Abstract
Background and purpose
Cardiovascular diseases and dementia are two major diseases in the elderly. Atherosclerosis is associated with future vascular events and cognitive impairment. The PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events (PRECISE) study is a population-based prospective cohort study with comprehensive evaluation of multiterritorial artery stenosis and plaque using advanced vascular imaging techniques and prospective collection of vascular events and cognitive assessments.
Methods
Between May 2017 and September 2019, the PRECISE study enrolled 3067 community-dwelling adults with ages between 50 and 75 years cluster sampled from six villages and four communities of Lishui city in China. Data are collected in face-to-face interviews at baseline, 2-year and 4-year follow-up visits. Brain MRI including high-resolution sequences for intracranial and carotidal arteries and CT angiography for thoracoabdominal arteries were performed at baseline and will be rescanned after 4 years. Cardiovascular/cerebrovascular events and cognitive assessment will be prospectively collected after the enrollment. Blood and urine samples were collected and biomarkers were tested at baseline.
Results
A total of 3067 subjects were enrolled, among which 53.5% were female with an average age of 61.2±6.7 years. Among them, 2.8%, 8.1%, 43.1% and 21.6% had a history of stroke, coronary heart diseases, hypertension and diabetes mellitus, respectively.
Conclusions
The PRECISE study is a population-based prospective cohort study with comprehensive evaluation of atherosclerotic stenosis and plaque using advanced vascular imaging techniques. Data from this cohort provide us an opportunity to precisely evaluate polyvascular atherosclerosis and its association with future vascular events and cognitive impairment.
Trial registration number
ClinicalTrials.gov Registry (NCT03178448).
Keywords: stroke, plaque, MRI, atherosclerosis
Introduction
Cardiovascular diseases and dementia are two major diseases and causes of mortality and disability in the elderly.1 2 Globally, there were an estimated 422.7 million cases of cardiovascular diseases and 17.92 million cardiovascular disease-related deaths, mainly ischaemic heart disease and stroke.3 The global number of people living with dementia more than doubled in the recent three decades and reached approximately 50 million in 2018.4 5 Recent studies showed that cardiovascular risk factors and unfavourable lifestyle were associated with cognitive decline and dementia,6 7 and incident coronary heart disease and stroke were associated with accelerated cognitive decline after the event.8 9 It is suggested to research and prevent cardiovascular diseases and dementia simultaneously.10
Atherosclerosis is the most common vascular disorder and accounts for the greatest number of cardiovascular events.11 Polyvascular atherosclerosis with coexistent lesions in multiple arterial territories, could be associated with higher risk of future cardiovascular/cerebrovascular diseases.12 13 By contrast, the association between atherosclerosis and future cognitive decline has not been well established. Furthermore, previous studies either roughly defined polyvascular diseases according to established clinically recognised arterial diseases in multiple arterial territories,12 or tested multiterritorial subclinical atherosclerosis without tests of intracranial and peripheral arteries.11 Previous studies showed a high prevalence (31%) of intracranial atherosclerotic stenosis in the elderly14 and 12% of patients had progression of artery stenosis after 2 years.15 Compared with Caucasian population, people in Asia might have higher prevalence of intracranial atherosclerosis which contributes to most cases of ischaemic stroke in Asian population.16 However, there are limited data about the prevalence and progression of intracranial atherosclerosis in Chinese population. Comprehensive evaluation of multiterritorial lesions in the whole body (both intracranial and extracranial) using advanced vascular imaging techniques is required to precisely assess the prevalence of polyvascular lesions and its association with future cardiovascular/cerebrovascular events and cognitive impairment.
The PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events (PRECISE) study is a population-based prospective cohort study with comprehensive evaluation of intracranial and extracranial artery stenosis and plaque using advanced vascular imaging techniques and longitudinal collection of cardiovascular/cerebrovascular events and cognitive impairment. In this report, we look at the rationale, study design, baseline data, as well as the strengths and potential limitations of the PRECISE study.
