Abstract
Aim & objectives
Clinical trials had concluded a significant relationship between implant failure and bruxism. A three-dimensional (3D) finite element analysis (FEA) was done to evaluate the stress distribution in straight and angled abutments around titanium and carbon fiber-reinforced polyetheretherketone (CFR-PEEK) implant with 2 different prosthetic crowns under parafunctional loading.
Materials and method
Twelve 3D models of bone block were created representing the maxillary right premolar area with osseointegrated implants. The models were divided in two group; CFR-PEEK implant (n = 6) and group titanium implant (n = 6).Each group was subdivided based on implants with three different abutments (straight, 15°, 25° angled abutments) and having two different prosthetic crowns: porcelain fused to metal (PFM) and polyetheretherketone (PEEK). A vertical load of 1000 N was applied to the central fossa and an oblique load of 500 N (30°) was applied to the buccal incline of the palatal cusp. The von Mises stresses and principal stresses were analyzed using ANSYS software.
Results
CFR-PEEK and titanium implants produced similar stress in bone under vertical and oblique loading. Straight abutment showed better results than 15° and 25° angled abutments in all the groups. PEEK crown produced lesser stress than PFM crown under vertical and oblique loading.
Conclusion
The study concluded that straight abutment along with PEEK crown could be given in patients with bruxism to reduce the stress concentration in bone, thus preventing possible implant failure. Titanium and CFR-PEEK implants with straight abutments if given, then it should be provided with an occlusal splint.
1. Introduction
The outcome of dental implants in bruxism has been of great importance in recent literature. There are clinical trials that have concluded a significant relationship between implant failure and bruxism.1In a recent clinical study, where 98 bruxers were compared to a matched group, reported that there is a significant increase in implant failure rate and the rate of mechanical and technical complications in implant-supported prosthesis in patients with bruxism.2 The most common complications seen were occlusal surface wear, loosened screws or abutments and implant fractures.3
Due to the lack of periodontal ligament in dental implants, they are rigidly connected to bone. Thus, the proprioceptive feedback mechanism of masticatory muscles is absent which would lead to marginal bone loss.4 A more homogenous stress distribution in the supporting tissues could be generated if the material of implants had an elastic modulus similar to that of bone.5
Polyetheretherketone (PEEK) is a polyaromatic polymers with a high mechanical performance, with an elastic modulus of 3–5 GPa which is much lower than that of the bone (13.7 GPa). Carbon fibre-reinforced polyetheretherketone is a variant of PEEK with an elastic modulus of 18 GPa which is near to that of bone.6Researchers have suggested that titanium and CFR-PEEK implants produce similar stresses in bone.7 Thus, it can be used as a material of choice for implant and its suprastructures to reduce the stress concentration in bone.
Ideally, implants should be placed parallel to each other and adjacent teeth and be aligned vertically to axial forces. However, achieving this may not be possible owing to deficiencies in the ridge’s anatomy. In this situation, the use of angulated implants or abutments would be helpful.8Clelland et al. concluded in their study that stress distribution in lesser angled abutments was more favourable.9 Thus, straight abutments can be used in bruxism patients to prevent greater stress concentration when compared to angled abutments.
In a recent study, it was concluded that PEEK crowns produced lower stress in bone when compared to porcelain fused to metal (PFM) crown.10 Thus, to prevent implant failure; we need to use a crown that will further decrease the stress generation in bruxism patients.
The proposed study assessed the stress distribution in straight and angled abutments (15° and 25°) around titanium implant and CFR-PEEK implant with PFM crown and PEEK crown, under different parafunctional loading conditions. Stress distribution in the implants and restorative crowns was evaluated by using a three-dimensional (3D) finite element analysis (FEA) study. The null hypothesis was that there would be no difference in the stress distribution in titanium and CFR-PEEK material irrespective of different abutment and prosthetic crown materials.
2. Materials and methods
Twelve 3D models of bone block were created representing the maxillary right premolar area with osseointegrated implants with prosthetic crowns. The models were divided in two groups; CFR-PEEK implant group (n = 6) and titanium implant group (n = 6). Each group was subdivided based on implants with three different abutments (straight, 15°, 25° angled abutments) and having two different prosthetic crowns: porcelain fused to metal (PFM) and polyetheretherketone (PEEK).
