Abstract
Background:
Determining whether a patient has a time critical medical condition requiring Helicopter Emergency Medical Services (HEMS) transportation is a challenge in acute ischemic stroke (AIS). Although HEMS is largely accepted as improving outcomes in time-sensitive conditions, overtriage of patients ineligible for acute stroke therapies places patients and providers at unnecessary risk and wastes limited healthcare resources.
Objectives:
We sought to identify how accurate our triage system was at identifying high yield EMS transfers. A better triage system would decrease the volume of low flight value HEMS transfers.
Methods:
We conducted a retrospective study over a one-year period. Low flight value was defined by acute therapy eligibility and presenting medical status.
Results:
Of the 141 AIS patients transferred by HEMS, 23 (16%) were deemed of low flight value; 14 (61%) were outside the acute treatment time windows for either IV tPA or Endovascular Therapy (EVT); 5(22%) were ineligible for EVT (NIHSS<6); 2 (9%) were ineligible for EVT (mRS≥3); and 2 (9%) were flown despite negative angiographic studies performed at transferring institution. 13 (57%) of the patients were interfacility transfers as opposed to direct HEMS transport from the field.
Conclusion:
HEMS transport for AIS patients plays a crucial role in delivering the best evidence-based care. However, a significant percent of patients did not meet criteria for its optimal utilization, most commonly due to expired treatment windows. Furthermore, low flight value transfers were initiated in spite of physician evaluation over 50% of the time. These results represent a unique opportunity to coordinate education and build effective triage paradigms across a system of stroke care.
Keywords: Aeromedical transport, stroke, thrombolytics, pre-hospital, triage
Introduction
Air medical transport can expedite care in time-sensitive medical situations and is a widely accepted means of transport for conditions such as trauma, stroke, and other critical illnesses. However, the benefits of this transport modality must be weighed against the risks to patients and healthcare providers, as well as the significant costs to the healthcare system and society. Overuse of air transport for trauma patients has been documented and judicious selection of patients has been recommended1. Determining whether a patient has a time critical medical condition requiring Helicopter Emergency Medical Services (HEMS) transportation is a challenge in acute ischemic stroke (AIS). Suboptimal triage of patients when they are ineligible for acute stroke therapies places patients and providers at unnecessary risk and consumes limited, costly healthcare resources. Moreover, an overtriage or acceptable miss rate for acute ischemic stroke has not been defined in the literature 2. There are many factors to be considered in the initial treatment and disposition of potential AIS patients. These variables include differentiating stroke and stroke mimics and eligibility for IV alteplase or endovascular therapy (EVT). In addition to driving immediate treatment decisions, these factors also determine transfer facility and transport modality. The recent evolution of stroke care has extended the treatment window to 24 hours for both EVT and IV alteplase. Patients are selected based on advanced imaging not widely available rather than elapsed time alone. This paradigm shift further increases the burden on first-contact providers who comprise our stroke systems of care 3, 4.
A recent narrative review likened HEMS in stroke to the “black box” for acute stroke care and research. The decision process to transfer a patient from the field to a particular center or from one facility to another is complex and the data available regarding this process is limited 5. Data-driven improvements in pre-hospital care are challenged by a lack of centralized EMS-run metrics and standardized triage for suspected stroke patients. This year, the AHA published a policy statement on stroke systems of care acknowledging the shortcomings of field triage and hospital bypass. In regards to the mode of transport itself, HEMS vs. ground guidance was conspicuously absent6.
As the tertiary flagship institution and only comprehensive stroke center (CSC) in a rural state, we sought to identify how accurate our triage system was at identifying ischemic stroke patients appropriate for HEMS. In this challenging rural environment, the majority of our residents live over 60 minutes from an intravenous tissue plasminogen activator (IV-tPA)-capable facility7. However, our state is one of the few states nationwide with state-mandated EMS protocols, a robust rural ED partnership with the academic emergency medical center at our university, and a maturing statewide Telestroke network 8. All of these factors set the stage for an evidence-based pragmatic approach to triage and transfer acute ischemic stroke patients throughout the region.
