Abstract
Aims
The coronavirus disease 2019 (COVID‐19) pandemic has created significant challenges to healthcare globally, necessitating rapid restructuring of service provision. This questionnaire survey was conducted amongst adult heart failure (HF) patients in the United Kingdom (UK), to understand the impact of COVID‐19 upon HF services.
Methods and results
The survey was conducted by the Pumping Marvellous Foundation, a UK HF patient charity. ‘Survey Monkey’ was used to disseminate the questionnaire in the Pumping Marvellous Foundation 's online patient group and in 10 UK hospitals (outpatient hospital and community HF clinics). There were 1050 responses collected (693/1050—66% women); 55% (579/1050) were aged over 60 years. Anxiety level was significantly higher regarding COVID‐19 (mean 7 ± 2.5 on anxiety scale of 0 to 10) compared with anxiety regarding HF (6.1 ± 2.4; P < 0.001). Anxiety was higher amongst patients aged ≤60 years about HF (6.3 ± 2.2 vs. 5.9 ± 2.5 in those aged >60 years; P = 0.005) and COVID‐19 (7.3 ± 2.3 vs. 6.7 ± 2.6 those aged >60 years; P < 0.001). Sixty‐five per cent of respondents (686/1050) reported disruption to HF appointments (cancellation or postponement) during the lockdown period. Thirty‐seven per cent reported disruption to medication prescription services, and Thirty‐four per cent reported inability to access their HF teams promptly. Thirty‐two per cent expressed reluctance to attend hospital (25% stated they would only attend hospital if there was no alternative, and 7% stated that they would not attend hospital at all).
Conclusions
The COVID‐19 pandemic has caused significant anxiety amongst HF patients regarding COVID‐19 and HF. Cancellation or postponement of scheduled clinic appointments, investigations, procedures, prescription, and monitoring services were implicated as sources of anxiety.
Keywords: Heart failure, Patient, Survey, COVID‐19
Introduction
Coronavirus disease 2019 (COVID‐19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). 1 COVID‐19 evolved into an international public health crisis rapidly after being discovered in December 2019 and was declared a pandemic by the World Health Organization on March 11, 2020. 2 In the United Kingdom (UK), the accelerating pace of the COVID‐19 pandemic resulted in the British government issuing a public lockdown from the 23rd of March 3 and a rapid shift in the focus of care in the National Health Service (NHS) ensued. Lockdown measures were first eased in England from 13 May 2020, 4 whereas other devolved UK nations eased lockdown measures more slowly (e.g. Scotland from 28 May onwards).
The COVID‐19 pandemic has created an unprecedented challenge to healthcare resources throughout the world. Hospitals rapidly restructured services in order to enable them to cope with the predicted high numbers of COVID‐19 patients. This led to the cancellation or postponement of elective appointments, and both inpatient as well as outpatient services were restricted to prioritize urgent cases. In particular, elective face‐to‐face appointments were reduced significantly and the threshold for admitting patients increased 5 in order to minimize the risk of exposure to COVID‐19 to at‐risk groups such as those with underlying cardiovascular conditions. 6 In addition to this, patients have also been reluctant to attend hospital due to self‐isolation, fear of contracting infection, and also perhaps a misinterpretation of government guidance that healthcare services are not open for non‐COVID‐19 healthcare including emergencies. 7 This trend has been reflected in the significantly reduced hospitalization rates for several acute cardiovascular conditions 8 such as acute coronary syndrome 9 , 10 , 11 as well as acute heart failure (HF) during the ongoing pandemic in the UK 12 , 13 but also in other parts of the world, 14 , 15 with these results suggesting a 50% reduction in acute HF hospitalizations during the first wave of the pandemic. HF patients also received seemingly conflicting advice, with initial communication from Public Health England (PHE) advising that they were amongst those at increased risk of severe illness from COVID‐19 16 ; however, subsequent communication excluded HF patients from the list of patients with chronic conditions classed as ‘clinically extremely vulnerable’. 17
The primary aim of this HF patient study was to ascertain the impact of the COVID‐19 lockdown upon adult HF patient care. The pandemic response has also prompted a rapid evolution of service delivery such as the use of virtual clinics (using telephone/video technology), remote monitoring, and ambulatory care. The Heart Failure Society of America and the European Society of Cardiology both recommend the use of tele‐health strategies such as virtual clinics (remote consultation using telephone or video technology) and remote monitoring of patient health parameters (weight, pulse, and blood pressure) as alternatives to minimize the need for in‐hospital visits, 18 , 19 and recent evidence during the pandemic has also suggested that telemedicine can have beneficial outcomes in HF. 5 , 20 However, it is currently unclear whether the full spectrum of service reconfiguration is acceptable as well as accessible to patients, and there is currently a lack of feedback regarding patients' opinions about suitability of various tele‐health strategies. We therefore incorporated patient feedback regarding service innovations into our survey and also sought to gauge HF patients' preferences regarding the newer models of care that they would like to see incorporated into or continued in their local HF services.
