Abstract
Objective:
We compared eating disorder (ED) characteristics and treatment seeking behaviors between self-identified competitive athletes and non-athletes in a large, community-based sample.
Method:
During the 2018 National Eating Disorders Awareness Week, 23,920 respondents, 14.7% of whom identified as competitive athletes, completed the National Eating Disorders Association online screen. Data were collected on demographics, disordered eating behaviors, probable ED diagnosis/risk, treatment history, and intent to seek treatment.
Results:
The sample was predominately White (81.8%), female (90.3%), and between 13–24 years (82.6%). Over 86% met criteria for an ED/subthreshold ED, and of those, only 2.5% were in treatment. Suicidal ideation was reported in over half of the sample. Athletes reported a significantly greater likelihood of engaging in and more frequent excessive exercise episodes than non-athletes. Athletes also reported a significantly lower likelihood of engaging in and less frequent binge-eating episodes compared with non-athletes. Athletes were more likely to screen positive for an ED/subthreshold ED than non-athletes, but percentages across all probable ED diagnoses were similar. No significant differences between athletes and non-athletes emerged on treatment history or intention to seek treatment post-screen (less than 30%).
Discussion:
Although the distribution of probable ED diagnoses was similar in athletes and non-athletes, symptom profiles related to disordered eating behavior engagement and frequency may differ. Athletes may be less likely to seek treatment due to stigma, accessibility, and sport-specific barriers. Future work should directly connect survey respondents to tailored treatment tools and increase motivation to seek treatment.
Keywords: eating disorders, disordered eating behaviors, athletes, online screen, treatment seeking
Introduction
Eating disorders (EDs) affect up to 5% of the population (Hudson et al., 2007; Smink, van Hoeken, & Hoek, 2012), and athletes often report a higher prevalence of EDs than non-athletes (Joy, Kussman, & Nattiv, 2016; Sundgot-Borgen & Torstveit, 2004; Thompson & Sherman, 2010). Specifically, one review reported that up to 8% of male-identified athletes and up to 33% of female-identified athletes screened positive for an ED (Bratland-Sanda and Sundgot-Borgen 2013). In addition, the prevalence of disordered eating behaviors (i.e., not threshold diagnoses) was higher in athletes than in non-athletes (up to 19% in male athletes and up to 45% in female athletes; Bratland-Sanda & Sundgot-Borgen, 2013). Despite widespread sports participation in the community at all competitive levels, most studies focus on elite and collegiate athletes, possibly due to the ease of recruiting through professional sport and college institutional channels (Thompson & Sherman, 2010). Findings in high-level and collegiate athletes are briefly summarized below for context; however, studies of community-based athlete samples (e.g., high school athletes, intramural athletes, “weekend warriors,” and older athletes beyond their peak elite status) across ED characteristics and treatment seeking are lacking.
Among high-level athletes, reported ED prevalence and disordered eating behavior frequency are typically higher than in non-athletes (e.g., Byrne & McClean, 2002; Thompson & Sherman, 2010; Torstveit, Rosenvinge, & Sundgot-Borgen, 2008). Reports on collegiate athletes are mixed. Although female collegiate athletes have demonstrated a higher prevalence of EDs and ED symptomatology than male-identified collegiate athletes (e.g., Krebs et al., 2019), it is less clear if the prevalence in collegiate athletes exceeds that of non-athlete collegiate students (Greenleaf et al., 2009; Johnson, Powers, and Dick, 1999). Across ED behaviors, one of the only studies comparing college athletes, independent exercisers, and non-exercisers observed greater severity of ED symptomatology at higher levels of sport participation (Holm-Denoma et al., 2009). Among other sport-specific ED risk factors, support for the association between identifying as an athlete and more severe ED psychopathology is growing (e.g., Palermo & Rancourt, 2019).
Treatment Barriers and Treatment Seeking in Athletes
In addition to well-established barriers to mental health treatment, including high cost, lack of availability and accessibility, stigma, and low perceived need (Eisenberg, Downs, Golberstien, & Zivin, 2009; Eisenberg, Nicklett, Roeder, & Kirz, 2011, Mojtabai et al., 2012), almost half of individuals with EDs do not recognize that their disorder warrants treatment (Gratwick-Sarll, Mond, & Hay, 2013; Mond, Hay, Rodgers, & Owen, 2006). Compounding these barriers to treatment, athletes experience rigorous training schedules, frequent travel for events, greater stigma around mental health than non-athletes (Gulliver, Griffiths, & Christensen, 2012), normalization of disordered eating behaviors, unsafe weight loss practices, and amenorrhea (Alwan et al., 2019; Currie, 2010; Thompson & Sherman, 2010). Factors such as lack of time, fear that seeking treatment demonstrates weakness (López & Levy, 2013; Reardon & Factor, 2010), and the perception that engaging in disordered eating behaviors and low weight will enhance performance (Martinsen, Bratland-Sanda, Eriksson, & Sundgot-Borgen, 2010; Werner et al., 2013) may also reduce treatment seeking. Despite the negative impact EDs have on athletic performance (e.g., low energy availability, dehydration, muscle loss, and high rates of injuries; El Ghoch et al., 2013; Thein-Nissenbaum et al., 2011), little information is available on treatment seeking behaviors, particularly in community athletes.
Screening Athletes for Eating Disorders
Online screening tools can reach large numbers of participants (Fitzsimmons-Craft et al., 2019) and deliver earlier access to interventions (Franko et al., 2013; Mountjoy et al., 2014; Rosen, 2010). The National Eating Disorders Association’s (NEDA; the largest U.S. non-profit for EDs) online screen is the first large-scale dissemination of a digital ED screen. In its first six months in 2017, over 71,000 adults aged 18 to 65+ across the United States completed the screen (Fitzsimmons-Craft et al., 2019). However, large-scale digital screening has yet to be harnessed to examine differences between athletes and non-athletes in a community sample.
In the current study using NEDA’s online screening tool, we assessed differences between self-identified competitive athletes and non-athletes in a community sample on: 1) the likelihood of engaging in and frequency of disordered eating behaviors; 2) ED diagnosis, evaluated by ED diagnostic and risk categories; and 3) treatment seeking behaviors, measured by current treatment status, intention to seek treatment, and intended treatment modalities following screen completion.
Methods
Procedure
This was an observational study using data from NEDA’s online screening tool during the 2018 National Eating Disorders Awareness Week (February 26, 2018-March 4, 2018) when almost 25% of annual screens are completed through NEDA’s website. Promotion of the screening tool was conducted via social media and emails through ad campaigns, NEDA’s helpline, and media articles. No specific recruitment strategies targeting athletes were implemented. Respondents accessed the confidential screen by going to NEDA’s website (https://www.nationaleatingdisorders.org/screening-tool). The screen was only offered in English, and a disclaimer at the beginning of the screen stated that it was intended for individuals ages 13 and older. Following completion, respondents received feedback based on their risk or probable diagnosis, referral information, and optional questions on future treatment seeking.
