Abstract
Background:
Maternal nutrition during pregnancy has a significant effect on the health of the offspring and mother, highlighting the need for identifying factors that may impact diet during pregnancy. Research in non-pregnant and pregnant populations suggest depression may play a role.
Objective:
Investigate the relationship between prenatal depression and diet quality during pregnancy overall and by race/ethnicity and explore the relationships between prenatal depression and the 12 Healthy Eating Index (HEI-2010) dietary components.
Design:
A cross-sectional secondary analysis of a cohort study of Kaiser Permanente Northern California women entering prenatal care between October 2011 and April 2013.
Participants/setting:
Participants included 1,160 adult pregnant women.
Main outcome measures:
Poor diet quality was defined as a HEI-2010 score in the lowest quartile.
Statistical analyses performed:
Logistic regression was used to assess the relationship between prenatal depression (defined as a depression diagnosis, PHQ-9 score of 10 or greater or antidepressant medication dispensing between the last menstrual period and completion of the FFQ) and poor diet quality overall and by race/ethnicity. T-tests and linear regression analyses were used to assess the relationships between prenatal depression and each of the 12 HEI-2010 dietary components.
Results:
159 (14%) of the participants had prenatal depression. Women with prenatal depression had nearly two times the odds of poor diet quality (OR:1.80;95%CI:1.23,2.60) compared to women without prenatal depression, after adjusting for potential confounders. Differences emerged by race/ethnicity; after adjusting for potential confounders the adjusted odds of poor diet quality were significant only among Hispanic women. Hispanic women with prenatal depression had an increased odds of poor diet quality compared to Hispanic women without prenatal depression (OR:2.66, 95%CI:1.15,6.06). Women with prenatal depression had a higher consumption of empty calories (from solid fats, alcohol, and added sugars; threshold for counting alcohol is greater than 13g/1,000 kcal ) (p=0.01) and lower consumption of greens and beans (p<0.05), total fruit (p<0.01), and whole fruit (p<0.01), compared to women without prenatal depression. Except for empty calories, these findings remained after adjusting for potential confounders.
Conclusions:
Study findings suggest that women with prenatal depression are at a higher risk of poor diet quality compared to women without prenatal depression, and the relationship is stronger among Hispanic women. Nutritional counseling interventions for women with depression should consider the use of culturally sensitive material and target limiting empty calories from solid fats, alcohol, and added sugars and encouraging eating more greens, beans and fruit.
Keywords: perinatal depression, diet quality, racial/ethnic disparities, dietary intake, Healthy Eating Index (HEI-2010)
INTRODUCTION
Maternal nutrition during pregnancy has a significant impact on fetal growth and development, as well as the woman’s health status during and after pregnancy. Both under- or over-nutrition during pregnancy is associated with poor long-term health outcomes of the offspring in childhood and adulthood, including metabolic disease and obesity1-4. A poor quality diet during pregnancy may also compromise maternal health by promoting obesity5,6, excessive gestational weight gain7 and postpartum weight retention8.
The assessment of overall diet quality has garnered attention because it considers the complex synergistic effect of food and nutrients rather than individual items. Index scores such as the Healthy Eating Index (HEI) - 20109 are often used to assess overall diet quality. The HEI-2010 measures conformance to the 2010 Dietary Guidelines for Americans (2010 DGAs)10 jointly published by the United States Department of Agriculture (USDA) and Department of Health and Human Services. Healthy eating patterns that are consistent with the 2010 DGAs emphasize fruits, vegetables, whole grains, fat-free/low fat milk and milk products, seafood, lean meats and poultry, eggs, beans and peas, and nuts and seeds while limiting intake of sodium, solid fats, added sugars, and refined grains10. Disparities in diet quality by race/ethnicity have been documented in the US among both non-pregnant11 and pregnant women12; specifically, suboptimal diet quality is more common among pregnant Hispanics and non-Hispanic Blacks.
Little is known about factors that may impact diet quality during pregnancy, but the nascent literature in both non-pregnant and pregnant populations suggests depression may play a role. Prenatal depression impacts up to 22% of pregnant women13,14 with higher rates in racial/ethnic minorities. An inverse relationship between prenatal depression and diet quality in low-income pregnant women has been suggested, such that women with prenatal depression reported a low-quality diet during pregnancy15. However, the research in pregnant populations is limited. Similar findings have also emerged in studies of non-pregnant populations 16,17.
The impact that maternal nutrition has on the long-term health of both the offspring and the mother highlights the need for a greater understanding of factors that may impact diet quality during pregnancy. If prenatal depression is related to poor diet quality, it will provide information for targeted interventions. Further, understanding differences in the individual HEI-2010 components may provide important information for dietary guidance. Thus, the purpose of this study was to investigate the differences in overall diet quality during pregnancy between women with and without prenatal depression and whether this relationship differs by race/ethnicity. Additionally, this study aimed to examine relationships between prenatal depression and the twelve individual HEI-2010 components in a cohort of pregnant women.
MATERIALS AND METHODS
Study Setting
The study setting was Kaiser Permanente Northern California (KPNC), a large group practice prepaid health plan that provides comprehensive medical services to members living in a 14-county region of Northern California (approximately 30% of the surrounding population). The demographic, racial/ethnic, and socioeconomic characteristics of the KPNC membership are representative of the population residing in the same geographic area except that the very poor and very wealthy are underrepresented18,19.
Study Design
The current analysis is a secondary data analysis using data from the Study of how Pre-pregnancy and Pregnancy Lifestyle Influences the Outcome of Delivery (PEAPOD) study. PEAPOD is a pregnancy cohort study in which participants were recruited from a sample of 12,662 KPNC reproductive-aged women members who completed a health survey between 2007 and 2009 and consented to be included in future research. Participants from this cohort who were pregnant between October 2011 and April 2013, English-speaking and 18 years of age or older were eligible to be recruited for the PEAPOD study. The PEAPOD study enrolled women throughout pregnancy to examine the associations between maternal lifestyle and gestational weight gain and preterm birth and childhood overweight/obesity. A total of 2,136 eligible participants were identified from KPNC’s electronic health records (EHR) and mailed a questionnaire to ascertain information on demographic characteristics including race, ethnicity and lifestyle behaviors during pregnancy, as well as a modified Block Food Frequency Questionnaire (FFQ). The questionnaire was conducted to obtain patient reported information on lifestyle and demographic factors not available in the EHR. Follow-up phone calls were conducted if the survey was not returned within 3 weeks. Return of the survey was considered consent. The PEAPOD study includes a total of 1,810 pregnancies (85% of the 2,136 originally identified as eligible) for which women completed the survey and FFQ. This study was approved by the Kaiser Permanente Northern California Institutional Review Board.
