Abstract
OBJECTIVES:
Hospitalized children experience frequent nighttime awakenings. Oral medications are commonly administered around the clock despite the comparable efficacy of daytime administration schedules, which promote sleep. With this study, we evaluated the effectiveness of a quality improvement initiative to increase the proportion of sleep-friendly antibiotic administration schedules.
METHODS:
Interprofessional stakeholders modified computerized provider order entry defaults for 4 oral antibiotic medications, from around the clock to administration occurring exclusively during waking hours. Additionally, care-team members received targeted education. Outcome measures included the proportion of sleep-friendly administration schedules and patient caregiver–reported disruptions to sleep. Pre- and posteducation surveys were used to evaluate education effectiveness. Balancing measures were missed antibiotic doses and related escalations of care.
RESULTS:
Interrupted time series analysis revealed a 72% increase (interceptpre: 18%; interceptpost: 90%; 95% confidence interval: 65%–79%; P < .001) in intercept for percentage of orders with sleep-friendly administration schedules (orders: npre = 1014 and npost = 649). Compared with preeducation surveys, care-team members posteducation were more likely to agree that oral medications scheduled around the clock cause sleep disruption (resident: 71% pre, 90% post [P = .01]; nurse: 63% pre, 79% post [P = .03]). Although sleep-friendly orders increased, patient caregivers reported an increase in sleep disruption due to medications (pre 28%, post 46%; P < .001).
CONCLUSIONS:
A simple, low-cost intervention of computerized provider order entry default modifications and education can increase the proportion of sleep-friendly oral antibiotic administration schedules for hospitalized children. Patient perception of sleep is impacted by multiple factors and often does not align with objective data. An increased focus on improving sleep during hospitalization may result in heightened awareness of disruptions.
Inadequate sleep in pediatric patients is associated with poor health outcomes such as an increased risk of diabetes and hypertension.1 Because sleep is essential to health and recovery, the American Academy of Nursing’s Choosing Wisely initiative recommends delaying routine overnight care, unless otherwise clinically indicated, in an effort to optimize patient sleep.2 Nevertheless, researchers report hospitalized children experience frequent awakenings,3–9 and medication administration is cited as a common disruptor to sleep.7–9
Although some medications must be administered around the clock, research reveals that certain oral antibiotics can be given with comparable efficacy in a sleep-friendly manner (2, 3, and 4 times exclusively during daytime hours), thereby promoting patient-centered care.10–16 Flexible medication administration schedules help inpatients sleep longer and align with their typical sleep patterns at home.17 Quality improvement (QI) efforts to promote sleep-friendly venous thromboembolism prophylaxis (VTE) administration schedules have contributed to reduced patient-reported nighttime sleep disruptions in adult general medicine patients.18 Despite the benefits of sleep-friendly administration schedules, oral antibiotic schedules for hospitalized children at our institution are programmed in the electronic health record (EHR) to default to around-the-clock administration.
Computerized provider order entry (CPOE) default options represent an effective mechanism to affect ordering practice.19 These defaults are unique in that they influence behavior in a noninterruptive manner and still empower physicians to use clinical judgment.19,20 Relying on aspects of human decision-making, such as individuals’ avoidance of change and greater fear of making errors of commission rather than omission,19 defaults have been used in multiple settings to improve patient care.19–22 Previous QI efforts at our institution have successfully improved patient sleep by using CPOE defaults and care-team education to decrease nighttime VTE prophylaxis in adults18 and limit unnecessary overnight blood pressure monitoring in children.9
In a 1-year needs assessment at an urban, academic medical center, caregivers of pediatric general medicine patients identified medications as one of the top disruptors to inpatient sleep.9 Although studies in the pediatric setting have called for interventions to limit disruptions,3–8 to our knowledge, no initiatives have been focused on optimizing medication administration schedules for hospitalized children’s sleep. Informed by previous institutional initiatives, we aimed to implement and evaluate the effectiveness of a QI intervention consisting of EHR modifications and care-team education to increase the proportion of sleep-friendly oral antibiotic administration schedules for hospitalized children.