2.1. Model generation
An edentulous maxilla of a human skull was scanned with a dental volumetric computed tomography device (HDI 100 series 3D Scanner with flex scan software). Using the scanned image, bone structure with a thickness of at least 20 mm for each axis present in the maxillary right premolar area was modeled. In the model a cortical bone thickness of 1.5 mm surrounding the cancellous bone was modeled in different colors.11
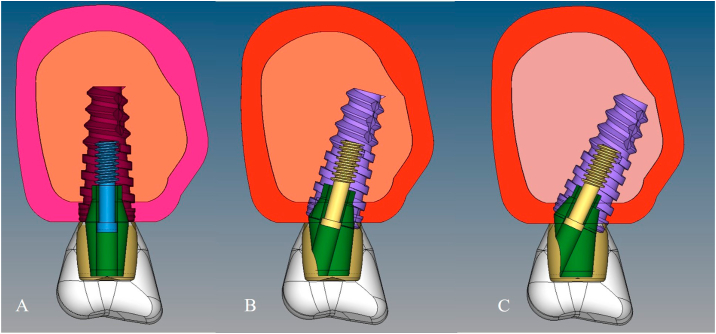
Titanium implants (4.2 mm diameter and 10 mm length; Adin-Touareg-S, Iberica dental implant system, Israel) with different titanium abutments (RS straight abutment, angled abutment 15°and angled abutment 25°; Adin, Iberica dental implant system, Israel) (Fig. 1a, b, 1c) and their inner screws were scanned with an optical scanner (HDI 100 series 3D Scanner with flex scan software). The standard tessellation language (STL) data of each component were transferred in to 3D modeling software (ANSYS software). On each model subsequently, the restorative crown was modeled on the abutment. In three titanium implant models with different abutments, PFM crown was modeled. Cobalt chromium coping of 0.5 mm thickness with porcelain thickness of 1 mm in the marginal area and 1.5 mm thick in the occlusal area of the functional cusp was modeled. In other three titanium implant model with different abutments, PEEK crown was modeled. A 0.5 mm thick PEEK coping layered with composite (1 mm thick in the marginal area and 1.5 mm thick in the occlusal area of the functional cusp) was modeled.12 In a similar manner, six CFR-PEEK implants with different abutments along with PFM and PEEK restorative crowns were also modeled with their respective properties.
Fig. 1.
Implant model generated of bone block with implant, abutment and crown, A, straight abutment, B, 15°abutment C, 25°abutment.
In all the twelve models, a dual-polymerized resin cement (Panavia F 2.0; Kuraray Medical Inc) layer 30 μm in thickness was defined between the abutment and crown to simulate clinical conditions.
2.2. Setting of materials properties
The Young’s modulus and Poisson ratio of each material were obtained from the manufacturer and published studies as shown in Table 1.11,13 The components in each model were presumed to be homogenous and isotropic. The boundary conditions were fixed at the alveolar bone level surrounding the implant surface.
Table 1.
Properties of the materials used in finite element analysis.
| Material | Young’s Modulus (GPa) | Poisson Ratio |
|---|---|---|
| Cortical bone | 13.7 | 0.30 |
| Cancellous bone | 1.37 | 0.30 |
| Titanium implant, abutment, screw | 110 | 0.35 |
| CFR-PEEK implant, abutment | 150 | 0.39 |
| Porcelain | 69 | 0.30 |
| PEEK | 4.1 | 0.40 |
| Composite | 10.7 | 0.30 |
| Dual core resin cement | 18.6 | 0.28 |
| Cobalt chromium (Co–Cr) | 218 | 0.33 |
2.3. Load and constraints
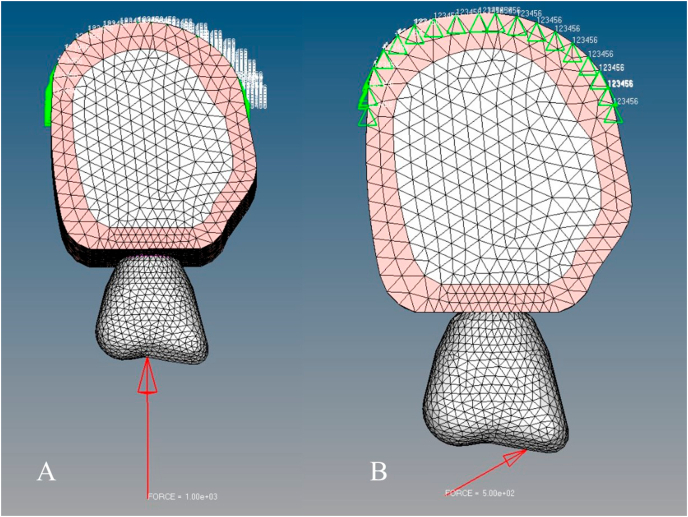
Parafunctional loading was simulated by applying axial & oblique loads. An axial load of 1000 N was applied on to the central fossa and an oblique load of 500 N (30°) was applied to the buccal incline of the palatal cusp (Fig. 2a and b).5 Distribution of stresses in implants and restorative crowns were detected by von Mises stress. Stress distribution around the bone was detected by principal stress analysis.