Methods
Overview of the PRECISE study
The PRECISE study is a population-based prospective cohort study in community-dwelling older adults living in Lishui city, Zhejiang province, southeast of China. The PRECISE study was designed to establish the prevalence of clinical or subclinical polyvascular lesions, 4-year progression rate of plaque in intracranial and carotidal arteries in community-dwelling older adults, and the association between polyvascular lesions and future risk of cognitive impairment, cardiovascular/cerebrovascular events and death. A steering committee consisting of members from both Beijing Tiantan Hospital and Lishui Hospital was established to design and organise the study. This population-based study will have both a cross-sectional and a longitudinal design. Individuals with complete baseline exams will enter into the prospective cohort and will be followed up for 4 years.
Study objectives
The primary objectives of the PRECISE study were to assess the prevalence of clinical or subclinical polyvascular lesions and 4-year progression rate of plaque in intracranial and carotidal arteries in an established cohort of community-dwelling older adults in China using vascular imaging techniques; to investigate both traditional and emerging genetic, metabolomic and environmental risk factors related to the existing intracranial and carotidal plaque and their progression; and to investigate the association between polyvascular lesions and future risk of cognitive impairment, cardiovascular/cerebrovascular events and death.
Study population
The target population of the PRECISE study is community-dwelling adults aged 50–75 years based on cluster sampling from six villages and four communities of Lishui city in southeast of China. The steering committee attempted to ensure population representativeness of the sample. These selected villages and communities are living communities (not occupational communities) with stable population with little population migration. They have well-established collaboration with Lishui Hospital in disease prevention and good administrative support for the study.
Exclusion criteria of this study included subjects with contraindications to magnetic resonance imaging (MRI) (eg, artificial tooth, implantable automatic defibrillator or any implanted metal device) and to computed tomography angiography (CTA) contraindication (eg, allergy to iodine contrast, thyroid disease and renal impairment or dysfunction), life expectancy ≤4 years due to advanced cancers and other diseases, and mental diseases. All eligible subjects with written informed consents were enrolled in the PRECISE study.
Baseline interviews and data collection
All the data collection was performed at Lishui Hospital through face-to-face interviews and examinations by centralised trained personnel following a standard data collection protocol that was developed by the steering committee (table 1). All interviewers were trained before the kick-off meeting. An electronic data capture system (EDC) was developed and used for data collection. All data elements from each participant were automatically checked for completeness, correct coding, value range and logical error through EDC. Independent data monitoring was also performed through EDC by an independent contract research organisation. All data were de-identified before data analysis.
Table 1.
Components of the PRECISE study
| Characteristics | Baseline (May 2017–September 2019) |
2-year follow-up (May 2019–September 2021) |
4-year follow-up (May 2021–September 2023) |
| Written informed consent | X | ||
| Demographics and socioeconomic status | X | ||
| Medical history | X | ||
| Family history | X | ||
| Diet and lifestyle assessment | X | ||
| Physical examination | X | ||
| ECG | X | ||
| Echocardiography | X | ||
| Fundus fluorescein photography | X | ||
| Ankle brachial index | X | ||
| Medications | X | X | X |
| Blood and urine sample | X | X | X |
| CTA scanning | X | X | |
| MRI scanning | X | X | X |
| Cognitive assessment | X | X | X |
| Vascular events | X | X |
CTA, CT angiography; PRECISE, PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events.
Demographics and vascular risk factors
Baseline demographics and vascular risk factors were collected through face-to-face interviews by trained research coordinators. Baseline data included demographics, socioeconomic status, medical history, family history, diet, physical activity, lifestyle, smoking and drinking status, and medication use.
Medical examinations
Medical examinations were performed for each participant through face-to-face interviews by trained investigators (physicians of corresponding department). Body mass index, blood pressure and pulse were collected. The blood pressure was measured with the participant in a seated position after 5 min of rest using an automated sphygmomanometer (OMRON Model HEM-7071, Omron Co.). Measurements were taken three times consecutively on the non-dominant arm, with a 1-minute interval between measurements for each participant. Blood pressure was recorded as the average of the second and third measurements. Hypertension was defined as either self-reported hypertension previously diagnosed by a physician or current use of antihypertensive agents or systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.17
Furthermore, heart function was examined using 12-lead electrocardiography and colour Doppler echocardiography. Retinal vessel was assessed using fundus fluorescein photography (retinal photography) and ankle-brachial index was assessed using Doppler ultrasound.