Methods
The survey was conducted by the Pumping Marvellous Foundation (PMF) which is the UK's largest patient‐led HF charity. PMF is funded via donations and fundraising by individuals, with support from the NHS and charitable organizations together with corporate sponsorship. An HF patient survey working group was constituted in May 2020, consisting of three HF patients, six HF cardiologists, one HF advanced nurse practitioner, and one HF nurse consultant. The HF patient survey working group devised the survey questionnaire (supporting information).
The anonymous questionnaire survey was disseminated from 15 June 2020 to 10 August 2020 to approximately 7000 adult HF patients. One mode of dissemination was through the online survey tool Survey Monkey, on the Pumping Marvellous Closed Online Patient Group. The other was by handing out 4000 cards (containing quick response codes with links to the survey) to HF patients who attended outpatient clinics or community HF clinics affiliated to 10 participating hospitals in the UK.
Heart failure patients were asked to rate their anxiety about HF and COVID‐19 on a scale of 0 (no anxiety) to 10 (highest anxiety level). The survey also consisted of questions regarding the impact of COVID‐19 lockdown upon outpatient HF clinic appointments (hospital as well as community HF services), cardiac investigations, procedures, and access to medications as well as HF counselling. Opinions were also sought regarding preference for service changes enforced by the pandemic. Statistical comparisons were performed based on gender and age groups (patients aged up to 60 years vs. those aged more than 60 years).
Statistical analysis
For the descriptive statistics of our patient population, we represent continuous variables as means with standard deviations (mean ± SD) when normally distributed and compared using a Student's t test. For non‐normal data, the parameters are described using medians with interquartile ranges and compared using Mann–Whitney test. Categorical data are expressed as percentages and compared using the χ 2 test.
Results
A total of 1050 adult HF patients and carers were surveyed from England (80%, 840), Scotland (10%, 100), Wales (8%, 87), and Northern Ireland (2%, 23). The majority of survey respondents (696 out of 1050—66%) were female and 55% (579/1050) were aged more than 60 years. Comprehensive patient demographics are detailed in Table 1 .
Table 1.
Demographics of heart failure questionnaire survey respondents
| Characteristic | n = 1050 | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 357 | 34.4 |
| Female | 693 | 66.6 |
| Prefer not to say | 5 | 0.4 |
| Age | ||
| 18–30 | 8 | 1 |
| 31–40 | 38 | 3 |
| 41–50 | 132 | 12 |
| 51–60 | 293 | 28 |
| 61–70 | 309 | 29 |
| 71–80 | 215 | 21 |
| >80 | 55 | 5 |
| Identification | ||
| Patient living with heart failure | 950 | 87 |
| Carer of patient | 100 | 9 |
| Location | ||
| England | 840 | 80 |
| Scotland | 100 | 10 |
| Wales | 87 | 8 |
| Northern Ireland | 23 | 2 |
The survey respondents reported a significantly higher degree of anxiety regarding COVID‐19 in comparison with anxiety regarding HF itself (mean 7 ± 2.5 on the anxiety scale vs. 6.1 ± 2.4; P < 0.001). This trend was similar amongst patient sub‐groups based on gender (male HF anxiety score 6.0 ± 2.2 vs. COVID anxiety score 7 ± 2.5, P < 0.001; and female HF anxiety score 6.1 ± 2.4 vs. COVID anxiety score 7 ± 2.4, P < 0.001) as well as age groups that is, patients aged up to 60 years vs. those aged more than 60 years.