Participants
Data were collected only from respondents who submitted their screen (n=26,659). Respondents were excluded if they 1) were under age 13 (n=325); 2) lived outside the U.S. (n=2,041); 3) did not provide a current weight and/or height (n=176); reported a current weight (<50 pounds or >625 pounds), height (<48 inches or >84 inches), or BMI values (<10 kg/m2 or >100 kg/m2) outside expected ranges (n=14; Fitzsimmons-Craft et al., 2019); 5) reported disordered eating behaviors outside expected ranges (more than 500 episodes of binge eating, vomiting, diuretic/laxative use, excessive exercise, fasting in the previous three months; n=60); or 6) did not report age, race, or gender which were included as covariates (n=123). Our total analytic sample comprised 23,920 observations.
Measures
Demographics:
Respondents completed items about age, gender, relationship status, current household income, race, ethnicity, and whether they were part of a special population (e.g., competitive athlete, veteran or active military, LGBTQ+). No specific definition of competitive athlete was provided, and all further mentions of athletes reference this designation. Frequency of suicidal thoughts over the past two weeks was also assessed with four response options: “not at all,” “several days,” “more than half the days,” and “nearly every day.” Those who endorsed any suicidal thoughts were directed to call 911 or the Crisis Call Center in the feedback portion of the screen.
Probable Diagnostic and Risk Categories and Disordered Eating Behaviors:
To determine risk and probable diagnostic category, we used the 18-item Stanford Washington-Eating Disorders Screen (SWED; Graham et al., 2018), which demonstrates good sensitivity (ranges from 0.68 for subthreshold‐BN to 0.90 for AN) and specificity (ranges from 0.79 subthreshold‐BED to 0.99 AN) for DSM-5 ED diagnoses. Responses categorized individuals using a hierarchical algorithm into one of the following diagnostic groups: (1) AN; (2) BN; (3) BED; (4) sub-threshold BN (subBN); (5) sub-threshold BED (subBED); (6) unspecified feeding or eating disorder (UFED); (7) avoidant/restrictive food intake disorder (ARFID); (8) at risk for an ED, defined as high weight and shape concerns with no other reported symptoms; or (9) no risk for an ED. Specific information on the items and diagnostic algorithm can be found elsewhere (Center for m2Health website; Graham et al., 2018). Throughout the remainder of the paper, any mention of screening positive for an ED or subthreshold ED indicates that it is a probable diagnosis. Disordered eating behaviors (binge eating and compensatory behaviors used to control weight and/or shape including vomiting, diuretic/laxative use, excessive exercise, and fasting) were also self-reported as part of the SWED. In the item text, definitions were provided for binge eating (“eating what most people would regard as an unusually large amount of food at one time with loss of control”), excessive exercise (“i.e. pushed yourself very hard; had to stick to a specific exercise schedule no matter what—for example even when you were sick/injured or if it meant missing a class or other important obligation; felt compelled to exercise”), and fasting (“intentionally not eaten anything at all for at least 24 hours in an attempt to prevent weight gain or to lose weight”).
Treatment Seeking:
Respondents indicated current treatment status by reporting either current ED treatment, prior treatment, or no treatment. After respondents completed the screen and received feedback, two optional items evaluated intention to seek treatment: “Do you intend to seek professional help and/or take any steps to address these concerns?” (response options: “definitely not,” “probably not,” “probably,” and “definitely”), followed by a checklist of treatment modalities they might pursue (e.g., medical doctor, support group). See Fitzsimmons-Craft et al. (2020) for more information on treatment seeking items.
Data Analysis
Analyses were conducted using Statistical Analysis Software (SAS) version 9.4 (2014). P-values were corrected for multiple testing using False Discovery Rate (FDR; Benjamini et al, 2001); corrected values (q-values) <.05 were considered significant. Descriptive statistics were conducted for demographic questions, disordered eating behaviors, ED diagnostic and risk categories, and current treatment status for the full sample, and for athletes and non-athletes. Sample means and standard deviations are reported for continuous and count variables. Given the large sample size, respondents with missing data were excluded for each analysis.
After Winsorizing the top .05% of the disordered eating behavior variables to account for skewed distributions (Salkind, 2010; see footnote of Table 1 for a more detailed description), we evaluated differences in mean frequencies of disordered eating behaviors (binge eating, fasting, vomiting, excessive exercise, and diuretic/laxative misuse) between athletes and non-athletes in the total sample with adjusted permutation t-tests to account for convenience sampling (see Westfall et al., 1999 and Gagne et al., 2012 for more information). To compare the likelihood of engaging in disordered eating behaviors across the two groups, we conducted logistic regressions using dichotomized versions of these variables (scored as 0 for no reported episodes in the last three months and 1 for any number of reported episodes in the last three months). Age, race, and gender were entered into models as covariates because athletes differed from non-athletes on these variables (all p’s<.01). To evaluate differences in frequencies of disordered eating behavior episodes between athletes and non-athletes, we conducted negative binomial regressions only including those who reported at least one episode of that behavior.
Table 1:
Demographic Characteristics for Athletes, Non-athletes, and the Total Samples
| Athletes n=3,509 % (n) | Non-athletes n=20,411 % (n) | Total n=23,920 % (n) | ||
|---|---|---|---|---|
| Age (years) | 13–17 | 57.3 (2,011) | 35.3 (7,196) | 38.5 (9,207) |
| 18–24 | 37.1 (1,301) | 45.3 (9,251) | 44.1 (10,552) | |
| 25–34 | 3.9 (138) | 12.0 (2,440) | 10.8 (2,578) | |
| 35–44 | 1.1 (37) | 3.7 (757) | 3.3 (794) | |
| 45–54 | 0.4 (15) | 2.1 (426) | 1.8 (441) | |
| 55–64 | 0.1 (5) | 1.3 (272) | 1.2 (277) | |
| 65+ | <0.1 (2) | 0.3 (69) | 0.3 (71) | |
| Gender | Female | 92.0 (3,227) | 90.0 (18,374) | 90.3 (21,601) |
| Male | 4.9 (171) | 4.7 (960) | 4.7 (1,131) | |
| Non-binary/third gender/prefer to self-describe | 3.1 (111) | 5.3 (1,077) | 5.0 (1,188) | |
| Race | American Indian/Alaska Native | 0.6 (21) | 0.9 (176) | 0.8 (197) |
| Asian | 3.2 (112) | 4.0 (816) | 3.9 (928) | |
| Black/African American | 1.7 (61) | 2.7 (542) | 2.5 (603) | |
| Native Hawaiian/Pacific Islander | 0.6 (20) | 0.2 48) | 0.3 (68) | |
| White | 82.9 (2,910) | 81.5 (16,644) | 81.8 (19,554) | |
| More than one race | 7.4 (259) | 5.9 (1,209) | 6.1 (1,468) | |
| Other | 3.6 (126) | 4.8 (976) | 4.6 (1,102) | |
| Annual Household Income | $0–19,999 | 13.8 (468) | 21.3 (4,191) | 20.2 (4,659) |
| $20,000–39,999 | 10.2 (344) | 16.9 (3,327) | 15.9 (3,671) | |
| $40,000–59,999 | 12.9 (437) | 15.5 (3,038) | 15.1 (3,475) | |
| $60,000–79,999 | 14.5 (492) | 13.3 (2,612) | 13.5 (3,104) | |
| $80,000–99,999 | 13.3 (450) | 9.4 (1,858) | 10.0 (2,308) | |
| $100,000–149,999 | 17.4 (589) | 12.8 (2,523) | 13.5 (3,112) | |
| $150,000+ | 17.8 (603) | 10.8 (2,118) | 11.8 (2,721) | |
| Hispanic | 9.7 (338) | 11.1 (2,253) | 10.9 (2,591) | |
| LGBTQ+ | 21.1 (739) | 26.1 (5,321) | 25.3 (6,060) | |
| Living with a Disability | 2.6 (91) | 4.0 (809) | 3.8 (900) | |
| Endorsed Any Suicidal Ideation | 50.5 (1,772) | 54.0 (11,019) | 53.5 (12,791) |
Descriptive statistics captured diagnostic and risk category frequencies for the whole sample and by athlete status. Because the SWED provides probable diagnoses, we regrouped the diagnostic categories into three outcomes: EDs/subthreshold EDs (AN, BN, BED, subBN, subBED, ARFID, PD, and UFED), at risk for an ED, and no risk for an ED. To evaluate whether identifying as an athlete was associated with ED/subthreshold ED, a chi-square test followed by a multinomial regression were conducted using the regrouped diagnostic variable, accounting for age, race, and gender.