Blood and urine sample collection
Fasting blood and morning urine samples are collected in face-to-face interviews at baseline, 2-year and 4-year follow-up visits. Several biomarkers were tested using the blood and urine samples, including blood routine examination, hypersensitive C reactive protein, free fatty acid, haemoglobin A1c, renal function tests, liver function tests, a complete lipid profile, serum myocardial enzymogram, blood electrolytes, urine routine examination and microalbuminuria. The standard oral glucose tolerance test was also performed at baseline in subjects without previously diagnosed diabetes, and fasting and 2-hour postload glucose, insulin and C-peptide levels were measured. Diabetes was defined as a self-reported diabetes previously diagnosed by a physician or current use of antidiabetic agents or fasting plasma glucose ≥7.0 mmol/L or 2-hour postload glucose ≥11.1 mmol/L or haemoglobin A1c≥6.5%.18
In addition, fasting blood samples and morning urine were collected and sent to the laboratory. The blood samples were centrifuged to obtain serum, plasma and extract white blood cells. All blood and urine samples were frozen in a −80°C freezer and then transported through cold chain to the central laboratory at Beijing Tiantan Hospital, where all specimens were stored at −80°C. The sample will be used for further assessment of biomarkers and genetic studies.
Imaging data collection
Structural and functional brain MRI including three-dimensional T1-weighted magnetization-prepared rapid-acquisition gradient-echo (3D T1w MPRAGE), two-dimensional T2-weighted (2D T2w), two-dimensional fluid-attenuated inversion recovery (2D FLAIR), diffusion-weighted imaging (DWI), susceptibility-weighted imaging (SWI), three-dimensional time-of-flight magnetic resonance angiography (3D-TOF MRA), resting-state fMRI and diffusion tensor imaging (DTI), is performed at baseline, 2-year and 4-year follow-up. Vascular MRI for intracranial and carotidal arteries is performed at baseline and 4-year follow-up. Vascular MRI includes 3D isotropic high-resolution black-blood T1w vessel wall imaging and Simultaneous Non-contrast Angiography and intraPlaque haemorrhage imaging. Thoracoabdominal CTA for coronary, aorta, renal, hepatic, pancreatic and iliofemoral arteries is performed both at baseline and 4-year follow-up. MRI scans are performed on a 3.0T scanner (Ingenia 3.0T, Philips, Best, The Netherlands). CTA scans are performed on a dual-source CT scanner (SOMATOM Force, Siemens Healthineers, Forchheim, Germany). All the MRI and CTA scans will be conducted on a designated machine by trained investigators based on a standardised protocol. These imaging techniques enable early detection of intracranial and extracranial vascular lesions, characterisation of the atherosclerotic composition and burden, monitoring of plaque progression in intracranial and carotidal arteries, and assessment of brain function. Imaging data are collected in digital imaging and communications in medicine (DICOM) format on discs and analysed by the imaging research centre at Beijing Tiantan Hospital. Polyvascular atherosclerotic plaques are defined as at least two affected sites in coronary, intracranial, carotidal, aorta, iliofemoral arteries or lower extremity arteries.11
Cognitive assessment
Cognitive assessment is performed through face-to-face interview by trained investigators (neurologists) at each visit. The training was conducted at Beijing Tiantan Hospital to minimise rater to rater variation. Montreal Cognitive Assessment (MoCA) was used for baseline cognitive assessment. At 2-year and 4-year follow-up visits, standard clinical and neuropsychological testing batteries will be performed, including MoCA, Mini-Mental State Exam scores, Geriatric Depression Scale, Digit Span, Rey Auditory Verbal Learning Test, Rey-Osterrieth Complex Figure Test, Trail Making A and B, Stroop Task, Verbal Fluency Test, Boston Naming Test, Clock Drawing Test, Symbol Digit Modalities Test, Neuropsychiatric Inventory and Clinical Dementia Rating. These tests have been validated in Chinese population with different education levels.19–24
Follow-up assessment
Field personnel will be in frequent contact with the study population to determine whether they develop any cardiovascular/cerebrovascular events or cognitive decline. All participants will be followed up through face-to-face interviews by trained investigators at 2 years and 4 years. Information of vascular risk factors and medication use, any death, cardiovascular/cerebrovascular events, systemic embolism and intravascular procedures during the follow-up periods will be queried at each follow-up visit. For suspected individuals with vascular events, medical documents from the admitting hospital will be collected and diagnosis made by hospital of level II or above will be confirmed. Suspected vascular events without hospitalisation will be judged by an independent endpoint judgement committee. Death will either be confirmed on a death certificate from the admitting hospital or from the local citizen registry.