Sixty‐five per cent (686/1050) of all respondents reported that their HF appointments were negatively impacted during the lockdown period of the COVID‐19 pandemic with 43% cancellation of scheduled hospital clinic appointments (321/743 appointments) and 22% cancellation of community HF clinic appointments (114/523) (Figure 1 ). Cardiac investigations (echocardiogram, holter monitoring, cardiac magnetic resonance imaging, and cardiac computed tomography scans) or procedures (angioplasty, pacemaker, cardiac bypass operation, and radiofrequency ablation) were also affected with 37% (362 out of 994) appointments cancelled and 46% (460/994) postponed (Figure 2 ). As shown in Figure 2 , the most commonly cancelled investigation was cardiac magnetic resonance imaging (112 reported cancellations), and the most commonly cancelled procedure was pacemaker implantation (38 cancellations). The most commonly postponed investigation was the holter monitor test (101), and the most commonly postponed procedure was pacemaker implantation (60 postponements). The most frequently performed investigation or procedure during this period was echocardiography (117). Twenty‐nine per cent (305/1050) of respondents reported that their appointments for HF counselling were cancelled.
Figure 1.

Outcomes of scheduled heart failure appointments during the lockdown period. (A) hospital and (B) community.
Figure 2.
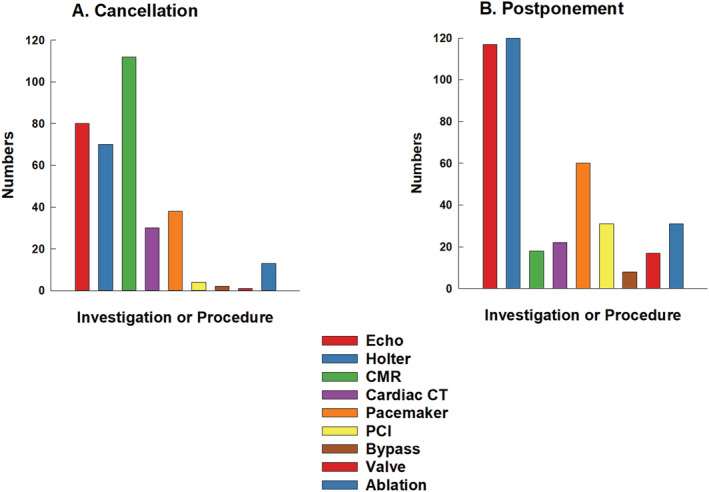
Number of investigations or procedures adversely affected. (A) Cancellation and (B) Postponement. CMR, cardiac magnetic resonance imaging; PCI, pacemaker implantation.
Thirty‐seven per cent (389/1050) of HF patients reported that their medication prescription was adversely affected by the pandemic, and 34% (357/1050) reported that they could not access their HF services/teams promptly. The majority of patients (68%) reported a willingness to attend hospital appointments if required (18% responded that they would have no concerns attending hospital, and 50% stated that they would attend hospital if there were appropriate measures to ensure patient safety, such as social distancing, availability of masks, and hand‐sanitization facilities). However, nearly a third of HF patients surveyed (32%) reported a reluctance to attend hospital (25% stated that they would only attend hospital if there was no alternative, and 7% stated that they would not attend hospital at all).
Respondents were also asked to choose service changes or new models of care that they would prefer to be continued or to be introduced in their local HF services (Figure 3 ). An overwhelming majority (71%) chose the ‘One stop diagnostic HF clinics’, consisting of a single visit incorporating HF consultant review and echocardiography. With regard to alternatives to physical attendance at HF clinics, telephone consultations were more popular (52% preferred this option) in comparison with video consultation (preferred by 34%). Thirty‐six per cent of HF patients stated that they would prefer home intravenous diuretic therapy as an alternative to hospital admission, and 29% preferred ambulatory or outpatient intravenous treatment. Fifty‐one per cent of patients preferred to have their blood pressure, pulse, and weight monitored at home (‘home‐monitoring’).