Fig. 2A.
Model showing vertical force applied on crown, B, Model showing oblique force applied on crown.
2.4. Meshing and contact characteristics
A discretization process with 10 nodes of tetrahedral elements was created for all the 3D models by using Hypermesh software. A total of 103,041 nodes and 72,771 elements were used for the straight abutment model, however, 102,646 nodes and 72,347 elements were used for the 15°abutment model. A total of 99,600 nodes and 70,141 elements were used for the 25°abutment model.
3. Results
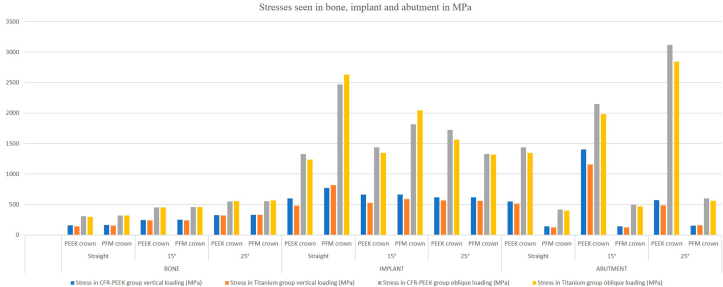
Using the finite element method, the calculations were performed as per the planned loading protocol. In each model, 1000 N of vertical load was applied to the central fossa and 500 N of oblique load (30°) was applied to the buccal incline of the palatal cusp. The stresses were calculated and noted within the bone, implant, abutment, cement layer and crown. The results found in bone, implant and abutments are mentioned in Table 2 and Fig. 3.
Table 2.
Stresses seen in bone, implant and abutment under vertical and oblique loading in MPa.
|
Components |
Abutment Angulation | Materials | Stress in CFR-PEEK group vertical loading (MPa) | Stress in Titanium group vertical loading (MPa) | Stress in CFR-PEEK group oblique loading (MPa) | Stress in Titanium group oblique loading (MPa) |
|---|---|---|---|---|---|---|
|
BONE |
Straight | PEEK crown | 157.343 | 144.205 | 307.892 | 296.215 |
| PFM crown | 165.168 | 153.539 | 320.223 | 318.839 | ||
| 15° | PEEK crown | 245.471 | 237.197 | 452.601 | 452.401 | |
| PFM crown | 249.095 | 242.054 | 457.664 | 459.297 | ||
| 25° | PEEK crown | 325.16 | 318.468 | 548.151 | 555.463 | |
| PFM crown | 333.395 | 331.885 | 552.27 | 565.862 | ||
|
IMPLANT |
Straight | PEEK crown | 601.051 | 479.283 | 1328 | 1240 |
| PFM crown | 772.52 | 818.582 | 2471 | 2632.09 | ||
| 15° | PEEK crown | 662.746 | 528.913 | 1438 | 1345 | |
| PFM crown | 662.045 | 590.811 | 1814 | 2046 | ||
| 25° | PEEK crown | 617.165 | 564.945 | 1724 | 1564 | |
| PFM crown | 616.537 | 559.116 | 1329 | 1316 | ||
|
ABUTMENT |
Straight | PEEK crown | 546.694 | 514.667 | 1436 | 1347 |
| PFM crown | 142.653 | 123.681 | 417.226 | 400.875 | ||
| 15° | PEEK crown | 1406 | 1156 | 2148 | 1980 | |
| PFM crown | 140.186 | 124.594 | 497.84 | 468.784 | ||
| 25° | PEEK crown | 570.349 | 486.189 | 3116 | 2841 | |
| PFM crown | 155.132 | 162.213 | 601.619 | 562.213 |
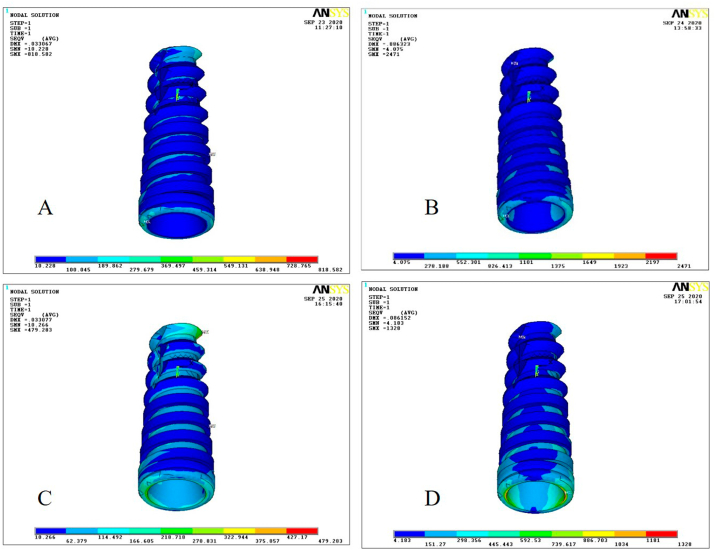
Fig. 3.
