Abstract
Whether glucocorticoid receptor α (GRα) serves a role in obstructive sleep apnea/hypopnea syndrome (OSAHS) remains unclear. However, it has been reported that GRα expression is decreased in the adenoids of patients with OSAHS. The present study aimed to evaluate the role of GRα in OSAHS and the underlying mechanism. Bioinformatics assays revealed that long noncoding RNA (lncRNA) X inactivate-specific transcript (XIST) was closely associated with GRα. Furthermore, reverse transcription-quantitative PCR showed that the expression of lncRNA XIST was significantly increased in the adenoids of patients with OSAHS compared with healthy controls. Further in vitro studies by Pearson correlation analysis, RNA pull-down assay, western blot analysis and ELISA demonstrated that XIST significantly decreased the expression of GRα and that significantly increased the production of inflammatory cytokines, including interleukin (IL)-8, tumor necrosis factor α, IL-6 and IL-1β, while the overexpression of GRα significantly decreased the production of these inflammatory cytokines in NP69 cells, a human nasopharyngeal epithelial cell line. Furthermore, XIST significantly increased the protein levels of nuclear factor κ-light-chain-enhancer of activated B cells (NF-κB) subunits, including Rel-B, c-Rel, P52, P50 and P65, which are associated with the transcription of cytokines. The stimulatory effect of XIST was significantly inhibited by the NF-κB inhibitor EVP4593. These results indicated that the stimulatory effect of XIST was dependent on NF-κB. In summary, the present study demonstrated that the XIST-GRα-NF-κB signaling pathway contributed to inflammation in the adenoids of patients with OSAHS.
Keywords: X inactivate-specific transcript, glucocorticoid receptor α, nuclear factor κ-light-chain-enhanced of activated B cells, obstructive sleep apnea/hypopnea syndrome, inflammation
Introduction
Obstructive sleep apnea/hypopnea syndrome (OSAHS) is the most common type of apnea (1). It is characterized by recurrent episodes of partial or complete upper airway collapse during sleep (2). OSAHS has been demonstrated to be associated with several comorbidities, including cardiovascular and neurodegenerative disorders, such as Alzheimer's disease and Parkinson's disease (3-5). Previous findings have shown that the physiological and pharmacological actions of glucocorticoids are mediated by the glucocorticoid receptor (GR), which is a member of the nuclear receptor superfamily of ligand-dependent transcription factors (6). Following glucocorticoid binding, GR induces or represses the transcription of target genes, which comprise up to 10-20% of the human genome (7). For instance, GR has been previously reported to positively regulate the transcription of FNDC5 in the liver (8), whilst another study revealed that Angptl4 is a GR primary target gene in hepatocytes and adipocytes (9). The expression of GRα has been demonstrated to be decreased in patients with OSAHS. For instance, the expression of GRα in the tonsil tissues of children with OSAHS was significantly lower compared with the tonsil tissues of children without OSAHS (10). However, the mechanism by which GRα is dysregulated in patients with OSAHS remains unknown.
Long noncoding RNAs (lncRNAs) are a class of transcripts >200 nucleotides in length (11). Generally, lncRNAs do not encode proteins (12). Accumulating data have indicated that lncRNAs exert crucial functions in gene regulation, biological processes and several diseases, including inflammation (13) and immune responses (14). LncRNA X inactivate-specific transcript (XIST) is a 17-kb long RNA and is transcribed from the inactive X chromosome in female mammalians. Previous studies have indicated that the expression of XIST is upregulated in various diseases, such as in basal-like human breast cancer (15) and cystic fibrosis (16). However, it remains unclear whether XIST serves a role in OSAHS.
It has been well documented that nuclear factor κ-light-chain-enhancer of activated B cells (NF-κB) serves a vital role in inflammation (17). The IκB kinase enzyme complex is part of the upstream NF-κB signal transduction cascade and the IκBα protein inactivates transcription factor of NF-κB by inhibiting the nuclear localization signals of NF-κB and sequestering it to an inactive state in the cytoplasm (18). NF-κB is a protein complex composed of homo- or heterodimers formed by different combinations of the five monomeric NF-κB subunits: p65/Rel A, Rel B, c-Rel, p50 and p52(19). Activated NF-κB regulated cell proliferation, apoptosis and the production of inflammatory cytokines, including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6 and IL-8 (20,21).
In conclusion, the present study specially focused on the role and mechanism of GRα in adenoids of patients with OSAHS, the results of which may provide a potential novel insight for treatment of OSAHS.
Materials and methods
Patients and sample collection
The present study was approved by the Ethics Committee and Animal Care Committee of the Affiliated Hangzhou First People's Hospital, Zhejiang University School of Medicine, Hangzhou, China. The legal guardians of all the participants read and signed informed consent forms. Both inclusion and exclusion criteria were first assessed through review of the electronic medical record. Inclusion criteria were: i) Age ≤12 years old; ii) able to obtain written informed consent from legal guardians; iii) hospitalized patients having a documented history of congestive heart failure in agreement with the 2013 ACCF/AHA heart failure definition (22); iv) anticipated hospitalization of >24 h. Exclusion criteria were: i) Established obstructive sleep apnea and/or previous exposure to positive airway pressure (PAP) therapy; ii) Presence of any active conditions that the investigators felt would interfere with testing or potential therapy (hemodynamic instability, respiratory failure, unconsciousness, pneumothorax, penetrating chest trauma, general nausea/vomiting, facial anomalies/facial trauma, upper gastrointestinal bleed or history of recent gastric surgery); iii) presence of a clinically significant illness or medical condition that the investigators felt would prohibit the subject from participating in the study (a number of subjects were ruled due to advanced COPD, malignancy or having a high baseline home oxygen requirement).
