency of OSC use (measured in hours and days), assessments of the motivation for OSC engagement, the quality of information provided, and influence on medical decision making. Statistical analyses were performed using STATA12 (StataCorp., College Station, TX) and PASW Statistics 18.0 software (SPSS Inc., Chicago, IL), and a p-value of <0.05 was considered significant. The coefficient of correlation, designated as “R”, was considered strongly correlated when >0.6, fairly correlated when 0.3–0.5, and weakly correlated when <0.3.12 The same parameters were used for negative R values.
Results
OSC use in the NoAAC iSGS1000 cohort
Of the 1065 individuals enrolled in the NoAAC iSGS1000 reached through survey invitation, 755 (70.9%) completed questionnaires. With a mean age of 51.8 ± 11.6 (range 21–82 years), the cohort was 98.6% female, 97.6% white, and 62.6% college educated. The social media platforms used for any reason included Facebook (n=660, 87.4%), LinkedIn (n=233; 30.9%), Instagram (n=149; 19.7%), Twitter (n=148; 19.6%), Snapchat (n=27; 3.6%), and Pinterest (n=16; 2.1%) (Figure 1A). In total, 441 (58.4%) of participants engaged in an iSGS-related OSC, almost all through Facebook (438, 99.3%), while 314 (41.6%) did not access an OSC (Figure 1B). In the cohort using OSC, participants spent an average of 2.5 ±3.3 hours per week (range 0–30 hours) on iSGS online groups. The frequency of visits to the main OSC were: more than once a day (N=73, 16.6%), once a day (N=113, 25.6%), multiple times a week (N=88, 20.0%), multiple times a month (N=104, 23.6%), and once a month or less (N=61, 13.8%)(Figure 1C).
Figure 1.
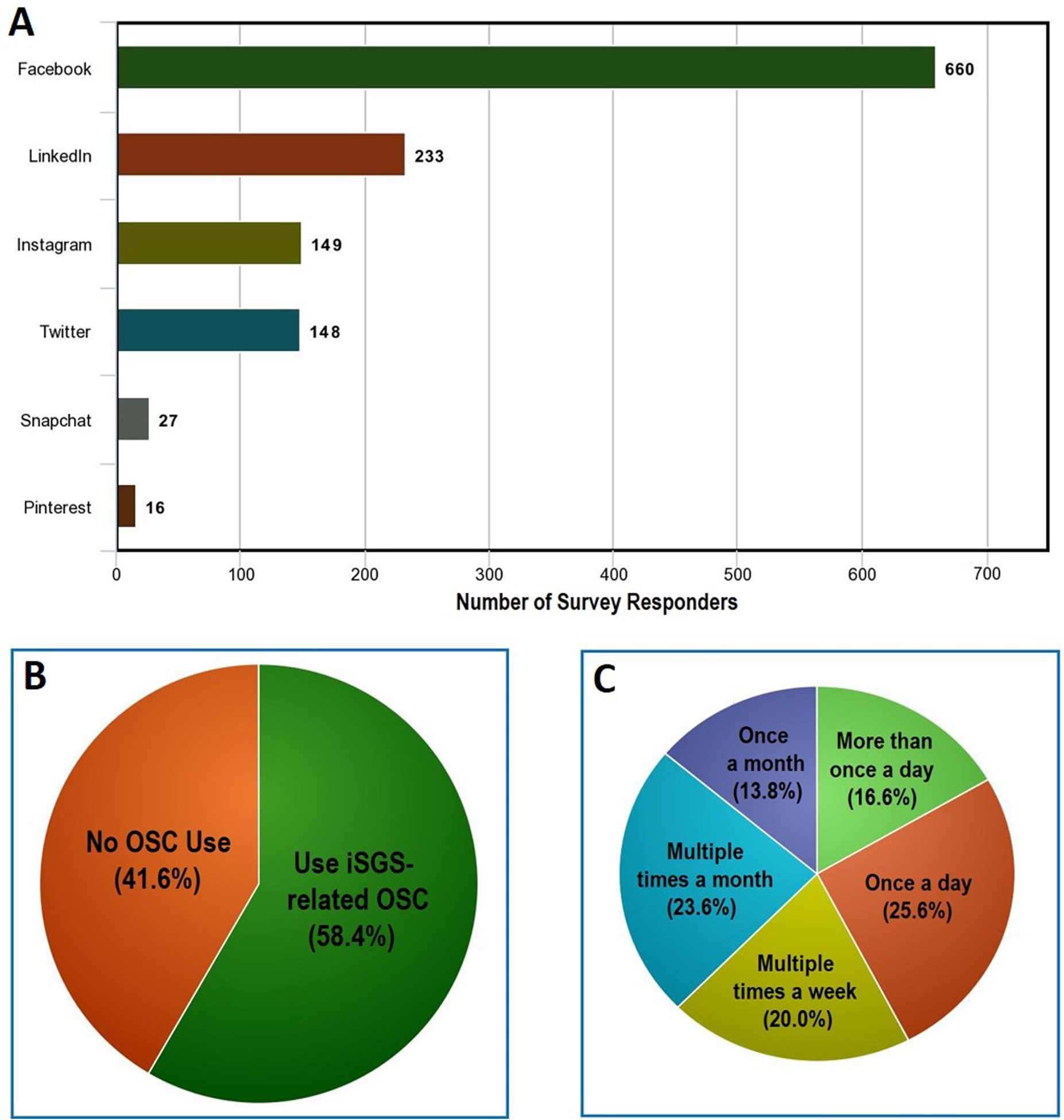
Online presence and iSGS-related OSC engagement of the study participants. (A) The social media platforms used for any reason, (B) breakdown of people using or not using iSGS-related OSC, and (C) Frequency of OSC engagement among people who use these platforms.
Patient Perception of an Online Support Community
More than 90% of respondents reported that they joined the OSC to hear from others with the same condition, and more than 85% specifically joined to learn about treatments (Table 1). We also investigated patients’ perception of the value of information and support provided by their OSC platforms. The majority of participants trusted the information provided, felt their privacy was protected in a safe sharing environment, and would recommend other iSGS participants join an OSC (Table 2). In order of preference, participants’ preferred form of support group for iSGS included an OSC (N=143, 32.5%), face-to-face physical group in their area (N=35, 8.0%), both (N=255, 58.0%), and neither (N=7, 1.6%).
Table 1.