Stress seen in bone, implant and abutments under vertical and oblique loading.
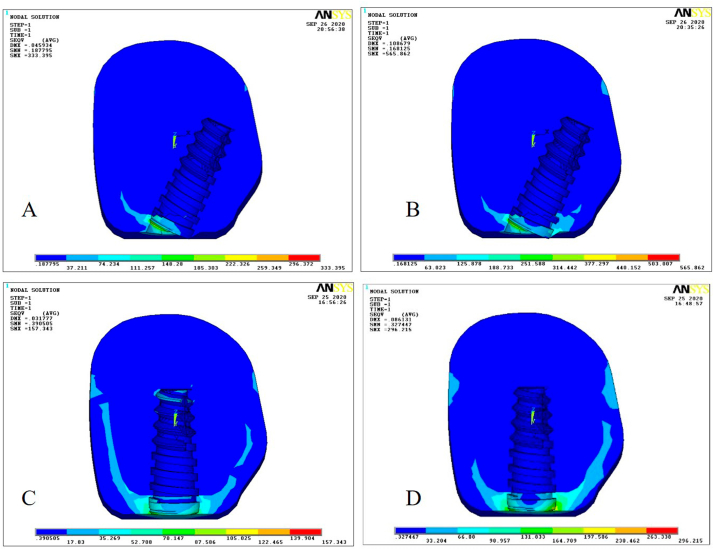
Under vertical and oblique loading, in both CFR-PEEK group and titanium group, the stress generation in bone was seen higher in 25° angled abutment with PFM crown (Fig. 4A and B) than 15° and straight abutment groups. The stress was seen lowest in straight abutment with PEEK crown in both CFR-PEEK and titanium group in both vertical and oblique loading (Fig. 4C and D). The stress concentration within the bone in all the groups, in both vertical and oblique loading, was seen at the crestal region near the implant abutment connection area.
Fig. 4.
A, Stress in bone for CFR-PEEK implant under vertical loading with 25° abutment and PFM crown, B, Stress in bone for titanium implant under oblique loading with 25° abutment and PFM crown, C, Stress in bone for CFR-PEEK implant under vertical loading with straight abutment and PEEK crown, D, Stress in bone for titanium implant under oblique loading with straight abutment and PEEK crown.
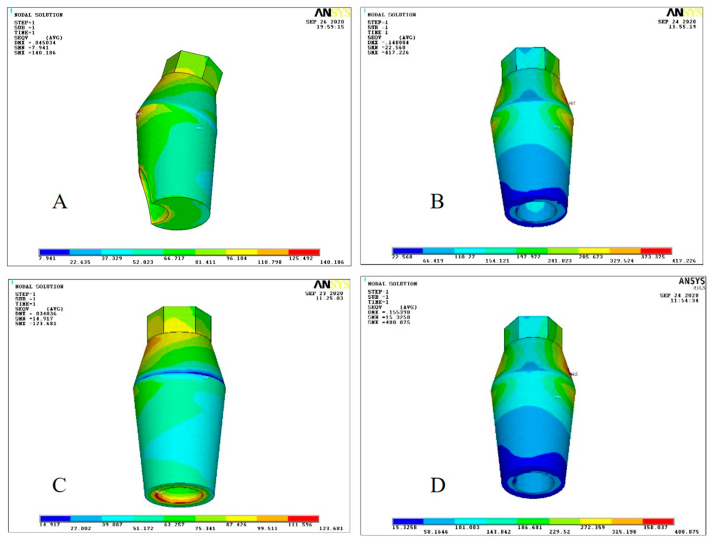
The stress generation within implant was seen highest in straight abutment group in both CFR-PEEK and titanium group with PFM crown in both vertical and oblique loading (Fig. 5A and B). However, the least stress was seen in straight abutment with PEEK crown in both groups under vertical and oblique loading (Fig. 5C and D). In both vertical and oblique loading, CFR-PEEK implant and titanium implant with PFM crown showed stress concentration at the neck of implant and at the apex region of the implant.