Measures
Prenatal depression —
Kaiser Permanente Northern California began implementing a universal perinatal depression screening program in 2010 in which women are screened two times during pregnancy (at the first prenatal visit and at their 24-week visit)14 using the Patient Health Questionnaire (PHQ-9). The PHQ-9 has been validated in many studies as an instrument for screening for depression with high sensitivity (> 88%) and specificity (> 88%) in obstetric patients20-24, as well as a tool to establish depression severity and outcome25. It includes nine questions with potential scores from zero to 27. A score of 10 or greater suggests moderate to severe depression. For this analysis prenatal depression was defined as any of the following between the start of pregnancy and the FFQ completion date: (1) a PHQ-9 score of 10 or greater (indicating moderate to more severe depression severity) (if more than one PHQ-9 score was greater than 10, the highest PHQ-9 score was used), (2) a depression diagnosis (International Classification of Diseases, Ninth Revision (ICD-9) codes26: 296.20-296.25, 296.30 - 296.35, 296.82, 298.0, 300.4, 309.0, 309.1, 309.28, 648.41-648.44, or 311), or (3) an antidepressant medication dispensing (see Table 1 online only for a list of medications).
Table 1.
List of Antidepressant Medications Included in the Definition of Prenatal Depression in a Study of Prenatal Depression and Diet Quality Conducted in Kaiser Permanente Northern California between 2011-2013.
| Amitriptyline |
| Bupropion |
| Citalopram |
| Desipramine |
| Doxepin |
| Duloxetine |
| Escitalopram Oxalate |
| Fluoxetine |
| Mirtazapine |
| Nefazodone |
| Nortriptyline |
| Paroxetine |
| Sertraline |
| Trazodone |
| Venlafaxine |
Diet Quality —
Dietary intake during pregnancy was assessed using a modified Block 2005 Food Frequency Questionnaire (FFQ) tailored to accommodate the diverse dietary habits of the multi-racial/ethnic study cohort and used in previous studies27,28. The FFQ is designed to collect information on usual dietary intake during the previous three months. The food list for the Block FFQ 2005 was developed from NHANES 1999-2000 dietary recall data29; the nutrient database was developed from the USDA Food and Nutrient Database for Dietary Studies (FNDDS), version 1.030. A series of “adjustment” questions provide greater accuracy in assessing fat and carbohydrate intake31. Individual portion size is asked for each food, and pictures are provided to enhance accuracy of quantification. Dietary supplement intake was not included in the FFQ. Participants reported their usual intake and portion sizes of food and beverages. The Block FFQ has demonstrated adequate reliability and validity in comparison to multiple dietary records32, serving as a useful instrument for estimating energy, food, and nutrient intakes among diverse populations including pregnant women27,33.
The HEI-2010 score was calculated using the simple HEI scoring algorithm method to assess overall diet quality on the individual level. The HEI-2010 score is a valid and reliable measure and was chosen over other measures of diet quality, such as the alternate Mediterranean diet scores34, because it reflects adherence to the 2010 Dietary Guidelines for Americans9. Notably, the HEI-2010 and not the HEI-201535 was used because the 2010 dietary guidelines covered the study period 2011-2013, whereas the 2015-2020 guidelines36 were not released until 2016. The HEI-2010 consists of 12 components (i.e., total fruit, whole fruit, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium and empty calories) with a maximum possible score of 10037. The HEI-2010 scores are inversely related to dietary intake for refined grains, sodium and empty calories components and positively related to dietary intake of the other 9 dietary components. Based on the distribution of the HEI-2010 scores, quartiles were calculated. For the primary outcome, participants who scored in the lowest quartile were classified as consuming a poor-quality diet and compared to participants in the second, third and fourth quartiles combined. The secondary outcome was the mean scores for each of the individual 12 components of the HEI-2010.
Race/Ethnicity.
Self-reported race/ethnicity was categorized as 1) non-Hispanic White, 2) Asian/Pacific Islander, 3) Hispanic, or 4) Other/Unknown. There were very few non-Hispanic Black participants, thus they were combined with American Indian/Alaskan Native, multiple races, other, or unknown race/ethnicity participants in the Other/Unknown category.
Confounders
Potential confounders were ascertained from both the self-report questionnaire and EHR data. Self-report variables were: maternal age at the start of pregnancy in years, marital status (married/partner versus single/divorced/widowed), maternal education (less than college versus college or greater), parity (0 versus 1 or more), any alcohol use during pregnancy (yes/no), any smoking during pregnancy (yes/no), and prenatal vitamin use (yes/no). Pre-pregnancy body mass index (BMI; kg/m2) was calculated using data from the questionnaire and supplemented with EHR data when missing. BMI was categorized as underweight (<18.5 kg/m2), normal weight (18.5 - < 25 kg/m2), overweight (25 - < 30 kg/m2) and obese (≥30 kg/m2)38.
Data Analysis
Differences in the percentage of women with prenatal depression (yes/no) across quartiles of the HEI-2010 total score were assessed with a chi-squared test. Bivariate analyses were conducted to compare characteristics between women with and without prenatal depression; chi-squared analyses were conducted for categorical data and t-tests for continuous data. Unconditional logistic regression analysis was used to obtain odds ratios (ORs) and confidence intervals (CIs) estimating the odds of poor diet quality (vs. good diet quality) given prenatal depression status. Covariates included in the models were chosen based on the literature and included maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking status during pregnancy, prenatal vitamin use during pregnancy, and race/ethnicity39-42. A likelihood ratio test was conducted to assess the interaction between prenatal depression and race/ethnicity on diet quality by comparing the full model with all covariates and an interaction term for race/ethnicity and prenatal depression to the nested model that excluded the interaction term. Tests for interaction generally have less power to assess statistical significance and thus a p-value < 0.10 was accepted for the cutoff suggesting statistical significance43. The aORs and 95% CIs from the full model were calculated and reported for non-Hispanic Whites, Hispanic and Asian/Pacific Islander women. A sensitivity analysis was conducted restricting the overall sample to participants who had a PHQ-9 screen and followed the same analytic methods described for the main analysis. T-tests assessed differences in the means of the 12 individual HEI-2010 between women with and without prenatal depression. Linear regression models were conducted to estimate the relationship between prenatal depression and each component of the HEI-2010 after adjusting for covariates. Chi-squared analyses were conducted to compare women in the final analytic sample to women who were excluded. A p-value of <0.05 was considered statistically significant. Data were extracted from the EHR and merged with survey data using SAS 9.4 (Cary, NC)44 and analyzed using R version 3.4.445.
RESULTS
Among the 1,810 pregnancies in the PEAPOD study the second pregnancy of any woman in the study period was excluded to avoid non-independent observations (n=13). Additionally, to ascertain depression status during pregnancy and prior to completing the FFQ, women who did not have at least one of the following were excluded: a PHQ-9 screen administered through the perinatal depression screening program, a clinical depression diagnosis, or an antidepressant medication fill after the start of pregnancy and before completing the FFQ (n=578). Finally, women whose response on the FFQ resulted in a food energy intake that was not considered plausible, defined as less than 800 kcal (n=38) or greater than 3500 kcal (n=21) were excluded. The final sample included 1,160 women (Figure 1). The median gestational age at FFQ completion was 25 weeks and more than 75% of the women completed the FFQ at 16 weeks gestation or later. Women excluded from the sample were more likely to have not taken prenatal vitamins during pregnancy compared to women in the sample (3.9% vs. 2.7%, p<0.05). There were no other significant differences between women in the study and women excluded from the study sample (Table 2).