Materials and Methods
We identified all stroke alerts arriving to our facility via HEMS during May 2017-August 2018. Utilizing ICD-10 codes, we stratified those with a discharge diagnosis of cerebrovascular ischemia. To assess the value added by air medical support, a retrospective review of the data available to the transferring providers was conducted. This study was approved by the local Institutional Review Board (IRB).
All cases were reviewed for the following variables: patient demographics, medical comorbidities, distance traveled, medical status at presentation including expiration within first 24 hours of admission, stroke subtype (ischemic, hemorrhagic, non-stroke, TIA), admission National Institute of Health Stroke Scale (NIHSS), acute stroke therapy (IV tPA and/or EVT) and reasons not received, if appropriate.
A low flight value HEMS transfer among AIS patients was defined if a patient fulfilled ≤ 1 of the following criteria:
Outside treatment windows (over 4 hours last known normal (LKN) for IV tPA and over 20 hours LKN for EVT, factoring in time to travel and receive intervention)
Lack of large vessel occlusion on vascular imaging prior to transfer
Clinical EVT criteria not met (NIHSS<6 or poor baseline functional status as defined by a Modified Rankin Scale (mRS) > 2)
Lack of other medical indication for HEMS (vitally unstable, concurrent trauma, intubated, actively seizing)
Results
During the study time period, there were 1116 stroke alerts in our emergency department. Among these, 288 HEMS transfers (25.8%) for suspected stroke syndrome were identified. Nearly half (49% or 141/288) of transfers had a discharge diagnosis of AIS; 4.8% (14/288) were hemorrhagic strokes; 6.9% (20/288) were TIA and 39% (113/288) had discharge diagnoses unrelated to cerebrovascular disease. 47% (135/288) were female, average age was 66 (range 16–96 years old), average NIHSS was 10 (range 0–38) average distance traveled was 62 road miles (range 15–367).
Of the 141 AIS HEMS transfers, 23 (16%) met definition to be of low flight value; 14 (61%) were outside the acute treatment time windows for either IV tPA or EVT; 5(22%) were ineligible for EVT (NIHSS<6); 2 (9%) were ineligible for EVT (mRS >2); and 2 (9%) were flown despite negative angiographic studies performed at the transferring facility (these patients were not tPA candidates). 13 (57%) of the patients were interfacility transfers where the decision to arrange HEMS occurred following physician evaluation.
113 or 39.2% (113/288) suspected stroke syndrome patients transferred via HEMS ultimately represented patients without a cerebrovascular discharge diagnosis. Excluding those who died within hours of arrival (2), 57% or 63/111 had a hospital length of stay (LOS) of ≤ 2 days, with 36% or 40/113 admitted for less than 1 day. 47% (53/113) were interfacility transfers as opposed to direct HEMS transports from the field.
Discussion
HEMS patients are more likely to have received thrombolytics or specialized care 9 and as a result, HEMS has been endorsed by the air medical community as the most appropriate method to transport acute stroke patients between hospitals. However, this recommendation must be weighed against the cost and potential risks to patients and medical personnel. Furthermore, the fact that this subset of AIS patients are more likely to have received more aggressive interventions does not sufficiently demonstrate that HEMS transport is justified.
In the era of thrombectomy and extended treatment windows, AIS management is evolving and decisions are increasingly complex for transferring providers. Although HEMS is most commonly used in inter-facility transport 10, it may also be employed directly from the field where the importance of adequate triage is even more impactful. This is especially true for the approximately 20% of Americans who develop a stroke far from a certified stroke center 7. As of this year, our statewide EMS system has adopted a large vessel occlusion (LVO) screen (FASTED/JOIN Triage) available as a customizable smartphone application (app). This identifies patients likely to have an LVO who are potentially eligible for EVT11. We have customized the app for our state to include additional data points that will assist in determining eligibility for EVT from first contact with the patient.