Fig. 5.
A, Stress in titanium implant under vertical loadingwith straight abutment and PFM crown, B, Stress in CFR-PEEK implant under oblique loading with straight abutment and PFM crown, C, Stress in titanium implant under vertical loading with straight abutment and PEEK crown, D, Stress in CFR-PEEK implant under oblique loading with straight abutment and PEEK crown.
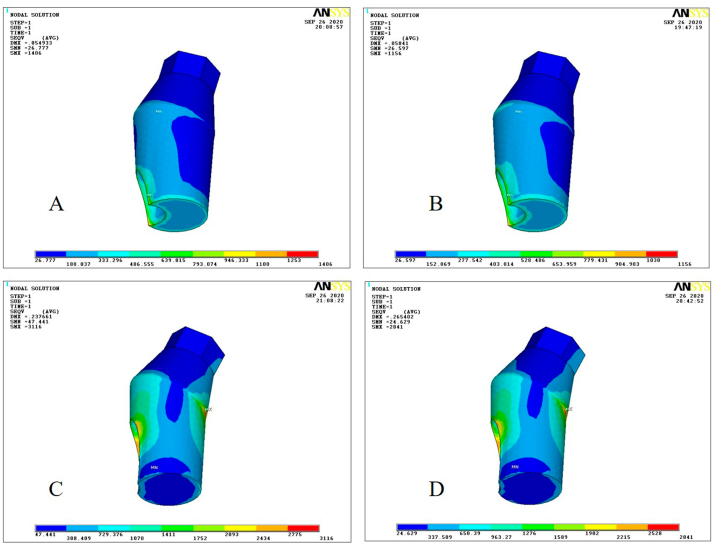
In case of abutments, in the CFR-PEEK group under vertical loading, least stress was seen in 15° abutment with PFM crown while under oblique loading straight abutment with PFM crown showed least stress concentration (Fig. 6A and B). In titanium group, straight abutment with PFM crown showed least stress under both vertical and oblique (Fig. 6C and D) loading. The highest stress was seen in 15° abutment with PEEK crown in both CFR-PEEK and titanium groups under vertical loading (Fig. 7A and B). Under oblique loading, in both CFR-PEEK and titanium groups, 25° abutment with PEEK crown showed the highest stress concentration (Fig. 7C and D). In vertical loading, CFR-PEEK and titanium abutment with PFM crown showed more stress concentration towards the implant-abutment connection area and neck area. In oblique loading, CFR-PEEK and titanium abutment with PFM crown showed more stress concentration towards the implant-abutment connection area.
Fig. 6.
A, Stress in CFR-PEEK 15° abutment under vertical loading with PFM crown, B, Stress in CFR-PEEK straight abutment under oblique loading with PFM crown, C, Stress in titanium straight abutment under vertical loading with PFM crown. D, Stress in titanium straight abutment under oblique loading with PFM crown.
Fig. 7.
A, Stress in CFR-PEEK 15° abutment under vertical loading with PEEK crown, B, Stress in titanium 15° abutment under vertical loading with PEEK crown, C, StressinCFR-PEEK 25°abutment under oblique loading with PEEK crown, D, Stress in titanium 25°abutment under oblique loading with PEEK crown.
In the cement layer, least stress was seen in 25° abutment with PFM crown in both CFR-PEEK and titanium group under vertical loading, however, under oblique loading, the least stress was seen in straight abutment with PFM crown in both the groups. The highest stresses were seen in 15° abutment with PEEK crown under vertical loading while under oblique loading the highest stress was seen in 25° abutment with PEEK crown in both the groups. Vertical loading of CFR-PEEK and titanium abutment with PFM crown showed stress concentration towards occlusal aspect in cement layer. Oblique loading of CFR-PEEK and titanium abutment with PFM crown showed stress concentration towards the neck area in the cement layer.
The von Mises stress in crowns cemented to CFR-PEEK and titanium groups were almost similar in both vertical and oblique loading. Under vertical loading, stresses seem to be more concentrated in the central fossa region of the PEEK/PFM crown cemented to CFR-PEEK and titanium abutment. Under oblique loading, stresses seem to be more concentrated in buccal inclines of palatal cusp of PEEK/PFM crown cemented to CFR-PEEK and titanium abutment.