Figure 1.
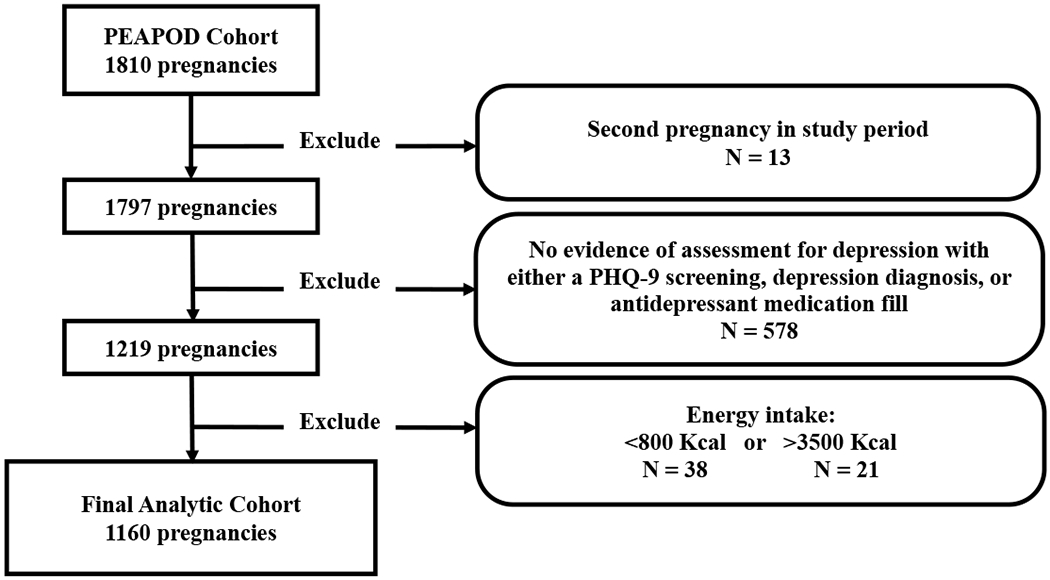
A Flow Diagram of the Inclusion and Exclusion Criteria for a Study on Prenatal Depression and Diet Quality during Pregnancy
Table 2.
Characteristics of Pregnant Women Included in the Analytic Sample (n=1160) Compared to Women participants of the PEAPOD Study that were Excluded from the Analytic Sample (n=637) in a Study of Prenatal Depression and Diet Quality conducted in Kaiser Permanente Northern California between 2011-2013.
| Excluded from study sample | Current Sample | ||
|---|---|---|---|
| n (%) | n (%) | ||
| 637 | 1160 | p-valuea | |
| Maternal age (at pregnancy start) | |||
| < 35 years age | 385 (60.4) | 704 (60.7) | 0.978 |
| 35+ years of age | 247 (38.8) | 446 (38.4) | |
| Missing | 5 (0.8) | 10 (0.9) | |
| Marital status | |||
| Single/Divorced/Separated | 34 (5.3) | 40 (3.4) | 0.081 |
| Married/Living with partner | 601 (94.3) | 1119 (96.5) | |
| Missing | 2 (0.3) | 1 (0.1) | |
| Maternal Education | |||
| < College | 40 (6.3) | 61 (5.3) | 0.349 |
| College + | 595 (93.4) | 1098 (94.7) | |
| Missing | 2 (0.3) | 1 (0.1) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 329 (51.6) | 631 (54.4) | 0.684 |
| Hispanic | 119 (18.7) | 213 (18.4) | |
| Asian/Pacific Islander | 118 (18.5) | 195 (16.8) | |
| Other/Unknownb | 71 (11.1) | 121 (10.4) | |
| Parity | |||
| 1+ | 375 (58.9) | 732 (63.1) | 0.086 |
| 0 | 262 (41.1) | 428 (36.9) | |
| Pre-pregnancy BMI | |||
| Underweight (<18.5 kg/m2) | 19 (3.0) | 32 (2.8) | 0.099 |
| Normal weight (18.5 - < 25 kg/m2) | 356 (55.9) | 626 (54.0) | |
| Overweight (25 - < 30 kg/m2) | 137 (21.5) | 270 (23.3) | |
| Obese (≥30 kg/m2) | 115 (18.1) | 227 (19.6) | |
| Missing | 10 (1.6) | 5 (0.4) | |
| Alcohol use during pregnancy | |||
| Yes | 148 (23.2) | 240 (20.7) | 0.232 |
| No | 489 (76.8) | 920 (79.3) | |
| Smoking during pregnancy | |||
| Yes | 13 (2.0) | 21 (1.8) | 0.871 |
| No | 624 (98.0) | 1139 (98.2) | |
| Prenatal Vitamin Use | |||
| Yes | 612 (96.1) | 1129 (97.3) | 0.041 |
| No | 25 (3.9) | 31 (2.7) | |
| Diet Qualityc | |||
| Poor quality diet | 168 (26.4) | 291 (25.1) | 0.588 |
| Good quality diet | 469 (73.6) | 869 (74.9) |
Chi-square test p-value.
Other/Unknown represents: Non-Hispanic Black, Native American/Alaskan Native, Multiple races, Other, Unknown or Not Reported.
Diet was assessed using the Healthy Eating Index (HEI-2010) score calculated from self-report dietary intake using a modified Block Food Frequency Questionnaire (FFQ). Poor quality diet was defined by scores that ranged in the lowest quartile (≤68.3). Good quality diet was defined by scores that ranged in the top three quartiles.
Characteristics of the Study Population
Descriptive characteristics of women with and without prenatal depression are presented in Table 3. Overall, 159 (14%) of the study participants had prenatal depression. Women with prenatal depression were less likely to have a college education, less likely to already have a child(ren), and more likely to report alcohol use or smoking during pregnancy compared to women without prenatal depression (all p<0.05).
Table 3.