As aforementioned, fasting blood and morning urine samples will be collected in face-to-face interviews at each follow-up visit following the same protocol as that at baseline. Structural and functional brain MRI scans and cognitive assessment will be performed at 2-year and 4-year follow-up visits. Vascular MRI scans for intracranial and carotidal arteries and CTA scans for thoracoabdominal arteries will be performed at 4-year follow-up visit. All MRI and CTA scans will be conducted on the same machine as that conducted at baseline by trained investigators based on a standardised protocol.
Outcomes measurements
Time to first composite vascular event, including any new event of non-fatal stroke (ischaemic or haemorrhagic), non-fatal myocardial infarction or cardiovascular death (including fatal stroke, fatal myocardial infarction and other cardiovascular death).
Time to first broadly defined composite vascular event, including any new event of non-fatal stroke, non-fatal myocardial infarction, cardiovascular death, vascular interventions (bypass graft, angioplasty, stent and amputation for ischaemia), or hospitalisations for vascular events (including unstable angina pectoris, transient ischaemic attack and other ischaemic arterial event including worsening of peripheral vascular disease).
Time to first individual aforementioned cardiovascular/cerebrovascular events.
4-year progression rate of atherosclerotic plaque in intracranial and carotidal arteries.
Time to first death of any cause.
Cognitive impairment at 2 years and 4 years.
Statistical analysis plan
According to previous studies, approximately 30% of participants may have polyvascular atherosclerotic plaques and it was associated with an increased risk of composite vascular event with a HR of 1.99,11 13 and 6% subjects may develop a composite vascular event after 4 years.13 25 With 3067 subjects and a probability of type I error of 5%, we have 98% statistical power to detect a HR of 2.0, and 79% power to detect a HR of 1.6 for polyvascular atherosclerotic plaques on composite vascular event, assuming an attrition rate of 10%. A previous study showed that approximately 30% subjects may have intracranial or carotidal atherosclerotic plaques11 14 and approximately 24% subjects may have progression of plaque after 4 years.15 With the 920 subjects with atherosclerotic plaques at baseline and a probability of type I error of 5%, we have 89% power to detect an OR of 1.7, and 80% power to detect an OR of 1.6 for a risk factor on progression of plaque, assuming 30% of subjects have the risk factor and an attrition rate of 10%.
At each follow-up, a participant will be considered as a dropout if the subject clearly refused to continue the study or cannot be reached after three phone contact attempts on three different days. Proportions will be used to describe the categorical variables, means with SD or median with the IQR will be used for continuous variables. In univariable analyses, t-test or Mann-Whitney test will be used to compare continuous variables, whereas χ2 test or fisher’s exact test will be used to compare the categorical variables. Kaplan-Meier plots of time-to-event outcomes of composite vascular events will be presented. The associations of polyvascular lesions and abovementioned risk factors with time to first vascular events and death will be performed by univariable and multivariable Cox proportional hazard regression model or competing risk analysis. HRs with their 95% CIs will be evaluated. Multivariable logistic regression analyses will be used to examine the association of risk factors and progression of atherosclerotic plaque and ORs with their 95% CIs will be evaluated. Global cognitive scores and standardised domain-specific scores for memory, language, visuospatial, attention and executive function domains will be calculated with adjustment for educational level. Generalised linear models or generalised mixed longitudinal models will be performed for the relationship between vascular risk factors and outcome of global or domain-specific cognitive impairment or cognitive decline. A two-sided p value<0.05 was considered to be statistically significant.