4. Discussion
In this study, we assessed the effect of parafunctional forces on implants, bone and supra-structures using FEA. The study aimed to assess the stress distribution with straight abutments and angled abutments around titanium implant and CFR-PEEK implant with PFM crown and PEEK crown, under different parafunctional loading conditions.The null hypothesis that there would be no difference in the stress distribution in titanium and CFR-PEEK material irrespective of different abutments and prosthetic crown materials was rejected.
Bruxism is characterized by grinding with or without clenching of the teeth. It is a nocturnal or diurnal parafunctional habit of the masticatory system occurring during sleep or while awake.14 The effect of prolonged parafunctional habits can give rise to temporomandibular joint disorder, abrasion on teeth, loss of periodontal support, failure of restorations on natural teeth and stresses on dental implants.14,15 In parafunctional loading excessive occlusal load on dental implants and their supra-structures causes bone loss around the implants and may leads to implant failure. Along with various factors, bruxism is also considered as one of the important factor for the failure of implant.15
There was a mixed opinion for implant placement in bruxism patients. Lindquist et al., in a 15-year prospective study concluded that clenching was not significantly associated with marginal bone loss and did not lead to problems with suprastructures.16 Several other studies contradicted the conclusion of Lindquist et al., as they reported a significant correlation between bruxism and dental implant or their suprastructures. Brägger et al. reported technical problems with implants in 60% of bruxist patients over 5 years, as compared with about 20% in their non-bruxist patients.17 Wannfors et al. concluded the existence of a significant relationship between implants and bruxism in their one-year prospective study.18
Similarly, Glauser et al. observed a higher percentage of implant loss in bruxists than in non-bruxists (41% versus 12%, after 1 year).19 Interestingly, Lindquist et al., in their further studies concluded that clenching does contribute significantly to marginal bone loss over a 6-year period.20 The available evidences do confirm the correlation between bruxism and implant failure.
Radaelli et al. found in their study that parafunctional loading increases stress levels in bone as well as implant and their substructures when compared to functional loading.4 Ayranci et al. compared the stresses in dental implants under heavy bruxing forces, using 3D FEA. They concluded that vertical forces produced the least stresses on implants and higher stresses were seen in the neck region of an implant under parafunctional loading.14 In our study, although similar result was found under vertical and oblique loading, in both CFR-PEEK group and titanium group but still the stress generated was less in bone with different abutments with PEEK crown in both CFR-PEEK and titanium group compared to PFM crown. The increased stresses in oblique loading could be due to the rigid connection between the implant and the bone. Oblique loads have been reported to increase stress values in peripheral bone and prosthetic components.11,21
Omori et al., in their systematic review, concluded that significantly more marginal bone loss was seen in implants supporting angled abutments than those supporting straight abutments.22 Cavallaro and Greenstein concluded that increased abutment angulations result in the placement of a greater amount of stress on prostheses and the surrounding bone than that associated with straight abutments.8 In concurrence with these studies, it was seen that straight abutments showed lesser stresses than angled abutments, within bone in both CFR-PEEK and titanium groups. Although stresses generated in bone were more in angled abutment but still the stress generated was less in angled abutments with PEEK crown when compared to PFM crown.
Several researchers had evaluated the effect of using different prosthetic materials on stress distribution in implants and peripheral bone structure and have reported that the change in prosthesis materials has only a minor effect on the stress patterns.23, 24, 25Bassit et al., demonstrated that using different occlusal surface materials does not produce different stresses in implants.26 To the contrary, in the present study, under parafunctional loading, it was observed that there was a difference in stress distribution using different prosthetic materials. In the present study, the least stresses were generated by the PEEK crown in bone and maximum stresses were taken up by the implant and abutment.
Flexible material such as composite resin reduces the stress concentration in the adhesive surface when it is used for the fabrication of prosthesis. In the present study, as composite layering was done on the PEEK crown, it was found that the stress distribution was better with PEEK crown compare to PFM crown. The result obtained is due to the direct proportional tendency between the elastic modulus of the restorative material and the stress concentration between restoration/cement and cement/tooth or implant.27
This study suggest that PEEK crown with composite layering could be given along with preventive measures such as night guards to reduce unwanted stresses generated in bruxism patients with implant prosthesis.28 The elastic modulus of the PEEK material is similar to that of bone and helps in inhibiting high stress peaks during load transfer at the bone-implant interface, and creates a stress shielding effect.29
There were certain limitations to the study such as the properties were considered to be homogenous and isotropic. The application of the loadings was a simplification of the actual clinical condition. The complexity of living organisms and internal biological phenomena is impossible to fully and precisely duplicate with individual-level specificity using a computer. Further study should be done in clinical conditions to better understand the parafunctional loading and its effect on implant and suprastructures.