Methods
Conceptual Framework
In designing our intervention, we used the culture, oversight accountability, system support, and training (COST) Framework for High-Value Care Intervention.23 This framework provides a multipronged approach to implementing high-value care.23 Using all 4 components of this framework is critical to effecting change.
Culture
We built on our institution’s preexisting culture of studying and promoting sleep for adult and pediatric inpatients. Caregivers of patients admitted to the pediatric general medicine ward of an urban, academic medical center identified medications as one of the top disruptions to inpatient pediatric sleep.9 Informal focus groups with nursing, pediatric infectious disease (PID), and pediatric pharmacy reported oral antibiotics as the primary medications with frequent around-the-clock dosing that could also be administered through flexible dosing schedules. We formed an interprofessional team of peer-champions to design, implement, and promote the intervention.
Oversight Accountability
Pediatric pharmacy reviews and verifies medication orders. PID and pediatric pharmacy receive reports regarding missed antibiotic doses and resulting escalations of care. Pharmacy informatics provided regular updates regarding sleep-friendly order use.
System Support
Using pharmacy informatics medication use data, pediatric pharmacy and PID helped identify 4 oral antibiotics as frequently prescribed, as well as effective and safe when scheduled exclusively during waking hours. Amoxicillin, amoxicillin-potassium clavulanate, cephalexin, and clindamycin were selected for the intervention.
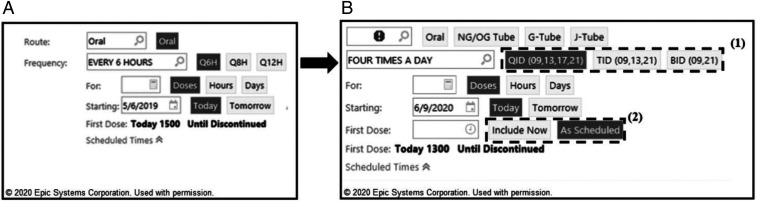
Pharmacy informatics modified pediatric inpatient medication records for the above 4 oral antibiotics in the EHR system Epic (Epic Systems Corporation, Verona, WI). Order entry systems that defaulted to administration around the clock every 6 hours (q6h), every 8 hours (q8h), and every 12 hours (q12h) were modified to default to a corresponding sleep-friendly option that avoided dosing during sleeping hours, such as 4 times per day (QID), 3 times per day (TID), and 2 times per day (BID), respectively (Fig 1).
FIGURE 1.
A, Preintervention CPOE default in the EHR for around-the-clock dosing (q6h, q8h, and q12h). B, Postintervention CPOE default to encourage sleep-friendly oral administration scheduling (QID, TID, and BID) for the targeted medications. Modified order screens included default sleep-friendly dosing schedules with preset daytime administration hours (1), and an “Include Now” option to administer medication immediately and then continue with the sleep-friendly administration schedule (2). G-Tube, gastrostomy tube; J-Tube, jejunostomy tube; NG, nasogastric; OG, orogastric.
The sleep-friendly administration schedules were preset to administration times of 9 am, 1 pm, 5 pm, and 9 pm for QID dosing; 9 am, 1 pm, and 9 pm for TID dosing; and 9 am and 9 pm for BID dosing. These preset times helped to ensure a consistent administration time was ordered for the appropriate waking hours, especially because institutional policy requires medications to be administered within a 1-hour window around the preset time. To prevent missed doses, an “Include Now” button allowed physicians to order an immediate dose of medication and then continue with sleep-friendly scheduling. Around-the-clock administration scheduling was maintained as an option, and physicians were encouraged to use their clinical judgment when ordering medications.
Before the modified order screens went live, changes were discussed with key stakeholders, including pediatric hospital medicine, pediatric QI, PID, pediatric pharmacy, and nurse managers. An electronic notification about the order screen modifications was circulated to all inpatient pediatric clinicians before rollout of the new order defaults in mid-July 2019.
Training
Education sessions covering the importance of sleep-friendly administration schedules and an introduction to the intervention were provided to physicians, nurses, and clinical pharmacy specialists via in-person and electronic presentations at the time of implementation and in the weeks after. Nurses and pharmacists were empowered to encourage physicians to employ sleep-friendly oral antibiotic administration schedules to promote patient sleep.