Demographic Characteristics of 1160 Pregnant Women Overall and by Depression Status in a Study of Prenatal Depression and Diet Quality conducted in Kaiser Permanente Northern California between 2011-2013.
| Overall | Depression | No Depression | ||
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p-valuea | |
| Total | 1160 | 159 (13.7%) | 1001 (86.3%) | |
| Maternal age (at pregnancy start) | ||||
| < 35 years age | 704 (60.7) | 89 (56.0) | 615 (61.4) | 0.374 |
| 35+ years of age | 446 (38.4) | 69 (43.4) | 377 (37.7) | |
| Missing | 10 (0.9) | 1 (0.6) | 9 (0.9) | |
| Marital status | ||||
| Single/Divorced/Separated | 40 (3.4) | 10 (6.3) | 30 (3.0) | 0.099 |
| Married/Living with partner | 1119 (96.5) | 149 (93.7) | 970 (96.9) | |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | |
| Maternal Education | ||||
| < College | 61 (5.3) | 15 (9.4) | 46 (4.6) | 0.037 |
| College + | 1098 (94.7) | 144 (90.6) | 954 (95.3) | |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 631 (54.4) | 89 (56.0) | 542 (54.1) | 0.030 |
| Hispanic | 213 (18.4) | 30 (18.9) | 183 (18.3) | |
| Asian/Pacific Islander | 195 (16.8) | 16 (10.1) | 179 (17.9) | |
| Other/Unknownb | 121 (10.4) | 24 (15.1) | 97 (9.7) | |
| Parity | ||||
| 1+ | 732 (63.1) | 85 (53.5) | 647 (64.6) | 0.009 |
| 0 | 428 (36.9) | 74 (46.5) | 354 (35.4) | |
| Pre-pregnancy Body Mass Index (BMI) | ||||
| Underweight (<18.5 kg/m2) | 32 (2.8) | 3 (1.9) | 29 (2.9) | 0.301 |
| Normal weight (18.5 - < 25 kg/m2) | 626 (54.0) | 79 (49.7) | 547 (54.6) | |
| Overweight (25 - < 30 kg/m2) | 270 (23.3) | 37 (23.3) | 233 (23.3) | |
| Obese (≥30 kg/m2) | 227 (19.6) | 40 (25.2) | 187 (18.7) | |
| Missing | 5 (0.4) | 0 (0.0) | 5 (0.5) | |
| Alcohol use during pregnancy | ||||
| Yes | 240 (20.7) | 43 (27.0) | 197 (19.7) | 0.043 |
| No | 920 (79.3) | 116 (73.0) | 804 (80.3) | |
| Smoking during pregnancy | ||||
| Yes | 21 (1.8) | 7 (4.4) | 14 (1.4) | 0.02 |
| No | 1139 (98.2) | 152 (95.6) | 987 (98.6) | |
| Prenatal Vitamin Use | ||||
| Yes | 1129 (97.3) | 154 (96.9) | 975 (97.4) | 0.894 |
| No | 31 (2.7) | 5 (3.1) | 26 (2.6) | |
| Diet Qualityc | ||||
| Poor quality diet | 291 (25.1) | 58 (36.5) | 233 (23.3) | 0.001 |
| Good quality diet | 869 (74.9) | 101 (63.5) | 768 (76.7) |
Chi-square test p-value.
Other/Unknown represents: Non-Hispanic Black, Native American/Alaskan Native, Multiple races, Other, Unknown or Not Reported.
Diet was assessed using the Healthy Eating Index (HEI-2010) score calculated from self-report dietary intake using a modified Block Food Frequency Questionnaire (FFQ). Poor quality diet was defined by scores that ranged in the lowest quartile (≤68.3). Good quality diet was defined by scores that ranged in the top three quartiles.
Healthy Eating Index-2010 Total Scores
The overall mean score for the HEI-2010 was 74.6 SD=10.0; the minimum score was 37.1 and the maximum score 95.8. The cutoff for the first quartile (poor diet quality) was 68.3. Several characteristics were significantly associated with poor diet quality (Table 4). Women with poor diet quality were more likely to be younger (<35 years), have less than a college education and to be obese compared to women with good diet quality.
Table 4.
Demographic Characteristics of 1160 Pregnant Women by Diet Quality in a Study of Prenatal Depression and Diet Quality Conducted in Kaiser Permanente Northern California between 2011-2013.
| Poor Diet Qualitya | Good Diet Qualitya | ||
|---|---|---|---|
| n (%) | n (%) | p-valueb | |
| 291 | 869 | ||
| Maternal age (at pregnancy start) | |||
| < 35 years age | 194 (66.7) | 510 (58.7) | 0.044 |
| 35+ years of age | 94 (32.3) | 352 (40.5) | |
| Missing | 3 (1.0) | 7 (0.8) | |
| Marital status | |||
| Single/Divorced/Separated | 14 (4.8) | 26 (3.0) | 0.288 |
| Married/Living with partner | 277 (95.2) | 842 (96.9) | |
| Missing | 0 (0.0) | 1 (0.1) | |
| Maternal Education | |||
| < College | 25 (8.6) | 36 (4.1) | 0.003 |
| College + | 265 (91.1) | 833 (95.9) | |
| Missing | 1 (0.3) | 0 (0.0) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 156 (53.6) | 475 (54.7) | 0.900 |
| Hispanic | 53 (18.2) | 160 (18.4) | |
| Asian/Pacific Islander | 53 (18.2) | 142 (16.3) | |
| Other/Unknownc | 29 (10.0) | 92 (10.6) | |
| Parity | |||
| 1+ | 182 (62.5) | 550 (63.3) | 0.874 |
| 0 | 109 (37.5) | 319 (36.7) | |
| Pre-pregnancy BMI | |||
| Underweight (<18.5 kg/m2) | 7 (2.4) | 25 (2.9) | 0.006 |
| Normal weight (18.5 - < 25 kg/m2) | 138 (47.4) | 488 (56.2) | |
| Overweight (25 - < 30 kg/m2) | 69 (23.7) | 201 (23.1) | |
| Obese (≥30 kg/m2) | 77 (26.5) | 150 (17.3) | |
| Missing | 0 (0.0) | 5 (0.6) | |
| Alcohol use during pregnancy | |||
| Yes | 59 (20.3) | 181 (20.8) | 0.906 |
| No | 232 (79.7) | 688 (79.2) | |
| Smoking during pregnancy | |||
| Yes | 11 (3.8) | 10 (1.2) | 0.008 |
| No | 280 (96.2) | 859 (98.8) | |
| Prenatal Vitamin Use | |||
| Yes | 277 (95.2) | 852 (98.0) | 0.016 |
| No | 14 (4.8) | 17 (2.0) |
Diet quality was assessed using the Healthy Eating Index (HEI-2010) score calculated from self-report dietary intake using a modified Block Food Frequency Questionnaire (FFQ). Poor quality diet was defined by scores that ranged in the lowest quartile (≤68.3). Good quality diet was defined by scores that ranged in the top three quartiles.
Chi-square test p-value.
Other/Unknown represents: Non-Hispanic Black, Native American/Alaskan Native, Multiple races, Other, Unknown or Not Reported.
Prenatal Depression and Diet Quality
Overall, women with prenatal depression had nearly twice the odds of poor diet quality (crude odds ratio (cOR): 1.89; 95% CI:1.32, 2.69) (Table 5) compared to women without prenatal depression. This relationship held after adjusting for potential confounders (adjusted OR: 1.80; 95% CI: 1.23, 2.60).
Table 5.