Finally, to evaluate differences in current treatment in those with an ED/subthreshold ED by athlete status, we conducted a logistic regression using two outcomes: current treatment versus a combined no treatment or prior treatment group. We report descriptive statistics for the optional intention to seek treatment questions. These were completed by 6.3% of the sample (n=1,495), and some cell sizes had <5 participants. We also conducted an exploratory chi-square test using a combined “probably” and “definitely” group (intent to seek treatment) and combined “probably not” and “definitely not” groups (no intent to seek treatment) to compare intent to seek treatment between athletes and non-athletes.
Results
The total number of respondents who completed the screen and met inclusion criteria was 23,920. Of those, 3,509 (14.7%) identified as an athlete.
Sample Description
Table 1 presents age, gender, annual income, race, ethnicity, and endorsement of any suicidal thoughts. The mean BMI for the sample was 24.6 kg/m2 (SD = 6.5 kg/m2). Overall, the sample consisted of predominantly White females between 13–24 years old. Over half (53.5%; n=12,791) indicated they thought about suicide several days, more than half the days, or nearly every day in the past two weeks.
Aim 1 Results: Disordered Eating Behaviors and Suicidal Ideation
Table 2 presents the frequencies of Winsorized disordered eating behaviors for the entire sample, athletes, and non-athletes, and results from the adjusted permutation t-tests. Athletes reported significantly more episodes of excessive exercise (10.97 versus 5.46) and fewer episodes of binge eating (8.38 versus 9.91) and diuretic/laxative use (1.37 versus 1.82) over the past three months than non-athletes.
Table 2:
Means of Disordered Eating Behaviors Episodes Over the Previous 3 Months for Total Sample, Athletes, and Non-Athletes, and Results from T-Test with Adjusted Permutations Q-Values.
| Total Sample | Results from T-Test with Adjusted Permutation Q-Values | ||||||
|---|---|---|---|---|---|---|---|
| Disordered Eating (DE) Behavior | Mean (SD) | Range | Respondents Reporting at least 1 Episode of DE Behavior % (n) | Athlete Mean (SD) | Non-athlete Mean (SD) | t-value | q-value |
| Binge Eating | 9.69 (18.72) | 0–270 | 74.85 (17,903) | 8.38 (16.44) | 9.91 (19.08) | 4.46 | <.001 |
| Vomiting | 3.41 (15.01) | 0–300 | 26.05 (6,231) | 3.08 (13.04) | 3.47 (15.32) | 1.39 | .211 |
| Diuretics/Laxatives | 1.76 (8.50) | 0–170 | 16.95 (4,053) | 1.37 (7.03) | 1.82 (8.72) | 2.92 | .006 |
| Excessive Exercise | 6.27 (14.97) | 0–150 | 48.52 (11,596) | 10.97 (19.59) | 5.46 (13.86) | 20.27 | <.001 |
| Fasting | 5.21 (12.58) | 0–150 | 50.70 (12,068) | 5.17 (12.54) | 5.23 (12.58) | 0.24 | .826 |
q-values (p-values adjusted for multiple tests using False Discovery Rate correction and, in this case, were adjusted using permutation methods) and associated means (SDs) that are bolded are significant results.
All means, SDs, and ranges represent sample after using Winsorizing technique where data points above >3 SDs are converted to the value at 3 SD above the mean, thereby limiting the effects of spurious outliers. Given skewed data distributions and a large portion of the sample reporting 0 episodes for each disordered eating behavior, we used the mean and SDs for the subset of respondents who reported at least 1 episode of the respective behavior and converted the data points above 3 SDs to equal the highest data point not considered an outlier.
Table 3 presents results from the logistic regression models for each dichotomized disordered eating behavior. Identifying as an athlete was significantly associated with an increased likelihood of engaging in excessive exercise (q<.001) and a decreased likelihood of engaging in binge eating (q<.001) and fasting (q<.001), accounting for age, gender, and race. No significant difference between athletes and non-athletes was observed for vomiting and diuretic/laxative use.
Table 3:
Logistic Regression and Negative Binomial Regression Models Comparing Athletes and Non-athletes Across Disordered Eating Engagement and Episode Frequency
| Logistic Regression Model | Negative Binomial Regression Model* | |||||
|---|---|---|---|---|---|---|
| Disordered Eating Behavior | Sample Size (n missing) | Odds Ratio [95% CI] | q-value | Sample Size Reporting at Least 1 Episode in Past 3 Months | Incidence Rate Ratio [95% CI] | q-value |
| Binge Eating | 23,920 (0) | 0.85 [0.78, 0.92] | <.001 | 17,903 | 0.91 [0.87, 0.95] | <.001 |
| Vomiting | 23,920 (0) | 0.92 [0.84, 1.00] | .071 | 6,231 | 0.97 [0.88, 1.06] | 0.545 |
| Diuretics/Laxatives | 23,907 (13) | 0.97 [0.87, 1.07] | .545 | 4,053 | 0.91 [0.82, 1.02] | .140 |
| Excessive Exercise | 23,899 (21) | 2.30 [2.13, 2.49] | <.001 | 11,596 | 1.40 [1.32, 1.47] | <.001 |
| Fasting | 23,805 (115) | 0.78 [0.73, 0.85] | <.001 | 12,068 | 0.99 [0.94, 1.05] | .826 |
q-values and associated odds ratios or parameter estimates that are bolded are significant results after FDR corrections.