Questions regarding reason for joining and potential benefits from OSC involvement.
| Thinking back to when you joined your main social media support group for idiopathic subglottic stenosis, what were your original reasons for joining? | |
| To hear from others with the same condition as me | 403 (91.4%) |
| To learn tips and hints in how to deal with iSGS | 385 (87.3%) |
| To learn about treatments including surgeries for iSGS | 380 (86.2%) |
| To gain support from people who understand what I am going through | 308 (69.8%) |
| To access papers and research about iSGS | 260 (59.0%) |
| To provide support for others going through the same as me | 252 (57.1%) |
| To learn about physicians treating iSGS | 246 (55.8%) |
| To share my experiences with other people going through the same as me | 231 (52.4%) |
| To meet other people in my area with iSGS | 174 (39.5%) |
| And what do you feel you have actually achieved from joining the social media support group for idiopathic subglottic stenosis? | |
| Heard from others experiencing the same as me | 386 (87.5%) |
| Learned about surgeries and treatments for iSGS | 377 (85.5%) |
| Learned tips and hints in how to deal with iSGS | 350 (79.4%) |
| Shared my experiences with other people going through the same as me | 321 (72.8%) |
| Supported others going through the same as me | 318 (72.1%) |
| Learned about the best doctors for treating iSGS | 309 (70.1%) |
| Gained support from people who understand what I am going through | 306 (69.4%) |
| Accessed papers and research about iSGS | 301 (68.3%) |
| Asked for advice | 255 (57.8%) |
| Met (face to face) other people in my area with iSGS | 106 (24.0%) |
| How would you describe your level of participation in your main social media support group for iSGS? | |
| I mostly read what others post | 245 (55.6%) |
| I read and comment on what others post | 111 (25.2%) |
| I read and comment on other’s posts and ask questions of others equally | 73 (16.6) |
| I mostly ask questions of others | 3 (0.7%) |
| Which of these do you consider to be most important in a support group? | |
| Learned about surgeries and treatments for iSGS | 320 (72.6%) |
| Heard from others experiencing the same as me | 311 (70.5%) |
| Learned tips and hints in how to deal with iSGS | 309 (70.1%) |
| Gained support from people who understand what I am going through | 253 (57.4%) |
| Supported others going through the same as me | 229 (51.9%) |
| Learned about the best doctors for treating iSGS | 225 (51.0%) |
| Accessed papers and research about iSGS | 215 (48.8%) |
| Shared my experiences with other people going through the same as me | 182 (41.3%) |
| Asked for advice | 181 (41.0%) |
| Meeting (face to face) other people in my area with iSGS | 66 (15.0%) |
Table 2.