Figure 3.
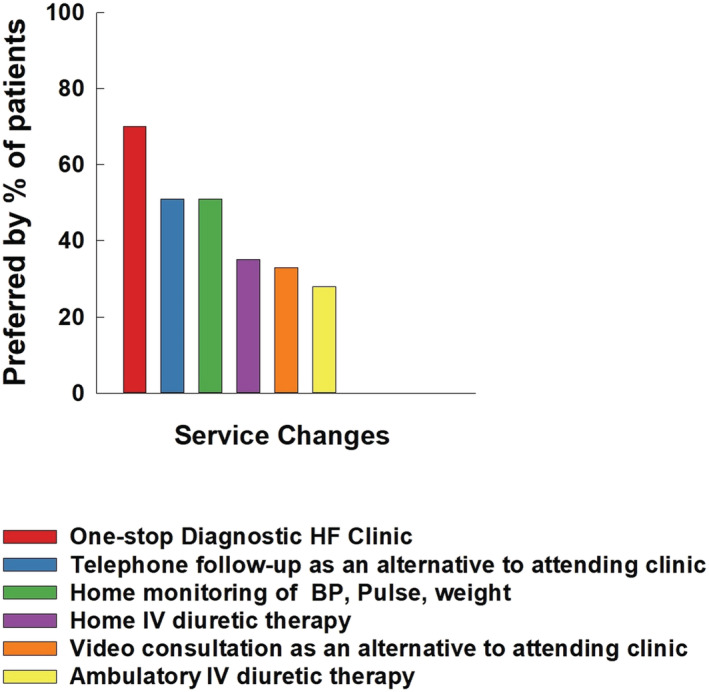
Services chosen by heart failure (HF) patients as preferred to be continued or introduced.
Survey responses were further analysed based on age groups (age ≤60 years vs. >60 years), and this is illustrated in detail in Table 2 and Figure 4. There was a greater degree of anxiety amongst younger patients (aged ≤60 years) vs. older patients (aged >60 years) both for HF (6.3 ± 2.2 vs. 5.9 ± 2.5; P = 0.005) and for COVID‐19 (7.3 ± 2.3 vs. 6.7 ± 2.6; P = 0.0003). Whilst HF patients aged ≤60 years had a higher number of appointments scheduled (2.5 ± 1.6) compared with older patients (1.8 ± 1.2; P < 0.001), younger patients also reported a higher proportion of disruption (cancellations or postponement) to clinic appointments as well as appointments for investigations/procedures in comparison with older patients (73% of patients in the group ≤60 years vs. 59% in the group aged >60 years; P < 0.001). It is therefore possible that the higher degree of anxiety was influenced by the fact that patients aged ≤60 years experienced a significantly higher proportion of appointment cancellations (hospital and community) as well as disruptions to medication prescription or monitoring. Older patients (age >60 years) were extremely wary of attending hospital with 34% opting to only attend hospital if there was no alternative or to not attend hospital at all, in comparison with 26% of patients aged ≤60 years who expressed this view (P = 0.004).
Table 2.