Negative binomial regression models only included the subset of the sample that reported at least 1 episode of the respective disordered eating behavior. Therefore, there were no missing data in each negative binomial regression model.
df=degrees of freedom, CI= Confidence Interval
Table 3 also presents results for the negative binomial regression models illustrating differences in frequencies of disordered eating behaviors between athletes and non-athletes who reported at least one episode of the respective behavior over the past three months. Identifying as an athlete was significantly associated with more frequent episodes of excessive exercise and less frequent episodes of binge eating after accounting for age, gender, and race. More specifically, athletes engaging in binge-eating report 10% fewer episodes than non-athletes, accounting for age, race, and gender. Similarly, athletes engaging in excessive exercise report 40% more frequent episodes than non-athletes, accounting for age, race, and gender.
Although suicidal ideation was frequent in both groups, significantly fewer athletes (50.5%) reported any suicidal ideation compared to non-athletes (54.0%), χ2(3, N=23,920) = 15.72, q=.003.
Aim 2 Results: Diagnostic and Risk Categories
Table 4 presents the results of diagnostic and risk categories for the entire sample, athletes, and non-athletes. Over 86% of the total sample screened positive for an ED/subthreshold ED. The distribution across diagnostic and risk categories was similar in athletes and non-athletes; the greatest percentage difference was in for athletes (7.5%) and non-athletes (10.4%) who were at risk for an ED.
Table 4:
Percentage (n) of the Total Sample, Athletes and Non-Athletes in Each Diagnostic and Risk Category
| Probable Diagnosis/Risk Category | Total % (n) | Athletes % (n) | Non-Athletes % (n) |
|---|---|---|---|
| Any ED | 86.7 (20,727) | 88.8 (3,116) | 86.3 (17,611) |
| AN | 5.6 (1,338) | 6.5 (227) | 5.4 (1,111) |
| BN | 8.8 (2,121) | 9.2 (322) | 8.8 (1,799) |
| BED | 3.1 (758) | 1.7 (60) | 3.4 (698) |
| Subthreshold BN | 26.9 (6,427) | 28.9 (1,013) | 26.5 (5,414) |
| Subthreshold BED | 4.5 (1,071) | 3.3 (115) | 4.7 (956) |
| PD | 1.2 (280) | 1.0 (37) | 1.2 (243) |
| Unspecified ED | 31.4 (7,515) | 33.6 (1,179) | 31.0 (6,336) |
| ARFID | 5.2 (1,217) | 4.6 (163) | 5.2 (1,054) |
| At risk | 9.9 (2,376) | 7.5 (264) | 10.4 (2,112) |
| No risk | 3.4 (817) | 3.7 (129) | 3.4 (688) |
AN = anorexia nervosa; BN = bulimia nervosa; BED = binge-eating disorder; PD = purging disorder; ARFID = avoidant/restrictive food intake disorder.
The diagnostic and risk categories are listed in a hierarchical manner with AN at the top and no risk at the bottom; respondents were assigned to one diagnostic/risk category based on their reported symptoms.