According to the apnea-hypopnea index, the patients were diagnosed with OSAHS when apnea-hypopnea occurred ≥ one time per hour, as previously described (23). Adenoid tissue specimens were collected from children with OSAHS (n=26) and healthy donors (n=21) with myocarditis at the Department of Otorhinolaryngology, Affiliated Hangzhou First People's Hospital, Zhejiang University School of Medicine, from May 2017 to May 2018. Mean age of the OSAHS group (19 females and 7 males) was 6.88±3.18 years. Mean age of the healthy donor group (19 females and 2 males) was 7.2±2.63 years. No local or systemic glucocorticoid treatment was given to any of the patients within 2 weeks to 2 months prior to the operations.
Cell cultures
Human nasopharyngeal epithelial cell line NP69 purchased from American Type Culture Collection (ATCC) was cultured in keratinocyte-SFM medium (Invitrogen; Thermo Fisher Scientific, Inc.). All cells were grown in a humidified incubator with a 5% CO2 atmosphere at 37˚C, as previously described (24). Additionally, EVP4593 (cat. no. HY-13812; MedChemExpress), an inhibitor of NF-κB signaling, was used to treat NP69 cells. DMSO was used as the control.
Cell transfections
Total RNA was extracted from adenoid tissue tissues and NP69 cells using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.) and synthesized into first-strand cDNA using an M-MLV Reverse Transcriptase kit (cat. no. 28025013; Invitrogen; Thermo Fisher Scientific, Inc.) as previously described (25). Full-length XIST was amplified from female genomic DNA (Roche diagnostics) and then digested with XbaI to obtain nucleotides 105-10747 of the XIST cDNA sequence (accession no. M97168) and inserted into pcDNA3.1 vectors (Invitrogen; Thermo Fisher Scientific, Inc.) to overexpress XIST. GRα overexpression plasmids were constructed using the pcDNA3.1 backbone from Sangon Biotechnology Co., Ltd. XIST short hairpin (sh) RNA sequences were inserted into shRNA vectors (Shanghai GenePharma Co., Ltd.). The actual DNA sequence of the shRNA that was ligated into the pGPH1 vector were as follows: sh-NC, 5'-CACCGCTATGATATCGTCTGTTTCAAGAGAACAGACGATATCATAGCTTTTTTG-3' and sh-XIST, 5'-CACCGCATCTGACTGTTATGTTTCAAGAGAACATAACAGTCAGATGCTTTTTTG-3'. Cells (1x105 cells/well) were seeded in 24-well plates and 500 µl of keratinocyte-SFM medium (Invitrogen; Thermo Fisher Scientific, Inc.) was added to each well. When the cells reached 40-60% confluence, the aforementioned vectors were transfected into cells at a final concentration of 50 nM using Lipofectamine® 2000 reagent (Invitrogen; Thermo Fisher Scientific, Inc.) at 37˚C and 5% CO2 for 48 h, according to the manufacturer's protocol.
RNA extraction and reverse transcription-quantitative PCR (RT-qPCR)
Total RNA was extracted from adenoid tissue tissues and NP69 cells using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.) and synthesized into first-strand cDNA using an M-MLV Reverse Transcriptase kit (cat. no. 28025013; Invitrogen; Thermo Fisher Scientific, Inc.) as previously described (25). qPCR was performed using a One Step TB Green PrimeScript RT-PCR kit II (cat. no. RR086A; Takara Bio, Inc.). mRNA expression levels were normalized to U6 and GAPDH using the 2-ΔΔCq method (26). The following thermocycling conditions were used: Initial denaturation at 95˚C for 3 min, followed by 40 cycles at 95˚C for 5 sec, 60˚C for 30 sec and at 72˚C for 45 sec, before final extension at 72˚C for 3 min. Primer sequences are listed in Table I.
Table I.
Primers used for reverse transcription-quantitative PCR.
| Gene | Forward | Reverse |
|---|---|---|
| GRα | CGAGCTCGTGTCTGTGACG | AGAAAGTCTCCCATTGCCCA |
| IL-8 | GAAGAGAGCTCTGTCTGGACC | ACTGGCATCTTCACTGATTCT |
| TNFα | CTGGGGCCTACAGCTTTGAT | GGCCTAAGGTCCACTTGTGT |
| IL-6 | TATGAACTCCTTCTCCACAAGCG | AATCTTCTCCTGGGGGTACTGG |
| IL-1β | GCAGAAGTACCTGAGCTCGC | CTTGCTGTAGTGGTGGTCGG |
| XIST | TGCATTTCCTTTCTGCCTCT | TGCCCACATATGCAAAGAAA |
| GAPDH | CCGCATCTTCTTTTGCGTCG | TTCACCTTCCCCATGGTGTC |
GRα, glucocorticoid receptor α; IL, interleukin; TNFα, tumor necrosis factor α; XIST, X inactivate-specific transcript.