In this article, the analyses focused on the baseline characteristics of the enrolled participants. Proportions were used to describe the categorical variables, means with SD or median with the IQR were used for continuous variables. All analyses were conducted with SAS V.9.4.
Results
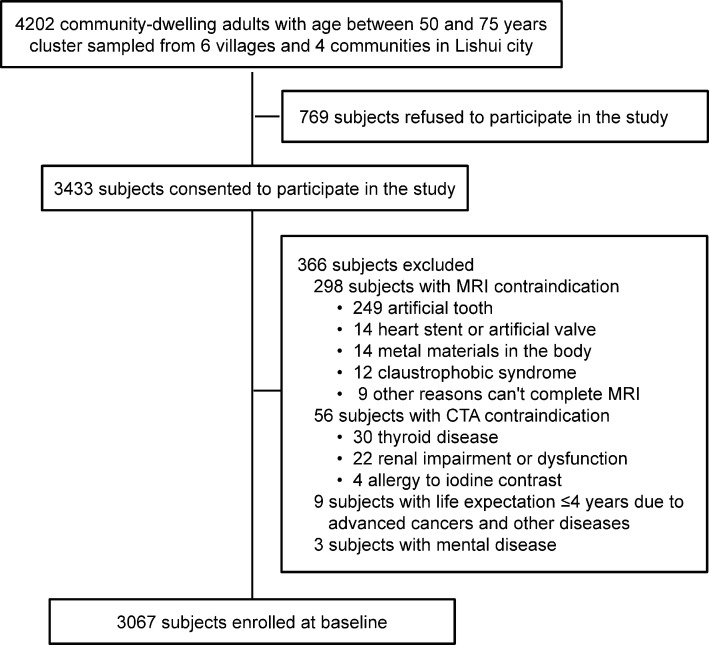
The baseline survey has been completed. We initially screened 4202 community-dwelling adults with ages between 50 and 75 years cluster sampled from six villages and four communities of Lishui city. There were 3433 subjects who consented to participate in the study. After exclusion of 298 subjects with MRI contraindication, 56 subjects with CTA contraindication, 9 subjects with life expectation ≤4 years and 3 subjects with mental disease, a total of 3067 subjects were eligible and enrolled at baseline between May 2017 and September 2019. The detailed participant enrollment flow chart is shown in figure 1. Subjects included in the study had similar sex and age distribution as those excluded (table 2).
Figure 1.
Flow chart of participant enrollment in the PRECISE study. CTA, CT angiography; PRECISE, PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events.
Table 2.
Characteristics of included and excluded subjects for the PRECISE study
| Characteristics | Included (N=3067) | Excluded (N=1135) | P value |
| Sex | |||
| Male, n (%) | 1427 (46.5) | 536 (47.2) | 0.69 |
| Female, n (%) | 1640 (53.5) | 599 (52.8) | |
| Age (years) | |||
| Mean±SD | 61.2±6.7 | 61.1±6.5 | 0.62 |
N, denominator; n, numerator; PRECISE, PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events.
Baseline characteristics of the participants are presented in table 3. Overall, 1640 (53.5%) subjects were female with the average age of 61.2±6.7 years. Among the 3067 participants, 96.9% of them were of Han ethnicity, 55.6% had education level of middle school or above, 20.5% and 18.7% were current smokers and current drinkers, respectively. Among them, 2.8%, 8.1%, 43.1% and 21.6% had a history of stroke, coronary heart diseases, hypertension and diabetes mellitus, respectively.
Table 3.