To optimize HEMS resources, it is essential we use data to design an evidence-based approach for transfer and attempt to define a clinically meaningful over-triage rate. Our study demonstrated a relatively low proportion (16%) of all HEMS stroke alerts with definitive diagnoses of AIS classified as of low flight value, however; these flights still represent a significant estimated cost to the healthcare system. At an average cost of $30,000/flight, an estimated $690,000 in total was required to provide a stroke safety net for our system.
This figure, however, only accounts for the 141 AIS HEMS recorded for the year, representing 49% of our institution’s HEMS stroke transfers overall. Excluding the other cerebrovascular disease cases (TIA and hemorrhagic stroke), a significant percentage (39%) of HEMS transfers for acute stroke syndrome were actually activated in patients lacking a cerebrovascular diagnosis at discharge. Among these, over half (57%) remained in the hospital 2 days of less, implying low acuity patients unlikely to benefit from air medical support. The reason(s) for HEMS in this subgroup should be further studied.
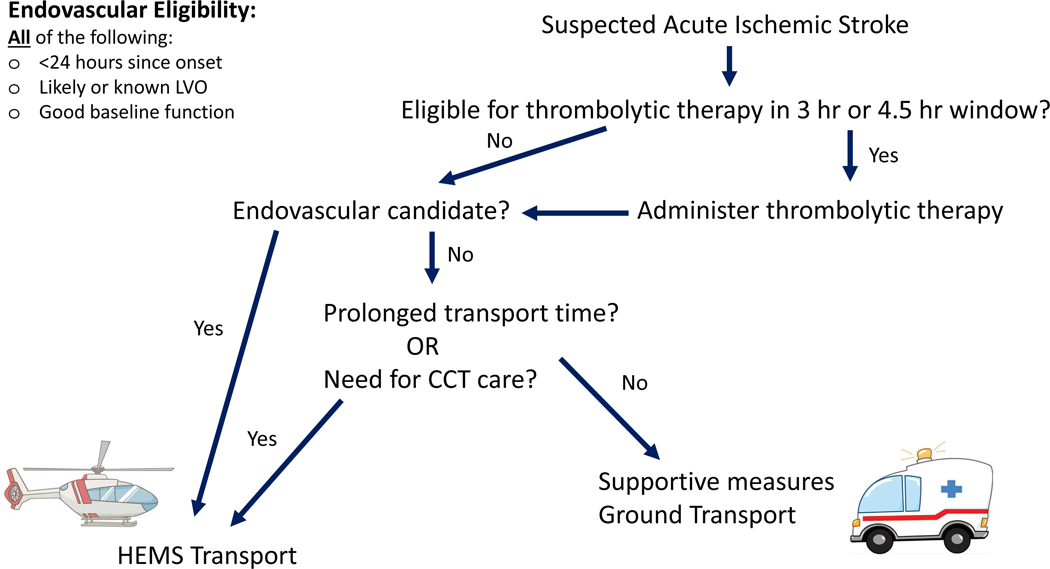
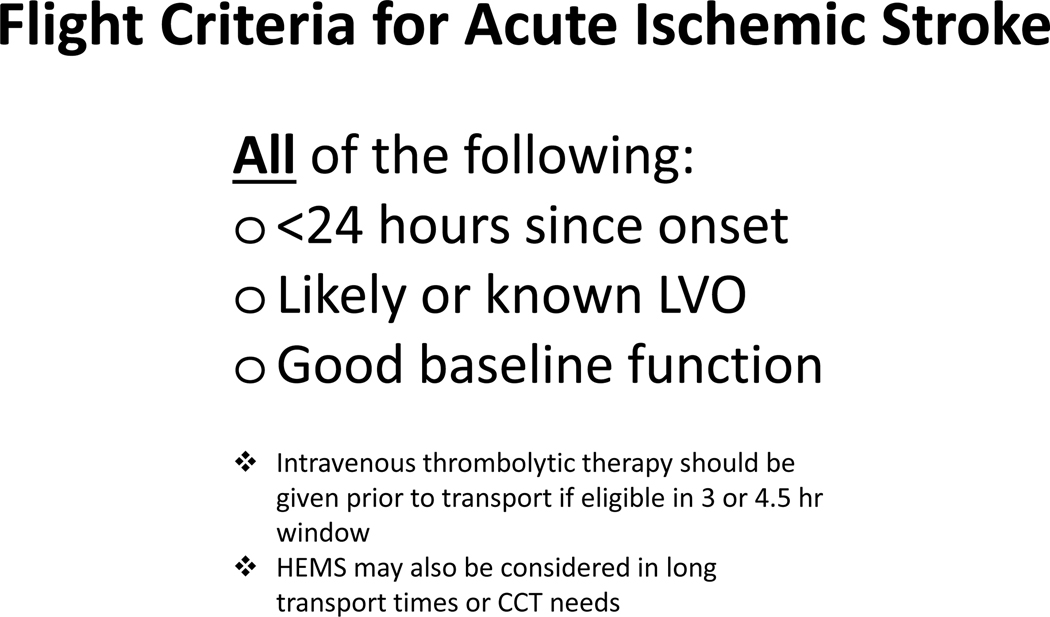
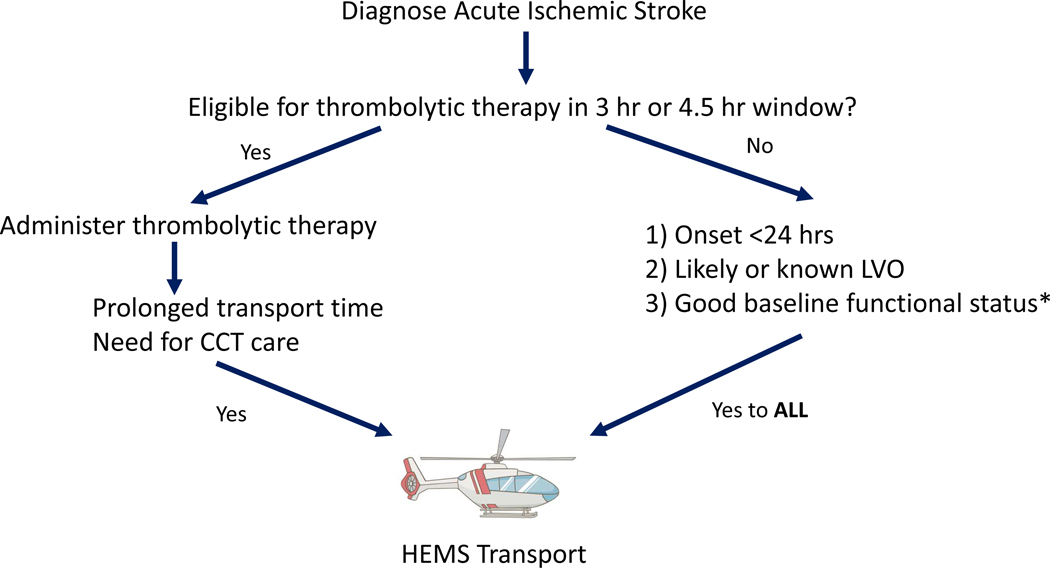
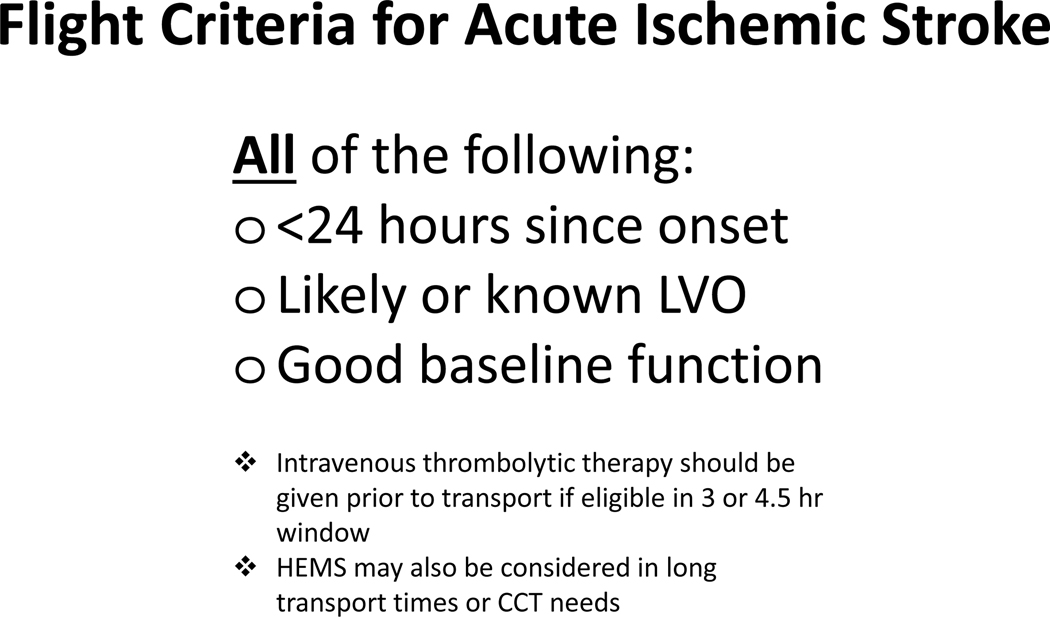
In addition, the decision to transfer a patient via HEMS in both the group with diagnoses unrelated to cerebrovascular disease and in the cases deemed to be of low flight value was made by a physician around half the time (47% and 57%, respectively), highlighting an opportunity for improvement. System-based changes such as wider adoption of CTA in local hospitals, automated advanced radiology interpretation employing