Western blotting
Cells were lysed with lysis buffer containing protease inhibitors (50 mM Tris-HCl pH 8; 50 mM NaCl; 0.5% NP-40). Total protein was extracted from adenoid tissues and NP69 cells using RIPA buffer (Thermo Fisher Scientific, Inc.). Protein concentration was determined using a bicinchoninic acid assay. Equal amounts of protein (5 µg for each sample) were resolved by 10% SDS-PAGE gels and transferred to PVDF membranes. Following blocking with 5% non-fat milk at 25˚C for 1 h, the membranes were immunoblotted with primary antibodies against GRα (cat. no. ab3580), IL-8 (cat. no. ab18672), tumor necrosis factor α (TNFα; cat. no. ab1793), IL-6 (cat. no. ab6672), IL-1β (cat. no. ab9722), Rel-B (cat. no. ab180127), Rel-C (cat. no. ab133251), P52 (cat. no. ab264236), P50 (cat. no. ab32360) and P65 (cat. no. ab16502) at a dilution of 1:1,000 overnight at 4˚C. All primary antibodies were purchased from Abcam. After washed using TBS + 0.1% Tween for 10 min three times, the membranes were exposed to horseradish peroxidase-conjugated goat anti-rabbit antibodies (1:5,000; cat. no. sc-2357, Santa Cruz Biotechnology, Inc.) Secondary antibodies and signals were detected using an ECL detection system (Thermo Fisher Scientific, Inc.). GAPDH (cat. no. ab8245; 1:1,000; Abcam) was used as the loading control. Images were analyzed using ImageJ software (version 1.51; National Institutes of Health).
ELISA
NP69 cell supernatants cultured in 24-well plates were collected and the production of inflammatory cytokines was measured using ELISA kits (R&D Systems, Inc.) including interleukin 6 (IL-6; cat. no. D6050), interleukin 8 (IL-8; cat. no. D8000C), tumor necrosis factor-α (TNF-α; cat. no. MTA00B) and interleukin-1β (IL-1β; cat. no. MLB00C), according to the manufacturer's protocols. Levels of inflammatory cytokines were quantified by normalizing the protein concentrations (27).
Bioinformatics analysis
The binding site of XIST and GRαwas predicted by starBase 2.0 website (http://starbase.sysu.edu.cn).
RNA pull-down assay
RNA pull-down assays were used to confirm the interaction between XIST and GRα. Bio-NC, Bio-XIST and Bio-XIST-Mutant constructs were synthesized by Shanghai Genepharma Co., Ltd. The sequences were shown in Supplementary Table I. XIST was labeled with biotin to generate the constructs. Sequences for the constructs are provided in Table SI. Bio-NC was used as the negative control and input, which is the cell lysate, was used as the positive control. Following this, RIPA lysis buffer (Sangon Biotech Co., Ltd.) containing RNase inhibitors (Invitrogen; Thermo Fisher Scientific, Inc.) was utilized to lyse cells. Bio-XIST-WT, Bio-XIST-MUT or Bio-NC constructs (200 pmol) were added to supernatants and Dynabeads™ M-270 Streptavidin (1 mg; cat. no. 65305; Invitrogen; Thermo Fisher Scientific, Inc.) and proteinase K (Sigma-Aldrich; Merck KGaA) were added and incubated with the supernatants overnight at 4˚C to isolate the RNA. Beads were isolated from the supernatant after centrifugation (2,500 x g, 5 min, 4˚C) and washed with wash buffer (10 mM Tris-HCl pH 7.5, 1 mM EDTA, 2 M NaCl and 0.1% Tween-20) followed by another centrifugation step (2,500 x g, 5 min, 4˚C). The pellet was then collected and the RNA-RNA complexes were eluted using Tris-EDTA buffer (Invitrogen; Thermo Fisher Scientific, Inc.) and purified using ethanol. Subsequently, the degree of XIST and GRα enrichment was analyzed by RT-qPCR as aforementioned.
Statistical analysis
Data are presented as mean ± standard deviation. For comparison between two groups, unpaired Student's t-test was applied. For comparison between multiple groups, data were analyzed by one-way ANOVA followed by Tukey's post hoc test. Pearson's correlation analysis was used to examine the correlation between the levels of XIST and GRα. Statistical analysis was performed using SPSS software (version 22.0; IBM Corp.). P<0.05 was considered to indicate a statistically significant difference.
Results
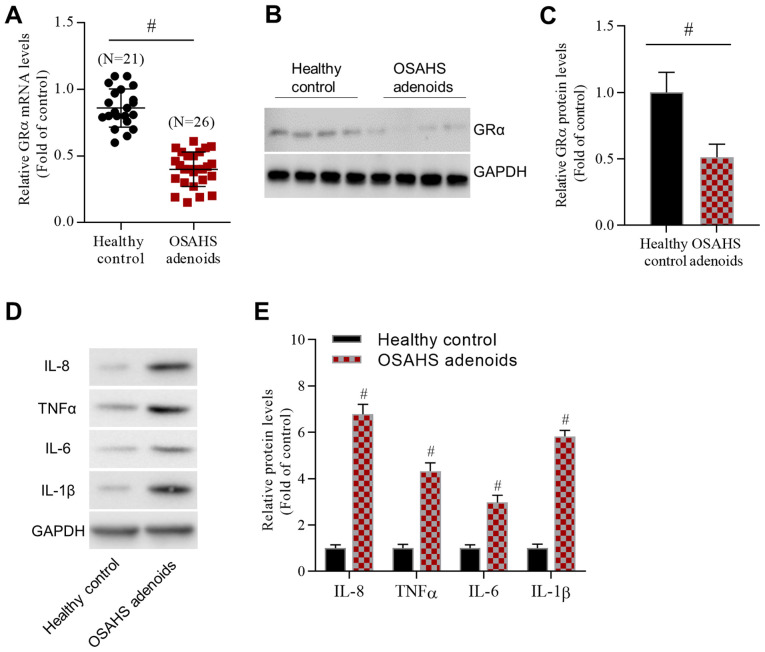
GRα is decreased in the adenoids of patients with OSAHS
Previous studies have demonstrated that GRα is an important factor in the inhibition of inflammation. The current study verified GRα expression in the adenoids of patients with OSAHS. GRα mRNA was significantly decreased in the adenoids of patients with OSAHS compared with healthy controls (Fig. 1A). Additionally, GRα protein levels were significantly decreased in the adenoids of patients with OSAHS compared with healthy controls (Fig. 1B and C). In contrast, the western blot results demonstrated that the protein levels of inflammatory cytokines, including IL-8, TNFα, IL-6 and IL-1β, were significantly increased in the adenoids of patients with OSAHS patients compared with healthy controls (Fig. 1D and E). In summary, GRα expression was decreased and inflammatory cytokine expression was increased in the adenoids of patients with OSAHS.