Participants’ perception of OSC platform.
| Questions | Definitely Not | Probably Not | Possibly | Probably | Very Probably | Definitely |
|---|---|---|---|---|---|---|
| I feel my privacy is protected | 7 (1.6%) | 32 (7.3%) | 59 (13.4%) | 90 (20.4%) | 129 (29.3%) | 123 (27.9%) |
| I can trust the information provided within the group | 5 (1.1%) | 23 (5.2%) | 41 (9.3%) | 64 (14.5%) | 121 (27.4%) | 185 (42.0%) |
| It provides a safe place where I can share my experiences without my friends/family reading everything | 5 (1.1%) | 23 (5.2%) | 41 (9.3%) | 64 (14.5%) | 121 (27.5%) | 186 (42.3%) |
| Based on your experiences, would you recommend that other people with iSGS join your main OSC? | 3 (0.7%) | 13 (3.0%) | 73 (16.7%) | 118 (26.9%) | 132 (30.1%) | 99 (22.6%) |
Factors influencing OSC Utilization
Patients who belonged to an OSCs were younger (49.4 ± 10.6 vs. 55.2 ± 12.1, p<0.001), college-educated (71.0% vs. 62.2%, p=0.014) and female (99.5% vs. 97.3%, p=0.037) when compared to non-members. Reasons cited for not joining an OSC were a lack of awareness of their existence (N=193, 61.5%), concern about privacy of medical information (N=63, 20.1%), reticence to use social media for support (N=37, 11.8%), and discomfort with using social media in general (N=32, 10.2%).
Among OSC users, we investigated patient factors impacting the frequency of OSCs use. Traditional social support (measured via the patient-reported MOS score) was weakly correlated with less hours spent on the OSC per week (R=−0.122, p=0.037). Interestingly, higher disease anxiety (measured via FoP scores) was also weakly correlated with more hours spent on an OSC per week (R=0.259, p<0.001), and daily OSC users had higher FoP affective scores compared to those engaging in OSC less than daily (10.7 ± 3.2 vs. 9.8 ± 3.2, p=0.006). Patient-perceived shared medical decision making with treating provider was also weakly correlated with less hours spent on OSC (R=−0.159, p=0.007). OSC frequency was not associated with the number of prior treatments, as participants using an OSC daily (N=173) versus those using it less than daily (N=268) did not differ in their number of prior treatments (5.4±6.6 vs. 5.6±6.8, p=0.776).
Impact of OSC use on Medical Decision-Making
The influence of OSC on medical decision making within the cohort was significant. 35% (154/441) reported requesting a specific treatment, and 27% (120/441) reported visiting a specific physician based on information they read on the OSC (Table 3). When dichotomizing responses to questions about medical decision making into “influence” (possibly, probably, very probably, or definitely) and “no influence” (definitely not, probably not); age and college education of the patient were not significantly associated with OSC “influence” on treatments requested, surgical approach, or specific physician visited (Table 4). We then tested the hypothesis that more frequent OSC use was associated with more influence on medical decision-making. When dichotomizing frequency of OSC use to daily vs less-then-daily, greater OSC use was associated with a higher percentage of patients that requested a specific treatment (46% vs. 32%, p=0.007) surgical approach (46% vs. 36%, p=0.046), and physician (49% vs. 37%, p=0.016) based on information they read on the OSC (Table 4). Lastly, among OSC users, participants who were influenced by OSC in surgical decision-making had significantly higher FoP affective score (10.5 ± 3.2 vs. 9.6 ± 3.1, p=0.008), which was also true for what treatments they requested from their physician (10.5 ± 3.2 vs. 9.5 ± 3.1, p=0.006).
Table 3.