Study of the Intervention
Measures
The intervention’s primary outcome measure was the proportion of sleep-friendly administration schedules ordered. Pharmacy informatics generated a use report for the targeted antibiotics pre- and postintervention. Medication orders were classified as sleep-friendly if scheduled to be administered QID, TID, or BID.
A secondary outcome measure was caregiver-reported perception of medications as a disruptor to sleep. During the intervention period, research assistants administered surveys that included the Potential Hospital Sleep Disruptions and Noises Questionnaire (PHSDNQ) to a convenience sample of caregivers of children admitted to the general pediatric ward (Supplemental Information). The PHSDNQ asks patients to rate the disruptiveness of certain nighttime hospital disruptions to sleep on a Likert scale and has been validated in the adult population.8,9,24,25 English-speaking patient caregivers who had slept the previous night in their child’s hospital room and whose child was awake, cognitively intact, and aged 30 days to 18 years were eligible. Exclusion criteria aimed to help target a population of largely healthy pediatric patients. Thus, patients who had recently undergone a procedure or had established diagnoses thought to affect sleep, such as tracheostomy, nasogastric or gastrostomy tube, or sleep apnea, were excluded. Additionally, those undergoing continuous EEG and known abuse victims were excluded. Research Electronic Data Capture version 8.11.0 (Vanderbilt University, Nashville, TN) was used to store all survey data.
Because the COST framework identifies training as a critical component to change behavior,23 we evaluated the effectiveness of our education sessions. This was measured by pre- and posteducation Likert-scale surveys that asked participants to agree or disagree with the statements “Oral medications scheduled q6h, q8h, or q12h are disruptive to patient sleep” and “At our hospital, oral medication dosing schedules are optimized for patient sleep.” The pre- and posteducation surveys were given immediately before and after the education sessions, respectively, to gauge the sessions’ immediate impact on participant knowledge. These questions were selected to assess care-team members’ understanding of the intervention and its importance, which would inform whether more extensive education about the intervention would be required. Surveys of participants who completed both a pre- and posteducation survey were included in our data analysis.
PID and pediatric pharmacy provided oversight of the intervention throughout its implementation and use, as a balancing measure. Specifically, PID and pediatric pharmacy were asked to report any instances of missed doses of the targeted antibiotics or escalations of patient care due to the intervention.
Analysis
A single-group interrupted time series analysis (ITSA) was used to plot the proportion of sleep-friendly orders for the targeted oral antibiotics each week. Postintervention was defined as starting on July 12, 2019, the date the modified order screens went live.
A PHSDNQ score of 1 was defined as “no sleep disruption” and a score of ≥2 was defined as “sleep disruption.” Caregiver responses were dichotomized and a χ2 test was used to compare the proportion of caregivers pre- and postintervention who reported disruption due to medications.
Pre- and posteducation survey responses were calculated and dichotomized at the median value of 4. Scores of 4 or 5 were considered an answer of “agree” and scores of <4 were considered an answer of “disagree.” A 2-sample test for proportions was used to compare the dichotomized data. Analyses were performed by using Stata 16.0 (Stata Corp, College Station, TX).
Ethical Considerations
The intervention received a formal determination of QI status according to institutional policy, and survey methods were approved by the institutional review board (12-1766).
Results
Primary Outcome Measure: Proportion of Sleep-Friendly Administration Schedules
In the 1-year preintervention period (July 2018–July 2019), 711 patients received 1014 orders for the antibiotics targeted in the intervention (amoxicillin, amoxicillin-potassium clavulanate, cephalexin, and clindamycin) because some patients were prescribed multiple oral antibiotics. In the 9 months postintervention (July 2019–April 2020), 466 patients received 649 orders for the targeted antibiotics.