There was a significant difference between athletes and non-athletes in the distribution across the regrouped diagnostic categories, χ2(2, N=23,920) = 27.05, q<.001. There was a significant difference between athletes and non-athletes in the distribution across the regrouped diagnostic categories from the multinomial regression model, χ2(2, N=23,920) = 27.05, q<.001. Post-hoc pairwise comparisons provided additional information on the sample diagnostic characteristics. When comparing ED/subthreshold ED and at-risk groups to the no risk group (the referent), results indicate that athletes had 30% fewer positive screens for an ED/subthreshold ED (q<.001) and 40% fewer positive screens for at-risk (q<.001) than non-athletes. When comparing ED/subthreshold ED group to the at-risk group (the referent), athletes had 18% more positive screens for an ED/subthreshold ED than non-athletes (q=.030).
Aim 3 Results: Treatment History and Intent to Seek Treatment
In the total sample, 2.3% had received prior ED treatment, 9.8% were currently in treatment, and 87.9% had not received any treatment for an ED. Figure 1 presents the treatment status for all respondents, athletes, and non-athletes who screened positive for an ED/subthreshold ED. Identifying as an athlete was not associated with current treatment status (q=.094).
Figure 1:
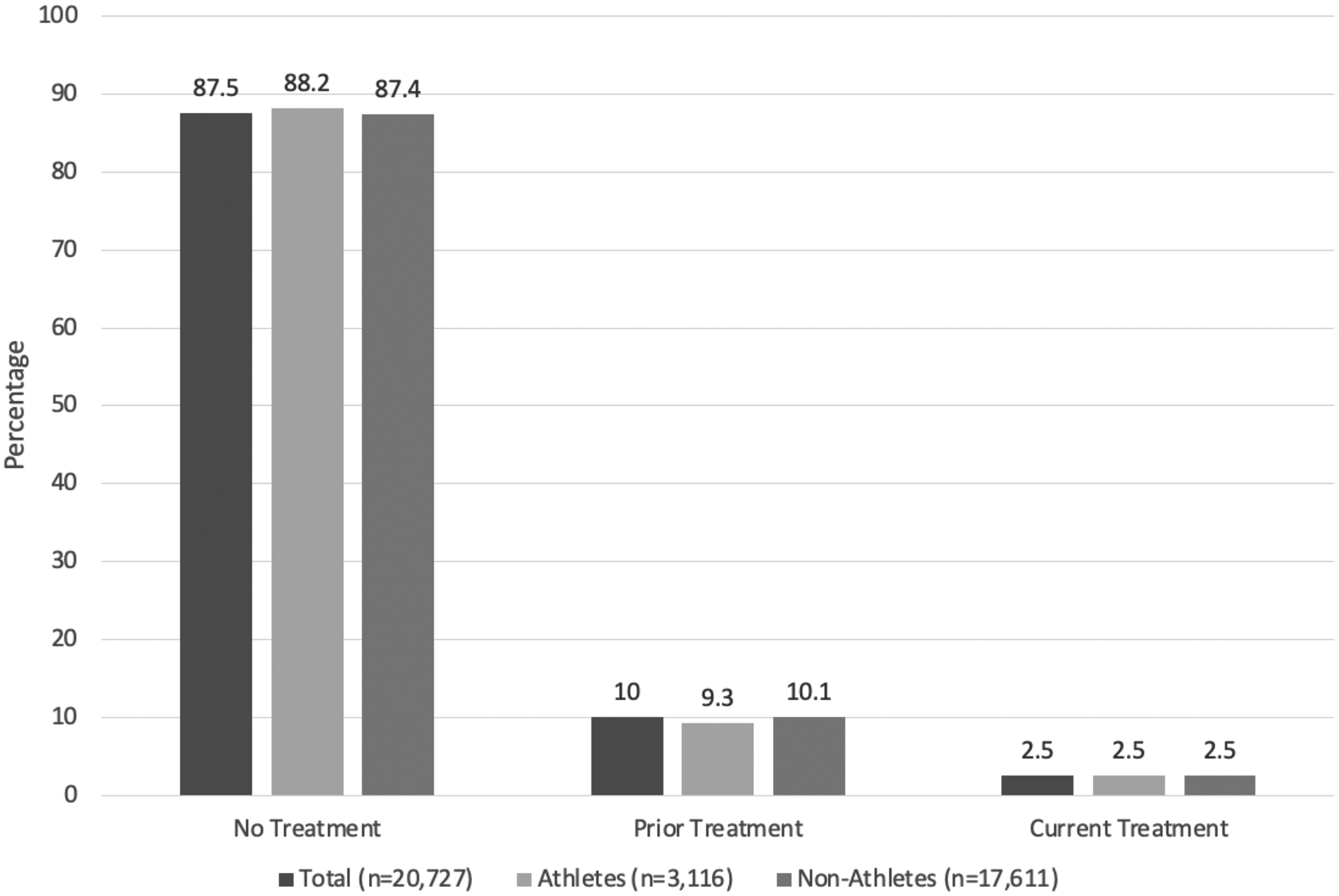
Treatment Status for Athletes and Non-Athletes who Screened Positive for an Eating Disorder/Subthreshold Eating Disorder
Finally, we reviewed intentions to seek treatment and preferred treatment modalities after respondents received tailored feedback. Of the 20,727 respondents who screened positive for an ED/subthreshold ED, 1,383 (168 were athletes) completed the optional questions. Figure 2 illustrates the distribution of intention to seek treatment for individuals who screened positive for an ED/subthreshold ED, athletes, and non-athletes. After receiving feedback based on their probable diagnosis, 78.0% of athletes and 71.0% of non-athletes reported that they would “probably not” or “definitely not” seek treatment; the difference was not statistically significant, χ2(1, N=1,383) = 3.91, q=.332.
Figure 2:
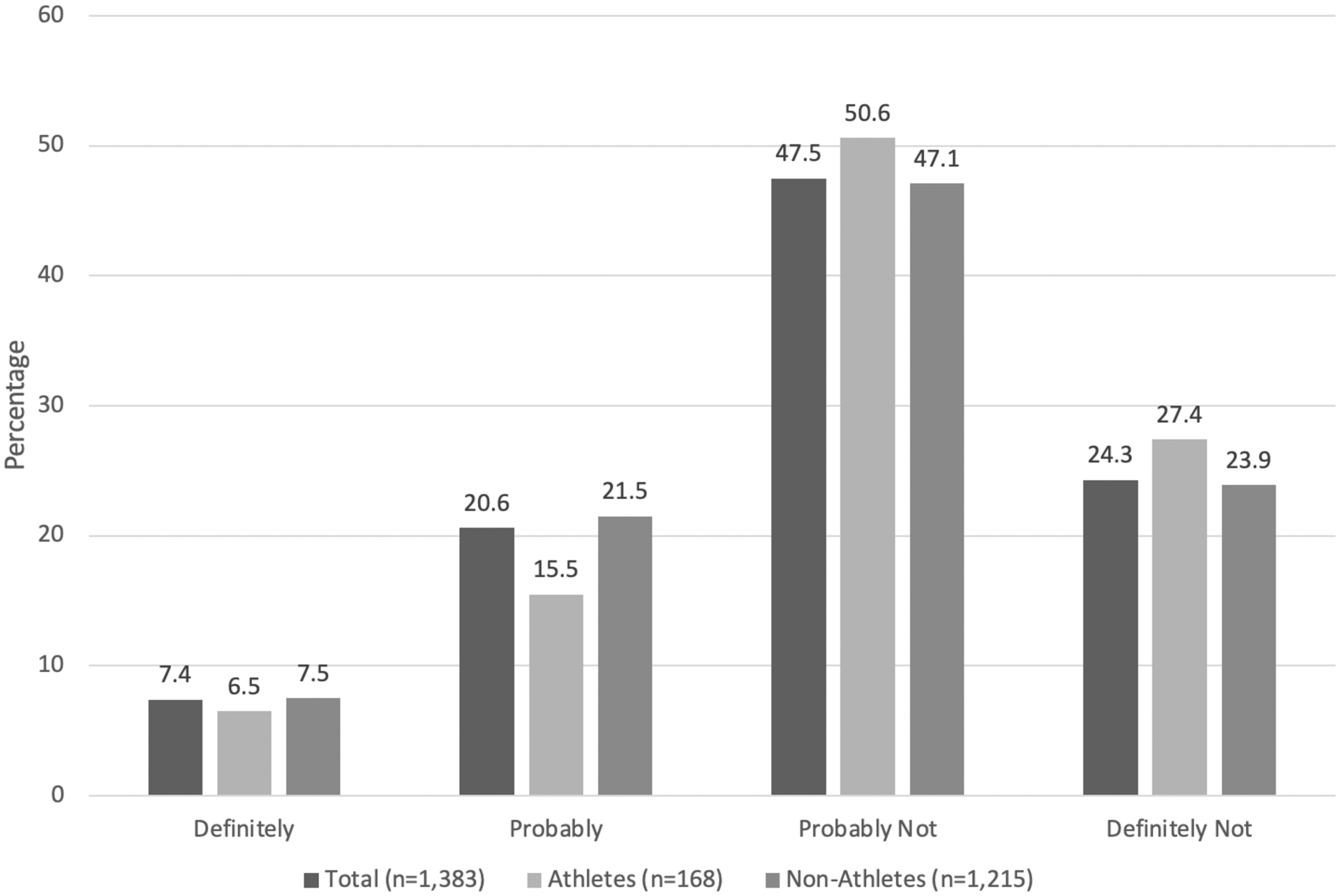
Histogram of Responses for Intention to Seek Future Treatment for Individuals who Screened Positive for an Eating Disorder or Subthreshold Eating Disorder
Table 5 provides descriptive results on treatment modalities for athletes and non-athletes who screened positive for an ED/subthreshold ED and completed the item on intention to seek treatment. Generally, respondents who indicated they were likely to seek treatment reported they would seek help from a mental health professional or a medical doctor.