Influence of OSC on decision-making
| Questions | Definitely Not | Probably Not | Possibly | Probably | Very Probably | Definitely |
|---|---|---|---|---|---|---|
| To what extent has the social media support group influenced your surgical decision-making? | 72 (16.3%) | 86 (19.5%) | 96 (21.8%) | 45 (10.2%) | 69 (15.6%) | 71 (16.1%) |
| To what extent has the social media support group influenced What treatments you have requested from your doctor? | 59 (13.4%) | 68 (15.4%) | 88 (20.0%) | 71 (16.1%) | 74 (16.8%) | 78 (17.7%) |
| To what extent has the social media support group influenced what doctor to see? | 131 (29.7%) | 96 (21.8%) | 51 (11.6%) | 43 (9.8%) | 28 (6.3%) | 89 (20.2%) |
| To what extent has the social media support group influenced What alternative treatments you have tried (e.g., CBD oil, acupuncture)? | 90 (20.4%) | 99 (22.4%) | 116 (26.3%) | 42 (9.5%) | 41 (9.3%) | 46 (10.4%) |
Table 4.
Comparison of people who were influenced by an OSC regarding different decision-making parameters, versus participants who were not influenced in that respective parameter.
| Variables influenced from engagement in OSC | Mean age (those influenced vs those that were not) | College-educated (those influenced vs those that were not) | Daily OSC use (those influenced vs those that were not) |
|---|---|---|---|
| Surgical decision-making (N=281, 63.7%) | 48.8±10.2 vs. 50.3±11.0 (p=0.170) | 71.9% vs. 70.0% (p=0.687) | 45.9% vs. 36.1% (p=0.046) |
| Treatments they requested from their physician (N=311, 70.5%) | 48.8±10.5 vs. 506±10.5 (p=0.118) | 72.4% vs. 68.0% (p=0.369) | 46.3% vs. 32.3% (p=0.007) |
| Visiting specific doctors (N=211, 47.8%) | 49.4±10.1 vs. 49.2±10.8 (p=0.902) | 71.1% vs. 71.0% (p=0.996) | 48.6% vs. 37.2% (p=0.016) |
| Alternative treatments (e.g. CBD oil, acupuncture) (N=245, 55.6%) | 48.1±10.2 vs. 50.7±10.6 (p=0.011)* | 70.2% vs. 71.9% (p=0.711) | 45.7% vs. 38.5% (p=0.133) |
| Visiting a specific physician or changing their physician (N=120, 27.2%) | 49.2±10.1 vs. 49.6±10.7 (p=0.773) | 78.5% vs. 68.2% (p=0.045) | 47.5% vs. 40.6% (p=0.190) |
Although statistically different, this may not be clinically significant.
Discussion
This study of 755 iSGS patients investigated the potential benefits of OSC involvement, characteristics that make patients more likely to engage with these platforms, and the influence of OSC on decision-making and disease management. The presented cohort was representative of this patient population in institutional studies.10 It was observed that OSC users were more likely to be younger, female, and college educated, while the most common reasons for not using OSC were privacy concerns, technical difficulties, and being unaware of these online resources. This cohort reported that the most important benefits from OSC were hearing from others’ experience, learning about surgeries and treatments, learning about other doctors, sharing experience with others, supporting others and gaining support, and learning about relevant research. More disease anxiety had a weak positive correlation with more time on OSC, while higher scores for social support and shared decision-making were weakly associated with less time on OSC. Lastly, more disease anxiety or daily OSC use were weakly associated with a larger influence of OSC on treatment choice. These findings pertaining to the utility of OSCs among iSGS patients provide important value to the existing literature and warrant similar investigations into other debilitating head and neck conditions. Overall, these findings support the hypothesis that OSC are greatly utilized and influential among iSGS patients, and their effect, which goes well beyond just emotional experience sharing, may be underappreciated.