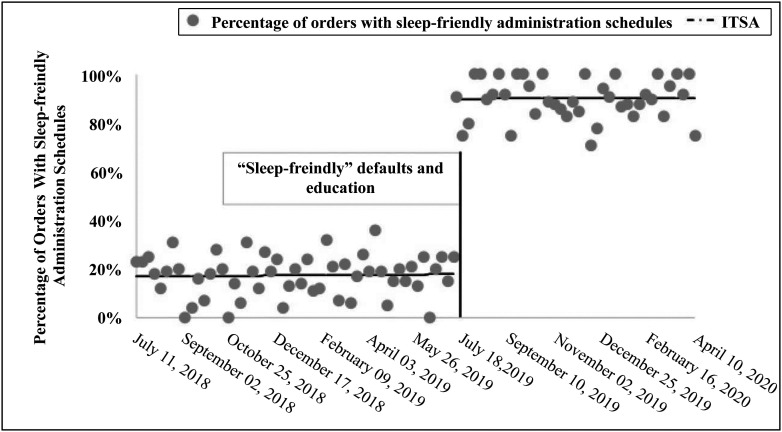
ITSA reveals that the percentage of orders with sleep-friendly administration schedules increased in intercept by 72% postintervention (interceptpre18%, interceptpost 90%; 95% confidence interval: 65%–79%; P < .001) (Fig 2). There were no significant decreases in the slope each week postintervention, demonstrating an overall change in practice rather than a temporary shift in prescribing patterns.
FIGURE 2.
ITSA graph depicting proportion of orders with sleep-friendly administration schedules for targeted oral antibiotics per week. ITSA is depicted by the dashed line, which reveals an increase in intercept of 72% after the intervention (interceptpre: 18%, interceptpost: 90%; 95% confidence interval: 65%–79%; P < .001).
Secondary Outcome Measure: Caregiver-Reported Patient Sleep Disruption
Pre- and postintervention, caregivers of patients completed 165 and 136 surveys, respectively. Demographic information and primary diagnoses of the survey populations are displayed in Table 1; no statistically significant differences were seen between the 2 groups. Caregivers reported an increase in disruptions due to medications (preintervention: 28%; postintervention: 46%; P < .001).
TABLE 1.
Descriptive Characteristics of Surveyed Patients
| Preintervention | Postintervention | P | |
|---|---|---|---|
| n (%) | n (%) | ||
| Age | .67 | ||
| <2 | 71 (43.0) | 54 (39.7) | |
| 2–5 | 52 (31.5) | 40 (29.4) | |
| 6–9 | 26 (15.8) | 21 (15.4) | |
| 10–13 | 7 (4.2) | 10 (7.4) | |
| ≥14 | 9 (5.5) | 11 (8.1) | |
| Sex | .91 | ||
| Male | 81 (49.1) | 68 (50.0) | |
| Female | 84 (50.9) | 68 (50.0) | |
| Race | .09 | ||
| Black | 122 (73.9) | 91 (66.9) | |
| White | 27 (16.4) | 18 (13.2) | |
| Hispanic | 12 (7.3) | 20 (14.7) | |
| Other | 4 (2.4) | 7 (5.2) | |
| Primary diagnosis | .50 | ||
| Respiratory | 93 (56.4) | 82 (60.3) | |
| Musculoskeletal and/or skin | 20 (12.1) | 19 (13.9) | |
| Gastrointestinal and/or liver | 17 (10.3) | 8 (5.9) | |
| Other | 14 (8.5) | 13 (9.6) | |
| Neurologic and/or CNS | 13 (7.9) | 5 (3.7) | |
| Kidney and/or genitourinary | 4 (2.4) | 6 (4.4) | |
| Not available | 4 (2.4) | 3 (2.2) |
CNS, central nervous system.