artificial intelligence (AI) and expansion of access to providers with neurologic expertise via telestroke will all contribute to the judicious use of HEMS. However, initial providers should have a clear understanding of the basic criteria for AIS treatment and access to tools that make this information readily accessible. We therefore propose the following decision tree (figure 1 and 2).
Figure 1:
Suggested HEMS transfer flowchart in acute ischemic stroke.
Figure 2:
High value flight criteria in acute ischemic stroke.
* Modified Rankin Score < 3 (responsible for most activities of daily living)
Strengths of our study include analyzing HEMS utilization at a large volume Joint Commission Certified comprehensive stroke center in a state with significant rural and triborder catchment area where efficient allocation of resources and thoughtful triage are essential. We were able to isolate the target population of AIS patients by only evaluating HEMS use in patients with a confirmed diagnosis of cerebrovascular ischemia. Furthermore, by defining HEMS flights of low value in a clinically meaningful manner to include any reasonable reason an ischemic stroke patient would have needed a higher level of care during transport, our results are more likely to represent a true rate of misutilization. Other authors have cited lack of acute ischemic stroke intervention as suboptimal HEMS utilization5, 12–15. However, these results are misleading as AIS patients who required more intensive medical care still should be eligible for HEMS even though they did not undergo an acute ischemic stroke intervention. Our inclusion of detailed clinical information such as transferring NIHSS and angiography results fundamental to transport triage further enhances the precision of our low value HEMS calculation.
Limitations:
Important limitations include those inherent to any retrospective review. We made every attempt to capture all stroke-related flights and minimize the variability related to multiple helicopter carriers and lack of a standardized EMS electronic medical record. However, it is possible we are underestimating the number of low flight value HEMS cases. Although our population of interest (AIS) was carefully defined, we must acknowledge that many first providers do not have the luxury of definitive diagnoses and are managing patients based on probabilities and clinical judgement. Therefore, it would be important to better understand the utilization patterns of those HEMS patients with suspected AIS as over one-third (39.2% or 113/288) of our total HEMS stroke alerts were ultimately not AIS cases.
Conclusion
HEMS transport for AIS patients plays a crucial role in delivering the best care. However, for a significant proportion of patients, air transport does not offer substantial benefit and these patients can be safely transported by other means, saving cost and allowing this valuable resource to be available for others in need. The majority of patients not requiring air transport are those outside of acute treatment windows. More than half of low flight value air transport cases were initiated after provider evaluation. These results represent a unique opportunity to coordinate education and build effective triage paradigms across a system of stroke care. We propose the above decision tree to assist EMS and first contact providers in making informed optimal transport decisions for patients with acute ischemic stroke.