The internet and OSCs are an important and powerful source of information for individuals with chronic medical diseases.13,14 The current COVID-19 pandemic also hypothetically propelled most people to use online sources and OSCs more frequently. OSCs that are created and maintained through social media platforms such as Facebook are unique in that retention rates are high with regular and frequent user engagement. Facebook alone has 1.47 and 2.23 billion worldwide daily and monthly active users, respectively.15 Interestingly, OSCs can go beyond social media platforms and exist as part of medical organizations. For instance, the Mayo Clinic created its own social network for patients after recognizing the importance of social media.16 This paradigm shift is part of a larger technocultural medical revolution that is unlike anything that has faced medicine in the past.3 Despite their emerging prevalence, the full impact of OSC use is unknown and demands investigation. It has been suggested that patients who are active online may also become more involved with shared decision-making, health maintenance, and overall better relationship with their providers.17–19 Traditionally, physical support groups provided valuable benefit to patients’ disease experience, quality of life, or improved management in chronic conditions such as diabetes,20 cancer,21 or substance addiction.22 With the emergence of OSCs, established primarily through social media platforms such as Facebook, these have evolved into a significant support platform for patient.2,23,24 Since OSC can contribute to patient empowerment, education, and a sense of community,25,26 their utilization and influence in the field of head and neck surgery can have important implications.
Among the evaluated factors, low social support and higher disease anxiety were potential drivers of elevated OSC utilization. This is similar to a study of patients with implantable cardiovascular defibrillators attending physical support groups, where support group attendees had higher trait anxieties and less satisfaction with their social support.27 This suggests that iSGS patients with less support from family/friends or those who are more anxious regarding their condition are more likely to pursue and benefit from OSC engagement. Given that the presented cohort’s biggest reason for not engaging in OSC was unawareness, iSGS patients that have higher anxiety or less social support can be directed towards these helpful and resourceful platforms by clinicians. Internet use and shared decision-making may also have an intimate relationship. In a study by Hu and colleagues, authors reported that physician trust and willingness to involve in decision making were not related to online information seeking, but most responders intended to ask their physician questions and request clinical resources based on online information.2 In this cohort, higher shared decision-making scores were associated with less time spent on OSC. This could mean that patients who are more proactive in shared decision making with their providers needed less time spent on OSC, or that those with less information from OSC were more likely to engage in interactive conversations with their provider for better informed decisions.
Although the frequency of OSC use was not associated with number of treatments, examination of how OSCs use in general influenced patient decision-making is important and potentially significant for both patients and clinicians. This study demonstrated that 32–35% of OSC users were significantly influenced by OSC regarding surgical decision-making or what treatment they requested, and 20–27% regarding what doctor they saw or what alternative treatments they tried. These findings are intriguing and point to a strong influence of these peer-controlled platforms regarding treatment direction and final actions by the patients. Previous reports showed that engagement with engagement with a breast cancer OSC led 31% of participants to seek a second opinion or bring additional information to the attention of their treating physician.24 Moreover, after participating in a prostate OSC, 29% of patients changed how their disease was treated.28 It is becoming clear that the utility of OSCs is not limited to emotional support as previously imagined, but it also play a key role in influencing decision-making, treatment directions, and patient empowerment.26 One interesting component of OSCs, as evident by this study’s cohort, is that only a small number of people actively post and respond to topics, relative to the large number of people that only read and react to posts. The fact that a small number of self-selected individuals influence medical care raises interesting questions about how patients generalize the information that they gain from these communities. Interestingly, both those who primarily write and those that primarily read posts can have similar benefits from OSCs.29,30
OSCs represent a new medium in which patient experience and decision-making is influenced. Historically, medical care was delivered and practiced within a “paternalistic” model in which information was given to a patient by a physician.31 The advent of online information and OSC groups has potentially transitioned this to a collaborative model with more patient empowerment. A new reality exists in which physicians must become comfortable with information being obtained outside of the confines of the physician’s office and recognize the power of those networks to influence their practice. Qualitative interviews of physicians highlight the opinion that without the proper scientific and medical background, there is a natural limit as to how much patients can direct their own medical care.32 Regardless, rather than questioning the legitimacy of the resource which may now be an inevitable factor in delivering medical care to patients, physicians should recognize the power of OSCs and incorporate open discussions of information obtained through these networks in clinical encounters. The role of physician participations in OSCs is also an interesting question that merits the input of patient groups and future studies.