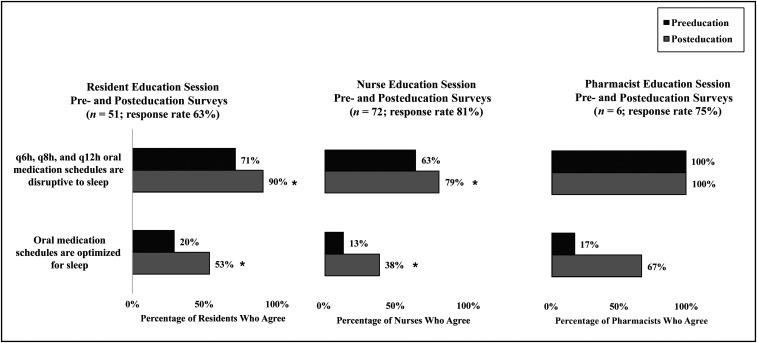
Care-Team Education Session Surveys
A total of 63% of residents (51 of 81), 81% of nurses (72 of 89), and 75% of pharmacy clinical specialists (6 of 8) completed a pre- and posteducation survey. Before education sessions, physicians and nurses demonstrated room for improvement regarding their knowledge of how around-the-clock scheduling can disrupt hospitalized children’s sleep; however, after education sessions, awareness improved (resident: 71% preintervention, 90% postintervention, P = .01; nurse: 63% preintervention, 79% postintervention, P = .03) (Fig 3). Pharmacy clinical specialists showed a higher baseline awareness of the impact of medications on patient sleep, with all agreeing that around-the-clock schedules are disruptive to sleep (Fig 3).
FIGURE 3.
Resident, nurse, and pharmacist responses to pre- and posteducation surveys regarding (1) the disruptiveness of different medication administration schedules to sleep and (2) if oral medication administration schedules at the hospital are optimized for sleep. * P < .05.
After education about the planned intervention, residents, nurses, and pharmacists reported a higher level of agreement that oral medications are optimized for sleep at the hospital (residents: 20% preintervention, 53% postintervention, P < .001; nurses: 13% preintervention, 38% postintervention, P = .001; pharmacists: 17% preintervention, 67% postintervention, P = .08) (Fig 3).
Balancing Measures
During the intervention, pediatric pharmacy and PID did not report any missed doses of the targeted antibiotics or escalation of care related to patients receiving sleep-friendly administration schedules.
Discussion
Summary
This QI initiative reveals that an intervention consisting of alterations to CPOE defaults and clinician education can significantly increase the proportion of sleep-friendly administration schedules for hospitalized children. ITSA reveals an increase of 72% in sleep-friendly orders postintervention, and education sessions displayed an increase of >15% in nurse and physician awareness that around-the-clock administration schedules are disruptive to sleep. Unexpectedly, despite a successful implementation and uptake of the intervention, patient caregivers reported an increase in sleep disruption due to medications. Although this study demonstrates that a simple, low-cost intervention can optimize oral antibiotic administration to support hospitalized children’s sleep, patient perception of sleep does not always align with objective data. An institutional focus on and commitment to improving sleep during hospitalization may result in heightened awareness of disruptions among patients and caregivers.
Interpretation
In previous studies, researchers have reported hospitalized children often experience awakenings and have noted the necessity of interventions to reduce sleep disruption,3–9 such as minimizing around-the-clock medication administration.5,7 To the best of our knowledge, this is the first QI initiative to promote sleep-friendly oral antibiotic administration schedules in hospitalized children through CPOE defaults and care-team member education. Consistent with the tenets of the COST framework, we used culture, oversight accountability, system support, and training to affect practice change.23 The increase in, but not complete transition to, sleep-friendly orders indicates that clinicians were empowered to use their judgment regarding the clinical appropriateness of sleep-friendly medication administration schedules for each patient. This finding supports the results of previous QI initiatives at our institution, which have revealed that EHR defaults paired with education can help limit nighttime disruptions through clinically appropriate reductions in overnight blood pressure monitoring in children9 and in overnight vitals and nighttime VTE prophylaxis in adults.18
A number of factors may explain the inconsistent finding that despite decreased overnight medication administration, caregivers reported increased sleep disruptions due to medications. First, the PHSDNQ does not specify the route or type of medications when asking caregivers about sleep disruption due to medications. Thus, it is possible the survey instrument’s specificity did not allow us to detect a decrease in sleep disruption due to oral antibiotic administration. Second, consistent with our team’s previous work in the adult and pediatric settings, we have found that patient and caregiver perceptions of sleep do not always align with objective data. We believe that a large contributor to this is our institution’s commitment to and discussion about improving patient sleep, which may have resulted in a heightened awareness among our patients about the potential disruptors that can occur overnight in a hospital. Overall, with our work, we highlight that although objective measures may point to an intervention’s success, patient-centered QI initiatives must take into account subjective measures as well.