Figure 1.
GRα is highly expressed in the adenoids of patients with OSAHS. (A) Reverse transcription-quantitative PCR data demonstrated changes in GRα mRNA levels. (B) Representative western blot images and (C) analyzed data reported changes in GRα protein levels. (D) Representative western blot images and (E) analyzed data revealed changes in the levels of inflammatory cytokines, including IL-8, TNFα, IL-6 and IL-1β. For IL-8, IL-6 and IL-1β, n=4/group. For TNFα, n=5/group. #P<0.05 vs. the healthy control group. GRα, glucocorticoid receptor α; OSAHS, obstructive sleep apnea/hypopnea syndrome; IL, interleukin; TNFα, tumor necrosis factor α.
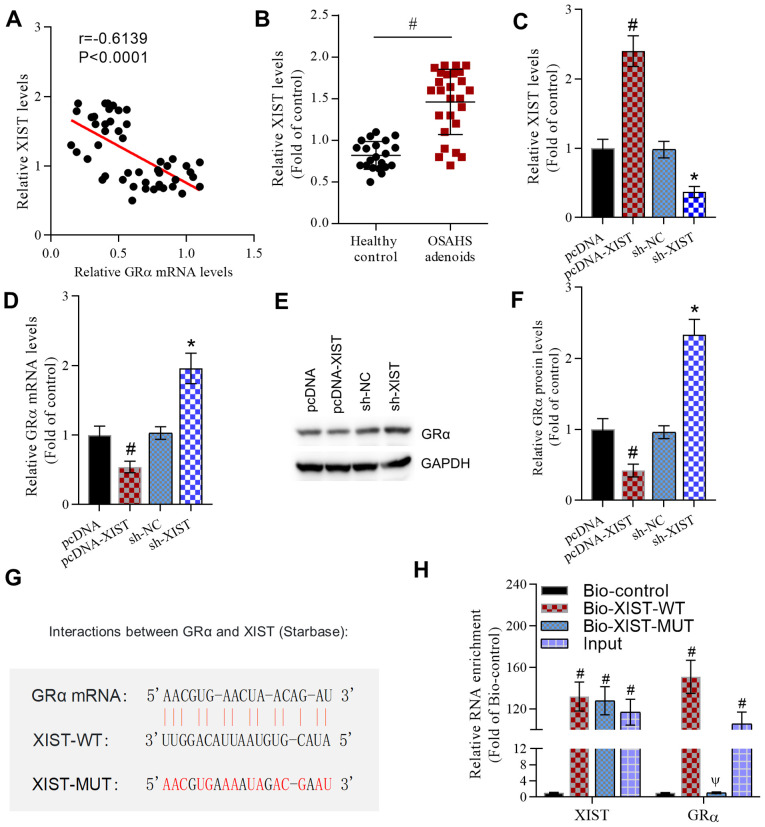
XIST negatively regulates GRα expression
A bioinformatics assay using the Starbase database demonstrated that lncRNA XIST was closely associated with GRα. To determine whether XIST interacted with GRα, the association between the expression levels of XIST and GRα was analyzed using Pearson's correlation analysis. According to the results, the expression of XIST was negatively correlated with the expression of GRα (Fig. 2A). In contrast to the expression of GRα, RT-qPCR demonstrated that the expression of XIST was significantly increased in the adenoids of patients with OSAHS compared with healthy controls (Fig. 2B). Furthermore, pcDNA-XIST significantly increased XIST levels and XIST shRNA significantly decreased XIST levels in NP69 cells compared with those in the pcDNA and sh-NC groups, respectively (Fig. 2C). Additionally, the potential effect of XIST on GRα expression was investigated. XIST overexpression significantly decreased GRα mRNA levels and XIST shRNA significantly increased GRα mRNA levels compared with those in the pcDNA and sh-NC groups, respectively (Fig. 2D). Similarly, pcDNA-XIST significantly decreased GRα protein levels and XIST shRNA significantly increased the GRα protein levels compared with those in the pcDNA and sh-NC groups, respectively (Fig. 2E and F). Following this, the interaction between XIST and GRα was examined. The predicted binding sites for XIST and GRα were obtained from the Starbase database (Fig. 2G). Bio-XIST-WT and Bio-XIST-MUT constructs were generated for RNA pull-down assays. The results demonstrated that XIST and GRα were enriched in the Bio-XIST-WT group compared with the Bio-XIST-MUT group (Fig. 2H). These results indicated that XIST negatively regulated GRα.
Figure 2.