Despite our rigorous approach, several limitations should be mentioned. This was a survey study and the extent of OSC utilization (e.g. hours) was subjectively reported by patients rather than objective measures such as OSC web metrics. Additionally, since individuals with iSGS are primarily female and Caucasian, the generalizability of these results to iSGS patients who do not fit these criteria are unknown. Furthermore, only individuals that were enrolled in NoACC cohort were enrolled, which could introduce selection bias as these individuals are possibly more interactive in managing their disease or participating in online resources. Lastly, it is unclear whether “weakly correlated” results are clinically significant, which would require future prospective studies focusing on these metrics and change in decision-making over time. Although it could be argued that some of the statistically different comparisons may be clinically similar (e.g., FoP affective scores), these results still demonstrate consistent and interesting trends regarding medical OSC use, warranting continuous investigations. Future research should also investigate whether some of the findings have a one-way direction (e.g. more disease anxiety causes more OSC engagement) or whether it is a self-reinforcing cycle. Given there also exist active Facebook groups for other conditions treated by otolaryngologists such as tinnitus, thyroid disease, and acoustic neuroma, future studies should also investigate whether certain disease characteristics (e.g. chronic nature, poor quality of life, gender/age skewness) make patients more receptive to OSC engagement. Despite these limitations, this study provides important findings that are novel in the field of Otolaryngology-Head and Neck Surgery. Medical researchers have only begun to investigate the power of social media as a platform for targeted public health interventions, which can benefit large populations in many ways.33 A better understanding of how medical professionals can support this important medium can potentially help patients beyond the immediate treatment that is provided.
Conclusion
Patients with iSGS commonly engage in an OSC, which can influence their disease experience and medical decision-making. OSC utilization was associated with younger age, female gender, college education, increased disease anxiety, and lower scores for social support and shared decision making. Many OSC users were influenced by this platform regarding what surgeries, treatments, and physicians were chosen. These support mediums are gaining popularity and influence, and continued investigation into their role in iSGS and other otolaryngologic diseases is warranted.
Funding:
This work was funded by grant 1409-22214 from the Patient Centered Outcomes Research Institute. Dr. Gelbard is also supported by grant R01HL146401-01 from the National Heart, Lung, and Blood Institute, NIH. The funding entities had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, approval, or decision to submit the manuscript for publication.
References
- 1.Fox S The Social Life of Health Information, 2011. 2011; http://pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx. Accessed 8/17/2018.
- 2.Hu X, Bell RA, Kravitz RL, Orrange S. The prepared patient: information seeking of online support group members before their medical appointments. J Health Commun. 2012;17(8):960–978. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson T, Frydman G. The first generation of e-patients. BMJ. 2004;328(7449):1148–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Uden-Kraan CF, Drossaert CHC, Taal E, et al. Coping with somatic illnesses in online support groups: Do the feared disadvantages actually occur? Comput Hum Behav. 2008;24(2):309–324. [Google Scholar]
- 5.Greene JA, Choudhry NK, Kilabuk E, Shrank WH. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. J Gen Intern Med. 2011;26(3):287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haik D, Kashanchi K, Tajran Sarah et al. The Online support Group as a community: A thematic content analysis of an online support group for Idiopathic Subglottis Stenosis. Ann Otol Rhinol Laryngol. 2019; 128:293–299. [DOI] [PubMed] [Google Scholar]
- 7.Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J. Twitter Social Media is an Effective Tool for Breast Cancer Patient Education and Support: Patient-Reported Outcomes by Survey. J Med Internet Res. 2015;17(7):e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huber J, Maatz P, Muck T, et al. The effect of an online support group on patients treatment decisions for localized prostate cancer: An online survey. Urol Oncol. 2017;35(2):37 e19–37 e28. [DOI] [PubMed] [Google Scholar]
- 9.Gerber BS, Eiser AR. The patient physician relationship in the Internet age: future prospects and the research agenda. J Med Internet Res. 2001;3(2):E15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope. 2016;126(6):1390–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haik D, Kashanchi K, Tajran S, et al. The online support group as a community: a thematic content analysis of an online support group for idiopathic subglottic stenosis. Ann Otol Rhinol Laryngol. 2019;128(4):293–299. [DOI] [PubMed] [Google Scholar]
- 12.Chan Y Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614–619. [PubMed] [Google Scholar]
- 13.Coulson NS, Buchanan H, Aubeeluck A. Social support in cyberspace: a content analysis of communication within a Huntington’s disease online support group. Patient education and counseling. 2007;68(2):173–178. [DOI] [PubMed] [Google Scholar]
- 14.Barak A, Boniel-Nissim M, Suler J. Fostering empowerment in online support groups. Computers in human behavior. 2008;24(5):1867–1883. [Google Scholar]
- 15.Results. FQ. https://s21.q4cdn.com/399680738/files/doc_financials/2018/Q2/Q2-2018-Earnings-Presentation.pdf. investorfbcom. 2018.