Survey analysis based on age groups (up to 60 years old vs. over 60 years old)
| ≤60 years n = 471/1050 | >60 years n = 579/1050 | P value | |
|---|---|---|---|
| Anxiety about HF (mean ± SD) (0 = no anxiety and 10 = highest anxiety level) | 6.3 ± 2.2 | 5.9 ± 2.5 | 0.005 |
| Anxiety about COVID (mean ± SD) (0 = no anxiety and 10 = highest anxiety level) | 7.3 ± 2.3 HF vs. COVID | 6.7 ± 2.6 HF vs. COVID | 0.0003 |
| Number of appointments scheduled (mean ± SD) | 2.5 ± 1.6 (1179 appointments) | 1.8 ± 1.2 (1081 appointments) | <0.001 |
| Percentage of patients with appointments, investigations, or procedures adversely affected | 73% of patients (344/471) | 59% of patients (342/579) | <0.001 |
| Face‐to face hospital appointments cancelled (% of total appointments) | 48% (190/393) | 37% (131/350) | 0.003 |
| Community appointments cancelled (% of total appointments) | 28% (64/228) | 17% (50/295) | 0.002 |
| Investigation/procedure cancelled (% of total appointments) | 40% (221/558 | 32% (141/436) | 0.04 |
| Investigation/procedure postponed (% of total appointments) | 51% (279/558) | 41% (181/436) | 0.008 |
| Prescription or monitoring affected (% of patients) | 43% (204/471) | 33% (189/579) | <0.001 |
| ‘Don't feel can access services’ (% of patients) | 33% (155/471) | 34% (199/579) | NS |
| Patients willing to attend hospital if required (% of patients) | 73% (345/471) | 66% (381/579) | 0.01 |
| ‘I would have no concerns about attending the hospital’ | 17% (79/471) | 19% (108/571) | |
| ‘I would attend the hospital if there were appropriate measures in place to ensure my safety’ | 56% (266/471) | 47% (273/579) | |
| Patients reluctant to attend hospital | 26% (126/471) | 34% (198/579) | 0.004 |
| ‘Would attend hospital only if no alternative’ | 23% (110/471) | 26% (150/579) | |
| ‘Would never attend hospital’ | 3% (16/471) | 8% (48/579 | |
| Preference for new service models | |||
| Telephone appointment | 56% (264/471) | 49% (282/579) | 0.02 |
| Video consultation | 44% (206/471) | 26% (149/579) | <0.001 |
| Ambulatory i.v. diuretic | 33% (156/471) | 25% (147/579) | 0.005 |
| Home i.v. diuretic | 40% (187/471) | 33% (191/579) | 0.02 |
| Home monitoring | 56% (265/471) | 47% (270/579) | 0.003 |
| One stop HF diagnostic clinic | 75% (354/471) | 67% (387/579) | <0.001 |
| Patients not under care of hospital HF team | 10% | 25% | |
| Patients not under care of community HF team | 29% | 34% | |
HF, heart failure; i.v., intravenous; NS, not significant.
NB. Out of 1050 patient responses, there were 41 instances (3.9%) when the sum of the individual appointments listed did not equal the total number quoted in response to Question 5 of the survey (supporting information). These numbers were similar in the two age groups (24/579 = 4% in the >60 years age group and 17/471 = 3.6% in the <60 years age group). In these instances, the sum of the individual appointments was used for data analysis.
Figure 4.

Age group comparisons [heart failure (HF) patients aged ≤60 years old vs. those aged >60 years old]. (A) Comparison of mean anxiety scores and (B) percentage of appointments of prescription adversely affected.
There was also a significant difference in terms of preference for newer models of HF services between the two age groups compared, with these service changes seemingly less popular amongst older HF patients (aged >60 years).
Discussion
Our questionnaire‐based adult HF patient survey is the first reported study which describes the impact of the COVID‐19 pandemic lockdown period upon HF services from a patient perspective in all four devolved nations in the UK. Our results show high anxiety levels particularly regarding COVID‐19 and especially amongst younger patients. It is likely that this was exacerbated by the cancellation or postponement of a large proportion of clinic appointments (hospital as well as community), elective investigations, and procedures, with the majority of survey respondents (65%) reporting that their HF appointments were adversely affected through cancellation or postponement. Whilst reassuringly the majority of respondents surveyed reported that they felt able to access their HF services, it is of great concern that over a third of patients reported that they had difficulties accessing their local HF services or obtaining HF medications.