Crude (cOR) and Adjusted Odds Ratios (aOR) for the Relationship between Prenatal Depression and Poor Diet Quality, Overall and by Race/Ethnicity in a Sample of 1160 Pregnant Women Recruited from Kaiser Permanente Northern California between 2011-2013.
| Poor Diet Qualitya | |||||
|---|---|---|---|---|---|
| n (%) | cORb | 95% CI | aORc | 95% CI | |
| Full sample (n=1160)d | |||||
| Depression (n=159) | 58 (36.5) | 1.89 | (1.32, 2.69) | 1.80 | (1.23, 2.60) |
| No depression (n=1001) | 233 (23.3) | 1 | 1 | ||
| Non-Hispanic White (n=631)e | |||||
| Depression (n=89) | 28 (31.5) | 1.48 | (0.90, 2.40) | 1.29 | (0.76, 2.15) |
| No depression (n=542) | 128 (23.6) | 1 | 1 | ||
| Hispanic (n=213)e | |||||
| Depression (n=30) | 13 (43.3) | 2.73 | (1.21,6.09) | 2.66 | (1.15, 6.06) |
| No depression (n=183) | 40 (21.9) | 1 | 1 | ||
| Asian/Pacific Islander (n=195)e | |||||
| Depression (n=17) | 7 (41.2) | 2.25 | (0.76, 6.38) | 2.32 | (0.77, 6.70) |
| No depression (n=179) | 46 (25.7) | 1 | |||
Diet was assessed using the Healthy Eating Index (HEI-2010) score calculated from self-report dietary intake using a modified Block Food Frequency Questionnaire (FFQ). Poor quality diet was defined by scores that ranged in the lowest quartile. Good quality diet was defined by scores that ranged in the top three quartiles.
crude odds ratio (cOR)
adjusted odds ratio (aOR)
A total of 1143 women were included in the adjusted analysis due to missing data. The analyses were adjusted for maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking status during pregnancy, prenatal vitamin use during pregnancy, and race/ethnicity.
Due to some missing covariate data, the total sample size for the adjusted analyses for each of the race/ethnicity categories were as follows: n= 623 for Non-Hispanic White, n= 210 for Hispanic, and n=191 for Asian. The analyses were adjusted for maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking status during pregnancy, prenatal vitamin use during pregnancy and an interaction term for race/ethnicity and prenatal depression status.
For Hispanic women, prenatal depression was significantly associated with an increase in the odds of poor diet quality. After adjusting for potential confounding, Hispanic women with prenatal depression had over two and a half times the odds of poor diet quality compared to those without prenatal depression (aOR: 2.66, 95% CI: 1.15, 6.06). The p-value for the likelihood ratio test of the interaction was p=0.11.
Prenatal Depression and HEI-2010 Component Scores
The mean scores for each component are listed in Table 6 for the total sample. Women with prenatal depression had a significantly lower mean HEI-2010 component score for empty calories compared to women without depression indicating a higher consumption of foods with solid fats, alcohol and added sugars (Mean:14.38, SE: 3.95 vs. Mean: 15.27, SE: 3.71, p<0.05). Additionally, women with prenatal depression had a significantly lower mean HEI-2010 component score for greens and beans (Mean: 3.49, SE: 1.60 vs. Mean: 3.79, SE: 1.48, p<0.05), total fruit (Mean: 4.16, SE: 1.19 vs. Mean: 4.43, SE: 1.01, p<0.05), and whole fruit (Mean: 4.45, SE: 1.05 vs. Mean: 4.70, SE: 0.76, p<0.01), indicating a lower dietary intake compared to women without prenatal depression. After adjusting for potential confounders the relationship between prenatal depression and solid fats, alcohol and added sugars approached statistical significance (p= 0.06), while significant relationships remained with prenatal depression and greens and beans, total fruit and whole fruit. No other significant relationships emerged between prenatal depression and any of the other eight HEI-2010 component scores even after adjusting for potential confounders.
Table 6.
Mean Score and Standard Error (SE) for each of the 12 HEI-2010a Components, Overall and by Depression Status and β coefficient for the Multivariable Linear Regression Model Assessing the Association between Prenatal Depression and Each of the 12 HEI-2010 Components in a Sample of 1160 Pregnant Women Recruited from Kaiser Permanente Northern California between 2011-2013.
| Overall | Depression | No Depression | Multivariable Modelc | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n=1160 | n=159 | n=1001 | n=1160 | ||||||
| HEI-2010 component | Mean | SE | Mean | SE | Mean | SE | p-valueb | β | p-value |
| Total vegetablesd | 3.62 | 1.19 | 3.56 | 1.18 | 3.63 | 1.19 | 0.47 | −0.06 | 0.55 |
| Greens and beansd | 3.74 | 1.50 | 3.49 | 1.60 | 3.79 | 1.48 | 0.03 | −0.28 | 0.03 |
| Total fruitd | 4.39 | 1.04 | 4.16 | 1.19 | 4.43 | 1.01 | <0.01 | −0.24 | <0.01 |
| Whole fruitd | 4.66 | 0.81 | 4.45 | 1.05 | 4.70 | 0.76 | <0.01 | −0.24 | <0.01 |
| Whole grainse | 7.23 | 2.75 | 6.92 | 2.77 | 7.28 | 2.74 | 0.13 | −0.40 | 0.09 |
| Dairye | 7.30 | 2.51 | 7.30 | 2.51 | 7.30 | 2.52 | 0.99 | −0.11 | 0.62 |
| Total protein foodsd | 4.62 | 0.67 | 4.56 | 0.75 | 4.63 | 0.66 | 0.27 | −0.08 | 0.20 |
| Seafood and plant proteinsd | 4.54 | 0.93 | 4.45 | 1.05 | 4.55 | 0.91 | 0.27 | −0.08 | 0.32 |
| Fatty acidse | 6.34 | 2.77 | 6.15 | 2.82 | 6.38 | 2.77 | 0.35 | −0.05 | 0.81 |
| Sodiume | 4.01 | 2.49 | 4.34 | 2.59 | 3.96 | 2.47 | 0.09 | 0.19 | 0.35 |
| Refined grainse | 9.01 | 1.78 | 8.82 | 2.07 | 9.04 | 1.73 | 0.20 | −0.29 | 0.06 |
| Empty caloriesf | 15.15 | 3.75 | 14.38 | 3.95 | 15.27 | 3.71 | 0.01 | −0.59 | 0.06 |
Healthy Eating Index- 2010.
T-test p-value.
A total of 1143 women were included in the adjusted analysis due to missing data. The analysis adjusted for maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking status during pregnancy, prenatal vitamin use during pregnancy, and race/ethnicity.
Component score ranges from 0 to 5.
Component score ranges from 0 to 10.
Calories from solid fats, alcohol and added sugar; threshold for counting alcohol is greater than 13 g/1000 kcal. Component score ranges from 0 to 20.
Sensitivity Analysis
Similar results emerged in the sensitivity analysis assessing the relationship between prenatal depression and diet quality restricting the sample to women with a PHQ-9 screening. 1,140 women received a PHQ-9 screening during routine prenatal care. Women with prenatal depression had greater odds of poor diet quality (cOR: 1.91; 95% CI: 1.31, 2.77) compared to women without prenatal depression. Although slightly attenuated, this relationship remained significant after adjusting for potential confounders (aOR: 1.76; 95% CI: 1.19, 2.59). Similar patterns emerged in the sensitivity analysis assessing the interaction between race/ethnicity and prenatal depression on diet quality when compared to the main analysis. Hispanic women with a positive PHQ-9 score (10 or greater) had a significant increased odds of poor diet quality compared to women without prenatal depression (aOR: 2.66, 95% CI: 1.12, 6.30) (Table 7).