XIST negatively regulates GRα expression. (A) Pearson's correlation analysis indicated a negative correlation between the XIST and GRα mRNA levels. r=-0.6139. P<0.0001. (B) RT-qPCR revealed increased XIST expression levels in the adenoids of patients with OSAHS compared with healthy controls. #P<0.05 as indicated. (C) RT-qPCR data demonstrated the effect of the overexpression or knockdown of XIST on XIST levels in NP69 cells. #P<0.05 vs. the pcDNA group and *P<0.05 vs. the sh-NC group. (D) RT-qPCR data revealed the effect of the overexpression or knockdown of XIST on GRα mRNA levels in NP69 cells. #P<0.05 vs. the pcDNA group and *P<0.05 vs. the sh-NC group. (E) Representative western blot images and (F) analyzed data demonstrated the effect of the overexpression or knockdown of XIST on GRα protein levels in NP69 cells. #P<0.05 vs. the pcDNA group and *P<0.05 vs. the sh-NC group. (G) The binding sites and mutated sites of XIST and GRα. (H) RNA pull-down assays confirmed the interaction between XIST and GRα. #P<0.05 vs. the Bio-control group and ΨP<0.05 vs. the Bio-XIST-WT group. No significance between GRα enrichment in Bio-XIST-MUT and Bio-control group. For XIST, n=4/group. For GRα, n=5/group. XIST, X inactivate-specific transcript; GRα, glucocorticoid receptor α; RT-qPCR, reverse transcription-quantitative PCR; OSAHS, obstructive sleep apnea/hypopnea syndrome; sh, short hairpin; NC, negative control; WT, wild-type; MUT, mutant.
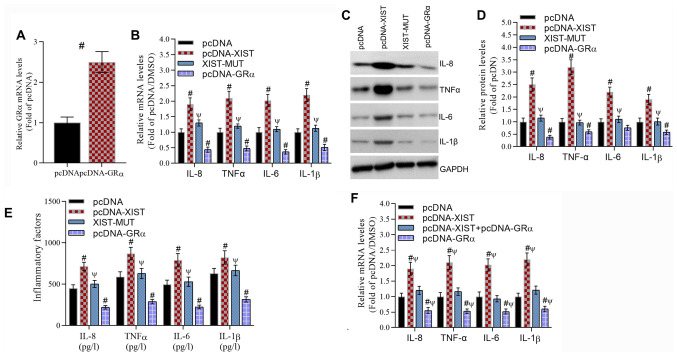
The XIST-GRα signaling pathway regulates the production of inflammatory cytokines
Whether the XIST-GRα axis regulated inflammation was investigated. GRα expression was significantly overexpressed by pcDNA-GRα transfection compared with that following pcDNA transfection (Fig. 3A). XIST significantly increased the mRNA levels (Fig. 3B), protein levels (Fig. 3C and D and E) concentrations of inflammatory cytokines, including IL-8, TNFα, IL-6 and IL-1β, compared with those in the pcDNA group. However, these stimulatory effects were reversed by XIST-MUT. Therefore, GRα overexpression significantly decreased the mRNA levels, protein levels and concentrations of IL-8, TNFα, IL-6 and IL-1β compared with those in the pcDNA group. Furthermore, the stimulatory effect of XIST on the production of inflammatory cytokines was significantly reversed by GRα compared with that in the pcDNA and pcDNA-XIST + pcDNA-GRα groups (Fig. 3F). These data indicated that the XIST-GRα signaling pathway contributed to the regulation of inflammatory cytokine production.
Figure 3.
XIST promotes the production of inflammatory cytokines, including IL-8, TNFα, IL-6 and IL-1β, that depend on the binding of XIST and GRα. (A) RT-qPCR data demonstrated the effect of GRα overexpression on GRα mRNA levels. #P<0.05 vs. the pcDNA group. (B) RT-qPCR data revealed the effect of XIST-WT, XIST-MUT and GRα overexpression on the mRNA levels of inflammatory cytokines. #P<0.05 vs. the pcDNA group and ΨP<0.05 vs. the XIST group. (C) Representative western blotting images and (D) analyzed data demonstrated the effect of XIST-WT, XIST-MUT and GRα overexpression on the protein levels of inflammatory cytokines. #P<0.05 vs. the pcDNA group and ΨP<0.05 vs. the XIST group. (E) Analyzed data revealed the effect of XIST-WT, XIST-MUT and GRα overexpression on the protein levels of inflammatory cytokines as determined by ELISA. #P<0.05 vs. the pcDNA group and ΨP<0.05 vs. the XIST group. (F) Analyzed data demonstrated that the inhibitory effect of GRα overexpression reversed the stimulatory effect of XIST on the protein levels of inflammatory cytokines as determined by ELISA. #P<0.05 vs. the pcDNA group and ΨP<0.05 vs. the XIST+GRα group. For IL-8, IL-6 and IL-1β, n=5/group. For TNFα, n=6/group. XIST, X inactivate-specific transcript; GRα, glucocorticoid receptor α; RT-qPCR, reverse transcription-quantitative PCR; WT, wild-type; MUT, mutant; IL, interleukin; TNFα, tumor necrosis factor α.