A number of studies have shown a significant reduction in admissions due to HF during the 1st peak of COVID‐19. 12 , 14 , 21 As demonstrated by our study, possible reasons for this include a reluctance or unwillingness to attend hospital (this was seen especially amongst the older patient group aged >60 years in our study), due to anxiety amongst HF patients about contracting COVID‐19 in hospital as well as a perception that clinical services were only open to treat COVID‐19 cases. This is reflected in our survey responses, which showed higher anxiety levels regarding COVID‐19 in comparison with anxiety about HF. High anxiety levels have been independently correlated with adverse HF outcomes in previous studies. 22 Interestingly, despite older people having a predilection for more severe COVID‐19 illness, anxiety levels were greater amongst the younger group of patients (aged up to 60 years). This is contrary to the common perception that older patients are likely to experience more anxiety due to a combination of social isolation as well as fear of contracting severe COVID‐19 illness. This paradoxical result may be in part due to the greater degree of disruption to clinic appointments and monitoring, as well as interruption to HF medication prescriptions amongst younger patients. In addition, it is also possible that younger patients feared hospitalization or dying more than older people and were perturbed about the possible impact of COVID‐19 upon their family or dependents such as school‐age children. Other possible reasons for greater apprehension amongst younger HF patients could have been related to specific financial concerns, fear of being made unemployed, or feeling pressurized to work in environments where physical distancing was difficult to achieve.
Patients with a new diagnosis of HF typically undergo an armamentarium of diagnostic investigations, followed by appropriate guideline directed management through timely follow‐up. Cancellation or postponement of these appointments can lead to HF decompensation, worsening of quality of life and also increase patients' anxiety levels regarding accessibility of HF services, risk of hospitalization or dying prematurely thereby triggering a vicious cycle. Delays in optimization of prognostic HF medications, investigations and procedural treatments, are likely to lead to worse HF outcomes such as acute decompensation, worsening of quality of life, and increased mortality.
Significantly, around one third of HF patients in our survey expressed a reluctance to attend hospital (25% stated that they would only attend hospital if there was no alternative and 7% stated that they would not attend hospital at all). The prevalence of this viewpoint was significantly higher amongst the older patient group (aged >60 years). Mixed messages regarding isolation or shielding may have caused confusion, leading to indecision amongst HF patients about accessing healthcare services. This may have contributed to the significantly lower hospital admission rates for HF during the pandemic, 12 , 13 but also to the worse outcomes in the form of higher mortality. 13 It is crucial therefore that healthcare services reach out to all patients, with reassurances that adequate precautions are being taken in healthcare settings (such as physical distancing, use of hand‐washing/sanitizing facilities, and personal protective equipment), in order to minimize the risk of transmission of coronavirus to patients in healthcare settings.
The response to the COVID‐19 pandemic triggered a rapid restructuring of healthcare services with an increased use of and reliance on tele‐cardiology services. The data available on the tele‐management of cardiology patients is conflicting. Whilst some trials have shown beneficial endpoints, 23 , 24 others have suggested a lack of improvement in outcomes. 25 , 26 Our survey results offer the first published report of adult HF patients' opinions regarding the acceptance and preference for ongoing continuation of these newer service models. Overall, the ‘one‐stop diagnostic HF clinic’ was the most popular service preference with over 70% of respondents opting for it to be continued. This concept minimizes the need for repeat HF clinic attendances by incorporating echocardiography and HF specialist review during the same consultation, thereby improving patient convenience and possibly reducing risk of exposure to COVID by minimizing hospital/healthcare facility attendance. This is also the objective of other services such home monitoring (blood pressure, pulse, weight), home treatment or ambulatory treatment with intravenous diuretics and virtual clinics (using telephone or video technology). However, these newer service models appeared to be less popular with patients, particularly with older patients. This is a pivotal finding of the study, with possible far‐reaching consequences because HF patients are frequently elderly and have a significant number of existing co‐morbidities. 27 Virtual or remote consultations can be challenging for healthcare providers to deliver due to the inability to conduct a physical examination, communication barriers with patients who have hearing impairment, reduced opportunity for consultation input from carers, and language barriers. Potential solutions include the use of tele‐health home monitoring of parameters such as pulse, blood pressure, heart rate and weight, educating patients to self‐examine for the presence/absence of fluid overload, and use of multi‐participant teleconference technology or loudspeaker function at the patient facing side of the consultation to help include carers and interpreters in the consultation process. It is therefore crucial that HF services engage with their patients to co‐design and evaluate novel services prior to widespread implementation. This should include a comprehensive understanding of: patient access barriers; acceptability of novel services; patient preferences; and local geographic and socio‐economic challenges that may exist, so that patient care can be delivered with parity.