Highlights:
1) Why is this topic important?
Optimization of aeromedical transport is understudied, especially as it is related to cerebrovascular patients.
2) What does this study attempt to show?
This study reviews the trends in helicopter emergency medical transport (HEMS) utilization in a comprehensive stroke center within a large rural academic medical center.
3) What are the key findings?
Among acute stroke cases, only 16% (23/141) were deemed of low flight value or over-triaged. However over 50% (13/23) of these occurred following provider evaluation, highlighting an important area of improvement for stroke systems of care.
4) How is patient care impacted?
By employing evidence-based strategies when transferring acute stroke patients, judicious use of limited resources minimizes burden on the healthcare system and individual patients.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Vercruysse GA, Friese RS, Khalil M, et al. Overuse of helicopter transport in the minimally injured: A health care system problem that should be corrected. J Trauma Acute Care Surg 2015;78:510–515. [DOI] [PubMed] [Google Scholar]
- 2.Katz BS, Adeoye O, Sucharew H, et al. Estimated Impact of Emergency Medical Service Triage of Stroke Patients on Comprehensive Stroke Centers: An Urban Population-Based Study. Stroke 2017;48:2164–2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018;379:611–622. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–1731. [DOI] [PubMed] [Google Scholar]
- 5.Leira EC, Stilley JD, Schnell T, Audebert HJ, Adams HP, Jr. Helicopter transportation in the era of thrombectomy: The next frontier for acute stroke treatment and research. Eur Stroke J 2016;1:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adeoye O, Nystrom KV, Yavagal DR, et al. Recommendations for the Establishment of Stroke Systems of Care: A 2019 Update. Stroke 2019;50:e187–e210. [DOI] [PubMed] [Google Scholar]
- 7.Adeoye O, Albright KC, Carr BG, et al. Geographic access to acute stroke care in the United States. Stroke 2014;45:3019–3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adcock AK, Choi J, Alvi M, et al. Expanding Acute Stroke Care in Rural America: A Model for Statewide Success. Telemed J E Health 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reiner-Deitemyer V, Teuschl Y, Matz K, et al. Helicopter transport of stroke patients and its influence on thrombolysis rates: data from the Austrian Stroke Unit Registry. Stroke 2011;42:1295–1300. [DOI] [PubMed] [Google Scholar]
- 10.Hutton CF, Fleming J, Youngquist S, Hutton KC, Heiser DM, Barton ED. Stroke and Helicopter Emergency Medical Service Transports: An Analysis of 25,332 Patients. Air Med J 2015;34:348–356. [DOI] [PubMed] [Google Scholar]
- 11.Martins SCO, Weiss G, Almeida AG, et al. Validation of a Smartphone Application in the Evaluation and Treatment of Acute Stroke in a Comprehensive Stroke Center. Stroke 2020;51:240–246. [DOI] [PubMed] [Google Scholar]
- 12.Olson MD, Rabinstein AA. Does helicopter emergency medical service transfer offer benefit to patients with stroke? Stroke 2012;43:878–880. [DOI] [PubMed] [Google Scholar]
- 13.Sequeira D, Martin-Gill C, Kesinger MR, et al. Characterizing Strokes and Stroke Mimics Transported by Helicopter Emergency Medical Services. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors 2016;20:723–728. [DOI] [PubMed] [Google Scholar]
- 14.Silbergleit R, Scott P, Md M, Md MBA. Cost–Effectiveness of Helicopter Transport of Stroke Patients for Thrombolysis. Academic Emergency Medicine 2003;10:966–972. [DOI] [PubMed] [Google Scholar]
- 15.Thomas SH, Cheema F, Cumming M, Wedel SK, Thomson D. N ONTRAUMA H ELICOPTER E MERGENCY M EDICAL S ERVICES T RANSPORT : A NNOTATED R EVIEW OF S ELECTED O UTCOMES - RELATED L ITERATURE. Prehospital Emergency Care 2002;6:242–255. [DOI] [PubMed] [Google Scholar]