Table 5:
Percentage (n) of Intended Treatment Modalities for Athletes and Non-Athletes who Screened Positive for an Eating Disorder or Subthreshold Eating Disorder
| All who responded to intention to seek treatment item (n=1,383) | All who responded “probably” or “definitely” to intention to seek treatment item (n=390) | |||
|---|---|---|---|---|
| Treatment Modality | Athletes % (n) n=168 | Non-Athletes % (n) n=1,215 | Athletes % (n) n=37 | Non-Athletes % (n) n=353 |
| Mental health professional | 19.6 (33) | 19.4 (236) | 64.9 (24) | 52.4 (185) |
| Medical doctor | 7.7 (13) | 10.5 (127) | 21.6 (8) | 28.3 (100) |
| NEDA helpline | 1.2 (2) | 4.0 (49) | 2.7 (1) | 9.9 (35) |
| Online program | 6.6 (11) | 6.8 (82) | 13.5 (5) | 11.6 (41) |
| Support group | 3.6 (6) | 5.6 (68) | 13.5 (5) | 13.9 (49) |
| Other | 7.1 (12) | 5.9 (72) | 5.4 (2) | 6.8 (24) |
Discussion
The current study reached a large sample of community-based, self-identified competitive athletes using an online ED screening tool. Individuals who took the screen clearly had a reason to be interested in EDs as only 3.4% of respondents screened at the no risk level and should be considered when interpreting results.
Disordered Eating Behaviors and Suicidal Ideation
Binge eating was the most common disordered eating behavior reported (approximately 75% reported at least one episode in the previous three months). The mean number of binge episodes was lower for athletes than non-athletes, and identifying as an athlete was associated with a reduced likelihood and frequency of binge eating. Previous studies have reported higher frequencies of binge eating in athletes than non-athletes, particularly at higher levels of competition (Holm-Denoma et al., 2009) and in sports emphasizing leanness (Thompson & Sherman, 2010); however, others concurred with our findings suggesting less frequent binge eating (e.g., Fortes et al., 2014). More detailed descriptions of athletes’ sport and level of competition may help reconcile these observations in future studies.
Excessive exercise and fasting were the most common compensatory behaviors, with approximately 50% engaging in these behaviors at least once over the previous three months. Athletes reported almost double the number of excessive exercise episodes as non-athletes, and they had a greater likelihood and frequency of excessive exercise episodes. Excessive exercise may be more frequent in athletes given their regular training regimens and, in some cases, to meet weight class requirements or improve aesthetics for judged sports. They may also be more likely to endorse excessive exercise due to social desirability or positive reinforcement from coaches, teammates, and support staff, which in turn may reduce treatment seeking if excessive exercise is mischaracterized or applauded. Of note, the definition of excessive exercise in the SWED, although generally accepted by researchers and clinicians, may be problematic for athletes who often train in spite of illness or injury. Several terms are used to describe maladaptive exercise, (e.g., exercise dependence, compulsive or excessive exercise), reflecting differences in conceptualizations and symptom presentations (e.g., Adkins & Keel, 2005; Scharmer et al., 2020). Thus, it is important that future studies clearly highlight the intent of the exercise and differentiate maladaptive exercise as part of ED psychopathology from an athlete’s training regimen.
Athletes also reported reduced likelihood of engaging in fasting than non-athletes. Findings are consistent with literature suggesting more weight control methods in non-athletes through fasting, vomiting, and diuretic/laxative to improve appearance rather than performance (Martinsen, Bratland-Sanda, Eriksson, & Sundgot-Borgen, 2010; Werner et al., 2013). The negative effects of energy deficit sport performance may reduce the likelihood of athletes engaging in these behaviors. Athletes also reported fewer mean diuretic/laxative use episodes, possibly due to the negative impacts such medications may have on nutrient uptake, energy levels, and sport performance. Although results were significant, the small difference found may not be clinically meaningful.
Finally, unexpectedly, over 50% of the sample endorsed suicidal ideation, with fewer athletes reporting any suicidal ideation than non-athletes. Despite several studies reporting associations between EDs and suicidal ideation (Franko & Keel, 2006; Pisetsky et al., 2013; Runfola et al., 2014; Yao et al., 2016), the extent to which the current sample reported suicidal ideation was much higher, underscoring the severity of illness for those completing the NEDA screen and the need for combined ED and suicide prevention and intervention for athletes and non-athletes alike.
Diagnostic and Risk Categories
The sample demonstrated a high frequency of probable and subthreshold EDs, in keeping with prior publications on the NEDA screen (Fitzsimmons-Craft et al., 2019). Significant differences emerged between athletes and non-athletes across ED diagnostic and risk categories, with the greatest difference in the at risk for an ED group. Athletes demonstrated a higher likelihood of a probable ED/subthreshold ED mirroring prior research (e.g., Thompson & Sherman 2010), and treatments and prognoses may differ across athletes and non-athletes considering the varying symptom presentations and risk and maintenance factors unique to each group. However, the small differences in ED diagnostic frequencies observed in this sample may be less clinically relevant than the more concerning observations that over half the sample reported suicidal ideation and almost 90% of the sample screened positive for an ED/subthreshold ED.
Treatment History and Intention to Seek Treatment
The number of respondents who reported current treatment who also screened positive for an ED/subthreshold ED was very low. Although intention to seek treatment did not differ between athletes and non-athletes, over 75% of athletes who received feedback about a probable ED or subthreshold ED reported no intention to seek treatment. This underscores the importance of increasing education about EDs, evaluating readiness to change and motivation, and improving treatment accessibility.
Taken together, athletes and non-athletes from the community who completed the NEDA screen generally had comparable frequencies of EDs, despite significant differences across grouped diagnostic and risk categories. Similarly, significant differences existed both in the likelihood and frequency of disordered eating behaviors, suggesting that ED profiles differ slightly between athletes and non-athletes; however, this is overshadowed by how few athletes and non-athletes were in treatment (or intended to seek treatment) despite the presence of both eating pathology and suicidal ideation. Fewer athletes were inclined to seek treatment after the screen, possibly reflecting reticence due to stigma, prioritizing performance over health, and/or lack of availability of and access to resources, among other potential barriers to treatment.
Strengths and Limitations
Strengths of the current study included large sample size and reach capturing many individuals with an ED/subthreshold ED. The screen was brief, confidential, and free, thus reducing potential barriers to information seeking. The screen was delivered by NEDA—a prominent and trusted ED advocacy organization—potentially providing a safe outlet to explore one’s risk for an ED.
Limitations include self-identification as an athlete rather than a specific definition. Although this was intentional to reach as many athletes as possible, we were unable to characterize level of athletic engagement. Future studies should include more questions for the athlete respondents (e.g., current level of competition, sport, average hours of training per week, etc.) to further characterize this group. Bot responses may have been inadvertently included. However, we excluded observations when values were extreme (often consistent with bot responses, <2% of original raw data), so the number of bot responses included were likely low. Respondents could also complete the survey more than once. A response authenticator could reduce the likelihood of including both bot responses and repeat observations in future implementations. The large sample size suggests that some tests that reached significance could be overpowered, despite correcting for skewed distributions and multiple tests. Finally, the percentage of the sample that completed the optional intent to seek treatment and treatment modality items was quite small.