To date, this is the 1st reported HF patient survey that explores the direct impact of COVID‐19 upon adult HF patient care, from a patient perspective. This study has several strengths including but not limited to a large sample size distributed across 10 hospitals in the UK with inclusion of a wide range of ages from all four nations in the UK. The study also benefits from having been undertaken during the final phases of the UK lockdown. This allowed us to capture a more complete picture of any disruptions that HF patients may have experienced during this time period. Importantly, the results should inform adult HF service transformation and resilience strategies in the event of a second pandemic wave, including the adoption of an approach that maintains elective services for people whose underlying health condition places them at high risk of hospitalization or premature death. Such an approach has the potential to minimize the anxiety and disruption to care, experienced by HF patients.
Limitations
General limitations exist when using a survey questionnaire study model. Such limitations are applicable to this study including the potential for responder bias and a response rate of approximately 15%. As the Survey Working Group, which devised the questionnaire also included three expert HF patients, we did not pre‐test the questionnaire amongst patients prior to dissemination. It is possible that non‐responders experienced no disruption to their appointments during the pandemic or, conversely, that they were either unable to access the technology to complete the survey or were not aware of the survey due to lack of contact with their HF team.
Conclusion
The COVID‐19 pandemic represents a unique inflection point in healthcare provision and required a rapid response from healthcare systems in order to cope with the burgeoning demand created by a new multisystem condition. We are already experiencing further waves of this pandemic across several geographical areas. Our survey results highlight that patients with chronic health conditions such as HF need to feel reassured that healthcare services can respond in a timely and robust manner when treating them, whilst also being able to cope with the burden created by COVID‐19. It is likely that the resulting healthcare disruptions for non‐COVID conditions in multiple countries led to the public concluding that healthcare facilities were ‘COVID‐19 hospitals’ and therefore less able to look after them. This, in combination with a real‐world reduction in services offered, possibly resulted in patients feeling that they could not rely on the services they had previously relied upon and had confidence in. It is important that healthcare authorities regain the trust of patients with chronic conditions such as HF, through firm reassurance that healthcare services are ready and capable of coping with the extra demand created by COVID‐19. However, this requires to be balanced with competing demands on other services. The results of our nationwide HF patient survey should influence the future direction of adult HF care in the event of future waves of COVID‐19 and help optimize service delivery under these exceptional circumstances, in order to minimize disruption to patient care.
Ethics
Our study complies with the Declaration of Helsinki; the research protocol complied with the institutional ethics, and the need for written consent was waived due to complete anonymization of data responses from the time of patients responding to the questionnaire survey to the time of data analysis (i.e. throughout the study).
Conflict of interest
None declared.
Funding
No external sources of funding were used.
Supporting information
Data S1 Supplementary information
Sankaranarayanan, R. , Hartshorne‐Evans, N. , Redmond‐Lyon, S. , Wilson, J. , Essa, H. , Gray, A. , Clayton, L. , Barton, C. , Ahmed, F. Z. , Cunnington, C. , Satchithananda, D. K. , and Murphy, C. L. (2021) The impact of COVID‐19 on the management of heart failure: a United Kingdom patient questionnaire study. ESC Heart Failure, 8: 1324–1332. 10.1002/ehf2.13209.
References
- 1. Gorbalenya AEBSC, Baric RS. The species severe acute respiratory syndrome‐related coronavirus: classifying 2019‐nCoV and naming it SARS‐CoV‐2. Nat Microbiol 2020; 5: 536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cucinotta D, Vanelli M. WHO declares COVID‐19 a pandemic. Acta Biomed 2020; 91: 157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prime Minister's statement on coronavirus (COVID‐19): 22 March 2020. 2020.
- 4. Prime Minister's statement on coronavirus (COVID‐19): 11 May 2020. 2020.