Baseline characteristics of the participants in the PRECISE study (n=3067)
| Characteristics | |
| Age (years), mean±SD | 61.2±6.7 |
| Female, n (%) | 1640 (53.5) |
| Han ethnicity, n (%) | 2973 (96.9) |
| Education, n (%) | |
| Illiteracy | 561 (18.3) |
| Elementary school | 802 (26.1) |
| Middle school | 932 (30.4) |
| High school | 581 (18.9) |
| University or above | 191 (6.2) |
| Current smoker, n (%) | 629 (20.5) |
| Current drinker, n (%) | 574 (18.7) |
| Medical history, n (%) | |
| Stroke | 87 (2.8) |
| Coronary heart diseases | 249 (8.1) |
| Hypertension | 1321 (43.1) |
| Diabetes mellitus | 663 (21.6) |
| Hypercholesterolemia | 616 (20.1) |
| Systolic blood pressure, mm Hg, median (IQR) | 128.5 (118–139) |
| Diastolic blood pressure, mm Hg, median (IQR) | 75(69–81) |
| Fasting plasma glucose, mmol/L, median (IQR) | 5.6 (5.2–6.1) |
| TC, mmol/L, median (IQR) | 5.2 (4.6–5.9) |
| TG, mmol/L, median (IQR) | 1.5 (1.0–2.1) |
| HDL-C, mmol/L, median (IQR) | 1.3 (1.1–1.6) |
| LDL-C, mmol/L, median (IQR) | 2.7 (2.3–3.3) |
| MoCA score, median (IQR) | 23(20-26) |
HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; MoCA, Montreal Cognitive Assessment; PRECISE, PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events; TC, total cholesterol; TG, triglyceride.
We compared participant characteristics in the PRECISE study with the nationwide data for demographics and major medical histories (table 4). Participants in the PRECISE study had similar sex and age distribution with national sampling survey data from China Statistical Yearbook.26 Participants in the PRECISE study also had similar prevalence of stroke, diabetes mellitus and hypertension as those data from nationwide population-based surveys.17 18 27
Table 4.
Comparison of participant characteristics in the PRECISE study and nationwide data
| Characteristics | PRECISE | Nationwide | Sources of nationwide data |
| Female, n (%) | 53.5 | 50.0 | China Statistical Yearbook 201826: national sampling survey data for subjects of 50–74 years in 2017. |
| Age (years), n (%) | |||
| 50–54 | 22.1 | 31.3 | |
| 55–59 | 24.3 | 19.4 | |
| 60–64 | 23.0 | 22.0 | |
| 65–69 | 18.7 | 16.7 | |
| 70–74 | 11.9 | 10.6 | |
| Medical history, n (%) | |||
| Stroke | 2.8 | 3.5 | Wang et al. Nationwide population-based stroke survey in 2013 (N=179 527; 50–79 years)27 |
| Diabetes mellitus | 21.6 | 20.2 | Wang et al. Nationwide population-based diabetes survey in 2013 (N=49 542;≥60 years)18 |
| Hypertension | 43.1 | 42.0 | Wang et al. China Hypertension Survey in 2012–2015 (N=197 609; 45–74 years)17 |
PRECISE, PolyvasculaR Evaluation for Cognitive Impairment and vaScular Events.
Discussion
The PRECISE study enrolled 3067 community-dwelling adults with an age between 50 and 75 years with comprehensive evaluation of intracranial and extracranial artery stenosis and plaque using advanced vascular imaging techniques. These imaging techniques enable early detection of intracranial and extracranial arterial lesions and characterisation of the atherosclerotic burden. Particularly, high-resolution vascular MRI scans for intracranial and carotidal arteries performed both at baseline and after 4 years enable quantitative measurements of lumen size and degree of stenosis, wall and/or plaque thickness, area and volume, and the composition and stability of the plaque.28 With comprehensive evaluation of whole artery stenosis and plaque, and together with cardiometabolic and genetic markers, the PRECISE study is expected to provide precise prediction of future cardiovascular/cerebrovascular diseases and cognitive impairment.
Another strength of the PRECISE study was the population representativeness of the participants. Based on cluster sampling from living communities (not occupational communities), participants in the PRECISE study have similar demographics and medical histories as data from surveys of a nationwide sample. The population representativeness of participants enables the study to estimate the prevalence of clinical or subclinical polyvascular lesions and generalisability of the findings from this study to general population.