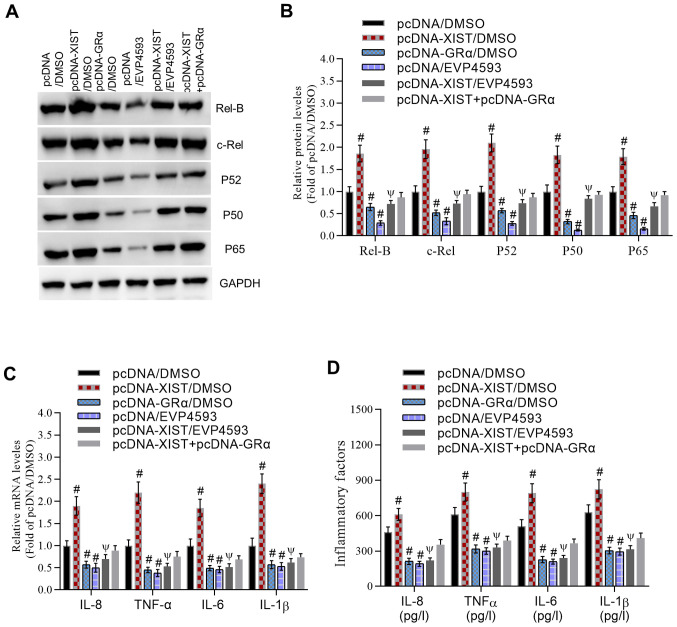
XIST regulates adenoidal inflammation through the GRα-mediated NF-κB pathway
Finally, we evaluated whether NF-κB was involved in XIST-GRα-induced inflammation. XIST significantly increased the protein levels of Rel-B, c-Rel, P52, P50 and P65 compared with that in the pcDNA/DMSO group (Fig. 4A and B). These effects were significantly inhibited by the NF-κB inhibitor EVP4593. Additionally, GRα inactivated the NF-κB pathway and significantly reversed XIST-induced expression of NF-κB pathway-associated proteins compared with that in the pcDNA-XIST/DMSO group. Similarly, XIST induced a significant increase in the mRNA levels (Fig. 4C) and concentrations (Fig. 4D) of IL-8, TNFα, IL-6 and IL-1β compared with those in the pcDNA/DMSO group. Furthermore, compared with those in the pcDNA-XIST/DMSO group, these levels were significantly inhibited by EVP4593 or GRα, counteracting the effects of XIST in facilitating the inflammatory response. These results indicated that XIST induced an inflammatory response through the GRα-mediated NF-κB pathway.
Figure 4.
XIST regulates adenoidal inflammation through the GRα-mediated NF-κB pathway. (A) Representative western blot images and (B) analyzed data demonstrated the inhibitory effect of the NFκB inhibitor EVP4593 and GRα on the XIST-induced increase in protein levels of Rel-B, c-Rel, P52, P50 and P65. (C) Reverse transcription-quantitative PCR data revealed the inhibitory effect of EVP4593 and GRα on the XIST-induced increase in the mRNA levels of inflammatory cytokines. (D) Analyzed data reported the inhibitory effect of EVP4593 and GRα on the XIST-induced increase in the protein levels of inflammatory cytokines as determined by ELISA. For IL-8, IL-6 and IL-1β, n=5/group. For TNFα, n=6/group. #P<0.05 vs. the pcDNA/DMSO group and ΨP<0.05 vs. the XIST/DMSO group. XIST, X inactivate-specific transcript; GRα, glucocorticoid receptor α; NF- κB, nuclear factor κ-light-chain-enhancer of activated B cells; IL, interleukin; TNFα, tumor necrosis factor α.
Discussion
OSAHS is a risk factor for hypertension, arrhythmia, coronary heart disease and other diseases (28). Therefore, investigating the specific molecular regulatory mechanisms of OSAHS is crucial. The current study evaluated whether GRα was involved in the inflammatory response in OSAHS. The results demonstrated that GRα expression was significantly decreased and XIST expression was significantly increased in the adenoids of patients with OSAHS compared with healthy controls. Further research revealed that XIST interacted with GRα and decreased GRα expression. Functionally, XIST increased the production of inflammatory cytokines, including IL-8, TNF-α, IL-6 and IL-1β, while GRα decreased their production. Furthermore, the results demonstrated that XIST-GRα axis-mediated inflammation was significantly inhibited by the NF-κB inhibitor EVP4593. These results indicated that the XIST-GRα-NF-κB signaling pathway contributed to inflammation in the adenoids of patients with OSAHS.
The current study reported that GRα was decreased in patients with OSAHS, which was consistent with a previous study that revealed that GRα was decreased in the tonsils of children with OSAHS (10). Furthermore, the present study demonstrated that decreased GRα contributed to increased inflammation in patients with OSAHS. Furthermore, the present study reported that XIST was upregulated and decreased the expression of GRα in patients with OSAHS. Consistent with the present study, accumulating data have demonstrated that XIST is upregulated and involved in various diseases, including basal-like human breast cancer (15) and cystic fibrosis (16). Shenoda et al (29) reported that XIST promotes inflammation through the pro-inflammatory transcription factor yin yang 1 in patients with complex regional pain syndrome. Those studies indicated that XIST served a critical role in inflammation. Additionally, XIST promotes the progression of non-small cell lung cancer through the microRNA (miR)-335/superoxide dismutase 2/reactive oxygen species pathway (30). Inhibition of XIST suppresses cell proliferation via modulation of the miR-744/ring finger protein 1 axis in non-small cell lung cancer (31). Suppression of XIST increases the secretion of exosomal miR-503, which triggers M1-M2 polarization of microglia and promotes brain metastasis (32). The results of the current study indicated that XIST interacted with GRα and inhibited GRα expression. GRα has been previously reported to serve an anti-inflammatory role in cardiomyocytes (33). The present study revealed that GRα alleviated the inflammatory response and inactivated the NF-κB pathway in NP69 cells.
Numerous previous studies have demonstrated that NF-κB serves a vital role in inflammation. For instance, it has been reported that NF-κB upregulated the synthesis and secretion of various pro-inflammatory cytokines, including TNF-α, IL-1β and IL-6. Fu et al (34) reported that pharmacologically inhibiting neddylation with MLN4924 suppressed pro-inflammatory cytokine generation through the NF-κB pathway in lipopolysaccharide (LPS)-stimulated HK2 cells and attenuates renal inflammation in LPS-induced acute kidney damage. Zhao et al (35) revealed that XIST upregulated TNF-α induced protein 1 expression to increase NF-kB activity and, therefore, exacerbating neuropathic pain in a rat model. XIST alleviates LPS-induced cell injury by modulating the Janus kinase/signal transducer and activator of transcription and NF-κB pathways (36). However, Ma et al (17) demonstrated that the expression of XIST was promoted by the activation of the NF-κB pathway and that XIST generated a negative feedback loop to regulate the NF-κB/NLR family CARD domain containing 6, leucine-rich repeat and PYD domain-containing protein 3 inflammasome pathways to mediate inflammatory processes. The aforementioned studies indicated that the association between XIST and NF-κB is complex. The present study identified that GRα suppressed activation of the NF-κB pathway and that XIST activated the NF-κB pathway through the inhibition of GRα. However, the underlying mechanism by which GRα inactivates the NF-κB pathway remains unclear. Future studies will investigate the mechanism by which GRα suppresses the activation of the NF-κB pathway in the progression of OSAHS.