- 5. McIlvennan CK, Allen LA, DeVore AD, Granger CB, Kaltenbach LA, Granger BB. Changes in care delivery for patients with heart failure during the COVID‐19 pandemic: results of a multicenter survey. J Card Fail 2020; 26: 635–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Madjid M, Safavi‐Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020; 5: 831–840. [DOI] [PubMed] [Google Scholar]
- 7. Shah N, Ahmed I, Nazir T. Heart failure‐related hospitalisation and management during the COVID‐19 pandemic: a reflection. Eur J Heart Fail 2020. 10.1002/ejhf.1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, Vaduganathan M. Fewer hospitalizations for acute cardiovascular conditions during the COVID‐19 pandemic. J Am Coll Cardiol 2020; 76: 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pessoa‐Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, Zamorano JL, Weidinger F, Achenbach S, Maggioni AP, Gale CP, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID‐19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes 2020; 6: 210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De RS, Spaccarotella C, Basso C, Calabro MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J 2020; 41: 2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. De FO, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso MW, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa GA, Sardella G, Fedele F, Monticone S, Montefusco A, Omede P, Pennone M, Patti G, Mancone M, de Ferrari GM. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in Northern Italy. N Engl J Med 2020; 383: 88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bromage DI, Cannata A, Rind IA, Gregorio C, Piper S, Shah AM, McDonagh TA. The impact of COVID‐19 on heart failure hospitalization and management: report from a heart failure unit in London during the peak of the pandemic. Eur J Heart Fail 2020; 22: 978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cannata A, Rind IA, Gregorio C, Bannister C, Albarjas M, Piper S, Shah AM, McDonagh TA. Temporal trends in decompensated heart failure and outcomes during COVID‐19: a multisite report from heart failure referral centres in London. Eur J Heart Fail 2020. 10.1002/ejhf.1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Frankfurter C, Buchan TA, Kobulnik J, Lee DS, Luk A, McDonald M, Ross HJ, Alba AC. Reduced rate of hospital presentations for heart failure during the COVID‐19 pandemic in Toronto, Canada. Can J Cardiol 2020; 36: 1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez GA, Moore CK, Lennep BW, McMullan MR, Butler J. Reductions in heart failure hospitalizations during the COVID‐19 pandemic. J Card Fail 2020; 26: 462–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Powis S, Whitty W. 200321_COVID‐19_CMO_MD_letter‐to‐GPs_FINAL_2.pdf. 2020. 2020.
- 17. Guidance on shielding and protecting people who are clinically extremely vulnerable from COVID‐19. 2020.
- 18. Abraham WT, Fiuzat M, Psotka MA, O'Connor CM. Heart failure collaboratory statement on remote monitoring and social distancing in the landscape of COVID‐19. JACC Heart Fail 2020; 8: 692–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The European Society for Cardiology . The European Society for Cardiology. ESC Guidance for the diagnosis and management of CV disease during the COVID‐19 pandemic. 2020.
- 20. Salzano A, D'Assante R, Stagnaro FM, Valente V, Crisci G, Giardino F, Arcopinto M, Bossone E, Marra AM, Cittadini A. Heart failure management during the COVID‐19 outbreak in Italy: a telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail 2020; 22: 1048–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Andersson C, Gerds T, Fosbol E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp‐Pedersen C, Kober L, Schou M. Incidence of new‐onset and worsening heart failure before and after the COVID‐19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 2020; 13: e007274. [DOI] [PubMed] [Google Scholar]
- 22. Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harv Rev Psychiatry 2018; 26: 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, Cartwright M, Rixon L, Knapp M, Henderson C, Rogers A, Fitzpatrick R, Hendy J, Newman S. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ 2012; 344: e3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ferrante D, Varini S, Macchia A, Soifer S, Badra R, Nul D, Grancelli H, Doval H. Long‐term results after a telephone intervention in chronic heart failure: DIAL (Randomized Trial of Phone Intervention in Chronic Heart Failure) follow‐up. J Am Coll Cardiol 2010; 56: 372–378. [DOI] [PubMed] [Google Scholar]
- 25. Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med 2010; 363: 2301–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Bohm M, Boll H, Baumann G, Honold M, Koehler K, Gelbrich G, Kirwan BA, Anker SD. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation 2011; 123: 1873–1880. [DOI] [PubMed] [Google Scholar]
- 27. Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, Rahimi K. Temporal trends and patterns in heart failure incidence: a population‐based study of 4 million individuals. Lancet 2018; 391: 572–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Supplementary information