It is important to note several aspects of the intervention that contributed to its successful implementation and adoption. Collaboration with interprofessional stakeholders to identify antibiotics with good oral bioavailability was important not only in ensuring the intervention was safe and effective but also essential in dissemination of the intervention to clinicians who would use the modified default. Additionally, the intervention aligned with an institutional culture to support sleep. During informal focus groups, nurses described efforts to cluster care to limit waking patients, which may explain why, when compared with residents, nurses were less likely to recognize around-the-clock medications as disruptive to sleep.
This study has several limitations. Generalizability of the intervention to other settings may be limited because it is a single-site study at an urban, academic center that uses an EHR. Currently, we are considering additional oral medications to target and are expanding sleep-friendly initiatives to a partner institution, which may help to further elucidate generalizability. Because pediatric general medicine patients on average have a short length of stay, we did not collect objectively measured sleep through actigraphy. Assessment of care-team member education occurred immediately before and after education sessions; thus, it is possible the effect of the education faded with time. Additionally, we evaluated the intervention’s effect on the proportion of sleep-friendly schedules holistically, and so we cannot state if the same outcome could have been achieved with just one of the intervention’s components, such as the education sessions or CPOE defaults, respectively. Finally, we were not able to review individual patient charts and thus could not identify if there were patients who could have received an oral antibiotic targeted in this intervention and instead were prescribed an intravenous formulation. Future work might include exploring potential barriers to transitioning patients to sleep-friendly oral antibiotic administration schedules.
Because sleep is critical to child development and successful recovery,1 it is important for institutions to examine whether certain hospital practices can be modified to limit sleep disruption. Consistent with the American Academy of Nursing’s Choosing Wisely campaign, the avoidance of unnecessary nighttime care is patient-centered care.2
Conclusions
Hospitalized children experience frequent nighttime awakenings, and oral medications are often scheduled around the clock despite comparable efficacy during waking hours. A simple, low-cost intervention consisting of CPOE defaults and education sessions can significantly increase and sustainably support sleep-friendly oral antibiotic administration scheduling for pediatric inpatients. Prioritizing sleep for patients is critical, yet perception of sleep disruption is impacted by multiple factors, and a focus on improving sleep during hospitalization may result in heightened awareness of disruptions.
Acknowledgments
We thank Edward Gomes, Ella Bradford, and Emma Picker for their help with data collection.
Footnotes
Ms Mozer aided in study design, conducted the analysis, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Bhagat and Seward aided in study design and intervention implementation and reviewed and revised the manuscript; Drs Konold and Kumar aided in intervention implementation and reviewed and revised the manuscript; Ms Anderson and Mr Mason aided in study design and reviewed and revised the manuscript; Mr Byron and Dr Peirce aided in data collection and reviewed and revised the manuscript; Drs Orlov and Arora conceptualized and designed the study, coordinated and supervised data collection methods, liaised with stakeholders during the intervention period, and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Heart, Lung, and Blood Institute (R25HL116372, K24HL136859). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Board of Internal Medicine Choosing Wisely Initiative. American Academy of Nursing: don’t wake patients for routine care choosing wisely. 2014. Available at: http://www.choosingwisely.org/clinician-lists/american-academy-nursing-avoid-waking-patients-for-routine-care/. Accessed June 14, 2019