Future Directions
Tracking treatment uptake after screen completion in athletes will provide critical information for streamlining community-based screens and facilitating treatment seeking. Given that three-quarters of respondents did not seek treatment two months following completion of the NEDA screen (Fitzsimmons-Craft et al., 2020), future uses of the screen may include increasing education and motivation for behavioral change and pairing respondents with immediate access to providers and tailored programs based on their ED presentation, a strategy of significant value for community-based athletes without direct access to providers through school-based athletic departments, professional teams, or sport governing bodies. Additionally, using screens to assess individuals from target populations, like athletes, and including measures developed specifically for such populations (e.g., the Eating Disorders Screen for Athletes; Hazzard et al., 2020) will provide opportunities to tailor ED prevention and treatment programs to their unique needs. Over 95% of athletes and non-athletes with an ED/subthreshold ED were not in treatment at the time of screening. Thus, it is imperative we improve access to evidence-based care, engage with respondents of online ED screens to directly connect them to resources and treatment options, and use study results to tailor care for unique populations including athletes.
Acknowledgements:
The authors would especially like to thank the National Eating Disorders Association and their staff for their generosity, support, and contributions to the screening tool. We would also like to thank all respondents and the research team for their time and dedication to this study. RF is supported by the National Science Foundation Graduate Research Fellowship Program under Grant No. (DGE-1650116). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation. CB acknowledges funding from the Swedish Research Council (Vetenskapsrådet, award: 538-2013-8864) and from the National Institutes of Health (R01 MH120170 and R01 MH119084). This work was supported by R01 MH100455, K08 MH120341, and K01 DK120778.
Conflict of Interest Statement:
Claire Mysko and Lauren Smolar both work for the National Eating Disorders Association as CEO and as Senior Director of Programs, respectively. CM Bulik reports: Shire (grant recipient, Scientific Advisory Board member); Idorsia (consultant); Pearson (author, royalty recipient). No other authors have conflicts to disclose.
Footnotes
Data Availability Statement:
Data for the current study are available upon request.
References
- Adkins EC, & Keel PK (2005). Does “excessive” or “compulsive” best describe exercise as a symptom of bulimia nervosa? International Journal of Eating Disorders, 38(1), 24–29. [DOI] [PubMed] [Google Scholar]
- Alwan N, Moss SL, Elliott-Sale KJ, Davies IG, & Enright K (2019). A Narrative Review on Female Physique Athletes: The Physiological and Psychological Implications of Weight Management Practices. International Journal of Sport Nutrition and Exercise Metabolism, 1–8. Advance online publication. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA. [Google Scholar]
- Benjamini Y, Drai D, Elmer G, Kafkafi N, Golani I (2001). Controlling the false discovery rate in behavior genetics research. Behavioral Brain Research, 125(1–2), 279–84. [DOI] [PubMed] [Google Scholar]
- Biesecker AC, & Martz DM (1999). Impact of coaching style on vulnerability for eating disorders: an analog study. Eating Disorders, 7(3), 235–244. [Google Scholar]
- Bratland-Sanda S, & Sundgot-Borgen J (2013). Eating disorders in athletes: Overview of prevalence, risk factors and recommendations for prevention and treatment. European Journal of Sport Science, 13(5), 499–508. [DOI] [PubMed] [Google Scholar]
- Brown GT, Hailine B, Kroshus E, Wilfert M (2014). Mind, body and sport: understanding and supporting student-athlete mental wellness. National Collegiate Athletic Association, Indianapolis, IN. [Google Scholar]
- Byrne S, & McLean N (2002). Elite athletes: effects of the pressure to be thin. Journal of Science and Medicine in Sport, 5, 80–94. [DOI] [PubMed] [Google Scholar]
- Chapman J, & Woodman T (2016). Disordered eating in male athletes: a meta-analysis. Journal of Sports Sciences, 34(2), 101–109. [DOI] [PubMed] [Google Scholar]
- Currie A (2010). Sport and eating disorders: Understanding and managing the risks. Asian Journal of Sports Medicine, 1(2), 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D, Downs MF, Golberstein E, & Zivin K (2009). Stigma and help seeking college students. Medical Care Research and Review, 66(5), 522–541. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Nicklett EJ, Roeder K, & Kirz NE (2011). Eating disorder symptoms among college students: prevalence, persistence, correlates, and treatment-seeking. Journal of American College Health, 59(8), 700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Ghoch M, Soave F, Calugi S, & Dalle Grave R (2013). Eating disorders, physical fitness and sport performance: a systematic review. Nutrients, 5(12), 5140–5160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Balantekin KN, Graham AK, Smolar L, Park D, Mysko C, … Wilfley DE (2019). Results of disseminating an online screen for eating disorders across the U.S.: Reach, respondent characteristics, and unmet treatment need. International Journal of Eating Disorders, 52(6), 721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Balantekin KN, Graham AK, DePietro B, Laing O, Firebaugh M, Smolar L, Park D, Mysko C, Funk B, Taylor CB, & Wilfley DE (2020). Preliminary data on help-seeking intentions and behaviors of individuals completing a widely available online screen for eating disorders in the U.S. International Journal of Eating Disorders, 53(9), 1556–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg S, & Lock J (2006). The relationship between perfectionism, eating disorders and athletes: a review. Minerva Pediatrica, 58(6), 525–36. [PubMed] [Google Scholar]
- Fortes L, Kakeshita IS, Almeida SS, Gomes AR, & Ferreira ME (2014). Eating behaviours in youths: A comparison between female and male athletes and non-athletes. Scandinavian Journal of Medicine & Science in Sports, 24(1), e62–e68. [DOI] [PubMed] [Google Scholar]
- Franko DL, & Keel PK (2006). Suicidality in eating disorders: Occurrence, correlates, and clinical implications. Clinical Psychology Review, 6, 769–782. [DOI] [PubMed] [Google Scholar]
- Franko D, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, et al. (2013). A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. American Journal of Psychiatry, 170(8), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagne DA, Von Holle A, Brownley KA, Runfola CD, Hofmeier S, Branch KE, & Bulik CM (2012). Eating disorder symptoms and weight and shape concerns in a large web-based convenience sample of women ages 50 and above: results of the Gender and Body Image (GABI) study. International Journal of Eating Disorders, 45(7), 832–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AK, Trockel M, Weisman H, Fitzsimmons-Craft EE, Balantekin KN, Wilfley DE, & Taylor CB (2018). A screening tool for detecting eating disorder risk and diagnostic symptoms among college-age women. Journal of American College Health, 67(4), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratwick-Sarll K, Mond J, & Hay P (2013). Self-recognition of eating-disordered behavior in college women: further evidence of poor eating disorders “mental health literacy”? Eating Disorders, 21(4), 310–327. [DOI] [PubMed] [Google Scholar]