5. Conclusion
Within the limitations of the present study following conclusion were drawn:
-
•
Stress generated in bone with straight abutment was less compared to 15° and 25° abutment placed over titanium and CFR-PEEK implants.
-
•
Stresses generated in bone in model with PEEK crown layered with composite was lesser when compared to PFM crown.
-
•
Titanium and CFR-PEEK implants with angled abutments generated more stresses under parafunctional loading and had a detrimental effect on bone and should be avoided.
-
•
Titanium and CFR-PEEK implants with straight abutments if given, then they should be provided with an occlusal splint.
Thus, the study concluded that when implants are placed in bruxism patients, a PEEK crown along with straight abutments could be given to reduce the stress generation in bone and to prevent possible implant failure.
Grant or other financial support
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Not applicable.
Declaration of competing interest
None.
Acknowledgment
We would like to thank Mr. Vijay Bhanu Thodeti, CADD Solutions, Andhra Pradesh, India, for carrying out the Finite Element Analysis.
References
- 1.Chrcanovic B.R., Kisch J., Albrektsson T., Wennerberg A. Bruxism and dental implant failures: a multilevel mixed effects parametric survival analysis approach. J Oral Rehabil. 2016;43(11):813–823. doi: 10.1111/joor.12431. [DOI] [PubMed] [Google Scholar]
- 2.Chrcanovic B.R., Kisch J., Albrektsson T., Wennerberg A. Bruxism and dental implant treatment complications: a retrospective comparative study of 98 bruxer patients and a matched group. Clin Oral Implants Res. 2017;28(7):e1–9. doi: 10.1111/clr.12844. [DOI] [PubMed] [Google Scholar]
- 3.Chrcanovic B.R., Albrektsson T., Wennerberg A. Bruxism and dental implants: a meta-analysis. Implant Dent. 2015;24(5):505–516. doi: 10.1097/ID.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 4.Radaelli M.T., Idogava H.T., Spazzin A.O., Noritomi P.Y., Boscato N. Parafunctional loading and occlusal device on stress distribution around implants: a 3D finite element analysis. J Prosthet Dent. 2018;120(4):565–572. doi: 10.1016/j.prosdent.2017.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Sheets C.G., Earthmann J.C. Natural intrusion and reversal in implant assisted prosthesis; evidence of and a hypothesis for the occurrence. J Prosthet Dent. 1993;70:513–520. doi: 10.1016/0022-3913(93)90265-p. [DOI] [PubMed] [Google Scholar]
- 6.Skinner H.B. Composite technology for total hip arthroplasty. Clin Orthop Relat Res. 1988;235:224–236. [PubMed] [Google Scholar]
- 7.Sarot J.R., Contar C.M., Cruz A.C., de Souza Magini R. Evaluation of stress distribution in CFR-PEEK dental implants by the three dimensional finite element method. J Mater Sci Mater Med. 2010;21:2079–2085. doi: 10.1007/s10856-010-4084-7. [DOI] [PubMed] [Google Scholar]
- 8.Cavallaro J., Jr., Greenstein G. Angled implant abutments: a practical application of available knowledge. J Am Dent Assoc. 2011;142(2):150–158. doi: 10.14219/jada.archive.2011.0057. [DOI] [PubMed] [Google Scholar]
- 9.Clelland N.L., Gilat A. The effect of abutment angulation on stress transfer for an implant. J Prosthet Dent. 1992;1(1):24–28. doi: 10.1111/j.1532-849x.1992.tb00422.x. [DOI] [PubMed] [Google Scholar]
- 10.Nahar R., Mishra S.K., Chowdhary R. Evaluation of stress distribution in an endodontically treated tooth restored with four different post systems and two different crowns-finite element analysis. J Oral Biol Craniofac Res. 2020;10(4):719–726. doi: 10.1016/j.jobcr.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaleli N., Sarac D., Külünk S., Öztürk Ö. Effect of different restorative crown and customized abutment materials on stress distribution in single implants and peripheral bone: a three-dimensional finite element analysis study. J Prosthet Dent. 2018;119(3):437–445. doi: 10.1016/j.prosdent.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Rosenstiel S.F., Land M.F., Fujimoto J. vol. 4. 2015. Contemporary Fixed Prosthodontics. St. Louis. [Google Scholar]