- 3.Stremler R, Adams S, Dryden-Palmer K. Nurses’ views of factors affecting sleep for hospitalized children and their families: a focus group study. Res Nurs Health. 2015;38(4):311–322 [DOI] [PubMed] [Google Scholar]
- 4.Herbert AR, de Lima J, Fitzgerald DA, Seton C, Waters KA, Collins JJ. Exploratory study of sleeping patterns in children admitted to hospital. J Paediatr Child Health. 2014;50(8):632–638 [DOI] [PubMed] [Google Scholar]
- 5.Erondu AI, Orlov NM, Peirce LB, et al. Characterizing pediatric inpatient sleep duration and disruptions. Sleep Med. 2019;57:87–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meltzer LJ, Davis KF, Mindell JA. Patient and parent sleep in a children’s hospital. Pediatr Nurs. 2012;38(2):64–71; quiz 72 [PubMed] [Google Scholar]
- 7.Linder LA, Christian BJ. Nighttime sleep characteristics of hospitalized school-age children with cancer. J Spec Pediatr Nurs. 2013;18(1):13–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peirce LB, Orlov NM, Erondu AI, et al. Caregiver and staff perceptions of disruptions to pediatric inpatient sleep. J Clin Sleep Med. 2018;14(11):1895–1902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook DJ, Arora VM, Chamberlain M, et al. Improving hospitalized children’s sleep by reducing excessive overnight blood pressure monitoring. Pediatrics. 2020;146(3):e20192217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kimberlin DW, Brady MT, Jackson MA, Long SS, eds; American Academy of Pediatrics. Red Book: 2018 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2018 [Google Scholar]
- 11.Cyriac JM, James E. Switch over from intravenous to oral therapy: a concise overview. J Pharmacol Pharmacother. 2014;5(2):83–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cleocin HCL. Package insert. Kalamazoo, MI: Pharmacia and Upjohn; 2020 [Google Scholar]
- 13.Keflex. Keflex Capsules (Cephalexin, USP) Prescribing Information. Germantown, MD: Advancis Pharmaceutical Corporation; 2005 [Google Scholar]
- 14.Curtin CD, Casey JR, Murray PC, et al. Efficacy of cephalexin two vs. three times daily vs. cefadroxil once daily for streptococcal tonsillopharyngitis. Clin Pediatr (Phila). 2003;42(6):519–526 [DOI] [PubMed] [Google Scholar]
- 15.Damrikarnlert L, Jauregui AC, Kzadri M. Efficacy and safety of amoxycillin/clavulanate (Augmentin) twice daily versus three times daily in the treatment of acute otitis media in children. The Augmentin 454 Study Group. J Chemother. 2000;12(1):79–87 [DOI] [PubMed] [Google Scholar]
- 16.Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin: a noninferiority trial. Pediatr Infect Dis J. 2006;25(9):761–767 [DOI] [PubMed] [Google Scholar]
- 17.Jarman H, Jacobs E, Walter R, Witney C, Zielinski V. Allowing the patients to sleep: flexible medication times in an acute hospital. Int J Nurs Pract. 2002;8(2):75–80 [DOI] [PubMed] [Google Scholar]
- 18.Arora VM, Machado N, Anderson SL, et al. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14(1):38–41 [DOI] [PubMed] [Google Scholar]
- 19.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357(13):1340–1344 [DOI] [PubMed] [Google Scholar]
- 20.Rubins D, Boxer R, Landman A, Wright A. Effect of default order set settings on telemetry ordering. J Am Med Inform Assoc. 2019;26(12):1488–1492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malhotra S, Cheriff AD, Gossey JT, Cole CL, Kaushal R, Ancker JS. Effects of an e-Prescribing interface redesign on rates of generic drug prescribing: exploiting default options. J Am Med Inform Assoc. 2016;23(5):891–898 [DOI] [PubMed] [Google Scholar]
- 22.Kim M, Kaplan SJ, Mitchell SH, et al. The effect of computerized physician order entry template modifications on the administration of high-risk medications in older adults in the emergency department. Drugs Aging. 2017;34(10):793–801 [DOI] [PubMed] [Google Scholar]
- 23.Costs of Care. “COST” Framework for High-Value Care Intervention. 2020. Available at: https://costsofcare.org/frameworks-surveys/. Accessed October 21, 2020
- 24.Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J Appl Psychol. 1985;70(1):22–28 [PubMed] [Google Scholar]
- 25.Grossman MN, Anderson SL, Worku A, et al. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med. 2017;13(2):301–306 [DOI] [PMC free article] [PubMed] [Google Scholar]