Table 7.
Sensitivity Analysis - Crude (cOR) and Adjusted Odds Ratios (aOR) for the Relationship between Prenatal Depression and Poor Diet Quality, Overall and by Race/Ethnicity, Excluding Women who did not have a PHQ-9 Screening Score in a Sample of 1140 Pregnant Women Recruited from Kaiser Permanente Northern California between 2011-2013.
| cOR | 95% CI | aOR | 95% CI | |
|---|---|---|---|---|
| Full sample (n=1140)a | ||||
| Depression (n=139) | 1.91 | (1.31, 2.77) | 1.76 | (1.19, 2.59) |
| No depression (n=1001) | 1 | 1 | ||
| Non-Hispanic White (n=616)b | ||||
| Depression (n=74) | 1.55 | (0.90, 2.60) | 1.36 | (0.77, 2.34) |
| No depression (n=542) | 1 | 1 | ||
| Hispanic (n=210)b | ||||
| Depression (n=27) | 2.86 | (1.22, 6.60) | 2.66 | (1.12, 6.30) |
| No depression (n=183) | 1 | 1 | ||
| Asian/Pacific Islander (n=195)b | ||||
| Depression (n=16) | 2.25 | (0.76, 6.38) | 2.35 | (0.78, 6.80) |
| No depression (n=179) | 1 | 1 | ||
Adjusted for maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking status during pregnancy, prenatal vitamin use during pregnancy, and race/ethnicity
Adjusted for maternal age, marital status, maternal education, parity, pre-pregnancy body mass index (BMI), alcohol use during pregnancy, smoking during pregnancy, prenatal vitamin use during pregnancy and interaction term for race/ethnicity and prenatal depression status.
DISCUSSION/COMMENT
Findings from this study suggest women with prenatal depression or high prenatal depressive symptoms may have a higher risk of poor diet quality compared to women without prenatal depression, and that the relationship may be stronger in Hispanic women. The findings remained significant after restricting the sample to women with a PHQ-9 screening score, suggesting that depressive symptoms at or above a threshold of moderate depression may be as important as a clinical depression diagnosis in the relationship with diet quality. While an inverse association between depression and diet quality has been found previously in pregnant women, the limited research to date has been conducted in small samples (fewer than 120) of low-income women15,42. This study adds to the literature findings from a large, racially/ethnically diverse sample of pregnant women.
Findings from this study are consistent with the majority of the limited studies in non-pregnant populations evaluating the relationship between depression and diet quality. In a study of breast cancer survivors, depressive symptoms and HEI scores were inversely related46. Similarly, Appelhans et al47 observed an association between higher depressive severity and lower diet quality in a sample of obese participants with major depressive disorder. An inverse association between depressive symptoms and diet quality was also noted in a representative sample of US adults48. In a sample of overweight and obese rural-dwelling adults, depressive symptoms predicted poor overall diet quality among the overweight participants, however findings did not replicate in the obese participants49. Three other studies documented mixed findings as well. For example, Rahe et al,40 did not find a significant relationship between depression as a homogenous entity, but did find a relationship between distinct subtypes of depression such that participants with atypical depression (depression with improved mood in response to positive events) reported the lowest diet quality scores. Two additional studies, one in a sample of obese and overweight women from disadvantaged neighborhoods50 and another in sample of middle-aged adults51 did not find a relationship between depressive symptoms and overall dietary quality. However, similar to the current study findings, the study of obese and overweight women from disadvantaged neighborhoods documented a significant relationship between depressive symptoms and greater saturated fats and total sugar intake50.
The underlying mechanisms that link depression and eating behavior may include psychological as well as sensory and physiological pathways. For example, several studies have demonstrated an association between the presences of depressive symptoms and emotional eating 50,52,53. Emotional eating is the propensity to choose to eat energy-dense sweet and high-fat foods in response to negative affects and stress52. Findings from the current study suggest that women with prenatal depression had a significantly lower HEI-2010 empty calories component score compared to women without prenatal depression. The HEI-2010 empty calorie component score is inversely related to dietary intake of empty calories; thus, in this study women with prenatal depression consumed a diet higher in solid fats, alcohol and added sugars (threshold for counting alcohol is greater than 13g/1,000 kcal) compared to women without prenatal depression. These findings suggest that women with prenatal depression may benefit from nutritional counseling targeted at limiting dietary intake from empty calories from solid fats, alcohol and added sugars. This study also found that women with prenatal depression consumed less overall greens and beans, total fruit and whole fruit compared to women without prenatal depression suggesting that nutritional counseling for women with prenatal depression may also target increasing consumption of fruit, greens and beans. Given that poor maternal diet quality during pregnancy has been linked to poor outcomes of both the offspring into adulthood1-3 and to the woman’s health5-8,54-57, further research is needed to understand the extent to which depression may contribute to these outcomes by influencing diet quality. This study is the first to our knowledge to assess the relationship between prenatal depression and individual HEI components.
Strengths and limitations
Dietary intake was assessed using a validated instrument which allowed us to construct a reliable and internally valid index of diet quality (as assessed with the HEI-2010) that represents a comprehensive assessment of a woman’s diet during pregnancy. Further, the HEI-2010 was designed to reflect the Dietary Guidelines for Americans9 and the use of this a priori diet score would allow comparability across studies in the United States, in contrast to the use of other data-driven study specific dietary scores. Additionally, prenatal depression was defined using a combination of clinical diagnoses, antidepressant medications and PHQ-9 scores all ascertained from EHR data. The sensitivity analyses restricting the sample to women uniformly screened for depression with the PHQ-9 during the study period demonstrates that symptom severity may be as important as a clinical diagnosis of prenatal depression in the relationship with diet quality. Finally, the authors acknowledge that the study was limited to English-speaking women and thus the associations observed among the Hispanic women may not be representative of non-English speaking Hispanic women.
This study offers some unique insights into the relationship between depression including depressive symptoms and diet quality in pregnant women; however, the findings and implications of this study should be interpreted with consideration of the limitations. Maternal dietary intake was self-reported using the FFQ, with potential recall bias and subsequent exposure misclassification58. There is no evidence that women with prenatal depression may recall their dietary intake differentially from women without prenatal depression. The mean HEI-2010 total score in the current study sample (74.6) was a little higher in comparison to some previous studies of pregnant women which have ranged from 54.2 – 6412,59, yet similar to others (mean HEI-2010 score of 6760) including a study conducted in pregnant women in Northern California (mean HEI-2010 score of 71.328). Causality cannot be inferred given the cross-sectional study design. Despite defining prenatal depression prior to the completion of the FFQ, the FFQ asks for dietary intake in the previous three months and thus there may be overlap of the timing of prenatal depression and dietary intake, thus the ability to determine the direction of the relationship is limited. It is plausible that the relationship between depression and diet is bidirectional. Observational studies have found that adherence to higher quality diets is associated with reduced future onset of depressive symptoms61. Additionally, recent clinical trials62,63 suggest dietary interventions may have a modest impact on reducing depressive symptoms. It is possible that depressive symptoms may be related to dietary misreporting, although research assessing this is insufficient64. The use of a validated and reliable instrument to assess dietary intake may diminish this possibility, however we note that previous validation studies in women did not report information on inclusion or exclusion of pregnant women with depression32,33. The study sample excluded over a quarter of the participants recruited into the PEAPOD study because they did not have any evidence of being assessed for depression. There were very few significant differences between the final study sample and those who were excluded. Finally, the relationship between prenatal depression and diet quality among non-Hispanic Black women was not able to be assessed given the sample size.