- 16.Kotsenas AL, Aase L, Arce M, et al. The social media DNA of Mayo Clinic—and health care. J Am Coll Radiol. 2018;15(1):162–166. [DOI] [PubMed] [Google Scholar]
- 17.Broom A Virtually he@lthy: the impact of internet use on disease experience and the doctor-patient relationship. Qual Health Res. 2005;15(3):325–345. [DOI] [PubMed] [Google Scholar]
- 18.Snipes RL, Ingram R, Jiang P. Information search in health care decision-making: A study of word-of-mouth and Internet information users. J Hosp Mark Public Relations. 2005;15(2):33–53. [DOI] [PubMed] [Google Scholar]
- 19.Iverson SA, Howard KB, Penney BK. Impact of internet use on health-related behaviors and the patient-physician relationship: a survey-based study and review. J Am Osteopath Assoc. 2008;108(12):699. [PubMed] [Google Scholar]
- 20.Gilden JL, Hendryx MS, Clar S, Casia C, Singh SP. Diabetes support groups improve health care of older diabetic patients. J Am Geriatr Soc. 1992;40(2):147–150. [DOI] [PubMed] [Google Scholar]
- 21.Cain EN, Kohorn EI, Quinlan DM, Latimer K, Schwartz PE. Psychosocial benefits of a cancer support group. Cancer. 1986;57(1):183–189. [DOI] [PubMed] [Google Scholar]
- 22.Tracy K, Wallace SP. Benefits of peer support groups in the treatment of addiction. Subst Abuse Rehabil. 2016;7:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Indian M, Grieve R. When Facebook is easier than face-to-face: Social support derived from Facebook in socially anxious individuals. Pers Individ Dif. 2014;59:102–106. [Google Scholar]
- 24.Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J. Twitter social media is an effective tool for breast cancer patient education and support: patient-reported outcomes by survey. J Med Internet Res. 2015;17(7):e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Idriss SZ, Kvedar JC, Watson AJ. The role of online support communities: benefits of expanded social networks to patients with psoriasis. Arch Dermatol. 2009;145(1):46–51. [DOI] [PubMed] [Google Scholar]
- 26.Van Uden-Kraan CF, Drossaert CH, Taal E, Seydel ER, van de Laar MA. Participation in online patient support groups endorses patients’ empowerment. Patient Educ Couns. 2009;74(1):61–69. [DOI] [PubMed] [Google Scholar]
- 27.Myers GM, James GD. Social support, anxiety, and support group participation in patients with an implantable cardioverter defibrillator. Prog Cardiovasc Nurs. 2008;23(4):160–167. [DOI] [PubMed] [Google Scholar]
- 28.Huber J, Maatz P, Muck T, et al. The effect of an online support group on patients׳ treatment decisions for localized prostate cancer: An online survey. Urol Oncol. 2017; 35:19–27. [DOI] [PubMed] [Google Scholar]
- 29.Setoyama Y, Yamazaki Y, Namayama K. Benefits of peer support in online Japanese breast cancer communities: differences between lurkers and posters. J Med Internet Res. 2011;13(4):e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Uden-Kraan C, Drossaert C, Taal E, Seydel E, van de Laar M. Self-reported differences in empowerment between lurkers and posters in online patient support groups. J Med Internet Res. 2008;10(2):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. Jama. 1992; 267(16):2221–2226. [PubMed] [Google Scholar]
- 32.Grünloh C, Myreteg G, Cajander Å, Rexhepi H. “Why do they need to check me?” Patient participation through eHealth and the doctor-patient relationship: qualitative study. J Med Internet Res. 2018;20(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huesch MD, Galstyan A, Ong MK, Doctor JN. Using social media, online social networks, and internet search as platforms for public health interventions: a pilot study. Health Serv Res. 2016;51:1273–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]