In summary, the present study demonstrated that XIST decreased the expression of GRα, thereby contributing to the initiation and development of OSAHS through an NF-κB-dependent signaling pathway. This may provide a potential target for the treatment of OSAHS.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
Funding: The current study was supported by the Hangzhou Science and Technology Development Plan Project (grant nos. 20170533B94 and 20170533B27).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author's contributions
ZZ conceived and designed the experiments. ZZ, HN, YL and BJ performed the experiments. ZZ and HN analyzed the data. ZZ and HN can authenticate the raw data in this study. All authors agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The current study was approved by the Ethics Committee and Animal Care Committee of the Affiliated Hangzhou First People's Hospital, Zhejiang University School of Medicine (Hangzhou, China). Informed consent was obtained from all participants included in the current study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Zhang L, Ou X, Zhu T, Lv X. Beneficial effects of estrogens in obstructive sleep apnea hypopnea syndrome. Sleep Breath. 2020;24:7–13. doi: 10.1007/s11325-019-01896-2. [DOI] [PubMed] [Google Scholar]
- 2.Gonzaga C, Bertolami A, Bertolami M, Amodeo C, Calhoun D. Obstructive sleep apnea, hypertension and cardiovascular diseases. J Hum Hypertens. 2015;29:705–12. doi: 10.1038/jhh.2015.15. [DOI] [PubMed] [Google Scholar]
- 3.Jordan AS, McEvoy RD. Gender differences in sleep apnea: Epidemiology, clinical presentation and pathogenic mechanisms. Sleep Med Rev. 2003;7:377–389. doi: 10.1053/smrv.2002.0260. [DOI] [PubMed] [Google Scholar]
- 4.Morong S, Hermsen B, de Vries N. Sleep-disordered breathing in pregnancy: A review of the physiology and potential role for positional therapy. Sleep Breath. 2014;18:31–37. doi: 10.1007/s11325-013-0849-9. [DOI] [PubMed] [Google Scholar]
- 5.Snyder B, Cunningham RL. Sex differences in sleep apnea and comorbid neurodegenerative diseases. Steroids. 2018;133:28–33. doi: 10.1016/j.steroids.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans RM. The steroid and thyroid hormone receptor superfamily. Science. 1988;240:889–895. doi: 10.1126/science.3283939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ren R, Oakley RH, Cruz-Topete D, Cidlowski JA. Dual role for glucocorticoids in cardiomyocyte hypertrophy and apoptosis. Endocrinology. 2012;153:5346–5360. doi: 10.1210/en.2012-1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HK, Jeong YJ, Song IS, Noh YH, Seo KW, Kim M, Han J. Glucocorticoid receptor positively regulates transcription of FNDC5 in the liver. Sci Rep. 2017;7(43296) doi: 10.1038/srep43296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuo T, Chen TC, Yan S, Foo F, Ching C, McQueen A, Wang JC. Repression of glucocorticoid-stimulated angiopoietin-like 4 gene transcription by insulin. J Lipid Res. 2014;55:919–28. doi: 10.1194/jlr.M047860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen X, Li JR. Glucocorticoid receptor expression in the tonsils of children with obstructive sleep apnea hypopnea syndrome. Genet Mol Res. 2016;15 doi: 10.4238/gmr.15017361. [DOI] [PubMed] [Google Scholar]
- 11.Choi SW, Kim HW, Nam JW. The small peptide world in long noncoding RNAs. Brief Bioinform. 2019;20:1853–1864. doi: 10.1093/bib/bby055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barth DA, Slaby O, Klec C, Juracek J, Drula R, Calin GA, Pichler M. Current concepts of non-coding RNAs in the pathogenesis of non-clear cell renal cell carcinoma. Cancers (Basel) 2019;11(1580) doi: 10.3390/cancers11101580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rapicavoli NA, Qu K, Zhang J, Mikhail M, Laberge RM, Chang HY. A mammalian pseudogene lncRNA at the interface of inflammation and anti-inflammatory therapeutics. Elife. 2013;2(e00762) doi: 10.7554/eLife.00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carpenter S, Aiello D, Atianand MK, Ricci EP, Gandhi P, Hall LL, Byron M, Monks B, Henry-Bezy M, Lawrence JB, et al. A long noncoding RNA mediates both activation and repression of immune response genes. Science. 2013;341:789–792. doi: 10.1126/science.1240925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richardson AL, Wang ZC, De Nicolo A, Lu X, Brown M, Miron A, Liao X, Iglehart JD, Livingston DM, Ganesan S. X chromosomal abnormalities in basal-like human breast cancer. Cancer Cell. 2006;9:121–132. doi: 10.1016/j.ccr.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 16.McKiernan PJ, Molloy K, Cryan SA, McElvaney NG, Greene CM. Long noncoding RNA are aberrantly expressed in vivo in the cystic fibrosis bronchial epithelium. Int J Biochem Cell Biol. 2014;52:184–191. doi: 10.1016/j.biocel.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 17.Ma M, Pei Y, Wang X, Feng J, Zhang Y, Gao MQ. LncRNA XIST mediates bovine mammary epithelial cell inflammatory response via NF-kappaB/NLRP3 inflammasome pathway. Cell Prolif. 2019;52(e12525) doi: 10.1111/cpr.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sadeghi A, Rostamirad A, Seyyedebrahimi S, Meshkani R. Curcumin ameliorates palmitate-induced inflammation in skeletal muscle cells by regulating JNK/NF-kB pathway and ROS production. Inflammopharmacology. 2018;26:1265–1272. doi: 10.1007/s10787-018-0466-0. [DOI] [PubMed] [Google Scholar]