Conclusions
Findings from this study suggest that women with prenatal depression and or prenatal depressive symptoms are at a higher risk of poor diet quality compared to women without prenatal depression, and the relationship is stronger among Hispanic women. Nutritional counseling interventions for women with depression may consider the use of culturally sensitive material, target limiting empty calories from solid fats, alcohol and added sugars and encourage eating more greens, beans and fruit. Additional prospective studies are needed to clarify the direction of the relationship.
Research Snapshot.
Research Question:
Is prenatal depression associated with diet quality during pregnancy as measured with the Healthy Eating Index-2010 (HEI-2010) and does this relationship differ by race/ethnicity? Are there differences in the 12 HEI-2010 dietary components for women with prenatal depression compared to women without prenatal depression?
Key Findings:
In this cross-sectional examination of 1160 pregnant participants in the PEAPOD study, findings suggest that women with prenatal depression (defined as either a depression diagnosis, positive screen on the Patient Health Questionnaire (PHQ-9), or antidepressant medication dispensing) may have a higher risk of poor diet quality (defined as falling in the lowest quartile of the HEI-2010 scores) compared to women without prenatal depression, and that the relationship may be stronger in Hispanic women. Women with prenatal depression had a significantly lower mean HEI-2010 component score for empty calories compared to women without depression indicating a higher percent energy intake from solid fats and added sugars. Additionally, women with prenatal depression had a significantly lower mean HEI-2010 component score for greens and beans, total fruit and whole fruit indicating a lower dietary intake per the density-based approach used by the HEI-2010 compared to women without prenatal depression.
Acknowledgements:
We are grateful to Linda Nkemere for her help with preparation of the manuscript and have received permission from her to acknowledge her contribution.
Funding/financial disclosure: This study was supported by a career development award to Dr. Avalos (K01MH103444) by the National Institute of Mental Health (NIMH). Dr. Zhu was also supported by NIH grants 5K12HD52163 and K01DK120807.
Footnotes
Conflict of interest: The authors report no conflict of interest.
References
- 1.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359(1):61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harding JE. The nutritional basis of the fetal origins of adult disease. Int J Epidemiol. 2001;30(1):15–23. [DOI] [PubMed] [Google Scholar]
- 3.Barker DJ. The fetal and infant origins of disease. Eur J Clin Invest. 1995;25(7):457–463. [DOI] [PubMed] [Google Scholar]
- 4.Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311(6998):171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao SK, Beresford SA, Frank LL, Schreiner PJ, Burke GL, Fitzpatrick AL. Modifications to the Healthy Eating Index and its ability to predict obesity: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2008;88(1):64–69. [DOI] [PubMed] [Google Scholar]
- 6.Boggs DA, Rosenberg L, Rodriguez-Bernal CL, Palmer JR. Long-term diet quality is associated with lower obesity risk in young African American women with normal BMI at baseline. J Nutr. 2013;143(10):1636–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uusitalo U, Arkkola T, Ovaskainen ML, et al. Unhealthy dietary patterns are associated with weight gain during pregnancy among Finnish women. Public Health Nutr. 2009;12(12):2392–2399. [DOI] [PubMed] [Google Scholar]
- 8.von Ruesten A, Brantsaeter AL, Haugen M, et al. Adherence of pregnant women to Nordic dietary guidelines in relation to postpartum weight retention: results from the Norwegian Mother and Child Cohort Study. BMC Public Health. 2014;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Human USDoAaUSDoHa, Services. Dietary Guidelines for Americans, 2010. Washington, DC: U.S. Government Printing Office;2010. [Google Scholar]
- 11.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodnar LM, Simhan HN, Parker CB, et al. Racial or Ethnic and Socioeconomic Inequalities in Adherence to National Dietary Guidance in a Large Cohort of US Pregnant Women. J Acad Nutr Diet. 2017;117(6):867–877 e863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukherjee S, Trepka MJ, Pierre-Victor D, Bahelah R, Avent T. Racial/Ethnic Disparities in Antenatal Depression in the United States: A Systematic Review. Matern Child Health J. 2016;20(9):1780–1797. [DOI] [PubMed] [Google Scholar]
- 14.Avalos LA, Raine-Bennett T, Chen H, Adams AS, Flanagan T. Improved Perinatal Depression Screening, Treatment, and Outcomes With a Universal Obstetric Program. Obstet Gynecol. 2016;127(5):917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fowles ER, Stang J, Bryant M, Kim S. Stress, depression, social support, and eating habits reduce diet quality in the first trimester in low-income women: a pilot study. J Acad Nutr Diet. 2012;112(10):1619–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quirk SE, Williams LJ, O’Neil A, et al. The association between diet quality, dietary patterns and depression in adults: a systematic review. BMC Psychiatry. 2013;13:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoerster KD, Wilson S, Nelson KM, Reiber GE, Masheb RM. Diet quality is associated with mental health, social support, and neighborhood factors among Veterans. Eat Behav. 2016;23:168–173. [DOI] [PubMed] [Google Scholar]
- 18.Gordon N Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011-12 California Health Interview Survey. Oakland, CA: Kaiser Permanente Division of Research;2015. [Google Scholar]
- 19.Gordon N A Comparison of Sociodemographic and Health Characteristics of the Kaiser Permanente Northern California Membership Derived from Two Data Sources: The 2008 Member Health Survey and the 2007 California Health Interview Survey. Oakland, CA: Kaiser Permanente Division of Research;2012. [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183(3):759–769. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Jama. 1999;282(18):1737–1744. [DOI] [PubMed] [Google Scholar]
- 23.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: a systematic review. Gen Hosp Psychiatry. 2007;29(5):388–395. [DOI] [PubMed] [Google Scholar]
- 25.Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Medical care. 2004;42(12):1194–1201. [DOI] [PubMed] [Google Scholar]
- 26.Corporation PMI. International Classification of Diseases, 9th Revision, Clinical Modification. Fifth ed. Los Angeles, CA: Practice Management Information Corporation; 1999. [Google Scholar]
- 27.Ferrara A, Hedderson MM, Brown SD, et al. The Comparative Effectiveness of Diabetes Prevention Strategies to Reduce Postpartum Weight Retention in Women With Gestational Diabetes Mellitus: The Gestational Diabetes' Effects on Moms (GEM) Cluster Randomized Controlled Trial. Diabetes Care. 2016;39(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu Y, Hedderson MM, Sridhar S, Xu F, Feng J, Ferrara A. Poor diet quality in pregnancy is associated with increased risk of excess fetal growth: a prospective multi-racial/ethnic cohort study. Int J Epidemiol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) NCfHSN. National Health and Nutrition Examination Survey: 1999-2000 Data Documentation, Codebook, and Frequencies. 2002; https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/DRXIFF.htm.