There were several limitations in this study. First, despite representative as a whole, potential selection bias was unavoidable in this study since the study population was selected from a rural community region. Individuals with contraindication of MRI and CTA scanning, especially those with metal materials in the body and renal impairment or dysfunction, were excluded from enrollment. Second, only MoCA was performed for baseline cognitive assessment which was restricted by education of the participant. The education level of participants in this study is relatively low; however, this reflects the real-life situation of the elderly population in China. Additionally, longitudinal progression of MoCA score between baseline and follow-up will be much valuable.
In conclusion, the PRECISE study is a population-based prospective cohort study in community-dwelling older adults with comprehensive evaluation of atherosclerotic stenosis and plaque using advanced vascular imaging techniques and longitudinal collection of vascular events and cognitive impairment. Data from the PRECISE study will provide precise evaluation of polyvascular atherosclerosis and its association with future cardiovascular/cerebrovascular events and cognitive impairment.
Footnotes
YP, JJ and XC contributed equally.
Contributors: YoW and TW had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: YP, JinJ, XC, JS, JL, ZZ, ShiL, WZ, TW and YoW. Supplying participants: SW, CZ, JiaJ, LL, LM and ShaL. Drafting of the manuscript: YP, JinJ, TW and YoW. Critical revision of the manuscript for important intellectual content: YiW, JS and JL. Statistical analysis: YP and HL. Study supervision and organisation of the project: YiW, XM, TW and YoW.
Funding: This study was supported by grants from Ministry of Science and Technology of the People’s Republic of China (2017YFC1310902, 2018YFC1311706, 2016YFC0901002, 2017YFC1310901, 2017YFC1307905 and 2018YFC1312801), Beijing Hospitals Authority Youth Programme (QML20190501), National Natural Science Foundation of China (81971091), Beijing Science and Technology Plan/Brain Science and Research North Science Center Project (Z181100001518005), The Strategic Priority Research Program of the Chinese Academy of Sciences (XDB39000000), Lishui Science & Technology Bureau (2019ZDYF18) and grants from AstraZeneca Investment (China) Co., Ltd (CSA2017KY007).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The protocol of the PRECISE study was approved by ethics committee at Beijing Tiantan Hospital (IRB approval number: KY2017-010-01) and ethics committee at Lishui Hospital (IRB approval number: 2016-42). All participants provided written informed consents before entering the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Data are available to researchers on request for purposes of reproducing the results or replicating the procedure by directly contacting the corresponding author.
References
- 1. Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2016 Neurology Collaborators . Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019;18:459–80. 10.1016/S1474-4422(18)30499-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. 10.1016/j.jacc.2017.04.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. GBD 2016 Dementia Collaborators . Global, regional, and national burden of Alzheimer's disease and other dementias, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019;18:88–106. 10.1016/S1474-4422(18)30403-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alzheimer's Disease International . World Alzheimer report 2018. The state of the art of dementia research: new frontiers. Available: https://www.alz.co.uk/research/world-report-2018 [Accessed 18 May 2019].