- Greenleaf C, Petrie TA, Carter J, & Reel JJ (2009). Female collegiate athletes: prevalence of eating disorders and disordered eating behaviors. Journal of American College Health, 57(5), 489–496. [DOI] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, & Christensen H (2012). Barriers and facilitators to mental health help-seeking for young elite athletes: a qualitative study. BMC Psychiatry, 12(1), 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazzard V, Schaefer L, Mankowski A, Carson T Lipson S, Fendrick C, & Crosby R, & Sonneville K (2020). Development and validation of the Eating Disorders Screen for Athletes (EDSA): A brief screening tool for male and female athletes. Psychology of Sport and Exercise, 50, 101745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm-Denoma JM, Scaringi V, Gordon KH, Van Orden KA, & Joiner TE (2009). Eating disorder symptoms among undergraduate varsity athletes, club athletes, independent exercisers, and nonexercisers. International Journal of Eating Disorders, 42(1), 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19–65. [DOI] [PubMed] [Google Scholar]
- Johnson C, Powers PS, & Dick R (1999). Athletes and eating disorders: the National Collegiate Athletic Association study. International Journal of Eating Disorders, 26(2), 179–188. [DOI] [PubMed] [Google Scholar]
- Joy E, Kussman A, & Nattiv A (2016). 2016 update on eating disorders in athletes: A comprehensive narrative review with a focus on clinical assessment and management. British Journal of Sports Medicine, 50(3), 154–162. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Fitzsimmons-Craft EE, & Wilfley DE (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50(3), 170–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs PA, Dennison CR, Kellar L, & Lucas J (2019). Gender differences in eating disorder risk among NCAA Division I cross country and track student-athletes. Journal of Sports Medicine, 5035871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López RL, & Levy JJ (2013). Student athletes’ perceived barriers to and preferences for seeking counseling. Journal of College Counseling, 16(1), 19–31. [Google Scholar]
- Martinsen M, Bratland-Sanda S, Eriksson AK & Sundgot-Borgen Jorunn. (2010). Dieting to win or to thin? A study of dieting and disordered eating among adolescent elite athletes and non-athlete controls. British Journal of Sports Medicine, 44, 70–6. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, … Kessler RC (2011). Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychological Medicine, 41(8), 1751–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond J, Hay P, Rodgers B, & Owen C (2006). Self-recognition of disordered eating among women with bulimic-type eating disorders: A community-based study. International Journal of Eating Disorders, 39(8), 747–753. [DOI] [PubMed] [Google Scholar]
- Mountjoy M, Sundgot‐Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. (2014). The IOC consensus statement: Beyond the Female Athlete Triad—Relative energy deficiency in sport. British Journal of Sports Medicine, 48(7), 491–497. [DOI] [PubMed] [Google Scholar]
- Palermo M, & Rancourt D (2019). An identity mis-match? The impact of self-reported competition level on the association between athletic identity and disordered eating behaviors. Eating Behaviors, 35, 101341. [DOI] [PubMed] [Google Scholar]
- Pisetsky EM, Thornton LM, Lichtenstein P, Pedersen NL, & Bulik CM (2013). Suicide attempts in women with eating disorders. Journal of Abnormal Psychology, 122(4), 1042–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon CL, & Factor RM (2010). Sport Psychiatry: a systematic review of diagnosis and medical treatment of mental illness in athletes. Sports Medicine, 40(11), 961–980. [DOI] [PubMed] [Google Scholar]
- Rodriguez NR, Di Marco NM, & Langley S (2009). American College of Sports Medicine position stand. Nutrition and athletic performance. Medicine & Science in Sports Exercise, 41(3), 709–731. [DOI] [PubMed] [Google Scholar]
- Rosen DS, American Academy of Pediatrics Committee on Adolescence (2010). Identification and management of eating disorders in children and adolescence. Pediatrics, 126, 1240–53. [DOI] [PubMed] [Google Scholar]
- Runfola CD, Thornton LM, Pisetsky EM, Bulik CM, & Birgegård A (2014). Self-image and suicide in a Swedish national eating disorders clinical register. Comprehensive Psychiatry, 55(3), 439–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkind NJ (2010). Encyclopedia of Research Design (Vols. 1–0, pp. 181–186). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- SAS [computer program]. (2014). Version 9.4. Cary, NC: SAS Institute Inc. [Google Scholar]
- Scharmer C, Gorrell S, Schaumberg K, & Anderson D (2020). Compulsive exercise or exercise dependence? Clarifying conceptualizations of exercise in the context of eating disorder pathology. Psychology of Sport and Exercise, 46, 101586. [PMC free article] [PubMed] [Google Scholar]
- Smink FRE, van Hoeken D, & Hoek HW (2012). Epidemiology of eating disorders: incidence, prevalence and mortality rates. Current Psychiatry Reports, 14(4), 406–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, & Bulik CM (2007). Risk factors for eating disorders. American Psychologist, 62(3), 181–198. [DOI] [PubMed] [Google Scholar]
- Sundgot-Borgen J (1994). Risk and trigger factors for the development of eating disorders in female elite athletes. Medicine and Science in Sports and Exercise, 26(4), 414–9. [PubMed] [Google Scholar]
- Sundgot-Borgen J (1993). Prevalence of eating disorders in elite female athletes. International Journal of Sport Nutrition, 3(1), 29–40. [DOI] [PubMed] [Google Scholar]
- Sundgot-Borgen J, & Torstveit MK (2004). Prevalence of eating disorders in elite athletes is higher than in the general population. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine, 14(1), 25–32. [DOI] [PubMed] [Google Scholar]
- Thein-Nissenbaum JM, & Carr KE (2011). Female athlete triad syndrome in the high school athlete. Physical Therapy in Sport, 12(3), 108–116. [DOI] [PubMed] [Google Scholar]
- Thompson RA, & Sherman RT (2010). Eating Disorders in Sport. New York, NY: Routledge. [Google Scholar]
- Thompson RA, & Sherman RT (1999). “Good athlete” traits and characteristics of anorexia nervosa: are they similar? Eating Disorders, 7(3), 181–190. [Google Scholar]
- Torstveit MK, Rosenvinge JH, & Sundgot-Borgen J (2008). Prevalence of eating disorders and the predictive power of risk models in female elite athletes: A Controlled Study. Scandinavian Journal of Medicine & Science in Sports, 18(1), 108–118. [DOI] [PubMed] [Google Scholar]
- Werner A, Thiel A, Schneider S, Mayer J, Giel KE, & Zipfel S (2013). Weight-control behaviour and weight-concerns in young elite athletes - a systematic review. Journal of Eating Disorders, 1, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westfall PHTR, Rom D, Wolfinger RD, Hochberg Y (1999). Multiple comparisons and multiple tests using the SAS system, p. 416. SAS Institute Inc.; Cary, NC. [Google Scholar]
- Yao S, Kuja-Halkola R, Thornton LM, Runfola CD, D’Onofrio BM, Almqvist C, … Bulik CM (2016). Familial liability for eating disorders and suicide attempts evidence from a population registry in Sweden. JAMA Psychiatry, 73(3), 284–291. [DOI] [PubMed] [Google Scholar]