- 13.Tekin S., Değer Y., Demirci F. Evaluation of the use of PEEK material in implant-supported fixed restorations by finite element analysis. Niger J Clin Pract. 2019;22(9):1252. doi: 10.4103/njcp.njcp_144_19. [DOI] [PubMed] [Google Scholar]
- 14.Ayranci F., Sivrikaya E.C., Omezli M.M. Is bone density or implant design more important in implant stress formation in patients with bruxism? Biotechnol Biotechnol Equip. 2017;31(6):1221–1225. [Google Scholar]
- 15.Lobbezoo F., Brouwers J.E., Cune M.S., Naeije M. Dental implants in patients with bruxing habits. J Oral Rehabil. 2006;33(2):152–159. doi: 10.1111/j.1365-2842.2006.01542.x. [DOI] [PubMed] [Google Scholar]
- 16.Lindquist L.W., Carlsson G.E., Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clin Oral Implants Res. 1996;7:329–336. doi: 10.1034/j.1600-0501.1996.070405.x. [DOI] [PubMed] [Google Scholar]
- 17.Brägger U., Aeschlimann S., Bürgin W., Hämmerle C.H., Lang N.P. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res. 2001;12(1):26–34. doi: 10.1034/j.1600-0501.2001.012001026.x. [DOI] [PubMed] [Google Scholar]
- 18.Wannfors K., Johansson B., Hallman M., Strandkvist T. A prospective randomized study of 1- and 2-stage sinus inlay bone grafts: 1-year follow-up. Int J Oral Maxillofac Implants. 2000;15:625–632. [PubMed] [Google Scholar]
- 19.Glauser R., Ree A., Lundgren A., Gottlow J., Hammerle C.H., Scharer P. Immediate occlusal loading of Brånemark implants applied in various jawbone regions: a prospective, 1 year clinical study. Clin Implant Dent Relat Res. 2001;3(4):204–213. doi: 10.1111/j.1708-8208.2001.tb00142.x. [DOI] [PubMed] [Google Scholar]
- 20.Lindquist L.W., Rockler B., Carlsson G.E. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J Prosthet Dent. 1988;59:59–66. doi: 10.1016/0022-3913(88)90109-6. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi J.M.F.K., Dayrell A.C., Consani R.L.X., de ArrudaNobilo M.A., Henriques G.E.P., Mesquita M.F. Stress evaluation of implant-abutment connections under different loading conditions: a 3D finite element study. J Oral Implantol. 2015;41:133–137. doi: 10.1563/AAID-JOI-D-11-00205. [DOI] [PubMed] [Google Scholar]
- 22.Omori Y., Lang N.P., Botticelli D., Papageorgiou S.N., Baba S. Biological and mechanical complications of angulated abutments connected to fixed dental prostheses: a systematic review with meta-analysis. J Oral Rehabil. 2020;47(1):101–111. doi: 10.1111/joor.12877. [DOI] [PubMed] [Google Scholar]
- 23.Stegaroiu R., Kusakari H., Nishiyama S., Miyakawa O. Influence of prosthesis material on stress distribution in bone and implant: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 1998;13:781–790. [PubMed] [Google Scholar]
- 24.Wang T.M., Leu L.J., Wang J.S., Lin L.D. Effects of prosthesis materials and prosthesis splinting on peri-implant bone stress around implants in poor quality bone: a numeric analysis. Int J Oral Maxillofac Implants. 2002;17:231–237. [PubMed] [Google Scholar]
- 25.Sertgöz A. Finite element analysis study of the effect of superstructure material on stress distribution in an implant-supported fixed prosthesis. Int J Prosthodont (IJP) 1997;10:19–27. [PubMed] [Google Scholar]
- 26.Bassit R., Lindsrom H., Rangerty B. In-vivo registration of force development with ceramic and acrylic resin occlusal materials on implant-supported prosthesis. Int J Oral Maxillofac Implants. 2002;55:34–38. [PubMed] [Google Scholar]
- 27.Tribst J.P., Dal Piva A.M., de Melo R.M., Borges A.L., Bottino M.A., Özcan M. Influence of restorative material and cement on the stress distribution of posterior resin-bonded fixed dental prostheses: 3D finite element analysis. J Mech Behav Biomed Mater. 2019;96:279–284. doi: 10.1016/j.jmbbm.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Perel M.L. Parafunctional habits, nightguards, and root form implants. Implant Dent. 1994;3:261–263. doi: 10.1097/00008505-199412000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Schwitalla A.D., Emara M.A., Spintig T., Lackmann J., Müller W.D. Finite element analysis of the biomechanical effects of PEEK dental implants on the peri-implant bone. J Biomech. 2015;48:1–7. doi: 10.1016/j.jbiomech.2014.11.017. [DOI] [PubMed] [Google Scholar]