- 6. Tosto G, Bird TD, Bennett DA, et al. The role of cardiovascular risk factors and stroke in familial Alzheimer disease. JAMA Neurol 2016;73:1231–7. 10.1001/jamaneurol.2016.2539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lourida I, Hannon E, Littlejohns TJ, et al. Association of lifestyle and genetic risk with incidence of dementia. JAMA 2019;322:430–7. 10.1001/jama.2019.9879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Levine DA, Galecki AT, Langa KM, et al. Trajectory of cognitive decline after incident stroke. JAMA 2015;314:41–51. 10.1001/jama.2015.6968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Xie W, Zheng F, Yan L, et al. Cognitive decline before and after incident coronary events. J Am Coll Cardiol 2019;73:3041–50. 10.1016/j.jacc.2019.04.019 [DOI] [PubMed] [Google Scholar]
- 10. Hachinski V, Einhäupl K, Ganten D, et al. Preventing dementia by preventing stroke: the Berlin manifesto. Alzheimers Dement 2019;15:961–84. 10.1016/j.jalz.2019.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fernández-Friera L, Peñalvo JL, Fernández-Ortiz A, et al. Prevalence, vascular distribution, and Multiterritorial extent of subclinical atherosclerosis in a middle-aged cohort: the PESA (progression of early subclinical atherosclerosis) study. Circulation 2015;131:2104–13. 10.1161/CIRCULATIONAHA.114.014310 [DOI] [PubMed] [Google Scholar]
- 12. Steg PG, Bhatt DL, Wilson PWF, et al. One-Year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007;297:1197–206. 10.1001/jama.297.11.1197 [DOI] [PubMed] [Google Scholar]
- 13. Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA 2010;304:1350–7. 10.1001/jama.2010.1322 [DOI] [PubMed] [Google Scholar]
- 14. Suri MFK, Qiao Y, Ma X, et al. Prevalence of intracranial atherosclerotic stenosis using high-resolution magnetic resonance angiography in the general population: the Atherosclerosis risk in Communities study. Stroke 2016;47:1187–93. 10.1161/STROKEAHA.115.011292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mizukami H, Shimizu T, Maki F, et al. Progression of intracranial major artery stenosis is associated with baseline carotid and intracranial atherosclerosis. J Atheroscler Thromb 2015;22:183–90. 10.5551/jat.26054 [DOI] [PubMed] [Google Scholar]
- 16. Wang Y, Zhao X, Liu L, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese intracranial atherosclerosis (CICAS) study. Stroke 2014;45:663–9. 10.1161/STROKEAHA.113.003508 [DOI] [PubMed] [Google Scholar]
- 17. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation 2018;137:2344–56. 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 18. Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 2017;317:2515–23. 10.1001/jama.2017.7596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lu J, Li D, Li F, et al. Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. J Geriatr Psychiatry Neurol 2011;24:184–90. 10.1177/0891988711422528 [DOI] [PubMed] [Google Scholar]
- 20. Yu J, Li J, Huang X. The Beijing version of the Montreal cognitive assessment as a brief screening tool for mild cognitive impairment: a community-based study. BMC Psychiatry 2012;12:156. 10.1186/1471-244X-12-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li H, Jia J, Yang Z. Mini-Mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis 2016;53:487–96. 10.3233/JAD-160119 [DOI] [PubMed] [Google Scholar]
- 22. Wang T, Xiao S, Li X, et al. Reliability and validity of the Chinese version of the neuropsychiatric inventory in mainland China. Int J Geriatr Psychiatry 2012;27:539–44. 10.1002/gps.2757 [DOI] [PubMed] [Google Scholar]
- 23. Chan AC. Clinical validation of the geriatric depression scale (GDS): Chinese version. J Aging Health 1996;8:238–53. 10.1177/089826439600800205 [DOI] [PubMed] [Google Scholar]
- 24. Chen Y, Lv C, Li X, et al. The positive impacts of early-life education on cognition, leisure activity, and brain structure in healthy aging. Aging 2019;11:4923–42. 10.18632/aging.102088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Song Y, Wu S, Liu X, et al. Association of systolic blood pressure levels with cardiovascular and cerebrovascular events and all-cause mortality: a result from the Kailuan study. Blood Press Monit 2016;21:149–54. 10.1097/MBP.0000000000000181 [DOI] [PubMed] [Google Scholar]
- 26. National Bureau of Statistics of China . China statistical Yearbook 2018. Beijing: China Statistics Press, 2018. [Google Scholar]
- 27. Wang W, Jiang B, Sun H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017;135:759–71. 10.1161/CIRCULATIONAHA.116.025250 [DOI] [PubMed] [Google Scholar]
- 28. Qiao Y, Guallar E, Suri FK, et al. Mr imaging measures of intracranial atherosclerosis in a population-based study. Radiology 2016;280:860–8. 10.1148/radiol.2016151124 [DOI] [PMC free article] [PubMed] [Google Scholar]