- 19.Nedjai B, Hitman GA, Church LD, Minden K, Whiteford ML, McKee S, Stjernberg S, Pettersson T, Ranki A, Hawkins PN, et al. Differential cytokine secretion results from p65 and c-Rel NF-κB subunit signaling in peripheral blood mononuclear cells of TNF receptor-associated periodic syndrome patients. Cell Immunol. 2011;268:55–59. doi: 10.1016/j.cellimm.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Ruland J. Return to homeostasis: Downregulation of NF-κB responses. Nature Immunol. 2011;12:709–714. doi: 10.1038/ni.2055. [DOI] [PubMed] [Google Scholar]
- 21.Lai JL, Liu YH, Liu C, Qi MP, Liu RN, Zhu XF, Zhou QG, Chen YY, Guo AZ, Hu CM. Indirubin inhibits LPS-induced inflammation via TLR4 abrogation mediated by the NF-κB and MAPK signaling pathways. Inflammation. 2017;40:1–12. doi: 10.1007/s10753-016-0447-7. [DOI] [PubMed] [Google Scholar]
- 22.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 23.Ye XH, Chen H, Yu Q, Zhu QL. Liver X receptor gene expression is enhanced in children with obstructive sleep apnea-hyperpnoea syndrome and cyclooxygenase-2 (COX-2) is correlated with severity of obstructive sleep apnea-hypopnea syndrome (OSAHS) Med Sci Monit. 2017;23:3261–3268. doi: 10.12659/msm.900947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo Z, Wang Y, Yang J, Zhong J, Liu X, Xu M. KAI1 overexpression promotes apoptosis and inhibits proliferation, cell cycle, migration, and invasion in nasopharyngeal carcinoma cells. Am J Otolaryngol. 2017;38:511–517. doi: 10.1016/j.amjoto.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Pathare AD, Deshpande AS. HGV-HCV/HBV co-infection in India: A pilot study. Asian J Transfus Sci. 2013;7:48–50. doi: 10.4103/0973-6247.106734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 27.Yu X, Wang D, Wang X, Sun S, Zhang Y, Wang S, Miao R, Xu X, Qu X. CXCL12/CXCR4 promotes inflammation-driven colorectal cancer progression through activation of RhoA signaling by sponging miR-133a-3p. J Exp Clin Cancer Res. 2019;38(32) doi: 10.1186/s13046-018-1014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burman D. Sleep disorders: Sleep-related breathing disorders. FP Essent. 2017;460:11–21. [PubMed] [Google Scholar]
- 29.Shenoda BB, Tian Y, Alexander GM, Aradillas-Lopez E, Schwartzman RJ, Ajit SK. miR-34a-mediated regulation of XIST in female cells under inflammation. J Pain Res. 2018;11:935–945. doi: 10.2147/JPR.S159458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu J, Yao L, Zhang M, Jiang J, Yang M, Wang Y. Downregulation of LncRNA-XIST inhibited development of non-small cell lung cancer by activating miR-335/SOD2/ROS signal pathway mediated pyroptotic cell death. Aging. 2019;11:7830–7846. doi: 10.18632/aging.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang J, Cai H, Dai Z, Wang G. Down-regulation of lncRNA XIST inhibits cell proliferation via regulating miR-744/RING1 axis in non-small cell lung cancer. Clin Sci (Lond) 2019;133:1567–1579. doi: 10.1042/CS20190519. [DOI] [PubMed] [Google Scholar]
- 32.Xing F, Liu Y, Wu SY, Wu K, Sharma S, Mo YY, Feng J, Sanders S, Jin G, Singh R, et al. Loss of XIST in breast cancer activates MSN-c-Met and reprograms microglia via exosomal miRNA to promote brain metastasis. Cancer Res. 2018;78:4316–4330. doi: 10.1158/0008-5472.CAN-18-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Song YX, Ou YM, Zhou JY. Gracillin inhibits apoptosis and inflammation induced by lipopolysaccharide (LPS) to alleviate cardiac injury in mice via improving miR-29a. Biochem Biophys Res Commun. 2020;523:580–587. doi: 10.1016/j.bbrc.2019.11.129. [DOI] [PubMed] [Google Scholar]
- 34.Fu Z, Liao W, Ma H, Wang Z, Jiang M, Feng X, Zhang W. Inhibition of neddylation plays protective role in lipopolysaccharide-induced kidney damage through CRL-mediated NF-kappaB pathways. Am J Transl Res. 2019;11:2830–2842. [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao Y, Li S, Xia N, Shi Y, Zhao CM. Effects of XIST/miR-137 axis on neuropathic pain by targeting TNFAIP1 in a rat model. J Cell Physiol. 2018;233:4307–4316. doi: 10.1002/jcp.26254. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y, Zhu Y, Gao G, Zhou Z. Knockdown XIST alleviates LPS-induced WI-38 cell apoptosis and inflammation injury via targeting miR-370-3p/TLR4 in acute pneumonia. Cell Biochem Funct. 2019;37:348–358. doi: 10.1002/cbf.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.