- 30.USDA. Food and Nutrient Database for Dietary Studies, 1.0. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group; 2004. [Google Scholar]
- 31.NutritionQuest. Questionnaires and Screeners. https://nutritionquest.com/assessment/list-of-questionnaires-and-screeners/. Accessed May 2019.
- 32.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43(12):1327–1335. [DOI] [PubMed] [Google Scholar]
- 33.Harley K, Eskenazi B, Block G. The association of time in the US and diet during pregnancy in low-income women of Mexican descent. Paediatr Perinat Epidemiol. 2005;19(2):125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agriculture USDoHaHSaUSDo. 2015–2020 Dietary Guidelines for Americans. 2015. [Google Scholar]
- 37.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prevention CfDCa. Defining Adult Overweight and Obesity. 2017; https://www.cdc.gov/obesity/adult/defining.html. Accessed May 2019.
- 39.Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychosocial influences in dietary patterns during pregnancy. J Am Diet Assoc. 2005;105(6):963–966. [DOI] [PubMed] [Google Scholar]
- 40.Rahe C, Baune BT, Unrath M, et al. Associations between depression subtypes, depression severity and diet quality: cross-sectional findings from the BiDirect Study. BMC Psychiatry. 2015;15:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chatzi L, Melaki V, Sarri K, et al. Dietary patterns during pregnancy and the risk of postpartum depression: the mother-child ‘Rhea’ cohort in Crete, Greece. Public Health Nutr. 2011;14(9):1663–1670. [DOI] [PubMed] [Google Scholar]
- 42.Fowles ER, Bryant M, Kim S, et al. Predictors of dietary quality in low-income pregnant women: a path analysis. Nurs Res. 2011;60(5):286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frazier PA TA, Barron KE. Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology. 2004;51(1):115–134. [Google Scholar]
- 44.SAS 9.4 Statements: Reference [computer program]. Cary, NC: SAS Institute Inc.; 2013. [Google Scholar]
- 45.R: A Language and Environment for Statistical Computing (Version 3.4.4) [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 46.Tangney CC, Young JA, Murtaugh MA, Cobleigh MA, Oleske DM. Self-reported dietary habits, overall dietary quality and symptomatology of breast cancer survivors: a cross-sectional examination. Breast Cancer Res Treat. 2002;71(2):113–123. [DOI] [PubMed] [Google Scholar]
- 47.Appelhans BM, Whited MC, Schneider KL, et al. Depression severity, diet quality, and physical activity in women with obesity and depression. J Acad Nutr Diet. 2012;112(5):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beydoun MA, Wang Y. Pathways linking socioeconomic status to obesity through depression and lifestyle factors among young US adults. J Affect Disord. 2010;123(1-3):52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abshire DA, Lennie TA, Chung ML, Biddle MJ, Barbosa-Leiker C, Moser DK. Body Mass Index Category Moderates the Relationship Between Depressive Symptoms and Diet Quality in Overweight and Obese Rural-Dwelling Adults. J Rural Health. 2018;34(4):377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whitaker KM, Sharpe PA, Wilcox S, Hutto BE. Depressive symptoms are associated with dietary intake but not physical activity among overweight and obese women from disadvantaged neighborhoods. Nutr Res. 2014;34(4):294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meegan AP, Perry IJ, Phillips CM. The Association between Dietary Quality and Dietary Guideline Adherence with Mental Health Outcomes in Adults: A Cross-Sectional Analysis. Nutrients. 2017;9(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Konttinen H, Mannisto S, Sarlio-Lahteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54(3):473–479. [DOI] [PubMed] [Google Scholar]
- 53.Ouwens MA, van Strien T, van Leeuwe JF. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite. 2009;53(2):245–248. [DOI] [PubMed] [Google Scholar]
- 54.Ikem E, Halldorsson TI, Birgisdottir BE, Rasmussen MA, Olsen SF, Maslova E. Dietary patterns and the risk of pregnancy-associated hypertension in the Danish National Birth Cohort: a prospective longitudinal study. Bjog. 2019;126(5):663–673. [DOI] [PubMed] [Google Scholar]
- 55.Timmermans S, Steegers-Theunissen RP, Vujkovic M, et al. Major dietary patterns and blood pressure patterns during pregnancy: the Generation R Study. Am J Obstet Gynecol. 2011;205(4):337 e331–312. [DOI] [PubMed] [Google Scholar]
- 56.Qiu C, Coughlin KB, Frederick IO, Sorensen TK, Williams MA. Dietary fiber intake in early pregnancy and risk of subsequent preeclampsia. Am J Hypertens. 2008;21(8):903–909. [DOI] [PubMed] [Google Scholar]
- 57.Shin D, Lee KW, Song WO. Dietary Patterns during Pregnancy Are Associated with Risk of Gestational Diabetes Mellitus. Nutrients. 2015;7(11):9369–9382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rothman KJ, Greenland S. Modern Epidemiology. 2nd Edition ed. Philadelphia: Lippincott Williams & Wilkins; 1998. [Google Scholar]
- 59.Shapiro AL, Kaar JL, Crume TL, et al. Maternal diet quality in pregnancy and neonatal adiposity: the Healthy Start Study. Int J Obes (Lond). 2016;40(7):1056–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grandy M, Snowden JM, Boone-Heinonen J, Purnell JQ, Thornburg KL, Marshall NE. Poorer maternal diet quality and increased birth weight(). J Matern Fetal Neonatal Med. 2018;31(12):1613–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Molendijk M, Molero P, Ortuno Sanchez-Pedreno F, Van der Does W, Angel Martinez-Gonzalez M. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. 2018;226:346–354. [DOI] [PubMed] [Google Scholar]
- 62.Bot M, Brouwer IA, Roca M, et al. Effect of Multinutrient Supplementation and Food-Related Behavioral Activation Therapy on Prevention of Major Depressive Disorder Among Overweight or Obese Adults With Subsyndromal Depressive Symptoms: The MooDFOOD Randomized Clinical Trial. JAMA. 2019;321(9):858–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ma J, Rosas LG, Lv N, et al. Effect of Integrated Behavioral Weight Loss Treatment and Problem-Solving Therapy on Body Mass Index and Depressive Symptoms Among Patients With Obesity and Depression: The RAINBOW Randomized Clinical Trial. JAMA. 2019;321(9):869–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maurer J, Taren DL, Teixeira PJ, et al. The psychosocial and behavioral characteristics related to energy misreporting. Nutr Rev. 2006;64(2 Pt 1):53–66. [DOI] [PubMed] [Google Scholar]


